Abstract
This review summarizes the available evidence-based data that form the basis for therapeutic intervention and covers the current status of glucocorticoid-induced osteoporosis (GIOP) management, regulatory requirements, and risk-assessment options. Glucocorticoids are known to cause bone loss and fractures, yet many patients receiving or initiating glucocorticoid therapy are not appropriately evaluated and treated. An European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis workshop was convened to discuss GIOP management and to provide a report by a panel of experts. An expert panel reviewed the available studies that discussed approved therapeutic agents, focusing on randomized and controlled clinical trials reporting on bone mineral density and/or fracture risk of at least 48 weeks’ duration. There is no evidence that GIOP and postmenopausal osteoporosis respond differently to treatments. The FRAX algorithm can be adjusted according to glucocorticoid dose. Available antiosteoporotic therapies such as bisphosphonates and teriparatide are efficacious in GIOP management. Several other agents approved for the treatment of postmenopausal osteoporosis may become available for GIOP. It is advised to stop antiosteoporotic treatment after glucocorticoid cessation, unless the patient remains at increased risk of fracture. Calcium and vitamin D supplementation as an osteoporosis-prevention measure is less effective than specific antiosteoporotic treatment. Fracture end-point studies and additional studies investigating specific subpopulations (pediatric, premenopausal, or elderly patients) would strengthen the evidence base and facilitate the development of intervention thresholds and treatment guidelines.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
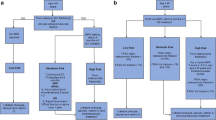
Glucocorticoids are widely used to suppress inflammation and to treat various immune-mediated diseases, such as rheumatic diseases (rheumatoid arthritis, polymyalgia rheumatica, systemic lupus erythematosus, vasculitis), lung diseases, inflammatory bowel disease, chronic liver disease, and skin diseases, or in organ transplant recipients. Glucocorticoid use is associated with deleterious effects on bone (Fig. 1), leading to glucocorticoid-induced osteoporosis (GIOP), a common cause of secondary osteoporosis. Long-term glucocorticoid therapy causes osteoporotic fractures in ~30–50 % of treated adult patients [reviewed in 1].
Effects of glucocorticoids on bone metabolism (adapted from [29, 35, 121]). Dkk-1 dickkopf-1, OPG osteoprotegerin, RANKL receptor activator of nuclear factor κB ligand, BMP bone morphogenetic protein, GSK3β glycogen synthase kinase 3β, PPAR peroxisome proliferator–activated receptor, Runx2 runt-related protein 2, AP-1 activator protein 1
A particular characteristic of GIOP is early rapid bone loss [2]. Early intervention with bone protective therapy is therefore important in individuals at increased risk of fracture [3]. Compared with postmenopausal osteoporosis, fewer studies have investigated treatment efficacy in GIOP patients [4], despite the fact that ~1.4–1.7 % of women in the United Kingdom above the age of 55 receive glucocorticoid therapy [5, 6]. Of note, glucocorticoid use varies markedly in different countries. The global longitudinal study of osteoporosis in women (GLOW) observational study reported higher use of glucocorticoids in women above the age of 55 years (2.7–4.6 %), but sampling was weighted toward older and less healthy subjects [7]. Although glucocorticoids are known to cause bone loss and fractures, many patients receiving or starting long-term glucocorticoid therapy are not appropriately evaluated and treated, in terms of bone health and fracture prevention [8].
This review summarizes the available evidence-based data that form the basis for therapeutic intervention and cover the current status of GIOP management, regulatory requirements, and options for risk assessment.
Methods
A workshop was convened to identify areas of consensus among a panel of experts (the authors), with the objective of discussing the available data for the evaluation and management of GIOP. The studies included in this position paper reflect those discussed by the panel during the workshop.
The studies discussed approved therapeutic agents, focusing on randomized controlled clinical trials (RCTs) of human subjects reported in English. The emphasis was on studies with information on bone mineral density (BMD) and/or fracture, with a minimum duration of 48 weeks. Relevant meta-analyses were also described. In cases where RCT data were not available as supportive evidence, qualitative literature reviews and expert-identified articles were used to summarize the existing evidence.
Epidemiology
Epidemiological data on GIOP mostly relate to oral glucocorticoid therapy given continuously for 3–6 months or longer. In 2000, ~0.9 % of the total adult population in the United Kingdom used oral glucocorticoids (2.5–7.5 mg prednisolone or equivalent) at any one time. Of these, an estimated 22 % took higher doses long term (>6 months) [6]. A pharmacies database study of glucocorticoid prescriptions in Iceland collected over a 2-year period, combined with information obtained from medical records, estimated that 26 % of patients on long-term glucocorticoid therapy (>6 months) develop osteoporosis [9].
Fracture rates increase with age regardless of glucocorticoid use in both men and women, but there is an additional dose-dependent increase in risk for people taking higher doses of oral glucocorticoids [10, 11]. Daily doses of ≥5 mg prednisolone have been shown to increase fracture risk by about 20 %, rising to 60 % in individuals on ≥20 mg/day [2, 12]. In a meta-analysis of ~42,000 subjects from seven cohort studies across different countries, current and past glucocorticoid use was an important predictor of fracture risk, independent of prior fracture and BMD. Relative risk of any fracture ranged from 1.98 at the age of 50 years to 1.66 at the age of 85 years. Relative risk ranged 2.63–1.71 and 2.48–4.42 for osteoporotic and hip fractures, respectively [13].
Cumulative glucocorticoid dose correlates strongly with loss of BMD [2]. A correlation has also been established between daily dose and fracture risk, which increases rapidly (within 3–6 months of initiating oral glucocorticoid therapy) and independently of underlying disease, age, and gender [14]. The underlying disease being treated often contributes to loss of bone mass and increased fracture risk [15]. Factors such as general health status, age, sex, body mass index (BMI), fracture history (personal and family), diet, exercise, smoking, alcohol consumption, and menopausal status must also be considered when evaluating fracture risk [12].
Nature of Glucocorticoid Therapy
Glucocorticoid doses and treatment schedules vary considerably among patients, complicating the quantification of fracture risk. Daily prednisolone doses as low as 2.5 mg have been associated with increased fracture risk [12]. However, the effects on bone of low-dose oral glucocorticoids, as well as of inhaled glucocorticoids and intermittent dosing, are not yet fully established [16].
An increased risk of vertebral fracture has been reported in patients on inhaled glucocorticoid therapy, although this effect was less pronounced than with systemic glucocorticoid therapy [16]. Inhaled low-dose glucocorticoids are not associated with increased fracture risk [17], whereas inhaled beclomethasone above 800 μg/day was associated with a small increase in fracture risk [18]. The metabolic impact of inhaled corticosteroids is reviewed elsewhere [19]. An increased risk of fracture has been reported in children on inhaled glucocorticoid therapy, but after adjusting for asthma severity, the risk disappeared. Thus, it is likely that the increase in fracture risk was related to the underlying disease as well [20].
Few studies have documented the effect of intermittent (pulse) therapy on bone metabolism. Early studies concluded that bone metabolism was not seriously affected during glucocorticoid pulse therapy but that hypercalciuria was consistently reported [21–23]. Although a significant increase is initially seen in serum calcium, parathyroid hormone (PTH), and 1,25-dihydroxyvitamin D, these values typically return to baseline levels in subsequent pulses. Rather than an actual increase in PTH levels, a greater sensitivity of bone cells to PTH induced by glucocorticoids has been advocated [24]. Contrary to expectations, the use of long-term, intermittent, high-dose glucocorticoids in children, after adjusting for BMI, has been linked with an increase in whole-body bone mineral content and maintenance of the bone mineral content of the lumbar spine [25]. Typically, however, there is an increased fracture risk associated with intermittent glucocorticoid use, with higher doses and more frequent use leading to greater risk [17]. Oral pulse therapy increases vertebral fracture risk similarly to inhaled glucocorticoids, but these patients are less likely to fracture than those on continuous therapy [26, 27].
Although withdrawal of glucocorticoids leads to a reduction in fracture risk, it is not clear whether the risk returns to baseline values [4, 27, 28]. In one case–controlled study, it took >1 year for fracture risk to return to the general population level [29]. There is some evidence that BMD loss is partially reversible upon cessation of glucocorticoid therapy [4, 10, 30]. This raises the question of when to discontinue antiosteoporotic treatment after cessation of glucocorticoid use as there is no current consensus.
Pathophysiology
Reduced bone formation is the key process in GIOP and probably the main difference between GIOP and postmenopausal osteoporosis. Even at low doses, glucocorticoids have been shown to rapidly and significantly suppress several indices of osteoblast activity, including serum propeptide of type I N-terminal procollagen (P1NP), propeptide of type I C-terminal procollagen (P1CP), and osteocalcin [31]. Glucocorticoid-induced apoptosis of osteoblasts and osteocytes has long been recognized in the pathophysiology of GIOP [1, 32, 33], but it is only in the past few years that our understanding of the molecular mechanisms involved has extended to a more in-depth process (Fig. 1).
It has been suggested that osteocyte–canalicular network interruption, could trigger apoptosis in the immediately surrounding cells and activate bone remodeling [34]. Recent studies have identified activation of caspase-3 as an important trigger for osteoblast and osteocyte apoptosis. Osteoblast loss has also been linked with activation of glycogen synthase kinase 3β (GSK3β), a serine/threonine-specific protein kinase involved in the Wnt signaling pathway [35].
In bone metabolism, the Wnt signaling pathway plays an important role in osteoblastogenesis. This pathway is negatively regulated by dickkopf-1 (Dkk-1) and sclerostin. Glucocorticoids upregulate expression of these inhibitors [36, 37], thereby suppressing the binding of Wnt to low-density lipoprotein receptor–related proteins 5 and 6 (LPR5/-6). This leads to a reduced ability to stabilize β-catenin and to the inhibition of bone formation by blocking the transcription of target genes [35].
Glucocorticoids also stimulate osteoblast precursor cells in bone marrow (bone marrow stromal cells) to differentiate toward adipogenesis instead of osteoblastogenesis. High-dose glucocorticoids may initiate this preferential shift through the repression of activator protein 1 (AP-1), which is further implicated in the regulation of genomic anti-inflammatory activity [35]. Other important processes include upregulation of expression of peroxisome proliferator–activated receptor γ2 (PPARγ2) and repression of runt-related protein 2 (Runx2) [35]. In contrast to osteoblastogenesis, osteoclastogenesis is rather promoted by glucocorticoid use. Osteoclast apoptosis is suppressed during glucocorticoid therapy, through both inhibition of osteoprotegerin (OPG) and increased expression of receptor activator for nuclear factor-κB ligand (RANKL). The Wnt signaling pathway is a candidate mechanism for glucocorticoid-mediated suppression of OPG. Direct effects of glucocorticoids on osteoclasts have been shown in vitro to result in a reduced capacity for bone resorption [35].
