Abstract
Autism spectrum disorder (ASD) is a common neurodevelopmental disorder, whose core symptom domains include impaired social communication and narrowed interests and/or repetitive behaviors; in addition, deficits of general cognition, neuromotor function, and movement ability can be observed. This study was designed to examine differences in neuromotor and cognitive functions for a group of young adults with ASD and age-matched controls. It was also of interest to assess whether changes in the intra-individual variability (IIV) of these selected neuromotor and cognitive tasks also occurred. Increased IIV in persons with ASD may reveal important organizational features of their neuromotor system that differ from neurotypical controls. Twenty neurotypical adult individuals (24.3 ± 2.8 years) and twenty adults with a clinician-assigned diagnosis of ASD (21.2 ± 4.4 years) participated in this study. Specific cognitive and motor assessments included Trails Making Tests A&B, Symbol Digit Modalities Test, Purdue Pegboard Test, simple reaction time, finger tapping, hand grip strength, balance, and gait. Results revealed that the ASD adults exhibited decreased upper limb strength and slower responses for finger tapping, hand dexterity, reaction times, and gait compared to the non-ASD controls. The general slowing of motor responses for the persons with ASD was also associated with increased within-subject variability during the reaction time, finger tapping, hand grip, and gait assessments compared to neurotypical adults, illustrating that IIV measures may be a useful marker of widespread neuromotor dysfunction for adults with ASD. Overall, these findings are consistent with clinical observations that abnormalities of movement performance and cognitive performance are an associated feature of ASD in young adults.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Autism spectrum disorder (ASD) is a common neurodevelopmental disorder which affects 1 in 68 children in the US (Baio 2012). While ASD is characterized by deficits in social communication, narrowed interests, and repetitive patterns of behavior, ASD can also have profound impact on neuromotor function and movement ability. Histopathological and neuroimaging evidences of cerebellar abnormalities and/or atrophy have been described in ASD, which may underlie this linkage between social and motor impairment (Rinehart et al. 2006; Mosconi et al. 2015a, b). In particular, Mosconi et al. (2015a) reported that persons with ASD have 35–95% fewer cerebellar Purkinje cells and that differences in the relative size of the deep cerebellar nuclei can also be found. Given that the prominent role the cerebellum plays in motor control and learning (Koziol et al. 2014), any deficits arising from this neurodevelopmental disorder would have a significant impact on the performance of many everyday movements.
Indeed, persons with ASD exhibit a range of changes in neuromotor function, including altered walking patterns, impairments in postural reactions, slower reaction times, and deficits in fine motor control and strength (Fournier et al. 2010a; Calhoun et al. 2011; Kern et al. 2013; Hocking et al. 2014; Alaniz et al. 2015; Kindregan et al. 2015; Hasan et al. 2017). However, other studies have not found differences in gait (Hallett et al. 1993), balance (Travers et al. 2013), or reaction time (Kofler et al. 2013; Ferraro 2016) for individuals with ASD of varying ages. Disparity in reported findings across studies may arise for a number of reasons. An obvious one is the differences in age range of the persons being assessed (Travers et al. 2013). Given the rapid rate and variability of development of the CNS in children through to adulthood, it is hardly surprising that comparing the responses of persons across a spectrum of ages (and studies) would reveal conflicting results. Indeed, it has been reported that both delays in development and under-development of balance control can be observed in this population across the lifespan (Minshew et al. 2004). Another issue is that the majority of studies exploring motor and cognitive changes in persons with ASD focused on only one or two measures of motor function (e.g., gait or reaction time or strength). Arguably, a greater understanding of the impact of any neural differences would be gained from assessment across a range of neuromotor and cognitive tasks in the same individual.
While the link between the cerebellum and motor function is well established, this structure has also been associated with a diverse array of cognitive, visuospatial, intellectual, language, affective, and social functions (Schmahmann and Sherman 1998). For example, it has been reported that projections from the anterior regions of the cerebellum connect to sensorimotor areas of the cerebrum, while those from the posterior cerebellum project to cognitive regions of the cortex (D’Mello and Stoodley 2015). Furthermore, disruption of cerebro-cerebellar feedback loops may be evident in populations with neurodevelopmental and/or psychiatric conditions underlying problems with motor function, language, cognition, skill acquisition, and/or social abilities in persons with ASD (D’Mello and Stoodley 2015; Mosconi et al. 2015b). Overall, it is apparent that changes in cerebellar function have been linked to both motor and cognitive declines for persons with ASD. Therefore, it is of interest to investigate the motor and cognitive behaviors that may be associated with cerebellar changes in an adult ASD population.
