Abstract
Î22-adrenergic receptors have been identified on human osteoblastic and osteoclastic cells, raising the question of a sympathetic regulation of bone metabolism. We investigated effects of treatment with Î2-adrenergic receptor antagonists (Î2-blockers) on bone turnover, bone mineral density (BMD), and fracture risk. Within the Danish Osteoporosis Prevention Study (DOPS) a population based, comprehensive cohort study of 2016 perimenopausal women, associations between treatment with Î2-blockers and bone turnover and BMD were assessed in a cross-sectional design at the start of study. Moreover, in a nested case-control design, fracture risk during the subsequent 5 years was assessed in relation to treatment with Î2-blockers at baseline. Multiple regression- and logistic regression-analyses were performed. Treatment with Î2-blockers was associated with a threefold increased fracture risk (ORadj 3.3; 95% CI: 1.1–9.4). Analyses on duration of treatment showed that women who had been treated for more than 8 years had a higher fracture risk (ORadj 5.3; 95% CI: 1.1–26.3) than those treated for less than 8 years (ORadj 2.4; 95% CI: 0.6–9.5). In addition, cross-sectional data showed 20% lower serum osteocalcin levels (an osteoblastic marker of bone formation) in women treated with Î2-blockers compared to untreated women (P < 0.001), whereas BMD at the lumbar spine and femoral neck did not differ between groups. Î2-blockers may decrease the activity of bone-forming cells and thereby increase fracture risk. However, confirmative studies and studies exploring mechanisms of action are needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Beta-adrenergic receptor antagonists (Î2-blockers) are extensively used in the treatment of arterial hypertension, ischemic heart diseases, certain cardiac arrhythmias, and migraine. Î22-adrenergic receptors have been identified on human osteoblastic and osteoclastic cells [1, 2], raising the question of a sympathetic regulation of bone metabolism [3]. In vitro studies in different lines of bone cells as well as in vivo studies in experimental animals have demonstrated effects of Î2-adrenergic receptor agonists and antagonists on bone metabolism, but the results reported have been conflicting. In different studies, Î2-adrenergic stimulation and inhibition have been reported to cause anabolic as well as catabolic effects on bone [3, 4, 5, 6, 7].
Further evidences on a sympathetic regulation of bone metabolism have been provided in recent studies on effects of leptin on bone metabolism [2, 8, 9]. Leptin is an adipocyte-derived hormone that circulates to the hypothalamus, thereby providing a feedback-loop to the central nervous system (CNS) about the state of body fat. In addition, a relation between leptin levels and bone mass has been suggested. Leptin may regulate bone metabolism either through a direct effect on bone cells and/or through central actions via its binding to receptors in the CNS [8, 9]. Recently, leptin has been shown to inhibit bone formation through the sympathetic nervous system via osteoblastic Î2-adrenergic receptors [2].
In humans, there are only few and conflicting data on the effects of Î2-blockers on bone metabolism and fracture risk. In a previous study from our group on patients with hyperthyroidism, the Î2-adrenergic antagonist propranolol did not affect bone loss, as determined by measurement of bone mineral content and histomorphometric measures of bone turnover [10]. However, in a recent analysis from the Geelong Osteoporosis Study, Pasco et al. [11] found a reduced fracture risk and an increased BMD in users of Î2-blockers compared to controls.
In the setting of the Danish Osteoporosis Prevention Study (DOPS) [12], a population-based, comprehensive cohort study, we investigated associations between treatment with Î2-blockers and bone turnover, bone mineral density (BMD), and fracture risk.
Subjects and Methods
Design
The present study was performed within DOPS, which is a 20-year prospective, open-label multi-center study (4 centers) on the effect of hormone replacement therapy (HRT) on BMD and fracture risk in 2016 perimenopausal women. DOPS is a population based, comprehensive cohort study [13] including a randomized arm (HRT or no treatment) and an arm based on self-selection (HRT or no treatment) in order to increase the external validity of the study. As first choice, participants received oral sequential therapy with Trisequens™ (estradiol/norethisterone), Novo Nordic, Denmark. If a change in the type of HRT was requested for reasons not requiring permanent discontinuation, a number of HRT alternatives were available, as previously detailed [14]. All drugs were delivered free of charge from the manufactures. The design is pragmatic, attempting to mimic the normal clinical situation. Study design and recruitment of participants have been detailed elsewhere [12]. The Central and Regional Ethical Committees and The Danish National Board of Health approved the study. Each participant gave informed consent and the study was conducted according to the Declaration of Helsinki II. The Good Clinical Practice (GCP) unit at Aarhus University monitored the study.
