Abstract
Summary
In this large-sample study, we demonstrated that osteogenesis imperfecta (OI) significantly impaired the quality of life (QoL) in children. Moderate/severe OI patients had worse QoL scores than patients with mild OI. Furthermore, the QoL for OI patients was correlated with the presence of pathogenic gene mutations.
Introduction
Osteogenesis imperfecta (OI) is a hereditary disease characterized by multiple fragility fractures and progressive skeletal deformities. No detailed investigations about the quality of life (QoL) have been carried out in a large sample of patients with OI. We evaluated the QoL and its influencing factors in a large and well-characterized OI cohort.
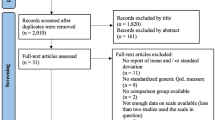
Methods
We used a validated questionnaire of PedsQL 4.0 to evaluate the health-related quality of life (HRQoL) of children and adolescents with OI. We compared HRQoL among patients with OI types I, III, and IV. The relationship between HRQoL and pathogenic mutations in candidate OI genes was investigated. We also evaluated the influencing factors of HRQoL in OI patients.
Results
A total of 138 children with OI and 138 healthy controls were enrolled in this study. The HRQoL scores of OI patients were 64.4 ± 30.0, 71.9 ± 22.2, 75.7 ± 24.8, 63.7 ± 24.5, and 68.9 ± 22.0 in physical, emotional, social, school functioning, and total score, respectively, which were significantly lower than those of healthy children (86.5 ± 12.7, 83.3 ± 16.0, 92.1 ± 11.8, 87.5 ± 11.8, and 87.3 ± 10.7, all p < 0.01). Moderate and severe OI (type III/IV) patients had poorer HRQoL scores than patients with mild OI (type I). Gene mutations inducing qualitative defects in type I collagen led to worse HRQoL scores than those with quantitative defects in type I collagen, except in emotional functioning. The total HRQoL score was positively correlated with family income, lumbar, and femoral bone mineral density (BMD) Z-scores and negatively correlated with disease severity and fracture frequency.
Conclusion
HRQoL was significantly impaired in OI patients, and patients with more severe OI had poorer HRQoL scores. For the first time, we found that children with qualitative defects in type I collagen had poorer HRQoL scores than those with quantitative defects in type I collagen.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteogenesis imperfecta (OI) is an inheritable, collagen-related disease characterized by increased bone fragility and recurrent fractures, with an incidence of 1 in every 15,000–20,000 neonates [1]. Multiple fractures will lead to progressive bone deformities, short stature, and restricted mobility. In 85–90% of cases, OI is mainly caused by mutations in the genes encoding type I collagen (COL1A1 or COL1A2), and these mutations follow an autosomal dominant inheritance pattern [2,3,4,5,6,7]. Mutations in COL1A1 or COL1A2 can lead to haploinsufficiency (with the synthesis of structurally normal collagen at about half the normal amount) or glycine substitution (synthesis and secretion of structurally abnormal collagen). According to the clinical severity and characteristics, OI is classified into five subtypes as follows: non-deforming OI with blue sclerae (type I), perinatally lethal OI (type II), and progressively deforming OI (type III), common variable OI (type IV), as well as OI with calcification in the interosseous membranes (type V) [8].
Moderate to severe OI patients may suffer from recurrent fractures, bone deformity, and ambulation limitation in their early life, which would impair their quality of life (QoL). However, health-related quality of life (HRQoL) in OI patients in China has not been investigated in detail. Large-sample studies have not been performed. OI widely varies in its clinical manifestations and causative pathogenic mutations. Therefore, OI studies to identify whether phenotypes and genotypes are correlated with a poor QoL in OI patients are necessary. Moreover, it is unclear which factors affect the QoL of OI patients.
In this single-center, cross-sectional study, we assessed HRQoL scores in a large cohort of OI children and compared these scores to those from healthy children. We also investigated whether OI patients with different clinical severities had different QoL scores/features, while evaluating the potential influencing factors of QoL, such as demographic status, bone turnover biomarker, bone mineral density (BMD), fracture frequency, pathogenic gene mutations, and bisphosphonate (BP) treatment.
