Abstract
An important objective of genetic research in osteoporosis is to translate genotype data into the prognosis of fracture. The present study sought to develop a prognostic model for predicting osteoporotic fracture by using information from a genetic marker and clinical risk factors. It was designed as a prospective epidemiological study which involved 894 women of Caucasian background aged 60+ years who had been followed for a median of 9 years (from 1989 and 2008, range 0.2–18 years). During the follow-up period, fragility fracture was ascertained by X-ray reports for all women. Bone mineral density (BMD) at the femoral neck was measured by dual-energy X-ray absorptiometry. Genotypes of the Sp1 binding site in the first intron of the collagen I alpha 1 (COLIA1) gene polymorphism were determined by polymerase chain reaction, digestion with BalI restriction enzyme, and agarose gel electrophoresis. The relationship between COL1A1 genotype and fracture was assessed by the Cox proportional hazards model, from which nomograms were developed for individualizing the risk of fracture. The distribution of COL1A1 genotypes was consistent with the Hardy-Weinberg equilibrium law: GG (63.8%), GT (32.6%), and TT (3.6%). During the follow-up period, there were 322 fractures, including 77 hip and 127 vertebral fractures. There was an overrepresentation of the TT genotype in the fracture group (6.2%) compared with the nonfracture group (2.3%). Compared with carriers of GT and GG, women carrying the TT genotype had increased risk of any fracture (relative risk [RR] = 1.91, 95% CI 1.21–3.00), hip fracture (RR = 3.67, 95% CI 1.69–8.00), and vertebral fracture (RR = 3.36, 95% CI 1.81–6.24). The incorporation of COL1A1 genotypes improved the risk reclassification by 2% for any fragility fracture, 4% for hip fracture, and 5% for vertebral fracture, beyond age, BMD, prior fracture, and fall. Three nomograms were constructed for predicting fracture risk in an individual woman based on age, BMD, and COLIA1 genotypes. These data suggest that the COLIA1 Sp1 polymorphism is associated with the risk of fragility fracture in Caucasian women and that the polymorphism could enhance the predictive accuracy of fracture prognosis. The nonograms presented here can be useful for individualizing the short- and intermediate-term prognosis of fracture risk and help identify high-risk individuals for intervention for appropriate management of osteoporosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
From the age of 60, the lifetime risk of fracture for women is 44% [1]. The lifetime risk of hip fracture for a white woman (1/6) is higher than the lifetime risk of developing breast cancer (1/9) [2]. A preexisting fracture confers a substantially increased risk of subsequent fracture [3, 4] and premature mortality [5], which in turn incurs significant heath-care costs [6, 7]. Currently, fewer than one-third of patients who sustain a fragility fracture are properly diagnosed and treated [8]. Therefore, one of the major priorities in osteoporosis research is to develop valid models for identifying individuals at high risk of fracture for allocating appropriate medical intervention [9].
Accumulated research evidence during the past three decades has suggested that advancing age, low bone mineral density (BMD) [10], low body mass index [11], smoking [12], corticosteroid use [13], and prior fractures [3, 4] are major independent predictors of fracture in women. Using these clinical risk factors, a number of prognostic models have recently been developed for predicting fracture risk [14–18]. The discriminatory value of these prognostic models is moderate to good, with areas under the receiver operating characteristic curve ranging 0.7–0.8 [17, 18]. However, there is still room for improving the predictive accuracy of these prognostic models by incorporating information from nonclinical risk factors.
Fracture liability is partially determined by genetic factors [19]. Twin studies suggest that approximately 48% of the liability to hip fracture is genetically related [20]. Among the genes that have been implicated in the regulation of fracture risk, the collagen I alpha 1 (COL1A1) gene has been consistently associated with fracture risk [21–28]. If the effect of COL1A1 on fracture risk is independent of clinical risk factors, then the incorporation of COL1A1 genotype could improve the prognosis of fracture.
A nomogram is a prognostic model that combines several risk factors to provide an accessible assessment tool to clinicians and patients. We have recently developed simple prognostic models for individualizing the risk of fracture [17] based on simple clinical risk factors. It is hypothesized that the incorporation of COL1A1 genotypes would improve the predictive accuracy of the nomogram. The present study was designed to test that hypothesis by developing a prognostic model for predicting fracture risk, taking into account COL1A1 genotype.
