Abstract
Osteoporosis-related hip fractures represent a substantial cause of mortality and morbidity in industrialized countries like Austria. Identification of groups at high risk for mortality after hip fracture is crucial for health policy decisions. To determine in-hospital, long-term, and excess mortality after osteoporosis-related hip fracture in Austrian patients, we conducted a retrospective cohort analysis of pseudonymized invoice data from Austrian social insurance authorities covering roughly 98 % of the entire population. The data set included 31,668 subjects aged 50 years and above sustaining a hip fracture between July 2008 and December 2010 with follow-up until June 2011, and an age-, gender-, and regionally matched control population without hip fractures (56,320 subjects). Kaplan–Meier and Cox hazard regression analyses served to determine unadjusted and adjusted mortality rates: Unadjusted all-cause 1-year mortality amounted to 20.2 % (95 % CI: 19.7–20.7 %). Males had significantly higher long-term, in-hospital, and excess mortality rates than females, but younger males exhibited lower excess mortality than their female counterparts. Advanced age correlated with increased long-term and in-hospital mortality, but lower excess mortality. Excess mortality, particularly in males, was highest in the first 6 months after hip fracture, but remained statistically significantly elevated throughout the observation period of 3 years. Longer hospital stay per fracture was correlated with mortality reduction in older patients and in patients with more subsequent fractures. In conclusion, more efforts are needed to identify causes and effectively prevent excess mortality especially in male osteoporosis patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Being a source of substantial morbidity and mortality, in particular among the elderly, hip fractures represent a significant public health concern [1, 2]. Osteoporosis-related bone loss and deterioration of bone quality with advancing age are the main cause of non-traumatic hip fractures [3, 4]. Whereas a decline in hip fracture incidence rates has been reported for a number of countries during the past years including Austria [5–8], mortality after fracture has remained consistently high [2, 9]. Both incidence and mortality rates follow a geographical pattern suggesting a north-south gradient with the highest risk reported from Northern Europe and North America [2, 10]. Thus, 1-year mortality rates have recently been described to range from 14 to 36 % [11]. Excess mortality rates, i.e., mortality among hip fracture patients as compared to that among the matched general population, were demonstrated to decrease dramatically during the first half year following fracture and remain elevated thereafter even after 10 years in some studies [12, 13]. Other investigations focusing on institutionalized patients, however, found no significant excess mortality already after 6 months [14, 15]. In addition, excess mortality following hip fracture was found to be inversely correlated with age [16].
Apart from advanced age and male gender, several comorbidities such as end-stage kidney disease, shock due to the fracture event, cardiac disease, congestive heart failure, and chronic liver disease have recently been determined as risk factors [16–18]. Consistently, a recent meta-analysis found a Charlson comorbidity index score of at least one, an American Society of Anesthesiologists score of at least three, and dementia predicted elevated mortality risk following hip fracture [19]. On the other hand, hip fracture itself was described to predict excess mortality independently from comorbidities and known hip fracture risk factors [20].
Previous epidemiologic studies in Austria on hip fracture reported short-term in-hospital mortality only [21, 22]. Therefore, we performed a comprehensive, retrospective nation-wide study, based on personalized data retrieved from social insurance registries from more than 31,000 elderly hip fracture patients and 56,000 controls to determine in-hospital mortality as well as long-term absolute and excess mortality.
