Abstract
We studied the effect of growth hormone (GH) replacement on bone mineral density (BMD) and some parameters of bone metabolism, including undercarboxylated osteocalcin (ucOC), an independent predictive marker of fracture risk, which has not been previously determined or compared during GH treatment. Measurements were performed at baseline and after 6, 12, 18 and 24 months of the initiation of the GH therapy in 21 adult patients with GH deficiency. Significant increases were observed in BMD after 1 year at the lumbar spine and after 1.5 years at the femoral neck. Serum total OC and carboxylated (c) OC increased and reached the maximum at 6 months, but the values remained over the baseline at both 12 and 18 months. The ucOC:total OC ratio changed contrarily: it decreased at 6 months, then increased again and reached the baseline level during the next 18 months. Serum calcium (Ca), phosphate (P) and total alkaline phosphatase (ALP) levels increased after 6 months, thereafter the Ca and P values decreased, while the total ALP remained elevated until 12 months. Serum parathormone decreased at 12 months and increased again thereafter. GH replacement therapy is associated with improvement of ucOC, a marker of fracture risk, which in addition to the increase of BMD, might contribute to the beneficial effect of GH replacement therapy on bone metabolism.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
It has previously been shown that adult patients with severe growth hormone deficiency (GHD) have reduced bone mineral density (BMD) and most of them develop osteopenia, or even osteoporosis [1, 2, 3, 4]. BMD correlates with the risk of fractures [5]. GH replacement therapy may decrease this risk [6, 7, 8], increase BMD after 12 months of treatment [9, 10, 11], and also increase the rate of bone turnover in adults [12, 13, 14, 15]. Both the biochemical markers of bone resorption (urinary hydroxyproline, pyridinoline, deoxypiridinoline, serum type I carboxyterminal cross-linked telopeptide [CTX-I] and bone formation (total alkaline phosphatase [ALP], total osteocalcin [OC], carboxyterminal propeptides of type I collagen) have been shown to increase during GH replacement [16, 17, 18, 19]. GH has a biphasic effect on bone remodelling: the initial increase of the resorption is followed by the increase of formation [20, 21, 22]. In addition to BMD, bone quality also seems to be dependent on other factors. One of the markers of bone formation, OC has a vitamin K-dependent gamma-carboxylation [23]. The importance of carboxylation of OC in the bone is not exactly known [24], but it may be related to bone quality [25, 26]. High serum concentration of undercarboxylated OC (ucOC) has been reportedly associated with increased risk of hip fracture and low BMD [27, 28, 29]. Thus, ucOC appears to be an independent predictor of hip fracture [23]. It has been concluded that combined measurement of the serum ucOC and BMD offers a more exact prediction of the fracture risk [30]. The risk of fracture is associated with low BMD, high serum ucOC concentration, i.e., with low carboxylated OC (cOC)/total OC ratio [24].
To explore our hypothesis that GH replacement may affect the carboxylation of OC, we studied the effects of 24 months of GH treatment in hypopituitary adults with GHD on BMD, serum total OC, cOC and ucOC levels.
Experimental Subjects
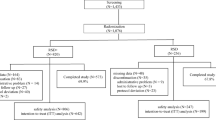
Twenty-one consecutive adult GHD patients (11 female, 10 male; ages 22–67, median 43 years) were analyzed in the present open, prospective study. Only one of the 11 female patients was postmenopausal and received sex hormone substitution. Severe GHD with one or more additional pituitary hormone deficits was determined by a peak serum GH response to insulin tolerance test (0.1–0.15 IU/kg insulin, blood glucose <2.2 mmol/l) of less than 3 µg/L, and in cases of isolated GHD, the arginine test (30 g/30 min iv) was performed as well. Multiple pituitary hormone deficiencies (n = l8) were adequately substituted for at least 4 months before starting the study (thyroxine 11, cortisone acetate 6, sexual steroids 18, desmopressin 7 patients). Eighteen patients had adult-onset (AO) and 3 had childhood-onset (CO) GHD. The GH replacement therapy was initiated after transsphenoidal surgery of pituitary adenoma (clinically non-functioning 11, prolactinoma 2 patients), or craniopharyngeoma (7 patients), and in one patient the GHD was idiopathic. The diagnosis of GHD was confirmed 1–16 years (mean 6.5) prior to the start of the GH substitution. GH (Genotropin, Pharmacia, Corp. Stockholm, Sweden in 9 patients; Humatrope, Lilly GmbH, Bad Hamburg, Germany in 10 patients; Norditropin, Novo Nordisk A/S Bagsvaerd, Denmark in 2 patients) was administered as daily subcutaneous self-injections. The average dose of GH was 1.2 IU/day (0.4 mg/day), maintaining the insulin-like growth factor-I (IGF-I) levels between the median and upper end of the age and gender-related reference range during therapy.