Methods and participants
Participants
This study was conducted from December 2016 to December 2017 in the Department of Endocrinology at Peking Union Medical College Hospital (PUMCH). A total of 138 children with OI from 2 to 18 years old were included, who were clinically diagnosed according to the following criteria: presence of a family history of OI, a history of more than one fracture under minor trauma and an age- and sex-adjusted BMD Z-score less than − 1.0 at either the lumbar spine or femoral neck, or absence of a family history with a typical history of low-trauma fractures in childhood, with at least one symptom or sign of OI, such as blue sclera, dentinogenesis imperfecta, and abnormal laxity of the ligaments [9]. Patients who suffered from new fractures in recent 3 months or had nonunion fractures were excluded.
The study was approved by the scientific ethics committee of Peking Union Medical College Hospital. All parents or guardians of OI patients provided written informed consent prior to participation in this study.
Evaluation of health-related quality of life
HRQoL was assessed by PedsQL version 4.0 questionnaire (Chinese version, http://pedsql.org), which is a validated multidimensional measure of QoL for children and adolescents. PedsQL 4.0 consisted of 23 questions covering four domains, including physical, emotional, social, and school functioning. The items were scored from 0 to 100, and higher scores indicated a better HRQoL. The missing data were replaced by the average scores of the completed items if at least half of the items in the actual scale were answered. The PedsQL Measurement Model consisted of developmentally appropriate forms for children ages 2–4, 5–7, 8–12, and 13–18 years old. Pediatric self-report was measured in children and adolescents ages 5–18 years old, and parent proxy-report of child HRQoL was measured for children and adolescents ages 2–18 years old.
We also assessed HRQoL in a control group that consisted of 138 age- and gender-matched healthy Chinese children. All of them came from local kindergartens and schools in the Shandong province.
Evaluation of phenotypes of OI
General information was collected including residence (in an urban or rural area), educational status of the parents (including primary school, junior middle school, senior middle school, or undergraduate), and annual family income.
Clinical information concerning OI was carefully collected including the condition of bone, dentin, joint, and sclerae. Fractures were suspected by medical history and confirmed by X-ray films of bone. A positive family history of bone fracture was investigated. OI patients were clinically classified into mild (type I), moderate (type IV), or severe (type III) according to the Sillence classification [8].
Fasting blood samples were acquired for the biochemical analysis. Serum levels of calcium (Ca), phosphate (P), and alkaline phosphatase (ALP) were measured by an automatic biochemical analyzer. Serum concentrations of parathyroid hormone (PTH), 25 hydroxy-vitamin D (25OHD), and β-cross-linked C-telopeptide of type I collagen (β-CTX, a bone resorption marker) were determined by an automated Roche electrochemiluminescence system (Roche Diagnostics, Switzerland) at the central laboratory of PUMCH.
Bone mineral density (BMD) at the lumbar spine (LS), femoral neck (FN), and total hip (TH) was measured by dual-energy X-ray absorptiometry (DXA, Lunar Prodigy, USA) at the Department of Radiology of PUMCH, with appropriate pediatric software. Then, we transformed BMD data to age- and gender-adjusted Z-scores according to the normal reference BMD in Asian children [10]. X-ray films of the skull, thoracolumbar spine, pelvis, and lower extremities were examined to evaluate bone deformity and bone fracture.
Patients received intravenous infusion of zoledronic acid (5 mg yearly), or oral alendronate (70 mg weekly), or no medication. All patients were supplemented with calcium (500 mg) and vitamin D3 (200 IU daily).
