Abstract
The aim of this study was to investigate the acute effects of oral glucocorticoids in doses used in clinical practice on biochemical indices of the function of osteoclasts, osteoblasts, and osteocytes. In 17 adult patients suffering from various medical pathologies requiring systemic steroid therapy that were never before treated with glucocorticoids, glucocorticoid treatment was initiated (mean prednisolone equivalent dose of 23.1 ± 12.7 mg/day, range 10–50). Fasting morning serum concentrations of osteocalcin (OC), amino-terminal propeptide of type I procollagen (PINP), type 1 collagen cross-linked C-telopeptide (βCTX), soluble receptor activator of nuclear factor kappaB ligand (sRANKL), osteoprotegerin (OPG), sclerostin, Dickkopf-1 (Dkk-1), and high-sensitivity C-reactive protein (hsCRP) were measured at baseline and on three consecutive days. Significant reductions in serum OC, PINP, OPG, sclerostin, and hsCRP were observed during 96 h of glucocorticoid administration, while serum βCTX showed a significant percentual increase. A significant positive correlation was found between serum concentrations of Dkk-1 and βCTX after 96 h of treatment with glucocorticoids. A significant drop in serum sclerostin, OPG, and OC observed in this study may reflect the rapid glucocorticoid-induced apoptosis of osteocytes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The anti-inflammatory, immunosuppressive, and antistress actions of glucocorticoids (GCs) play a protective role in vivo. Between 2.7 and 4.6 % of postmenopausal women are reported as currently taking oral GCs [1]. One of the principal complications of long-term GC use is a profound alteration of bone metabolism. Rapid bone loss is most marked on endocortical surfaces [2]. Fracture risk increases already during the first 6 months of therapy and is positively related to daily dose [3], emphasizing the medical need to understand the biology of GC-induced bone loss so that clinicians can effectively prevent and treat this disease [4]. Supraphysiological concentrations of GC induce an early upregulation of genes associated with osteoclast cytoskeletal reorganization and organic bone matrix degradation [5] and stimulate bone resorption by promoting osteoclast survival and activity [6, 7]. GCs also inhibit the Wnt/β-catenin signaling pathway, enhance bone marrow stromal cell development toward the adipocyte lineage rather than toward the osteoblast lineage, and rapidly and significantly impair proliferation and differentiation, survival, and function of osteoblasts [5, 8, 9]. GCs also induce the loss of osteocytes by apoptosis and by autophagy [10, 11]. Osteocytes produce negative regulators of the Wnt/b-catenin pathway such as Dickkopf-1 (Dkk-1) and sclerostin, the key components regulating the number and activity of bone-forming osteoblasts [12] as well as osteoprotegerin (OPG) and the receptor activator of nuclear factor kappaB ligand (RANKL), the key components involved in osteoclast differentiation [13]. These changes favor reduction in new bone formation, a decrease in bone mass, and impaired quality of bone [4, 14, 15].
In clinical practice, high-dose (15 mg/kg daily for 10 days) iv methylprednisolone caused an immediate and persistent decrease in the serum marker of type 1 collagen synthesis (amino-terminal propeptide of type I procollagen, PINP) and osteocalcin (OC) in 13 patients suffering from multiple sclerosis [16] and in nine asthmatics treated with high iv dosages of betamethasone (0.65 mg/h) [17]. Serum concentrations of PINP were also significantly reduced after 2 weeks’ exposure to a low dose of prednisone (5 mg daily) in healthy postmenopausal women [18]. Bone-specific alkaline phosphatase, another marker of osteoblast function, did not change significantly during administration of higher doses of GCs [16, 18]. Effects of GCs on bone resorption markers are dose-dependent. High-dose iv GCs cause a rapid and transient increase of serum marker of type-1 collagen degradation (type 1 collagen cross-linked C-telopeptide, βCTX) [16, 18]. The above studies, however, did not evaluate the acute-phase reactants to assess a possible association between reduced inflammation and changes in the bone turnover markers after GC administration. To further assess the effects of oral GCs in doses used in clinical practice on osteoclast, osteoblast, and osteocyte function, we measured serum concentrations of the proven markers of bone remodeling, such as βCTX, PINP, and OC [19], simultaneously with the other possible mediators of the effects of GCs on bone, including soluble RANKL (sRANKL); its decoy receptor OPG [20]; two inhibitors of the Wnt/β-catenin signaling pathway, sclerostin and Dkk-1 [12]; and the high-sensitivity C-reactive protein (hsCRP).
