Abstract
The association of dietary patterns and bone health is not yet well known, and findings from the rare previous studies conducted on this issue are contradictory. We assessed the dietary patterns in relation to bone mineral density (BMD) in a sample of menopausal Iranian women. In this cross-sectional study, 160 menopausal women aged 50–85 were studied and their femoral neck and lumbar spine BMDs were measured by dual-energy X-ray absorptiometry. Dietary intakes were assessed with a validated 168-item food frequency questionnaire, and dietary patterns were identified by a principal component factor analysis method. Overall, six dietary patterns emerged, two of which had a significant association with BMD. After adjusting for potential confounders, women who had higher scores for the first (high in high-fat dairy products, organ meats, red or processed meats and nonrefined cereals) and the second (high in French fries, mayonnaise, sweets and desserts and vegetable oils) dietary patterns we identified were more likely to have BMD below the median in the lumbar spine (odds ratio 2.29; 95 % confidence interval 1.05–4.96; p = 0.04) and the femoral neck (odds ratio 2.83, 95 % confidence interval 1.31–6.09; p < 0.01), respectively, compared to women with lower scores. Dietary patterns abundant in foods with high content of saturated fatty acids (similar to factor 1) or with low density of nutrients (similar to factor 2) are detrimental to bone health in menopausal Iranian women. These findings highlight the importance of proper food selection for maintaining bone health.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Osteoporosis is a major public health concern in Western societies, and its prevalence is currently on the rise in the developing world [1]. In Iran, the prevalence of osteoporosis among menopausal women is considerable, contributing to over 36,026 lost years of healthy life in 2001 according to the disability-adjusted life-years index [2, 3]. Given the high prevalence of this debilitating disease and its associated complications (e.g., fractures) and health care costs [4, 5], maintaining bone mineral density (BMD) in the first place seems crucial. BMD is largely influenced by genetic, endocrine, mechanical and nutritional factors [6], with the latter category being of prime importance because it can be changed [7].
Thus far, the most common approach to testing the association between dietary intake and bone health has been based on evaluating certain nutrients or foods. However, diets are composed of a variety of food items and complex combinations of nutrients, and therefore, evaluating certain nutrients or foods in isolation does not account for cumulative intercorrelations and interactions among foods and nutrients [8, 9]. To address this limitation, a “dietary pattern” approach (overall diet) has been widely used to evaluate the diet–disease relationship [10, 11]. By means of this multifactorial approach, interactions among foods and nutrients and the effect of confounding variables are controlled for [9, 12], and the etiologic role of diets in disease pathogenesis can be better clarified [13].
Despite its prominence, the association of dietary patterns and BMD is not yet well studied, and findings from the rare studies conducted on this issue are contradictory. Although some studies have revealed a negative association between unhealthy dietary patterns (i.e., high in red and processed meats, fats and sweets) and BMD [14–17], or a positive relationship between healthy dietary patterns (i.e., high fruit and vegetable intake) and BMD [14–16], others have failed to show such associations [18, 19]. In particular, no previous studies in the Middle East have assessed the attributes of dietary patterns to bone health, while the unique characteristics of the Middle Eastern diet and the rapid nutrition transition taking place in this region necessitates close investigation of this issue. Therefore, we sought to assess the relationship between dietary patterns and BMD in a sample of menopausal Iranian women.
Materials and Methods
Population and Sampling
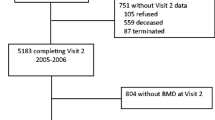
In this cross-sectional study, 213 menopausal women (aged 50–85 years) who were admitted to a bone densitometry center in Tehran, Iran, were consecutively enrolled for participation in the present study (winter 2011). Menopause was defined as lack of menstrual cycle during the past 12 months. Of these women, 160 met the inclusion criteria (mean age 60 ± 8.4 years), which included not following a specific diet (n = 11), lack of consumption of alcohol or drugs that affect bone metabolism (n = 29) such as glucocorticoids, antacids, diuretics, thyroxin, calcitonin, and anticoagulants (except for antiresorptive medications) and not having diagnosed endocrine (such as abnormal menopause or diabetes), gastrointestinal, rheumatoid and renal disorders (n = 13).
Protocols and procedures of this study were approved by the ethics board of the National Nutrition and Food Technology Research Institute (WHO Collaborating Center), Iran, and all participants provided written informed consent after being informed of the purpose of this research.