One other feature of behavior and movement responses for persons with ASD has been that they often exhibit greater variability when compared to non-ASD counterparts (Klein et al. 2006; Geurts et al. 2008; Adamo et al. 2014). In particular, increases in movement variability over successive trials within a single person (i.e., intra-individual variability, IIV) have been commonly reported, especially under reaction time conditions (Klein et al. 2006; Adamo et al. 2014). The significance of this pattern of findings is centered on the view that such increases in variability reveal important organizational features of the neuromotor system (Klein et al. 2006; Geurts et al. 2008; Kofler et al. 2013; Adamo et al. 2014). Furthermore, changes in the neuromotor system arising either from the typical process of aging and/or neurological diseases (e.g., Parkinson’s) are commonly reflected by increases in IIV of selected movement indices (Hultsch et al. 2002; Dykiert et al. 2012b; Batterham et al. 2014; Bielak et al. 2014; Bunce et al. 2017; Bauermeister et al. 2017). For persons with ASD, there is speculation that differences in the pattern of IIV for various cognitive and/or motor skills could potentially be used as a (bio)marker of the neural changes with this disorder and may provide a more stable feature of the neuromotor differences underlying ASD (Kofler et al. 2013).
The current study was designed to investigate differences in neuromotor and cognitive function between young adults with ASD and age-matched neurotypical controls and to examine relations between walking, balance, reaction time, and specific quantitative measures of cognitive ability. In addition, it was of interest to assess differences in IIV for selected neuromotor tasks, including upper limb strength, reaction time, finger tapping speed, and walking ability between the two groups. It was predicted that the movement responses of the ASD persons would be slower overall, with declines in gait speed, finger tapping speed, slower reaction times, and decreased responses for the pegboard test compared to the age-matched neurotypical controls. It was also anticipated that, in addition to the slower movement responses, ASD adults would also exhibit lower hand grip strength values compared to controls. Finally, ASD individuals would demonstrate increased within-subject variability for the reaction time, gait, hand grip, and finger tapping tasks, and that measures of motor behavior would be positively correlated with measures of cognitive ability.
Methods
Participants
Twenty neurotypical adult individuals of both sexes (controls, age range 24.3 ± 2.8 years; 8 males) and twenty adults with a clinically assigned and documented diagnosis of ASD (age range 21.2 ± 4.4 years; 14 males) were recruited to participate in this study. The control group consisted of individuals without personal or family histories of major psychiatric or substance abuse disorders. In addition to their clinically documented diagnosis, inclusionary criteria for the ASD group included full-scale IQ > 70 and good expressive language skills. This criterion ensured that all participants were capable of understanding the directions of each task and had the ability to end their participation if they were not motivated to continue with the study. Differences between groups were confirmed by statistically significant scores on the Social Responsiveness Scale-2 [SRS-2; (Constantino et al. 2003)]. The summarized results of this analysis are presented in Table 1.
Experimental design
Participants were assessed for their cognitive and motor functions on 2 non-consecutive days. Assessments on day 1 typically lasted 1.5 h and included the SRS-2, Trails Making Tests A&B (TMT), Symbol Digit Modalities Test, finger tapping speed, and Purdue Pegboard Test. Testing on the second day lasted 1 h, and included hand grip strength, standing balance, simple reaction time, and walking ability. All participants were under direct observation by a member of the research team during both sessions to ensure that they fully understood directions and completed tasks. Details of these tests are as follows.
Social Responsiveness Scale-2 (SRS-2)
The SRS-2 is a commonly used 65-item scale that rates the level of reciprocal social behavior and ASD symptoms for the ASD individual. It generates a total and subscale t scores that denote the degree of social impairment (higher scores indicate more severe impairment). Total t scores below 59 are typically not associated with ASD, scores between 60 and 65 indicate mild ASD, between 66 and 75 can be associated with moderate ASD, and scores above 76 indicate severe ASD. The scale has demonstrated high construct and discriminate validity and high test–retest reliability (Constantino et al. 2003).
Trails Making Tests A&B (TMT)
These tests provide an assessment of each person’s attention, visual search and scanning, sequencing, and cognitive flexibility (Salthouse 2011). In Trails A, participants are asked to rapidly connect 25 numbers in ascending order with paper and pencil, and in Trails B, they must connect alternating numbers and letters in numerical and alphabetical order, dividing their attention between these two cognitive tasks and demonstrating rapid cognitive flexibility.
Symbol Digit Modalities Test (SDMT)
This assessment captures key neurocognitive functions including attention, visual scanning, and motor speed (Sheridan et al. 2006). Participants use a key showing number (1 through 9) and symbol pairs to write numbers that match their corresponding symbols. The score is based upon the number of correct matches obtained in 90 s.
Reaction time
Participants completed a simple reaction time (RT) task where upper limb (index finger) and lower limb (foot) responses were collected. All responses were performed with the individuals preferred limb. After completing five practice trials, each person completed 20 trials with each segment. A visual stimuli was provided for the RT response and participants responded by depressing a timing switch with either their foot or finger. Prior to analysis, RT data were trimmed by eliminating those trials which were 150 ms or less (Bauermeister et al. 2017). A total of seven trials were eliminated by this process and were replaced with the individual’s mean RT for that task. The average (mean) and intra-individual variability (IIV) for the RT measures were calculated. IIV measures were based upon the between-trial standard deviation (SD) RT measures for each individual.