Subjects and Methods
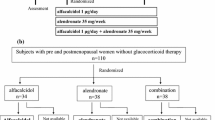
Study Design
We prospectively enrolled adult patients suffering from various medical pathologies requiring systemic steroid therapy who were never before treated with GCs and in whom GC treatment was currently initiated. All participants gave their written informed consent before enrollment. The study protocol and informed consent documents were prepared according to the Declaration of Helsinki and approved by the local ethical review board.
Before inclusion into the study, patients underwent a clinical examination (a full clinical history including details of comorbidity, detailed personal history of rheumatic disease, fracture history, alcohol intake, smoking, height loss, family history of osteoporosis, and hip fracture) and physical and laboratory examination.
One day before the initiation of GC treatment and each day before sampling, patients were asked to fast from 8:00 p.m. overnight. They were instructed to maintain normal hydration. At baseline and then after 24, 48, and 96 h, venous blood samples were collected for the assessment of biochemical markers. Immediately after sampling, the blood was centrifuged and the serum directly stored at −70 °C.
End points were changes in serum markers of osteoblast, osteocyte, and osteoclast activity during the first 96 h after initiation of GC therapy.
Patients
Included were 17 patients, 3 premenopausal women (age range 19–36 years, body mass index [BMI] 18.1–24.8 kg/m2), 10 postmenopausal women (age range 19–87 years, BMI 19.8–31.9 kg/m2), and 3 men (age range 53–63 years, BMI range 23.6–37.3 kg/m2) indicated for treatment with GCs. The indications for treatment with GCs were as follows: rheumatoid arthritis (n = 5), polymyalgia rheumatica (n = 3), systemic lupus erythematosus (n = 2), Churg–Strauss syndrome (n = 1), polymyositis (n = 3), Takayasu arteritis (n = 1), antisynthetase syndrome (n = 1), and pyrophosphate arthropathy (n = 1). Exclusion criteria were Expanded Disability Status Scale greater than 5.5, history of diseases affecting bone, prolonged immobilization (more than 3 weeks), and/or treatment with drugs known to influence bone metabolism, including GCs, any time.
At baseline, three patients were treated with hydrochloroquine, three with methotrexate, one with cyclosporine, and one with cyclophosphamide at recruitment. None of these patients was on biological therapy during the study. None of these patients was bedridden. Patients received a mean prednisolone equivalent dose of 23.1 ± 12.7 mg/day (range 10–50). Additional calcium and vitamin D supplements were provided on the third day after completion of blood study sampling. For ethical reasons it was not possible to postpone initiation of treatment by 4 days in order to perform the control tests of baseline reproducibility of the markers enabling each patient to be his or her own control. Therefore, the control group consisted of nine healthy adult volunteers (six women, three men, mean age 38.9 ± 11.3 years) who participated in the study after their written informed consent was obtained.
Biochemical Analysis
Fasting morning blood samples were obtained by antecubital venipuncture at baseline and before GC administration each day during treatment.
An enzyme-linked immunosorbent assay (ELISA) was used according to the manufacturer’s instructions, and the results were read and calculated by the ELISA reader Tecan Sunrise (Schoeller Instruments, Prague, Czech Republic). The studied parameters included serum concentrations of sRANKL (Ampli-sRANKL ELISA; Biomedica Medizinprodukte, Vienna, Austria; intra-assay imprecision coefficient of variation (CV) 9 %, interassay imprecision CV 3 %, detection limit 0.02 pmol/L), OPG (Osteoprotegerin ELISA, Biomedica Medizinprodukte; intra-assay imprecision CV 4 %, interassay imprecision 8 %, detection limit 0.14 pmol/L), Dickkopf-1 (Dkk-1 ELISA, Biomedica Medizinprodukte; intra-assay imprecision CV 8 %, interassay imprecision CV 12 %, detection limit 0.38 pmol/L), and human sclerostin (Human SOST ELISA; USCN Life Science, Brussels, Belgium; detection range 0.312–20 μg/L, detection limit <0.081 μg/L).
Serum OC, PINP, βCTX, intact parathyroid hormone (iPTH), and 25-hydroxyvitamin D [25(OH)D] were determined using electrochemiluminescence-based immunoanalysis (Cobas Analyzer; Roche Diagnostics, Mannheim, Germany). hsCRP was assessed using the immunoturbidimetric test (AU 400; Beckman Coulter, Prague, Czech Republic). The within-run imprecision of βCTX was below 7 % for samples between 200 and 500 ng/L and below 10 % for very low βCTX concentration samples. The within-run imprecision of iPTH was 5.4 % at serum concentration 3.2 pmol/L and 4.0 % at 6.6 pmol/L. The within-run imprecision of OC was <5 % at concentrations of 11–40 μg/L. The within-run imprecision of PINP was below 5 % at concentrations of 20–90 μg/L. The within-run imprecision of hsCRP was 2 %. The serum concentration of calcium was determined using the colorimetric color test Calcium Arzenazo III on the AU 400 analyzer.