Materials and Methods
Study Design
The present study was part of the ongoing Dubbo Osteoporosis Epidemiology Study, which was designed as a prospective population-based investigation, in which women aged 60+ years in 1989 were invited to participate. The study details and protocol have been described elsewhere [1]. Briefly, Dubbo is a city located approximately 400 km from Sydney, with a population of 32,000 people. It was selected for the study due to its stable population and geographic isolation, which allow total ascertainment of fracture incidence. This study was approved by the St. Vincent’s Ethics Committee, and written informed consent was obtained from each participant.
Measurements and Fracture Ascertainment
The original study population included 888 men and 1,402 women progressively recruited from 1989 and 1994. However, in this study, clinical history and anthropometric data from 915 women, who had provided blood samples for genetic analysis, were analyzed. Each woman was interviewed by a nurse coordinator at initial and subsequent visits at approximately 2-year intervals. At each visit a structured questionnaire was administered to collect data, including lifestyle factors (i.e., smoking habits, dietary calcium intake) and anthropometric variables (including weight and height) were measured. In addition, any history of falls in the preceding 12 months and any history of fractures after the age of 50 were recorded.
BMD (g/cm2) was measured at the lumbar spine (LSBMD) and the femoral neck (FNBMD) by dual-energy X-ray absorptiometry with a LUNAR DPX-L densitometer (GE Lunar, Madison, WI). The precision of BMD measurements in normal subjects at our institution is 1.3% at the lumbar spine and 3.5% at the femoral neck [29]. In this study, FNBMD was used in the development of the prognostic model because it is less susceptible to age-related degenerative changes than LSBMD.
Fractures were recorded from radiology centers servicing the Dubbo area, and the circumstances surrounding the fractures were determined by personal interview. All fractures included in the study were low-trauma fractures caused by a fall from standing height or less. Vertebral fractures were clinically diagnosed. There was no systemic X-ray screening before the study to identify prevalent or asymptomatic vertebral fractures. Incidentally found, i.e., asymptomatic, vertebral fractures were included, provided that there was no known malignancy or metabolic bone disease. Morphometric vertebral fractures were not considered in the analysis.
Genotyping
Blood samples were collected at baseline and in each subsequent visit for genetic and biochemical analyses, and DNA was extracted from leukocytes. The polymorphism of G to T in the first intron of the COL1A1 gene was genotyped by the restriction fragment length polymorphism method with MscI (New England Biolabs, Beverly, MA) and an isoschizomer of BalI. Digestions were analyzed by 3% agarose gel electrophoresis. Genotypes for this restriction site were denoted as GG, GT, and TT, with T being the minor allele. To validate the accuracy of genotyping, 30 subjects were randomly regenotyped with 100% consistency.
Data Analysis
The association between clinical risk factors and COL1A1 genotype and fracture was analyzed by the Cox proportional hazards model. In this model, the time from entry to fracture was considered an end point. Based on estimated parameters of the optimal model, nomograms with the inclusion of COL1A1, age, FNBMD, prior fracture, and fall were constructed using the Design library within the R system [30, 31]. In order to assess the incremental prognostic value attributable to COL1A1 genotypes, a reclassification analysis [32] was performed. Two specific models were considered: model I, with age and BMD, prior fracture, and fall, and model II, with age, BMD, prior fracture, fall, and COL1A1 genotypes. The area under the receiver operating characteristic curve [33] was not used because it is too insensitive to change [34]. In this reclassification analysis, the 10-year probability of fracture was estimated by each model and then classified into three risk groups: <10%, 10–20%, and >20%. The proportion of women who would be reclassified into three risk groups between the model without COL1A1 genotypes and the model with COL1A1 genotypes was calculated, and this proportion is regarded as the net improvement in prediction.