Measurements
All questionnaires were administered through interviews, and measurements were performed by a trained dietitian. General questionnaires were used to collect participants’ sociodemographic, lifestyle and clinical information, including age (years), education (less than a high school diploma, high school diploma or more), parity (n), smoking (yes, no), age at menarche (years), history of hormone replacement therapy (yes, no), fragility fracture history (yes, no), supplement intake (including calcium, vitamin D, multivitamins, minerals, glucoseamines, omega-3 fatty acids, phytoestrogens) (yes, no), and antiresorptive drug use, including bisphosphonates and selective estrogen receptor modulators (yes, no).
Weight and height were measured while participants were wearing lightweight clothing and no shoes. Weight was measured with digital scales (Seca 881, Germany) and was recorded to the nearest 0.1 kg. Height was measured with a stadiometer (Seca 214 portable stadiometer) and was recorded to the nearest 0.1 cm. Body mass index (BMI) was then calculated by dividing weight (kg) by the square of height (m).
A trained technician used a Hologic bone densitometer (Hologic Discovery W QDR Series, Hologic Inc., Bedford, MA, USA) to perform dual-energy X-ray absorptiometry to measure the BMD of the left femoral neck and lumbar spine (L1–L4) (g/cm2). The Hologic QDR densitometer was initially calibrated by the manufacturer, and it was calibrated continuously and automatically throughout the study using an automatic internal reference system. Quality control measures were performed automatically according to the guidelines for standard operating procedures. The coefficient of variation of the BMD was 1 %.
Dietary Assessment
Participants’ dietary intake during the past year was assessed with a valid and reliable semiquantitative food frequency questionnaire (FFQ) [20]. The FFQ consisted of 168 food items with standard serving sizes, and participants were asked to specify their frequency of consumption for each food item on a daily, weekly, monthly or yearly basis. These reported intakes were then converted to daily frequencies, and a manual for household measures [21] was used to convert intake frequencies to daily grams of food intake. Energy and nutrient content of foods were then calculated with the USDA food composition table included in the Nutritionist 4 software (First Databank; Hearst, San Bruno, CA, USA). We refrained from using the Iranian food composition table because it is incomplete and contains information on a limited number of raw food items [22]. However for some traditional Iranian food items that are not included in Nutritionist 4 (e.g., traditional breads and some dairy products such as Kashk), the Iranian food composition table was used [22].
In addition, relative accuracy of reported energy intakes was assessed dividing the energy intake by basal metabolic rate in order to control its confounding effect in the analyses. Basal metabolic rate was calculated from participants’ sex, age, weight and height by the Schofield equation [23]. Energy intake/basal metabolic rate values of <1.35 indicated underreporting, 1.35–2.39 normal reporting and ≥2.4 overreporting of energy intake [24]. Final analyses were conducted only on participants who completed ≥60 % of FFQ items (n = 154).
Physical Activity Assessment
Physical activity was measured by multiplying metabolic equivalent (MET) derived from a valid self-reported physical activity questionnaire by hour and day (MET∙h∙d) [25]. Physical activity measures derived from this questionnaire were categorized into nine groups ranging from sleep/rest (MET 0.9) to vigorous physical activity (MET > 6). This questionnaire has been previously used among Tehranian adult women and has yielded consistent results [26].
Statistical Analysis
All analyses were performed by SPSS software, version 16 (SPSS, Chicago, IL), and a p-value of <0.05 was considered significant. To reduce the complexity of data, the initial 168 food items were categorized into 25 predefined food groups according to similarity of their nutrient profiles (e.g., low-fat or high-fat dairy products, refined or nonrefined cereals). Culinary usage was also taken into account for grouping together some food items (e.g., tea and coffee). In addition, some food items were considered as individual food groups as a result of their unique nutrient content (e.g., eggs) or because they represented a distinct dietary pattern (e.g., French fries).
Principal component factor analysis with varimax rotation was then administered to identify optimal uncorrelated dietary patterns (factors) and to yield a simple matrix with improved interpretability. Eigenvalues of ten factors was >1, and the Scree plot identified six distinct dietary factors to be retained in the present research. We chose to keep six factors to simplify further analyses. Factor scores for each participant and each dietary pattern were calculated by adding the intake from each of the food groups weighted by factor loading [27]. Factor loading is the correlation coefficient between individual food groups and each of the dietary patterns.
