Abstract
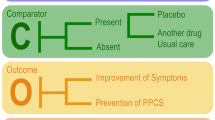
Following mild traumatic brain injury (TBI), patients may self-treat symptoms of concussion, including post-traumatic headache, taking over-the-counter (OTC) analgesics. Administering one dose of OTC analgesics immediately following experimental brain injury mimics the at-home treated population of concussed patients and may accelerate the understanding of the relationship between brain injury and OTC pharmacological intervention. In the current study, we investigate the effect of acute administration of OTC analgesics on neurological function and cortical cytokine levels after experimental diffuse TBI in the mouse. Adult, male C57BL/6 mice were injured using a midline fluid percussion (mFPI) injury model of concussion (6–10 min righting reflex time for brain-injured mice). Experimental groups included mFPI paired with either ibuprofen (60 mg/kg, i.p.; n = 16), acetaminophen (40 mg/kg, i.p.; n = 9), or vehicle (15 % ethanol (v/v) in 0.9 % saline; n = 13) and sham injury paired OTC medicine or vehicle (n = 7–10 per group). At 24 h after injury, functional outcome was assessed using the rotarod task and a modified neurological severity score. Following behavior assessment, cortical cytokine levels were measured by multiplex ELISA at 24 h post-injury. To evaluate efficacy on acute inflammation, cortical cytokine levels were measured also at 6 h post-injury. In the diffuse brain-injured mouse, immediate pharmacological intervention did not attenuate or exacerbate TBI-induced functional deficits. Cortical cytokine levels were affected by injury, time, or their interaction. However, levels were not affected by treatment at 6 or 24 h post-injury. These data indicate that acute administration of OTC analgesics did not exacerbate or attenuate brain-injury deficits which may inform clinical recommendations for the at-home treated mildly concussed patient.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Traumatic brain injury (TBI) is a major cause of death and disability throughout the world (Langlois et al. 2006; Reilly 2007; Roozenbeek et al. 2013). In the USA between 2002 and 2006, the Centers for Disease Control and Prevention estimated 52,000 deaths, 275,000 hospitalizations, and 1,365,000 emergency department visits resulting from TBI each year (Faul et al. 2010). It is also estimated that as high as 42 % of TBIs are not included in these statistics because 1.2–4.3 million survivors of mild TBI annually do not seek medical attention (Setnik and Bazarian 2007) and likely self-medicate.
The mechanical forces of TBI initiate a cascade of secondary injury processes, including inflammation, which continue for days to weeks following injury (Werner and Engelhard 2007). In conflicting studies, cerebral inflammation has been shown to contribute to either beneficial or deleterious effects after traumatic insult [for review, see (Morganti-Kossmann et al. 2002)]. TBI triggers a cascade of inflammation-mediating cytokines (Morganti-Kossmann et al. 2001; Frugier et al. 2010; Semple et al. 2010; Ziebell and Morganti-Kossmann 2010), which can elicit a range of responses including cell differentiation, immune activation, and cell death (Allan and Rothwell 2001). For the present study, the midline fluid percussion injury (mFPI) experimental model in the mouse induces multifocal neuropathology with translational application to mild diffuse TBI, or concussion. Principally in the first day after mFPI in mice, we have reported significantly increased levels of pro-inflammatory cytokine IL-1β in the cortex (Rowe et al. 2014b) along with acute neurological impairments manifested within 1 h of injury (Rowe et al. 2014a). In diffuse TBI, the effects of clinically relevant acute pharmacological inhibition of inflammation on functional outcome are not yet understood.
Secondary injury processes initiated by TBI, including inflammation, are tractable therapeutic targets. Inflammation in the wake of TBI is, in part, mediated by the conversion of membrane-released arachidonic acid into pro-inflammatory prostaglandins by cyclooxygenase-2 (COX-2) (Dash et al. 2000). NSAIDs are widely available over-the-counter drugs used to treat acute pain and inflammation, with mechanisms of action to block COX-1 and/or COX-2, thereby slowing the production of prostaglandins (Vane 1971). Acetaminophen, on the other hand, is presented as an analgesic with actions on cannabinoid receptors (Ottani et al. 2006; Dani et al. 2007), with weaker inflammatory properties. Previous studies suggest anti-inflammatory drugs improve outcome following brain injury as early as 72 h post-injury (Gopez et al. 2005; Ng et al. 2012; Thau-Zuchman et al. 2012; Chio et al. 2013; Gatson et al. 2013). Treatment with the highly specific COX-2 inhibitor DFU [5,5-dimethyl-3(3-fluorophenyl)-4(4-methylsulfonyl)phenyl-2(5H)-furanone] administered daily for 3 days following lateral cortical impact in rats attenuated injury-induced prostaglandin production in the brain and improved functional recovery measured by the Morris water maze and neuroscore at 72 h post-injury (Gopez et al. 2005). Carprofen, a COX-2 inhibitor, administered daily for 7 days following experimental TBI using a closed head injury (CHI) model in mice, also improved functional recovery (Thau-Zuchman et al. 2012). Recovery of function measured by the NSS, however, was not present until 72 h post-injury (Thau-Zuchman et al. 2012). Treatment with anti-inflammatory minocycline for 14 days following CHI in mice resulted in improved NSS scores starting at 72 h post-injury, with improvements lasting through day 7 (Ng et al. 2012). These studies suggest that inhibiting inflammation after mild to severe TBI can improve functional recovery; however, there is evidence to suggest that treatment with ibuprofen over an extended time frame may worsen cognitive outcome. Rats which were continuously treated with ibuprofen for 4 months following lateral fluid percussion injury performed significantly worse in the Morris water maze than non-treated brain-injured rats (Browne et al. 2006). Taken together, previous reports indicate that repeated doses of OTC analgesics, depending on the time frame, may be beneficial or detrimental to recovery from TBI. The acute nature of neurological impairments induced by the mFPI model necessitates acute behavioral analysis to assess the effects of pharmacological intervention (Rowe et al. 2014a). The current study delivers ibuprofen and acetaminophen to determine whether a single treatment with common over-the-counter (OTC) analgesics after diffuse TBI promotes recovery or worsens behavioral outcome.