Results
During the follow-up period (median 9 years, range 0.2–18), 332 women had sustained at least one fragility fracture, including 77 hip and 127 clinical vertebral fractures. Women with fracture were older and had lower body weight, shorter stature, and lower BMD than women without fracture (Table 1). The differences were more pronounced in patients with hip fracture, in which FNBMD was approximately 1 standard deviation (SD) lower than in women without fracture. However, there were no significant differences in smoking habit, alcohol consumption, and dietary calcium intake between the fracture and nonfracture groups.
COL1A1 Genotypes and Fracture Risk
The Sp1 binding genotypes of the COL1A1 gene were successfully determined in 894 women. The distribution of COL1A1 genotypes was consistent with the expected frequencies by the Hardy–Weinberg equilibrium law: GG (63.8%), GT (32.6%), and TT (3.6%). There were no statistically significant differences in age, weight, and BMD among the genotypes (Table 2). However, carriers of the TT genotype had significantly greater height than those with the GG genotype. Women homozygous for the T allele had a greater dietary calcium intake than those without the allele (P = 0.02).
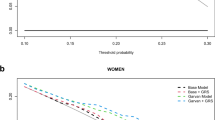
Among the fracture group, 6.2% (n = 20) of fracture cases were carriers of the TT genotype; this proportion was significantly higher than that in the nonfracture group (2.3%, P = 0.03) (Table 1). In addition, the frequency of this homozygote was more prevalent in the hip fracture group (9.4%) and the vertebral fracture group (8.9%) compared with the nonfracture group. Furthermore, women with the TT genotype had a greater cumulative probability of fracture than those with the GG or GT genotype (Fig. 1)
Risk Factors for Fracture
Advancing age, weight loss, shorter stature, lower BMD at the femoral neck or lumbar spine, and a history of fractures and falls were associated with high risk of any fracture, hip or vertebral (Table 3). In hip fracture, the magnitude of association was more pronounced in which every 5 years of advancing age or 10 kg of lower weight had a double risk of hip fracture (Table 3). Similarly, women who were 5 cm shorter had a 50% risk of sustaining a hip fracture, but the magnitude of effect was reduced in non-hip fractures (Table 3).
BMD at both the femoral neck and lumbar spine was consistently associated with the risk of all types of fracture. Indeed, FNBMD was the most consistent predictor of hip fracture with a 3.35-fold (95% confidence interval [CI] 2.67–4.19) increase in hip fracture risk for every SD lower in BMD, while each SD lower in LSBMD was associated with a double risk of vertebral fracture (Table 3). The same relationship was observed for other fracture types, albeit with lesser effect size. There was no significant association between a history of falls and vertebral fracture risk.
Women carrying the TT genotype had an increased risk of any fracture (relative risk [RR] = 1.91, 95% CI 1.21–3.04), hip (RR = 4.21, 95% CI 1.88–9.45), and vertebral (RR = 3.57, 95% CI 1.89–6.77) fracture compared to women with the GG genotype. There were no statistically significant associations between the GT and GG genotypes for any type of fractures (Table 3). Therefore, in multivariable analysis, participants with GT and GG genotypes were combined into one group and compared with those with the TT genotype. This was in agreement with a previous study [25]. When age, FNBMD, and a history of fractures and falls were adjusted in a multivariable Cox proportional hazards model, the strength of association between TT genotype and risk of all fractures did not change or was even stronger (Table 4).
Reclassification Analysis
For any fracture, approximately 13% of women were reclassified into higher or lower risk categories in the model containing COL1A1 genotypes (Table 5). This reclassification was 30% for hip fracture and 33% for clinical vertebral fracture (Table 5). On further analysis by fracture status to account for the “correct” movement into risk categories (higher risk for women in whom fracture had occurred and lower risk for women free of fracture), the inclusion of COL1A1 genotypes mainly improved the classification of nonfracture rather than fracture cases. For example, in 561 women who had not sustained a fragility fracture, the model with COL1A1 genotypes reclassified 17 down and eight up, a net improvement of nine (or ~2%). On the other hand, among 317 women who sustained a fracture, the model with COL1A1 genotypes was tied with the model without COLIA1 genotypes. The overall net reclassification improvement was 4% for hip fracture and 5% for clinical vertebral fracture.