Participants
We recruited participants by direct mailing to a random subsample of Danish Caucasian females aged 45–58 years. Subjects were 3–24 months past their last menstrual bleeding or having experienced perimenopausal symptoms (including menstrual irregularities) in combination with elevated serum FSH levels. We excluded individuals with metabolic bone disease, osteoporosis defined as non-traumatic vertebral fractures, current estrogen use, ever treated with glucocorticoids for more than 6 months, current or past malignancy, chronic disease if newly diagnosed or out of control, and hospitalization due to alcohol or drug addiction.
Data Collection
All participants were clinically examined and were structurally interviewed at baseline in order to assess risk factors and prognostic factors for osteoporosis, including age, menopausal age, anthropometric variables, physical activity (hours per week spent on jogging, gymnastics, cycling, swimming, and standing/walking on the job), previous and present illnesses, gynecological history, and use of drugs, vitamin supplements, alcohol and tobacco [12]. We used a 7-day food record to assess current daily intakes of vitamins and minerals. A dietician using food models and photographs during a 15-min. validation interview evaluated serving sizes and cooking habits. The diet contents of energy, vitamins, and minerals were analyzed using a computerized database (“Dankost”, software version 1.3b), containing information on diet composition based on official Danish food tables [15]. After 5 years of follow-up, participants were asked whether they had sustained a fracture during the study period. If so, reported fractures were validated by review of hospital discharge records. In addition, X-rays of the spine were obtained as lateral projections of the spine covering Th4 to L5 at inclusion and after 5 years. The images were reviewed by trained radiologists. A fracture was defined as more than 20% reduction in the height of a vertebrae compared to the highest vertical distance of that vertebrae.
BMD Measurements
At baseline, we measured BMD at the lumbar spine (L2-L4) and femoral neck. We used carefully cross-calibrated QDR 1000/W and 2000/W densitometers (Hologic, Inc, Waltham, MA) in all four centers [12]. The in vivo precision errors (BMD) were 1.5% (spine) and 2.1% (femoral neck), respectively. We assessed the long-term stability of the equipment by daily scans of an anthropometric phantom in each center. Changes were <0.2%/year [12].
Biochemistry
We collected blood and urine specimens at baseline. Serum 25-hydroxyvitamin D was measured by a radioimmunoassay (RIA) using rachitic rat kidney cytosol as a binding protein [16]. The intra- and interassay coefficients of variation were 9.4% and 13.5%, respectively. Serum osteocalcin was measured by RIA using rabbit antiserum against bovine osteocalcin [17]. Intact, purified bovine osteocalcin verified by amino acid analysis and antisera against bovine osteocalcin was generously provided by J. Poser (Procter and Gamble Company, Cincinnati, OH). The sera showed full cross-reactivity between human and bovine osteocalcin. The intra- and interassay CVs were 5 and 10%, respectively. Total alkaline phosphatase activity in serum was measured spectrophotometrically and serum bone isoenzyme alkaline phosphatase activity (bone-ALP) was determined by lectin precipitation [18]. The intra-assay CV was 8% and the interassay CV was 25%. The renal excretion of hydroxyproline was collected on a gelatine-restricted diet (second void morning spot urine) and determined spectrophotometrically with p-dimethylaminobenzaldehyde as substrate, according to the manufacturer’s direction (Organon Teknika, Boxtel, The Netherlands). The hydroxyproline excretion was expressed as a ratio relative to the renal creatinine excr etion i.e., hydroxyproline/creatinine-ratio (urinary OHP/creatinine ratio, Î1/4 mol/mmol).
Assessments of Associations Between use of Î2-Blockers and Bone Mineral Density and Fracture Risk
Separate analyses were carried out in order to determine associations between use of Î2-blockers and BMD, bone turnover, and fracture risk:
Cross-sectional Studies on Bone Mineral Density and Bone Turnover
Cross-sectional analyses were carried out on data collected at baseline to assess associations between use of Î2-blockers and BMD of the lumbar spine and femoral neck. Also the relationship between use of Î2-blockers and bone turnover was assessed by measurements of biochemical markers of bone formation (osteocalcin and bone-ALP) and bone resorption (urinary hydroxyproline/creatinine-ratio).
Nested Case-control Study
During the 5-year follow-up period, 163 participants sustained a fracture (cases). For each fracture case, we selected 6 subjects from the population who had not sustained a fracture during the study period (controls). The controls were randomly selected except that they were matched to cases on the use of HRT during the study period (no HRT use, intermittent use, or continuous use).
Statistics
We assessed differences between groups using the chi-square test (Fisher’s Exact test) for categorical variables and two-sample t-test or Mann-Whitney U-test for continuous variables, as appropriate, after testing for normal distributions. As several of included variables were not normally distributed, descriptive data are provided as a median value with the interquartile range (the distance between the first quartile (25th percentile) and the third quartile (75th percentile) values) as a measure of the spread of data.
