Abstract
Hyperhomocysteinemia (HHCY) has been shown to disturb bone metabolism and to increase the incidence of osteoporosis and osteoporotic fractures. However, there is a complete lack of information on whether these metabolic alterations affect bone repair. The aim of this study was to analyze the impact of HHCY on fracture healing. One group of mice was fed a homocystine-supplemented diet (n = 12), whereas another group received the accordant standard diet for control (n = 13). Four weeks after the stable fixation of a closed femoral fracture, animals were killed to prepare bones for histomorphometric and biomechanical analyses. In addition, blood samples were obtained to evaluate serum concentration of homocysteine (HCY). Quantitative analysis of blood samples revealed severe HHCY as indicated by significantly increased serum concentrations of HCY in animals fed the homocystine-supplemented diet (102.2 ± 64.5 μmol/l) compared to controls (2.8 ± 1.5 μmol/l). Biomechanical evaluation of bone repair revealed significantly decreased bending stiffness of the femora of homocystine-fed animals (45.5 ± 18.2 N/mm) compared with controls (64.6 ± 15.8 N/mm). Histomorphometric analysis demonstrated a slightly smaller callus diameter in HHCY animals but no significant differences in the tissue composition of the callus. In conclusion, the homocystine-supplemented diet leads to severe HHCY, which is associated with an impaired biomechanical quality of the healing bone.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In Western civilization hyperhomocysteinemia (HHCY) represents a widespread metabolic condition, which has been shown to be a risk factor for cardiovascular disease and osteoporosis [1, 2]. The main causes of HHCY in mostly elderly people are deficiencies of vitamin B6, vitamin B12, and folate, as well as renal dysfunction [2–5].
During recent years, several studies have reported an increased incidence of osteoporosis and osteoporotic fractures in patients with HHCY [6, 7]. In vivo studies on rats showed adverse effects of HHCY on bone metabolism [8–10]. In vitro studies have indicated that homocysteine (HCY) is capable of stimulating the proliferation of osteoclasts and the apoptosis of preosteoblastic cells [11, 12]. This seems to result in a negative bone turnover, as shown by clinical trials analyzing serological markers of bone metabolism [13].
While HHCY has been indicated as a new risk factor for osteoporosis and osteoporotic fractures, there is no information on whether these metabolic alterations also affect fracture healing. During secondary fracture healing, intramembranous bone formation by osteoblasts occurs in the early healing phase, whereas in the intermediate phase mainly endochondral bone formation can be seen. In this phase calcified cartilage is resorbed by osteoclasts and the resorption lacunae are filled by the activity of the osteoblasts. In the late, remodeling phase of fracture healing the osteoclasts reduce the callus volume by bone resorption [14].
An unphysiological proliferation of preosteoblastic cells and osteoclasts under an elevated HCY serum concentration might affect, therefore, the bone healing process. Accordingly, our hypothesis was that HHCY induced by a homocystine-supplemented diet is associated with impaired fracture repair.
Methods
Experimental Design
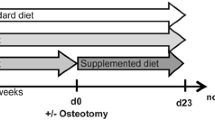
For the present study CD-1 mice (30–40 g body weight, n = 12) were fed a homocystine-supplemented diet (C1000 + 1.5% homocystine; Altromin, Lage, Germany). Based on data of a previous study on rats [10], we started a homocystine-supplemented diet 3 weeks prior to fracture. Controls were fed the accordant standard diet (1324, Altromin; n = 13). Based on a fracture healing study in osteopenic mice [15], animals were killed 4 weeks after fracture to prepare bones for radiological, histomorphometric, and biomechanical analyses. In addition, blood samples were obtained to evaluate serum concentration of HCY.