Factor scores were then categorized into first (reference) and second category according to the median. BMD values for femoral neck and lumbar spine were also categorized into below and above the median (reference). Multiple logistic regression analysis was then used to calculate adjusted odds ratios (ORs) and 95 % confidence intervals (CIs) for the risk of having BMD below the median in relation to identified dietary patterns in three separate models. In model 1, the effects of age and BMI were adjusted for as potential confounders, and in model 2, the effect of physical activity and parity were also controlled. In the third model, we adjusted model 2 for smoking, education, fragility fracture history, history of hormone replacement therapy, supplement intake, antiresorptive drug use, age at menarche and relative accuracy of energy reporting.
For comparing categorical variables among different dietary patterns or BMD categories, we used Fisher’s exact test or the chi-square test, as appropriate. To evaluate the continuous variables, the Kolmogorov–Smirnov test was initially used to assess the normality assumption, and the independent sample t-test and Mann–Whitney U-test were used for comparison, where appropriate.
Results
Table 1 presents participants’ characteristics in relation to different categories of BMD. The mean BMDs for lumbar spine and femoral neck among menopausal women were 0.87 ± 0.17 and 0.67 ± 0.11 g/cm2, respectively. Significant differences were observed for age, BMI, physical activity and parity among the categories of femoral neck and lumbar spine BMDs (p < 0.05). Table 2 presents the six dietary patterns that emerged, the food groups included in each pattern and their factor loadings. Large absolute factor loadings indicate strong association between dietary patterns and food groups, whereas the plus and minus signs refer to the direction of the relationship. The first dietary pattern that emerged was characterized by high consumption of high-fat dairy products, organ meats, red or processed meats and nonrefined cereals. The second dietary pattern was abundant in French fries, mayonnaise, sweets and desserts, and vegetable oils. The third dietary pattern had high intakes of hydrogenated fats, pickles, eggs and soft drinks, while the fourth dietary pattern was associated with high intakes of vegetables, low-fat dairy products, fruits and fruit juices, legumes and fish, and low intakes of salt. The significant characteristic of the fifth dietary pattern was its high condiment and potatoes and its low refined cereals content. The sixth dietary pattern was characterized by high consumption of snacks, tea and coffee, poultry and nuts. These six dietary patterns explained 48.27 % of total variance in dietary intakes.
The characteristics of participants in different score categories (below and above the median) for each of the six derived dietary patterns are shown in Table 3. We observed significant difference in age, BMI, parity, femoral neck BMD, education, supplement intake and relative accuracy of energy reporting between the different categories of dietary patterns (p < 0.05). Table 4 presents the adjusted ORs and 95 % CIs for the risk of having BMD below the median in femoral neck and lumbar spine in relation to dietary patterns. After adjusting for several potential confounders (model 3), those in the second category of the first dietary pattern scores had significantly higher probability of having lumbar spine BMD below the median value, compared to those in the first category (OR 2.29, 95 % CI 1.05–4.96; p = 0.04). Participants in the second category had a significantly higher risk of having BMD below the median in femoral neck after adjustment for age and BMI in model 1 (OR 2.05, 95 % CI 1.03–4.07; p = 0.04), although this relationship was not statistically significant in the second and third models. In addition, those in the second category of the second dietary pattern scores were significantly at higher risk of having BMD below the median in femoral neck in model 3, compared to those in the first category (OR 2.83, 95 % CI 1.31–6.09; p < 0.01). No significant association was observed between other dietary patterns and femoral neck or lumbar spine BMD values.
Discussion
To our knowledge, this is the first study in the Middle East region to evaluate the association between dietary patterns and BMD. Findings suggest that menopausal women in the upper category of the first (high consumption of high-fat dairy products, organ meats, red or processed meats and nonrefined cereals) and second (abundant in French fries, mayonnaise, sweets and desserts, and vegetable oils) dietary pattern scores had a higher risk of having BMD below the median in the lumbar spine and femoral neck regions, respectively, compared to those in the lower categories.
In this research, the mean BMD values at the femoral neck and lumbar spine were 0.67 and 0.87 g/cm2, respectively, which are lower than those reported by Akhbari in Tehran in 2007 (0.97 g/cm2 at the femoral neck and 1.25 g/cm2 at the lumbar spine, respectively) [28]. However, these differences may be partly due to the older age of women in our study (50–85 years) compared to Akhbari’s research (20–40 years). This assumption is further confirmed by the fact that the prevalence of osteoporosis in the present research (15.6 % at femoral neck and 31.2 % at lumbar spine) was comparable to those reported among Tehranian women aged 60–69 years (17 % in total hip and 38 % in lumbar spine) [29] .