Multiple regression analyses (all variables entered) were used to study associations between treatment with Î2-blockers and bone turnover and BMD in order to adjust for potential influence of other covariates on BMD. Assumptions for multiple regression analyses were tested using normal probability plots, and models were only accepted if residual plots were compatible with a normal distribution. In multiple regression analyses, treatment with medicine as well as current smoking and use of vitamin supplements were coded as “1”, whereas no use of medicine, non-smoking status and no use of vitamin supplements were coded as “0”.
Finally, logistic regression analyses (all variables entered) were used to study differences between subjects with a fracture and control subjects. All statistical analyses were performed using the Statistical Package for Social Sciences (SPSS 8.0) for Windows.
Results
A total of 38 patients (2%) were treated with Î2-blockers at baseline. Characteristics of studied subjects are outlined in Table 1. Subjects in the Î2-blocker group had been treated with Î2-blockers for a median time period of 8 years. Î2-blocker-treated subjects had a lower dietary calcium intake and lower plasma osteocalcin levels than untreated subjects. In addition, smoking and use of thiazide and loop diuretics was more frequent in Î2-blocker-treated subjects than in the untreated group. Î2-blockers were prescribed for the treatment of hypertension (n = 30), migraine (n = 4), cardiac arrhythmia (n = 2), tremor (n = 1), and unknown (n = 1). Table 2 displays type and dose of Î2-blockers used.
Effects of Î2-Blockers on Bone Turnover
Serum osteocalcin levels were lower in women treated with Î2-blockers than in untreated women (P < 0.001) (Table 1). Additionally, multiple regression analysis including all variables shown in Table 1, showed that treatment with Î2-blockers was an independent determinant of serum osteocalcin levels (dependent variable), with lower levels in Î2-blockers treated subjects than in untreated subjects (Î2 coefficient –2.8, P = 0.004). However, multiple regressions analyses revealed no differences between users- and non-users of Î2-blockers on serum 25-hydroxyvitamin D levels (P = 0.86), serum bone-ALP levels (P = 0.18), or urinary OHP/creatinine ratio (P = 0.60).
Effects of Î2-Blockers on Bone Mineral Density
Baseline BMD at the lumbar spine and femoral neck did not differ between treated and untreated subjects (Table 1). Similarly, multiple regressions analyses revealed no associations between users- and non-users of Î2-blockers and BMD at the lumbar spine (P = 0.09) or femoral neck (P = 0.75).
Nested Case-Control Study
During the 5-year follow-up period, 140 study subjects sustained a fracture of the appendicular skeleton. In addition, X-ray of the spine revealed incident vertebral fractures in 26 subjects. Three subjects had both a vertebral fracture and a fracture of the appendicular skeleton. Thus, a total of 163 study subjects sustained a fracture during the 5-year follow-up period (cases). For each case, we randomly selected 6 control subjects from the same cohort, matched on whether they had received HRT during the study period.
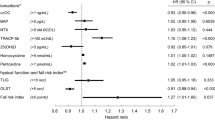
Table 3 shows baseline characteristics of cases and controls. More cases than controls had sustained a fracture before the start of the study (P = 0.03) and compared to controls, cases had a lower baseline BMD at the lumbar spine (P < 0.001) and femoral neck (P < 0.001). Table 4 presents the crude and adjusted ORs from logistic regression analyses on associations between risk of fracture and treatment with Î2-blockers. In an unadjusted analysis, treatment with Î2-blockers was associated with non-significant increased fracture risk (crude odds ratio 2.2; 95% CI: 0.8 to 5.6). After controlling for the influence of variables shown in Table 3, the risk of fracture was statistically significantly increased (adjusted odds ratio 3.3; 95% CI: 1.1 to 9.4). In addition, the increase in fracture risk was more pronounced in women who had been treated with Î2-blockers for more than 8 years than in women who reported treatment for less than 8 years (Table 4).
In order to study whether the underlying diseases necessitating Î2-blocker treatment influenced the association between fracture risk and treatment with Î2-blockers, we also studied associations between fracture risk and treatment with non-Î2-blocker cardiovascular drugs. In our cohort, 6 women were treated with calcium channel blockers and 25 with ACE inhibitors. As each of the two groups was too small to perform the analyses, they were combined (n = 31). Logistic regression analyses, similar to those detailed above, on associations between risk of fracture and treatment with one of the two drugs, did not reveal any significant relationship (crude OR = 0.3; 95% CI: 0.4 to 2.3). Nor did we find any significant association between risk of fracture and treatment with ACE inhibitors/calcium channel blockers after controlling for the influence of variables shown in Table 3 (adjusted OR = 0.5; 95% CI: 0.1 to 4.2).