Methods
Study Design and Patients
In this retrospective nation-wide study, pseudonymized patient data were retrieved from thirteen Austrian social insurance authorities covering roughly 98 % of the entire population, using as database program SAS, version 9.3 (SAS Institute Inc., Cary, North Carolina, USA). We identified 31,668 inpatients aged 50 years and above having sustained a hip fracture between July 2008 and December 2010. Follow-up data on survival were available until June 2011. Baseline characteristics of the study population are shown in Table 1. Mean follow-up time after release from hospital upon first fracture recorded in the study period (the index fracture) was 528 days (95 % CI: 524–531 days). Diagnosis of hip fractures was in agreement with the ICD-10 definition S72 [23]. Information on sex, age at hospital discharge from index fracture, residence, subsequent fractures, date of death, and hip fracture-related length of hospital stay was available. Furthermore, 56,320 individuals without hip fractures matched for age, sex, and residency served as control population, whose mean follow-up time was 964 days (95 % CI: 962–966 days). Recruitment of control subjects was performed using the “ranuni” function which is a tool implemented in the SAS statistical software, version 9.3 (SAS Institute Inc., Cary, North Carolina, USA). This function generated a uniform distribution on the interval (0, 1) covering all persons in our database who were registered by Austrian social insurance authorities, with the exclusion of individuals without a history of hip fracture.
Data Analysis
Kaplan–Meier survival analysis identified crude all-cause mortality rates, and Cox hazard regression modeling yielded mortality rates adjusted for age, gender, number of fractures, and hip fracture-related hospital days per fracture. Validity of the proportional hazard assumption was verified in all instances by log-minus-log representations of hazards over time. The χ 2, Fisher´s exact as well as Mann–Whitney U tests, where appropriate, informed on differences that, at a confidence level of 95 %, were considered statistically significant. All analyses were conducted in SPSS, version 19 (SPSS Inc., Chicago, Illinois, USA).
Crude and excess all-cause mortality rates were calculated for two time points of reference: Embarking on directly obtainable dates of hospital discharge after first fracture in our study disregarded those patients who died in hospital upon first fracture. On the other side, hospital admission dates, equaling dates of first fracture, were ascertainable from hip fracture-related hospital days only for those patients who sustained no more than one fracture within the study interval (24,902 of 31,668, corresponding to 78.6 %; Table 1), because records of hip fracture-related hospital days were available in total only. To allow also for patients with ≥2 fractures in the study interval (maximum: 22 fractures), median hospital days contingent upon patient age and gender were calculated for each number of fractures (Online Resource, supplemental Table 1), which served to assess the proportion of hospital days assigned to each fracture. Rounded hospital days pertaining to the first fracture were thus subtracted from the known date of hospital discharge, resulting in an estimate of the date of first fracture for patients with ≥2 fractures.
Results
Table 1 lists baseline characteristics of the fracture study population. Most female hip fracture patients were aged 85–89 years, whereas most males were 80–84 years. With respect to number of fractures, gender proportions were similar regardless of number of fractures. However, χ 2 analysis revealed a statistically significant difference (P < 0.001) between patients with only one fracture and those with more fractures (not shown). Patients sustaining a hip fracture stayed a mean of 22.0 (SD: 16.4) days in hospital (median 16 days (IQR: 17); Online Resource, supplemental Table 1). Women stayed significantly longer in hospital than men overall (median 17 days (IQR: 17) vs 16 days (IQR: 16), P < 0.001), which was particularly reflected by patients between 65 and 89 years at hospital discharge after index fracture. Overall and for both genders, peak age for hospital days was between 75 and 84 years, i.e., up to a median of 18 days (IQR: 18) corresponding to a mean of 23.8 (SD: 17.4) days among female patients aged 75–79.
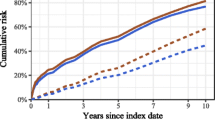
Cumulative hazards for mortality following hospital admission upon index fracture are shown in Fig. 1: Overall, 1-year mortality rates in women and men were 18.6 % (95 % CI: 18.1–19.1 %) and 24.5 % (95 % CI: 23.6–25.5 %), respectively (Fig. 1; Online Resource, supplemental Table 2). Online Resource, supplemental Table 2 provides detailed information on cumulative all-cause mortality rates of various time intervals from 30 days to two and a half years after both first hospital discharge and date of first admission (estimated for ≥2 fractures from hip fracture-related hospital days). As expected, cumulative mortality increases in both women and men over time, and at all time points, men are more prone to death than women (Fig. 1; Online Resource, supplemental Table 2). Furthermore, mortality sharply increases above 80 years in women and 75 years in men (Table 2).
