Abstract
Rett syndrome, an X-linked neurodevelopmental disorder primarily affecting girls, is frequently characterized by a reduced bone mineral density (BMD) with an increased risk of fragility fractures. The aim of the study was to assess bone status by DXA technique and by quantitative ultrasound (QUS) in subjects with Rett syndrome and to evaluate which DXA or QUS parameters better correlate with clinical features. In 156 Rett subjects (mean age 13.6 ± 8.2 years) and in 62 controls, we measured BMD at femoral neck (BMD-FN) and at total femur (BMD-TF). Apparent volumetric bone mineral density (vBMAD) was also calculated. In all subjects, QUS parameters at phalanges by Bone Profiler-IGEA (amplitude-dependent speed of sound: AD-SoS and bone transmission time: BTT) were evaluated. We found that both DXA parameters and QUS parameters were significantly lower in Rett subjects than in controls. All clinical characteristics were positively correlated to BMD-FN, BMD-TF, AD-SoS, and BTT (p < 0.001) but not with vBMAD-FN. All ultrasonographic parameters were significantly correlated to BMD-FN and BMD-TF, whereas vBMAD-FN showed only positive significant correlation with densitometric parameters (p < 001). In Rett subjects BMD-FN was predicted primarily by weight and movement capacity, whereas vBMAD-FN was predicted by weight, height, and calcium intake. Moreover, AD-SoS was predicted by weight, height, and age, while BTT was predicted only by height. In conclusion, in our study the performance of QUS at phalanges was similar to those of BMD at femur, therefore, both areal BMD at femur and QUS at phalanges (AD-SoS and BTT) may be equally useful in the evaluation of skeletal status in Rett patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rett syndrome is a predominantly neurological disorder and a primary cause of severe mental retardation in girls with an incidence of approximately 1 in 10,000 female births [1].
Subjects with Rett syndrome appear to develop normally up to 6–18 months of age. However, girls with classical Rett syndrome are often delayed in development, at least from 5–6 months of age, especially in terms of postural delay (ability to sit and stand unsupported and rise to standing) [2]. The head circumference of Rett girls is normal at birth; however, it begins to decelerate in its growth at 2–3 months of age [3]. Distinctive aspects contributing to the diagnosis include developmental regression, with accompanying loss of hand skills, mobility skills, and speech and stereotypical hand movements. As the syndrome progresses, social withdrawal and loss of language become apparent with features reminiscent of autism. In Rett subjects, the mental deficiency is accompanied by reduced motor coordination and the development of ataxia and gait apraxia. Associated features such as microcephaly, respiratory/autonomic abnormalities, [4] seizures, scoliosis, growth deficits, and early hypotonia are very prevalent. About 96 % of classic Rett’s syndrome subjects have mutations in the gene that encodes MeCP2, whereas other forms are largely associated with other genetic mutations, such as CDKL5 in the early onset seizure variant and FOXG1 mutations in the congenital variant. The MeCP2 is a multifunctional nuclear protein, with potentially important roles in chromatin architecture, regulation of RNA splicing, and active transcription [5].
Clinical data show that, along with neurological defects, females with Rett syndrome frequently have marked decreases in bone mineral density (BMD) [6–19]. As a consequence of the low bone mass, Rett girls are at an increased risk of fragility fractures, and it has been reported that 25–40 % of Rett girls have fracture at some time during their lives [7, 12, 14, 18]. Moreover, most subjects are growth retarded as part of the syndrome, therefore assessing bone status poses a special problem. Dual-energy X-ray absorptiometry (DXA) is the “gold standard” for evaluating bone mineral density both in adults and children. Hitherto, the DXA at central skeleton has only been carried out in few studies on subjects with Rett syndrome. In recent years, there has been a growing interest in using quantitative ultrasound (QUS) as an alternative method for non-invasive assessment of skeletal status [20]. The attractiveness of the use of QUS for bone measurements in children and adolescents lies in its lack of ionizing radiation, its ease of use, portability, and low cost. Moreover QUS, namely QUS at phalanges, seems to be less influenced by motion artifacts than central DXA [21]. These advantages have encouraged pediatric studies, and some cross-sectional normative data for children and adolescents have been produced [22]. Moreover, several studies suggest that phalanges may be an appropriate measurement site because this site is sensitive to changes in bone status. However, there appears to be few data available in the literature that has compared phalangeal QUS to femoral BMD measured by DXA in children and adolescents.