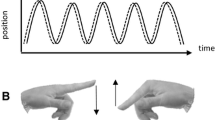
Finger tapping speed
All participants completed a tapping task using their index finger of each limb. Each person performed the task in a seated position with their forearms resting on a table. They were asked to tap on a force sensor as fast as possible. Five trials were performed for each limb. The average (mean) and intra-individual variability (IIV) for the ‘finger tapping speed’ measures were calculated. As with the RT data, IIV measures were based upon the between-trial standard deviation (SD) measures for each individual.
Purdue Pegboard Test
This evaluation was performed using the Purdue Pegboard Test (Model 32020, Lafayette Instrument Co., IL) and assesses fine goal-directed movements by measuring fingertip dexterity, hand–eye coordination, and bimanual coordination (Barbeau et al. 2015). The test measures the ability of persons to put as many pegs as possible into the pegboard in four different conditions: using their preferred (P) hand, non-preferred (N) hand, both (B) hands simultaneously, and an “assembly condition” using alternating hands. The score for the P, N, and B conditions was recorded as the number of pieces placed within 30 s. The “assembly condition” involves using both hands to assemble a peg, washer, collar, and washer as quickly and accurately as possible within 60 s.
Hand grip strength
Grip strength (in kg) for both upper arms was recorded using the JamarH dynamometer (Sammons Preston Rolyan Inc., Bolingbrook, IL). Individuals were seated in an armless chair with shoulders adducted and neutrally rotated, elbow flexed at 90°, forearms in neutral position, and wrist between 0° and 30° of dorsiflexion. Participants were instructed to squeeze the handle as hard as possible. Three trials were performed with the overall average (mean) and intra-individual variability (IIV) for the strength measures calculated. IIV measures of hand grip strength were based upon the between-trial standard deviation (SD) measures for each individual.
Gait
Participants performed ten walking trials over a 25 ft distance. Five trials were performed at their preferred speed (PWS) and five subsequent trials performed as fast as possible. Light gates were positioned at the beginning and end of the walking path to record overall time. Each person’s walking performance was assessed using a 20 ft straight GAITRite pressure sensitive walking surface (CIR Systems, Havertown PA). Gait data were sampled at 150 Hz and processed using the Protokinetics PKMAS software (ProtoKinetics LLC). Average (mean) and IIV measures were calculated for the following spatio-temporal gait variables: step/stride length (cm), step/stride time (s), gait velocity (cm/s), and cadence. All gait-related IIV calculations were based upon the between-trial standard deviation (SD) for each individual.
Balance
Each person’s general balance ability was assessed across four postural conditions, namely: (1) eyes open/firm surface, (2) eyes closed/firm surface, (3) eyes open/foam surface, and (4) eyes closed/foam surface. The foam surface was 15 cm thick and of medium density. Postural motion (quantified by center of pressure (COP) excursion in the anterior–posterior (AP) and medio-lateral (ML) directions) was collected, while individuals stood on a Bertec balance plate (model BP6040). COP data sampled at 100 Hz and filtered using a second-order low-pass Butterworth filter (cut-off frequency 50 Hz). The dependent measures determined for postural sway included: total path length, mean COP velocity, and mean COP excursion in the ML and AP directions. Analyses of the COP data were performed using the Matlab software (Mathworks R14).
Data analysis
Inferential analyses were conducted using a within-subject repeated-measures generalized linear model. In addition, cross-correlation analysis was performed to assess the relation between the cognitive and neuromotor measures (both average and IIV). All statistical analyses were performed using SAS statistical software (v 9.3, SAS Institute Inc., NC), with the risk of Type I error set at p < 0.05.
Results
The following evaluations were performed for each person; cognition (i.e., Trails Making Tests A&B (TMT) and Symbol Digit Modalities Test), simple reaction time, finger tapping speed, hand grip strength, Purdue Pegboard Test, standing balance, and walking ability. The results of the analyses are as follows.
Cognitive assessments
Significant group differences were found for results of the Symbol Digit Modalities Test (F1,38 = 20.96; p < 0.001) with the ASD persons scoring higher than the controls. SDMT captures processing speed, attention, visual scanning, and motor speed. No significant differences were found between the two groups for the Trail Making Tests (A, F1,38 = 1.34; p = 0.25; B, F1,38 = 1.41; p = 0.24) which is a measure of processing speed.
Reaction time
This test assesses the time taken for a person to react to a single visual stimulus. Individuals performed this task with both an upper (i.e., finger) and lower limb (i.e., foot) segment. For the mean RT values, a significant group effect was found for the reaction time scores for the hand (F1,38 = 10.06; p < 0.01) and the foot (F1,38 = 16.98; p < 0.001). For both measures, the control group exhibited significantly faster reaction times. For the IIV RT data, significant group differences were found for hand (F1,38 = 5.64; p < 0.05) and the foot (F1,38 = 9.18; p < 0.01) with the ASD individuals demonstrating greater within-subject variability of responses compared to the control group. Table 2 includes a summary of the results for the reaction time, finger tapping, hand grip, and Purdue Pegboard Test, with significant group effects highlighted.