The current study investigated the effects of acetaminophen and ibuprofen—two common analgesic drugs with different anti-inflammatory mechanisms—on neurological function and cortical cytokine levels after diffuse TBI in the mouse. We hypothesized that acute pharmacological inhibition of injury-induced inflammation will lead to a decrease in inflammatory cytokines, possibly altering functional outcome.
Methods
Animals
Male C57BL/6 mice (Harlan Laboratories, Inc., Indianapolis, IN) were used for all experiments (n = 57). Mice were housed in a 12-h light/12-h dark cycle at a constant temperature (23 °C ± 2 °C) with food and water available ad libitum according to the Association for Assessment and Accreditation of Laboratory Animal Care International. All mice used in this study were singly housed. Mice were acclimated to their environment following shipment for at least 3 days prior to any experiments. After surgery, mice were evaluated daily for postoperative care by a physical examination and documentation of each animal’s condition. Animal care was approved by the Institutional Animal Care and Use Committees at St. Joseph’s Hospital and Medical Center (Phoenix, AZ).
Midline fluid percussion injury (mFPI)
Mice (20–24 g) were subjected to midline fluid percussion injury (mFPI) consistent with methods previously described (Lifshitz 2008). Group sizes are indicated in the “Results” section and figure legends for individual studies. Mice were anesthetized using 5 % isoflurane in 100 % oxygen for 5 min, and the head of the mouse was placed in a stereotaxic frame with continuously delivered isoflurane at 2.5 % via nosecone. While anesthetized, body temperature was maintained using a Deltaphase® isothermal heating pad (Braintree Scientific Inc., Braintree, MA). A midline incision was made exposing bregma and lambda, and fascia was removed from the surface of the skull. A trephine (3 mm outer diameter) was used for the craniotomy, centered on the sagittal suture between bregma and lambda without disruption of the dura. An injury cap prepared from the female portion of a Luer-Loc needle hub was fixed over the craniotomy using cyanoacrylate gel and methyl-methacrylate (Hygenic Corp., Akron, OH). The incision was sutured at the anterior and posterior edges and topical lidocaine ointment was applied. The injury cap was closed using a Luer-Loc cap and mice were placed in a heated recovery cage and monitored until ambulatory before being returned to their sleep cage.
For injury induction 24 h post-surgery, mice were re-anesthetized with 5 % isoflurane delivered for 5 min. The cap was removed from the injury-hub assembly, and the dura was visually inspected through the hub to make sure it was intact with no debris. The hub was then filled with normal saline and attached to a tube connected to the male end of the fluid percussion device (Custom Design and Fabrication, Virginia Commonwealth University, Richmond, VA). An injury of moderate severity for our injury model (1.4 atm) was administered by releasing the pendulum onto the fluid-filled cylinder. Sham-injured mice underwent the same procedure except the pendulum was not released. Mice were monitored for the presence of a forearm fencing response, and righting reflex times were recorded for the injured mice as indicators of injury severity (Hosseini and Lifshitz 2009). The righting reflex time is the total time from the initial impact until the mouse spontaneously rights itself from a supine position. The fencing response is a tonic posturing characterized by extension and flexion of opposite arms that has been validated as an overt indicator of injury severity (Hosseini and Lifshitz 2009). The injury hub was removed and the brain was inspected for uniform herniation and integrity of the dura. The dura was intact in all mice; none were excluded as technical failures. The incision was cleaned using saline and closed using sutures. Moderate brain-injured mice had righting reflex recovery times greater than 6 min and a positive fencing response. Sham-injured mice recovered a righting reflex within 20 s. After spontaneously righting, mice were placed in a heated recovery cage and monitored until ambulatory (approximately 5–15 min) before being returned to their cage. Adequate measures were taken to minimize pain or discomfort.
Pharmacological intervention
All mice received either vehicle or drug treatment immediately following induction of injury or sham. Drugs were administered intraperitoneally in 100 µl of sterile vehicle solution of normal saline and 15 % (v/v) ethanol. Drug-treated mice received either ibuprofen (60 mg/kg; Sigma-Aldrich, St. Louis, MO) or acetaminophen (40 mg/kg; Sigma-Aldrich, St. Louis, MO). These doses were chosen with respect to clinically relevant doses. Dose translations from human to mice were based on body surface area (Reagan-Shaw et al. 2008) and were maintained within the maximum daily dose recommended by the United States Federal Drug Administration (www.fda.gov). Both drugs were compared to the same vehicle-treated control group treated with normal saline and 15 % (v/v) ethanol.