Surgical Procedure
All experiments were performed according to the National Institutes of Health guidelines for the use of experimental animals and were approved by the German legislation on the protection of animals. Mice were anesthetized by an i.p. injection of xylazine (25 mg/kg) and ketamine (75 mg/kg). The right femur of each animal was fractured by a three-point bending device [16] and stabilized by an intramedullary screw (0.5 mm diameter, 18 mm length), which provides a standardized bending flexibility with axially and rotationally stable fracture fixation by interfragmentary compression [17] (Fig. 1). This closed fracture model is associated with only minor trauma of the periosteum and the surrounding soft tissue. Fracture configuration, i.e., a closed midshaft fracture type A2–A3 according to the AO classification [18], and implant position were documented by X-rays (Fig. 1) (Inside IP-21 high-resolution dental film; Kodak, Rochester, NY) after surgery and prior to death.
Serum Analysis of HCY Concentration
Prior to death, blood samples were obtained by vena cava puncture. After 30 minutes of coagulation, serum was separated from the cellular compartment by centrifugation. Serum samples were stored at −80°C until batched analysis. Serum concentration of HCY was measured by means of gas chromatography mass spectrometry as described previously [19]. Intra- and interassay coefficients of variation were 3.2% and 6.7%, respectively.
Biomechanical Testing
After removal of the intramedullary screws, the mouse femora were embedded at the distal end in aluminum tubes of 10 mm diameter using polymethylmethacrylate (Technovit 3040; Kulzer, Wehrheim, Germany). The tubes were fixed in a three-point testing device (Fig. 2), which allowed rotation of the fixed bone in the anterior–posterior direction. The proximal end of the femur was placed on a support at a distance of 9.25 mm to the distal end (Fig. 2). A materials testing machine (Zwick Z10; Zwick, Ulm, Germany) generated a dorsal deflection in the center of the femur (at the level of the fracture) with a constant velocity of 1 mm/minute and a maximum force of 10 N. Load and deflection were monitored continuously as a load–deflection curve. The stiffness of the healed bones was determined from the slope within the linear part of the curve.
Histology
For histological examinations, the undecalcified bones were fixed in 4% formalin, dehydrated with ethanol, and embedded in polymethylmethacrylate (VLC 7200, Kulzer, Wehrheim, Germany). Then, in the sagittal plane 70-μm slices were cut, ground, and surface-stained with paragon (toluidine blue and basic fuchsin). The longitudinal histological sections were examined with light microscopy (Axiophot; Zeiss, Oberkochen, Germany) using a digital caliper (Digit-Cal 15P 118704; Tesa, Renens, Switzerland) at 200-fold magnification. Two regions of interest were defined, one in the ventral part and one in the dorsal part of the periosteal callus formation (Fig. 3). Up to 12 squared regions of interest (0.625 × 0.625 mm2 each) were defined (up to six at the ventral side and six at the dorsal side of the femur, Fig. 3) and used for quantitative histomorphology (Fig. 3). Each of the squared regions was analyzed using a grid ocular with 10 vertical and 10 horizontal lines. The tissue visible underneath the 100 points created by the grid was analyzed and counted [20]. The tissue was defined as bone, fibrocartilage, or connective tissue (including bone marrow).
Statistics
All data are given as means ± standard deviation (SD). U-tests (Mann–Whitney) were performed using the SAS software package (JMP; SAS Institute, Cary, NC). A Bonferroni adaptation for multiple testing was performed. P < 0.05 was considered to indicate significant differences.
Results
Radiological Analysis
X-rays revealed no major implant or fracture dislocation over the 4-week observation period either in bones of HHCY animals or in bones of normohomocysteinemic controls. X-rays demonstrated in all animals an osseous bridging of the fracture gap after 4 weeks of bone repair.
Serum Analysis of HCY Concentration
Animals fed the homocystine-supplemented diet showed a significantly (P = 0.0006) increased serum concentration of HCY compared to controls (102.2 ± 64.5 vs. 2.8 ± 1.5 μmol/l). HHCY mice showed the same mobility and vitality as normohomocysteinemic controls. In accordance, we did not observe significant differences in the body weight of the animals. One to 3 days after surgery, all animals of both groups showed unrestricted physical activity without limping.