Multivariable models including the three independent predictive factors age, FNBMD and COL1A1 genotype were developed for the risk of any, hip, or vertebral fracture. The areas under the curve of these models were 0.76, 0.88, and 0.72 for predictive models of any, hip, and vertebral fracture, respectively. Based on parameters obtained from multiple Cox proportional hazards models, nomograms were developed for prediction of any fracture (Fig. 2a), hip fracture (Fig. 2b), and clinical vertebral fracture (Fig. 2c).
Prognostic nomograms for predicting the probability of sustaining any fragility fracture (a), hip fracture (b), and vertebral fracture (c) based on age, FNBMD T score, history of fractures and falls, and genotype. Instruction for usage: Draw a vertical line from “Age” to the “Total Points” axis to determine the score for age. Repeat the process for the other risk factors to obtain total points, and from the “Total Points” axis draw a vertical line to the 5-year and 10-year risk axes to estimate the probability of sustaining a fracture in the next 5 and 10 years, respectively
Clinical Applications of the Nomogram
Patient 1
Patient 1 was a 75-year-old woman with an FNBMD T score of –2.5 (osteoporosis), one prior fracture, one fall in the last 12 month, and GG genotype. Her age (Fig. 2b) scored 18 points, T score 60 points, prior fracture 9 points, fall 3 points, and GG genotype 0 points. Therefore, the total points for the woman were 90 on the “Total Points” axis, giving an estimated 5-year average risk of hip fracture of ~10%.
Patient 2
Patient 2 was a 60-year-old woman with an FNBMD T score of –2 (osteopenia), one prior fracture, one fall in the last 12 months, and TT genotype. Her age (Fig. 2b) scored 5 points, T score 55 points, prior fracture 9 points, fall 3 points, and TT genotype 23 points. Therefore, the total points for the woman were 95 on the “Total Points” axis, giving an estimated 10-year average risk of hip fracture of ~12%.
Discussion
Although several candidate genes have been suggested to be associated with fracture, the replication of these findings has been poor [35], as is often seen in other fields of research [36]. Among the candidate genes of osteoporosis that have been studied, the association between COL1A1 and fracture has been independently replicated in several studies [21]. However, the extent to which the genetic information could improve fracture prognosis is largely unknown. The present result confirmed that women carrying the COLIA1 Sp1 TT genotype had an increased risk of fragility fracture, including hip and vertebral fracture, and that the use of this polymorphism could improve the predictive accuracy of fracture prognosis over and above that of age and FNBMD.
Our result is consistent with an earlier meta-analysis which found an additive association between the COL1A1 gene variant and fracture risk [26]. In that meta-analysis, the risk of any fracture among TT carriers was increased by 1.78-fold compared to those with the G allele [26]; however, in a large-scale study on 20,708 Caucasian participants, the TT genotype was associated with a 33% increased risk of incident vertebral fracture, and this association was independent of BMD [37]. Taken together, these data suggest that the COL1A1 gene is a suitable candidate gene for improving the predictive value of existing prognostic models of fracture. In this study, we have demonstrated a simple way to translate a genetic effect into such prognostic models for individualizing fracture risk.
Developing a genetic test for assessment of genetic predisposition to fracture is one of the goals in osteoporosis research. This means using genetic testing to identify individuals with higher risk of fracture, who could be encouraged either to change lifestyle factors or to take medications to reduce fracture risk. Prognosis based on our nomogram model could be helpful in fracture prediction by providing an absolute risk rather than placing individuals into risk-group strata usually expressed by relative risk. This absolute risk approach allows a better appreciation of fracture risk to an individual because it takes into account the time dimension of the risk.
There are some major advantages of using genetic markers as prognostic factors of fracture risk. First, since an individual’s genotype is time-invariant, it is easier to estimate its effect size and to incorporate its information in a prognostic model. Second, as the association between COL1A1 and fracture risk appears to be independent of clinical risk factors, the use of such a genetic marker can potentially improve the predictive value. Third, although there is no genetic therapy for individuals at high risk of fracture, the use of genetic markers could help segregate individuals at high risk from those with low risk of fracture and help manage the burden of osteoporosis in the community.