Behavioral testing
Rotarod
Sensorimotor function was assessed using the Economex Rotarod system from Columbus Instruments (Columbus, OH). Mice were pre-trained for three consecutive days. The first 2 days were acclimation (60 s at 4 rpm for 3 trials), and on day three, baseline scores were collected using the test day procedures (see below). For the test at 24 h post-injury, mice were placed on the rod with a starting speed of 4 rpm, and rod rotation speed was continuously increased over 5 min up to a max speed of 28 rpm, as previously published (Bachstetter et al. 2013). The trial ended when the mouse fell from the rod or 5 min elapsed. Two trials were performed at each time point. Data are presented (average of two trials) as latency to fall in seconds and total distance traveled in centimeters. Improvement in performance is presented as the difference in each mouse’s baseline score and test day score, where positive numbers indicate improvement in the task.
Neurological severity score (NSS)
Post-traumatic neurological impairments were assessed at 24 h post-injury using an eight-point NSS paradigm adapted from those previously used in experimental models of TBI (Chen et al. 1996; Semple et al. 2010; Pleasant et al. 2011; Ziebell et al. 2011). One point was given for failure on an individual task, and no points were given if a mouse completed a task successfully. Mice were observed for hindlimb flexion, startle reflex, and seeking behavior (presence of these behaviors was considered successful task completion). Mice traversed in sequence, 3-, 2-, and 1-cm beams. The beams were elevated and mice were given 1 min to travel 30 cm on the beams. The task was scored as a success if the mouse traveled 30 cm with normal forelimb and hindlimb position (forelimb/hindlimb did not hang from the beam). Mice were also required to balance on a 0.5-cm beam and a 0.5-cm round rod for 3 s in a stationary position with front paws between hind paws. Nonparametric data are presented as a composite score ranging from 0 to 8 representing performance on all tasks combined. High final NSS scores were indicative of task failure and interpreted as neurological impairment.
Tissue preparation and cytokine quantification
At 6 or 24 h post-injury, mice were given an overdose of sodium pentobarbital and transcardially perfused with ice-cold phosphate buffered saline (PBS). Mice were decapitated and the brains were dissected on ice. Cortical biopsies (2 mm diameter × 2 mm thickness) were taken and snap frozen in methanol cooled over dry ice and then stored at −80 °C. The protein levels of a panel of inflammation-related cytokines were measured by Quansys Biosciences Mouse Cytokine IR Q-Plex assay (Quansys Biosciences, Logan, UT), according to manufacturer protocol. Cortical biopsies were bead-homogenized using a Precellys 24 in 200 µl of ice-cold Tris-buffered lysis solution supplemented with protease inhibitor cocktail (Complete Protease Inhibitor Cocktail Mini Tablet, Roche Diagnostics, Mannheim, Germany). The cortical homogenate was centrifuged at 3,000 RCF for 20 min at 4 °C in a microcentrifuge. The resulting supernatant (25 µl) was loaded per well of the Q-Plex plate, and cytokine levels were determined by Q-Plex assay. Cytokine levels in the cortex were normalized to the total amount of protein in the sample, as determined by BCA Protein Assay (Thermo Scientific, Rockford, IL).
Statistical analysis
Data are shown as mean ± SEM and analyzed using statistical software (GraphPad Prism 6). For analysis of behavior, uninjured shams from all drug treatment groups were combined and used as a single control (see results). Differences in rotarod performance following TBI were determined by one-way analysis of variance (ANOVA) followed by Sidak’s multiple comparisons test. Nonparametric NSS data were analyzed by Kruskal–Wallis ANOVA, followed by Dunn’s comparison post hoc test (see “Results”). Differences in cytokine concentrations were analyzed by two-way ANOVA. Statistical significance was assigned when p < 0.05.
Results
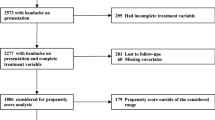
It was not anticipated that drug treatment would change functional outcome in the uninjured sham mice. Statistical analyses confirmed no significant change in rotarod performance or NSS between any sham treatment groups. Vehicle-treated, ibuprofen-treated, and acetaminophen-treated shams were combined into a single control. As anticipated, anti-inflammatory treatment altered cytokine levels in sham treatment groups; cytokine data were analyzed without combining shams.
Diffuse TBI reduced motor performance on the rotarod task regardless of pharmacological intervention
To assess motor function, we used the rotarod task as previously published (Bachstetter et al. 2013). Across groups, there was a significant effect on latency to stay on the rotarod (F(3, 53) = 3.688, p = 0.0174; Fig. 1a; sham n = 27, vehicle-treated injury n = 10, ibuprofen-treated injury n = 12, acetaminophen-treated injury n = 8). Rotarod latency was significantly reduced in vehicle-treated and ibuprofen-treated brain-injured mice compared to sham mice at 24 h post-injury (Fig. 1a). There was no significant latency reduction in acetaminophen-treated brain-injured mice compared to shams (Fig. 1a). Further analysis of rotarod performance confirmed the latency data with distance traveled, showing similar significant effects on distance traveled (F(3, 53) = 3.909, p = 0.0135; Fig. 1b). Distance traveled was significantly reduced in both vehicle and ibuprofen-treated brain-injured mice compared to uninjured sham. There was no difference in distance traveled by acetaminophen-treated brain-injured mice compared to shams. To compensate for trial-based learning, improvement in motor performance was analyzed. Latencies (Fig. 1c) and distances (Fig. 1d) of each mouse at 24 h post-injury were compared to their individual baseline scores at training. Brain-injured mice treated with vehicle and ibuprofen showed significantly less improvement in latency to stay on the rod compared to the improvement of uninjured shams (F(3, 53) = 4.553, p = 0.0065; Fig. 1c). Acetaminophen-treated brain-injured mice did not show a difference in improvement compared to uninjured shams (Fig. 1c). All brain-injured mice, regardless of treatment, showed significantly less improvement in distance traveled compared to shams (F(3, 53) = 6.017, p = 0.0013; Fig. 1d).