To explore potential interactions among treatments with Î2-blockers, HRT, and fracture risk we restricted the analysis to those who had not received HRT during the 5-year follow-up. The analysis showed an increased fracture risk (adjusted odds ratio 5.0; 95% CI: 1.4 to 17.5). Similarly, restricting the analysis to those who had received HRT continuously during the study period, a trend towards an increased fracture risk was found (adjusted odds ratio 2.8; 95% CI: 0.2 to 47.3).
Discussion
In a sample of perimenopausal Danish women, we found treatment with Î2-blockers to be associated with a threefold increased fracture risk and an increase in fracture risk with increased duration of treatment. Moreover, the increase in fracture risk was lower in subjects who had received estrogen treatment during the study period than in non-estrogen-treated subjects, indicating that estrogen treatment may partly reverse the increased fracture risk associated with Î2-blocker treatment. In addition, treatment affected bone metabolism, as serum osteocalcin levels were lower in women treated with Î2-blockers than in untreated women. However, we were unable to demonstrate any significant effect of Î2 blockers treatment on BMD at the lumbar spine or femoral neck.
Effect of Î2-Blockers on Bone Mass (BMD) and Fracture Risk
Conflicting results have been reported on the effect of Î2-blockers on bone mass and BMD [3]. In animal experimental studies, Î2-adrenergic blockade has been reported to cause a positive effect on bone mass. Minkowitz et al. [5] found increased trabecular bone formation in rats treated with propranolol for 12 weeks, and Takeda et al. [2] reported an increased bone formation rate and an increased number of osteoblasts, causing an increased bone volume, in mice treated with propranolol for 5 weeks. Thus, according to these studies in experimental animals, a reduced osteoblastic cell activity may be compensated for by an increased number of osteoblastic cells, causing a net positive effect on bone. However, adrenergic antagonists on different cell lines have demonstrated not only bone anabolic but also catabolic action [3]. In addition, conflicting results have been reported on the effects of adrenergic agonists. For example, in one study, adrenergic agonists were shown to exert anabolic effects on cancellous bone in ovariectomized rats [19], whereas in another study adrenergic agonists were found to stimulate bone resorption in neonatal mouse calvarias [1].
Only a few studies have been published on the effect of Î2-blockers on human bone. In a previous study from our group, propranolol treatment did not affect the accelerated bone loss in patients with hyperthyroidism [10]. Similarly, in the present study, we were unable to demonstrate any difference in BMD between Î2-blocker treated- and untreated subjects. Conversely, in a recent study from Australia, treatment with Î2-blockers was found to be associated with an increased BMD and a decreased fracture risk in postmenopausal women [11]. The reason for the discrepancy between our findings and those in the Australian study is not obvious. However, important differences exist in study design between the two studies. In the study from Australia, Pasco et al. [11] recruited women older than 50 years who sustained a fracture during a 2-year period. After the fracture episode (median 59 days post-fracture) study subjects were interviewed and BMD was measured. A total of 559 fracture cases were included. In addition, 775 women who did not sustain a fracture were included in the study as controls. In contrast, our study subjects were recruited before the occurrence of a fracture. A clinical examination, including an interview and osteodensitometric measurements, was performed at a baseline visit. After the baseline visit, we followed our studied subjects for 5 years. In contrast to our design, selection bias may occur if studied subjects are sampled due to a fracture episode. Following fracture, mortality may increase and a fracture may be associated with co-morbidity, making it difficult for subjects with a fracture to participate in a subsequent scientific study [20, 21].
Most subjects treated with Î2-blockers receive the treatment due to cardiovascular diseases. Potentially, a fracture may have more severe consequences in patients with cardiovascular diseases than in otherwise healthy subjects. If so, the true number of fractures in subjects treated with Î2-blockers (i.e., subjects with cardiovascular diseases) may be underestimated if studied subjects are recruited after the fracture episode. Other differences between ours and the Australian study are the completeness of fracture assessment and the age of studied subjects. In our study, X-rays of the spine were obtained in all subjects at inclusion and at the 5-years follow-up visit, whereas in the Australian study, spine X-rays were only obtained in subjects in whom a vertebral fracture was suspected. Our study subjects were perimenopausal women with a median age of 50 years at baseline, whereas the women in the Australian study had a median age of 70 years. However, it is uncertain to what extent this may affect treatment with Î2-blockers on fracture risk. Further studies are needed to resolve this question.
In the Australian study, treatment with Î2-blockers was associated with an increased BMD at the hip and ultradistal forearm [11]. However, as osteodensitometric measurements were performed approximately 2 months after the fracture had occurred, certain limitations may apply to this finding, as BMD may be affected by the fracture itself [22, 23, 24]. If the cardiovascular diseases necessitating treatment with Î2-blockers affect the co-morbidity associated with a fracture, it may be difficult to make interpretations on associations between treatment with Î2-blockers and BMD, if osteodensitometric measurements are performed after the fracture occurs. Actually, in the Australian study, no significant effect of treatment with Î2-blockers on BMD was found in the group of women who had not sustained a fracture, i.e., in the control group (112 users compared to 663 non-users of Î2-blockers). This may indicate that interactions exist between treatment with Î2-blockers, fracture risk, and BMD levels measured after the fracture episode. Further studies are needed to resolve this question.