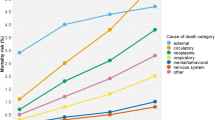
In-hospital mortality was analyzed for all fractures occurring during the study period (Table 3), amounting to overall 3.6 % (95 % CI: 3.4–3.8 %) and 4.0 % (95 % CI: 3.8–4.3 %) at first and last fracture, respectively. Male patients had an elevated mortality rate (P < 0.001) at both their first (5.1 %, 95 % CI: 4.6–5.6 %) and last fracture (5.7 %, 95 % CI: 5.2–6.2 %). Reported by age groups, overall in-hospital mortality was lowest among patients aged 60–64 years both for first and last fractures. In contrast, in-hospital mortality was as high as 8.9 % (95 % CI: 7.2–10.6 %) among individuals aged 95 years and above. At all ages except for patients aged 50–54 and 60–64 years, men had significantly higher in-hospital mortality than women.
Unadjusted and adjusted hazard ratios (HRs) were calculated for mortality of the entire study interval based on first admission dates (estimated for ≥2 fractures) including variables gender, age group, hospital days, and number of fractures (Table 4). Men´s hazard of shorter time to death relative to female patients rose from 1.3 in the unadjusted analysis to approximately 1.75 in any of the adjusted models, and advanced age entailed a mortality risk of more than 12-fold for the oldest in relation to the youngest patients. Moreover, an effect of hospital days per fracture on risk reduction was evident in the adjusted cases, resulting in a 0.3–0.4 % hazard reduction of each additional hospital day in the adjusted models. Finally, sustaining more than one fracture was associated with improved survival. An interaction model comprising all variables (Online Resource, supplemental Table 3) demonstrated that more advanced age increased mortality hazard, likewise more hospital days per fracture were weakly but significantly associated with higher risk. In detail, male patients at age 70–79 years were at elevated mortality risk, whereas increased hospitalization time reduced risk in patients aged 75 years and over and in patients sustaining three fractures.
Next, we determined hip fracture patients´ mortality risk relative to a control population represented by individuals without a history of hip fracture. Indeed, we found increased risk at all time points up to 3 years as compared to controls (Table 5): Excess mortality expressed as relative hazard (RH) was highest within 30 days after hip fracture, being twice as high in men as compared to women (RH 16.28 (95 % CI: 12.47–21.26) versus 8.29 (95 % CI: 7.09–9.70), respectively, first admission as reference time point). RHs decreased considerably within 6 months in both men and women, but remained statistically significant for the whole observation period. Furthermore, supplemental Tables 4 and 5 in the Online Resource show age-group dependent RHs for the first and second year, respectively. RHs decreased with advancing age, with the exception of males aged 95 years and over where RH increased again. Interestingly, whereas women displayed RHs higher than their age-matched male counterparts up to 65–69 years both within the first and during the second year, and RHs within the second year were roughly equal among genders between 70 and 80 years of age, it was men´s RHs that exceeded those of women at ages above.
Discussion
Herein, we present a large-scale up-to-date analysis of mortality rates up to 3 years after hip fractures in Austrian patients in the period of 2008–2011. As expected and also described previously for the same population, hip fractures occur much more frequently in women than in men (ratio roughly 3:1), comparable to other nation-wide studies [8, 12, 24–26]. Interestingly, the proportion of men decreased at subsequent fractures (Table 1, “Results” section) probably being partially related to higher male mortality after first hip fracture.
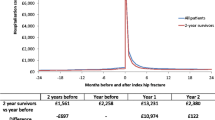
We also analyzed length of hospital stay due to hip fracture. As compared to a previous publication from the same country analyzing data from 1995, we found very similar hospitalization time in both investigations (mean 22 days) [21]. Also, peak mean hospital days were between 75 and 84 years in both studies. Advanced age seemed to be associated with longer hospitalization among women as compared with men in the same report [21], though no P values are listed. Overall, our results on age- and gender-adjusted length of hospital stay after hip fracture suggest no substantial changes from 1995–2011 [21].