Detection of pathogenic mutations
Genomic DNA was extracted from the peripheral blood leukocytes of OI patients and 100 unaffected healthy individuals under the standard protocols using a DNA Extraction Kit (QIAamp DNA, Qiagen, Germany). A next-generation sequencing (NGS)-based panel (Illumina HiSeq2000 platform, Illumina, Inc., San Diego, CA, USA) was developed by our research team, covering all exons of 19 genes related to OI, including COL1A1, COL1A2, BMP1, CREB3L1, CRTAP, FKBP10, IFITM5, LEPRE1, P4HB, PLOD2, PPIB, PLS3, SEC24D, SERPINF1, SERPINH1, SP7, SPARK, TMEM38B, and WNT1 [11,12,13,14]. The sequencing was performed to 98.95% coverage for a mean depth of 200× on target regions in each of the chromosomes. NGS data was analyzed according to a protocol that was described previously [11]. Mutations identified by NGS were further confirmed by Sanger sequencing and co-segregation analysis. Variants including missense mutations, nonsense mutations, frame shift mutations, and splice site mutations were expected to be pathogenic. The pathogenicity of missense mutations causing substitution of amino acids was predicted with Polyphen2 software (http://genetics.bwh.harvard.edu/pph2/). The pathogenicity of splice site mutations was predicted utilizing NNSPLICE0.9 (http://www.fruitfly.org/) and Human Splicing Finder (http://www.umd.be/HSF3/HSF.html). Mutations causing an early stop codon or frameshift in COL1A1 were considered quantitative mutations of type I collagen, namely haploinsufficiency. Mutations leading to amino acid substitutions in the triple helical domain of COL1A1 or COL1A2 were regarded as qualitative changes in type I collagen.
Statistical analysis
The general characteristics of the patients were expressed using descriptive statistics. For continuous variables, mean ± standard deviation (SD) was recorded. For categorical variables, the percentage of each group was presented. The comparison between OI patients and healthy controls was performed using an independent sample t test and chi-square tests. The correlation between HRQoL scores in OI patients and multiple variables was analyzed by a Spearman correlation coefficient test.
p values less than 0.05 were considered to be statistically significant. All statistical analyses were carried out using SPSS 24.0 software (SPSS Inc., Chicago, IL, USA).
Results
General characteristics of children with OI
The general characteristics of OI patients and healthy controls are shown in Table 1. A total of 138 children with OI were included, with an average age of 10.0 ± 4.4 years old. The educational levels of the parents of OI patients were primary school (3.5%), junior middle school (39.1%), senior middle school (22.6%), undergraduate, or higher (34.8%). Notably, the annual family income was significantly lower in patients with OI than in healthy children, and 21% of the families with a child with OI had an income less than 2890 USD (≈ 20,000 RMB) per year (p < 0.001). There were no significant differences in age, gender, place of residence, or parents’ educational level between OI patients and healthy controls.
Clinical phenotypes of OI patients
The clinical characteristics of OI patients are shown in Table 2. There were 73, 30, and 35 children with types I, III, and IV OI, respectively. The average bone fracture frequency was 1.5 ± 1.5 per year. The total bone fracture frequency was 3.5 ± 2.0, 10.0 ± 7.1, and 5.7 ± 2.9 for OI type I, III, and IV, respectively. Seventy-five percent of OI patients could walk independently, and 25% patients were in wheelchairs. The majority of patients (86.1%) had blue sclera, 51.0% had hypermobility of the joints, and 20.9% had dentinogenesis imperfecta. Forty-nine percent of the patients had a positive family history of OI. Seventy-seven percent of patients received bisphosphonate treatment, with an average treatment course of 2.5 years.
Serum levels of Ca, P, 25OHD, and PTH were within age-matched normal ranges. At the time of performing the questionnaires, patients in the BPs-treatment group underwent an average of 2.5 ± 1.7 years’ drug treatment, and their BMD Z-scores at the LS and FN were in the normal range (1.0 ± 2.0 and 0.0 ± 2.3, respectively) after BPs treatment. The average BMD Z-scores at the LS and FN of the non-BPs-treatment group were − 2.2 ± 1.1 and − 3.5 ± 2.2, respectively.