Materials and Methods
The parameters were measured at baseline, as well as 6, 12, 18 and 24 months after initiation of GH replacement therapy. BMD was measured by dual-energy X-ray absorptiometry at the lumbar spine (L2-L4), left femoral neck, and the distal third of the nondominant radius using a Hologic QDR 4500C instrument (Hologic, Waltham, MA, USA). For analysis, software version 9.03D was used. Lumbar spine and radial BMD Z-scores and T-scores were calculated according to the Hologic-supplied reference curves. NHANES III normative data were used as a reference database for femoral bone density measurements. Quality control was maintained by daily scanning of an anthropometric spine phantom. The coefficient of variation of BMD measurements on the spine phantom over a period of 4 years in our laboratory was 0.35%.
Serum parameters were determined by specific immunoassay kits for IGF-I (Nichols, RIA; normal range in females 84–398, in males 104–450 µg/L; sensitivity 20 µg/l; intraassay coefficient of variation [CV] 2.9; interassay CV 9.8%), for total OC (Roche Elecsys System; electrochemiluminescence immunoassay [ECLIA] normal range in premenopause 12–41, in postmenopause 20–48, in males 11–46 µg/L; sensitivity 0.5 µg/L; intraassay CV 4.0, interassay CV 6.5%), for CTX-I (Roche Elecsys System; ECLIA, normal range in premenopause 0.16–0.44, in postmenopause: 0.33–0.78, in males 0.16–0.44, sensitivity 0.01 µg/L, intraassay CV 1.8, interassay CV 4.3%), for parathormone (Bio-Rad, IRMA; normal range 1.0–6.5 pmol/L; sensitivity 0.4 pmol/L; intraassay CV 5.6, interassay CV 9.3%), and by usual commercial kits for serum and urine calcium (Ca), serum and urine phosphate (P), total alkaline phosphatase (ALP). The ucOC was determined after hydroxyapatite extraction of total OC (Sigma-C5267; RIA, calcium-phosphatite trifibric, intraassay CV 2.1%, interassay CV 4.3%) [31]. The cOC was calculated as the difference of total OC and ucOC. Blood samplings were performed in the morning between 0800 and 0900 after an overnight fasting, and the first samples were drawn in the same season of the year. The 24-hour urinary P and Ca excretions were determined on normal diet. Plasma samples were stored at −20°C for less than 3 months until used for the assay.
Serum IGF-I concentration was expressed as the means of IGF-I standard deviation (SD) scores, which corresponded to the number of SD differences from the age- and sex-related normal mean values. IGF-I SD score was calculated as Z-score in relation to age-specific values [32]:

The reference population included randomly selected 2500 healthy Swedes. Treatment effects were analyzed using ANOVA with repeated measures, and in cases of significance, Tukey test was applied. P values less than 0.05 were considered significant. Correlations were calculated according to Pearson. Results were expressed as mean ± S.E.
Results
Serum total OC and cOC showed an increase at 6 months, followed by a moderate decrease, but the values remained elevated above baseline until 18 months (Fig. 1). On the other hand, the cOC:ucOC ratio and cOC:total OC ratio showed a significant increase, while the ucOC:total OC ratio showed a significant decrease after 6 months of GH replacement therapy (Table 1). The measured resorption marker CTX-I levels did not change significantly during the study. Serum Ca and P values rose at 6 months, serum total ALP at 6 and 12 months, and a transient decrease of PTH value was observed at 12 months (Table 1).
During GH therapy the serum IGF-I SD score increased significantly from abnormally low pretreatment values to the normal target range (Table 1). At the start of the therapy 9 patients had osteoporosis, 9 had osteopenia, and 3 had normal BMD - based on WHO criteria (T score <−2.5, between −2.5 and −1.0 or >−1.0, the lowest T-score of the measured regions is considered). At the end of the study only 3 subjects were osteoporotic, 12 osteopenic and the T score values of 6 patients were within the normal range.