No adverse effects of pharmacological intervention on injury-induced motor deficits on the rotarod task. a Injury significantly impaired motor performance as indicated by reduced latency to stay on the rotarod (mean ± SEM; F(3, 53) = 3.688, p = 0.0174), with significant differences between vehicle-treated and ibuprofen-treated brain-injured mice compared to uninjured shams at 24 h post-injury. There was no significant difference between acetaminophen-treated brain-injured mice compared to uninjured shams. b Reduced distance traveled on the rotarod also indicated a significant injury-induced impairment in motor function (mean ± SEM; F(3, 53) = 3.909, p = 0.0135). There was a significant difference between vehicle-treated and ibuprofen-treated brain-injured mice compared to uninjured shams at 24 h post-injury. There was no difference in distance traveled by acetaminophen-treated brain-injured mice compared to uninjured shams. c Brain injury significantly impaired the improvement in latency to stay on the rotarod from baseline (mean ± SEM; F(3, 53) = 4.553, p = 0.0065) indicated by a difference between vehicle-treated and ibuprofen-treated brain-injured mice compared to uninjured shams at 24 h post-injury. d Brain injury also significantly impaired improvement in distance traveled (mean ± SEM; F(3, 53) = 6.017, p = 0.0013) between vehicle-treated, ibuprofen-treated, and acetaminophen-treated brain-injured mice compared to uninjured shams at 24 h post-injury. (Sham n = 27, vehicle-treated injury n = 10, ibuprofen-treated injury n = 12, acetaminophen-treated injury n = 8; *p < 0.05; **p < 0.01)
Overall, diffuse brain injury reduced motor performance measured on the rotarod task. Acetaminophen-treated brain-injured mice did not show injury-induced impairments measured by latency (Fig. 1a, c) or distance (Fig. 1b), but did have a significantly worse improvement in distance from baseline compared to uninjured shams (Fig. 1d). However, the acetaminophen-treated brain-injured mice did not show significant improvements in motor impairments compared to all other brain-injured groups (F(2, 27) = 0.5684, p = 0.5730; Fig. 1a; F(2, 27) = 1.063, p = 0.03594; Fig. 1b; F(2, 27) = 0.06751, p = 0.9349; Fig. 1c). Acute pharmacological intervention, regardless of drug, did not exacerbate or attenuate brain-injury-induced motor deficits.
Diffuse TBI resulted in neurological impairments regardless of pharmacological intervention
All brain-injured mice showed significant neurological impairments measured by the NSS compared to uninjured shams, regardless of pharmacological intervention (KW(4, 57) = 27.37, p < 0.001; Fig. 2; sham n = 27, vehicle-treated injury n = 10, ibuprofen-treated injury n = 12, acetaminophen-treated injury n = 8). At 24 h post-injury, all brain-injured groups had significantly higher NSS scores compared to uninjured shams. There was no significant effect of post-injury pharmacological treatment.
No adverse effects of pharmacological intervention on injury-induced neurological impairments. Significant neurological impairments were detected between groups, as measured by modified NSS (mean ± SEM; KW(4, 57) = 27.37, p < 0.001). Dunn’s multiple comparisons test indicated vehicle-treated, ibuprofen-treated, and acetaminophen-treated brain-injured mice showed significantly higher NSS scores compared to uninjured shams 24 h post-injury. There were no significant changes in function between any brain-injured groups regardless of treatment. (Sham n = 27, vehicle-treated injury n = 10, ibuprofen-treated injury n = 12, acetaminophen-treated injury n = 8; *p < 0.05; ***p < 0.001)
Diffuse TBI resulted in increased cytokine levels at 6 or 24 h post-injury regardless of pharmacological intervention
Upon brain dissection, no differences in hemorrhage or gross pathology were noted among treatment groups. To determine the changes in the inflammatory response following diffuse brain injury, we measured inflammatory cytokines in whole cortex at select time points following injury (6, 24 h). Data from both time points and all measured analytes are presented as measured concentration from cortical homogenate (pg/ml/mg) ± SEM (Table 1). Pro-inflammatory cytokines were found to increase by 6 h post-injury but did not remain increased at 24 h post-injury (Fig. 3). Anti-inflammatory cytokines were not altered at 6 h post-injury but increased by 24 h post-injury (Fig. 4). For all analytes, effect of pharmacological treatment was evaluated across brain-injured groups via one-way ANOVA revealing no significant differences in OTC analgesic-treated versus vehicle-treated groups.