The aim of our study was twofold:
(1) to evaluate bone status, as assessed by DXA technique and by quantitative ultrasound, in subjects with Rett syndrome;
(2) to evaluate which DXA or QUS parameters better correlate with clinical features of Rett syndrome.
Materials and Methods
Study population
We studied 156 subjects (age range 4–33 years; mean age 13.6 ± 8.2) affected by Rett syndrome, referred to the Department of Paediatric Neuropsychiatry of Siena from June 2012 to December 2013. This Department has a long history of research on Rett syndrome and many subjects from different parts of Italy undergo a routine annual follow-up examination in Siena. The diagnosis of Rett syndrome was made according to the internationally accepted diagnostic criteria [1, 23]. The patients who had experienced a fragility fracture or who had been treated with antiresorptive drugs in the previous 12 months were excluded. The patients with severe cardiac or pulmonary complications or with a life expectancy of less than 24 months were also excluded. Also Rett subjects on parenteral nutrition or with feeding tube were excluded. Sixty-two similar age range healthy subjects were used as controls. The study was approved by the Ethics Committee for human investigation of our Institution and informed consent was obtained according to the rules of the Ethics Committee. Questionnaires completed by parents provided information on clinical data, level of mobility, use of anticonvulsants or calcium/Vitamin D supplements, history of fracture, and dietary calcium intake of the Rett patients. Pubertal status was categorized into three groups: a prepubertal group of Tanner stages 1 and 2, a pubertal group of Tanner stage 3–5, and a postpubertal group of subject of over 16 years.
In our subjects, MECP2 mutations were present in 129 subjects (82.7%), CDKL5 mutations were present in four subjects (2.6 %), and no information about genetic status was available for the other 23 subjects. At the time of the evaluation 49 (31.4 %), subjects were non ambulatory whereas the others presented a severe 52 (33.3 %) or a mild-moderate 55 (35.4 %) ambulatory impairment. The ambulatory impairment was defined as severe, when the ambulation was possible only with assistance.
Densitometric and Ultrasonographic Measurements
In all subjects, we performed areal BMD at femoral sub regions (femoral neck: BMD-FN and total hip: BMD-TF) by dual-energy X-ray absorptiometry (Hologic QDR 4500, Bedford-MA, US). To reduce the effect of body size on BMD, apparent volumetric bone mineral density (vBMAD) of femoral neck (vBMAD-FN) was also calculated [24–26]. All scans were performed by the same operator, while the subjects were wearing light indoor clothing and no removable metal objects. The Rett subjects with severe involuntary muscle contractions or uncontrollable movements were lightly sedated with midazolam (0.2 mg/kg/dose) before the scan to prevent repetitive involuntary movements which could invalidate the analysis.
Moreover, in all subjects QUS parameters were evaluated at phalanges using a QUS device (Bone Profiler, IGEA, Italy). The device used is based on the transmission of ultrasound through the distal end of the first phalangeal diaphysis in the proximity of the condyles of the last four fingers of the hand. Bone Profiler measures the amplitude-dependent speed of sound (AD-SoS, m/s) and some parameters derived from the analysis of the graphic trace of the QUS signal [27, 28]. AD-SoS depends on the signal amplitude because it is calculated by considering the time when the electrical signal, generated by the ultrasound mechanical wave at the receiving probe, reaches an amplitude of 2 mV [27]. Among the parameters derived from the analysis of the QUS graphic trace, we have considered the bone transmission time (BTT, μs) which is the difference between the time when the first peak of the signal received attains its maximum and the time that would have been measured if only soft tissue and not bone was present between the transducers. Therefore BTT, unlike AD-SoS, is largely independent of ultrasound attenuation and soft tissue bias, and it depends almost exclusively on bone properties [29]. AD-SoS and BTT were measured in the non-dominant hand, and the final result is the average AD-SoS and BTT of the last four fingers. The AD-SoS and BTT values of Rett patients and controls were converted to Z scores using the normative data obtained from a reference pediatric Italian population [22].
In our Institution, the precision of AD-SoS and BTT evaluated in children was 0.7 and 0.8 %, respectively. In addition, the standardized coefficient of variation (sCV) was calculated for each QUS parameter according to the formula: sCV = CV%/range/mean, where range was the difference between the 5th and the 95th percentile of the population. The sCV was 3.7 % for AD-SoS and 2.6 % for BTT. The precision assessed in five Rett patients measured five times on one day by the same operator (C.C.) by repositioning has given similar results (CV = 0.5 and 0.8 % for AD-SoS and BTT, respectively).