Genotypes of OI patients
In this cohort, 117 patients underwent molecular analysis, and 111 patients were identified to carry causative mutations of OI, including mutations in COL1A1 (n = 65), COL1A2 (n = 28), IFITM5 (n = 8), SERPINF1 (n = 3), TMEM38B (n = 2), WNT1 (n = 2), SERPINH1 (n = 1), PLOD2 (n = 1), and PLS3 (n = 1). We identified 101 patients with autosomal dominant (AD) inherited OI, 9 patients with autosomal recessive (AR) inherited OI, and 1 patient with X-linked inherited OI. Among these patients, COL1A1 and COL1A2 mutations included 43 missense mutations, 12 nonsense mutations, 23 splice site mutations, 13 frameshift mutations, 1 microdeletion, and 1 chromosome translocation. There were 24 haploinsufficiency mutations and 42 glycine substitutions in the triple helical domains. Detailed information concerning these pathogenic gene mutations is shown in Fig. 1.
HRQoL of OI patients
The results of HRQoL are shown in Figs. 2, 3, and 4. HRQoL scores of OI patients and healthy controls respectively were 64.4 ± 30.0 vs. 86.5 ± 12.7 in physical functioning, 71.9 ± 22.2 vs. 83.3 ± 16.0 in emotional functioning, 75.7 ± 24.8 vs. 92.1 ± 11.8 in social functioning, 63.7 ± 24.5 vs. 87.5 ± 11.8 in school functioning, and 68.9 ± 22.0 vs. 87.3 ± 10.7 in total score (all p < 0.001) (Fig. 2). OI patients had significantly lower HRQoL scores in all domains than healthy controls. In clinical subgroup analysis, the physical function was 74.9 ± 22.1, 48.6 ± 36.3, and 56.0 ± 30.7 in OI types I, III, and IV patients, respectively, which indicated that mild OI patients (type I) had better physical QoL scores than moderate OI (type IV) and severe OI (type III) patients (p < 0.01). Compared with OI type I patients, OI type IV patients had lower QoL scores in the social and school domains, and OI type III patients had lower QoL scores in the emotional and social domains. No significant differences were found in all domains of HRQoL between type III and type IV OI patients (all p > 0.05) (Fig. 3).
Comparison of HRQoL scores between subgroups of OI. a Comparison of HRQoL scores between patients of AD and AR + XL inheritance, b comparison of HRQoL scores between patients with COL1A1 and COL1A2 mutations, c comparison of HRQoL scores between patients with haploinsufficiency and amino acid substitution in type I collagen. AD, autosomal dominant; AR, autosomal recessive; XL, X chromosome linked. Significant differences were illustrated by **p < 0.01 or *p < 0.05. The error bars indicate the standard deviation
HRQoL scores did not significantly differ between male and female OI patients, and between patients from rural and urban areas (all p > 0.05). The BP and non-BP treatment group had the same component ratio in OI types I, III, and IV (Supplemental Fig. 1). There were no significant differences in all domains of HRQoL between the BP and non-BP treatment group (Supplemental Fig. 2, all p > 0.05).
The relationship between HRQoL and genotypes of OI was further investigated. Patients with qualitative defects in type I collagen had poorer HRQoL scores in all domains than those with quantitative defects in type I collagen, except for emotional functioning (75.8 ± 23.3 vs. 63.2 ± 30.8 in physical functioning, 78.1 ± 19.5 vs. 70.7 ± 23.4 in emotional functioning, 86.9 ± 20.1 vs. 70.6 ± 28.1 in social functioning, and 74.7 ± 24.7 vs. 58.0 ± 25.1 in school functioning, and 78.9 ± 19.4 vs. 65.6 ± 23.8 in total score, p = 0.047, 0.194, 0.008, 0.011, 0.023, respectively) (Fig. 4c, Table 1S). Moreover, no differences were found in the HRQoL scores between autosomal dominant, autosomal recessive, and X-linked inheritance of OI, as well as between COL1A1 and COL1A2 mutations (Fig. 4a, b).