In addition to their direct effects on osteoblasts, osteoclasts, and osteocytes, glucocorticoids exert indirect effects on bone by reducing intestinal calcium absorption and increasing renal calcium clearance and by affecting gonadal hormones and the neuromuscular system (as seen by an increased propensity for falls in glucocorticoid-treated patients) [1]. Overall, these effects on bone metabolism contribute to early and rapid bone loss and increased fracture risk [1, 29, 38, 39]. Furthermore, continuous exposure to glucocorticoids has been shown to increase expression of genes that inhibit bone mineralization (Dmp-1, Phex). Glucocorticoid transrepression of two important matrix proteins, osteocalcin and type 1 collagen, may have an additional effect on bone mineralization [35].
Comparisons of the pathophysiology of GIOP and postmenopausal osteoporosis may have some parallels with comparisons of osteoporosis in men vs. women. Although the pathophysiology of osteoporosis differs between the sexes, there are similarities in the relationship of BMD to fracture and treatment response. In the context of GIOP, however, additional factors, such as age and comorbidity profiles and the fact that glucocorticoids have a negative effect on muscle strength, may obscure such parallels. Patients with GIOP fracture at a lower BMD value than those with postmenopausal osteoporosis [2]. A potential biological basis for the focus on older age as an independent risk factor was highlighted in studies indicating that the effects of glucocorticoids on bone are dependent on autocrine actions of 11β-hydroxysteroid dehydrogenase type 1 (11β-HSD1), the expression of which facilitates local synthesis of active glucocorticoids in osteoblasts, affecting their proliferation and differentiation. Age-specific variation in osteoblastic 11β-HSD1 was characterized using primary cultures of human osteoblasts. 11β-HSD1 reductase activity was detected in all osteoblast cultures, which correlated positively with age. Moreover, glucocorticoid treatment caused a time- and dose-dependent increase in 11β-HSD1 activity compared with controls. Thus, activation of glucocorticoids at an autocrine level within bone may have a role in the age-related decrease in bone formation and increased GIOP risk [40].
Intervention Thresholds
In GIOP, the terms “prevention” and “treatment” distinguish between the initiation of antiosteoporosis intervention at the start of glucocorticoid therapy and after ≥3 months of glucocorticoid therapy. Ideally, however, the timing of antiosteoporotic intervention in GIOP would be based on absolute fracture risk [41]. The World Health Organization (WHO) developed the FRAX® computer-based fracture risk-assessment tool (http://www.shef.ac.uk/FRAX) to calculate 10-year fracture probability from clinical risk factors with or without BMD testing [42, 43]. This risk-assessment tool provides estimates of fracture probability in individuals receiving glucocorticoid doses (2.5–7.5 mg/day), whereas the algorithm can be adjusted according to glucocorticoid dose defined in terms of prednisolone-equivalent doses [44]. For low-dose exposure (<2.5 mg/day prednisolone equivalent) the probability of a major fracture may need revising downward, depending on age, whereas with high doses (>7.5 mg/day) probabilities can be revised upward [44, 45].
Various guidelines for GIOP stress the importance of initiating antiosteoporosis prophylaxis in patients receiving chronic glucocorticoid therapy [46, 47]. The most recent (2010) recommendations from the American College of Rheumatology (ACR) are stratified by glucocorticoid dose and fracture risk based on FRAX calculations. They recommend that low- and medium-risk patients (FRAX <10 and 10–20 % probability of a major fracture, respectively) should be treated if their glucocorticoid dose is ≥7.5 mg/day. High-risk patients (FRAX >20 %) should be treated if they receive glucocorticoids at any dose for >1 month or if they are on ≥5 mg/day prednisolone equivalent even for <1 month [46]. The 10 % threshold is lower than the generally accepted 20 % threshold for postmenopausal osteoporosis in use in North America.
Further recommendations from the ACR include avoiding routine osteoporosis prophylaxis in young women of childbearing potential who are due to receive glucocorticoids for <3 months. In premenopausal women who will receive glucocorticoids for ≥3 months, it is assumed that the fracture risk is high enough to recommend treatment with alendronate, risedronate, zoledronic acid, or teriparatide to prevent GIOP [46].
A joint Guideline Working Group of the International Osteoporosis Foundation (IOF) and European Calcified Tissue Society (ECTS) recently published a framework for the development of national guidelines for the management of GIOP [47]. The IOF–ECTS recommends that, in postmenopausal women and men aged ≥50 years exposed to ≥3 months of oral glucocorticoids, a decision should be made on whether to consider treatment directly or to assess risk with adjusted FRAX (with or without BMD testing). This decision should be based on history of fracture, age (≥70 years), and glucocorticoid dose (≥7.5 mg/day); intervention thresholds will depend on the country. In premenopausal women and men aged <50 years exposed to ≥3 months of oral glucocorticoids, treatment should be considered in patients with prior fracture. Treatment decisions in individuals with no prior fracture should be based on clinical judgment. In addition, it is recommended that all individuals receiving glucocorticoid therapy should be counseled as to the risks of treatment. General measures (e.g., good nutrition and regular weight-bearing exercise) should be taken, and patients should be monitored as appropriate (Appendix) [47].
Regulatory Requirements
Current European guidelines for the evaluation of new medicinal products in the treatment of primary osteoporosis do not include any requirements for GIOP [48, 49]. However, work is in progress to provide guidelines for this group of patients, including pediatric subjects. The similarities with respect to the pathophysiology of bone loss between GIOP and postmenopausal osteoporosis, including increased bone resorption (at least initially in GIOP) and reduced bone formation, form the basis of the claim for a BMD end point in GIOP as being sufficient (reviewed in [41]).
In line with WHO guidelines [50], patients starting glucocorticoid therapy and/or those already on glucocorticoid therapy may be included in phase III clinical trials. Stratification by duration of glucocorticoid use may be recommended. Phase III trials in GIOP should aim to demonstrate a minimum of 2-year superior antifracture efficacy (vertebral and/or nonvertebral fractures) vs. placebo in a randomized, double-blind study. For the treatment of GIOP in postmenopausal women, bridging studies may be performed with drugs (same formulation, dose, and route of administration) already approved in this patient population, provided that the trial in postmenopausal osteoporosis lasts ≥1 year, that spine BMD will be the primary end point, and that the comparator is an approved and established treatment for GIOP. Bridging studies are not considered to be adequate or appropriate in premenopausal women.
Due to uncertainties regarding the exact effect of a specific therapy on facture rates in men and the double BMD-based extrapolation (from postmenopausal women to men without GIOP, then to men with GIOP), three-armed studies of new chemical entities in men with primary osteoporosis vs. new chemical entities in men with GIOP versus an active comparator in GIOP are recommended.
Osteoporosis Treatment in GIOP
Although GIOP and postmenopausal osteoporosis are pathophysiologically different, approved treatments are similar in both groups of patients, with some geographical variations. For instance, vitamin D metabolites and analogs are used in GIOP, but neither 1α-hydroxyvitamin D3 (alfacalcidol) nor 1,25-dihydroxyvitamin D3 (calcitriol) is approved for this indication in Europe or North America [28, 51]. There is no convincing evidence that GIOP and postmenopausal osteoporosis respond differently to current treatments. However, some are restricted to the indication of postmenopausal osteoporosis [selective estrogen receptor modulators (SERMs), tibolone, calcitonin, and strontium ranelate in Europe].
Treatment of GIOP in Different Population Subgroups
The evidence base in GIOP is limited, and information on glucocorticoid response and safety is incomplete for some subpopulations, especially premenopausal women, pediatric subjects, and older adults. To date, few fractures have been recorded in premenopausal women enrolled in RCTs of bisphosphonates and teriparatide (these women have higher baseline BMD values) [52–55]. Initiation of bisphosphonates is recommended in premenopausal patients on high-dose steroids with evidence of a prevalent fracture (Appendix). The 2010 ACR guidelines recommend newer therapies such as zoledronic acid and teriparatide, along with alendronate and risedronate, for the treatment of GIOP in women of childbearing potential with a prior fragility fracture. Estrogen replacement is no longer endorsed in these women [46]. This panel believes that bone protective therapy may be indicated in premenopausal women and younger men, e.g., in individuals with a history of fracture or those receiving high glucocorticoid doses. Women of childbearing potential should be under appropriate contraception before introducing bisphosphonates at relatively high doses because of potential deleterious effects on the fetus.
Pediatricians tend to treat children with glucocorticoids because of low bone mass [56]. Reported fracture rates in children with GIOP are very similar to those seen in postmenopausal women [57]. Age must be taken into consideration when evaluating fracture rates as baseline fracture risk in pediatric disease is high. Peak fracture rate in children occurs between the ages of 8 and 15 years, independent of the use of glucocorticoids. Conservative measures (Appendix) may be inadequate in the pediatric population, giving rise to fragility fractures; and the growing skeleton may be especially vulnerable to adverse glucocorticoid effects on bone formation. Safety concerns have been raised about the use of bisphosphonates in children, and their efficacy in pediatric populations remains unclear [58].
Further studies are needed to differentiate between population subgroups, particularly adolescents and children, for whom there are insufficient data to provide evidence-based guidelines for GIOP prevention and treatment. In general, however, the lowest possible effective glucocorticoid dose should be used for a limited period. Alternative approaches such as calcium and vitamin D supplementation, exercise, and balanced diet should also be considered (Appendix) [59]. If BMD decreases, or even remains stable in a growing individual, bisphosphonate treatment may be recommended. Bisphosphonates should also be considered when higher doses of glucocorticoids are likely to be used long term or in patients with a history of fracture [60]. Preliminary studies in children with GIOP have suggested a benefit of bisphosphonate intervention during periods of high bone turnover [61], but the pharmacokinetics of alendronate in different age groups have yet to be described in larger subsets of patients [62]. A Cochrane review of bisphosphonate treatment (including oral alendronate, clodronate, and intravenous [iv] pamidronate) in 281 children 0–18 years with GIOP concluded that further evaluation of bisphosphonates among children with secondary osteoporosis is justified but did not support bisphosphonates as standard therapy [63]. These drugs were well tolerated with short-term use (≤3 years).
Calcium and Vitamin D Supplementation
Intestinal calcium absorption is decreased in GIOP, for reasons that are not fully understood, making the prescription of calcium and vitamin D supplementation a logical approach [64]. Vitamin D increases intestinal calcium absorption and may have a role in the maintenance of muscular strength. Two meta-analyses demonstrated a clinically and statistically significant prevention of bone loss at the lumbar spine and forearm with vitamin D and calcium in glucocorticoid-treated patients, with vitamin D plus calcium being superior to calcium alone or no therapy in GIOP management. Prophylactic treatment with vitamin D plus calcium can therefore be recommended as a minimum preventive strategy for GIOP in patients receiving long-term glucocorticoids (Appendix) [65, 66].
Studies investigating the efficacy of calcium and vitamin D supplementation in glucocorticoid-treated patients fall into three categories: prevention studies, treatment studies, and studies on both prevention and treatment (Table 1). Prevention studies are those that enroll patients within 3–4 months of starting glucocorticoid therapy and are mostly designed to maintain BMD. Treatment studies are those that enroll patients who have been on glucocorticoid therapy for >3–4 months, in whom an intervention is expected to increase BMD. In general, prevention studies used higher glucocorticoid doses and evaluated patients at greater risk, whereas treatment studies used lower doses; baseline T-Scores were similar in both study types. Despite having an effect on BMD, calcium and vitamin D supplementation as a preventive measure in osteoporosis is much less effective than specific antiosteoporotic treatments, regardless of the subpopulation under study (postmenopausal and premenopausal women, or men) [52–55].