Biochemical Parameters
In Rett subjects and controls, blood samples were also collected under fasting conditions to evaluate serum calcium levels (Ca), phosphate (P), intact parathyroid hormone (PTH), and 25-Hydroxyvitam D (25OHD). Serum PTH was assessed by an immunoradiometric assay using two goat polyclonal antibodies against the human PTH molecule (DiaSorin, Saluggia, Italy). The results were expressed in picograms per milliliter, and the intra- and inter-assay coefficients of variation were 3.6 and 4.9 %, respectively. Serum 25OHD was determined by a radioimmunometric method (25-Hydroxyvitam D, DiaSorin, MN, USA). In our Institution, the intra- and inter-assay coefficients of variation for 25OHD were 6.8 and 9.2 %, respectively.
Statistical Analysis
The variables normally distributed were expressed as mean ± SD, and the significance between the means was tested using Student’s t test. Instead BMI were not distributed normally, therefore, these variables were also expressed as median, and the significance between the means was tested using the Mann–Whitney test.
The correlations between the groups were analyzed with the Pearson’s correlation test and the Spearman’s correlation where appropriate. Separate multiple linear regression models (method: Stepwise) were used to assess independent predictors of BMD-FN, BMD-TF, vBMAD-FN, AD-SoS, and BTT, while age, weight, height, scoliosis, movement capacity, antiepileptic drugs (AEDs), and calcium intake were included as independent variables in the models. For each model, the regression coefficients (b-coefficients) and their 95 % confidence intervals were described. All tests were two-sided, and p < 0.05 was considered statistically significant. All statistical tests were performed using SPSS 10.1 statistical software (SPSS 10.1).
Results
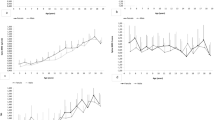
Clinical characteristics of the Rett subjects and of the control group are reported in Table 1. Thirty-six percent (57 out of 156) of Rett subjects and 31 % (19 out of 62) of controls were in Tanner stages 1–2, 40 % (62 out of 156) of Rett subjects and 40 % (25 out of 62) of controls had reached Tanner stages 3 through 5, and finally 24 % (37 out of 156) of Rett subjects and 29 % (18 out of 62) of controls were over 20 years old. As expected, the Rett subjects were significantly shorter in height and lower in weight than the control group. Densitometric and ultrasonographic parameters of the Rett subjects and of the control group are reported in Table 2. In Rett subjects, the values of BMD-FN, BMD-TF, and vBMAD-FN were significantly lower than in control subjects. Moreover, both AD-SoS and BTT were significantly lower in the Rett subjects than in controls (p < 0.05). Among biochemical parameters, serum Ca, P, and PTH did not show any significant difference between the two groups, whereas serum 25OHD was lower in the Rett subjects without reaching any statistical significance.
Correlation between clinical characteristics, densitometric and ultrasonographic parameters in Rett subjects and controls are reported in Table 3. All clinical characteristics were positively correlated to BMD-FN, BMD-TF, AD-SoS, and BTT (p < 0.001) but not with vBMAD-FN. All ultrasonographic parameters were significantly correlated to BMD-FN and BMD-FT, whereas vBMAD-FN showed only positive significant correlation with densitometric parameters (p < 001), a moderate positive correlation with weight and a positive but not significant correlation with weight and ultrasonographic parameters.
Of the 156 Rett subjects, 68 (43.6 %) presented scoliosis. When the Rett subjects were separated into two groups according to the presence or absence of scoliosis, the Rett subjects with scoliosis showed densitometric and ultrasonographic parameters lower than the Rett subjects without scoliosis. However, the difference reached statistical significance for AD-SoS in the prepubertal group (p < 0.05), for BTT in the pubertal group (p < 0.05), and for BMD-TF in the postpubertal group (p < 0.05) (Table 4).
In Table 5, we reported multiple linear regression analysis of predictors of bone mineral density and QUS parameters in Rett subjects. The analysis was performed by including in the model age, weight, height, movement capacity, scoliosis, AEDs, and calcium intake as independent variables. In Rett subjects, BMD-FN was predicted primarily by weight and movement capacity, whereas vBMAD-FN was predicted by weight, height, and calcium intake. Moreover, AD-SoS was predicted by weight, height, and age, while BTT was predicted only by height.