The GH replacement therapy increased BMD at the lumbar and femoral regions (Fig. 2) and Z-score at the lumbar spine was (12 months −0.8 ± 0.27, P < 0.001; 18 months; −0.51 ± 0.25, P < 0.05; 24 months 0.44 ± 0.26 vs −1.21 ± 0.29, P < 0.001), and at the femoral neck (18 months 0.23 ± 0.22, P < 0.01; 24 months 0.30 ± 0.19 vs −0.19 ± 0.26, P < 0.01). The T-score at the lumbar spine was (12 months −1.04 ± 0.24, 18 months −0.98 ± 0.23, 24 months −0.81 ± 0.26 vs −1.56 ± 0.26, P < 0.01), and at the femoral neck increased (18 months −0.30 ± 0.22, 24 months −0.20 ± 0.19 vs −0.73 ± 0.24, P < 0.01). The radius values remained unchanged (6 months −1.45 ± 0.33, 12 months −1.35 ± 0.31, 18 months −1.18 ± 0.30, 24 months −1.22 ± 0.31 vs −1.43 ± 0.32).
Discussion
The uniform conclusion of more than one decennial experience of human GH therapy in adults with GHD is that untreated adulthood-onset GHD is associated with reduced bone mass assessed by BMD measurements, and that hormone replacement has a beneficial effect on bone metabolism.
The main finding of our study is that GH replacement therapy in patients with GHD resulted in potentially important changes not only in serum total OC but also cOC, ucOC levels and their ratios. Both total OC and cOC increased significantly after 6 months and decreased moderately thereafter, but both remained elevated above baseline until 18 months. Thus, the elevation of serum total OC levels does not simply indicate an improvement of cOC with significant increases between 6 and 18 months during treatment. Accordingly, the cOC:total OC ratio significantly increased at 6 months compared with pretreatment values. As cOC may be related more directly to bone formation than total OC, the changes observed in our study seem to be particularly important for the beneficial effect of GH treatment on bone metabolism. The BMD is probably the most important, but not the only predictor of the osteoporotic fracture. Recently, Wuster et al. [8] demonstrated that patients with GHD have a high risk of fractures. The quality of bone, i.e., the strength of bone, is dependent on several factors such as architecture and microdamage [33, 34]. In this respect it seems especially important that the carboxylation of OC is considered as an independent predictor of bone fragility [24, 26, 28, 29, 30].
OC is the major noncollagen protein in bone and reflects osteoblast number and function. It contains 49 amino acids but it is a product of a larger intracellular precursor molecule. OC is a marker of bone formation and turnover, although its exact role in bone metabolisms remains to be established. Posttranslational modification of OC occurs through gamma carboxylation. Gamma carboxylation is largely responsible for Ca binding properties of OC. The fully carboxylated state of OC is required for normal bone formation. Biochemical mechanisms by which ucOC could be associated with impaired bone metabolism are not known, but it is suggested that ucOC a direct product of osteoblast can be inhibitory on osteoblast function [30, 31]. Vitamin K mediates the gamma-carboxylation of glutamyl residues of several bone proteins, including OC [35]. Vitamin K insufficiency, due to low intake or clinical use of vitamin K antagonists as anticoagulants, has been associated with higher ucOC concentration [35, 36, 37, 38, 39], lower BMD [28] and increased risk of fracture [27, 29, 30].
The concentrations of cOC and ucOC have not been previously determined or compared in patients with GH deficiency before and during treatment. A few earlier studies suggested somewhat higher ucOC concentrations in osteoporotic patients with vertebral or hip fractures than in healthy controls [35, 37]. However, it is not entirely clear whether treatment with drugs other than GH could influence ucOC, cOC, or their ratio in osteoporotic patients.
In conclusion, our results confirm previous data of open studies that low BMD is present in patients with GHD and that this decrease can be inversed by GH therapy. More importantly, our finding of an improvement of ucOC raises the possibility of a previously unrecognized mechanism by which GH replacement exerts its beneficial effects on bone metabolism. It is possible that the combination of ucOC and cOC measurements, and bone mass determination might improve the assessment of bone fragility in GHD patients. The effect of GH treatment on OC carboxylation and bone fracture rate should be investigated in a randomized, double-blind, placebo-controlled study.