Our finding of an increased fracture risk in users of Î2-blockers despite absence of a difference in BMD could indicate that the fracture risk was not mediated by differences in BMD, but perhaps rather by an altered bone biomechanical competence not reflected in BMD (e.g. an altered microarchitecture) or by an increased risk of falls. Falls may be the results of a decrease in blood pressure, an increased presence of dizziness or cardiac rhythm disturbances (bradycardia and AV-block in particular). However, it is difficult to establish a link between falls and fractures in users of drugs because not all falls may be recorded and not all falls may result in a fracture. Thus, further studies are needed in animals as well as in humans to clarify effects of adrenergic antagonist and agonists on bone.
Our findings of decreased serum osteocalcin levels in the group of Î2-blocker-treated subjects compared to the untreated group may be explained by a direct effect of Î2-adrenergic antagonists on osteoblasts. Î22-adrenergic receptors have been identified by gene expression analyses in primary mouse osteoblasts and in human SaOS-2 osteoblastic cells [2], and sympathectomy induced by guanethidine, which specifically destroys sympathetic adrenergic fibers has been shown to reduce the activity of osteoblasts [4]. Moreover, Î2-adrenergic agonists (isoproterenol and norepinephrine) and antagonists (propranolol) have been shown to affect the function of osteoblasts [2]. Normally, Î22-adrenergic receptors are G-coupled receptors that signal through the cAMP pathway [25]. Accordingly, treatment of osteoblastic cells with Î2-adrenergic agonists increases, whereas Î2-adrenergic antagonists decreased cAMP production [2, 7].
The cAMP pathway is a major intercellular signal transduction mechanism that regulates osteoblastic function and metabolism, including regulation of osteocalcin expression [26]. Similar to Î22-adrenergic receptors, the parathyroid hormone (PTH) receptor activates intracellular signal transduction through the cAMP pathways, and in vitro studies have shown that PTH increases osteocalcin synthesis through a cAMP-dependent mechanism of action [26, 27]. Moreover, in human studies, treatment with PTH and PTH-related peptide have been shown to increase plasma osteocalcin levels [28, 29], whereas decreased osteocalcin levels have been found in subjects with idiopathic hypoparathyroidism and following surgery for primary hyperparathyroidism [30, 31, 32, 33]. Thus, the association in our study between treatment with Î2-blockers and low serum osteocalcin levels is most likely explained by a direct reduction in osteoblastic cell activity by Î2-blockers, i.e., a decreased cAMP production due to a pharmacological blockade of Î22-adrenergic receptors.
Limitations to Study
Strengths of our study are the prospective design of fracture assessment, a long study duration, and the fact that identification of fractures was not reliant on self-reports, but was validated against hospital records. In addition to fracture assessment, we measured BMD and levels of biochemical markers of bone turnover in order to assess not only fracture risk but also effects of Î2-blockade on bone metabolism. Moreover, we included a large number of potential confounders known to affect bone metabolism and fracture risk. Inclusion of these confounders turned out to be important as a statistical significant increase in fracture risk emerged after confounder adjustment. However, although we adjusted for several potential confounding factors, our results may still be influenced by potential confounding factors not included in the analyses. As most of our subjects were treated with Î2-blockers due to arterial hypertension, it may be speculated that hypertension per se may increase fracture risk. However, conflicting results have been reported on whether arterial hypertension influences BMD [34, 35], and hypertension has not been shown to increase risk of fracture [36, 37]. Moreover, our additional analyses on women treated with non-Î2-blocker cardiovascular drugs (ACE-inhibitors or calcium channel blockers) did not reveal associations between fracture risk and drug treatment/cardiovascular diseases. Therefore, it is unlikely that the underlying cardiovascular diseases cause the increased fracture risk observed by us.
Due to the relatively small number of subjects treated with Î2-blockers in our cohort, our ability to perform sub-analyses was limited. However, in a stratified analysis on duration of use of Î2-blockers, we found a biological plausible increased fracture risk with increased duration of treatment. Further studies should focus on whether a dose-effect relationship also exists. Moreover, certain characteristics that vary among different types of Î2-blockers may affect their ability to affect bone, e.g., differences in lipid solubility, relative affinity for Î21 and Î22 receptors.