Considering all-cause mortality, we found death rates of 4.8 and 20.2 % after 30 days and 1 year, respectively. These numbers are among the lowest compared to investigations of similar size from other countries. A large retrospective cohort study from Denmark observed 13 and 29 % deaths after 30 days and 1 year, respectively, accounting for all subjects irrespective of age; first patients were, however, recruited already in 1977 [12]. A more recent Danish nation-wide cohort study including all hip fracture patients between 1999 and 2002 that were born up to 1945 revealed a cumulative 1-year mortality rate of 26.4 % for female and 37.1 % for male patients [24]. Bass et al. [27] retrospectively analyzed survival in veterans aged 65 and above registered in the US Medicare database, reporting unadjusted mortality rates of 9.7 and 32.2 % for 30 days and 1 year, respectively. A retrospective cohort study of Canadian hip fracture patients aged over 50 found all-cause mortality at 1 year post-fracture to be 36.3 % [28]. Along the same lines, in-hospital mortality of overall 4.0 % (95 % CI: 3.8–4.3 %) reported herein (Table 3) is low compared with previous reports from Austria including all age groups that stated 6.8 % in 1995 [21], and 3.8 and 3.2 % for male and female patients, respectively, in 2004 [22]. Reports from other countries incorporating patients aged 65 and over stated 4.5 % in a nationwide Danish study [29]), 5.1 % in New York state hospitals over a period of 12 years [30], and as high a figure as 14.3 % in an extensive investigation from England [31]. Conversely, nationwide investigations from South Korea including hip fracture patients aged 50 and older stated overall 1-year mortality of 16.55 % in 2003 [25] and ranging from 17.8 to 19.0 % between 2005 and 2007 [32]. Recently, a nationwide study from Taiwan on patients aged 60 years and over reported declining annual hip fracture-related mortality from overall 18.10 % in 1999 to 13.98 % in 2009, corresponding to an average 1-year mortality of 16.32 % for the whole time interval, and 1-month mortality was even found as low as 2.49 % [33]. Thus, Austrian hip fracture patients seem to be at lower mortality risk as compared to most other countries except Eastern Asian populations.
Our results underscore the role of advanced age and male gender in hip fracture patients´ mortality risk. Moreover, our analyses show that both longer hospitalization time per fracture and more fractures are in association with a significantly reduced risk. Well in line, longer medical care in hospital after hip fracture correlated with lower mortality in Japan as compared with the United States, even upon adjustment for confounding factors [34]. Alternatively, an Australian study claimed longer waiting times for healthier patients destined to enter a rehabilitation center than for more co-morbid patients who are transferred to nursing homes usually rather quickly [35]. However, variable interaction confers a statistically significant effect of longer hospitalization at age 75 and over, associated with decreased mortality risk. This implies that aged patients who need more time to recover benefit in particular from longer in-hospital care. Thus following the explanation offered by Williams et al. [35], one would have to assume either low co-morbidity or particularly long waiting times until rehabilitation among older patients; both scenarios are unlikely in Austrian patients. Concerning subsequent fractures as protective factor, this could be due to the fact that surviving patients are relatively healthy but prone to the next fracture as a consequence of osteoporosis.
Notably, the impact of gender and consecutive fractures as such vanished in the interaction model unless in conjunction with other variables (Online Resource, supplemental Table 3): Though hazards rose with age independently of gender, interaction terms revealed a significantly elevated HR for men aged 70–74 compared to their female counterparts, implying particular mortality risk for male patients of that age. Relevance for fracture number was observed only in interaction with hospital days per fracture entailing risk reduction for (at least) three fractures (no statistical significance for ≥4 fractures is probably due to low patient numbers, HRs for 4 and ≥5 fractures are below that for 3 fractures); therefore it is patients with more subsequent fractures who benefit the most from a longer stay in hospital in terms of survival.