Some studies have shown that bone loss can be attenuated by using more polar vitamin D derivatives. Supplementation with calcium and active vitamin D metabolites (alfacalcidol or calcitriol) blunts the decline in lumbar spine and femoral neck BMD in patients on glucocorticoid therapy compared with untreated patients [68, 69]. However, a study in patients with asthma reported ineffective inhibition of both lumbar spine and femoral neck BMD decreases with calcitriol supplementation [70]. To date, only one head-to-head comparator study of vitamin D supplementation (alfacalcidol) versus bisphosphonates (alendronate) has been conducted. However, the study was not double-blinded [71]. This study is discussed further in the bisphosphonates section. In a study of 103 patients starting long-term glucocorticoid therapy who were randomized to receive calcium with or without calcitriol and/or calcitonin supplementation for 1 year, a greater degree of bone loss from the lumbar spine occurred in patients treated with calcium alone than in patients treated with calcium plus calcitriol with or without calcitonin (mean rate of change –4.3, –0.2, and –1.3 %, respectively; p = 0.0035). Treatment did not have a significant effect on bone loss at the femoral neck and distal radius [68].
A meta-analysis showed that, compared with no treatment or calcium alone, supplementation with active vitamin D derivatives resulted in a higher BMD increase and more effective reduction of vertebral fracture risk. Compared with bisphosphonates, however, active vitamin D treatment is not as potent at increasing BMD [71, 72]. Overall, the incidence of vertebral fractures in glucocorticoid-treated patients receiving calcium and vitamin D from 48 weeks to 2 years, according to quantitative morphometric analyses, ranged from 3.7 [53] to 18.0 % [52, 54, 73, 74] and was consistently lower in patients who received antiosteoporosis treatment (Table 1).
Bisphosphonates in the Treatment of GIOP
Bisphosphonates are the current standard of care for GIOP.
Etidronate
A 12-month, double-blind, multicenter study in 141 patients initiating glucocorticoid therapy randomized patients to receive etidronate (400 mg/day for 14 days, every 3 months) or placebo [67]. All patients received calcium 500 mg/day. The demographic distribution was characteristic of GIOP trials, with men accounting for one-third of participants, postmenopausal women for half, and the remaining being premenopausal women; mean age was around 60 years. As this was a prevention study rather than a treatment study, the primary end point was maintenance of BMD at 1 year. Significant maintenance of lumbar spine BMD was seen in the etidronate group compared with a loss of BMD in the placebo group (p < 0.05). When these data were broken down into subgroups, the difference between etidronate-treated and placebo-treated patients remained statistically significant in premenopausal (p = 0.015) and postmenopausal (p = 0.001) women, but not in men. The difference in femoral neck BMD was not statistically significant (Table 1) [67].
This study included a population with a high rate of prevalent vertebral fracture (49 vs. 45 % in the placebo- and etidronate-treated groups, respectively). A fair number of participants had rheumatoid arthritis and were older, which may explain higher baseline fracture prevalence compared with other studies. Fewer new vertebral fractures were reported in the etidronate group (8.8 %) than the placebo group (15.4 %) (Table 1). In addition, no patients in the etidronate group had multiple fractures compared with 9.2 % of patients in the placebo group [67]. Etidronate therapy reduced the proportion of postmenopausal women with new vertebral fractures by 85 % compared with placebo (7/32 vs. 1/31, p = 0.05). Etidronate-treated postmenopausal women also had significantly fewer vertebral fractures per patient (p = 0.04). No significant difference in the rate of new vertebral fractures was observed among male patients, and no new vertebral fractures occurred in either group in premenopausal women.
A number of smaller studies have evaluated etidronate in GIOP, including two other prevention trials [75, 76] and two treatment studies [77, 78]. Overall, the prevention studies reported BMD maintenance, whereas the treatment studies reported increases in BMD.
Alendronate
A combined analysis of data from two double-blind RCTs investigated the use of alendronate in the treatment of 477 men and women aged 18–80 years with GIOP [53]. Participants were randomized to 48-week treatment with alendronate or placebo, stratified into “prevention” and “treatment” arms according to prior glucocorticoid exposure. One hundred and sixty patients entered the prevention arm. Two treatment arms were established according to duration of glucocorticoid therapy: 99 patients had 4–12 months of glucocorticoid therapy, and 218 were treated for >12 months. All patients received background calcium (800–1,000 mg/day) and vitamin D (250–500 IU/day) supplementation. At baseline, 43 % of patients had lumbar spine BMD within 1 standard deviation (SD) below the peak value for sex-matched healthy young adults; 32 % had osteoporosis, as defined by a lumbar spine T-Score <–2 SD. Loss of lumbar spine BMD was noted in the placebo group, but this was not statistically significant compared with alendronate-treated patients overall. Loss of femoral neck BMD was also noted in the placebo group, whereas a slight improvement was seen in the alendronate group (p < 0.01) (Table 1) [53].
When considering the prevention versus treatment groups separately, patients in the prevention arm had a lumbar spine BMD response in favor of alendronate that was highest in patients on the 10-mg dose. A gain in lumbar spine BMD from baseline to week 48 was reported in all four subgroups (men, premenopausal and postmenopausal women, and estrogen-treated postmenopausal women) [53]. At 1 year, the combined analysis showed a 38 % reduction in lumbar spine BMD in the placebo group (not statistically significant). Few new vertebral fractures occurred during the study, and the incidence of morphometrically defined vertebral fractures in the alendronate groups (combined 5 and 10 mg) was not significantly lower than that in the placebo group. The majority of new vertebral fractures occurred in postmenopausal women (5/134 in the alendronate groups vs. 4/53 in the placebo group, p = 0.05) [53].
Compared with the etidronate trial discussed above [66], patients in the alendronate study were, on average, younger and received a lower dose of glucocorticoids. They were also less likely to have a prevalent vertebral fracture. Other demographic characteristics were similar between the two studies. Both trials found no differences in male patients, and no new vertebral fractures occurred in premenopausal women [53]. The selected patient populations did not allow for further comparison of fracture risk between the two studies. A 2-year extension of the alendronate trial revealed that the effect of 10 mg alendronate on lumbar spine BMD plateaued after ~1 year [73]. However, upon taking the large number of dropouts into consideration, the extension study showed a progressive decline in femoral neck BMD and indicated that, after longer follow-up, femoral neck BMD may decline more than spine BMD. Overall, there were fewer patients with new vertebral fractures in the alendronate group compared with the placebo group (0.7 vs. 6.8 %, p = 0.026). No new vertebral fractures occurred in patients treated with any dose of alendronate during the second year [73].
In most studies on GIOP, the increase in lumbar spine BMD was smaller than the reported effect in postmenopausal women [53, 71, 73, 79–81]; it was similar in one study [82] and greater in another (small) study [83]. These comparisons should, however, be interpreted with caution as the treatment duration and the comparator arms in these studies were not consistent with those used in the postmenopausal osteoporosis studies.
The pooled estimate of the relative risk for vertebral fracture for alendronate ≥5 mg in postmenopausal osteoporosis was 0.52 (95 % CI 0.43–0.65) [79], and similar values for vertebral fracture risk in GIOP patients treated with alendronate have been published [73, 79, 80]. In three of the alendronate trials, the reported effect on vertebral fracture reduction in GIOP patients was lower than that in postmenopausal women [71, 73, 83]. Again, this comparison must be interpreted with caution as none of the differences were statistically significant. The studies were small and underpowered, and each used different doses and treatment durations and included patients with different underlying diseases.
Risedronate
Two key risedronate trials (one prevention study, one treatment study) have been carried out in the context of GIOP (Table 1) [52, 74, 84].
The prevention study was a 1-year RCT in 228 patients (151 women, 77 men, mean age ~59 years) initiating glucocorticoid therapy treated with risedronate (2.5 or 5.0 mg) or placebo, with maintenance of lumbar spine BMD as a primary outcome. All patients received calcium (500 mg/day), and vitamin D supplementation (up to 500 IU/day) was recommended for patients whose baseline serum levels of 25-hydroxyvitamin D3 were below the lower limit of the normal range. Mean prednisone dose was >20 mg/day [52]. At 1 year, lumbar spine BMD was maintained from baseline with both risedronate doses and was significantly greater than in the placebo-treated group (p < 0.05). Similarly, in femoral neck BMD, maintenance of BMD was observed with 5 mg risedronate (p < 0.05) and, to a lesser extent, with 2.5 mg risedronate, with a decline seen in the placebo group. At 1 year, a trend toward a reduced incidence of vertebral fracture was observed in the 5 mg risedronate group compared with the placebo group (5.7 vs. 17.3 %, p = 0.072). This trend was also seen in men (1/19 in the 5 mg risedronate group vs. 4/17 in the placebo group). None of the premenopausal women sustained a vertebral fracture [52].
The treatment study was a 1-year RCT in 290 patients (181 women, 109 men, mean age ~58 years) with a mean duration of glucocorticoid therapy at study entry of around 5 years who were randomized to receive either risedronate (2.5 or 5 mg) or placebo, with lumbar spine BMD as a primary outcome [74]. All patients received calcium (1,000 mg/day) and vitamin D (400 IU/day) supplementation. Mean prednisone dose was 15 mg/day [74]. This study differed from other GIOP trials in that it included a sufficient number of men to demonstrate a positive effect in reducing fracture risk. At 1 year, significantly greater mean lumbar spine and femoral neck BMD values were reported for the 5 mg risedronate group compared with placebo and for the subgroups of men, premenopausal women, and postmenopausal women. New vertebral fractures were reported in 15 % of patients in the placebo group and in 5 % in each risedronate group. The incidence of vertebral fracture was reduced by an estimated 70 % relative to placebo in both risedronate groups (p = 0.125). Statistical significance was achieved when the data of both risedronate trials were combined (p = 0.042) (Table 1) [74].
The positive effect in males seen in the treatment study was confirmed by pooling data with the prevention study [54]. Fewer patients in the risedronate groups experienced multiple vertebral fractures compared with placebo, and multiple vertebral fracture risk reduction in the risedronate 5 mg group was statistically significant (p = 0.005). Compared with placebo, a lower incidence of vertebral fracture was observed in men (66 % reduction, p = 0.12) and in postmenopausal women (73 % reduction, p = 0.05) in the risedronate 5 mg group [54].
Pamidronate
The question of whether early, intermittent, iv pamidronate administration could prevent GIOP was addressed in a small randomized study in 27 corticosteroid-naive patients who commenced long-term corticosteroid therapy at a daily dose of ≥10 mg prednisolone. Patients were randomly allocated to receive either pamidronate (induction infusion 90 mg iv followed by 30 mg iv every 3 months) or calcium (800 mg/day) for as long as glucocorticoid therapy was continued. At 1 year, the 14 patients in the pamidronate group showed a significant increase in lumbar spine BMD (3.6 %) and femoral neck BMD (2.2 %). In the 13 patients randomized to calcium, a significant BMD reduction of –5.3 % was observed at both the lumbar spine and femoral neck [85]. A second study from the same authors, with a similar design, confirmed that BMD loss was greater in the calcium-only group. No new vertebral fractures occurred during the 1-year study [86].