Another study limitation, due to the relatively small number of subjects treated with Î2-blockers, is a low statistical power for detecting differences in BMD between treated and untreated subjects. For example, our statistical power to detect a 5% difference in BMD at the femoral neck between treated and untreated subjects was as low as 33% at a 5% significant level. Thus, our data do not exclude the fact that treatment with Î2-blockers may affect BMD. Further studies with larger samples are needed to resolve this question. Moreover, reanalyzing of previous randomized studies on treatment with Î2-blockers may also help.
Conclusions
In perimenopausal women, treatment with Î2-blockers was associated with a threefold increased risk of fracture. Moreover, duration of treatment was positively associated with risk of fracture. Women treated with Î2-blockers had lower osteocalcin levels than untreated women which may suggest decreased bone formation as the mechanism of action by which Î2-blockers increase risk of fracture. However, confirmative studies and studies exploring mechanisms of action are needed.
References
RE Moore CK Smith CS Bailey EF Voelkel AH Tashjian SuffixJr (1993) ArticleTitleCharacterization of beta-adrenergic receptors on rat and human osteoblast-like cells and demonstration that beta-receptor agonists can stimulate bone resorption in organ culture Bone Miner 23 301–315 Occurrence Handle1:CAS:528:DyaK2cXjtFKgsLc%3D Occurrence Handle7908582
S Takeda F Elefteriou R Levasseur X Liu L Zhao KL Parker D Armstrong P Ducy G Karsenty (2002) ArticleTitleLeptin regulates bone formation via the sympathetic nervous system Cell 111 305–317 Occurrence Handle10.1016/S0092-8674(02)01049-8 Occurrence Handle1:CAS:528:DC%2BD38XovVakurk%3D Occurrence Handle12419242
A Togari (2002) ArticleTitleAdrenergic regulation of bone metabolism: possible involvement of sympathetic innervation of osteoblastic and osteoclastic cells Microsc Res Tech 58 77–84 Occurrence Handle10.1002/jemt.10121 Occurrence Handle1:CAS:528:DC%2BD38XmsVWrtr0%3D Occurrence Handle12203706
MS Herskovits IJ Singh (1984) ArticleTitleEffect of guanethidine-induced sympathectomy on osteoblastic activity in the rat femur evaluated by 3H-proline autoradiography Acta Anat (Basel) 120 151–155 Occurrence Handle1:STN:280:BiqD1MzjvFU%3D
B Minkowitz AL Boskey JM Lane HS Pearlman VJ Vigorita (1991) ArticleTitleEffects of propranolol on bone metabolism in the rat J Orthop Res 9 869–875 Occurrence Handle1:CAS:528:DyaK38XnsF2qug%3D%3D Occurrence Handle1919850
T Takeuchi T Tsuboi M Arai A Togari (2001) ArticleTitleAdrenergic stimulation of osteoclastogenesis mediated by expression of osteoclast differentiation factor in MC3T3-E1 osteoblast-like cells Biochem Pharmacol 61 579–586 Occurrence Handle10.1016/S0006-2952(00)00591-8 Occurrence Handle1:CAS:528:DC%2BD3MXhsVOhs7s%3D Occurrence Handle11239501
RJ Majeska B Minkowitz W Bastian TA Einhorn (1992) ArticleTitleEffects of beta-adrenergic blockade in an osteoblast-like cell line J Orthop Res 10 379–384 Occurrence Handle1:CAS:528:DyaK38Xkt1Shu74%3D Occurrence Handle1349041
J Cornish KE Callon U Bava et al. (2002) ArticleTitleLeptin directly regulates bone cell function in vitro and reduces bone fragility in vivo J Endocrinol 175 405–415 Occurrence Handle1:CAS:528:DC%2BD38Xptlaktbc%3D Occurrence Handle12429038
P Ducy M Amling S Takeda et al. (2000) ArticleTitleLeptin inhibits bone formation through a hypothalamic relay: a central control of bone mass Cell 100 197–207 Occurrence Handle10.1016/S0092-8674(00)81558-5 Occurrence Handle1:CAS:528:DC%2BD3cXotFChsw%3D%3D Occurrence Handle10660043
L Mosekilde B Jastrup F Melsen B Lund OH Sørensen HE Nielsen H Yde (1984) ArticleTitleEffect of propranolol treatment on bone mass, bone mineral content, bone remodelling, parathyroid function and vitamin D metabolism in hyperthyroidism Eur J Clin Invest 14 96–102 Occurrence Handle1:STN:280:BiuB3snjsVM%3D Occurrence Handle6428910