The above serum markers, hsCRP, calcium, and phosphorus, were measured at baseline and after 24, 48, and 96 h of GC treatment. Serum 25(OH)D was measured at baseline. Serum specimens collected from all sampling days were analyzed simultaneously at the end of the study.
Bone Densitometry
Bone mineral density (BMD) was measured using dual-energy X-ray absorptiometry by the bone densitometer GE Prodigy (GE Healthcare, Madison, WI; software 12.10.113) at the lumbar spine, proximal femur, and femoral neck. Short-term in vivo precision errors for the lumbar spine, total femur, and femoral neck were 0.7, 0.9, and 1.8 %, respectively. BMD was expressed as a T score.
Statistical Methods
Statistical analysis of data was performed using SigmaPlot 10 software package (Systat Software, Erkrath, Germany). Relationships between variables (absolute and percent change from baseline) were explored using Pearson product moment correlation coefficients (r and p values reported). Differences in percentage change between the times were assessed by analysis of variance. Where appropriate, the Tukey test was used for comparisons. Results were considered statistically significant at the level of 0.05.
Results
Baseline characteristics of patients under study are given in Table 1. At baseline, BMD at the lumbar spine or proximal femur was in the range of osteoporosis (≤−2.5 T score) in one patient and normal (>−1 T score) in five patients. Serum 25(OH)D levels were in the deficient range (<25 nmol/L) in 9 of 17 patients and in the insufficient range (25–50 nmol/L) in 4 of 17 patients; serum iPTH concentrations were in the normal range in 12 of 17 patients; in five they were 7.2–17.3 pmol/L, with normal serum calcium. Serum concentrations of hsCRP >5 mg/L were observed in 13 of 17 patients.
At baseline, no significant correlations were observed between age, BMI, iPTH, 25(OH)D, hsCRP, and the other biochemical indices, except for significant positive correlations observed between serum PINP and OC (r = 0.82, p < 0.001), OPG and OC (r = 0.83, p < 0.001), and OPG and PINP (r = 0.62, p = 0.008) and a significant negative correlation between PINP and hsCRP (r = −0.51, p = 0.036).
During 96 h of GC administration, a significant reduction of serum OC, PINP, OPG, and sclerostin was observed (Fig. 1). Compared with baseline, after 24, 48, and 96 h, hsCRP was reduced by 23.2 ± 21.3 % (nonsignificant), 44.6 ± 28.6 % (p < 0.05), and 66.2 ± 21.7 % (p < 0.05), respectively. During 96 h of GC administration, serum βCTX showed a significant percentual increase (Fig. 1), while the increase in Dkk-1 did not reach statistical significance. A significant positive correlation was found between serum concentrations of Dkk-1 and βCTX (Fig. 2) after 96 h of treatment with GCs. This correlation was not significantly influenced by baseline iPTH, 25(OH)D, and hsCRP serum concentrations (Table 2). Also, the significant positive correlation between serum OPG and PINP was not significantly influenced by baseline iPTH, 25(OH)D, and hsCRP serum concentrations. No significant correlations were observed between age or sex and the biochemical indices studied. The increase in serum sRANKL (by 57 %) and sRANKL/OPG (by 77 %) did not reach statistical significance.
Change from baseline in serum markers in 17 patients treated with glucocorticoids (mean ± SE). *p < 0.05 versus baseline (ANOVA on ranks). Dotted lines indicate controls. a βCTX (filled circles) and PINP (empty circles). b Dkk-1 (filled circles) and sclerostin (empty circles). c Osteoprotegerin (filled circles) and osteocalcin (empty circles)
A significant correlation was observed between change in hsCRP and change in PINP and between change in hsCRP and change in sRANKL/OPG ratio (Fig. 3). Daily dose of GCs was borderline inversely correlated with change from baseline in serum PINP (r = −0.482, p = 0.05) but not with the other indices.