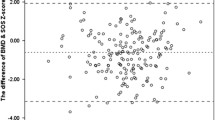
When the subjects with Rett syndrome were separated in three groups on the basis of the capacity of movement, the Rett subjects who were non ambulatory showed BMD-FN, vBMAD-FN, AD-SoS, and BTT to be lower than in Rett subjects without mobility impairment. The differences between the three groups reached statistical significance for BMD-FN and BTT but not for vBMAD-FN and AD-SoS (Fig. 1).
Discussion
This study analyzed the largest sample of subjects with Rett syndrome to date and considered two different methods for the evaluation of bone status.
Our findings show that both densitometric and ultrasonographic parameters were significantly lower in Rett subjects than in controls, and that these were similarly influenced by the anthropometric parameters and mobility. These findings are in agreement with the few previous studies carried out to date by others authors [6–19] who evaluated BMD by DXA or QUS in both children and young adult affected by Rett syndrome.
The bone health of children and adolescents has become an increasingly important medical concern. In particular, there is growing recognition that low bone mass and fractures may complicate several genetic and acquired chronic disorders of childhood [30]. The pediatric skeleton can be assessed using different techniques such as dual-energy X-ray absorptiometry, quantitative computed tomography, peripheral quantitative computed tomography, quantitative ultrasonography, magnetic resonance imaging, or X-ray. Nevertheless, DXA remains the preferred method for clinical measurements of bone density in children because of its availability, reproducibility, speed, low exposure to ionizing radiation, and robust pediatric reference data [31, 32]. Also for children with contractures who cannot be positioned properly for spine or whole-body studies, measurements of the lateral distal femur may be a useful alternative measurement [33].
The most significant limitation of DXA is its reliance on areal rather than volumetric BMD; consequently, it does not provide information on the depth of the bone. As wider and longer bones also tend to be thicker, larger bones have artificially inflated areal BMD measurements, resulting in an artificial underestimation of bone density in people of lower stature, irrespective of a potentially underlying chronic disease. This confounding factor of poor growth becomes significant also in subjects with Rett syndrome suffering from decreased somatic growth.
It is therefore even questionable whether DXA should be used in the growing child at all, in effect DXA does not distinguish between cortical and trabecular bone. Moreover, the DXA technique provides little data on bone geometry and trabecular microarchitecture. However, bone circumference, periostal and endostal dimensions, and trabecular microarchitectural parameters, such as trabecular thickness, number, spacing, orientation, connectivity, and the ratio of plate- and rod-like structures, all contribute to bone strength [34]. However, at present there is no evidence in children that areal BMD is predictive of future fracture risk [35].
In 1992, Carter et al. introduced a method of estimating vBMD by the calculation of bone mineral apparent density (BMAD, grams per cubic centimeter), which reduces the confounding effect of the bone size [24]. In our study, in accordance with the previous study by Roende et al. [24] the dependence of BMD on bone and body size was corrected by calculating BMAD at femoral neck as the most accurate indicator of volumetric density. Also with regard to the association with clinical failure, our data seem to be in agreement with Roende et al. [17] which showed that vBMAD at femur was significantly associated to antiepileptic treatment and movement capacity; but none of these associations with BMAD at femur remained significant in a multiple-adjusted model including age and BMI. In our Rett subjects, when BMD and vBMAD were regressed against scoliosis, movement capacity, AEDs, and calcium intake we found similar relationships for BMD and vBMAD. However, other studies found that BMAD was less dependent on body size than BMD [24, 36].
A possible explanation of this discordance could be that in Rett subjects the influence of height seems to be less confounding for femoral neck vBMAD respect to areal BMD values, [37] so the measurement at femur represents a good site for Rett subjects [17].
However, despite this lack of agreement in literature regarding the more important usefulness of vBMAD or BMD, the femur represents a valuable skeletal site for the assessment of bone status in Rett subjects. One other important finding of this study was that the Rett subjects showed QUS parameters significantly lower with respect to controls. These findings seem to be in agreement with the previous studied by both our group and others where QUS was used in the evaluation of bone status in both children and adolescents affected by Rett syndrome [8, 11, 13, 19].