JA Pasco MJ Henry KM Sanders MA Kotowicz E Seeman GC Nicholson (2004) ArticleTitleBeta-adrenergic blockers reduce the risk of fracture partly by increasing bone mineral density: Geelong Osteoporosis Study J Bone Miner Res 19 19–24 Occurrence Handle1:CAS:528:DC%2BD2cXnt1Khug%3D%3D Occurrence Handle14753732
L Mosekilde AP Hermann NH Beck P Charles SP Nielsen OH Sorensen (1999) ArticleTitleThe Danish Osteoporosis Prevention Study (DOPS): project design and inclusion of 2000 normal perimenopausal women Maturitas 31 207–219 Occurrence Handle10.1016/S0378-5122(99)00006-7 Occurrence Handle1:STN:280:DyaK1M3ntFKguw%3D%3D Occurrence Handle10340280
AR Jadad (1998) Randomised Controlled Trials. A user’s guide BMJ Books London
P Vestergaard AP Hermann J Gram LB Jensen N Kolthoff B Abrahamsen C Brot P Eiken (1997) ArticleTitleImproving compliance with hormonal replacement therapy in primary osteoporosis prevention Maturitas 28 137–145 Occurrence Handle10.1016/S0378-5122(97)00076-5 Occurrence Handle1:STN:280:DyaK1c7ot1Oqsw%3D%3D Occurrence Handle9522321
A Moller (1989) Food composition tables. Publication No. SC3 The Danish National Food Agency Copenhagen
B Lund OH Sorensen (1979) ArticleTitleMeasurement of 25-hydroxyvitamin D in serum and its relation to sunshine, age and vitamin D intake in the Danish population Scand J Clin Lab Invest 39 23–30 Occurrence Handle1:CAS:528:DyaE1MXlt1anurw%3D Occurrence Handle523951
P Charles JW Poser L Mosekilde FT Jensen (1985) ArticleTitleEstimation of bone turnover evaluated by 47Ca-kinetics. Efficiency of serum bone gamma-carboxyglutamic acid-containing protein, serum alkaline phosphatase, and urinary hydroxyproline excretion J Clin Invest 76 2254–2258 Occurrence Handle1:CAS:528:DyaL28XosVOrtw%3D%3D Occurrence Handle3878367
K Brixen HK Nielsen EF Eriksen P Charles L Mosekilde (1989) ArticleTitleEfficacy of wheat germ lectin-precipitated alkaline phosphatase in serum as an estimator of bone mineralization rate: comparison to serum total alkaline phosphatase and serum bone Gla-protein Calcif Tissue Int 44 93–98 Occurrence Handle1:STN:280:BiaC3srms1Q%3D Occurrence Handle2783876
A Pataki K Muller G Bilbe JR Green M Glatt (1996) ArticleTitleAnabolic effects of beta-2-agonists, formoterol and salbutamol on cancellous bone of ovariectomized (OVX) rat Bone 9 A116
C Olsson C Petersson A Nordquist (2003) ArticleTitleIncreased mortality after fracture of the surgical neck of the humerus: a case-control study of 253 patients with a 12-year follow-up Acta Orthop Scand 74 714–717 Occurrence Handle10.1080/00016470310018252 Occurrence Handle14763704
O Johnell JA Kanis A Oden I Sernbo I Redlund-Johnell C Petterson C Laet ParticleDe B Jonsson (2004) ArticleTitleMortality after osteoporotic fractures Osteoporos Int 15 38–42 Occurrence Handle10.1007/s00198-003-1490-4 Occurrence Handle1:STN:280:DC%2BD2c%2FitlOhsw%3D%3D Occurrence Handle14593451
BM Ingle SM Hay HM Bottjer R Eastell (1999) ArticleTitleChanges in bone mass and bone turnover following ankle fracture Osteoporos Int 10 408–415 Occurrence Handle10.1007/s001980050247 Occurrence Handle1:STN:280:DC%2BD3c7ht1OjsQ%3D%3D Occurrence Handle10591839
DR Dirschl RC Henderson WC Oakley (1997) ArticleTitleAccelerated bone mineral loss following a hip fracture: a prospective longitudinal study Bone 21 79–82 Occurrence Handle10.1016/S8756-3282(97)00082-3 Occurrence Handle1:STN:280:ByiA2MnlslE%3D Occurrence Handle9213011
MM Petersen PM Gehrchen PK Nielsen B Lund (1997) ArticleTitleLoss of bone mineral of the hip assessed by DEXA following tibial shaft fractures Bone 20 491–495 Occurrence Handle10.1016/S8756-3282(97)00028-8 Occurrence Handle1:STN:280:ByiB1M%2FmtVY%3D Occurrence Handle9145248
JL Benovic C Staniszewski F Mayor SuffixJr MG Caron RJ Lefkowitz (1988) ArticleTitleBeta-adrenergic receptor kinase. Activity of partial agonists for stimulation of adenylate cyclase correlates with ability to promote receptor phosphorylation J Biol Chem 263 3893–3897 Occurrence Handle1:CAS:528:DyaL1cXhs1Wqu7k%3D Occurrence Handle2831211