Comparator Studies
Zoledronic Acid Versus Risedronate
The HORIZON study was a 1-year multinational, multicenter, randomised, double-blind, double-dummy, stratified, and active-controlled clinical trial in 265 men and 568 women (373 postmenopausal, 195 premenopausal). The aim was to determine whether a single iv infusion of zoledronic acid (5 mg) was noninferior to oral risedronate treatment (5 mg/day) in the prevention and treatment of GIOP. Randomization was stratified by subpopulation (prevention/treatment) and by gender. All patients received background calcium (1,000 mg/day) and vitamin D (400–1,200 IU/day) supplementation [87].
Zoledronic acid was more effective than risedronate at increasing lumbar spine BMD and total-hip BMD from baseline levels at 12 months in both the treatment and the prevention groups (p < 0.0001 and p < 0.01, respectively). Results by treatment versus prevention subpopulations showed that increased lumbar spine BMD was favored by zoledronic acid in the treatment arm, whereas the prevention subpopulation showed maintenance of baseline BMD levels in the risedronate group [87].
No difference in the frequency of new vertebral fractures between treatment groups was observed. When the treatment and the prevention subgroups were combined, the frequency of new vertebral fractures was very low (five in the zoledronic acid group, three in the risedronate group) [87].
Alendronate Versus Alfacalcidol
The STOP study was a 18-month, randomized, double-dummy, double-blind clinical trial in 201 patients with a rheumatic disease who were starting a 6-month course of glucocorticoids (prednisone equivalent ≥7.5 mg/day). Patients were randomized to receive either alendronate 10 mg/day or alfacalcidol 1 μg/day. If indicated, patients received calcium 500 mg/day and/or vitamin D3 400 IU/day [71].
Greater change in lumbar spine BMD from baseline levels was seen in the alendronate group versus the alfacalcidol group (4 % magnitude of difference, 95 % CI 2.4–5.5; p < 0.001). Similar findings were reported for total-hip and femoral neck BMD. There were fewer fractures in the alendronate group compared with the alfacalcidol group, but the difference was not statistically significant. The hazard ratio (HR) for nonvertebral fracture in the alendronate group compared with the alfacalcidol group was 0.7 (95 % CI 0.1–4.0). Three patients in the alendronate group had a new vertebral deformity compared with eight patients in the alfacalcidol group, of whom three had symptomatic vertebral fractures (HR = 0.4, 95 % CI 0.1–1.4) [71].
Ibandronate Versus Alfacalcidol
The comparative efficacy and safety of ibandronate (2 mg iv every 3 months) with alfacalcidol (oral 1 μg/day) was investigated in a 3-year prospective cohort study in 115 patients with GIOP (lumbar spine BMD T-Score ≤–2.5). All patients received calcium supplementation (500 mg/day) [88].
After 3 years, greater increases from baseline in mean BMD were reported at the lumbar spine (13.3 vs. 2.6 %, p < 0.001) and, to a lesser extent, in the femoral neck (5.2 vs. 1.9 %, p < 0.001) with ibandronate versus alfacalcidol. Vertebral fracture risk was also reduced (8.6 vs. 22.8 %, respectively; p = 0.043, corresponding to a 62 % reduction in vertebral fracture risk with ibandronate), although the study was not powered to show a difference between the groups with respect to fracture incidence. Fewer nonvertebral fractures occurred with ibandronate compared to active vitamin D treatment (not significant). Patients treated with ibandronate injections also experienced less back pain (p < 0.001) and less loss of height (p = 0.001) than patients receiving oral alfacalcidol [88].
Response to Bisphosphonate Treatment
The rationale for assessing whether treatment response in GIOP patients is the same as in non-GIOP patient populations lies in the fact that GIOP patients have a very high frequency of underlying conditions. Because of the high prevalence of comorbidities in GIOP patients that may confound the overall treatment response, there is a possibility that a number of GIOP patients are “inadequate responders” to antiosteoporotic treatment [73].
A review of antifracture efficacy in GIOP performed in the context of a health technology–assessment exercise in the United Kingdom concluded that the point estimate for reduction of vertebral fracture was identical to that of postmenopausal osteoporosis, despite the smaller numbers of GIOP patients involved [4]. This suggests that there is no difference in treatment response between GIOP and postmenopausal osteoporosis.
Safety of Long-Term Bisphosphonate Use
Bisphosphonates are the most common antiosteoporotic agents used in the treatment of GIOP. Because all trials conducted on GIOP to date have been of limited duration, it is not yet possible to address whether prolonged bisphosphonate treatments of GIOP and of postmenopausal osteoporosis [89] are associated with similar safety issues.
Teriparatide in the Treatment of GIOP
One way to counter reduced bone formation in GIOP is with the use of teriparatide, a recombinant form of PTH that stimulates osteoblast activity and inhibits osteoblast apoptosis. In general, teriparatide is reserved for more severe GIOP and osteoporosis. High cost and the need for daily subcutaneous injections have relegated teriparatide to second-line therapy or for use in patients with severe disease in many countries.
Teriparatide Versus Alendronate
To date, the largest teriparatide study in GIOP is a randomized, double-blind, double-dummy, active comparator-controlled study with alendronate with a 18-month outcome and 3-year follow-up [90–92]. Each group contained 214 patients, mostly women (69 % in the alendronate group, 72 % in the teriparatide group), with an average age of 57 and 56 years, respectively. At study entry, average duration of glucocorticoid therapy was ~2 years with a mean dose of 7.5–7.8 mg/day. Around 45 % of patients were on >10 mg/day. Prior nonvertebral fracture was recorded in 42–44 % of patients; 25–30 % had a prevalent vertebral fracture [92].
Teriparatide displayed a clear benefit in lumbar spine and femoral neck BMD at 12, 24, and 36 months compared with alendronate. Lumbar spine BMD data showed significant between-group differences as early as 6 months in favor of teriparatide and continued significant differences between groups at 6–18 months and at end point. The absolute increment in BMD was similar to that seen in postmenopausal osteoporosis studies [93]. At 12 months, changes in total-hip BMD were observed in favor of teriparatide (p = 0.01). This remained significant at 18 months (3.8 ± 0.6 % in the teriparatide group, 2.4 ± 0.6 % in the alendronate group), when the between-group difference was 1.4 % (95 % CI 0.4–2.4). Within-group BMD changes from baseline at the lumbar spine and total hip were significant at all time points (p < 0.001). Changes from baseline in biochemical markers of bone formation (P1NP) and bone resorption [C-terminal telopeptide of type 1 collagen (CTX)] were significantly greater in the teriparatide group compared with the alendronate group [92].
Importantly, radiographic vertebral fracture rates at 36 months were lower with teriparatide compared to alendronate (1.7 vs. 7.7 %, p = 0.007) (Table 1). No clinical vertebral fractures were observed in the teriparatide group compared with four in the alendronate group (p = 0.037). There was no significant difference between the groups with respect to nonvertebral fracture rate (about 7 % in each group). Overall, adverse effects were similar between the groups. Although they occurred at a low frequency, nausea, dyspnea, insomnia, viral infections, elevated blood calcium, and symptomatic hypercalcemia were more frequent in the teriparatide-treated patients [92].
In a subanalysis, results by population subgroup were stratified according to menopausal status and gender. At baseline, 8–12 % of the 67 premenopausal women had a prevalent vertebral fracture compared with 32–39 % of the 277 postmenopausal women and 22–25 % of the 83 men. At 18 months, mean percent increases from baseline in lumbar spine BMD were greater in the teriparatide versus alendronate group in all subpopulations. The subanalysis concluded that teriparatide increased lumbar spine BMD to a greater extent than alendronate in all three GIOP subpopulations [55]. Based on these findings and the known pathophysiology of GIOP, teriparatide might be considered as a therapeutic strategy for patients at high risk of fracture.
Teriparatide Versus Estrogen
The effects of teriparatide and hormone replacement therapy on GIOP were investigated in 51 postmenopausal women randomized to receive either teriparatide + estrogen (n = 28) or estrogen alone (n = 23). All patients received background calcium (1,500 mg/day) and vitamin D3 (800 IU/day) supplementation. In the teriparatide arm, an increase in lumbar spine BMD of about 12 % was reported compared with estrogen (p < 0.001), along with a very rapid increase in bone formation and resorption markers (osteocalcin and deoxypyridinoline cross-links, respectively). The increase in resorption markers was somewhat delayed compared with formation markers [94].
Follow-Up
Most available data indicate that in individuals taking continuous oral glucocorticoids, bone loss and fracture risk increase with the dose and duration of therapy [11]. Based on expert opinion, regular BMD measurements (once a year or every 2 years) may be indicated in patients receiving high doses of glucocorticoids (Appendix). Furthermore, treatment may be revised if BMD decreases or if patients experience one or more fracture during therapy. In addition, data on markers of bone turnover in monitoring GIOP treatments are limited. Fracture risk declines after cessation of glucocorticoid therapy; as such, bone protective therapy may be simultaneously withdrawn. After treatment is stopped, risk assessment at the end of treatment is generally made on the basis of age, BMD, and fracture history [51].
Expert consensus recommends that bisphosphonate therapy may be withdrawn in a subject on glucocorticoids if BMD is close to normal and the patient is no longer at increased risk of fracture or when glucocorticoids are stopped.
Perspectives for the Treatment of GIOP
Drugs approved for the Treatment of Osteoporosis but not GIOP
Raloxifene
Raloxifene is a nonsteroidal SERM that binds to the estrogen receptor and reduces vertebral fracture and the rate of bone loss in postmenopausal women [96, 97]. Other SERMs are also available.
Few studies of raloxifene have been conducted in postmenopausal women on glucocorticoids. In a small randomized study, 114 long-term glucocorticoid-treated (prednisolone 6.7 ± 5.9 mg/day) postmenopausal women received either raloxifene (60 mg/day) or placebo, in addition to calcium and calcitriol supplementation. Five percent of patients had baseline vertebral fractures. At 1 year, lumbar spine (+1.3 ± 0.4 %, p = 0.004) and hip (+1.0 ± 0.4 %, p = 0.01) BMD increased in the raloxifene arm. In the placebo group, a decrease in lumbar spine (–0.9 ± 0.4 %, p = 0.045) and hip (–0.8 ± 0.3 %, p = 0.01) BMD was observed. There were no significant changes in femoral neck BMD. Three new fractures occurred in the placebo-treated patients compared with none in the raloxifene arm. Bone formation and resorption markers decreased significantly in the raloxifene group but not in the placebo group. The authors concluded that raloxifene displayed significant effects on BMD and was well tolerated in postmenopausal women receiving long-term glucocorticoid therapy [98].
Strontium Ranelate
Studies of strontium ranelate have demonstrated its antifracture efficacy in postmenopausal women at varying degrees of fracture risk [99, 100]. Apart from an animal study, there are no published data on the effect of strontium ranelate in GIOP. The effects of alendronate and strontium ranelate administration on bone were investigated in glucocorticoid-treated rats. After 9 weeks of treatment with methylprednisolone (5.0 mg/kg/day, 5 days/week), strontium ranelate (900 mg/kg/day) was found to be superior to alendronate (1.0 mg/kg/day) in terms of increased BMD at the femoral neck and lumbar spine and in terms of histomorphometric parameters related to bone formation [101]. Strontium ranelate may therefore become a potential treatment in GIOP.