The advantages for the use of QUS in the assessment of bone status in children and adolescents lie in its lack of ionizing radiation, ease of use, portability, and low cost. However, despite its proven advantages, the use of QUS remains controversial, due to scarce knowledge of the physical mechanism of ultrasound in assessing bone characteristics and the difficulty in comparing the results obtained by QUS with those acquired by DXA. The decision for using QUS at phalanges was prompted by the consideration that calcaneus presents some limitations in children and adolescents (e.g., motion artifacts), and by the possibility of obtaining additional information on bone status by the analysis of QUS graphic trace at phalanges.
In our study, the measurements taken at the distal metaphysis of the proximal phalanges show a high correlation with BMD at femur measured by DXA. Also Pluskiewicz et al. in a pediatric population [38] showed a good correlation between AD-SoS measured at the phalanges and BMD at both lumbar spine and total body.
Moreover, in some studies carried out in children and adolescents with disturbances of growth QUS and DXA parameters showed similar results, suggesting that both methods are able to identify a reduced bone mineral status [21].
The ability of QUS to detect a reduced mineralization of bone similarly to DXA has been confirmed also in other studies carried out on healthy children or on pediatric populations with mineral disorders or chronic diseases [39, 40].
In contrast other previous reports failed to show any association between QUS and DXA parameters, in particular Christoforidis et al. found that in healthy adolescents, Ad-SOS measurements taken at the distal metaphysis of the proximal phalanges did not show any correlation with lumbar spine and total body BMD measured by DXA, and also in another study no agreement was recorded between the two methods in the identifying thalassemic patients at risk of osteoporosis [41, 42].
Moreover, when densitometric and ultrasonographic variables were analyzed in multivariate regression analyses as dependent variables, using anthropometric and clinical parameters as independent variables, low BMD values measured at femur and low AD-SoS at phalanges were predicted equally by weight and height, to strengthening the results of our study. Moreover, the movement capacity influenced DXA and QUS parameters equally.
Our study presents some limitations. In fact, this study is cross-sectional and cannot be used to form any conclusions regarding the risk of osteoporosis and fragility fractures in Rett subjects.
Another limitation of this study is that in seriously ill Rett subjects the reproducibility of DXA and QUS measurements depends very much on the skill of operator.
In conclusion, in our study, the BMD at femur was confirmed as a useful method for the assessment of bone status in Rett subjects. Moreover, the performance of QUS at phalanges was similar to those of BMD at femur. Therefore, both BMD at femur and QUS at phalanges may be equally useful in the evaluation of skeletal status in Rett subjects.
References
Neul JL, Kaufmann WE, Glaze DG, Christodoulou J, Clarke AJ, Bahi-Buisson N, Leonard H, Bailey ME, Schanen NC, Zappella M, Renieri A, Huppke P, Percy AK, RettSearch Consortium (2010) Rett syndrome: revised diagnostic criteria and nomenclature. Ann Neurol 68:944–950
Hagberg B (2002) Clinical manifestations and stages of Rett syndrome. Ment Retard Dev Disabil Res Rev 8:61–65
Schultz RJ, Glaze DG, Motil KG, Armstrong DD, del Junco DJ, Hubbard CR, Percy AK (1993) The pattern of growth failure in Rett syndrome. Am J Dis Child 147:633–637
Julu PO, Kerr AM, Apartopoulos F, Al-Rawas S, Engerström IW, Engerström L, Jamal GA, Hansen S (2001) Characterization of breathing and associated central autonomic dysfunction in the Rett disorder. Arch Dis Child 85:29–37
Chahrour M, Zoghb HY (2007) The story of Rett syndrome: from clinic to neurobiology. Neuron 56:422–437
Haas RH, Dixon SD, Sartoris DJ, Hennessy MJ (1997) Osteopenia in Rett syndrome. J Pediatr 131:771–774
