Abstract
Osteoporosis and hypertension are two frequent diseases among the aging population that share a similar etiopathology and often coexist. Moreover, treatment of hypertension affects bone mineral density and, therefore, can worsen osteoporosis. This narrative review considers the influence of the main etiologic factors that contribute to the development of hypertension and osteoporosis and examines the effect of the most often used antihypertensives on bones. A computerized literature search of relevant English publications regarding the etiology of hypertension and osteoporosis as well as the impact of antihypertensives on osteoporosis from 1996 to 2011 was completed in October 2011. The latest update in the search was performed from May to June 2012. The most relevant nongenetic factors in the etiology of osteoporosis and hypertension are low calcium intake, vitamin D and vitamin K deficiency, high consumption of sodium salt, and the effects of different forms of nitric oxide. Thiazide diuretics are the only antihypertensives that have a positive influence on bone mineral density. For other antihypertensive drugs, the data are conflicting, indicating that they may have a potentially negative or positive influence on bone mineral density and fracture risk reduction. Some studies did not find a correlation between the use of antihypertensives and bone mineral density. Due to the frequent coexistence of hypertension and osteoporosis, when selecting long-term antihypertensive therapy the potential effects of antihypertensive drugs on development, worsening, or improvement of osteoporosis should also be considered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of osteoporosis and hypertension continues to rise due to the aging population and the impact of lifestyle. There is a high probability of the coexistence of these two diseases [1]. According to data from 2006, more than 200 million people in the world had osteoporosis [2]. In 2000 alone, it was estimated that in Europe there were about 2.7 million fractures in women and men attributed to osteoporosis. The associated direct costs were approximately €36 billion [3]. According to the estimates of the International Osteoporosis Foundation, after the age of 50, osteoporotic fracture will happen to every third woman and every fifth man. In their lifetime, osteoporosis-related fractures occur in 30–50 % of women and 15–30 % of men [4].
Osteoporosis and hypertension share a similar etiopathology that involves a genetic base as well as the influence of various nongenetic factors. The most relevant etiological factors for both diseases are low calcium intake and level, vitamin D and vitamin K deficiency, high consumption of sodium salt, and low or very high nitric oxide levels. Reduction of bone mineral density (BMD) is related to hypertension, and it seems to be one of the major cardiovascular risk factors for fractures [5–7]. Antihypertensive drugs can have a indirect impact on osteoporosis by ameliorating the detrimental effects of high blood pressure as well as the direct effects on bone metabolism, strength, and density [1, 7–10].
The results of more studies that evaluated a relationship between hypertension, antihypertensive medications, and osteoporosis have been published in the last few years. Therefore, the main aim of this narrative review was to consider the most relevant etiologic factors that contribute to the development of hypertension and osteoporosis and to analyze the published data regarding the effect of the most often used antihypertensives on bones.
Methods
A computerized literature search of relevant articles written in English regarding the etiology of hypertension and osteoporosis as well as the impact of antihypertensives on osteoporosis published from 1996 to 2011 was completed in October 2011. An updated search of the literature was performed from May to June 2012.
References of interest were identified through searches of Medline, Web of Science, and Google Scholar. Combinations of search terms were “etiologic factors” and “hypertension/osteoporosis,” “bones,” and “fractures”; “antihypertensive medications” (thiazide diuretics, loop diuretics, angiotensin-converting enzymes inhibitors, beta-blockers, calcium channel blockers, alpha-blockers) and “osteoporosis.” Review articles were also scanned to find additional eligible studies. In addition, the reference lists of all original articles and previous systematic reviews were hand-searched for other relevant articles. Duplicates were removed. The collected pieces of information included an author, year of study and publication, group of antihypertensive or specific drugs that were used, age and size of the studied population. Studies with the following outcomes were included: changes in BMD values expressed in percent change or in grams per centimeter squared, fracture risk expressed as percent change or odds ratio (OR), skeletal effects, bone marrow perfusion, and influence on bone metabolism. Eventually 53 articles were selected for this review.
Relations Between Bone and the Vascular System
In the pathophysiology of osteoporosis and hypertension, the most relevant etiological factors are low intake and level of calcium, vitamin D and vitamin K deficiency, increased intake of sodium salts, and low or very high nitric oxide levels.
Calcium
Calcium, as the main bone mineral, has a great impact upon bone strength and the balance of the bone remodeling process. It has been found that people with hypertension have reduced intestinal absorption and increased calcium urinary elimination, which has, as a consequence, a reduction of calcium concentration in the plasma, secondary activation of parathyroid glands, and increased mobilization of calcium from the bones [1, 5, 6]. Currently, there are two hypotheses to explain the cause of increased renal calcium leak in hypertensive patients: the central blood volume increase hypothesis and the renal calcium leak hypothesis. According to the first hypothesis, an increase of the overall volume enhances calcium urinary excretion. The second hypothesis assumes that calcium leaks because of a disorder at the tubule level. In both cases, the lowering of calcium in the serum activates parathyroid hormone (PTH), which further increases bone turnover [1]. It has been shown in women that the difference in annual bone mass loss depends on systolic blood pressure levels [8]. In men increased systolic blood pressure was statistically significantly correlated with a reduction of BMD in the trochanter (p = 0.04), while increased diastolic blood pressure was related to a reduction of BMD (p ≤ 0.01) and bone mineral content (p ≤ 0.05) of the entire body [5].