The RANKL/RANK/OPG Pathway: Denosumab
The cytokine RANKL is essential for osteoclast differentiation and activation [102]. OPG is an endogenous inhibitor of RANKL that acts as a decoy receptor [103]. Based on the role of the RANKL/RANK/OPG system in controlling bone resorption, a human monoclonal antibody against RANKL (denosumab) was developed and has been shown to exert beneficial effects in women with postmenopausal osteoporosis [104].
Glucocorticoids affect expression of both RANKL and OPG (Fig. 1) [105–107]. A recent study showed that OPG prevented prednisolone-induced osteocyte apoptosis in mice and that RANKL inhibition with OPG attenuates the increased rate of glucocorticoid-induced osteocyte apoptosis [108]. In an earlier study, it was shown that deterioration of bone strength in prednisolone-treated human RANKL knock-in mice was prevented by denosumab. Denosumab treatment conferred a reduction in bone turnover and an increase in BMD at the femur and lumbar spine compared with placebo [109]. Together, these preclinical data add a potentially new dimension to the mode of action of denosumab in GIOP. Indeed, two recent reports described osteocytes as a major source of RANKL, perhaps more important than osteoblasts themselves [110, 111]. However, the clinical relevance of these findings remains to be determined.
Only one study has investigated the effect of denosumab in glucocorticoid-treated rheumatoid arthritis patients participating in a phase II clinical trial [112]. In addition to methotrexate, 218 patients were allocated to treatment with denosumab 60 mg, denosumab 180 mg, or placebo by subcutaneous injection at baseline and at 6 months. In a post hoc analysis, denosumab increased lumbar spine and hip BMD compared with placebo and reduced biochemical markers of bone turnover, regardless of concomitant use of glucocorticoids [113]. Denosumab therefore is potentially another effective agent in the treatment of GIOP.
Other Molecules on the Horizon: Future Directions in GIOP Treatment
There is evidence that glucocorticoids increase the levels of cathepsin K, a cysteine protease expressed in osteoclasts that degrades type 1 collagen, the principal bone matrix protein [114, 115]. Cathepsin K inhibition with agents such as odonacatib is therefore an attractive approach to reduce bone resorption in GIOP because of maintained bone formation.
Genetic studies unraveling the pivotal role of the Wnt signaling pathway in bone metabolism have led to the development of strategies targeting this pathway to increase bone formation. As discussed above, this key bone-anabolic pathway is negatively regulated by Dkk-1 and sclerostin, and expression of these Wnt inhibitors is upregulated by glucocorticoids [36, 37]. Interestingly, inhibition of Dkk-1 appears to reverse the glucocorticoid-induced suppression of osteoblast differentiation. An antibody to sclerostin was shown to enhance bone strength in mice treated with dexamethasone [116]. Thus, blocking these Wnt inhibitors may result in a specific effect in GIOP. So far, all data are from animal studies, and this therapeutic approach has not been applied in clinical practice. However, there are caveats associated with blocking Wnt inhibitors. During prednisone treatment of a patient with impaired sclerostin production, a decrease in bone resorption was observed [117]. Therefore, because glucocorticoids confer multiple effects that play a role in GIOP, targeting the Wnt signaling pathway for therapeutic purposes may be more complicated than initially thought.
Finally, another approach that may result in novel treatment perspectives for GIOP is the development of selective glucocorticoid receptor modulators. A glucocorticoid receptor–modulating compound has been found to have specific anti-inflammatory efficacy without affecting osteoblast function, but this strategy remains in early development and has so far not resulted in any clinical investigation [118, 119].
Conclusions
Glucocorticoids are widely prescribed to suppress a variety of diseases but are associated with well-established deleterious effects on bone, leading to GIOP. Both inhaled and intermittent glucocorticoids appear to be safer than continuous oral use with respect to vertebral fracture risk, though both options are also associated with possible deleterious effects on bone. There are very little data on fracture risk in patients who receive intermittent pulse glucocorticoids, and current guideline recommendations do not address this treatment modality. Appropriate treatment of patients receiving or initiating long-term glucocorticoid therapy is imperative in order to maintain bone health and prevent fractures.
The pathophysiology of GIOP is not interchangeable with that of postmenopausal osteoporosis. However, the same treatments are used in both populations, and available evidence suggests that GIOP does not significantly differ from postmenopausal osteoporosis in terms of response to therapy. Thus, despite differences in pathophysiology, treatment response might be the same in GIOP as in postmenopausal osteoporosis, although this needs to be confirmed in additional analyses. Lower treatment intervention thresholds have been proposed in GIOP patients. Prior fracture is generally accepted as a treatment criterion; age, glucocorticoid dose and treatment duration, as well as childbearing potential should also be considered. One main issue is that the evidence on antifracture efficacy is still limited, as are data on markers of bone turnover in monitoring GIOP treatments. At the onset of glucocorticoid therapy, it is recommended that antiosteoporotic treatment should be initiated in individuals at increased risk of fracture (postmenopausal women and older men with a history of fracture, older adults aged ≥70 years, or postmenopausal women and men aged ≥50 years on high doses of glucocorticoids) [47]. Bone protective therapy may also be considered in younger individuals (premenopausal women and younger men), again in the event of a previous fracture history or in those receiving high-dose glucocorticoids.
The investigation of subpopulations of GIOP patients is an interesting point as data in older adult, pediatric, and premenopausal patients treated with glucocorticoids are currently insufficient. There may be some value in performing a meta-analysis of all data from premenopausal women across all studies as there might be a specific treatment benefit in the premenopausal population compared with postmenopausal women.
Vitamin D and calcium have a role in GIOP and should, in general, be routinely administered as supplementary therapy in GIOP studies. As a general measure in the management of GIOP, recommending a healthy lifestyle may be useful in reducing the adverse effects of glucocorticoids on bone, although there is no direct evidence that such measures reduce fracture risk. Good nutrition, physical activity, and avoidance of tobacco use and alcohol abuse are recommended (level-C evidence in patients exposed to glucocorticoids for longer than 3 months) [46, 51]. Additional recommended measures in the management of glucocorticoid-treated patients include glucocorticoid-sparing therapy and use of alternative formulations or administration routes. As a preventive measure, even if calcium and vitamin D do have a beneficial effect on BMD, it is much lower compared with added antiosteoporotic treatment—in some cases regardless of the subpopulation under study (postmenopausal and premenopausal women or men). Moreover, even if BMD is maintained with calcium and vitamin D alone, their effect on fracture is conjectural. Calcium and vitamin D supplementation may be used alone in very-low-risk cases (e.g., therapy with ≤7.5 mg prednisolone equivalent per day for <3 months in premenopausal women or in patients with high bone mass). Of note, the threshold of ≤7.5 mg equivalent prednisolone may be considered on the border of a high dose (FRAX nomenclature) and associated with a degree of risk. In recent years, there has been a tendency to revise down these thresholds, although glucocorticoid treatment duration also needs to be taken into account.
Data show that vitamin D derivatives are more active than vitamin D, but no head-to-head comparative studies have been conducted. A trend toward improved BMD and lower fracture rates has been observed with active metabolites, but this is counterbalanced by the risk of hypercalcemia and hypercalciuria with the use of more polar vitamin D derivatives [68]. There are no data on whether glucocorticoid-treated patients have lower vitamin D levels compared with the general population. Glucocorticoid-responsive elements have been identified in the vitamin D receptor and other genes that control vitamin D synthesis, so it is conceivable that glucocorticoids could influence the metabolism of vitamin D [120].
Absence of evidence of fracture risk reduction in GIOP should not be interpreted to mean that antiosteoporotic drugs are ineffective. Available GIOP studies are often short term and do not include very large numbers of participants. There is good evidence for a number of drugs in the treatment of postmenopausal osteoporosis, with respect to the effect on spinal and proximal femur BMD and on reductions in vertebral fracture.
Bisphosphonates appear to be of benefit in individuals with GIOP. These agents are the most commonly used in GIOP treatment and generally well tolerated, but they are associated with adverse reactions [95]. Regular BMD measurements may be indicated in patients receiving high doses of glucocorticoids, and treatment may be adjusted in the event of a BMD decrease or multiple fractures during therapy. Fracture risk declines after cessation of glucocorticoid therapy. As such, bone protective therapy may be simultaneously withdrawn, but there is no consensus on the recommended timing for withdrawal.
A major issue in GIOP is reduced bone formation. Bone formation is stimulated by teriparatide therapy, suggesting that teriparatide may be one of the most effective available therapies in GIOP. Teriparatide has been shown to have superior BMD efficacy compared with alendronate, but side effects are more commonly observed with teriparatide. In general, teriparatide is reserved for more severe GIOP and osteoporosis.
In addition to bisphosphonates and teriparatide, several drugs currently approved in some countries for the treatment of postmenopausal osteoporosis, such as raloxifene, strontium ranelate, and denosumab, may become an option in GIOP. Other potential future treatments of GIOP include cathepsin K inhibitors, inhibitors of components of the Wnt signaling pathway, and selective glucocorticoid receptor modulators.
In summary, the available evidence shows that many of the therapies effective in postmenopausal osteoporosis are also effective in the treatment of GIOP. Fracture end-point studies and additional studies investigating specific subpopulations are needed to strengthen this conclusion.