Serum concentrations of hsCRP, PINP, and RANKL/OPG ratio (median values and 75 % CI) at baseline (empty circle), 24 h (filled square), 48 h (empty triangle), and 96 h (filled triangle). Change in hsCRP versus change in PINP, r = 0.68, p < 0.001. Change in hsCRP versus change in RANKL/OPG ratio, r = 0.25, p = 0.042
Discussion
Our main objective in the current study was to understand whether the acute changes in serum biochemical markers of bone turnover are associated with changes in mediators of the effects of GCs on osteoblasts and osteocytes. We studied a heterogeneous and small group of adults suffering from various chronic, low-grade systemic inflammations requiring systemic steroid therapy. The subjects received a medium dose of oral GCs for 4 days. As expected, treatment with GCs resulted in a fast and significant drop in serum hsCRP, an acute-phase reactant. Serum hsCRP level has been reported to be a significant predictor of low-trauma fracture [21, 22], and circulating levels of inflammatory markers correlate with bone resorption markers and predict change in BMD [23, 24]. However, other studies did not find a significant correlation between hsCRP and serum C-telopeptide as a marker of bone resorption [22, 25]. In the present study, we also did not find an association between hsCRP and serum CTX at baseline. However, we observed a significant negative correlation between hsCRP and PINP at baseline, indicating reduced osteoblastic bone formation in patients with chronic inflammation. This is in agreement with histomorphometry of bone biopsy specimens indicating reduced bone formation in non-steroid-treated patients with rheumatoid arthritis [26] and with a reduction in the markers of bone formation in juvenile chronic arthritis [27].
In agreement with previous studies in healthy subjects [16, 17, 28, 29] and in patients suffering from various medical pathologies requiring steroid therapy [16, 17, 28, 29], we observed a significant drop in serum OC and PINP concentrations after starting treatment with GCs. Gene expression of both OC and procollagen-α1(I) is directly downregulated by GCs [30]. In this study, a significant reduction in serum OPG is in good agreement with inhibition by dexamethasone of OPG in human osteoblastic lineage cells [31]. OPG functions as a decoy receptor that is able to neutralize both the cell-bound and soluble forms of RANKL. In mice, the suppressive effect of GCs on spinal BMD, cortical thickness, and strength was prevented by OPG [32].
Interestingly enough, a decrease in the serum markers of bone formation was accompanied by a significant reduction in serum sclerostin. Osteocytes, but no other cells of the osteoblastic lineage, express sclerostin, a Runx2-dependent product of the SOST gene. Sclerostin is a potent antagonist of bone morphogenetic proteins critical for osteoblastogenesis (BMP −2, −4, −5, −6, and −7) and appears to bind to lipoprotein-related receptors 5 and 6 (LRP5 and LRP6) to inhibit canonical Wnt/β-catenin signaling [33]. Locally, sclerostin acts as a negative regulator of late-osteoblast/preosteocyte differentiation, inhibits osteoblast proliferation, promotes osteoblast apoptosis, and suppresses mineralization of osteoblastic cells [34]. Loss of sclerostin in humans causes the high-bone mass disorders Van Buchem disease [35] and sclerosteosis [36], and administration of an antisclerostin antibody increases bone formation in mice treated with GCs [37]. It was suggested that transient reductions in sclerostin levels with daily injections of PTH could contribute to the antiapoptotic signaling triggered by this regimen [38]. Conversely, sclerostin stimulates apoptosis of cultured human osteoblastic cells [39], and transgenic mice overexpressing sclerostin exhibit low bone mass. In this study, the significant drop in serum sclerostin was associated with a decrease, rather than an increase, in markers of bone formation, reflecting a GC-induced apoptosis of osteocytes [6, 40]. This is in good agreement with decreased circulating sclerostin levels in patients with endogenous hypercortisolism, which increase during biochemical remission of the disease [41].
The modest increase in serum βCTX peaking at 24–48 h of GC treatment is consistent with previous reports [16, 19]. Simultaneously, we observed only a trend to increase in serum sRANKL, which is reminiscent of the poor and nonconsistent association between circulating OPG and RANKL with biochemical markers of bone turnover and BMD [42], although when measured in the bone marrow high correlations can be observed [43]. Also, lack of sensitivity of currently available assays may impair correlation analysis with conventional bone marker measurements. Although GCs stimulate RANKL synthesis and reduce osteoclast death by apoptosis [6], the ability of osteoclasts to resorb bone is impaired due to cytoskeletal abnormalities that prevent osteoclasts from anchoring efficiently bone and developing an adequate brush border. The response of osteoclasts to macrophage colony-stimulating factor, a cytokine produced by osteoblasts, is specifically impaired [7].
In this study, a significant positive correlation was observed between increase in serum βCTX and Dkk-1, another Wnt inhibitor. Although Dkk-1 disrupts the Wnt cascade by binding to Wnt coreceptors LRP5 and LRP6, resulting in the inhibition of osteoblast differentiation [44], it could lead to increased osteoclastic activity and overall bone turnover through enhanced osteoblast-dependent osteoclastogenesis by upregulating RANKL and/or downregulating OPG [45]. Expression of Dkk-1 in human osteoblasts and osteocytes is enhanced by GCs and may lead to enhanced osteoblast-dependent osteoclastogenesis [46], osteoblast apoptosis, and bone mass loss [47, 48].