Approximately 99 % of overall calcium resides in the bones, mostly in the form of hydroxyapatite crystals. The remaining 1 % of free calcium is in the extracellular fluid and plays an important role in a series of vital processes. At low calcium intake, blood levels are maintained by releasing calcium from the bones. If inadequate calcium levels extend over a longer period of time, the bones become porous and prone to fractures [11, 12].
Calcium acts upon blood pressure, directly increasing peripheral vascular resistance or indirectly by means of other electrolytes, among which sodium is of special importance. Available data show an inverse ratio between calcium levels in vascular smooth muscle cells and bone calcium. When the serum calcium level is low, the calcium concentration in vascular smooth muscle cells is increased, leading to an elevation of vascular resistance and vasoconstriction [12, 13]. Higher amounts of calcium intake enhance the loss of sodium and thus reduce the intravascular volume, which again leads to a reduction of peripheral vascular resistance and blood pressure [5, 13]. Calcium is also important for vascular calcification, which, by cellular mechanisms, resembles the formation and resorption of bones [14]. It has been found that almost all atherosclerotic lesions are calcified and that vascular calcification is a risk factor for increasing the general population’s mortality from cardiovascular diseases [15].
Vitamin D
Vitamin D controls the absorption of calcium and phosphates in the small intestine and increases calcium reabsorption from the kidney tubules and its mobilization from the bones. Vitamin D controls the absorption and reabsorption of calcium by affecting the synthesis of calcium-binding protein, which is important for the calcium transport process. It influences bone formation and bone resorption, stimulates synthesis of osteocalcin (protein of bone matrix), and reduces collagen synthesis while indirectly stimulating the activity and maturation of osteoclasts. The effect of vitamin D on the bones is complex, and its direct impact on calcium mobilization has not yet been completely elucidated. However, it is well known that poor bone mineralization occurs in those individuals who are deficient in vitamin D [11]. Severe vitamin D deficiency causes rickets or osteomalacia, where the new bone, the osteoid, is not mineralized. Less severe vitamin D deficiency causes an increase of serum PTH, which results in high bone turnover and increased bone resorption, causing bone loss and releasing calcium ions into the blood [16, 17]. This can lead to osteoporosis and fractures [16]. Fracture risk is increased regardless of the individual’s BMD as the bone is eroded and the skeleton becomes weak [17]. Additionally, vitamin D has been linked with the maintenance of muscular strength. Patients with vitamin D deficiency (with or without osteoporosis) have reduced muscle mass and strength. It was demonstrated that primarily the weight-bearing antigravity muscles of the lower limb are affected by vitamin D deficiency. This may explain the increased number of falls seen in the vitamin D-deficient elderly [18]. Therefore, increased fracture risk is not only caused by changes in bone remodeling and BMD but also connected with an increased propensity to falls due to the loss of muscular strength [17]. It has been shown that vitamin D supplements in a daily dose greater than 700 IU can reduce the risk of falling [1].
Epidemiological studies suggest that vitamin D insufficiency is related to a number of other disorders frequently observed among the elderly, including cardiovascular disorders such as hypertension [19]. Studies conducted in the general population show that low vitamin D levels (determined by the plasma concentration of 25-hydroxyvitamin D [25(OH)D]) are correlated with higher hypertension prevalence, chronic heart failure, and hyperparathyroidism [20]. There is also an inverse correlation of 25(OH)D plasma concentration with diastolic pressure levels [19].
The mechanisms by which vitamin D affects cardiovascular diseases are different. Vitamin D stimulates the synthesis of prostacyclin in vascular smooth muscle cells. Studies have also shown a positive correlation between 25(OH)D and 1,25-dihydroxyvitamin D (1,25[OH]2D) levels and dilation of blood vessels mediated by the blood flow [20]. In addition, vitamin D inhibits the proliferation of smooth muscle cells in blood vessels, suppresses vascular calcification, and affects the cytokine and renin–angiotensin systems [15, 20].