References
Canalis E, Mazziotti G, Giustina A, Bilezikian JP (2007) Glucocorticoid-induced osteoporosis: pathophysiology and therapy. Osteoporos Int 18(10):1319–1328
van Staa TP, Leufkens HG, Cooper C (2002) The epidemiology of corticosteroid-induced osteoporosis: a meta-analysis. Osteoporos Int 13(10):777–787
Compston JE (2007) Emerging consensus on prevention and treatment of glucocorticoid-induced osteoporosis. Curr Rheumatol Rep 9(1):78–84
Kanis JA, Stevenson M, McCloskey EV, Davis S, Lloyd-Jones M (2007) Glucocorticoid-induced osteoporosis: a systematic review and cost–utility analysis. Health Technol Assess 11(7):iii–iv, ix–xi, 1–231
Walsh LJ, Wong CA, Pringle M, Tattersfield AE (1996) Use of oral corticosteroids in the community and the prevention of secondary osteoporosis: a cross sectional study. BMJ 313(7053):344–346
Van Staa TP, Leufkens HG, Abenhaim L, Begaud B, Zhang B, Cooper C (2000) Use of oral corticosteroids in the United Kingdom. QJM 93(2):105–111
Diez-Perez A, Hooven FH, Adachi JD, Adami S, Anderson FA, Boonen S, Chapurlat R, Compston JE, Cooper C, Delmas P, Greenspan SL, Lacroix AZ, Lindsay R, Netelenbos JC, Pfeilschifter J, Roux C, Saag KG, Sambrook P, Silverman S, Siris ES, Watts NB, Nika G, Gehlbach SH (2011) Regional differences in treatment for osteoporosis. The Global Longitudinal Study of Osteoporosis in Women (GLOW). Bone 49(3):493–498
Saag KG, Gehlbach SH, Curtis JR, Youket TE, Worley K, Lange JL (2006) Trends in prevention of glucocorticoid-induced osteoporosis. J Rheumatol 33(8):1651–1657
Gudbjornsson B, Juliusson UI, Gudjonsson FV (2002) Prevalence of long term steroid treatment and the frequency of decision making to prevent steroid induced osteoporosis in daily clinical practice. Ann Rheum Dis 61(1):32–36
Van Staa TP, Leufkens HG, Abenhaim L, Zhang B, Cooper C (2000) Oral corticosteroids and fracture risk: relationship to daily and cumulative doses. Rheumatology (Oxford) 39(12):1383–1389
Steinbuch M, Youket TE, Cohen S (2004) Oral glucocorticoid use is associated with an increased risk of fracture. Osteoporos Int 15(4):323–328
Van Staa TP, Leufkens HG, Abenhaim L, Zhang B, Cooper C (2000) Use of oral corticosteroids and risk of fractures. J Bone Miner Res 15(6):993–1000
Kanis JA, Johansson H, Oden A, Johnell O, de Laet C, Melton IL, Tenenhouse A, Reeve J, Silman AJ, Pols HA, Eisman JA, McCloskey EV, Mellstrom D (2004) A meta-analysis of prior corticosteroid use and fracture risk. J Bone Miner Res 19(6):893–899
Kroger H, Honkanen R, Saarikoski S, Alhava E (1994) Decreased axial bone mineral density in perimenopausal women with rheumatoid arthritis—a population based study. Ann Rheum Dis 53(1):18–23
Adachi JD, Papaioannou A (2005) In whom and how to prevent glucocorticoid-induced osteoporosis. Best Pract Res Clin Rheumatol 19(6):1039–1064
van Staa TP, Leufkens HG, Cooper C (2001) Use of inhaled corticosteroids and risk of fractures. J Bone Miner Res 16(3):581–588
Leib ES, Saag KG, Adachi JD, Geusens PP, Binkley N, McCloskey EV, Hans DB (2011) Official positions for FRAX clinical regarding glucocorticoids: the impact of the use of glucocorticoids on the estimate by FRAX of the 10 year risk of fracture from Joint Official Positions Development Conference of the International Society for Clinical Densitometry and International Osteoporosis Foundation on FRAX. J Clin Densitom 14(3):212–219
Etminan M, Sadatsafavi M, Ganjizadeh Zavareh S, Takkouche B, FitzGerald JM (2008) Inhaled corticosteroids and the risk of fractures in older adults: a systematic review and meta-analysis. Drug Saf 31(5):409–414
Wlodarczyk JH, Gibson PG, Caeser M (2008) Impact of inhaled corticosteroids on cortisol suppression in adults with asthma: a quantitative review. Ann Allergy Asthma Immunol 100(1):23–30
Van Staa TP, Bishop N, Leufkens HG, Cooper C (2004) Are inhaled corticosteroids associated with an increased risk of fracture in children? Osteoporos Int 15(10):785–791
Bijlsma JW, Duursma SA, Bosch R, Raymakers JA, Huber-Bruning O (1988) Acute changes in calcium and bone metabolism during methylprednisolone pulse therapy in rheumatoid arthritis. Br J Rheumatol 27(3):215–219
Bijlsma JW, Duursma SA, Huber-Bruning O (1986) Bone metabolism during methylprednisolone pulse therapy in rheumatoid arthritis. Ann Rheum Dis 45(9):757–760
Van der Veen MJ, Bijlsma JW (1992) Effects of different regimes of corticosteroid treatment on calcium and bone metabolism in rheumatoid arthritis. Clin Rheumatol 11(3):388–392
Rizzoli R, von Tscharner V, Fleisch H (1986) Increase of adenylate cyclase catalytic-unit activity by dexamethasone in rat osteoblast-like cells. Biochem J 237:447–454
Leonard MB, Feldman HI, Shults J, Zemel BS, Foster BJ, Stallings VA (2004) Long-term, high-dose glucocorticoids and bone mineral content in childhood glucocorticoid-sensitive nephrotic syndrome. N Engl J Med 351(9):868–875
McEvoy CE, Ensrud KE, Bender E, Genant HK, Yu W, Griffith JM, Niewoehner DE (1998) Association between corticosteroid use and vertebral fractures in older men with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 157(3 Pt 1):704–709
De Vries F, Bracke M, Leufkens HG, Lammers JW, Cooper C, Van Staa TP (2007) Fracture risk with intermittent high-dose oral glucocorticoid therapy. Arthritis Rheum 56(1):208–214
Compston J (2010) Management of glucocorticoid-induced osteoporosis. Nat Rev Rheumatol 6(2):82–88
Vestergaard P, Rejnmark L, Mosekilde L (2008) Fracture risk associated with different types of oral corticosteroids and effect of termination of corticosteroids on the risk of fractures. Calcif Tissue Int 82(4):249–257
Laan RF, van Riel PL, van de Putte LB, van Erning LJ, van’t Hof MA, Lemmens JA (1993) Low-dose prednisone induces rapid reversible axial bone loss in patients with rheumatoid arthritis. A randomized, controlled study. Ann Intern Med 119(10):963–968
Ton FN, Gunawardene SC, Lee H, Neer RM (2005) Effects of low-dose prednisone on bone metabolism. J Bone Miner Res 20(3):464–470
Weinstein RS, Jilka RL, Parfitt AM, Manolagas SC (1998) Inhibition of osteoblastogenesis and promotion of apoptosis of osteoblasts and osteocytes by glucocorticoids. Potential mechanisms of their deleterious effects on bone. J Clin Invest 102(2):274–282
Weinstein RS (2009) Glucocorticoid-induced osteoporosis. In: MR ASB (ed) Primer on the metabolic bone diseases and disorders of mineral metabolism. John Wiley & Sons, Hoboken, NJ. doi:10.1002/9780470623992.ch58
Rochefort GY, Pallu S, Benhamou CL (2010) Osteocyte: the unrecognized side of bone tissue. Osteoporosis Int 21:1457–1469
Den Uyl D, Bultink IE, Lems WF (2011) Advances in glucocorticoid-induced osteoporosis. Curr Rheumatol Rep 13(3):233–240
Hayashi K, Yamaguchi T, Yano S, Kanazawa I, Yamauchi M, Yamamoto M, Sugimoto T (2009) BMP/Wnt antagonists are upregulated by dexamethasone in osteoblasts and reversed by alendronate and PTH: potential therapeutic targets for glucocorticoid-induced osteoporosis. Biochem Biophys Res Commun 379(2):261–266
Yao W, Cheng Z, Busse C, Pham A, Nakamura MC, Lane NE (2008) Glucocorticoid excess in mice results in early activation of osteoclastogenesis and adipogenesis and prolonged suppression of osteogenesis: a longitudinal study of gene expression in bone tissue from glucocorticoid-treated mice. Arthritis Rheum 58(6):1674–1686
Hofbauer LC, Rauner M (2009) Live and let die: molecular effects of glucocorticoids on bone cells. Mol Endocrinol 23(10):1525–1531
Weinstein RS, Nicholas RW, Manolagas SC (2000) Apoptosis of osteocytes in glucocorticoid-induced osteonecrosis of the hip. J Clin Endocrinol Metab 85(8):2907–2912
Cooper MS, Rabbitt EH, Goddard PE, Bartlett WA, Hewison M, Stewart PM (2002) Osteoblastic 11beta-hydroxysteroid dehydrogenase type 1 activity increases with age and glucocorticoid exposure. J Bone Miner Res 17(6):979–986
Compston J, Reid DM, Boisdron J, Brandi ML, Burlet N, Cahall D, Delmas PD, Dere W, Devogelaer JP, Fitzpatrick LA, Flamion B, Goel N, Korte S, Laslop A, Mitlak B, Ormarsdottir S, Ringe J, Rizzoli R, Tsouderos Y, Van Staa T, Reginster JY (2008) Recommendations for the registration of agents for prevention and treatment of glucocorticoid-induced osteoporosis: an update from the Group for the Respect of Ethics and Excellence in Science. Osteoporos Int 19(9):1247–1250
Kanis JA, Johnell O, Oden A, Johansson H, McCloskey E (2008) FRAX and the assessment of fracture probability in men and women from the UK. Osteoporos Int 19(4):385–397
Kanis JA, McCloskey EV, Johansson H, Strom O, Borgstrom F, Oden A (2008) Case finding for the management of osteoporosis with FRAX—assessment and intervention thresholds for the UK. Osteoporos Int 19(10):1395–1408
Kanis JA, Johansson H, Oden A, McCloskey EV (2011) Guidance for the adjustment of FRAX according to the dose of glucocorticoids. Osteoporos Int 22(3):809–816
Ström O, Borgström F, Kanis JA, Compston J, Cooper C, McCloskey EV, Jönsson B (2011) Osteoporosis: burden, health care provision and opportunities in the European Union. Arch Osteoporos. doi: 10.1007/s11657-011-0060-1
Grossman JM, Gordon R, Ranganath VK, Deal C, Caplan L, Chen W, Curtis JR, Furst DE, McMahon M, Patkar NM, Volkmann E, Saag KG (2010) American College of Rheumatology 2010 recommendations for the prevention and treatment of glucocorticoid-induced osteoporosis. Arthritis Care Res (Hoboken) 62(11):1515–1526
Lekawasam S, Adachi JD, Agnusdei D, Bilezikian J, Boonen S, Borgström F, Cooper C, Diez Perez A, Eastell R, Hofbauer LC, Kanis JA, Langdahl BL, Lesnyak O, Lorenc R, McCloskey E, Messina OD, Napoli N, Obermayer-Pietsch B, Ralston SH, Sambrook PN, Silverman S, Sosa M, Stepan J, Suppan G, Wahl DA, Compston JE; for the Joint IOF-ECTS GIO Guidelines Working Group (2012) A framework for the development of guidelines for the management of glucocorticoid-induced osteoporosis. Osteoporos Int. doi: 10.1007/s00198-012-1958-1
Committee for Medicinal Products for Human Use (CHMP) (2006) Guideline on the evaluation of medicinal products in the treatment of primary osteoporosis. Doc. ref. CPMP/EWP/552/95 Rev. 2. European Medicines Agency, London