Our findings of significant associations between dietary patterns with BMD are in line with those of the previous studies; the first dietary pattern in this research replicates those of the study of Tucker et al. [15] (high consumption of meat, dairy and bread) and the study of Kontogianni et al. [18] (high intake of meat, dairy, cereals and olive oil), although the particular dietary patterns in these studies were not associated with BMD. The relationship we observed between lower BMD and the first dietary pattern in the present study might be due to the higher consumption of foods rich in saturated fatty acids and with higher omega 6/omega 3 ratios in this dietary pattern. This assumption is supported by an inverse association of saturated fatty acids with BMD observed in the NHANES III study [30]. In addition, total fat intake has shown a positive relationship with bone fragility and a negative association with BMD in women [31–33]. The ratio of linoleic acid/α-linolenic acid has also shown a negative association with BMD in both men and women [34]. Several mechanisms justify the effect of dietary fats on bone health, among which alterations in calcium absorption, prostaglandin synthesis, osteoblasts formation and oxidation of lipids play major roles [35–38]. These findings highlight the potential important role of dietary fats in bone health, especially among women.
Moreover, evidence suggests that the release of alkaline salts from bone for maintaining acid–base balance may cause osteoporosis in the long term [39]. Therefore, the association we observed between the first dietary pattern and BMD below the median value might also stem from higher dietary acid load as a result of higher intakes of acid-forming foods, such as meat and nonrefined cereals, than of alkali-forming foods, such as fruits and vegetables in this dietary pattern, which could potentially dissolve bone minerals and facilitate bone resorption [40, 41]. In addition, mild and chronic acidosis resulting from this dietary pattern could inhibit osteoblast function and increase osteoclast activity, and in consequence limit bone formation and decrease its density [42].
The second dietary pattern in our study resembled one of those in the study of Hardcastle et al. [16], the one the authors named the “snack food pattern.” In our study, this pattern was associated with lower BMD in menopausal women. In addition, dietary patterns similar to the second pattern in the present study have been previously associated with lower BMD in both premenopausal and menopausal women [14, 15, 17]. This could be justified by the high consumption of foods with higher ratios of omega 6/omega 3 and also with low density of essential nutrients for bone health such as protein, calcium, phosphorous, potassium, magnesium, vitamin C and K in this dietary pattern. These nutrients play key roles in the formation and maintenance of bone structure and its metabolic reactions and processes, and they induce several benefits for bone health [43–48]. The effect of protein intake on bone health is complicated by other foods that are consumed concurrently with proteins [49]. However, low protein intakes compromise bone quality [50–52], and different studies strongly support the positive association between protein intakes and BMD, especially among menopausal women [43, 53–57]. Generally, these findings show that replacing foods that are beneficial to bone health with those associated with lower BMD (similar to our second pattern) could be detrimental to BMD.
Although several studies have shown the potential benefits of fruits and vegetables to BMD and bone mineral content in adults [14–16, 44–46, 58–62], such an association has not been confirmed among menopausal women [15, 18, 19, 45, 63]. This was also confirmed in the present study, in which no significant association was found between the fourth dietary pattern (characterized by high intake of vegetables, low-fat dairy products, fruits and fruit juices, and fish, as well as a low intake of salt) and the femoral neck and lumbar spine BMD of menopausal women. This dietary pattern was to some extent similar to the “healthy dietary patterns” that emerged in the studies of Okubo et al. [14] and Hardcastle et al. studies [16], which were associated with higher BMD in premenopausal and menopausal women, respectively. In contrast, Tucker et al. failed to show any significant association between a dietary pattern rich in fruits, vegetables and cereals and BMD in elderly women [15]. This finding has also been confirmed in other similar studies [18, 19]. Generally, the potential mechanism suggested for the association of higher BMD and diets rich in fruits and vegetables is the lower dietary acid load in these dietary patterns, or formation of a positive calcium balance due to higher intake of particular nutrients in these foods, including magnesium and potassium [64]. However, high intake of acid-forming foods such as legumes and cheese in the fourth dietary pattern of our study might have increased renal acid load, neutralized the beneficial alkali-forming effects of fruit and vegetables and altered the acid–base balance [65–67], and hence have prevented observation of a positive relationship between the fourth dietary pattern and BMD in menopausal women in our study. In addition, the high variability in nutrient content of fruits and vegetables consumed in this study suggest that the different effect of these nutrients on BMD might have resulted in an overall insignificant association. Lack of significant associations between other dietary patterns in this study and BMD values could be attributed to omission or displacement of key food groups by less nutrient-dense foods in those dietary patterns, or categorization of some food groups with different effects in one dietary pattern or lower consumption of these food groups among menopausal women of this study.