Vitamin K
There are two different forms of vitamin K: K1 (phylloquinone), which originates mainly from green, leafy vegetables, and K2 (menaquinones, MK), which is produced by bacteria and mostly found in fermented foods such as cheese and fermented soy beans [21, 22]. Vitamin K forms available in food supplements or pharmaceutical preparations are K1, MK-4, and MK-7. In Western society, K2 forms only 10–20 % of the total vitamin K intake. However, K2 is absorbed much better from food than K1 and may represent 50 % of the total vitamin K absorbed [23]. Liver is the main target tissue for vitamin K1. Vitamin K2 is preferentially taken up by extrahepatic tissues such as bone and arteries [21], and some menaquinones seem to have a greater effect in preventing arterial calcification than K1 [22]. Bone and arterial vessel walls, under physiological conditions, can convert K1 into MK-4. Also, there is some evidence that MK-4 could be associated with production of interleukin-6, regulation of prostaglandin E2 synthesis, or inhibition of the mevalonate pathway [22].
Both forms of vitamin K are coenzymes of γ-glutamyl carboxylase, and they are important for formation of K-dependent γ-carboxyglutamate (GLa) proteins [24] that regulate blood coagulation, vascular calcification, bone mineralization, cell growth, and apoptosis [25]. Vitamin K2, however, is more effective than vitamin K1 with respect to osteoclastogenesis; likewise, hypocholesterolemic effects and the ability to slow atherosclerotic progression have only been observed with vitamin K2 [22]. GLa proteins important for bone metabolism are bone GLa-protein osteocalcin synthesized by osteoblasts and matrix GLa-protein (MGP), synthesized primarily by chondrocytes and vascular smooth muscle cells [25, 26]. Vitamin K deficiency can lead to suboptimal γ-carboxylation and production of functionally defective GLa proteins as well as impairment of their function [24, 26]. MGP is the strongest inhibitor of tissue calcification presently known [25]. γ-Carboxylation is essential for the MGP inhibitory effect on calcification. Undercarboxylated MGP and impaired vitamin K status have been associated with vascular calcification and cardiovascular mortality [24–26].
Osteocalcin GLa residues bind and incorporate calcium into hydroxyapatite crystals [24]. Reduced vitamin K availability leads to the synthesis of undercarboxylated osteocalcin, which has low affinity for the hydroxyapatite bone matrix; therefore, an insufficient amount of calcium is incorporated into bones and BMD decreases [21, 24]. Several clinical trials indicated that vitamin K supplementation may result in decreased bone loss and maintenance of bone strength [25]. It has been shown that 3-year coadministration of vitamin K1, minerals, and vitamin D substantially reduced bone loss at the femoral neck in healthy postmenopausal women. The difference between women receiving vitamin K1, minerals, and vitamin D and placebo group was 1.7 % (95 % Cl: 0.35–3.44), while the difference between group receiving minerals and vitamin D was 1.3 % (95 % Cl: 0.10–3.41). A meta-analysis which pooled data from seven trials found that oral supplementation with menaquinone reduced bone loss and prevented fractures; ORs for vertebral, hip, and all nonvertebral fractures were 0.40 (95 % CI 0.25–0.65), 0.23 (95 % CI 0.12–0.47), and 0.19 (95 % CI 0.11–0.35), respectively [27]. The recommended daily intake of vitamin K for prevention of vascular calcification and bone loss needs to be determined.
Sodium
The intake of certain cations through food can affect osteoporosis and hypertension. For instance, high sodium intake through sodium salts can lead to salt-induced volume expansion, increased glomerular filtration rate (GFR), and increased calcium excretion [6]. In addition, due to competition between sodium and calcium ions, reabsorption of calcium in the kidney is decreased [28]. When the absorbed calcium is less than the amount needed to offset this loss, bone remodeling activity is elevated and calcium is released from bone [28]. In women, there is an inverse ratio between sodium intake (measured as Na+/creatinine in urine) and BMD of the hip and lumbar spine [29]. Reduced sodium intake can have a positive effect on the balance of calcium and the lowering of blood pressure [6]. During very small intake or sodium losses, the body can effectively prevent the development of sodium deficiency by decreasing the blood pressure. In contrast, in cases of high sodium intake, the sodium balance is maintained by the rise of blood pressure and excretion of excess sodium by the pressure–natriuresis mechanism [30].
Nitric Oxide
Nitric oxide (NO) is another factor that has an essential role in bone and blood vessel function. NO causes vasodilation and contributes to the physiological control of blood pressure. In addition, NO protects against atherogenesis by inhibiting adhesion and aggregation of thrombocytes as well as proliferation of smooth muscles [31]. The NO effect on bones appears to be dose-dependent and relies upon the activities of different forms of NO synthases or on NO levels. Lack of a constitutive form of NO synthase accelerates atherosclerosis and osteoporosis, while inducible NO synthase, i.e., high concentrations of NO, enhances bone loss by increasing osteoclastic bone resorption, inhibiting osteoblast proliferation, and increasing osteoblast apoptosis [15, 32]. It has been shown that NO donors in vitro decrease bone resorption by reducing the number and activity of osteoclasts and increase the proliferation and differentiation of osteoblasts, osteocalcin synthesis, and mineralization by osteoblastic cells [32, 33].