Dickkopf-1 is highly expressed in osteocytes as well as in several other cell types. Despite this, serum concentrations of Dkk-1 are assumed to reflect expression of Dkk-1 in the bone microenvironment and predict the extent of some bone diseases [49, 50]. In a cohort study in postmenopausal women with established osteoporosis, serum Dkk-1 levels were significantly higher in osteoporotic women compared with controls [51].
Despite an initial significant negative correlation between hsCRP and PINP values, administration of GCs was associated with a significant drop in both serum hsCRP and PINP concentrations. The positive correlation between hsCRP and the sRANKL/OPG ratio after GC administration was driven mainly by the drop in serum OPG concentrations. Thus, in this study, the reduced inflammation was not associated with reduction in sRANKL and serum CTX but, rather, was associated with decreased serum concentrations of markers synthesized by osteoblasts and osteocytes (PINP, OC, OPG, and sclerostin). The results are in good agreement with negative effects of GCs on bone remodeling; however, they do not support a causal relationship between CRP, a sensitive marker of chronic, low-grade systemic inflammation, and the response of bone turnover markers to GC.
Several limitations of the study must be taken into account. First, due to the pilot observational design of the study and the small number of subjects, the conclusions must be interpreted with caution. The relationship between hsCRP and PINP in non-steroid-treated patients with diseases has not been studied previously and requires confirmation by a larger study. Long-term blood sampling and BMD measurements would be required to study changes and differences in the markers between different dosages of GCs. Second, it is unclear to what extent serum concentrations of sclerostin and RANKL correlate with local cytokine production or action within the bone microenvironment. In addition, we did not measure inflammatory cytokines, such as IL-1, IL-6, and TNF-α. Third, our group of adult patients suffering from various medical pathologies requiring systemic steroid therapy was heterogeneous in terms of age, menopausal status, inflammatory activity of the primary disease, and vitamin D serum concentrations. The latter reflects real clinical practice where initiation of GC therapy cannot be held off until vitamin D saturation. Three of the patients were treated with hydrochloroquine, a known inhibitor of 25-(OH)D-1α-hydroxylase which could result in low serum 1,25(OH)2D levels with consequent effects on osteoblasts. However, excluding these patients did not modify the results significantly (data not shown). The number of subjects in this study was too small to allow a search for differences among subgroups and perhaps to see an expected correlation between 25(OH)D levels and PTH. We acknowledge that, for ethical reasons, each patient could not be used as his or her own control. This cannot be substituted with the current control group. Therefore, the changes in the markers after administration of GCs were compared with the baseline values, and the control group was used to document the reproducibility of the measurements in healthy adults.
In conclusion, medium-dose, short-term oral GC regimens cause an immediate decrease of the biochemical markers of osteoblast and osteocyte activity (PINP, OC, OPG, and sclerostin) and a moderate increase of the biochemical marker of bone resorption (βCTX). Other randomized studies are warranted to test the markers and mediators of the effects of GCs on bone to identify high–fracture risk patients and to implement preventive therapy before rapid bone loss occurs.