Finger tapping speed
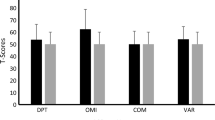
Individuals were instructed to tap on a flat surface, using their index finger, as fast as possible. This task was performed with both the preferred and non-preferred fingers. For the tapping speed, no significant main effect due to either limb (F1,38 = 3.23; p = 0.09) or group (F1,38 = 2.58; p = 0.17) were observed. In addition, no limb by group interaction effect was observed (F1,38 = 0.31; p = 0.77). However, for the intra-individual differences, a significant group effect was observed (F1,38 = 9.80; p < 0.05) with the ASD group exhibiting greater within-subject variability compared to the control group. No limb differences were observed for the IIV results (F1,38 = 0.08; p = 0.77). Figure 1 highlights the group differences for the mean and IIV values for reaction time (both hand and foot) and finger tapping speed.
Bar graphs depicting differences in average and intra-individual variability (IIV) of simple reaction time (for the hand and foot) and finger tapping speed between the ASD young adults and the controls. Error bars represent one SE of the mean. Significant differences between groups are denoted with an asterisk (*)
Purdue Pegboard Test
This test which provides requires finger dexterity, hand–eye coordination, and bimanual coordination. Inferential analysis revealed significant group differences for performance of this test with the preferred hand (F1,38 = 13.36; p < 0.001) and non-preferred hand (F1,38 = 11.53; p < 0.001), when performed with both hands (F1,38 = 15.01; p < 0.001) and for the assembly task (F1,38 = 15.24; p < 0.001). IIV is not reported for this measure as no repeat trials were conducted. As illustrated in Fig. 2, the control individuals scored higher than the ASD adults across all assessments.
Bar graphs depicting differences in the average and IIV of the hand grip strength measures between the ASD young adults and the controls. Group differences in the responses for the Purdue Pegboard Tests are also shown. Error bars represent one SE of the mean. Significant differences between groups are denoted with an asterisk (*)
Hand grip strength
Bilateral assessments of hand grip strength (in kg) were performed for all individuals. A significant group effect was found for the mean hand grip strength (F1,38 = 5.97; p < 0.05) with the control individuals exhibiting greater strength compared to the ASD individuals. A significant limb effect was also found (F1,38 = 29.68; p < 0.001) with hand grip strength being greater for the preferred limb for both groups. For the intra-individual differences, a significant group effect was observed (F1,38 = 4.03; p < 0.05) with the ASD group exhibiting greater within-subject variability for the hand grip strength values compared to the neurotypical controls. No limb by group interaction effect was observed for either the mean (F1,38 = 0.17; p = 0.68) or IIV hand grip measures (F1,38 = 0.06; p = 0.86). Figure 2 illustrates the differences in the average (mean) and IIV for hand grip strength between the two groups.
Gait
For the gait assessment, individuals were performed ten walking trials over a 25 ft distance. Five trials were performed at their preferred speed (PWS) and five subsequent trials performed as fast as possible. For the PWS trials, a significant group effect was found for cadence (F1,38 = 9.09; p < 0.01), gait velocity (F1,38 = 5.59; p < 0.0), step time (F1,38 = 8.34; p < 0.01), and stride time (F1,38 = 9.16; p < 0.01). For this condition, the control individuals walked at a faster preferred speed with increased step and stride times compared to the ASD individuals. For the IIV of the gait measures, significant group differences were found for stride length (F1,38 = 6.43; p < 0.05) and stride time (F1,38 = 9.39; p < 0.01) with the ASD individuals exhibiting greater within-subject variability for these measures compared to the controls.
For the fast-speed gait conditions, a significant group effect was found for gait velocity (F1,38 = 8.33, p < 0.01), step time (F1,38 = 4.85, p < 0.05), and stride time (F1,38 = 4.87; p < 0.05). Overall, the ASD persons walked at a slower speed with decreased step and stride times compared to the controls. For the IIV of the gait measures, significant group differences were found for stride length (F1,38 = 5.41; p < 0.05) and stride time (F1,38 = 4.17; p < 0.05) with the ASD individuals exhibiting greater within-subject variability for these measures compared to the controls. Figure 3 illustrates the differences in the average (mean) and IIV of selected gait metrics between the two groups for the fast walking speed condition. Table 3 includes a summary of the results for the walking tasks, with significant group differences for the various gait metrics being highlighted.
Bar graphs depicting differences in the average and IIV of stride time, step time, and stride length between the ASD young adults and the controls. Results are shown for the fast-speed gait condition only. Error bars represent one SE of the mean. Significant differences between groups are denoted with an asterisk (*)
Balance
Balance ability of the ASD and control individuals was assessed under conditions where vision (i.e., eyes open/eyes closed) and support surface (i.e. firm/foam) were manipulated. For the eyes open/firm support condition, no significant differences between the controls and ASD adults were found for path length (F1,38 = 3.47; p = 0.08), COP velocity (F1,38 = 0.05; p = 0.83), mean AP (F1,38 = 1.35; p = 0.25), and ML sway (F1,38 = 0.03; p = 0.86). For the eyes open/foam support condition, no significant differences between the controls and ASD adults were found for path length (F1,38 = 1.36; p = 0.25), COP velocity (F1,38 = 1.17; p = 0.28), mean AP (F1,38 = 2.46; p = 0.13), and ML sway (F1,38 = 0.06; p = 0.81).