The potential usefulness of genetic testing for fracture risk prediction can be evaluated by comparing the discriminative accuracy of predictions based on models which do and do not include the genetic information. Traditionally, the increase in the area under the receiver operating characteristic curve was considered a measure of improvement; however, in recent years it has become clear that such a measure is not optimal because it is relatively insensitive, leading to omission of important prognostic factors [33]. In our study, for example, for hip fracture prediction, the area under the receiver operating characteristic curve for model with age, BMD T score, prior fracture, and fall was 0.86; when COL1A1 genotypes were added to the model, the value increased to 0.88—a modest improvement. However, using the reclassification analysis, it was shown that the improvement of prognosis due to COL1A1 genotypes was substantial, with ~5% reclassification for hip and vertebral fractures. Moreover, in a further analysis, the improvement was mainly in the specificity, not the sensitivity, of prognosis. This is perhaps not surprising because the relative frequency of the “risk genotype” (TT) is only 5% in the population and the magnitude of association between the genotype and fracture risk is modest.
The ultimate aim of developing a prognostic model is to provide clinicians and each individual with his or her risk estimate to guide clinical decisions. At present, individuals with low BMD (i.e., T scores less than −2.5) or with a history of low-trauma fracture are recommended for therapeutic intervention [38, 39]. This recommendation is logical and appropriate since these individuals have higher risk of fracture [40, 41] and treatment can reduce their risk of fracture [42–44]. However, because fracture is a multifactorial event, there is more than one way that an individual can attain the risk conferred by either low BMD or a prior fracture [45]. Indeed, as shown in this study, a 60-year-old woman with a T score of −2.3 could have the same risk of fracture as a 75-year-old woman with a T score of −1 if the two are carriers of genotype TT. These data support the informativeness of a multivariable prognostic model and the limitation of a risk stratification–based approach for risk assessment for an individual.
It has been suggested that treatment should be considered for postmenopausal women and men aged 50 years or more [46] (1) with a preexisting hip or clinical vertebral fracture or a morphometric vertebral fracture, (2) with FN- or LSBMD T score ≤−2.5 after excluding secondary cause of osteoporosis, and (3) with FN- or LSBMD T score between −1 and −2.5 and a 10-year risk of hip fracture ≥3% or a 10-year risk of major osteoporotic fracture ≥20%. The nomogram presented here and the FRAX model [15] in conjunction with the above guidelines can help select suitable individuals for intervention.
A number of considerations should be taken into account in extrapolating the present findings to other populations. The present finding was based on an association—not linkage—analysis and, as such, does not necessarily show that the COL1A1 gene is directly involved, rather than being a marker for nearby genes that are linked to hip fracture liability. The data were based on a sample of Caucasian women, whose lifestyles and environmental living conditions are relatively homogeneous; hence, they may not apply to women in other populations or to men. The number of fractures, particularly hip fracture, together with the low frequency of the TT genotype were modest, resulting in a rather wide confidence interval of the estimate of association between the gene and fracture. The sample size, as in most studies to date, was not sufficient to examine potential gene–environment interactions, which might improve fracture risk prediction. There are likely many other genes associated with fracture risk which were not considered in the present model.
Both prognosis and treatment decisions are concerned with an individual. Each individual is a unique case because there is no “average individual” in the population. The uniqueness of an individual can be defined in terms of the individual’s environmental and genetic factors. The knowledge of genetics, in combination with environmental factors, can shift our current risk-stratification approaches to a more individualized evaluation and treatment of osteoporosis. To this end, these data indicate that a risk genotype of the COL1A1 gene is associated with an increased risk of fracture and that the incorporation of this genetic information into a prognostic model could enhance its accuracy and predictive value for an individual. These data support the potential utility of genetic information in an individual’s absolute fracture risk prediction.