References
Diez-Perez A, Hooven FH, Adachi JD, Adami S, Anderson FA, Boonen S, Chapurlat R, Compston JE, Cooper C, Delmas P, Greenspan SL, Lacroix AZ, Lindsay R, Netelenbos JC, Pfeilschifter J, Roux C, Saag KG, Sambrook P, Silverman S, Siris ES, Watts NB, Nika G, Gehlbach SH (2011) Regional differences in treatment for osteoporosis. The Global Longitudinal Study of Osteoporosis in Women (GLOW). Bone 49:493–498
Henneicke H, Herrmann M, Kalak R, Brennan-Speranza TC, Heinevetter U, Bertollo N, Day RE, Huscher D, Buttgereit F, Dunstan CR, Seibel MJ, Zhou H (2011) Corticosterone selectively targets endo-cortical surfaces by an osteoblast-dependent mechanism. Bone 49:733–742
Van Staa TP, Leufkens HG, Abenhaim L, Zhang B, Cooper C (2000) Use of oral corticosteroids and risk of fractures. J Bone Miner Res 15:993–1000
Canalis E, Mazziotti G, Giustina A, Bilezikian JP (2007) Glucocorticoid-induced osteoporosis: pathophysiology and therapy. Osteoporos Int 18:1319–1328
Yao W, Cheng Z, Busse C, Pham A, Nakamura MC, Lane NE (2008) Glucocorticoid excess in mice results in early activation of osteoclastogenesis and adipogenesis and prolonged suppression of osteogenesis: a longitudinal study of gene expression in bone tissue from glucocorticoid-treated mice. Arthritis Rheum 58:1674–1686
Weinstein RS (2010) Glucocorticoids, osteocytes, and skeletal fragility: the role of bone vascularity. Bone 46:564–570
Kim HJ, Zhao H, Kitaura H, Bhattacharyya S, Brewer JA, Muglia LJ, Ross FP, Teitelbaum SL (2006) Glucocorticoids suppress bone formation via the osteoclast. J Clin Invest 116:2152–2160
Smith E, Frenkel B (2005) Glucocorticoids inhibit the transcriptional activity of LEF/TCF in differentiating osteoblasts in a glycogen synthase kinase-3beta-dependent and -independent manner. J Biol Chem 280:2388–2394
Ohnaka K, Tanabe M, Kawate H, Nawata H, Takayanagi R (2005) Glucocorticoid suppresses the canonical Wnt signal in cultured human osteoblasts. Biochem Biophys Res Commun 329:177–181
O’Brien CA, Jia D, Plotkin LI, Bellido T, Powers CC, Stewart SA, Manolagas SC, Weinstein RS (2004) Glucocorticoids act directly on osteoblasts and osteocytes to induce their apoptosis and reduce bone formation and strength. Endocrinology 145:1835–1841
Xia X, Kar R, Gluhak-Heinrich J, Yao W, Lane NE, Bonewald LF, Biswas SK, Lo WK, Jiang JX (2010) Glucocorticoid-induced autophagy in osteocytes. J Bone Miner Res 25:2479–2488
Guo J, Liu M, Yang D, Bouxsein ML, Saito H, Galvin RJ, Kuhstoss SA, Thomas CC, Schipani E, Baron R, Bringhurst FR, Kronenberg HM (2010) Suppression of Wnt signaling by Dkk1 attenuates PTH-mediated stromal cell response and new bone formation. Cell Metab 11:161–171
Nakashima T, Hayashi M, Fukunaga T, Kurata K, Oh-Hora M, Feng JQ, Bonewald LF, Kodama T, Wutz A, Wagner EF, Penninger JM, Takayanagi H (2011) Evidence for osteocyte regulation of bone homeostasis through RANKL expression. Nat Med 17:1231–1234
Dempster DW (1989) Bone histomorphometry in glucocorticoid-induced osteoporosis. J Bone Miner Res 4:137–141
Lane NE, Yao W, Balooch M, Nalla RK, Balooch G, Habelitz S, Kinney JH, Bonewald LF (2006) Glucocorticoid-treated mice have localized changes in trabecular bone material properties and osteocyte lacunar size that are not observed in placebo-treated or estrogen-deficient mice. J Bone Miner Res 21:466–476
Dovio A, Perazzolo L, Osella G, Ventura M, Termine A, Milano E, Bertolotto A, Angeli A (2004) Immediate fall of bone formation and transient increase of bone resorption in the course of high-dose, short-term glucocorticoid therapy in young patients with multiple sclerosis. J Clin Endocrinol Metab 89:4923–4928
Ekenstam E, Stalenheim G, Hallgren R (1988) The acute effect of high dose corticosteroid treatment on serum osteocalcin. Metabolism 37:141–144
Ton FN, Gunawardene SC, Lee H, Neer RM (2005) Effects of low-dose prednisone on bone metabolism. J Bone Miner Res 20:464–470
Szappanos A, Toke J, Lippai D, Patocs A, Igaz P, Szucs N, Futo L, Glaz E, Racz K, Toth M (2010) Bone turnover in patients with endogenous Cushing’s syndrome before and after successful treatment. Osteoporos Int 21:637–645