For the eyes closed/firm support condition, no significant differences between the controls and ASD adults were found for path length (F1,38 = 0.04; p = 0.84), COP velocity (F1,38 = 0.41; p = 0.52), mean AP (F1,38 = 0.84; p = 0.36), and ML sway (F1,38 = 1.55; p = 0.22). For the eyes closed/foam support condition, no significant differences between the controls and ASD adults were found for path length (F1,38 = 1.95; p = 0.17), COP velocity (F1,38 = 0.43; p = 0.51), mean AP (F1,38 = 0.14; p = 0.71), and ML sway (F1,38 = 0.63; p = 0.43).
Correlation analysis
To assess the relation between the cognitive and neuromotor measures (both average and IIV), cross-correlation analyses were performed. However, no meaningful significant results for either of the two groups emerged from this analysis.
Discussion
This study was designed to examine differences in motor and cognitive functions between young adults with ASD and age-matched controls. It was also of interest to assess whether IIV of selected measures of neuromotor function was different between the young adults with ASD compared to the age-matched neurotypical controls. The results revealed that the motor function of the ASD young adults was characterized by slower responses, with decreased finger tapping speed and general hand dexterity, slower reaction times, and decreased gait speed. The ASD group also showed decreased upper limb strength. In parallel with the pattern of neuromotor slowing, ASD individuals exhibited increased within-subject variability during the reaction time, finger tapping, strength, and walking tasks.
Cognitive differences and neuromotor slowing in ASD
The results of the current study revealed as a number of differences in neuromotor and cognitive functions between the two groups. For the cognitive tasks, the ASD and control participants had similar performance on the TMT A and B; however, they differed in their performance on the SDMT in that the ASD participants were not able to correctly pair as many items as the control participants. This aligns with the previous research, which reported that adults with ASD exhibit slower processing speed compared to controls of similar age, although this difference was not evident for children (Travers et al. 2014).
The ASD adults also exhibited slower reaction times (for both the upper and lower limbs) compared to the age-matched controls, a result which is consistent with the previous research showing similar differences between ASD children and neurotypical children of similar age (Inui and Suzuki 1998; Karalunas et al. 2014; Barbeau et al. 2015). Indeed, with regard to motor function, the ASD persons showed a general slowing across all metrics, with decreases in finger tapping speed, lower scores on the Purdue Pegboard Test, and decreased gait speed. In addition to slowed motor responses, the young adults with ASD also had decreased upper limb strength. This latter result is of some significance given that reduced hand grip strength has been reported for children with ASD (David et al. 2009; Kern et al. 2013; Wang et al. 2015), but not for adults with ASD. As the majority of the previous ASD studies have tended to focus on motor function differences in children, the current findings have some relevance in showing that neuromotor differences seen in childhood for persons with ASD can persist through to adulthood.
With regards to walking, a number of notable differences were observed between the gait of the controls and the ASD group. Generally speaking, the ASD individuals walked slower (under both self-selected preferred and fast-speed conditions) with decreased step and stride times. These results build upon the general premise that the overall walking patterns of children and young adults with ASD tend to differ from age-matched controls (Calhoun et al. 2011; Weiss et al. 2013). An exception to this pattern was the study conducted by Hallett et al. (1993) who found no differences between ASD adults and age-matched controls when walking at a person’s self-selected pace for these same metrics although methodological differences in how gait data were collected and subject numbers could contribute to the differences. In keeping with the finding of slower gait speed, our results also revealed that the ASD adults exhibited slower finger tapping speed, fine motor (i.e., Purdue Pegboard Test) and simple reaction times (for both the hand and foot). The slower reaction time values are certainly consistent with the previous studies who have reported similar results for children diagnosed with ASD (Geurts et al. 2008; Adamo et al. 2014; Barbeau et al. 2015). However, it should be noted that two recent reviews have challenged this assumption (Kofler et al. 2013; Ferraro 2016).
Similarly, deficits in balance control have been widely reported for children with ASD (Fournier et al. 2010b, 2014; Bhat et al. 2011), although a few comparable assessments of balance control in adults with ASD have been previously reported. Our finding of no difference between ASD adults and age-matched controls highlights the confounding nature that a person age may play given that the neuromotor responses of children and adolescents with ASD often vary from ASD adults (Travers et al. 2013). Another possibility is that the balance tasks assessed were not sufficiently challenging to differentiate between the two adult groups. The assessments used in the current study required the individuals to stand in the preferred bilateral stance, while vision and/or the support surface were manipulated. However, many previous studies of balance control in ASD individuals have only repotted differences under more challenging conditions including unanticipated perturbations (Bhat et al. 2011) and single-leg stance (Travers et al. 2013; Graham et al. 2015). Indeed, while Travers et al. (2013) reported balance differences during single-leg stance conditions, they also found no differences in balance measures between ASD individuals and age-matched neurotypical persons during two legged standing tasks under vision conditions similar to that performed in our study [i.e., eyes open and closed (Travers et al. 2013)]. Consequently, it would appear that any postural differences between neurotypical adults and ASD persons are more likely to emerge under more challenging balance conditions.