This study has several strengths; first, to our knowledge, this is the first study to evaluate the association of Middle Eastern diet with BMD among menopausal women. Moreover, the similarity of some of the dietary patterns in the present study with those identified in previous research facilitated comparisons of results between the studies. In addition, considering all the demographic and lifestyle confounders and adjusting all analyses for these factors reduced the probability of residual confounding bias. The fourth strength of this research was the high participation rate (>90 %), which reduces the probability of selection bias.
However, several limitations are also inherent in the present study. As a pilot hypothesis-generating study with a cross-sectional design, no causal relationship can be inferred between the dietary patterns we identified and BMD. In addition, because participants were recruited exclusively from a bone densitometry center in the capital city of Iran, Tehran, our sample might not represent postmenopausal women in general in Iran. However, our participants were from different socioeconomic backgrounds and different geographical areas, with 20.8 % residing in northern parts of Tehran (the most affluent), 24.0 % living in the east, 18.8 % in the west, 23.4 % in the center (middle class), and 13.0 % in the southern districts of Tehran (the most disadvantaged). Therefore, it is likely that findings from this study could be generalized to postmenopausal women living in Tehran.
Although FFQ is a standard instrument for collecting data on diet, estimates derived from this tool are not free of errors, and therefore, identification of dietary patterns based on the FFQs in the present study is another limitation. The third limitation is related to the subjective and arbitrary decisions that researchers make during factor analysis, which could to some extent affect the results or interpretation of the findings [68]. Dietary pattern analysis is also criticized because of the dependence of derived factors on the population under study so that significant differences are observed between dietary patterns of individuals from different races, geographic location and culture. Therefore, the validity and reliability of our findings need to be confirmed in other populations.
In conclusion, findings from this study show that dietary patterns characterized by high consumption of high-fat dairy products, organ meats, processed or red meats, and nonrefined cereals or high consumption of French fries, mayonnaise, sweets and desserts, and vegetable oils are associated with lower femoral neck or lumbar spine BMD among menopausal Iranian women. Overall, these findings highlight the importance of following an appropriate dietary pattern for maintaining bone health.
References
Genant HK, Cooper C, Poor G, Reid I, Ehrlich G, Kanis J, Nordin BE, Barrett-Connor E, Black D, Bonjour JP, Dawson-Hughes B, Delmas PD, Dequeker J, Ragi Eis S, Gennari C, Johnell O, Johnston CC Jr, Lau EM, Liberman UA, Lindsay R, Martin TJ, Masri B, Mautalen CA, Meunier PJ, Khaltaev N et al (1999) Interim report and recommendations of the World Health Organization Task-Force for Osteoporosis. Osteoporos Int 10:259–264
Jamshidian Tehrani M, Kalantari N, Azadbakht L, Rajaie A, Hooshiar-rad A, Golestan B et al (2003) The prevalence of osteoporosis among women aged 40–60 in Tehran. Iran J Endocrinol Metab 5:271–276
Abolhassani F, Mohammadi M, Soltani A (2004) Burden of osteoporosis in Iran. Iranian J Publ Health (suppl 1):18–28. http://journals.tums.ac.ir/
Sambrook P, Cooper C (2006) Osteoporosis. Lancet 367(9527):2010–2018
Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A (2007) Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res 22:465–475
McGuigan FE, Murray L, Gallagher A, Davey-Smith G, Neville CE, Van’t Hof R, Boreham C, Ralston SH (2002) Genetic and environmental determinants of peak bone mass in young men and women. J Bone Miner Res 17:1273–1279