Possible factors influencing HRQoL in OI patients
Family income, height Z-score, LS BMD Z-score, FN BMD Z-score, severity of OI, and fracture frequency was correlated with HRQoL scores in OI patients. Family income was correlated with total score (R = 0.240, p = 0.020), physical functioning (R = 0.247, p = 0.016), and social functioning (R = 0.284, p = 0.006). Z-score of height was correlated with total score (R = 0.319, p = 0.001), physical functioning (R = 0.239, p = 0.005), social functioning (R = 0.371, p < 0.001), and school functioning (R = 0.295, p = 0.001). Z-score of LS and FN BMD were both correlated with total score (R = 0.260, p = 0.004; R = 0.351, p < 0.001, respectively), physical functioning (R = 0.320, p < 0.001; R = 0.398, p < 0.001), and social functioning (R = 0.203, p = 0.026; R = 0.333, p < 0.001). Moreover, the LS BMD Z-score was correlated to school functioning (R = 0.274, p = 0.003). Severity of OI was negatively correlated with all domains of HRQoL, especially total score (R = − 0.390, p < 0.001). Fracture frequency was negatively correlated with total score (R = − 0.284, p = 0.001), physical functioning (R = − 0.221, p = 0.014), social functioning (R = − 0.294, p = 0.001), and school functioning (R = − 0.230, p = 0.011). However, serum levels of 25OHD, PTH, ALP, and β-CTX were not correlated to any HRQoL domain.
Discussion
In this study, we performed a detailed investigation into the HRQoL scores of a large cohort of OI children and evaluated the factors that influence the quality of life. We found that HRQoL was remarkably impaired in OI children across all domains, and patients with more severe OI had poorer HRQoL scores. We found for the first time that the pathogenic genotype of OI was correlated with the HRQoL scores of patients, and patients with structural changes in type I collagen had poorer HRQoL scores than those with quantitative defects in type I collagen.
As far as we know, there are very few studies focusing on quality of life in OI patients [15,16,17,18]. As reported by Fano and Vanz, patients with OI had impaired physical functioning in HRQoL, and patients with severe phenotypes had poorer HRQoL values than those with mild OI [19, 20]. Bone pain, scoliosis, and activity limitations were postulated to be related to worse physical QoL scores [21]. Consistent with previous findings, we found that physical functions were significantly impaired in OI patients, and the disease severity was correlated to HRQoL scores. We also found that physical functions were positively correlated to family income, height Z-score, BMD Z-score at the LS and FN, and negatively correlated to disease severity and fracture frequency in OI patients.
It remained uncertain whether OI affected mental, social, and school functions. Several studies reported no significant impairment in social function and happiness scores in children with OI [22,23,24,25]. However, children with OI type III were reported to have lower scholastic, friendship, and romance competencies [22]. Another study reported a more substantial decrease in the social functioning of children with OI type III/IV than those with OI type I [19]. Patients with OI were reported to experience various degrees of negative feelings in “isolation by peers,” “fear of fractures,” and “difficulty in coping with challenges” [26]. In this study, we found that OI significantly impaired physical, emotional, and school functioning in OI patients. Patients with moderate/severe OI had worse HRQoL scores than patients with mild OI. This indicated that OI patients with physical disabilities could consequently have low levels of well-being and life satisfaction. Therefore, we should pay more attention to the mental and social status of OI patients.
Bisphosphonates are widely used to treat bone fragility in OI patients, which can increase bone mineral density and reduce bone fracture risks [27,28,29]. A previous study found that one treatment cycle (6 months) of zoledronate infusion did not significantly improve HRQoL scores [30]. Another small sample study in OI children found that denosumab treatment could increase BMD, but bone pain and the QoL of the patients were not improved [31]. A recent study compared quality of life, functional, and bone outcomes in OI patients that underwent BP therapy in childhood versus those undergoing BP treatment in adulthood. Results suggested that treatment with BPs at an earlier age improved physical activity, particularly in less severe forms of OI, but may not alter overall quality of life [32]. Similar with previous studies, we found that there was no difference in QoL in the BP versus and non-BP treated group. However, we did not prospectively evaluate the effects of BP treatment on the QoL of OI patients in this cross-sectional study. Whether BPs could improve HRQoL scores in OI patients requires further investigative in a prospective, randomized controlled, long-term study.