The in vivo effects of NO donors were examined in several studies, resulting in conflicting outcomes. A large epidemiological study of nitrate use in 124,655 individuals (2,000 cases and 373,962 age- and sex-matched controls) who had sustained a fracture showed that the use of nitrates was associated with an 11 % reduction of the likelihood for the risk of any fracture (adjusted OR = 0.89, 95 % CI 0.86–0.92) and a 15 % reduction of the likelihood for the risk of hip fracture (adjusted OR = 0.85, 95 % CI 0.79–0.92) [34]. Also, a small, randomized, open-label study which involved young premenopausal women undergoing oophorectomy, who received either standard hormone replacement therapy or nitroglycerin ointment, showed that nitroglycerin therapy was as effective as estrogen in preventing bone loss [35]. On the other hand, a larger randomized, double-blind, placebo-controlled clinical trial by the same group of investigators showed no benefit of transdermal nitroglycerin in preventing bone loss in early postmenopausal women [36]. Frequent headache causing suboptimal adherence to treatment was given as a possible explanation for the negative findings [32]. Another randomized, double-blind, placebo-controlled clinical trial on the use of transdermal nitroglycerin in postmenopausal women showed modestly increased BMD and decreased bone resorption [33]. Further studies are necessary to determine not only the influence of NO donors on BMD but also the influence on fracture risk [32].
Antihypertensives and Bones
Certain groups of antihypertensive drugs have been shown to increase BMD and reduce the risk of fractures. However, the question is whether antihypertensives have a specific direct or indirect effect on bones due to the blood pressure decrease and the consequential effect on calcium metabolism. It has been shown that people using certain antihypertensives have a lower fracture risk than the general population, which favors the assumption that antihypertensives have a direct effect on bones [8].
It has been confirmed that thiazide diuretics have a positive effect on BMD. However, for other groups of antihypertensives, the data are controversial (Table 1). In some studies antihypertensives showed a potentially negative effect on bones [41, 42], while in other studies there is no correlation between the use of antihypertensives and their effect on bones [43, 44]. However, a number of studies show a positive effect of antihypertensive drugs on BMD and reduction of fracture risk [8–10].
It is believed that antihypertensive medications can worsen orthostatic hypotension. However, the majority of studies have not found an association or have even demonstrated an improvement in postural blood pressure changes in patients on antihypertensive medications. When considering the individual classes, peripheral vasodilators, specifically alpha-adrenoceptor antagonists and nondihydropyridine calcium channel antagonists, can exacerbate postural blood pressure changes and lead to orthostatic hypotension and, therefore, should be avoided in the elderly. Angiotensin-converting enzyme inhibitors, angiotensin-receptor antagonists, and beta-blockers with intrinsic sympathomimetic activity are less likely to worsen orthostatic hypotension. Careful management of electrolyte disturbance can decrease the risk of developing orthostatic hypotension with diuretic use [45].
Thiazide Diuretics
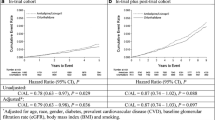
Thiazides have been examined in hypertensive and normotensive individuals; the first data about a positive effect on BMD and reduction of fracture risk date back from the early 1990s [46–48]. In a randomized, double-blind, and placebo-controlled study conducted in normotensive examinees, the use of thiazide diuretics led to the preservation of BMD in the hips and spine [49]. In a prospective cohort study, thiazides reduced the risk for hip fracture (adjusted hazard ratio = 0.46, 95 % CI 0.21–0.96) in the general population, but this protective effect disappeared 4 months after the cessation of their use [50]. Other studies also confirmed a positive effect of thiazides on BMD in postmenopausal women, normotensive examinees, and the general population [9, 10, 51]. A summary of thiazide diuretics effects is given in Table 2.
Thiazides can have direct and indirect effects on the cells involved in bone metabolism by affecting electrolyte discharge in the kidneys [1, 12]. In sodium and calcium homeostasis thiazides act by inhibition of cotransporters for sodium and chlorine (SCCTs) in the nephron and bones [1]. In the distal tubule SCCTs are responsible for reabsorption of sodium and chlorine. SCCT gene mutation can lead to the preservation of sodium and consequential volume enhancement, which causes increased urinary calcium excretion. According to some authors, mutations of the gene for this cotransporter could be correlated with both osteoporosis and hypertension [52]. Thiazides inhibit SCCTs, reduce sodium reabsorption, and increase urinary loss of sodium. A decrease in the level of sodium consequentially leads to calcium leak. The hypocalciuric effect increases the availability of calcium, lowers PTH level, and reduces bone metabolism [1]. Increased sodium loss is accompanied by a respective chlorine loss so that, in order to preserve electroneutrality, reabsorption of bicarbonates is increased [53]. Elevated bicarbonate concentration in the serum leads to mild metabolic alkalosis. This mild metabolic alkalosis reduces the bones’ buffer activity as well as bone mass loss, which might be due to increased acidity induced by intake of food causing an acidic reaction in the organism [10].