References
RC Cuneo F Salomon GA MacGauley PH Sonksen (1992) ArticleTitleThe growth hormone deficiency syndrome in adults. Clin Endocrinol 37 387–397 Occurrence Handle1:STN:280:ByyC3sjkt1Q%3D
C Wuster (1993) ArticleTitleGrowth hormone and bone. Acta Endocrinol 128 S14–S18
T Rosen T Hansson H Granhed J Szucs B-A Bengtsson (1993) ArticleTitleReduced bone mineral content in adult patients with growth hormone deficiency. Acta Endocrinol 129 201–206 Occurrence Handle1:STN:280:ByuD38ngvFI%3D Occurrence Handle8212984
H de Boer GJ Blok A van Lingen GJ Teule P Lips EA van der Veen (1994) ArticleTitleConsequences of childhood-onset growth hormone deficiency for adult bone mass. J Bone Miner Res 9 1319–1326 Occurrence Handle1:STN:280:ByqD28jgtlY%3D Occurrence Handle7976513
LJ Melton EJ Atkinson WM O’Fallon HW Wahner BL Riggs (1993) ArticleTitleLong-term fracture prediction by bone mineral assessed at different skeletal sites. J Bone Miner Res 8 1227–1233 Occurrence Handle8256660
T Rosen L Wilhelmsen K Landin-Wilhelmsen G Lappas B-A Bengtsson (1997) ArticleTitleIncreased fracture frequency in adult patients with hypopituitarism and GH deficiency. Eur J Endocrinol 137 240–245 Occurrence Handle1:CAS:528:DyaK2sXntVyksLs%3D Occurrence Handle9330587
C Wuster (2000) ArticleTitleFracture rates in patients with growth hormone deficiency. Horm Res 54 31–35 Occurrence Handle10.1159/000053295 Occurrence Handle1:CAS:528:DC%2BD3MXhs12rsr8%3D Occurrence Handle11146377
C Wuster R Abs B-A Bengtsson H Bennmarker U Feldt-Rasmussen E Hernberg-Stahl JP Monson B Westberg P Wilton (2001) ArticleTitleThe influence of growth hormone deficiency, growth hormone replacement therapy, and other aspects of hypopituitarism on fracture rate and bone mineral density. J Bone Miner Res 16 398–405 Occurrence Handle1:CAS:528:DC%2BD3MXptlyjtg%3D%3D Occurrence Handle11204440
B-A Bengtsson S Eden L Lonn H Kvist A Stokland G Lindstedt I Bosaeus J Tolli L Sjostrom OG Isaksson (1993) ArticleTitleTreatment of adults with growth hormone (GH) deficiency with recombinant human GH. J Clin Endocrinol Metab 76 309–317 Occurrence Handle1:STN:280:ByyC28zhvFM%3D Occurrence Handle8432773
J Rodriguez-Arnao I James A Jabbar PJ Trainer D Perrett GM Besser RJ Ross (1998) ArticleTitleSerum collagen crosslink as marker of bone turn-over during GH replacement therapy in growth hormone-deficient adults. Clin Endocrinol 48 455–462 Occurrence Handle10.1046/j.1365-2265.1998.00405.x Occurrence Handle1:CAS:528:DyaK1cXjs12ksb0%3D
JM Gomez N Gomez J Fiter J Soler (2000) ArticleTitleEffects of long-term treatment with GH in the bone mineral density of adults with hypopituitarism and GH deficiency and after discontinuation of GH replacement. Horm Metab Res 32 66–70 Occurrence Handle1:CAS:528:DC%2BD3cXisVygs7k%3D Occurrence Handle10741688
A Schlemmer JS Johansen SA Pedersen JO Jorgensen C Hassager C Christiansen (1991) ArticleTitleThe effect of growth hormone (GH) therapy on urinary pyridinoline cross-links in GH-deficient adults. Clin Endocrinol 35 471–476 Occurrence Handle1:STN:280:By2C3MbotFE%3D
A Binnerts GR Swart JH Wilson N Hoogerbrugge HA Pols JC Birkenhager SW Lamberts (1992) ArticleTitleThe effect of growth hormone administration in growth hormone-deficient adults on bone, protein, carbohydrate and lipid homeostasis, as well as on body composition. Clin Endocrinol 37 79–87 Occurrence Handle1:CAS:528:DyaK38Xls1Citb4%3D
TM Bianda Y Glatz R Bouillon ER Froesch C Schmid (1998) ArticleTitleEffects of short-term insulin-like growth factor-I (IGF-I) or growth hormone (GH) treatment on bone metabolism and on production of 1,25-dihydroxycholecalciferol in GH-deficient adults. J Clin Endocrinol Metab 83 81–87