Kitchin B, Morgan S (2003) Nutritional considerations in osteoporosis. Curr Opin Rheumatol 15:476–480
Jacques PF, Tucker KL (2001) Are dietary patterns useful for understanding the role of diet in chronic disease? Am J Clin Nutr 73:1–2
Hu FB (2002) Dietary pattern analysis: a new direction in nutritional epidemiology. Curr Opin Lipidol 13:3–9
Newby PK, Tucker KL (2004) Empirically derived eating patterns using factor or cluster analysis: a review. Nutr Rev 62:177–203
Kant AK (2004) Dietary patterns and health outcomes. J Am Diet Assoc 104:615–635
Hu FB, Rimm E, Smith-Warner SA, Feskanich D, Stampfer MJ, Ascherio A, Sampson L, Willett WC (1999) Reproducibility and validity of dietary patterns assessed with a food-frequency questionnaire. Am J Clin Nutr 69:243–249
Jacobs DR Jr, Steffen LM (2003) Nutrients, foods, and dietary patterns as exposures in research: a framework for food synergy. Am J Clin Nutr 78(suppl 3):508S–513S
Okubo H, Sasaki S, Horiguchi H, Oguma E, Miyamoto K, Hosoi Y, Kim MK, Kayama F (2006) Dietary patterns associated with bone mineral density in premenopausal Japanese farmwomen. Am J Clin Nutr 83:1185–1192
Tucker KL, Chen H, Hannan MT, Cupples LA, Wilson PW, Felson D, Kiel DP (2002) Bone mineral density and dietary patterns in older adults: the Framingham Osteoporosis Study. Am J Clin Nutr 76:245–252
Hardcastle AC, Aucott L, Fraser WD, Reid DM, Macdonald HM (2011) Dietary patterns, bone resorption and bone mineral density in early post-menopausal Scottish women. Eur J Clin Nutr 65:378–385
McNaughton SA, Wattanapenpaiboon N, Wark JD, Nowson CA (2011) An energy-dense, nutrient-poor dietary pattern is inversely associated with bone health in women. J Nutr 141:1516–1523
Kontogianni MD, Melistas L, Yannakoulia M, Malagaris I, Panagiotakos DB, Yiannakouris N (2009) Association between dietary patterns and indices of bone mass in a sample of Mediterranean women. Nutrition 25:165–171
Langsetmo L, Poliquin S, Hanley DA, Prior JC, Barr S, Anastassiades T, Towheed T, Goltzman D, Kreiger N, CaMos Research Group (2010) Dietary patterns in Canadian men and women ages 25 and older: relationship to demographics, body mass index, and bone mineral density. BMC Musculoskelet Disord 11:20
Esfahani FH, Asghari G, Mirmiran P, Azizi F (2010) Reproducibility and relative validity of food group intake in a food frequency questionnaire developed for the Tehran Lipid and Glucose Study. J Epidemiol 20:150–158
Ghaffarpour M, Houshiar-Rad A, Kianfar H (1999) The manual for household measures, cooking yields factors and edible portion of foods. Agriculture Sciences Press, Tehran
Azar M, Sarkisian E (1980) Food composition table of Iran. National Nutrition and Food Research Institute, Shaheed Beheshti University, Tehran
Goldberg GR, Black AE, Jebb SA, Cole TJ, Murgatroyd PR, Coward WA, Prentice AM (1991) Critical evaluation of energy intake data using fundamental principles of energy physiology: 1. Derivation of cut-off limits to identify under-recording. Eur J Clin Nutr 45:569–581
Johansson L, Solvoll K, Bjorneboe GE, Drevon CA (1998) Under- and overreporting of energy intake related to weight status and lifestyle in a nationwide sample. Am J Clin Nutr 68:266–274
Aadahl M, Jorgensen T (2003) Validation of a new self-report instrument for measuring physical activity. Med Sci Sports Exerc 35:1196–1202
Rezazadeh A, Rashidkhani B, Omidvar N (2010) Association of major dietary patterns with socioeconomic and lifestyle factors of adult women living in Tehran. Iran Nutr 26:337–341
Kim JO, Mueller CW (1978) Factor analysis: statistical methods and practical issues. Sage, Thousand Oaks
Akhbari H (2007) The distribution of bone mineral density in healthy women in Tehran. Turk J Med Sci 37:27–30
Moayyeri A, Soltani A, Bahrami H, Sadatsafavi M, Jalili M, Larijani B (2006) Preferred skeletal site for osteoporosis screening in high-risk populations. Public Health 120:863–871