Angiotensin-Converting Enzyme Inhibitors
It is assumed that angiotensin acts on bones directly via angiotensin AT1 receptors on osteoblasts and stimulates the release of mediators which activate osteoclasts and indirectly by regulating blood flow in the bone marrow capillaries. It has been shown that angiotensin II affects calcium metabolism by causing a drop in free calcium plasma concentration while simultaneously increasing PTH. Angiotensin-converting enzyme inhibitors (ACEIs) are thought to block these effects of angiotensin [8, 9].
There are fewer data for ACEIs than for thiazide diuretics, and they mostly date from the post-year 2000 period. All of the available data discuss the positive effect of ACEIs on bones. The potential benefit for bones is shown (increase of BMD at some regions) by the use of ACEIs in hypertensive patients at risk for osteoporosis [9]. In patients who used ACEIs, the adjusted risk for any fracture was reduced by 7 % (OR = 0.93, 95 % CI 0.90–0.96) compared to the control group [8]. Still, studies conducted so far are very few in number and have their limitations, and there is no conclusive consensus concerning the effect of ACEIs on BMD. Also, it is possible that different responses to antihypertensive treatment with ACEIs are due to an ACE insertion/deletion genetic polymorphism [24, 54]. The deletion D allele has been shown to result in increased expression of the ACE gene, and interestingly the DD genotype is associated with an increased risk of hypertension, diabetic renal disease, and cardiovascular complications [54]. Subjects with the DD polymorphism seem to respond better to antihypertensives with respect to bone mass, whereas those with the ID exhibit a poor response to antihypertensives [24]. A summary of the ACEI effect is given in Table 3.
For angiotensin receptor blockers, it is assumed that the mechanism of the effect on bones could be similar to that of ACEIs [1, 8], but there are considerably fewer data on angiotensin receptor blockers. The use of an angiotensin AT1 receptor blocker, olmesartan, appeared to attenuate osteoclast activation with angiotensin II [24].
Beta-Blockers
Many osteoblasts in the bone marrow have been noted as localized immediately close to sympathetic neurons. It has been shown in both in vitro (on cell lines of bone marrow) and in vivo (on animal models) studies that antagonists and agonists of beta-adrenergic receptors have an effect on bone metabolism. In humans, beta2-adrenergic receptors have been identified on osteoblasts and osteoclasts [37]. It is assumed that the beta-blocker effect on bones is related to the role of the sympathetic nervous system in the regulation of bone metabolism [8, 37].
The effect of beta-blockers on human bones has been considered in only a few studies, while beta-adrenergic stimulation and inhibition showed anabolic and catabolic effects on the bones [8]. The limitation of these observational studies lies in the fact that beta-blockers are prescribed for different indications and comedication.
In a study of perimenopausal women who used beta-blockers, mostly for hypertension, there was no significant difference in BMD between treated and untreated women but there was a reduction of osteoblast activity and a threefold increased risk of fracture [41]. A study that monitored women who had been on beta-blockers for 7 years, mostly for hypertension, did not show any consistent correlation between the use of these medications and changes in BMD and fracture risk [43]. Contrary to these findings, the results of two studies from 2004 indicate a BMD increase and lower fracture risk in women over 50 years (adjusted OR = 0.68, 95 % CI 0.49–0.96) [37] and lower fracture risk in the general population for both men and women (overall adjusted OR = 0.77, 95 % CI 0.72–0.83) on beta-blocker therapy [55]. A 9 % reduction in bone fracture risk (adjusted OR = 0.91, 95 % CI 0.88–0.93) in people who used beta-blockers has been confirmed in a large pharmacoepidemiological study done in Denmark in 2006 [8].
The results of a large number of epidemiological studies point to a useful effect of beta-blockers on bone mass or fractures. A recent meta-analysis of eight studies has shown that beta-blockers reduce the risk of hip fracture (RR = 0.72, 95 % CI 0.63–0.81) or any other fracture (RR = 0.86, 95 % CI 0.76–0.98). However, many of the studies are observational. Prospective randomized clinical studies are needed that would take into consideration the doses of beta-blockers and the differences among them [56, 57]. A summary of the beta-blocker effects is given in Table 4.
Calcium Channel Blockers
The effect of calcium channel blockers (CCBs) on bone metabolism was examined in the 1990s in a few studies with a small number of examinees (n = 10–20). The collected data have not shown any considerable effect of calcium antagonists on bone metabolism. Yet, in view of the fact that the number of examinees was small, there is no clear estimate of the effect of CCBs on the indicators of bone tissue homeostasis. One of the assumptions is that long-term use of CCBs can be related to osteoporosis, due to reduction of bone marrow perfusion, shown in healthy volunteers [38]. On the other hand, no evidence for an altered fracture risk for users of CCBs was shown in a case–control fracture study [55]. Also, in a pharmacoepidemiological study, conducted in the general population with a larger number of examinees, CCBs reduced the risk of fractures by 6 % (adjusted OR = 0.94, 95 % CI 0.91–0.96). The decreased risk is larger with the use of CCBs that are not derivates of dihydropyridine [8]. A summary of the calcium antagonist effects is given in Table 5.