Committee for Medicinal Products for Human Use (CHMP) (2010) Concept paper on the need for an addendum on the clinical investigation of medicinal products intended for treatment of glucocorticoid-induced osteoporosis. Doc. ref. EMA/CHMP/EWP/15912/2010. European Medicines Agency, London
World Health Organization (1998) Guidelines for preclinical evaluation and clinical trials in osteoporosis. WHO, Geneva, Switzerland
Compston J (2011) Clinical question: what is the best approach to managing glucocorticoid-induced osteoporosis? Clin Endocrinol (Oxf) 74(5):547–550
Cohen S, Levy RM, Keller M, Boling E, Emkey RD, Greenwald M, Zizic TM, Wallach S, Sewell KL, Lukert BP, Axelrod DW, Chines AA (1999) Risedronate therapy prevents corticosteroid-induced bone loss: a twelve-month, multicenter, randomized, double-blind, placebo-controlled, parallel-group study. Arthritis Rheum 42(11):2309–2318
Saag KG, Emkey R, Schnitzer TJ, Brown JP, Hawkins F, Goemaere S, Thamsborg G, Liberman UA, Delmas PD, Malice MP, Czachur M, Daifotis AG (1998) Alendronate for the prevention and treatment of glucocorticoid-induced osteoporosis. Glucocorticoid-Induced Osteoporosis Intervention Study Group. N Engl J Med 339(5):292–299
Wallach S, Cohen S, Reid DM, Hughes RA, Hosking DJ, Laan RF, Doherty SM, Maricic M, Rosen C, Brown J, Barton I, Chines AA (2000) Effects of risedronate treatment on bone density and vertebral fracture in patients on corticosteroid therapy. Calcif Tissue Int 67(4):277–285
Langdahl BL, Marin F, Shane E, Dobnig H, Zanchetta JR, Maricic M, Krohn K, See K, Warner MR (2009) Teriparatide versus alendronate for treating glucocorticoid-induced osteoporosis: an analysis by gender and menopausal status. Osteoporos Int 20(12):2095–2104
Shaw NJ (2008) Management of osteoporosis in children. Eur J Endocrinol 159(Suppl 1):S33–S39
Van Staa TP, Cooper C, Leufkens HG, Bishop N (2003) Children and the risk of fractures caused by oral corticosteroids. J Bone Miner Res 18(5):913–918
Marini JC (2003) Do bisphosphonates make children’s bones better or brittle? N Engl J Med 349(5):423–426
Dore RK (2010) How to prevent glucocorticoid-induced osteoporosis. Cleve Clin J Med 77(8):529–536
Bianchi ML (2002) Glucorticoids and bone: some general remarks and some special observations in pediatric patients. Calcif Tissue Int 70(5):384–390
Inoue Y, Shimojo N, Suzuki S, Arima T, Tomiita M, Minagawa M, Kohno Y (2008) Efficacy of intravenous alendronate for the treatment of glucocorticoid-induced osteoporosis in children with autoimmune diseases. Clin Rheumatol 27(7):909–912
Nakhla M, Denker AE, Connor JD, Carpenter TO, Walson PD, Porras AG, Matthews CZ, Larson P, Freeman A, Wagner JA, Ward LM (2011) Bioavailability and short-term tolerability of alendronate in glucocorticoid-treated children. Clin Ther 33(10):1516–1523
Ward L, Tricco AC, Phuong P, Cranney A, Barrowman N, Gaboury I, Rauch F, Tugwell P, Moher D (2007) Bisphosphonate therapy for children and adolescents with secondary osteoporosis. Cochrane Database Syst Rev 4: CD005324
Devogelaer JP (2006) Glucocorticoid-induced osteoporosis: mechanisms and therapeutic approach. Rheum Dis Clin North Am 32(4):733–757
Homik J, Suarez-Almazor ME, Shea B, Cranney A, Wells G, Tugwell P (2000) Calcium and vitamin D for corticosteroid-induced osteoporosis. Cochrane Database Syst Rev 2:CD000952
Amin S, LaValley MP, Simms RW, Felson DT (1999) The role of vitamin D in corticosteroid-induced osteoporosis: a meta-analytic approach. Arthritis Rheum 42(8):1740–1751
Adachi JD, Bensen WG, Brown J, Hanley D, Hodsman A, Josse R, Kendler DL, Lentle B, Olszynski W, Ste-Marie LG, Tenenhouse A, Chines AA (1997) Intermittent etidronate therapy to prevent corticosteroid-induced osteoporosis. N Engl J Med 337(6):382–387
Sambrook P, Birmingham J, Kelly P, Kempler S, Nguyen T, Pocock N, Eisman J (1993) Prevention of corticosteroid osteoporosis. A comparison of calcium, calcitriol, and calcitonin. N Engl J Med 328(24):1747–1752
Talalaj M, Gradowska L, Marcinowska-Suchowierska E, Durlik M, Gaciong Z, Lao M (1996) Efficiency of preventive treatment of glucocorticoid-induced osteoporosis with 25-hydroxyvitamin D3 and calcium in kidney transplant patients. Transplant Proc 28(6):3485–3487
McDonald CF, Zebaze RM, Seeman E (2006) Calcitriol does not prevent bone loss in patients with asthma receiving corticosteroid therapy: a double-blind placebo-controlled trial. Osteoporos Int 17(10):1546–1551
De Nijs RN, Jacobs JW, Lems WF, Laan RF, Algra A, Huisman AM, Buskens E, de Laet CE, Oostveen AC, Geusens PP, Bruyn GA, Dijkmans BA, Bijlsma JW (2006) Alendronate or alfacalcidol in glucocorticoid-induced osteoporosis. N Engl J Med 355(7):675–684
De Nijs RN, Jacobs JW, Algra A, Lems WF, Bijlsma JW (2004) Prevention and treatment of glucocorticoid-induced osteoporosis with active vitamin D3 analogues: a review with meta-analysis of randomized controlled trials including organ transplantation studies. Osteoporos Int 15(8):589–602
Adachi JD, Saag KG, Delmas PD, Liberman UA, Emkey RD, Seeman E, Lane NE, Kaufman JM, Poubelle PE, Hawkins F, Correa-Rotter R, Menkes CJ, Rodriguez-Portales JA, Schnitzer TJ, Block JA, Wing J, McIlwain HH, Westhovens R, Brown J, Melo-Gomes JA, Gruber BL, Yanover MJ, Leite MO, Siminoski KG, Nevitt MC, Sharp JT, Malice MP, Dumortier T, Czachur M, Carofano W, Daifotis A (2001) Two-year effects of alendronate on bone mineral density and vertebral fracture in patients receiving glucocorticoids: a randomized, double-blind, placebo-controlled extension trial. Arthritis Rheum 44(1):202–211
Reid DM, Hughes RA, Laan RF, Sacco-Gibson NA, Wenderoth DH, Adami S, Eusebio RA, Devogelaer JP (2000) Efficacy and safety of daily risedronate in the treatment of corticosteroid-induced osteoporosis in men and women: a randomized trial. European Corticosteroid-Induced Osteoporosis Treatment Study. J Bone Miner Res 15(6):1006–1013
Jenkins EA, Walker-Bone KE, Wood A, McCrae FC, Cooper C, Cawley MI (1999) The prevention of corticosteroid-induced bone loss with intermittent cyclical etidronate. Scand J Rheumatol 28(3):152–156
Roux C, Oriente P, Laan R, Hughes RA, Ittner J, Goemaere S, Di Munno O, Pouilles JM, Horlait S, Cortet B (1998) Randomized trial of effect of cyclical etidronate in the prevention of corticosteroid-induced bone loss. Ciblos Study Group. J Clin Endocrinol Metab 83(4):1128–1133
Geusens P, Dequeker J, Vanhoof J, Stalmans R, Boonen S, Joly J, Nijs J, Raus J (1998) Cyclical etidronate increases bone density in the spine and hip of postmenopausal women receiving long term corticosteroid treatment. A double blind, randomised placebo controlled study. Ann Rheum Dis 57(12):724–727
Pitt P, Li F, Todd P, Webber D, Pack S, Moniz C (1998) A double blind placebo controlled study to determine the effects of intermittent cyclical etidronate on bone mineral density in patients on long-term oral corticosteroid treatment. Thorax 53(5):351–356
Wells GA, Cranney A, Peterson J, Boucher M, Shea B, Robinson V, Coyle D, Tugwell P (2008) Alendronate for the primary and secondary prevention of osteoporotic fractures in postmenopausal women. Cochrane Database Syst Rev 1:CD001155
Shane E, Addesso V, Namerow PB, McMahon DJ, Lo SH, Staron RB, Zucker M, Pardi S, Maybaum S, Mancini D (2004) Alendronate versus calcitriol for the prevention of bone loss after cardiac transplantation. N Engl J Med 350(8):767–776
Takeda S, Kaneoka H, Saito T (2008) Effect of alendronate on glucocorticoid-induced osteoporosis in Japanese women with systemic autoimmune diseases: versus alfacalcidol. Mod Rheumatol 18(3):271–276
Sambrook PN, Kotowicz M, Nash P, Styles CB, Naganathan V, Henderson-Briffa KN, Eisman JA, Nicholson GC (2003) Prevention and treatment of glucocorticoid-induced osteoporosis: a comparison of calcitriol, vitamin D plus calcium, and alendronate plus calcium. J Bone Miner Res 18(5):919–924
Okada Y, Nawata M, Nakayamada S, Saito K, Tanaka Y (2008) Alendronate protects premenopausal women from bone loss and fracture associated with high-dose glucocorticoid therapy. J Rheumatol 35(11):2249–2254
Reid DM, Adami S, Devogelaer JP, Chines AA (2001) Risedronate increases bone density and reduces vertebral fracture risk within one year in men on corticosteroid therapy. Calcif Tissue Int 69(4):242–247
Boutsen Y, Jamart J, Esselinckx W, Stoffel M, Devogelaer JP (1997) Primary prevention of glucocorticoid-induced osteoporosis with intermittent intravenous pamidronate: a randomized trial. Calcif Tissue Int 61(4):266–271
Boutsen Y, Jamart J, Esselinckx W, Devogelaer JP (2001) Primary prevention of glucocorticoid-induced osteoporosis with intravenous pamidronate and calcium: a prospective controlled 1-year study comparing a single infusion, an infusion given once every 3 months, and calcium alone. J Bone Miner Res 16(1):104–112
Reid DM, Devogelaer JP, Saag K, Roux C, Lau CS, Reginster JY, Papanastasiou P, Ferreira A, Hartl F, Fashola T, Mesenbrink P, Sambrook PN (2009) Zoledronic acid and risedronate in the prevention and treatment of glucocorticoid-induced osteoporosis (HORIZON): a multicentre, double-blind, double-dummy, randomised controlled trial. Lancet 373(9671):1253–1263
Ringe JD, Dorst A, Faber H, Ibach K, Sorenson F (2003) Intermittent intravenous ibandronate injections reduce vertebral fracture risk in corticosteroid-induced osteoporosis: results from a long-term comparative study. Osteoporos Int 14(10):801–807
Hollick RJ, Reid DM (2011) Role of bisphosphonates in the management of postmenopausal osteoporosis: an update on recent safety anxieties. Menopause Int 17(2):66–72
Devogelaer JP, Adler RA, Recknor C, See K, Warner MR, Wong M, Krohn K (2010) Baseline glucocorticoid dose and bone mineral density response with teriparatide or alendronate therapy in patients with glucocorticoid-induced osteoporosis. J Rheumatol 37(1):141–148