The basis for the slowing of movement responses probably reflects neural changes found in young adults with ASD. Movement slowing is reported in normal aging and the emergence of neurological disorders/diseases. For example, the declines in neuromotor functioning that can develop with increasing age and Parkinson’s disease (PD) have been linked to deficits across multiple neuromotor processes; they include slowing of reaction time, preferred walking speed, strength, and finger tapping speed (MacDonald et al. 2003; Batterham et al. 2014; Bielak et al. 2014; Morrison and Newell 2017). Indeed, Hallett et al. (1993) speculated that the gait differences which they observed in adults with autism were the result of non-specific changes in the neurological systems underlying motor control, such as the cerebellum while Vilensky et al. (1981) drew similarities between the gait patterns of persons with ASD to PD (Vilensky et al. 1981). More recent studies have provided support for both these views, implicating both the basal ganglia and cerebellum in the pathogenesis of the movement abnormalities of ASD (Middleton and Strick 2000; Nayate et al. 2005; Rinehart et al. 2006; Wang et al. 2015). With specific reference to the cerebellum, it has been reported that individuals with ASD have 35–95% fewer cerebellar Purkinje cells and that differences in the relative size of the deep cerebellar nuclei can also be found (Mosconi et al. 2015a). Irrespective of the specific neural loci, the consequences of any widespread deficits in neural mechanisms would be expected to present across a range of movements rather than be restricted to one or two specific tasks. In this regard, the collective results of the current study illustrate that the impact of differences in motor function with ASD is not task-dependent and reflected in the performance of specific movements. Rather, the differences observed are probably indicative of widespread and varied changes in neuromotor function, manifesting themselves during the performance of more dynamic actions rather than during static balance tasks.
There were no notable relationships between the motor and cognitive tasks for the ASD group despite the neurobiological evidence that both motor and cognitive functions can be linked to cerebellar function. It would be of use to continue to investigate this relationship utilizing additional assessments, age groups, and functional levels of ASD.
Increased intra-individual variability in ASD
One feature often associated with persons with ASD is differences in the variability of their responses with the pattern of higher variability being used as a marker for distinguishing between controls and persons with ASD (Klein et al. 2006; Geurts et al. 2008; Adamo et al. 2014). To date, the majority of studies of intra-individual differences have largely focused on RT tasks (Klein et al. 2006; Adamo et al. 2014), even though more general motor deficits are also common. In addition to the pattern of generally slower movement responses and decreased strength, the results of the current study revealed that the ASD individuals also exhibited greater variability over trials (i.e., IIV) across the RT, hand grip strength, finger tapping, and walking tasks. While higher within-subject variability for young adults with ASD is consistent with the previous reports (Rinehart et al. 2006; Geurts et al. 2008; Kofler et al. 2013; Adamo et al. 2014; Mottron et al. 2014), the current findings illustrate that the variability cited in ASD children and adolescents continues through to adulthood.
The significance of these increases in IIV across a range of motor tasks cannot be understated as they support the previous view that the deficits in neuromotor function for persons with ASD is manifested by concurrent slowing and increased variability of responses. However, because this pattern is not specific to ASD, it would appear to be indicative of widespread deficits in neuromotor function per se. The previous research has reported a similar trend for both healthy older adults and for patients with neurological diseases, such as PD (Hultsch et al. 2002; Dykiert et al. 2012a; Batterham et al. 2014; Bielak et al. 2014; Bunce et al. 2017; Bauermeister et al. 2017). Taken together, these findings highlight that abnormalities of neuromotor function may be characterized by both slowing and increased variability. While increased within-subject variability for persons with ASD is consistent with previous reports (Rinehart et al. 2006; Geurts et al. 2008; Kofler et al. 2013; Adamo et al. 2014; Mottron et al. 2014), the current findings illustrate that the variability changes cited in ASD children and adolescents continue through to adulthood. Furthermore, consistent with the results showing a widespread slowing of responses, the prevalence of increased variability across different neuromotor tasks supports the view that the impact of the neural changes in ASD are manifested across a range of motor performance tasks and are not specific to one single activity.
Conclusions
This study investigated differences in reaction time, finger tapping, hand dexterity, strength, balance, and walking ability between young adults with ASD and control individuals of similar age. Overall, young adults with ASD exhibited a general slowing of movement responses, reflected by decreased finger tapping speed, general hand dexterity, slower reaction times, and decreased gait speed. Decreased hand grip was also found for the ASD individuals. In addition to the slower movement responses, ASD individuals were more variable during the reaction time, tapping, strength, and walking tasks. Consequently, loss of strength, the general slowing of motor functions (i.e., gait, reaction time, and tapping speed), and increased variability of these same motor responses may reflect the phenotype or phenotypic subtype of young adults with ASD. These findings indicate that IIV measures may be a useful marker of widespread neuromotor dysfunction.