The mechanism by which CCBs influence bones is not yet clear. It has been shown that nifedipine inhibits PTH secretion in postmenopausal women suffering from osteoporosis, while verapamil reduces the secretion of osteocalcin and inhibits the PTH-stimulated takeover of calcium in osteoblasts [38, 39].
Loop Diuretics
Loop diuretics are the only group of antihypertensives in which existing studies mostly point to a negative effect on BMD. The possible reason for this is that they increase calcium leak in the kidneys, the level of PTH, and 1,25(OH)2D in the plasma. In one case–control study in patients who used loop diuretics, the adjusted risk for hip fracture increased 16 % (OR = 1.16, 95 % CI 1.10–1.23), while the risk for any kind of fracture increased 4 % (OR = 1.04, 95 % CI 1.01–1.07) [40]. In a 1-year, randomized, double-blind, placebo-controlled study conducted in 87 postmenopausal women, bumetanide decreased BMD in the hip by 2 % and BMD in the entire body by 1.4 % [42].
Alpha-Blockers
As for the effect of other antihypertensives on bones, such as alpha-blockers, there are no data from pharmacoepidemiological studies, probably because they are considerably less used antihypertensives. It is not known if alpha-blockers have a direct effect on bones, but it has been shown that they indirectly increase the risk of hip or femur fractures in men. They induce, with their vasodilatory effect, faintness, weakness, postural hypotension, and syncope, thus increasing the risk of falls and fractures. The use of other antihypertensive agents, like beta-blockers, diuretics, calcium channel blockers, and ACEIs, was not associated with an increased risk of hip/femur fractures, thus supporting a direct effect of alpha-blockers [58].
Conclusion
Osteoporosis and hypertension are asymptomatic diseases with common etiological factors and an increased incidence of complications in the aging population. Antihypertensives are widely used in older patients. Due to the frequent coexistence of hypertension and osteoporosis, the choice of antihypertensive therapy should take into consideration their effect on bones and fracture risk.
For the time being, thiazide diuretics are the only antihypertensives that have been confirmed to have a positive effect on the preservation of BMD and to reduce the risk of fracture. Since there are negative findings about loop diuretics’ effect on bones for those patients who are at an increased risk for osteoporosis or already have osteoporosis, preference should be given to thiazide diuretics. Based upon current results, we cannot estimate with certainty the effect of inhibitors of angiotensin-converting enzyme, antagonists of angiotensin receptors, alpha- or beta-blockers, and calcium channel blockers on bones. Further research is needed in order to confirm their possible positive or negative effects.
This narrative review has certain limitations. First, the analysis was based only on published data and complete retrieval was not possible. Further, study populations were heterogenous in terms of patients’ age, gender, comorbidities, and ethnic origin. Also, the effect of a particular antihypertensive on bones can depend on its duration of use. The reviewed articles included different types of studies ranging from randomized clinical trials to pharmacoepidemiological studies.
References
Pérez-Castrillόn JL, Justo I, Sanz-Cantalapiedra A, Pueyo C, Hernández G, Dueñas A (2005) Effect of the antihypertensive treatment on the bone mineral density and osteoporotic fracture. Curr Hypertens Rev 1:61–66
Reginster JY, Burlet N (2006) Osteoporosis: a still increasing prevalence. Bone 38:S4–S9
European Society for Clinical and Economic Aspect of Osteoporosis and Osteoarthritis (2008) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 19:399–428
International Osteoporosis Foundation. Osteoporosis general. http://www.iofbonehealth.org/facts-and-statistics.html. Accessed 14 July 2009
Metz JA, Morris CD, Roberts LA, McClung MR, McCarron DA (1999) Blood pressure and calcium intake are related to bone density in adult males. Br J Nutr 81:383–388
Cappucio FP, Meilahn E, Zmuda JM, Cauley JA (1999) High blood pressure and bone-mineral loss in elderly white women: a prospective study. Study of Osteoporotic Fractures Research Group. Lancet 354:971–975