R Fernholm M Bramnert E Hagg A Hilding DJ Baylink S Mohan M Thoren (2000) ArticleTitleGrowth hormone replacement therapy improves body composition and increases bone metabolism in elderly patients with pituitary disease. J Clin Endocrinol Metab 85 4104–4112 Occurrence Handle1:CAS:528:DC%2BD3cXotlWnur4%3D Occurrence Handle11095440
HM Whitehead C Boreham EM Mellrath B Sheridan L Kennedy AB Atkinson DR Hadden (1992) ArticleTitleGrowth hormone treatment of adults with growth hormone deficiency: results of a 13-month placebo-controlled cross-over study. Clin Endocrinol 36 45–52 Occurrence Handle1:STN:280:By2B3MjitFA%3D
J Bollerslev J Moller S Thomas O Djoseland JS Christiansen (1996) ArticleTitleDose-dependent effects of recombinant human growth hormone on biochemical markers of bone and collagen metabolism in adult growth hormone deficiency. Eur J Endocrinol 135 666–671 Occurrence Handle1:CAS:528:DyaK2sXntlCgsg%3D%3D Occurrence Handle9025710
AF Attanasio SW Lamberts AM Matranga MA Birkett PC Bates NK Valk J Hilsted B-A Bengtsson CJ Strasburger (1997) ArticleTitleAdult growth hormone (GH)-deficient patients demonstrate heterogeneity between childhood onset and adult onset before and during human GH treatment. Adult Growth Hormone Deficiency Study Group. J Clin Endocrinol Metab 82 82–88 Occurrence Handle1:CAS:528:DyaK2sXkt1Smsg%3D%3D Occurrence Handle8989238
A Sartorio S Ortolani E Galbiati G Conte V Vangeli M Arosio S Porretti G Faglia (2001) ArticleTitleEffects of 12-month GH treatment on bone metabolism and bone mineral density in adults with adult-onset GH deficiency. J Endocrinol Invest 24 224–230 Occurrence Handle1:CAS:528:DC%2BD3MXks1Klt7w%3D Occurrence Handle11383908
N Bravenboer P Holzmann H de Boer JC Roos EA van der Veen P Lips (1997) ArticleTitleThe effect of growth hormone (GH) on histomorphometric indices of bone structure and bone turnover in GH-deficient men. J Clin Endocrinol Metab 82 1818–1822 Occurrence Handle1:CAS:528:DyaK2sXjs1akt7Y%3D Occurrence Handle9177389
PV Carroli ER Christ B-A Bengtsson L Carlsson JS Christiansen D Clemmons R Hintz K Ho Z Laron P Sizonenko PH Sonksen T Tanaka M Thorner (1998) ArticleTitleGrowth hormone deficiency in adulthood and the effects of growth hormone replacement: a review. J Clin Endocrinol Metab 83 382–392 Occurrence Handle1:CAS:528:DyaK1cXhtVSntbY%3D Occurrence Handle9467546
C Ohlsson B-A Bengtsson OGP Isaksson TT Andreassen MC Slootweg (1998) ArticleTitleGrowth hormone and bone. Endocr Rev 19 55–79 Occurrence Handle1:CAS:528:DyaK1cXhtlagtL8%3D Occurrence Handle9494780
MJ Seibel SP Robins JP Bilezikian (1997) ArticleTitleSerum undercarboxylated osteocalcin and the risk of hip fracture. J Clin Endocrinol Metab 82 717–718 Occurrence Handle1:CAS:528:DyaK2sXhsl2js7s%3D Occurrence Handle9062470
H Luukinen SM Kakonen K Pettersson K Koski P Laippala T Lovgren SL Kivela HK Vaananen (2000) ArticleTitleStrong prediction of fractures among older adults by the ratio of carboxylated to total serum osteocalcin. J Bone Miner Res 15 247–248
G Liu M Peacock (1998) ArticleTitleAge-related changes in serum undercarboxylated osteocalcin and its relationships with bone density, bone quality, and hip fracture. Calcif Tissue Int 62 286–289 Occurrence Handle10.1007/s002239900432 Occurrence Handle1:CAS:528:DyaK1cXhvFygu78%3D Occurrence Handle9504950
T Sugiyama S Kawai (2001) ArticleTitleCarboxylation of osteocalcin may be related to bone quality: a possible mechanism of bone fracture prevention by vitamin K. J Bone Miner Res 19 146–149 Occurrence Handle10.1007/s007740170034 Occurrence Handle1:CAS:528:DC%2BD3MXlslWhu7c%3D