References
Adamo N, Huo L, Adelsberg S, Petkova E, Castellanos FX, Di Martino A (2014) Response time intra-subject variability: commonalities between children with autism spectrum disorders and children with ADHD. Eur Child Adolesc Psychiatry 23:69–79
Alaniz ML, Galit E, Necesito CI, Rosario ER (2015) Hand strength, handwriting, and functional skills in children with autism. Am J Occup Ther 69:1–9
Baio J (2012) Prevalence of autism spectrum disorders—autism and developmental disabilities monitoring network, 14 sites, United States, 2008. Morb Mortal Wkly Rep (MMWR) 61:1–19
Barbeau EB, Meilleur A-AS, Zeffiro TA, Mottron L (2015) Comparing motor skills in autism spectrum individuals with and without speech delay. Autism Res 8:682–693
Batterham PJ, Bunce D, Mackinnon AJ, Christensen H (2014) Intra-individual reaction time variability and all-cause mortality over 17 years: a community-based cohort study. Age Ageing 43:84–90
Bauermeister S, Sutton G, Mon-Williams M et al (2017) Intraindividual variability and falls in older adults. Neuropsychology 31:20–27
Bhat AN, Landa RJ, Galloway JC (2011) Current perspectives on motor functioning in infants, children, and adults with autism spectrum disorders. Phys Ther 91:1116–1129
Bielak AA, Cherbuin N, Bunce D, Anstey KJ (2014) Intraindividual variability is a fundamental phenomenon of aging: evidence from an 8-year longitudinal study across young, middle, and older adulthood. Dev Psychol 50:143–151
Bunce D, Haynes BI, Lord SR, Gschwind YJ, Kochan NA, Reppermund S, Brodaty H, Sachdev PS, Delbaere K (2017) Intraindividual stepping reaction time variability predicts falls in older adults with mild cognitive impairment. J Gerontol A Biol Sci Med Sci 72:832–837
Calhoun M, Longworth M, Chester VL (2011) Gait patterns in children with autism. Clin Biomech (Bristol Avon) 26:200–206
Constantino JN, Davis SA, Todd RD et al (2003) Validation of a brief quantitative measure of autistic traits: comparison of the social responsiveness scale with the autism diagnostic interview-revised. J Autism Dev Disord 33:427–433
D’Mello AM, Stoodley CJ (2015) Cerebro-cerebellar circuits in autism spectrum disorder. Front Neurosci 9:408
David FJ, Baranek GT, Giuliani CA, Mercer VS, Poe MD, Thorpe DE (2009) A pilot study: coordination of precision grip in children and adolescents with high functioning autism. Pediatr Phys Ther 21:205–211
Dykiert D, Der G, Starr JM, Deary IJ (2012a) Age differences in intra-individual variability in simple and choice reaction time: systematic review and meta-analysis. PLoS One 7:e45759
Dykiert D, Der G, Starr JM, Deary IJ (2012b) Sex differences in reaction time mean and intraindividual variability across the life span. Dev Psychol 48:1262–1276
Ferraro FR (2016) No evidence of reaction time slowing in autism spectrum disorder. Autism 20:116–122
Fournier KA, Hass CJ, Naik SK, Lodha N, Cauraugh JH (2010a) Motor coordination in autism spectrum disorders: a synthesis and meta-analysis. J Autism Dev Disord 40:1227–1240
Fournier KA, Kimberg CI, Radonovich KJ et al (2010b) Decreased static and dynamic postural control in children with autism spectrum disorders. Gait Posture 32:6–9
Fournier KA, Amano S, Radonovich KJ, Bleser TM, Hass CJ (2014) Decreased dynamical complexity during quiet stance in children with autism spectrum disorders. Gait Posture 39:420–423
Geurts HM, Grasman RP, Verte S, Oosterlaan J, Roeyers H, van Kammen SM, Sergeant JA (2008) Intra-individual variability in ADHD, autism spectrum disorders and Tourette’s syndrome. Neuropsychologia 46:3030–3041
Graham SA, Abbott AE, Nair A, Lincoln AJ, Muller RA, Goble DJ (2015) The influence of task difficulty and participant age on balance control in ASD. J Autism Dev Disord 45:1419–1427
Hallett M, Lebiedowska MK, Thomas SL, Stanhope SJ, Denckla MB, Rumsey J (1993) Locomotion of autistic adults. Arch Neurol 50:1304–1308
Hasan CZ, Jailani R, Md Tahir N, Ilias S (2017) The analysis of three-dimensional ground reaction forces during gait in children with autism spectrum disorders. Res Dev Disabil 66:55–63
Hocking DR, Menant JC, Kirk HE, Lord S, Porter MA (2014) Gait profiles as indicators of domain-specific impairments in executive control across neurodevelopmental disorders. Res Dev Disabil 35:203–214
Hultsch DF, MacDonald SW, Dixon RA (2002) Variability in reaction time performance of younger and older adults. J Gerontol B Psychol Sci Soc Sci 57:101–115