Biomechanical Analysis
Four weeks after fracture, bending stiffness of the callus was significantly (P = 0.03) decreased in animals fed the homocystine-supplemented diet compared to those which received the control diet (45.5 ± 18.2 vs. 64.6 ± 15.8 N/mm).
Histomorphometric Analysis
Three femora in the control group and three femora in the HHCY group could not be used for histomorphological analyses because the section was out of plane of the intramedullary canal. All samples demonstrated a typical pattern of secondary fracture healing with osseous bridging of the fracture gap after 4 weeks of fracture healing. The callus was dominated by woven bone undergoing remodeling. The femora of the homocystine-fed animals showed a slightly smaller callus diameter and a minor fraction of bone in the callus area compared with the control group; however, these differences did not prove statistically different (Table 1). Fibrous cartilage could be found in none of the 10 control mice but in two of the nine homocystine-fed mice (Table 1). This indicates that in these two animals the bone healing and remodeling process was delayed in comparison to the mice which did not show any remaining cartilage.
Discussion
The results of the present study confirmed our hypothesis that a homocystine-supplemented diet is associated with impaired fracture repair.
The results of the serum analysis provide evidence for the functionality of the diet used to induce HHCY. Animals fed the homocystine-supplemented diet developed severe HHCY [5], with a nearly 40-fold increase of HCY serum concentration (102.2 ± 64.5 μmol/l) compared to that of controls (2.8 ± 1.5 μmol/l). So far, only a few studies have analyzed the effect of HHCY on bone metabolism using animal models. By treating rats with methionine, Ozdem et al. [8] induced a HCY serum concentration of 16 μmol/l, which represents moderate HHCY [5]. Herrmann and coworkers [9] also generated moderate HHCY (27 ± 8.8 μmol/l) in rats by a methionine-supplemented diet; however, they additionally induced intermediate HHCY (54.0 ± 46.0 μmol/l) by the application of a homocystine-supplemented diet. Results of this study demonstrated a reduced histomorphometric bone area and decreased biomechanical strength of femora of rats with HHCY compared to those of control animals. This study further indicated a correlation between the impact of HHCY on bone and the serum concentration of HCY. In accordance, the induction of moderate HHCY caused only a minor alteration of bone microarchitecture and strength, while intermediate HHCY critically impaired bone microarchitecture and strength [9]. An additional animal study has shown that reduced bone quality in rats with HHCY is associated with an accumulation of HCY in bone tissue [10].
The present study shows that severe HHCY leads to a significant alteration of bone repair as indicated by the reduced bending stiffness (–30%) of the healed bones in HHCY mice. The difference can be explained by the smaller callus diameter at the fracture site. The bending rigidity (R = E · I) is dependent on the second moment of inertia (I = [D4 − d4] · π/64) and the material properties (modulus of elasticity, E). Taking into consideration the external diameter of the callus (D) and the inner diameter of the intramedullary canal (d) as well as the bone content in the callus (bone in Table 1), we can estimate a second moment of inertia of 0.25 mm4 for the HHCY group and one of 0.48 mm4 for the control group. These calculations are based on the average values of the two groups and show a difference of 47%. The reason for an even higher difference in I than in bending stiffness might be the inhomogeneously distributed bone within the callus. Bone at a large distance to the symmetry axis of the femur has a significantly higher effect on the second moment of inertia than bone, which is closer to it. There might also be an effect on the tissue quality (E) of the callus; however, this cannot be evaluated by the present results.
Bone healing after 4 weeks under stable fixation showed for both groups a solid bony bridging of the fracture with a relatively small callus. The tissue composition of the callus revealed no significant differences between the two groups (Table 1). The result that two mice of the HHCY group still showed cartilage in the fracture healing area indicates that the process of remodeling was somewhat delayed in this group. The calluses of the control group showed a larger diameter at the level of the fracture but a smaller area than the calluses of the HHCY mice. For the bending stiffness of the healing bone, however, the diameter of the calcified callus at the level of the fracture and not the callus area is the important factor.