Vestergaard P, Rejnmark L, Mosekilde L (2009) Hypertension is a risk factor for fractures. Calcif Tissue Int 84:103–111
Rejnmark L, Vestergaard P, Mosekilde L (2006) Treatment with beta-blockers, ACE inhibitors, and calcium-channel blockers is associated with a reduced fracture risk: a nationwide case-control study. J Hypertens 24:581–589
Lynn H, Kwok T, Wong SYS, Woo J, Leung PC (2006) Angiotensin converting enzyme inhibitor use is associated with higher bone mineral density in elderly Chinese. Bone 38:584–588
Ott SM, LaCroix AZ, Scholes D, Ichikawa L, Wu K (2008) Effects of three years of low-dose thiazides on mineral metabolism in healthy elderly persons. Osteoporos Int 19:1315–1322
Rang HP et al. (2012) Bone metabolism. In: Rang and Dale`s pharmacology. 7th ed, Churchill Livingstone, Elsevier, Philadelphia, pp 432–441
Power ML, Heaney RP, Kalkwarf HJ et al (1999) The role of calcium in health and disease. Am J Obstet Gynecol 181:1560–1569
Zemel MB (2001) Calcium modulation of hypertension and obesity: mechanisms and implications. J Am Coll Nutr 20:428S–435S
McFarlane SI, Muniyappa R, Shin JJ, Bahtiyar G, Sowers JR (2004) Osteoporosis and cardiovascular disease: brittle bones and boned arteries, is there a link? Endocrine 23(1):1–10
Zitterman A, Schleithoff SS, Koerfer R (2005) Putting cardiovascular disease and vitamin D insufficiency into perspective. Br J Nutr 94:483–492
Lips P (2006) Vitamin D physiology. Prog Biophys Mol Biol 92:4–8
Boonen S, Vanderschueren D, Haentjens P, Lips P (2006) Calcium and vitamin D in the prevention and treatment of osteoporosis—a clinical update. J Intern Med 259:539–552
Glerup H, Mikkelsen K, Poulsen L, Hass E, Overbeck S, Andersen H et al (2000) Hypovitaminosis D myopathy without biochemical signs of osteomalacic bone involvement. Calcif Tissue Int 66(6):419–424
Mosekilde L (2005) Vitamin D and the elderly. Clin Endocrinol (Oxf) 62:265–281
London GM, Guérin AP, Verbeke FH et al (2007) Mineral metabolism and arterial functions in end-stage renal disease: potential role of 25-hydroxyvitamin D deficiency. J Am Soc Nephrol 18:613–620
Braam LA, Knapen MH, Geusens P et al (2003) Vitamin K1 supplementation retards bone loss in postmenopausal women between 50 and 60 years of age. Calcif Tissue Int 73:21–26
Vermeer C, Shearer M, Zittermann A et al (2004) Beyond deficiency: potential benefits of increased intakes of vitamin K for bone and vascular health. Eur J Nutr 43:325–335
Knapen MH J, Schurgers L, Vermeer C (2007) Vitamin K2 supplementation improves hip bone geometry and bone strength indices in postmenopausal women. Osteoporos Int 18:963–972
Anagnostis P, Karagiannis A, Kakafika AI, Tziomalos K, Athyros VG, Mikhailidis DP (2009) Atherosclerosis and osteoporosis: age-dependent degenerative processes or related entities? Osteoporos Int 20:197–207
Cranenburg CME, Schurgers JL, Vermeer C (2007) Vitamin K: The coagulation vitamin that became omnipotent. Thromb Haemost 98:120–125
Adams J, Pepping J (2005) Vitamin K in the treatment and prevention of osteoporosis and arterial calcification. Am J Health Syst Pharm 62
Cockayne S, Adamson J, Lanham-New S, Shearer M, Gilbody S, Torgerson D (2006) Vitamin K and the prevention of fractures—systematic review and meta-analysis of randomized controlled trials. Arch Intern Med 166:1256–1261
Heaney PR (2006) Role of dietary sodium in osteoporosis. J Am Coll Nutr 25(3):271S–276S
Woo J, Kwok T, Leung J, Tang N (2009) Dietary intake, blood pressure and osteoporosis. J Hum Hypertens 23:451–455
Karppanen H, Karppanen P, Mervaala E (2005) Why and how to implement sodium, potassium, calcium, and magnesium changes in food items and diets? J Hum Hypertens 19:S10–S19
Rang HP et al. (2012) The vascular system. In: Rang and Dale`s Pharmacology. 7th ed, Churchill Livingstone, Elsevier, Philadelphia, pp 265–282
Khosla S (2011) Is nitroglycerin a novel and inexpensive treatment for osteoporosis? JAMA 305(8):826–827
Jamal SA, Hamilton CJ, Eastell R, Cummings SR (2011) Effect of nitroglycerin ointment on bone density and strength in postmenopausal women. JAMA 05(8):800–807
Rejnmark L, Vestergaard P, Mosekilde L (2006) Decreased fracture risk in users of organic nitrates: a nationwide case-control study. J Bone Miner Res 21(11):1811–1817
Wimalawansa SJ (2000) Nitroglycerin therapy is as efficacious as standard estrogen replacement therapy (Premarin) in prevention of oophorectomy-induced bone loss: a human pilot clinical study. J Bone Miner Res 15(11):2240–2244