Diffuse brain injury increased pro-inflammatory cytokines in the cortex at 6 h post-injury regardless of pharmacological treatment. For all analytes, the effect of pharmacological treatment was evaluated across brain-injured groups via one-way ANOVA revealing no significant differences in OTC analgesic-treated versus vehicle-treated groups. a IL-1α was increased in the cortex following brain injury at 6 h post-injury compared to uninjured shams but failed to reach significance (mean ± SEM; F(1, 30) = 1.192, p = 0.2837). Overall, IL-1α decreased 24 h post-injury to levels that were undetectable (UD) preventing statistical analysis. b IL-6 was significantly increased in the cortex following brain injury at 6 h post-injury compared to uninjured shams (mean ± SEM; F(1, 30) = 4.468, *p = 0.0430). Though there was an evident trend of both ibuprofen and acetaminophen toward reduction of injury-induced IL-6 compared to vehicle, these differences did not reach statistical significance (F(2, 18) = 1.818, p = 0.1909). There were no significant injury-induced changes in IL-6 at 24 h post-injury (mean ± SEM; F(1, 22) = 0.02819, p = 0.8682); however, levels were significantly lower compared to levels at 6 h post-injury (mean ± SEM; F(1, 58) = 14.76, † p = 0.0003). c TNF-α was significantly increased in the cortex following brain injury at 6 h post-injury compared to uninjured shams (mean ± SEM; F(1, 30) = 6.853, *p = 0.0137). There were no significant injury-induced changes in IL-6 at 24 h post-injury (mean ± SEM; F(1, 23) = 1.756, p = 0.1981); however, levels were significantly lower compared to levels at 6 h post-injury (mean ± SEM; F(1, 59) = 11.38, † p = 0.0013). (6 h: sham n = 5 per treatment, injury n = 7 per treatment; 24 h: sham n = 5 per treatment, injury n = 4–5 per treatment)
Neither brain injury nor pharmacological treatment altered anti-inflammatory cytokine levels in the cortex at 6 h or 24 h post-injury. For all analytes, effect of pharmacological treatment was evaluated across brain-injured groups via one-way ANOVA revealing no significant differences in OTC analgesic-treated versus vehicle-treated groups. a IL-4 was undetectable in the cortex at 6 h post-injury, and levels were not statistically analyzed. IL-4 was present in the cortex 24 h post-injury, and there were no significant injury-induced changes compared to uninjured shams (mean ± SEM; F(1, 23) = 1.047, p = 0.3169). Overall, IL-4 increased 24 h post-injury compared to 6 h post-injury; however, levels were undetectable (UD) preventing statistical analysis. b There were no injured-induced changes in IL-10 in the cortex at 6 h (mean ± SEM; F(1, 30) = 0.2279, p = 0.6366) or 24 h (mean ± SEM; F(1, 23) = 0.6964, p = 0.4126) post-injury compared to uninjured shams. Levels of IL-10 were significantly higher at 24 h post-injury compared to levels at 6 h post-injury (mean ± SEM; F(1, 59) = 0.1672, † p < 0.0001). (6 h: sham n = 5 per treatment, injury n = 7 per treatment; 24 h: sham n = 5 per treatment, injury n = 4-5 per treatment)
Diffuse brain injury resulted in increased cortical levels of pro-inflammatory cytokines IL-6 and TNF-α when compared to uninjured shams at 6 h post-injury (F(1, 30) = 4.468, p = 0.0430, Fig. 3b; F(1, 30) = 6.853, p = 0.0137, Fig. 3c). Another pro-inflammatory cytokine, IL-1α exhibited a modest increase in response to injury which failed to reach statistical significance (F(1, 30) = 1.192, p = 0.2837; Fig. 3a). Significant injury effects are denoted in Fig. 3 by asterisks. No significant injury effects were noted in pro-inflammatory cytokine levels at 24 h post-injury. By 24 h post-injury, IL-6 (F(1, 58) = 14.76, p = 0.0003, Fig. 3b), IL-12 (F(1,59) = 35.61, p < 0.001, Table 1), and TNF-α (F(1, 59) = 11.38, p = 0.0013; Fig. 3c) were each decreased compared to their respective 6-h measurements. Additionally, pro-inflammatory cytokines IL-1α, IL-1β, and IFNγ were reduced to undetectable levels at 24 h, precluding statistical comparisons. Significant effects of time between 6 and 24 h measurements are denoted in Fig. 3 by crosses.
Diffuse brain injury did not alter cortical levels of anti-inflammatory cytokines IL-4 or IL-10 when compared to uninjured shams at 6 h post-injury (F(1, 23) = 1.047, p = 0.3169; F(1, 30) = 0.2279, p = 0.6366, Fig. 4a, b) or 24 h post-injury (F(1, 23) = 0.6964, p = 0.4126, Fig. 4b). IL-4 levels were increased at 24 h post-injury compared to 6 h post-injury; however, 6 h IL-4 levels were undetectable, precluding statistical comparisons (Fig. 4a). Levels of IL-2 and IL-10 were significantly increased at 24 h post-injury compared to 6 h post-injury (F(1, 59) = 0.1672, p < 0.0001, Fig. 4b; F(1,59) = 25.87, p < 0.0001, Table 1). Significant effects of time between 6 and 24 h measurements are denoted in Fig. 3 by crosses.