Corwin RL, Hartman TJ, Maczuga SA, Graubard BI (2006) Dietary saturated fat intake is inversely associated with bone density in humans: analysis of NHANES III. J Nutr 136:159–165
Cooper C, Atkinson EJ, Hensrud DD, Wahner HW, O’Fallon WM, Riggs BL, Melton LJ III (1996) Dietary protein intake and bone mass in women. Calcif Tissue Int 58:320–325
Kato I, Toniolo P, Zeleniuch-Jacquotte A, Shore RE, Koenig KL, Akhmedkhanov A, Riboli E (2000) Diet, smoking and anthropometric indices and postmenopausal bone fractures: a prospective study. Int J Epidemiol 29:85–92
Michaelsson K, Holmberg L, Mallmin H, Wolk A, Bergstrom R, Ljunghall S (1995) Diet, bone mass, and osteocalcin: a cross-sectional study. Calcif Tissue Int 57:86–93
Weiss LA, Barrett-Connor E, von Muhlen D (2005) Ratio of n-6 to n-3 fatty acids and bone mineral density in older adults: the Rancho Bernardo Study. Am J Clin Nutr 81:934–938
Haag M, Magada ON, Claassen N, Bohmer LH, Kruger MC (2003) Omega-3 fatty acids modulate ATPases involved in duodenal Ca absorption. Prostaglandins Leukot Essent Fatty Acids 68:423–429
Watkins BA, Li Y, Lippman HE, Feng S (2003) Modulatory effect of omega-3 polyunsaturated fatty acids on osteoblast function and bone metabolism. Prostaglandins Leukot Essent Fatty Acids 68:387–398
Parhami F (2003) Possible role of oxidized lipids in osteoporosis: could hyperlipidemia be a risk factor? Prostaglandins Leukot Essent Fatty Acids 68:373–378
Corwin RL (2003) Effects of dietary fats on bone health in advanced age. Prostaglandins Leukot Essent Fatty Acids 68:379–386
Wachman A, Bernstein DS (1968) Diet and osteoporosis. Lancet 1(7549):958–959
Bushinsky DA (2001) Acid–base imbalance and the skeleton. Eur J Nutr 40:238–244
Sellmeyer DE, Stone KL, Sebastian A, Cummings SR (2001) A high ratio of dietary animal to vegetable protein increases the rate of bone loss and the risk of fracture in postmenopausal women. Study of Osteoporotic Fractures Research Group. Am J Clin Nutr 73:118–122
Krieger NS, Sessler NE, Bushinsky DA (1992) Acidosis inhibits osteoblastic and stimulates osteoclastic activity in vitro. Am J Physiol 262(3 pt 2):F442–F448
Ilich JZ, Kerstetter JE (2000) Nutrition in bone health revisited: a story beyond calcium. J Am Coll Nutr 19:715–737
Tucker KL, Hannan MT, Chen H, Cupples LA, Wilson PW, Kiel DP (1999) Potassium, magnesium, and fruit and vegetable intakes are associated with greater bone mineral density in elderly men and women. Am J Clin Nutr 69:727–736
Macdonald HM, New SA, Golden MH, Campbell MK, Reid DM (2004) Nutritional associations with bone loss during the menopausal transition: evidence of a beneficial effect of calcium, alcohol, and fruit and vegetable nutrients and of a detrimental effect of fatty acids. Am J Clin Nutr 79:155–165
New SA, Bolton-Smith C, Grubb DA, Reid DM (1997) Nutritional influences on bone mineral density: a cross-sectional study in premenopausal women. Am J Clin Nutr 65:1831–1839
Whiting SJ, Boyle JL, Thompson A, Mirwald RL, Faulkner RA (2002) Dietary protein, phosphorus and potassium are beneficial to bone mineral density in adult men consuming adequate dietary calcium. J Am Coll Nutr 21:402–409
Booth SL, Broe KE, Gagnon DR, Tucker KL, Hannan MT, McLean RR, Dawson-Hughes B, Wilson PW, Cupples LA, Kiel DP (2003) Vitamin K intake and bone mineral density in women and men. Am J Clin Nutr 77:512–516
Heaney RP (1998) Excess dietary protein may not adversely affect bone. J Nutr 128:1054–1057
Heaney RP (1996) Age considerations in nutrient needs for bone health: older adults. J Am Coll Nutr 15:575–578
Bonjour JP, Schurch MA, Rizzoli R (1997) Proteins and bone health. Pathol Biol (Paris) 45:57–59
Macdonald HM, New SA, Fraser WD, Campbell MK, Reid DM (2005) Low dietary potassium intakes and high dietary estimates of net endogenous acid production are associated with low bone mineral density in premenopausal women and increased markers of bone resorption in postmenopausal women. Am J Clin Nutr 81:923–933