Inui N, Suzuki K (1998) Practice and serial reaction time of adolescents with autism. Percept Mot Skills 86:403–410
Karalunas SL, Geurts HM, Konrad K, Bender S, Nigg JT (2014) Annual research review: reaction time variability in ADHD and autism spectrum disorders: measurement and mechanisms of a proposed trans-diagnostic phenotype. J Child Psychol Psychiatry 55:685–710
Kern JK, Geier DA, Adams JB, Troutman MR, Davis GA, King PG, Geier MR (2013) handgrip strength in autism spectrum disorder compared with controls. J Strength Cond Res 27:2277–2281
Kindregan D, Gallagher L, Gormley J (2015) Gait deviations in children with autism spectrum disorders: a review. Autism Res Treat 2015:741480
Klein C, Wendling K, Huettner P, Ruder H, Peper M (2006) Intra-subject variability in attention-deficit hyperactivity disorder. Biol Psychiatry 60:1088–1097
Kofler MJ, Rapport MD, Sarver DE, Raiker JS, Orban SA, Friedman LM, Kolomeyer EG (2013) Reaction time variability in ADHD: a meta-analytic review of 319 studies. Clin Psychol Rev 33:795–811
Koziol LF, Budding D, Andreasen N et al (2014) Consensus paper: the cerebellum’s role in movement and cognition. Cerebellum 13:151–177
MacDonald SW, Hultsch DF, Dixon RA (2003) Performance variability is related to change in cognition: evidence from the Victoria Longitudinal Study. Psychol Aging 18:510–523
Middleton FA, Strick PL (2000) Basal ganglia and cerebellar loops: motor and cognitive circuits. Brain Res Rev 31:236–250
Minshew NJ, Sung K, Jones BL, Furman JM (2004) Underdevelopment of the postural control system in autism. Neurology 63:2056–2061
Morrison S, Newell KM (2017) Aging and slowing of the neuromotor system. In: Pachana NA (ed) Encyclopedia of geropsychology. Springer, Singapore, pp 215–226
Mosconi MW, Mohanty S, Greene RK, Cook EH, Vaillancourt DE, Sweeney JA (2015a) Feedforward and feedback motor control abnormalities implicate cerebellar dysfunctions in autism spectrum disorder. J Neurosci 35:2015–2025
Mosconi MW, Wang Z, Schmitt LM, Tsai P, Sweeney JA (2015b) The role of cerebellar circuitry alterations in the pathophysiology of autism spectrum disorders. Front Neurosci 9:296
Mottron L, Belleville S, Rouleau GA, Collignon O (2014) Linking neocortical, cognitive, and genetic variability in autism with alterations of brain plasticity: the trigger-threshold-target model. Neurosci Biobehav Rev 47:735–752
Nayate A, Bradshaw JL, Rinehart NJ (2005) Autism and Asperger’s disorder: are they movement disorders involving the cerebellum and/or basal ganglia? Brain Res Bull 67:327–334
Rinehart NJ, Tonge BJ, Bradshaw JL, Iansek R, Enticott PG, McGinley J (2006) Gait function in high-functioning autism and Asperger’s disorder: evidence for basal-ganglia and cerebellar involvement? Eur Child Adolesc Psychiatry 15:256–264
Salthouse TA (2011) What cognitive abilities are involved in trail-making performance? Intelligence 39:222–232
Schmahmann JD, Sherman JC (1998) The cerebellar cognitive affective syndrome. Brain 121(Pt 4):561–579
Sheridan LK, Fitzgerald HE, Adams KM et al (2006) Normative symbol digit modalities test performance in a community-based sample. Arch Clin Neuropsychol 21:23–28
Travers BG, Powell PS, Klinger LG, Klinger MR (2013) Motor difficulties in autism spectrum disorder: linking symptom severity and postural stability. J Autism Dev Disord 43:1568–1583
Travers BG, Bigler ED, Tromp do PM et al (2014) Longitudinal processing speed impairments in males with autism and the effects of white matter microstructure. Neuropsychologia 53:137–145
Vilensky JA, Damasio AR, Maurer RG (1981) Gait disturbances in patients with autistic behavior: a preliminary study. Arch Neurol 38:646–649
Wang Z, Magnon GC, White SP, Greene RK, Vaillancourt DE, Mosconi MW (2015) Individuals with autism spectrum disorder show abnormalities during initial and subsequent phases of precision gripping. J Neurophysiol 113:1989–2001
Weiss MJ, Moran MF, Parker ME, Foley JT (2013) Gait analysis of teenagers and young adults diagnosed with autism and severe verbal communication disorders. Front Integr Neurosci 7:33
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Morrison, S., Armitano, C.N., Raffaele, C.T. et al. Neuromotor and cognitive responses of adults with autism spectrum disorder compared to neurotypical adults. Exp Brain Res 236, 2321–2332 (2018). https://doi.org/10.1007/s00221-018-5300-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00221-018-5300-9