Recent in vitro and in vivo studies demonstrated that an elevated HCY concentration induces a shift of bone metabolism toward bone resorption [8, 9, 11]. In addition, several cross-sectional studies have shown a significant correlation between an elevated HCY concentration and increased bone resorption markers [13, 21]. These findings were confirmed by in vitro studies, indicating an HCY-dependent increase in the activity of osteoclasts [11, 22]. On the other hand, the effect of HHCY on bone metabolism is still a topic of controversy because other studies rebut a correlation between an elevated HCY serum concentration and an increased risk of osteoporotic fractures [23].
HHCY is further thought to affect the activity of preosteoblastic cells and osteoblasts, which represent key cell types during fracture healing [1, 12]. However, the data on this issue are also conflicting. In vitro studies revealed a moderate stimulation of osteoblasts by the addition of low concentrations of HCY, while toxic effects on osteoblasts have been reported by the addition of high concentrations of HCY [1].
Taken together, the present study demonstrates for the first time that a homocystine-supplemented diet leads to severe HHCY, which disturbs bone repair in mice. Further studies, however, are necessary to analyze whether altered proliferation and activity of osteoclasts and osteoblasts are responsible for these outcomes and how important these findings are for patients with HHCY undergoing fracture treatment.
References
Herrmann M, Peter Schmidt J, Umanskaya N, Wagner A, Taban-Shomal O, Widmann T, Colaianni G, Wildemann B, Herrmann W (2007) The role of hyperhomocysteinemia as well as folate, vitamin B6 and B12 deficiencies in osteoporosis: a systematic review. Clin Chem Lab Med 45:1621–1632
Herrmann W (2001) The importance of hyperhomocysteinemia as a risk factor for diseases: an overview. Clin Chem Lab Med 39:666–674
Clarke R, Refsum H, Birks J, Evans JG, Johnston C, Sherliker P, Ueland PM, Schneede J, McPartlin J, Nexo E, Scott JM (2003) Screening for vitamin B12 and folate deficiency in older persons. Am J Clin Nutr 77:1241–1247
Refsum H, Smith AD, Ueland PM, Nexo E, Clarke R, McPartlin J, Johnston C, Engbaek F, Schneede J, McPartlin C, Scott JM (2004) Facts and recommendations about total homocysteine determinations: an expert opinion. Clin Chem 50:3–32
Stanger O, Herrmann W, Pietrzik K, Fowler B, Geisel J, Dierkes J, Weger M (2003) DACH-LIGA Homocystein (German, Austrian and Swiss Homocysteine Society). Consensus paper on the rational clinical use of homocysteine, folic acid and B-vitamins in cardiovascular and thrombotic diseases: guidelines and recommendations. Clin Chem Lab Med 41:1392–1403
McLean RR, Jacques PF, Selhub J, Tucker KL, Samelson EJ, Broe KE, Hannan MT, Cupples LA, Kiel DP (2004) Homocysteine as a predictive factor for hip fracture in older persons. N Engl J Med 350:2042–2049
van Meurs JB, Dhonukshe-Rutten RA, Pluijm SM, van der Klift M, de Jonge R, Lindemans J, de Groot LC, Hofman A, Witteman JC, van Leeuwen JP, Breteler MM, Lips P, Pols HA, Uitterlinden AG (2004) Homocysteine levels and the risk of osteoporotic fracture. N Engl J Med 350:2033–2041
Ozdem S, Samanci S, Tasatargil A, Yildiz A, Sadan G, Donmez L, Herrmann M (2007) Experimental hyperhomocysteinemia disturbs bone metabolism in rats. Scand J Clin Lab Invest 67:748–756