P Szulc MC Chapuy PJ Meunier PD Delmas (1993) ArticleTitleSerum undercarboxylated osteocalcin is a marker of the risk of hip fracture in elderly women. J Clin Invest 91 1769–1774 Occurrence Handle1:CAS:528:DyaK3sXktVKnsbw%3D Occurrence Handle8473517
P Szulc M Arlot MC Chapuy F Duboeuf PJ Meunier PD Delmas (1994) ArticleTitleSerum undercarboxylated osteocalcin correlates with hip bone mineral density in elderly women. J Bone Miner Res 9 1591–1595 Occurrence Handle1:CAS:528:DyaK2MXhslCltLw%3D Occurrence Handle7817805
P Szulc MC Chapuy PJ Meunier PD Delmas (1996) ArticleTitleSerum undercarboxylated osteocalcin is a marker of the risk of hip fracture: a three-year follow-up study. Bone 18 487–488 Occurrence Handle10.1016/8756-3282(96)00037-3 Occurrence Handle1:STN:280:BymA3MbhvFQ%3D Occurrence Handle8739908
B Merle PD Delmas (1990) ArticleTitleNormal carboxylation of circulating osteocalcin (bone Gla-protein) in Paget’s disease of bone. Bone Miner 11 237–245 Occurrence Handle1:STN:280:By6D1MfjslQ%3D Occurrence Handle2176559
P Vergnaud P Garnero PJ Meunier G Breatr K Kamihagi PD Delmas (1997) ArticleTitleUndercarboxylated osteocalcin measured with a specific immunoassay predicts hip fracture in elderly women: the EPIDOS Study. J Clin Endocrinol Metab 82 719–724
B-A Bengtsson R Abs H Bennmarker JP Monson U Feldt-Rasmussen E Hernberg-Stahl B Westberg P Wilton C Wuster (1999) ArticleTitleThe effects of treatment and the individual responsiveness to growth hormone (GH) replacement therapy in 665 GH-deficient adults. J Clin Endocrinol Metab 76 309–317
C Coopper (1993) ArticleTitleThe epidemiology of fragility fractures: Is there a role for bone quality? Calcif Tissue Int 53 S23–S26 Occurrence Handle8275375
CM Schnitzler (1993) ArticleTitleBone quality: a determinant for certain risk factors for bone fragility. Calcif Tissue Int 53 S27–S31 Occurrence Handle8275376
M Takahashi K Naitou T Ohishi K Kushida M Miura (2001) ArticleTitleEffect of vitamin K and/or D on undercarboxylated and intact osteocalcin in osteoporotic patients with vertebral or hip fractures. Clin Endocrinol 54 219–224 Occurrence Handle10.1046/j.1365-2265.2001.01212.x Occurrence Handle1:CAS:528:DC%2BD3MXitlSgs7k%3D
CM Gundberg SD Nieman S Abrams H Rosen (1998) ArticleTitleVitamin K status and bone health: an analysis of methods for determination of undercarboxylated osteocalcin. J Clin Endocrinol Metab 83 3258–3266
NC Binkley DC Krueger JA Engelke AL Foley JW Suttie (2000) ArticleTitleVitamin K supplementation reduces serum concentration of under-γ-carboxylated osteocalcin in healthy young and elderly adults. Am J Clin Nutr 72 1523–1528 Occurrence Handle1:CAS:528:DC%2BD3cXosl2mt7w%3D Occurrence Handle11101481
MH Knapen BS Hellemons-Boode M Langenberg-Ledeboer JA Knottnerus K Hamulyak PA Price C Vermeer (2000) ArticleTitleEffect of oral anticoagulant treatment on markers for calcium and bone metabolism. Haemostasis 30 290–297 Occurrence Handle10.1159/000054146 Occurrence Handle1:CAS:528:DC%2BD3MXktlCksbs%3D Occurrence Handle11356997
A Zittermann (2001) ArticleTitleEffects of vitamin K on calcium and bone metabolism. Curr Opin Clin Nutr Metab Care 4 483–487 Occurrence Handle10.1097/00075197-200111000-00003 Occurrence Handle1:CAS:528:DC%2BD38Xhslersg%3D%3D Occurrence Handle11706280
Acknowledgements
This work was supported by research grants OTKA and ETT (T035216, 022/2003).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hubina, E., Lakatos, P., Kovács, L. et al. Effects of 24 Months of Growth Hormone (GH) Treatment on Serum Carboxylated and Undercarboxylated Osteocalcin Levels in GH-Deficient Adults . Calcif Tissue Int 74, 55–59 (2004). https://doi.org/10.1007/s00223-002-2149-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-002-2149-4