G Boguslawski LV Hale XP Yu RR Miles JE Onyia RF Santerre S Chandrasekhar (2000) ArticleTitleActivation of osteocalcin transcription involves interaction of protein kinase A- and protein kinase C-dependent pathways J Biol Chem 275 999–1006 Occurrence Handle10.1074/jbc.275.2.999 Occurrence Handle1:CAS:528:DC%2BD3cXntleitg%3D%3D Occurrence Handle10625638
XP Yu S Chandrasekhar (1997) ArticleTitleParathyroid hormone (PTH 1-34) regulation of rat osteocalcin gene transcription Endocrinology 138 3085–3092 Occurrence Handle10.1210/en.138.8.3085 Occurrence Handle1:CAS:528:DyaK2sXkslSisLg%3D Occurrence Handle9231754
MJ Horwitz MB Tedesco C Gundberg A Garcia-Ocana AF Stewart (2003) ArticleTitleShort-term, high-dose parathyroid hormone-related protein as a skeletal anabolic agent for the treatment of postmenopausal osteoporosis J Clin Endocrinol Metab 88 569–575 Occurrence Handle10.1210/jc.2002-021122 Occurrence Handle1:CAS:528:DC%2BD3sXhtlChsb8%3D Occurrence Handle12574182
F Cosman J Nieves L Woelfert V Shen R Lindsay (1998) ArticleTitleAlendronate does not block the anabolic effect of PTH in postmenopausal osteoporotic women J Bone Miner Res 13 1051–1055 Occurrence Handle1:CAS:528:DyaK1cXjvFSmuro%3D Occurrence Handle9626638
T Steinichel P Christiansen A Vesterby R Ullerup I Hessov LE Mosekilde F Melsen (2000) ArticleTitlePrimary hyperparathyroidism: bone structure, balance, and remodeling before and 3 years after surgical treatment Bone 26 535–543 Occurrence Handle10.1016/S8756-3282(00)00260-X Occurrence Handle10773596
M Kanatani T Sugimoto H Kaji K Ikeda K Chihara (2001) ArticleTitleSkeletal responsiveness to parathyroid hormone in pseudohypoparathyroidism Eur J Endocrinol 144 263–269 Occurrence Handle1:CAS:528:DC%2BD3MXisFagtLw%3D Occurrence Handle11248746
L Mortensen L Hyldstrup P Charles (1997) ArticleTitleEffect of vitamin D treatment in hypoparathyroid patients: a study on calcium, phosphate and magnesium homeostasis Eur J Endocrinol 136 52–60 Occurrence Handle1:CAS:528:DyaK2sXhslGmt7Y%3D Occurrence Handle9037127
K Kruse U Kracht K Wohlfart U Kruse (1989) ArticleTitleBiochemical markers of bone turnover, intact serum parathyroid hormone and renal calcium excretion in patients with pseudohypoparathyroidism and hypoparathyroidism before and during vitamin D treatment Eur J Pediatr 148 535–539 Occurrence Handle1:STN:280:BiaA3crmt1A%3D Occurrence Handle2744015
K Tsuda I Nishio Y Masuyama (2001) ArticleTitleBone mineral density in women with essential hypertension Am J Hyperten 14 704–707 Occurrence Handle10.1016/S0895-7061(01)01303-6 Occurrence Handle1:STN:280:DC%2BD38%2FitF2isg%3D%3D
DA Hanley JP Brown A Tenenhouse et al. (2003) ArticleTitleAssociations among disease conditions, bone mineral density, and prevalent vertebral deformities in men and women 50 years of age and older: cross-sectional results from the Canadian Multicentre Osteoporosis Study J Bone Miner Res 18 784–790 Occurrence Handle1:STN:280:DC%2BD3s7ls1Whtw%3D%3D Occurrence Handle12674340
DT Felson D Sloutskis JJ Anderson JM Anthony DP Kiel (1991) ArticleTitleThiazide diuretics and the risk of hip fracture. Results from the Framingham Study JAMA 265 370–373 Occurrence Handle10.1001/jama.265.3.370 Occurrence Handle1:STN:280:By6D1c%2Fis1w%3D Occurrence Handle1984536
AZ LaCroix J Wienpahl LR White RB Wallace PA Scherr LK George J Cornoni Huntley AM Ostfeld (1990) ArticleTitleThiazide diuretic agents and the incidence of hip fracture N Engl J Med 322 286–290 Occurrence Handle1:STN:280:By%2BC3Mvjtlw%3D Occurrence Handle2296269
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rejnmark, L., Vestergaard, P., Kassem, M. et al. Fracture Risk in Perimenopausal Women Treated with Beta-Blockers. Calcif Tissue Int 75, 365–372 (2004). https://doi.org/10.1007/s00223-004-0222-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-004-0222-x