Kearns AE, Khosla S, Kostenuik PJ (2008) Receptor activator of nuclear factor kappaB ligand and osteoprotegerin regulation of bone remodeling in health and disease. Endocr Rev 29:155–192
Schett G, Kiechl S, Weger S, Pederiva A, Mayr A, Petrangeli M, Oberhollenzer F, Lorenzini R, Redlich K, Axmann R, Zwerina J, Willeit J (2006) High-sensitivity C-reactive protein and risk of nontraumatic fractures in the Bruneck study. Arch Intern Med 166:2495–2501
Pasco JA, Kotowicz MA, Henry MJ, Nicholson GC, Spilsbury HJ, Box JD, Schneider HG (2006) High-sensitivity C-reactive protein and fracture risk in elderly women. JAMA 296:1353–1355
Ding C, Parameswaran V, Udayan R, Burgess J, Jones G (2008) Circulating levels of inflammatory markers predict change in bone mineral density and resorption in older adults: a longitudinal study. J Clin Endocrinol Metab 93:1952–1958
Kim BJ, Yu YM, Kim EN, Chung YE, Koh JM, Kim GS (2007) Relationship between serum hsCRP concentration and biochemical bone turnover markers in healthy pre- and postmenopausal women. Clin Endocrinol (Oxf) 67:152–158
Nabipour I, Larijani B, Vahdat K, Assadi M, Jafari SM, Ahmadi E, Movahed A, Moradhaseli F, Sanjdideh Z, Obeidi N, Amiri Z (2009) Relationships among serum receptor of nuclear factor-kappaB ligand, osteoprotegerin, high-sensitivity C-reactive protein, and bone mineral density in postmenopausal women: osteoimmunity versus osteoinflammatory. Menopause 16:950–955
Compston JE, Vedi S, Mellish RW, Croucher P, O’Sullivan MM (1989) Reduced bone formation in non-steroid treated patients with rheumatoid arthritis. Ann Rheum Dis 48:483–487
Pereira RM, Falco V, Corrente JE, Chahade WH, Yoshinari NH (1999) Abnormalities in the biochemical markers of bone turnover in children with juvenile chronic arthritis. Clin Exp Rheumatol 17:251–255
Paglia F, Dionisi S, De Geronimo S, Rosso R, Romagnoli E, Raejentroph N, Ragno A, Celi M, Pepe J, D’Erasmo E, Minisola S (2001) Biomarkers of bone turnover after a short period of steroid therapy in elderly men. Clin Chem 47:1314–1316
Sasaki N, Kusano E, Ando Y, Yano K, Tsuda E, Asano Y (2001) Glucocorticoid decreases circulating osteoprotegerin (OPG): possible mechanism for glucocorticoid induced osteoporosis. Nephrol Dial Transplant 16:479–482
Webster JC, Cidlowski JA (1999) Mechanisms of glucocorticoid-receptor-mediated repression of gene expression. Trends Endocrinol Metab 10:396–402
Hofbauer LC, Gori F, Riggs BL, Lacey DL, Dunstan CR, Spelsberg TC, Khosla S (1999) Stimulation of osteoprotegerin ligand and inhibition of osteoprotegerin production by glucocorticoids in human osteoblastic lineage cells: potential paracrine mechanisms of glucocorticoid-induced osteoporosis. Endocrinology 140:4382–4389
Weinstein RS, O’Brien CA, Almeida M, Zhao H, Roberson PK, Jilka RL, Manolagas SC (2011) Osteoprotegerin prevents glucocorticoid-induced osteocyte apoptosis in mice. Endocrinology 152:3323–3331
van Bezooijen RL, Roelen BA, Visser A, van der Wee-Pals L, de Wilt E, Karperien M, Hamersma H, Papapoulos SE, ten Dijke P, Lowik CW (2004) Sclerostin is an osteocyte-expressed negative regulator of bone formation, but not a classical BMP antagonist. J Exp Med 199:805–814
Li X, Zhang Y, Kang H, Liu W, Liu P, Zhang J, Harris SE, Wu D (2005) Sclerostin binds to LRP5/6 and antagonizes canonical Wnt signaling. J Biol Chem 280:19883–19887
Balemans W, Ebeling M, Patel N, Van Hul E, Olson P, Dioszegi M, Lacza C, Wuyts W, Van Den Ende J, Willems P, Paes Alves AF, Hill S, Bueno M, Ramos FJ, Tacconi P, Dikkers FG, Stratakis C, Lindpaintner K, Vickery B, Foernzler D, Van Hul W (2001) Increased bone density in sclerosteosis is due to the deficiency of a novel secreted protein (SOST). Hum Mol Genet 10:537–543
Brunkow ME, Gardner JC, Van Ness J, Paeper BW, Kovacevich BR, Proll S, Skonier JE, Zhao L, Sabo PJ, Fu Y, Alisch RS, Gillett L, Colbert T, Tacconi P, Galas D, Hamersma H, Beighton P, Mulligan J (2001) Bone dysplasia sclerosteosis results from loss of the SOST gene product, a novel cystine knot-containing protein. Am J Hum Genet 68:577–589