Hannan MT, Tucker KL, Dawson-Hughes B, Cupples LA, Felson DT, Kiel DP (2000) Effect of dietary protein on bone loss in elderly men and women: the Framingham Osteoporosis Study. J Bone Miner Res 15:2504–2512
Promislow JH, Goodman-Gruen D, Slymen DJ, Barrett-Connor E (2002) Protein consumption and bone mineral density in the elderly: the Rancho Bernardo Study. Am J Epidemiol 155:636–644
Rapuri PB, Gallagher JC, Haynatzka V (2003) Protein intake: effects on bone mineral density and the rate of bone loss in elderly women. Am J Clin Nutr 77:1517–1525
Dawson-Hughes B, Harris SS (2002) Calcium intake influences the association of protein intake with rates of bone loss in elderly men and women. Am J Clin Nutr 75:773–779
Devine A, Dick IM, Islam AF, Dhaliwal SS, Prince RL (2005) Protein consumption is an important predictor of lower limb bone mass in elderly women. Am J Clin Nutr 81:1423–1428
Lin PH, Ginty F, Appel LJ, Aickin M, Bohannon A, Garnero P, Barclay D, Svetkey LP (2003) The DASH diet and sodium reduction improve markers of bone turnover and calcium metabolism in adults. J Nutr 133:3130–3136
New SA, Robins SP, Campbell MK, Martin JC, Garton MJ, Bolton-Smith C, Grubb DA, Lee SJ, Reid DM (2000) Dietary influences on bone mass and bone metabolism: further evidence of a positive link between fruit and vegetable consumption and bone health? Am J Clin Nutr 71:142–151
McGartland CP, Robson PJ, Murray LJ, Cran GW, Savage MJ, Watkins DC, Rooney MM, Boreham CA (2004) Fruit and vegetable consumption and bone mineral density: the Northern Ireland Young Hearts Project. Am J Clin Nutr 80:1019–1023
Prynne CJ, Mishra GD, O’Connell MA, Muniz G, Laskey MA, Yan L, Prentice A, Ginty F (2006) Fruit and vegetable intakes and bone mineral status: a cross sectional study in 5 age and sex cohorts. Am J Clin Nutr 83:1420–1428
Zalloua PA, Hsu YH, Terwedow H, Zang T, Wu D, Tang G, Li Z, Hong X, Azar ST, Wang B, Bouxsein ML, Brain J, Cummings SR, Rosen CJ, Xu X (2007) Impact of seafood and fruit consumption on bone mineral density. Maturitas 56:1–11
Kaptoge S, Welch A, McTaggart A, Mulligan A, Dalzell N, Day NE, Bingham S, Khaw KT, Reeve J (2003) Effects of dietary nutrients and food groups on bone loss from the proximal femur in men and women in the 7th and 8th decades of age. Osteoporos Int 14:418–428
Buclin T, Cosma M, Appenzeller M, Jacquet AF, Décosterd LA, Biollaz J, Burckhardt P (2001) Diet acids and alkalis influence calcium retention in bone. Osteoporos Int 12:493–499
Massey LK (1998) Does excess dietary protein adversely affect bone? Symposium overview. J Nutr 128:1048–1050
Remer T, Manz F (1995) Potential renal acid load of foods and its influence on urine pH. J Am Diet Assoc 95:791–797
Remer T, Manz F (1994) Estimation of the renal net acid excretion by adults consuming diets containing variable amounts of protein. Am J Clin Nutr 59:1356–1361
Martinez ME, Marshall JR, Sechrest L (1998) Factor analysis and the search for objectivity. Am J Epidemiol 148:17–19
Acknowledgments
We thank the participants for their enthusiastic support. We are grateful to the members of National Nutrition and Food Technology Research Institute for their kind collaboration. This work was supported by a grant from “National Nutrition and Food Technology Research Institute (WHO Collaborating Center)” of Shahid Behehshti University of Medical Sciences, Iran.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors have stated that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Karamati, M., Jessri, M., Shariati-Bafghi, SE. et al. Dietary Patterns in Relation to Bone Mineral Density Among Menopausal Iranian Women. Calcif Tissue Int 91, 40–49 (2012). https://doi.org/10.1007/s00223-012-9608-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-012-9608-3