Relative hazards (RHs) for all-cause excess mortality during various time intervals from hospital admission upon index fracture in our patients are comparable with those of a previous meta-analysis [13] although male mortality rates are slightly higher among our patients where RHs dropped to below 2 after 6 months and remained in this range up to 3 years. Our results are in line with others reporting a rapid decline within the first year post-fracture, yet a persistent elevation for an observation period of as long as 10 years [12, 13]. In contrast, studies investigating institutionalized patients reported no significant excess mortality among patients surviving the first 6 months after fracture [14, 15]. Another observation in our study is that during both first and second year post-fracture, excess mortality up to 69 years of age was higher among women than men. However, these findings should be interpreted cautiously in view of the large-sized 95 % CIs at these age groups that are due to fewer study subjects and more censored cases at those ages as compared with more advanced age groups. On the other hand, studies from South Korea [32] and Taiwan [33] found higher female excess mortality rates up to 79 years in the first and second year post-fracture, and higher male excess mortality only after 80 years of age. These findings are at odds with another study claiming excess mortality to be higher in men than women at all ages [36] but are consistent with results of a meta-analysis that reported higher excess mortality for men only at 70 years and above [13].
Enhanced administration of anti-resorptive drugs such as bisphosphonates in conjunction with effective ortho-geriatric care measures could be causative for the low mortality rates following hip fracture reported herein in relation to data from other countries. Also, we found reduced in-hospital mortality relative to one previous national study that analyzed data from 1995 [21]. In recent years in Austria, a number of ortho-geriatric care services were initiated before or within the study interval of the present investigation, however, on a regional and local basis rather than as part of an overarching, co-ordinated nationwide program [37–39]. These initiatives not only ensure due prescription of medication like bisphosphonates and adherence to therapy, they also implement and reinforce integrated measures of postoperative care [40, 41]. Mortality data from one such care center on hip fracture patients aged 80 years and above were reported to be 2.8 % in hospital and 23.2 % one year post-fracture, which is strikingly low for this age group [42]. Moreover, mortality outcomes of international ortho-geriatric service programs suggest improved survival rates at least in hospital (summarized in [40]), therefore declining in-hospital and perhaps also lowered longer term mortality might in part be attributed to efficacious ortho-geriatric care measures in Austria. As for bisphosphonates, an increase in their prescription during the 2000s was demonstrated to coincide with a reduction in hip fracture incidence in two studies [43, 44], and during the same period, a decreasing trend in hip fracture incidence was also observed in Austria [8]. Further, there is evidence for an impact of bisphosphonate treatment on prolonged survival after hip fractures [45–47]. The fact that male excess mortality rates are above those seen in other studies might be based on suboptimal osteoporosis treatment in these patients, as previously described for Denmark [47]. Collectively, disparate study results during the last 10–15 years on short-term and long-term mortality after hip fracture reported at different times and in different countries could mirror varying evolution stages in the implementation of ortho-geriatric services and anti-resorptive treatment regimes alike.
Our study is subject to several limitations. First, no information on lifestyle factors and co-morbidities was available. Second, the date of first admission was not directly available for 21.4 % of patients sustaining more than one fracture during the study interval, for whom it had to be assessed from hip fracture-related hospital days. An alternative to this approach would have been exclusion of subsequent fractures like elsewhere [29], however, we believe that such a procedure would have conferred a substantial bias to our investigation. Third, mean follow-up time of 528 days for hip fracture patients did not permit conclusions on long-term mortality beyond 3 years, unlike other previous comparable studies (e.g., [12–14]). Finally, there was no criterion to ensure that first fractures recorded in the study period (index fractures for which hospital discharge dates were available) were first fractures that patients sustained: Exclusion of index fractures that were in fact not patients´ first fractures might have tilted estimates towards slightly shorter survival times. On the other hand, we are convinced that substantive strengths of our work encompass (i) the participation of almost all social insurance authorities, corresponding to coverage of approximately 98 % of the total Austrian population, (ii) the access to personalized data thus ruling out multiple registrations, implying that all fracture events could be unambiguously assigned to study subjects, and (iii) the allowance for mortality rates beginning with hospital discharge upon first fracture in the study interval, which represents valuable information regarding survivors of (first) hospitalization.