Marenzana M, Greenslade K, Eddleston A, Okoye R, Marshall D, Moore A, Robinson MK (2011) Sclerostin antibody treatment enhances bone strength but does not prevent growth retardation in young mice treated with dexamethasone. Arthritis Rheum 63:2385–2395
Bellido T, Ali AA, Plotkin LI, Fu Q, Gubrij I, Roberson PK, Weinstein RS, O’Brien CA, Manolagas SC, Jilka RL (2003) Proteasomal degradation of Runx2 shortens parathyroid hormone-induced anti-apoptotic signaling in osteoblasts. A putative explanation for why intermittent administration is needed for bone anabolism. J Biol Chem 278:50259–50272
Sutherland MK, Geoghegan JC, Yu C, Turcott E, Skonier JE, Winkler DG, Latham JA (2004) Sclerostin promotes the apoptosis of human osteoblastic cells: a novel regulation of bone formation. Bone 35:828–835
Bonewald LF (2011) The amazing osteocyte. J Bone Miner Res 26:229–238
van Lierop AH, van der Eerden AW, Hamdy NA, Hermus AR, den Heijer M, Papapoulos SE (2012) Circulating sclerostin levels are decreased in patients with endogenous hypercortisolism and increase after treatment. J Clin Endocrinol Metab 97:E1953–E1957
Rogers A, Eastell R (2005) Circulating osteoprotegerin and receptor activator for nuclear factor kappaB ligand: clinical utility in metabolic bone disease assessment. J Clin Endocrinol Metab 90:6323–6331
Eghbali-Fatourechi G, Khosla S, Sanyal A, Boyle WJ, Lacey DL, Riggs BL (2003) Role of RANK ligand in mediating increased bone resorption in early postmenopausal women. J Clin Invest 111:1221–1230
Morvan F, Boulukos K, Clement-Lacroix P, Roman Roman S, Suc-Royer I, Vayssiere B, Ammann P, Martin P, Pinho S, Pognonec P, Mollat P, Niehrs C, Baron R, Rawadi G (2006) Deletion of a single allele of the Dkk1 gene leads to an increase in bone formation and bone mass. J Bone Miner Res 21:934–945
Glass DA 2nd, Karsenty G (2006) Canonical Wnt signaling in osteoblasts is required for osteoclast differentiation. Ann N Y Acad Sci 1068:117–130
Fujita K, Janz S (2007) Attenuation of WNT signaling by DKK-1 and -2 regulates BMP2-induced osteoblast differentiation and expression of OPG, RANKL and M-CSF. Mol Cancer 6:71
Ohnaka K, Taniguchi H, Kawate H, Nawata H, Takayanagi R (2004) Glucocorticoid enhances the expression of Dickkopf-1 in human osteoblasts: novel mechanism of glucocorticoid-induced osteoporosis. Biochem Biophys Res Commun 318:259–264
Wang FS, Ko JY, Yeh DW, Ke HC, Wu HL (2008) Modulation of Dickkopf-1 attenuates glucocorticoid induction of osteoblast apoptosis, adipocytic differentiation, and bone mass loss. Endocrinology 149:1793–1801
Kaiser M, Mieth M, Liebisch P, Oberlander R, Rademacher J, Jakob C, Kleeberg L, Fleissner C, Braendle E, Peters M, Stover D, Sezer O, Heider U (2008) Serum concentrations of DKK-1 correlate with the extent of bone disease in patients with multiple myeloma. Eur J Haematol 80:490–494
Voskaridou E, Christoulas D, Xirakia C, Varvagiannis K, Boutsikas G, Bilalis A, Kastritis E, Papatheodorou A, Terpos E (2009) Serum Dickkopf-1 is increased and correlates with reduced bone mineral density in patients with thalassemia-induced osteoporosis. Reduction post-zoledronic acid administration. Haematologica 94:725–728
Anastasilakis AD, Goulis DG, Polyzos SA, Gerou S, Pavlidou V, Koukoulis G, Avramidis A (2008) Acute changes in serum osteoprotegerin and receptor activator for nuclear factor-kappaB ligand levels in women with established osteoporosis treated with teriparatide. Eur J Endocrinol 158:411–415
Acknowledgments
We acknowledge the professional cooperation of Ms. Ludmila Hauptvoglova. The study was supported by the Grant Agency of Charles University in Prague (GAUK 84208/2008) and by the Ministry of Health (MZd CR 000 237280).
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors have stated that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Brabnikova Maresova, K., Pavelka, K. & Stepan, J.J. Acute Effects of Glucocorticoids on Serum Markers of Osteoclasts, Osteoblasts, and Osteocytes. Calcif Tissue Int 92, 354–361 (2013). https://doi.org/10.1007/s00223-012-9684-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-012-9684-4