References
Nguyen ND, Ahlborg HG, Center JR, Eisman JA, Nguyen TV (2007) Residual lifetime risk of fractures in women and men. J Bone Miner Res 22:781–788
No authors listed (2003) Stat Bite: Lifetime risk of being diagnosed with cancer. J Natl Cancer Inst 95:1745
Kanis JA, Johnell O, De Laet C, Johansson H, Oden A, Delmas P, Eisman J, Fujiwara S, Garnero P, Kroger H, McCloskey EV, Mellstrom D, Melton LJ, Pols H, Reeve J, Silman A, Tenenhouse A (2004) A meta-analysis of previous fracture and subsequent fracture risk. Bone 35:375–382
Center JR, Bliuc D, Nguyen TV, Eisman JA (2007) Risk of subsequent fracture after low-trauma fracture in men and women. JAMA 297:387–394
Cauley JA, Thompson DE, Ensrud KC, Scott JC, Black D (2000) Risk of mortality following clinical fractures. Osteoporos Int 11:556–561
Melton LJ 3rd, Gabriel SE, Crowson CS, Tosteson AN, Johnell O, Kanis JA (2003) Cost-equivalence of different osteoporotic fractures. Osteoporos Int 14:383–388
Randell A, Sambrook PN, Nguyen TV, Lapsley H, Jones G, Kelly PJ, Eisman JA (1995) Direct clinical and welfare costs of osteoporotic fractures in elderly men and women. Osteoporos Int 5:427–432
Eisman J, Clapham S, Kehoe L (2004) Osteoporosis prevalence and levels of treatment in primary care: the Australian Bone Care Study. J Bone Miner Res 19:1969–1975
Raisz LG (2005) Pathogenesis of osteoporosis: concepts, conflicts, and prospects. J Clin Invest 115:3318–3325
Johnell O, Kanis JA, Oden A, Johansson H, De Laet C, Delmas P, Eisman JA, Fujiwara S, Kroger H, Mellstrom D, Meunier PJ, Melton LJ 3rd, O’Neill T, Pols H, Reeve J, Silman A, Tenenhouse A (2005) Predictive value of BMD for hip and other fractures. J Bone Miner Res 20:1185–1194
De Laet C, Kanis JA, Oden A, Johanson H, Johnell O, Delmas P, Eisman JA, Kroger H, Fujiwara S, Garnero P, McCloskey EV, Mellstrom D, Melton LJ 3rd, Meunier PJ, Pols HA, Reeve J, Silman A, Tenenhouse A (2005) Body mass index as a predictor of fracture risk: a meta-analysis. Osteoporos Int 16:1330–1338
Kanis JA, Johnell O, Oden A, Johansson H, De Laet C, Eisman JA, Fujiwara S, Kroger H, McCloskey EV, Mellstrom D, Melton LJ, Pols H, Reeve J, Silman A, Tenenhouse A (2005) Smoking and fracture risk: a meta-analysis. Osteoporos Int 16:155–162
Kanis JA, Johansson H, Oden A, Johnell O, de Laet C, Melton IL, Tenenhouse A, Reeve J, Silman AJ, Pols HA, Eisman JA, McCloskey EV, Mellstrom D (2004) A meta-analysis of prior corticosteroid use and fracture risk. J Bone Miner Res 19:893–899
Black DM, Steinbuch M, Palermo L, Dargent-Molina P, Lindsay R, Hoseyni MS, Johnell O (2001) An assessment tool for predicting fracture risk in postmenopausal women. Osteoporos Int 12:519–528
Kanis JA, Johnell O, Oden A, Johansson H, McCloskey E (2008) FRAX and the assessment of fracture probability in men and women from the UK. Osteoporos Int 19:385–397
van Staa TP, Geusens P, Kanis JA, Leufkens HG, Gehlbach S, Cooper C (2006) A simple clinical score for estimating the long-term risk of fracture in post-menopausal women. QJM 99:673–682
Nguyen ND, Frost SA, Center JR, Eisman JA, Nguyen TV (2007) Development of a nomogram for individualizing hip fracture risk in men and women. Osteoporos Int 18:1109–1117
Nguyen ND, Frost SA, Center JR, Eisman JA, Nguyen TV (2008) Development of prognostic nomograms for individualizing 5-year and 10-year fracture risks. Osteoporos Int 19:1431–1444
Nguyen TV, Eisman JA (2006) Pharmacogenomics of osteoporosis: opportunities and challenges. J Musculoskelet Neuronal Interact 6:62–72