Discussion
In the diffuse brain-injured mouse, immediate pharmacological intervention with over-the-counter analgesics did not adversely affect sensorimotor or neurological outcome. A single, clinically relevant dose of ibuprofen or acetaminophen was hypothesized to reduce early inflammation leading to a worsened functional outcome. In the current study, we show immediate treatment with ibuprofen or acetaminophen did not impact TBI-induced functional deficits measured by the rotarod and NSS. We also show drug treatment did not alter expression of cortical cytokines at 24 h post-injury.
There is no approved pharmacological treatment for TBI and current medical care focuses primarily on controlling physiological parameters including intracranial pressure and blood pressure (Wang et al. 2006), as well as pain. Severity of TBI is categorized based on the Glasgow Coma Scale (GCS) which reliably classifies the severity of TBI based on clinical symptoms with a total GCS score classifying their injury as mild (score: 13–15), moderate (score: 9–12) or severe (score: <9) (Prins et al. 2013). Given the majority of human TBI encompasses mild to moderate diffuse brain injury for which self-medication may be the primary treatment, the current study sought to replicate the real-life situation in which a survivor of mild TBI self-medicates with a single dose of an OTC analgesic. For this study, we used a moderate severity diffuse brain injury which in our injury model (mFPI) reflects a mild clinical TBI (GCS 13–15). The most frequent symptom after TBI is post-traumatic headache TBI (Theeler et al. 2013), making ibuprofen and acetaminophen principal choices for self-medication. Administering one dose of over-the-counter (OTC) analgesics immediately following brain injury mimics the at-home treated population of concussed patients and may accelerate the understanding of the relationship between brain injury and OTC pharmacological intervention. Administering ibuprofen, an NSAID and COX inhibitor, in opposition to administering acetaminophen, an analgesic with weak anti-inflammatory properties allowed for the investigation of inflammation inhibition on brain injury-induced deficits.
While clinical and experimental data suggest the chronic overproduction of pro-inflammatory cytokines contributes to the progression of pathology in TBI (Schmidt et al. 2005; Lloyd et al. 2008; Cao et al. 2012), the role of immediate inflammation is less clear. Inflammation is critical to the repair process and health of the organism, however, inflammation that is excessive or prolonged can exacerbate damage after the primary injury (Bachstetter et al. 2013). Previous reports have shown that multiple doses of analgesics can alter not only functional outcome but also cellular mechanisms following experimental TBI, see review (Rowe et al. 2013). In this study, a single dose of ibuprofen or acetaminophen given at the time of injury did not attenuate or exacerbate injury-induced sensorimotor or neurological deficits measured 24 h post-injury. Previous studies suggest anti-inflammatory drugs can improve outcome following brain injury as early as 72 h post-injury (Gopez et al. 2005; Ng et al. 2012; Thau-Zuchman et al. 2012; Chio et al. 2013; Gatson et al. 2013). Treatment with the highly specific COX-2 inhibitor DFU [5,5-dimethyl-3(3-fluorophenyl)-4(4-methylsulfonyl)phenyl-2(5H)-furanone] following lateral cortical impact in rats attenuated injury-induced prostaglandin production in the brain and improved functional recovery measured by the Morris water maze and neuroscore at 72 h post-injury (Gopez et al. 2005). Carprofen, a COX-2 inhibitor, administered following closed head injury (CHI) in mice, also improved functional recovery (Thau-Zuchman et al. 2012). Recovery of function measured by the NSS, however, was not present until 72 h post-injury (Thau-Zuchman et al. 2012). Treatment with anti-inflammatory minocycline following CHI in mice resulted in improved NSS scores starting at 72 h post-injury, with improvements lasting through day 7 (Ng et al. 2012). These studies suggest that inhibiting inflammation can improve functional recovery. While the administration of analgesics has been primarily shown to positively influence functional outcome, these studies have incorporated multiple dosing strategies either before or after TBI. While the results are experimentally valid, they do not address the situation faced by a mildly concussed individual not seeking medical attention. In this scenario, an individual would likely self-treat prominent symptoms, including headache, with OTC analgesics immediately post-injury. Experimentally, it would be expected that a single dose of OTC analgesics would have less profound effects upon outcome than a more aggressive dosing strategy.
In the current study, we found that a single dose of OTC analgesics did not attenuate or exacerbate TBI-induced functional deficits. Sensorimotor deficits measured by the rotarod task were present in brain-injured groups compared to uninjured shams regardless of drug treatment at the time of injury. Similarly, brain-injured groups had neurological deficits measured by a modified NSS compared to uninjured shams regardless of drug treatment. Multiple studies have shown analgesics to provide neuroprotection from TBI when administered continually, such that a single clinically relevant dose of OTC analgesics does not affect the pathophysiological and molecular cascades induced by diffuse brain injury. In this way, any initial inhibition of inflammation provided by a single analgesic dose may not prevent the development of neurological deficits by 24 h post-injury. It is also possible that the route of drug administration used in this study reduced the bioavailability of the compounds. Alternate administration routes could increase the bioavailability of the drugs and should be considered for future studies, recognizing the reduced clinical applicability. Overall, this study shows one dose of OTC analgesics given immediately following injury does not alter functional outcome. Given that the OTC analgesics administered in the current study did not worsen behavioral outcome, they may be safe for the clinical treatment of post-traumatic symptoms. It is of note, though, that some anti-inflammatory drugs, including ibuprofen, are not indicated for clinical use after TBI due to their anti-coagulant effects increasing the possibility of intracranial bleeding (Maiese 2008).