So far, no studies have focused on the relationship between pathogenic gene mutations and HRQoL scores in OI patients. We demonstrated for the first time that patients with qualitative mutations in type I collagen had poorer HRQoL scores than patients with quantitative mutations in type I collagen. Quantitative defects in type I collagen always led to a milder OI phenotype. However, qualitative mutations could result in more severe phenotypes of OI [11, 33]. Therefore, we speculated that the lower HRQoL scores in patients with qualitative defects are likely due to the more severe OI phenotypes, including more frequent fractures, more severe bone deformity, and activity constraints. Furthermore, although patients with COL1A1 mutations had higher scores (in all domains) than those with COL1A2 mutations, these differences were not statistically significant. However, since COL1A1 and COL1A2 play different functions in the biosynthesis of collagen, whether COL1A1 and COL1A2 mutations lead to different severities and QoL scores requires further investigation.
There were several strengths in our study. For one, we studied a large sample of patients, where we determined HRQoL scores in many OI patients. We reported for the first time that an OI patient’s quality of life is correlated to the types of mutations in genes related to OI. We also evaluated the possible factors that influence HRQoL scores, which would be useful to improve the quality of life in OI patients. However, there were also limitations in this study. First, due to the lack of a disease-specialized questionnaire, we utilized a generalized questionnaire of PedsQL to assess HRQoL in OI patients. A specialized questionnaire pertinent to OI or other skeletal diseases needs to be established. Second, this was a cross-sectional study, which could not prospectively evaluate the effects of BP treatment on HRQoL scores in OI patients and could not avoid a degree of bias. Third, differences in social status may introduce bias in the QoL score. However, the reason for the difference in social status was probably that 85–90% of OI patients acquired their OI through autosomal dominant inheritance, and our patients’ parents may also suffer from OI, which affects their ability to work and earn money.
In summary, in this large-sample study, we demonstrated that OI significantly impaired HRQoL scores in OI children. Moderate/severe OI patients had worse HRQoL scores than patients with mild OI. HRQoL scores in OI patients were closely correlated to pathogenic gene mutations, and patients with qualitative mutations in type I collagen had poorer HRQoL scores than those with quantitative changes in the amount of type I collagen. HRQoL scores were also correlated with many factors, including family income, height Z-score, BMD Z-scores at the lumbar spine and femoral neck, disease severity, and fracture frequency.
References
Marini JC, Forlino A, Bächinger HP, Bishop NJ, Byers PH, Paepe A, Fassier F, Fratzl-Zelman N, Kozloff KM, Krakow D, Montpetit K, Semler O (2017) Osteogenesis imperfecta. Nat Rev Dis Primers 3:17052
Lim J, Grafe I, Alexander S, Lee B (2017) Genetic causes and mechanisms of osteogenesis imperfecta. Bone 102:40–49
Marini JC, Reich A, Smith SM (2014) Osteogenesis imperfecta due to mutations in non-collagenous genes. Curr Opin Pediatr 26(4):500–507
Song Y, Zhao D, Xu X, Lv F, Li L, Jiang Y, Wang O, Xia W, Xing X, Li M (2018) Novel compound heterozygous mutations in SERPINH1 cause rare autosomal recessive osteogenesis imperfecta type X. Osteoporos Int 29(6):1389–1396