Saag KG, Shane E, Boonen S, Marin F, Donley DW, Taylor KA, Dalsky GP, Marcus R (2007) Teriparatide or alendronate in glucocorticoid-induced osteoporosis. N Engl J Med 357(20):2028–2039
Saag KG, Zanchetta JR, Devogelaer JP, Adler RA, Eastell R, See K, Krege JH, Krohn K, Warner MR (2009) Effects of teriparatide versus alendronate for treating glucocorticoid-induced osteoporosis: thirty-six-month results of a randomized, double-blind, controlled trial. Arthritis Rheum 60(11):3346–3355
Neer RM, Arnaud CD, Zanchetta JR, Prince R, Gaich GA, Reginster JY, Hodsman AB, Eriksen EF, Ish-Shalom S, Genant HK, Wang O, Mitlak BH (2001) Effect of parathyroid hormone (1–34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N Engl J Med 344(19):1434–1441
Lane NE, Sanchez S, Modin GW, Genant HK, Pierini E, Arnaud CD (1998) Parathyroid hormone treatment can reverse corticosteroid-induced osteoporosis. Results of a randomized controlled clinical trial. J Clin Invest 102(8):1627–1633
Rizzoli R, Reginster JY, Boonen S, Breart G, Diez-Perez A, Felsenberg D, Kaufman JM, Kanis JA, Cooper C (2011) Adverse reactions and drug-drug interactions in the management of women with postmenopausal osteoporosis. Calcified Tissue Int 89:91–104
Delmas PD, Bjarnason NH, Mitlak BH, Ravoux AC, Shah AS, Huster WJ, Draper M, Christiansen C (1997) Effects of raloxifene on bone mineral density, serum cholesterol concentrations, and uterine endometrium in postmenopausal women. N Engl J Med 337(23):1641–1647
Ettinger B, Black DM, Mitlak BH, Knickerbocker RK, Nickelsen T, Genant HK, Christiansen C, Delmas PD, Zanchetta JR, Stakkestad J, Gluer CC, Krueger K, Cohen FJ, Eckert S, Ensrud KE, Avioli LV, Lips P, Cummings SR (1999) Reduction of vertebral fracture risk in postmenopausal women with osteoporosis treated with raloxifene: results from a 3-year randomized clinical trial. Multiple Outcomes of Raloxifene Evaluation (MORE) investigators. JAMA 282(7):637–645
Mok CC, Ying KY, To CH, Ho LY, Yu KL, Lee HK, Ma KM (2011) Raloxifene for prevention of glucocorticoid-induced bone loss: a 12-month randomised double-blinded placebo-controlled trial. Ann Rheum Dis 70(5):778–784
Meunier PJ, Roux C, Seeman E, Ortolani S, Badurski JE, Spector TD, Cannata J, Balogh A, Lemmel EM, Pors-Nielsen S, Rizzoli R, Genant HK, Reginster JY (2004) The effects of strontium ranelate on the risk of vertebral fracture in women with postmenopausal osteoporosis. N Engl J Med 350(5):459–468
Reginster JY, Seeman E, De Vernejoul MC, Adami S, Compston J, Phenekos C, Devogelaer JP, Curiel MD, Sawicki A, Goemaere S, Sorensen OH, Felsenberg D, Meunier PJ (2005) Strontium ranelate reduces the risk of nonvertebral fractures in postmenopausal women with osteoporosis: Treatment of Peripheral Osteoporosis (TROPOS) study. J Clin Endocrinol Metab 90(5):2816–2822
Sun P, Cai DH, Li QN, Chen H, Deng WM, He L, Yang L (2010) Effects of alendronate and strontium ranelate on cancellous and cortical bone mass in glucocorticoid-treated adult rats. Calcif Tissue Int 86(6):495–501
Lacey DL, Timms E, Tan HL, Kelley MJ, Dunstan CR, Burgess T, Elliott R, Colombero A, Elliott G, Scully S, Hsu H, Sullivan J, Hawkins N, Davy E, Capparelli C, Eli A, Qian YX, Kaufman S, Sarosi I, Shalhoub V, Senaldi G, Guo J, Delaney J, Boyle WJ (1998) Osteoprotegerin ligand is a cytokine that regulates osteoclast differentiation and activation. Cell 93(2):165–176
Simonet WS, Lacey DL, Dunstan CR, Kelley M, Chang MS, Luthy R, Nguyen HQ, Wooden S, Bennett L, Boone T, Shimamoto G, DeRose M, Elliott R, Colombero A, Tan HL, Trail G, Sullivan J, Davy E, Bucay N, Renshaw-Gegg L, Hughes TM, Hill D, Pattison W, Campbell P, Sander S, Van G, Tarpley J, Derby P, Lee R, Boyle WJ (1997) Osteoprotegerin: a novel secreted protein involved in the regulation of bone density. Cell 89(2):309–319
Cummings SR, San Martin J, McClung MR, Siris ES, Eastell R, Reid IR, Delmas P, Zoog HB, Austin M, Wang A, Kutilek S, Adami S, Zanchetta J, Libanati C, Siddhanti S, Christiansen C (2009) Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med 361(8):756–765
Hofbauer LC, Gori F, Riggs BL, Lacey DL, Dunstan CR, Spelsberg TC, Khosla S (1999) Stimulation of osteoprotegerin ligand and inhibition of osteoprotegerin production by glucocorticoids in human osteoblastic lineage cells: potential paracrine mechanisms of glucocorticoid-induced osteoporosis. Endocrinology 140(10):4382–4389
Sivagurunathan S, Muir MM, Brennan TC, Seale JP, Mason RS (2005) Influence of glucocorticoids on human osteoclast generation and activity. J Bone Miner Res 20(3):390–398
Vidal NO, Brandstrom H, Jonsson KB, Ohlsson C (1998) Osteoprotegerin mRNA is expressed in primary human osteoblast-like cells: down-regulation by glucocorticoids. J Endocrinol 159(1):191–195
Weinstein RS, O’Brien CA, Almeida M, Zhao H, Roberson PK, Jilka RL, Manolagas SC (2011) Osteoprotegerin prevents glucocorticoid-induced osteocyte apoptosis in mice. Endocrinology 152(9):3323–3331
Hofbauer LC, Zeitz U, Schoppet M, Skalicky M, Schuler C, Stolina M, Kostenuik PJ, Erben RG (2009) Prevention of glucocorticoid-induced bone loss in mice by inhibition of RANKL. Arthritis Rheum 60(5):1427–1437
Nakashima T, Hayashi M, Fukunaga T, Kurata K, Oh-Hora M, Feng JQ, Bonewald LF, Kodama T, Wutz A, Wagner EF, Penninger JM, Takayanagi H (2011) Evidence for osteocyte regulation of bone homeostasis through RANKL expression. Nat Med 17(10):1231–1234
Xiong J, Onal M, Jilka RL, Weinstein RS, Manolagas SC, O’Brien CA (2011) Matrix-embedded cells control osteoclast formation. Nat Med 17(10):1235–1241
Cohen SB, Dore RK, Lane NE, Ory PA, Peterfy CG, Sharp JT, van der Heijde D, Zhou L, Tsuji W, Newmark R (2008) Denosumab treatment effects on structural damage, bone mineral density, and bone turnover in rheumatoid arthritis: a twelve-month, multicenter, randomized, double-blind, placebo-controlled, phase II clinical trial. Arthritis Rheum 58(5):1299–1309
Dore RK, Cohen SB, Lane NE, Palmer W, Shergy W, Zhou L, Wang H, Tsuji W, Newmark R (2010) Effects of denosumab on bone mineral density and bone turnover in patients with rheumatoid arthritis receiving concurrent glucocorticoids or bisphosphonates. Ann Rheum Dis 69(5):872–875
Jia J, Yao W, Guan M, Dai W, Shahnazari M, Kar R, Bonewald L, Jiang JX, Lane NE (2011) Glucocorticoid dose determines osteocyte cell fate. FASEB J 25(10):3366–3376
Stoch SA, Wagner JA (2008) Cathepsin K inhibitors: a novel target for osteoporosis therapy. Clin Pharmacol Ther 83(1):172–176
Marenzana M, Greenslade K, Eddleston A, Okoye R, Marshall D, Moore A, Robinson MK (2011) Sclerostin antibody treatment enhances bone strength but does not prevent growth retardation in young mice treated with dexamethasone. Arthritis Rheum 63(8):2385–2395
Van Lierop AH, Hamdy NA, Papapoulos SE (2010) Glucocorticoids are not always deleterious for bone. J Bone Miner Res 25(12):2796–2800
Gerber AN, Masuno K, Diamond MI (2009) Discovery of selective glucocorticoid receptor modulators by multiplexed reporter screening. Proc Natl Acad Sci USA 106(12):4929–4934
Rauch A, Gossye V, Bracke D, Gevaert E, Jacques P, Van Beneden K, Vandooren B, Rauner M, Hofbauer LC, Haegeman G, Elewaut D, Tuckermann JP, De Bosscher K (2011) An anti-inflammatory selective glucocorticoid receptor modulator preserves osteoblast differentiation. FASEB J 25(4):1323–1332
Morrison N, Eisman J (1993) Role of the negative glucocorticoid regulatory element in glucocorticoid repression of the human osteocalcin promoter. J Bone Miner Res 8(8):969–975
Cooper MS (2004) Sensitivity of bone to glucocorticoids. Clin Sci (Lond) 107(2):111–123
Acknowledgements
The Alliance for Better Bone Health (Sanofi and Warner Chilcott) provided an unrestricted educational grant to support this publication. The Alliance has had no editorial control over this publication.
Author information
Authors and Affiliations
Corresponding author
Additional information
J. A. has received consultant/speaker fees from Amgen, Eli Lilly, GlaxoSmithKline, Merck, Novartis, Pfizer, Procter & Gamble, Roche, Sanofi Aventis, and Warner Chilcott. B. M. is an employee and owns stock in Eli Lilly. S. P. has received consultant/speaker fees from Amgen, Merck, Novartis, GlaxoSmithKline, Eli Lilly, and Roche. J.-Y. R. has received consulting and lecture fees, has been on paid advisory boards, and/or has received grant support from Servier, Novartis, Negma, Lilly, Wyeth, Amgen, GlaxoSmithKline, Roche, Merckle, Nycomed, NPS, Theramex, UCB, Merck Sharp and Dohme, Rottapharm, IBSA, Genevrier, Teijin, Teva, Ebewee Pharma, Zodiac, Analis, Novo-Nordisk, and Bristol Myers Squibb. R. R. has received lecture fees and/or has been on advisory boards for Amgen, Novartis, Servier, Roche, Nycomed, and Danone. S. R. has received consultant/speaker fees from Novartis, Merck, and Eli Lilly. W. D. owns stock in Amgen and Eli Lilly. All other authors have stated that they have no conflict of interest.
Appendix: General Measures and Recommendations in GIOP Management
Appendix: General Measures and Recommendations in GIOP Management
General measures |
|---|
Glucocorticoid-sparing therapy: reduce glucocorticoid dose whenever possible |
Consider alternative route of glucocorticoid administration |
Advise good nutrition, especially with calcium and vitamin D |
Recommend regular weight-bearing exercise |
Avoid tobacco use and alcohol abuse |
Assess falls risk and advise accordingly |
Monitoring recommendations during glucocorticoid therapy |
|---|
Assess adherence to therapy, including calcium and vitamin D |
If suspect vertebral fracture, assess by X-ray or DXA-based vertebral fracture assessment |
Measure height annually and BMD at appropriate intervals (especially in patients on high glucocorticoid dose) |
Measure serum P1NP after 3 months of teriparatide therapy |
Rights and permissions
About this article
Cite this article
Rizzoli, R., Adachi, J.D., Cooper, C. et al. Management of Glucocorticoid-Induced Osteoporosis. Calcif Tissue Int 91, 225–243 (2012). https://doi.org/10.1007/s00223-012-9630-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-012-9630-5