Wimalawansa SJ, Grimes JP, Wilson AC, Hoover DR (2009) Transdermal nitroglycerin therapy may not prevent early postmenopausal bone loss. J Clin Endocrinol Metab 94(9):3356–3364
Pasco JA, Henry MJ, Sanders KM, Kotowicz MA, Seeman E, Nicholson GC (2004) Beta-adrenergic blockers reduce the risk of fracture partly by increasing bone mineral density: Geelong osteoporosis study. J Bone Miner Res 19:19–24
Shih TTF, Chang CJ, Tseng WYI et al (2004) Effect of calcium channel blockers on vertebral bone marrow perfusion of the lumbar spine. Radiology 231:24–30
Žofkova I, Kancheva RL (1995) The effect of nifedipine on serum parathyroid hormone and calcitonin in postmenopausal women. Life Sci 57(11):1087–1096
Rejnmark L, Vestergaard P, Mosekilde L (2006) Fracture risk in patients treated with loop diuretics. J Intern Med 259:117–124
Rejnmark L, Vestergaard P, Kassem M et al (2004) Fracture risk in perimenopausal women treated with beta-blockers. Calcif Tissue Int 75:365–372
Rejnmark L, Vestergaard P, Heickendorff L, Andreasen F, Mosekilde L (2006) Loop diuretics increase bone turnover and decrease BMD in osteopenic postmenopausal women: results from a randomized controlled study with bumetanide. J Bone Miner Res 21:163–170
Reid IR, Gamble GD, Grey AB et al (2005) β-blocker use, BMD, and fractures in the study of osteoporotic fractures. J Bone Miner Res 20:613–618
Zacharieva S, Shigarminova R, Nachev E et al (2003) Effect of amlodipine and hormone replacement therapy on blood pressure and bone markers in menopause. Methods Find Exp Clin Pharmacol 25(3):209
Hajjar I (2005) Postural blood pressure changes and orthostatic hypotension in the elderly patient: impact of antihypertensive medications. Drugs Aging 22(1):55–68
Sowers MR, Clark MK, Jannausch ML, Wallace RB (1993) Body size, estrogen use and thiazide diuretic use affect 5-year radial bone loss in postmenopausal women. Osteoporos Int 3:314–321
Cauley JA, Cummings SR, Seeley DG et al (1993) Effects of thiazide diuretic therapy on bone mass, fractures, and falls. Ann Intern Med 118:666–673
Jones G, Nguyen Tuan, Sambrook PN, Eisman JA (1995) Thiazide diuretics and fractures: can meta-analysis help? J Bone Miner Res 10:106–111
LaCroix AZ, Ott SM, Ichikawa L, Scholes D, Barlow WE (2000) Low-dose hydrochlorothiazide and preservation of bone mineral density in older adults: a randomized, double-blind, placebo-controlled trial. Ann Intern Med 133:516–526
Schoofs MWCJ, van der Klift M, Hofman A et al (2003) Thiazide diuretics and the risk for hip fracture. Ann Intern Med 139:476–482
Bolland MJ, Ames RW, Horne AM, Orr-Walker BJ, Gamble GD, Reid IR (2007) The effect of treatment with a thiazide diuretic for 4 years on bone density in normal postmenopausal women. Osteoporos Int 18:479–486
Cruz DN (2001) The renal tubular Na–Cl co-transporter (NCCT): a potential genetic link between blood pressure and bone density? Nephrol Dial Transpl 16:691–694
Alkalosis, metabolic. http://emedicine.medscape.com/article/906819-overview. Accessed 24 Oct 2009
Haque SF, Ahmad M, Khan AU, Gupta V, Khan AS (2011) Angiotensin converting enzyme insertion/deletion gene polymorphism and genomic sequence in diabetic nephropathy. Biomed Res 22(2):173–177
Schlienger RG, Kraenzlin ME, Jick SS, Meier CR (2004) Use of β-blockers and risk of fractures. JAMA 292:1326–1332
Takeda S (2009) Osteoporosis: a neurosceletal disease? Int J Biochem Cell Biol 41:455–459
Wiens M, Etminan M, Gill SS, Takkouche B (2006) Effects of antihypertensive drug treatment on fracture outcomes: a meta-analysis of observational studies. J Intern Med 260:350–362
Souverein PC, Van Staa TP, Egberts ACG, de la Rosette MCH, Cooper C, Leufkens HGM (2003) Use of α-blockers and the risk of hip/femur fractures. J Intern Med 254:548–554
Acknowledgments
K. I. is supported by the Ministry of Education and Science, Republic of Serbia (project 175064, 2011–2014).
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors have stated that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Ilić, K., Obradović, N. & Vujasinović-Stupar, N. The Relationship Among Hypertension, Antihypertensive Medications, and Osteoporosis: A Narrative Review. Calcif Tissue Int 92, 217–227 (2013). https://doi.org/10.1007/s00223-012-9671-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-012-9671-9