Taken together, our results demonstrate in a nation-wide retrospective study that recent all-cause mortality rates including in-hospital mortality after hip fracture among elderly patients are low in Austria compared with many other countries, however, male excess mortality is elevated. Moreover, in a multivariate model accounting for variable interactions, we found that longer hospital care favors patients aged 75 and above and those sustaining (at least) three fractures the most, and that the highest gender difference in mortality risk after hip fracture is among patients aged 70–79 years with males at greater risk. Further research is necessary to identify causes of male excess mortality. Elderly male osteoporotic patients are therefore an important high-risk group after hip fracture in Austria.
References
Dhanwal DK, Dennison EM, Harvey NC, Cooper C (2011) Epidemiology of hip fracture: worldwide geographic variation. Indian J Orthop 45:15–22
Haleem S, Lutchman L, Mayahi R, Grice JE, Parker MJ (2008) Mortality following hip fracture: trends and geographical variations over the last 40 years. Injury 39:1157–1163
Armstrong AL, Wallace WA (1994) The epidemiology of hip fractures and methods of prevention. Acta Orthop Belg 60(Suppl 1):85–101
McClung MR (2003) Pathogenesis of osteoporotic hip fractures. Clin Cornerstone 5(Suppl 2):22–29
Abrahamsen B, Vestergaard P (2010) Declining incidence of hip fractures and the extent of use of anti-osteoporotic therapy in Denmark 1997–2006. Osteoporos Int 21:373–380
Maravic M, Taupin P, Landais P, Roux C (2011) Change in hip fracture incidence over the last 6 years in France. Osteoporos Int 22:797–801
Støen RO, Nordsletten L, Meyer HE, Frihagen JF, Falch JA, Lofthus CM (2012) Hip fracture incidence is decreasing in the high incidence area of Oslo, Norway. Osteoporos Int 23:2527–2534
Dimai HP, Svedbom A, Fahrleitner-Pammer A, Pieber T, Resch H, Zwettler E et al (2011) Epidemiology of hip fractures in Austria: evidence for a change in the secular trend. Osteoporos Int 22:685–692
Giversen IM (2007) Time trends of mortality after first hip fractures. Osteoporos Int 18:721–732
Kanis JA, Odén A, McCloskey EV, Johansson H, Wahl DA, Cooper C (2012) A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int 23:2239–2256
Miyamoto RG, Kaplan KM, Levine BR, Egol KA, Zuckerman JD (2008) Surgical management of hip fractures: an evidence-based review of the literature. I: femoral neck fractures. J Am Acad Orthop Surg 16:596–607
Vestergaard P, Rejnmark L, Mosekilde L (2007) Increased mortality in patients with a hip fracture-effect of pre-morbid conditions and post-fracture complications. Osteoporos Int 18:1583–1593
Haentjens P, Magaziner J, Colón-Emeric CS, Vanderschueren D, Milisen K, Velkeniers B et al (2010) Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med 152:380–390
Tosteson ANA, Gottlieb DJ, Radley DC, Fisher ES, Melton LJ III (2007) Excess mortality following hip fracture: the role of underlying health status. Osteoporos Int 18:1463–1472
Rapp K, Becker C, Lamb SE, Icks A, Klenk J (2008) Hip fractures in institutionalized elderly people: incidence rates and excess mortality. J Bone Miner Res 23:1825–1831
Abrahamsen B, van Staa T, Ariely R, Olson M, Cooper C (2009) Excess mortality following hip fracture: a systematic epidemiological review. Osteoporos Int 20:1633–1650
Frost SA, Nguyen ND, Black DA, Eisman JA, Nguyen TV (2011) Risk factors for in-hospital post-hip fracture mortality. Bone 49:553–558