Herrmann M, Wildemann B, Claes L, Klohs S, Ohnmacht M, Taban-Shomal O, Hubner U, Pexa A, Umanskaya N, Herrmann W (2007) Experimental hyperhomocysteinemia reduces bone quality in rats. Clin Chem 53:1455–1461
Herrmann M, Tami A, Wildemann B, Wolny M, Wagner A, Schorr H, Taban-Shomal O, Umanskaya N, Ross S, Garcia P, Hübner U, Herrmann W (2009) Hyperhomocysteinemia induces a tissue specific accumulation of homocysteine in bone by collagen binding and adversely affects bone. Bone 44:467–475
Koh JM, Lee YS, Kim YS, Kim DJ, Kim HH, Park JY, Lee KU, Kim GS (2006) Homocysteine enhances bone resorption by stimulation of osteoclast formation and activity through increased intracellular ROS generation. J Bone Miner Res 21:1003–1011
Sakamoto W, Isomura H, Fujie K, Deyama Y, Kato A, Nishihira J, Izumi H (2005) Homocysteine attenuates the expression of osteocalcin but enhances osteopontin in MC3T3-E1 preosteoblastic cells. Biochim Biophys Acta 1740:12–16
Dhonukshe-Rutten RA, Pluijm SM, de Groot LC, Lips P, Smit JH, van Staveren WA (2005) Homocysteine and vitamin B12 status relate to bone turnover markers, broadband ultrasound attenuation, and fractures in healthy elderly people. J Bone Miner Res 20:921–929
Gerstenfeld LC, Cullinane DM, Barnes GL, Graves DT, Einhorn TA (2003) Fracture healing as a post-natal developmental process: molecular, spatial, and temporal aspects of its regulation. J Cell Biochem 88:873–884
Li M, Healy DR, Li Y, Simmons HA, Crawford DT, Ke HZ, Pan LC, Brown TA, Thompson DD (2005) Osteopenia and impaired fracture healing in aged EP4 receptor knockout mice. Bone 37:46–54
Bonnarens F, Einhorn TA (1984) Production of a standard closed fracture in laboratory animal bone. J Orthop Res 2:97–101
Holstein JH, Matthys R, Histing T, Becker SC, Fiedler M, Garcia P, Meier C, Pohlemann T, Menger MD (2009) Development of a stable closed femoral fracture model in mice. J Surg Res 153:71–75
Müller M, Nazarian S, Koch P, Schatzker J (1990) The comprehensive classification of fractures of long bones. Springer Verlag, New York
Obeid R, Kuhlmann MK, Kohler H, Herrmann W (2005) Response of homocysteine, cystathionine, and methylmalonic acid to vitamin treatment in dialysis patients. Clin Chem 51:196–201
Claes L, Ruter A, Mayr E (2005) Low-intensity ultrasound enhances maturation of callus after segmental transport. Clin Orthop Relat Res 430:189–194
Gerdhem P, Ivaska KK, Isaksson A, Pettersson K, Vaananen HK, Obrant KJ, Akesson K (2007) Associations between homocysteine, bone turnover, BMD, mortality, and fracture risk in elderly women. J Bone Miner Res 22:127–134
Herrmann M, Widmann T, Colaianni G, Colucci S, Zallone A, Herrmann W (2005) Increased osteoclast activity in the presence of increased homocysteine concentrations. Clin Chem 51:2348–2353
Perier MA, Gineyts E, Munoz F, Sornay-Rendu E, Delmas PD (2007) Homocysteine and fracture risk in postmenopausal women: the OFELY study. Osteoporos Int 18:1329–1336
Acknowledgement
This work was supported by the research program of the Medical Faculty of the University of Saarland (1000/T201000138 HOMFOR 06/84).
Author information
Authors and Affiliations
Corresponding author
Additional information
J. Schmalenbach and M. Herrmann contributed equally to this work.
Rights and permissions
About this article
Cite this article
Claes, L., Schmalenbach, J., Herrmann, M. et al. Hyperhomocysteinemia Is Associated with Impaired Fracture Healing in Mice. Calcif Tissue Int 85, 17–21 (2009). https://doi.org/10.1007/s00223-009-9262-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-009-9262-6