Leonard H, Thompson M, Glasson E, Fyfe S, Leonard S, Ellaway C, Bower C, Christodoulou J, Ellaway C (1999) Metacarpophalangeal pattern profile and bone age in Rett syndrome: further radiological clues to the diagnosis. Am J Med Genet 83:88–95
Cepollaro C, Gonnelli S, Bruni D, Pacini S, Martini S, Franci MB, Rossi S, Hayek J, Zappella M, Gennari C (2001) Dual X-ray absorptiometry and bone ultrasonography in patients with Rett syndrome. Calcif Tissue Int 69:259–262
Ellis KJ, Shypailo RJ, Hardin DS, Perez MD, Motil KJ, Wong WW, Abrams SA (2001) Z score prediction model for assessment of bone mineral content in paediatric diseases. J Bone Miner Res 16:1658–1664
Budden SS, Gunness ME (2003) Possible mechanisms of osteopenia in Rett syndrome: bone histomorphometric studies. J Child Neurol 18:698–702
Zysman L, Lotan M, Ben-Zeev B (2006) Osteoporosis in Rett syndrome: a study on normal values. Sci World J 6:1619–1630
Motil KJ, Ellis KJ, Barrish JO, Caeg E, Glaze DG (2008) Bone mineral content and bone mineral density are lower in older than in younger females with Rett syndrome. Pediatr Res 64:435–439
Gonnelli S, Caffarelli C, Hayek J, Montagnani A, Cadirni A, Franci B, Lucani B, Rossi S, Nuti R (2008) Bone ultrasonography at phalanxes in patients with Rett syndrome: a 3-year longitudinal study. Bone 42:737–742
Downs J, Bebbington A, Woodhead H, Jacoby P, Jian L, Jefferson A, Leonard H (2008) Early determinants of fractures in Rett syndrome. Pediatrics 121:540–546
Shapiro JR, Bibat G, Hiremath G, Blue ME, Hundalani S, Yablonski T, Kantipuly A, Rohde C, Johnston M, Naidu S (2010) Bone mass in Rett syndrome: association with clinical parameters and MECP2 mutations. Pediatr Res 68:446–451
Jefferson AL, Woodhead HJ, Fyfe S, Briody J, Bebbington A, Strauss BJ, Jacoby P, Leonard H (2011) Bone mineral content and density in Rett syndrome and their contributing factors. Pediatr Res 69:293–298
Roende G, Ravn K, Fuglsang K, Andersen H, Nielsen JB, Brøndum-Nielsen, Jensen JE (2011) DXA-measurements in Rett syndrome reveal small bones with low bone mass. J Bone Miner Res 26:2280–2286
Roende G, Ravn K, Fuglsang K, Andersen H, Vestergaard A, Brøndum-Nielsen K, Jensen JE, Nielsen JP (2011) Patients with Rett syndrome sustain low-energy fractures. Pediatr Res 69:359–364
Caffarelli C, Gonnelli S, Tanzilli L, Hayek J, Vichi V, Franci MB, Lucani B, Nuti R (2012) The relationship between serum ghrelin and body composition with bone mineral density and QUS parameters in subjects with Rett syndrome. Bone 50:830–835
Gluer CC, International Quantitative Ultrasound Consensus Group (1997) Quantitative ultrasound techniques for the assessment of osteoporosis: expert agreement on current status. J Bone Miner Res 12:1280–1288
Baroncelli GI (2008) Quantitative ultrasound methods to assess bone mineral status in children: technical characteristics, performance, and clinical application. Pediatr Res 63:220–228
Baroncelli GI, Federico G, Vignolo M, Valerio G, del Puente A, Maghnie M, Baserga M, Farello G, Saggese G, Phalangeal Quantitative Ultrasound Group (2006) Cross-sectional reference data for phalangeal quantitative ultrasound from early childhood to young-adulthood according to gender, age, skeletal growth, and pubertal development. Bone 39:159–173
Hagberg B, Hanefeld F, Percy A, Skjeldal O (2002) An update on clinically applicable diagnostic criteria in Rett syndrome. Eur J Paediatr Neurol 6:293–297
Carter DR, Bouxsein ML, Marcus R (1992) New approaches for interpreting projected bone densitometry data. J Bone Miner Res 7:37–145
Lu PW, Cowell CT, Loyd-Jones SA, Briody JN, Howman-Giles R (1996) Volumetric bone mineral density in normal subjects, aged 5–27 years. J Clin Endocrinol Metab 81:1586–1590
Ward KA, Ashby RL, Roberts SA, Adams JE, Mughal MZ (2007) UK reference data for the Hologic QDR Discovery dual energy X-ray absorptiometry scanner in healthy children aged 6–17 years. Arch Dis Child 92:53–59