Xu XJ, Lv F, Liu Y, Wang JY, Ma DD, Asan WJW, Song LJ, Jiang Y, Wang O, Xia WB, Xing XP, Li M (2017) Novel mutations in FKBP10 in Chinese patients with osteogenesis imperfecta and their treatment with zoledronic acid. J Hum Genet 62(2):205–211
Barbirato C, Trancozo M, Rebouças MR, Sipolatti V, Nunes VR, Paula F. (2016) Analysis of FKBP10, SERPINH1, and SERPINF1 genes in patients with osteogenesis imperfecta. Genet Mol Res 15(3): gmr.15038665
Eyre DR, Weis MA (2013) Bone collagen: new clues to its mineralization mechanism from recessive osteogenesis imperfecta. Calcif Tissue Int 93(4):338–347
Sillence DO, Senn A, Danks DM (1979) Genetic heterogeneity in osteogenesis imperfecta. J Med Genet 16:101–116
Bradbury LA, Barlow S, Geoghegan F, Hannon RA, Stuckey SL, Wass JA, Russell RG, Brown MA, Duncan EL (2012) Risedronate in adults with osteogenesis imperfecta type I: increased bone mineral density and decreased bone turnover, but high fracture rate persists. Osteoporosis Int 23:285–294
Khadilkar AV, Sanwalka NJ, Chiplonkar SA, Khadilkar VV, Mughal MZ (2011) Normative data and percentile curves for dual energy X-ray absorptiometry in healthy Indian girls and boys aged 5-17 years. Bone 48(4):810–819
Liu Y, Asan MD, Lv F, Xu X, Wang J, Xia W, Jiang Y, Wang O, Xing X, Yu W, Wang J, Sun J, Song L, Zhu Y, Yang H, Wang J, Li M (2017) Gene mutation spectrum and genotype-phenotype correlation in a cohort of Chinese osteogenesis imperfecta patients revealed by targeted next generation sequencing. Osteoporos Int 28(10):2985–2995
Lv F, Xu X, Song Y, Li L, Asan WJ, Yang H, Wang O, Jiang Y, Xia W, Xing X, Li M (2018) Novel mutations in PLOD2 cause rare Bruck syndrome. Calcif Tissue Int 102(3):296–309
Wang JY, Liu Y, Song LJ, Lv F, Xu XJ, San A, Wang J, Yang HM, Yang ZY, Jiang Y, Wang O, Xia WB, Xing XP, Li M (2017) Novel mutations in SERPINF1 result in rare osteogenesis imperfecta type VI. Calcif Tissue Int 100(1):55–66
Liu Y, Wang J, Ma D, Lv F, Xu X, Xia W, Jiang Y, Wang O, Xing X, Zhou P, Wang J, Yu W, ASAN LM (2016) Osteogenesis imperfecta type V: genetic and clinical findings in eleven Chinese patients. Clin Chim Acta 462:201–209
Dogba MJ, Bedos C, Durigova M, Montpetit K, Wong T, Glorieux FH, Rauch F (2013) The impact of severe osteogenesis imperfecta on the lives of young patients and their parents—a qualitative analysis. BMC Pediatr 13:153
Edwards TC, Patrick DL, Topolski TD (2003) Quality of life of adolescents with perceived disabilities. J Pediatr Psychol 28:233–241
Engelbert RH, Uiterwaal CS, Gerver WJ, van der Net JJ, Pruijs HE, Helders PJ (2004) Osteogenesis imperfecta in childhood: impairment and disability. A prospective study with 4-year follow-up. Arch Phys Med Rehab 85:772–778
Hill CL, Baird WO, Walters SJ (2014) Quality of life in children and adolescents with osteogenesis imperfecta: a qualitative interview based study. Health Qual Life Outcomes 2014; 12:54
Fano V, del Pino M, Rodríguez Celin M, Buceta S, Obregón MG (2013) Osteogenesis imperfecta: quality of life in children. Arch Argent Pediatr 111(4):328–331
Vanz AP, van de Sande Lee J, Pinheiro B, Zambrano M, Brizola E, da Rocha NS, Schwartz IVD, de Souza Pires MM, Félix TM (2018) Health-related quality of life of children and adolescents with osteogenesis imperfecta: a cross-sectional study using PedsQL™. BMC Pediatr 18(1):95