Belmont PJ Jr, Garcia EJ, Romano DM, Bader JO, Nelson KJ, Schoenfeld AJ (2014) Risk factors for complications and in-hospital mortality following hip fractures: a study using the National Trauma Data Bank. Arch Orthop Trauma Surg 134:597–604
Norring-Agerskov D, Laulund AS, Bruun Lauritzen J, Rønnov Duus B, van der Mark S, Mosfeldt M et al (2013) Metaanalysis of risk factors for mortality in patients with hip fracture. Dan Med J 60:A4675
Farahmand BY, Michaëlsson K, Ahlbom A, Ljunghall S, Baron JA (2005) Survival after hip fracture. Osteoporos Int 16:1583–1590
Koeck CM, Schwappach DLB, Niemann FM, Strassmann TJ, Ebner H, Klaushofer K (2001) Incidence and costs of osteoporosis-associated hip fractures in Austria. Wien Klin Wochenschr 113:371–377
Dorner T, Weichselbaum E, Lawrence K, Stein KV, Rieder A (2009) Austrian osteoporosis report: epidemiology, lifestyle factors, public health strategies. Wien Med Wochenschr 159:221–229
World Health Organization (2004) ICD-10: International statistical classification of diseases and related health problems (10th rev., 2nded.). World Health Organization, Geneva.
Kannegaard PN, van der Mark S, Eiken P, Abrahamsen B (2010) Excess mortality in men compared with women following a hip fracture. National analysis of comedications, comorbidity and survival. Age Ageing 39:203–209
Kang H-Y, Yang K-H, Kim YN, Moon S-H, Choi W-J, Kang DR et al (2010) Incidence and mortality of hip fracture among the elderly population in South Korea: a population-based study using the National Health Insurance claims data. BMC Public Health 10:230
Chau PH, Wong M, Lee A, Ling M, Woo J (2013) Trends in hip fracture incidence and mortality in Chinese population from Hong Kong 2001-09. Age Ageing 42:229–233
Bass E, French DD, Bradham DD, Rubenstein LZ (2007) Risk-adjusted mortality rates of elderly veterans with hip fractures. Ann Epidemiol 17:514–519
Morin S, Lix LM, Azimaee M, Metge C, Caetano P, Leslie WD (2011) Mortality rates after incident non-traumatic fractures in older men and women. Osteoporos Int 22:2439–2448
Laubjerg Daugaard C, Jørgensen HL, Riis T, Lauritzen JB, Duus BR, van der Mark S (2012) Is mortality after hip fracture associated with surgical delay or admission during weekends and public holidays? A retrospective study of 38,020 patients. Acta Orthop 83:609–613
Su H, Aharonoff GB, Hiebert R, Zuckerman JD, Koval KJ (2003) In-hospital mortality after femoral neck fracture: do internal fixation and hemiarthroplasty differ? Am J Orthop 32:151–155
Bottle A, Aylin P (2006) Mortality associated with delay in operation after hip fracture: observational study. BMJ 332:947–951
Yoon H-K, Park C, Jang S, Jang S, Lee Y-K, Ha Y-C (2011) Incidence and mortality following hip fracture in Korea. J Korean Med Sci 26:1087–1092
Wang C-B, Lin C-FJ, Liang W-M, Cheng C-F, Chang Y-J, Wu H-C et al (2013) Excess mortality after hip fracture among the elderly in Taiwan: a nationwide population-based cohort study. Bone 56:147–153
Kondo A, Zierler BK, Isokawa Y, Hagino H, Ito Y, Richerson M (2010) Comparison of lengths of hospital stay after surgery and mortality in elderly hip fracture patients between Japan and the United States – the relationship between the lengths of hospital stay after surgery and mortality. Disabil Rehabil 32:826–835
Williams N, Hardy BM, Tarrant S, Enninghorst N, Attia J, Oldmeadow C et al (2013) Changes in hip fracture incidence, mortality and length of stay over the last decade in an Australian major trauma centre. Arch Osteoporos 8:150