Our experimental model of concussion has shown increased levels of pro-inflammatory cytokines peaking between 3 and 9 h post-injury (Bachstetter et al. 2013; Rowe et al. 2014b). In the current study, we measured a panel of inflammation-related interleukins at 6 and 24 h post-injury to investigate the presence or absence of inflammation following injury and at the time behavioral testing was completed. Interestingly, the pattern of cytokine levels over time reflected their functionality and immune properties. Immune mediators that are secreted following brain injury can be divided into subgroups: archetypal pro-inflammatory cytokines (IL-1, TNF, IL-6), anti-inflammatory cytokines (IL-2, IL-4, IL-10, transforming growth factor-beta), and the chemotactic cytokines or chemokines (Banchereau et al. 2012; Woodcock and Morganti-Kossmann 2013). Our data showed, regardless of pharmacological treatment, pro-inflammatory cytokines were increased in the cortex at 6 h but not 24 h post-injury. In contrast, we found anti-inflammatory cytokines were increased in the cortex at 24 h post-injury compared to 6 h post-injury. Our experimental model of injury has shown injury-induced increases in cortical chemokines with a similar time course as the pro-inflammatory cytokines measured in this study, reaching significant increases at 6 h post-injury (Bachstetter et al. 2013). While chemokines were not measured in the current study, based on previously reported data, we predict similar increases occurred.
IL-1α and IL-1β are key mediators of the inflammatory response both peripherally and centrally (Woodcock and Morganti-Kossmann 2013). The IL-1 family of cytokines are regulators of inflammation in relation to acute TBI (Woodcock and Morganti-Kossmann 2013), and previous temporal associations of injury-induced cytokine levels in our injury model have shown increased IL-1β peaking between 3 and 9 h post-injury (Bachstetter et al. 2013; Rowe et al. 2014b). In this study, there were increases in production of IL-1 but the injury effect did not reach significance. By 24 h post-injury, the IL-1 cytokines had become undetectable supporting the role of IL-1 in acute inflammation following TBI. IL-6 and TNF-α are also associated with the acute immune response following TBI. Our study measured cytokines identified as key regulators of the acute phase response including IL-6 and TNF-α (Gabay and Kushner 1999). We found both IL-6 and TNF-α were significantly increased in brain-injured cortex compared to uninjured sham at 6 h supporting their role as key regulators of the acute phase response. When measured at 24 h post-injury, there was a time-dependent reduction in pro-inflammatory cytokines (IL-1α, IL-1β, IL-6, IL-12, IFNγ) suggesting that acute inflammation following experimental diffuse brain injury has resolved, which may or may not emerge at later time points.
In contrast, we found a time-dependent increase in anti-inflammatory cytokines (IL-2, IL-4, and IL-10) at 24 h post-injury compared to 6 h post-injury. IL-10 has been shown to have inhibitory effects on the production of pro-inflammatory cytokines (IL-1, IL-6, TNF-α) which supports different patterns of anti-inflammatory versus pro-inflammatory cytokines after diffuse brain injury. IL-10 is significantly increased at 24 h post-injury which could have inhibitory effects on the pro-inflammatory cytokines, which further validates IL-10 inhibition of IL-1β and TNF to dampen the inflammatory response (Woodcock and Morganti-Kossmann 2013). Overall, there were both injury-induced and time-dependent changes in cortical cytokine levels at both 6 and 24 h post-injury; however, there were no alterations dependent upon pharmalogical intervention.
Regardless of treatment, there were no significant reductions in cytokine levels following the administration of OTC analgesics with varying anti-inflammatory properties. Overall, immediate pharmacological intervention following brain injury did not adversely impact functional outcome as indicated by performance on the rotarod and NSS task. Further investigation is needed to determine whether multiple doses of over-the-counter analgesics attenuate injury-induced deficits. It is possible that chronic treatment may impact the course of recovery following TBI. Ibuprofen administered chronically over a 4-month period to rats subjected to FPI led to a decline in cognitive function, as measured by the Morris water maze (Browne et al. 2006). Future studies should extend the functional evaluation beyond 24 h post-injury. It is possible that the single dose given in this study may have improved or worsened functional outcome at later post-injury time points.
Conclusion
In the diffuse brain-injured mouse, immediate pharmacological intervention did not attenuate or exacerbate TBI-induced functional deficits. Pro-inflammatory cortical cytokine levels were increased at 6 h post-injury, and anti-inflammatory cytokines were increased at 24 h post-injury. We conclude that while a single dose of OTC analgesics does not significantly inhibit the immediate injury-induced inflammation, it does not adversely affect functional outcome. Further investigation is needed to examine time of drug treatment and multiple dosing.