Michaelsson K, Melhus H, Ferm H, Ahlbom A, Pedersen NL (2005) Genetic liability to fractures in the elderly. Arch Intern Med 165:1825–1830
Efstathiadou Z, Tsatsoulis A, Ioannidis JP (2001) Association of collagen I alpha 1 Sp1 polymorphism with the risk of prevalent fractures: a meta-analysis. J Bone Miner Res 16:1586–1592
Grant SF, Reid DM, Blake G, Herd R, Fogelman I, Ralston SH (1996) Reduced bone density and osteoporosis associated with a polymorphic Sp1 binding site in the collagen type I alpha 1 gene. Nat Genet 14:203–205
McGuigan FE, Armbrecht G, Smith R, Felsenberg D, Reid DM, Ralston SH (2001) Prediction of osteoporotic fractures by bone densitometry and COLIA1 genotyping: a prospective, population-based study in men and women. Osteoporos Int 12:91–96
Langdahl BL, Ralston SH, Grant SF, Eriksen EF (1998) An Sp1 binding site polymorphism in the COLIA1 gene predicts osteoporotic fractures in both men and women. J Bone Miner Res 13:1384–1389
Bernad M, Martinez ME, Escalona M, Gonzalez ML, Gonzalez C, Garces MV, Del Campo MT, Martin Mola E, Madero R, Carreno L (2002) Polymorphism in the type I collagen (COLIA1) gene and risk of fractures in postmenopausal women. Bone 30:223–228
Mann V, Ralston SH (2003) Meta-analysis of COL1A1 Sp1 polymorphism in relation to bone mineral density and osteoporotic fracture. Bone 32:711–717
Uitterlinden AG, Burger H, Huang Q, Yue F, McGuigan FE, Grant SF, Hofman A, van Leeuwen JP, Pols HA, Ralston SH (1998) Relation of alleles of the collagen type I alpha1 gene to bone density and the risk of osteoporotic fractures in postmenopausal women. N Engl J Med 338:1016–1021
Nguyen TV, Esteban LM, White CP, Grant SF, Center JR, Gardiner EM, Eisman JA (2005) Contribution of the collagen I alpha1 and vitamin D receptor genes to the risk of hip fracture in elderly women. J Clin Endocrinol Metab 90:6575–6579
Nguyen TV, Sambrook PN, Eisman JA (1997) Sources of variability in bone mineral density measurements: implications for study design and analysis of bone loss. J Bone Miner Res 12:124–135
Harrell FE Jr, Lee KL DBM (1996) Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med 15:361–387
Harrell FE Jr, Margolis PA, Gove S, Mason KE, Mulholland EK, Lehmann D, Muhe L, Gatchalian S, Eichenwald HF (1998) Development of a clinical prediction model for an ordinal outcome: the World Health Organization multicentre study of clinical signs and etiological agents of pneumonia, sepsis and meningitis in young infants. WHO/ARI Young Infant Multicentre Study Group. Stat Med 17:909–944
Pencina MJ, D’Agostino RB Sr, D’Agostino RB Jr, Vasan RS (2008) Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med 27:157–172 discussion 207–112
Lasko TA, Bhagwat JG, Zou KH, Ohno-Machado L (2005) The use of receiver operating characteristic curves in biomedical informatics. J Biomed Inform 38:404–415
Cook NR (2008) Statistical evaluation of prognostic versus diagnostic models: beyond the ROC curve. Clin Chem 54:17–23
Nguyen TV, Center JR, Eisman JA (2008) Pharmacogenetics of osteoporosis and the prospect of individualized prognosis and individualized therapy. Curr Opin Endocrinol Diabetes Obes 15:481–488
Lasky-Su J, Lyon HN, Emilsson V, Heid IM, Molony C, Raby BA, Lazarus R, Klanderman B, Soto-Quiros ME, Avila L, Silverman EK, Thorleifsson G, Thorsteinsdottir U, Kronenberg F, Vollmert C, Illig T, Fox CS, Levy D, Laird N, Ding X, McQueen MB, Butler J, Ardlie K, Papoutsakis C, Dedoussis G, O’Donnell CJ, Wichmann HE, Celedon JC, Schadt E, Hirschhorn J, Weiss ST, Stefansson K, Lange C (2008) On the replication of genetic associations: timing can be everything!. Am J Hum Genet 82:849–858