Wuster C, Albanese C, De Aloysio D, Duboeuf F, Gambacciani M, Gonnelli S, Gluer CC, Hans D, Joly J, Register YJ, De Terlizzi F, Cadossi R, The Phalangeal Osteosonogrammetry Study Group (2000) Phalangeal osteosonogrammetry study: age-related changes, diagnostic sensitivity, and discrimination power. J Bone Miner Res 15:1603–1614
Montagnani A, Gonnelli S, Cepollaro C, Bruni D, Franci MB, Lucani B, Gennari C (2002) Graphic trace analysis of quantitative ultrasound at phalanxes seems to improve the diagnosis of primary hyperparathyroidism among patients with low bone mass. Osteoporos Int 13:222–227
Barkmann R, Lusse S, Stampa B, Sakata S, Heller M, Gluer CC (2000) Assessment of the geometry of human finger phalanges using quantitative ultrasound in vivo. Osteoporos Int 11:745–755
Bianchi ML (2007) Osteoporosis in children and adolescents. Bone 41:486–495
Gordon CM, Bachrach LK, Carpenter TO, Crabtree N, El-Hajj Fuleihan G, Kutilek S, Lorenc RS, Tosi LL, Ward KA, Ward LM, Kalkwarf HJ (2008) Dual energy X-ray absorptiometry interpretation and reporting in children and adolescents: the 2007 ISCD Pediatric Official Positions. J Clin Densitom 11:43–58
Crabtree NJ, Arabi A, Bachrach LK, Fewtrell M, El-Hajj Fuleihan G, Kecskemethy HH, Jaworski M, Gordon CM (2014) Dual-energy X-ray absorptiometry interpretation and reporting in children and adolescents: the revised 2013 ISCD Pediatric Official Positions. J Clin Densitom. doi:10.1016/j.jocd.2014.01.003
Bachrach LK, Sills IN, Section on Endocrinology (2011) Clinical report—bone densitometry in children and adolescents. Pediatrics 127:189–194
Leonard MB, Bachrach LK (2001) Assessment of bone mineralization following renal transplantation in children: limitations of DXA and confounding effects of delayed growth and development. Am J Transpl 1:193–1969
Specker BL, Schoenau E (2005) Quantitative bone analysis in children: current methods and recommendations. J Pediatr 146:726–73110
Jergas M, Breitenseher M, Gluer CC, Yu W, Genant HK (1995) Estimates of volumetric bone density from projectional measurements improve the discriminatory capability of dual X-ray absorptiometry. J Bone Miner Res 10:1101–1110
Kroger H, Kotaniemi A, Vainio P, Alhava E (1992) Bone densitometry of the spine and femur in children by dual-energy X-ray absorptiometry. Bone Miner 17:75–85
Pluskiewicz W, Adamczyk P, Drozdzowska B, Szprynger K, Szczepanska M, Halaba Z, Karasek D (2003) Skeletal status in children and adolescents with chronic renal failure before onset of dialysis or on dialysis. Osteoporos Int 14:283–288
Fielding KT, Nix DA, Bachrach LK (2003) Comparison of calcaneus ultrasound and dual X-ray absorptiometry in children at risk of osteopenia. J Clin Densitom 6:7–15
Baroncelli GI, Federico G, Bertelloni S, Sodini F, De Terlizzi F, Cadossi R, Saggese G (2003) Assessment of bone quality by quantitative ultrasound of proximal phalanxes of the hand and fracture rate in children and adolescents with bone and mineral disorders. Pediatr Res 54:125–13630
Christoforidis A, Perifanis V, Papadopoulou E, Dimitriadou M, Kazantzidou E, Vlachaki E, Tsatra I (2009) Poor correlations between measurements of bone quality by quantitative ultrasound sonography and dual energy X-ray absorptiometry in patients with beta-thalassaemia major. Eur J Haematol 82:15–21
Christoforidis A, Printza N, Gkogka C, Siomou E, Challa A, Kazantzidou E, Kollios K, Papachristou F (2011) Comparative study of quantitative ultrasonography and dual-energy X-ray absorptiometry for evaluating renal osteodystrophy in children with chronic kidney disease. J Bone Miner Metab 29:321–327
Human and Animal Rights and Informed Consent
All procedures performed in the present study was in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Disclosures
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Caffarelli, C., Hayek, J., Pitinca, M.D.T. et al. A Comparative Study of Dual-X-ray Absorptiometry and Quantitative Ultrasonography for the Evaluating Bone Status in Subjects with Rett Syndrome. Calcif Tissue Int 95, 248–256 (2014). https://doi.org/10.1007/s00223-014-9888-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-014-9888-x