Dahan-Oliel N, Oliel S, Tsimicalis A (2016) Quality of life in osteogenesis imperfecta: a mixed-methods systematic review. Am J Med Genet A 170A(1):62–76
Engelbert RH, Custers JW, van der Net J (1997) Functional outcome in osteogenesis imperfecta: disability profiles using the PEDI. Pediatr Phys Ther 9(1):18–22
Engelbert RH, van der Graaf Y, van Empelen R, Beemer FA, Helders PJ (1997) Osteogenesis imperfecta in childhood: impairment and disability. Pediatrics 99(2):E3
Montpetit K, Dahan-Oliel N, Ruck-Gibis J, Fassier F, Rauch F, Glorieux F (2011) Activities and participation in young adults with osteogenesis imperfecta [comparative study]. J Pediatr Rehabil Med 4(1):13–22
Sousa T, Bompadre V, White KK (2014) Musculoskeletal functional outcomes in children with osteogenesis imperfecta: associations with disease severity and pamidronate therapy. J Pediatr Orthop 34(1):118–122
Tsimicalis A, Denis-Larocque G, Michalovic A, Lepage C, Williams K, Yao TR, Palomo T, Dahan-Oliel N, Le May S, Rauch F (2016) The psychosocial experience of individuals living with osteogenesis imperfecta: a mixed-methods systematic review. Qual Life Res 25:1877–1896
Lindahl K, Kindmark A, Rubin CJ, Malmgren B, Grigelioniene G, Söderhäll S, Ljunggren Ö, Åström E (2016) Decreased fracture rate, pharmacogenetics and BMD response in 79 Swedish children with osteogenesis imperfecta types I, III and IV treated with Pamidronate. Bone 87:11–18
Dwan K, Phillipi CA, Steiner RD, Basel D (2014) Bisphosphonate therapy for osteogenesis imperfecta. Cochrane Database Syst Rev D5088
Marginean O, Tamasanu RC, Mang N, Mozos I, Brad GF (2017) Therapy with pamidronate in children with osteogenesis imperfecta. Drug Des Devel Ther 11:2507–2515
Tsimicalis A, Boitor M, Ferland CE, Rauch F, Le May S, Carrier JI, Ngheim T, Bilodeau C (2018) Pain and quality of life of children and adolescents with osteogenesis imperfecta over a bisphosphonate treatment cycle. Eur J Pediatr 177(6):891–902
Hoyer-Kuhn H, Stark C, Franklin J, Schoenau E, Semler O (2017) Correlation of bone mineral density on quality of life in patients with osteogenesis imperfecta during treatment with denosumab. Pediatr Endocrinol Rev 15(Suppl 1):123–129
Feehan AG, Zacharin MR, Lim AS, Simm PJ (2018) A comparative study of quality of life, functional and bone outcomes in osteogenesis imperfecta with bisphosphonate therapy initiated in childhood or adulthood. Bone 113:137–143
Lin HY, Chuang CK, Su YN, Chen MR, Chiu HC, Niu DM, Lin SP (2015) Genotype and phenotype analysis of Taiwanese patients with osteogenesis imperfecta. Orphanet J Rare Dis 10:152
Acknowledgments
We thank the staff in the radiology department for measurement of the bone mineral density and interpretation of X-ray films of bone. We also thank the patients with OI and healthy children for completing the questionnaires.
Funding
This study was supported by National Natural Science Foundation of China (No. 81570802), the National Key Research and Development Program of China (No. 2016YFC0901501), and CAMS Initiative for Innovative Medicine (2016-I2M-3-003).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the scientific ethics committee of Peking Union Medical College Hospital.
Conflicts of interest
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Song, Y., Zhao, D., Li, L. et al. Health-related quality of life in children with osteogenesis imperfecta: a large-sample study. Osteoporos Int 30, 461–468 (2019). https://doi.org/10.1007/s00198-018-4801-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-018-4801-5