Ralston SH, Uitterlinden AG, Brandi ML, Balcells S, Langdahl BL, Lips P, Lorenc R, Obermayer-Pietsch B, Scollen S, Bustamante M, Husted LB, Carey AH, Diez-Perez A, Dunning AM, Falchetti A, Karczmarewicz E, Kruk M, van Leeuwen JP, van Meurs JB, Mangion J, McGuigan FE, Mellibovsky L, del Monte F, Pols HA, Reeve J, Reid DM, Renner W, Rivadeneira F, van Schoor NM, Sherlock RE, Ioannidis JP (2006) Large-scale evidence for the effect of the COLIA1 Sp1 polymorphism on osteoporosis outcomes: the GENOMOS study. PLoS Med 3:e90
Cummings SR (2006) A 55-year-old woman with osteopenia. JAMA 296:2601–2610
Sambrook PN, Eisman JA (2000) Osteoporosis prevention and treatment. Med J Aust 172:226–229
Nguyen ND, Pongchaiyakul C, Center JR, Eisman JA, Nguyen TV (2005) Identification of high-risk individuals for hip fracture: a 14-year prospective study. J Bone Miner Res 20:1921–1928
Dargent-Molina P, Douchin MN, Cormier C, Meunier PJ, Breart G (2002) Use of clinical risk factors in elderly women with low bone mineral density to identify women at higher risk of hip fracture: the EPIDOS prospective study. Osteoporos Int 13:593–599
Cranney A, Guyatt G, Griffith L, Wells G, Tugwell P, Rosen C (2002) Meta-analyses of therapies for postmenopausal osteoporosis IX: summary of meta-analyses of therapies for postmenopausal osteoporosis. Endocr Rev 23:570–578
Nguyen ND, Eisman JA, Nguyen TV (2006) Anti-hip fracture efficacy of bisphosphonates: a bayesian analysis of clinical trials. J Bone Miner Res 21:340–349
Vestergaard P, Jorgensen NR, Mosekilde L, Schwarz P (2007) Effects of parathyroid hormone alone or in combination with antiresorptive therapy on bone mineral density and fracture risk—a meta-analysis. Osteoporos Int 18:45–57
Nguyen TV (2007) Individualization of osteoporosis risk. Osteoporos Int 18:1153–1156
National Osteoporosis Foundation (2008) Clinician’s guide to prevention and treatment of osteoporosis. National Osteoporosis Foundation, Washington DC
Acknowledgements
This work was supported by the National Health and Medical Research Council of Australia. We appreciate the expert assistance of Janet Watters and Donna Reeves in interviewing, data collection, and measurement of BMD. We also appreciate the invaluable help of the Dubbo community. We thank Mr. J. McBride and the IT group of the Garvan Institute of Medical Research for the management and maintenance of the database. We also thank Chehani Alles for her assistance in the genotyping. J. A. E.’s research, including the Dubbo Osteoporosis Epidemiology Study, has been supported by and/or he has provided consultation to Amgen, deCode, Eli Lilly, GE Lunar, Merck Sharp and Dohme, Novartis, Roche-GSK, Sanofi-Aventis, Servier, and Wyeth Australia. J. R. C. has been supported by and/or given educational talks for Eli Lilly, Merck Sharp and Dohme, and Sanofi-Aventis. T. V. N. is supported by a senior research fellowship from the Australian National Health and Medical Research Council. N. D. N. is supported by a grant from the AMBeR (Australian Medical Bioinformatics Resource).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tran, B.N.H., Nguyen, N.D., Center, J.R. et al. Enhancement of Absolute Fracture Risk Prognosis with Genetic Marker: The Collagen I Alpha 1 Gene. Calcif Tissue Int 85, 379–388 (2009). https://doi.org/10.1007/s00223-009-9296-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-009-9296-9