Sterling RS (2011) Gender and race/ethnicity differences in hip fracture incidence, morbidity, mortality, and function. Clin Orthop Relat Res 469:1913–1918
Zwettler E, Eichbauer H, Lehner E, Vargas J, Bakewell S, Kara M et al (2009) Secondary hip fracture prevention through integrated clinical approaches involving specialists, general practitioners and nurses. Bone 44(Suppl 2):201
Kammerlander C, Gosch M, Blauth M, Lechleitner M, Luger TJ, Roth T (2011) The Tyrolean Geriatric Fracture Center: an orthogeriatric co-management model. Z Gerontol Geriatr 44:363–367
Mikosch P, Gosch M (2013) Osteoporose – Therapie und sektorenübergreifendes Management. Wien Med Wochenschr 163:455–461
Kammerlander C, Roth T, Friedman SM, Suhm N, Luger TJ, Kammerlander-Knauer U et al (2010) Ortho-geriatric service—a literature review comparing different models. Osteoporos Int 21(Suppl 4):S637–S646
Gosch M, Roth T, Kammerlander C, Joosten-Gstrein B, Benvenuti-Falger U, Blauth M et al (2011) Treatment of osteoporosis in postmenopausal hip fracture patients after geriatric rehabilitation: changes over the last decade. Z Gerontol Geriatr 44:381–386
Kammerlander C, Gosch M, Kammerlander-Knauer U, Luger TJ, Blauth M, Roth T (2011) Long-term functional outcome in geriatric hip fracture patients. Arch Orthop Trauma Surg 131:1435–1444
Alves SM, Economou T, Oliveira C, Ribeiro AI, Neves N, Goméz-Barrena E et al (2013) Osteoporotic hip fractures: Bisphosphonates sales and observed turning point in trend. A population-based retrospective study. Bone 53:430–436
Fisher AA, O´Brien ED, Davis MW (2009) Trends in hip fracture epidemiology in Australia: possible impact of bisphosphonates and hormone replacement therapy. Bone 45:246–253
Lyles KW, Colón-Emeric CS, Magaziner JS, Adachi JD, Pieper CF, Mautalen C et al (2007) Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl J Med 357:1799–1809
Beaupre LA, Morrish DW, Hanley DA, Maksymowych WP, Bell NR, Juby AG et al (2011) Oral bisphosphonates are associated with reduced mortality after hip fracture. Osteoporos Int 22:983–991
Bondo L, Eiken P, Abrahamsen B (2013) Analysis of the association between bisphosphonate treatment survival in Danish hip fracture patients-a nationwide register-based open cohort study. Osteoporos Int 24:245–252
Acknowledgments
We thank Katrin Danninger (Oberösterreichische Gebietskrankenkasse), Alexandra Ferdin (Versicherungsanstalt öffentlich Bediensteter), Jana Fischer (Niederösterreichische Gebietskrankenkasse), Peter Haubenberger (Sozialversicherungsanstalt der Gewerblichen Wirtschaft), Michael Hueber (Versicherungsanstalt für Eisenbahnen und Bergbau), Renato Kasseroller (Salzburger Gebietskrankenkasse), Claudia Kastelic (Sozialversicherungsanstalt der Bauern), Tobias Lingenhöle (Vorarlberger Gebietskrankenkasse), Ursula Riess (Kärntner Gebietskrankenkasse), Marianne Schmid (Steiermärkische Gebietskrankenkasse), Cornelia Siess (Wiener Gebietskrankenkasse), and Norbert Thiemann (Tiroler Gebietskrankenkasse) from the Austrian social insurance authorities for provision of the data.
Human and Animal Rights and Informed Consent
The local Ethics Committee approved the study which was performed according to the Declaration of Helsinki.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Brozek, W., Reichardt, B., Kimberger, O. et al. Mortality After Hip Fracture in Austria 2008–2011. Calcif Tissue Int 95, 257–266 (2014). https://doi.org/10.1007/s00223-014-9889-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-014-9889-9