References
Allan SM, Rothwell NJ (2001) Cytokines and acute neurodegeneration. Nat Rev Neurosci 2:734–744. doi:10.1038/35094583
Bachstetter AD, Rowe RK, Kaneko M, Goulding D, Lifshitz J, Van Eldik LJ (2013) The p38alpha MAPK regulates microglial responsiveness to diffuse traumatic brain injury. J Neurosci 33:6143–6153
Banchereau J, Pascual V, O’Garra A (2012) From IL-2 to IL-37: the expanding spectrum of anti-inflammatory cytokines. Nat Immunol 13:925–931. doi:10.1038/ni.2406
Browne KD, Iwata A, Putt ME, Smith DH (2006) Chronic ibuprofen administration worsens cognitive outcome following traumatic brain injury in rats. Exp Neurol 201:301–307
Cao T, Thomas TC, Ziebell JM, Pauly JR, Lifshitz J (2012) Morphological and genetic activation of microglia after diffuse traumatic brain injury in the rat. Neuroscience 225:65–75
Chen Y, Constantini S, Trembovler V, Weinstock M, Shohami E (1996) An experimental model of closed head injury in mice: pathophysiology, histopathology, and cognitive deficits. J Neurotrauma 13:557–568
Chio CC, Chang CH, Wang CC et al (2013) Etanercept attenuates traumatic brain injury in rats by reducing early microglial expression of tumor necrosis factor-alpha. BMC Neurosci 14:33
Dani M, Guindon J, Lambert C, Beaulieu P (2007) The local antinociceptive effects of paracetamol in neuropathic pain are mediated by cannabinoid receptors. Eur J Pharmacol 573:214–215. doi:10.1016/j.ejphar.2007.07.012
Dash PK, Mach SA, Moore AN (2000) Regional expression and role of cyclooxygenase-2 following experimental traumatic brain injury. J Neurotrauma 17:69–81
Faul M, Xu L, Wald MM, Coronado VG (2010) In: Centers for disease control and prevention NCfIPaC (ed) Traumatic brain injury in the United States: emergency department visits, hospitalizations and deaths 2002–2006. Atlanta, GA
Frugier T, Morganti-Kossmann MC, O’Reilly D, McLean CA (2010) In situ detection of inflammatory mediators in post mortem human brain tissue after traumatic injury. J Neurotrauma 27:497–507
Gabay C, Kushner I (1999) Acute-phase proteins and other systemic responses to inflammation. N Engl J Med 340:448–454
Gatson JW, Liu MM, Abdelfattah K, Wigginton JG, Smith S, Wolf S, Minei JP (2013) Resveratrol decreases inflammation in the brain of mice with mild traumatic brain injury. J Trauma Acute Care Surg 74:470–474; discussion 474–475
Gopez JJ, Yue H, Vasudevan R et al (2005) Cyclooxygenase-2-specific inhibitor improves functional outcomes, provides neuroprotection, and reduces inflammation in a rat model of traumatic brain injury. Neurosurgery 56:590–604
Hosseini AH, Lifshitz J (2009) Brain injury forces of moderate magnitude elicit the fencing response. Med Sci Sports Exerc 41:1687–1697
Langlois JA, Rutland-Brown W, Wald MM (2006) The epidemiology and impact of traumatic brain injury: a brief overview. J Head Trauma Rehabil 21:375–378
Lifshitz J (2008) Fluid percussion injury In: Chen J, Xu X-M, Zhang J (eds) Animal models of acute neurological injuries. The Humana Press Inc., Totowa, NJ
Lloyd E, Somera-Molina K, Van Eldik LJ, Watterson DM, Wainwright MS (2008) Suppression of acute proinflammatory cytokine and chemokine upregulation by post-injury administration of a novel small molecule improves long-term neurologic outcome in a mouse model of traumatic brain injury. J Neuroinflammation 5:28
Maiese K (2008) Head injuries: diagnosis and treatment. In: The merck manual home health handbook, vol 2013. Merck Sharp & Dohme Corp., Whitehouse Station, NJ
Morganti-Kossmann MC, Rancan M, Otto VI, Stahel PF, Kossmann T (2001) Role of cerebral inflammation after traumatic brain injury: a revisited concept. Shock 16:165–177
Morganti-Kossmann MC, Rancan M, Stahel PF, Kossmann T (2002) Inflammatory response in acute traumatic brain injury: a double-edged sword. Curr Opin Crit Care 8:101–105
Ng SY, Semple BD, Morganti-Kossmann MC, Bye N (2012) Attenuation of microglial activation with minocycline is not associated with changes in neurogenesis after focal traumatic brain injury in adult mice. J Neurotrauma 29:1410–1425
Ottani A, Leone S, Sandrini M, Ferrari A, Bertolini A (2006) The analgesic activity of paracetamol is prevented by the blockade of cannabinoid CB1 receptors. Eur J Pharmacol 531:280–281. doi:10.1016/j.ejphar.2005.12.015
Pleasant JM, Carlson SW, Mao H, Scheff SW, Yang KH, Saatman KE (2011) Rate of neurodegeneration in the mouse controlled cortical impact model is influenced by impactor tip shape: implications for mechanistic and therapeutic studies. J Neurotrauma 28:2245–2262
Prins M, Greco T, Alexander D, Giza CC (2013) The pathophysiology of traumatic brain injury at a glance. Dis Model Mech 6:1307–1315
Reagan-Shaw S, Nihal M, Ahmad N (2008) Dose translation from animal to human studies revisited. FASEB J 22:659–661
Reilly P (2007) The impact of neurotrauma on society: an international perspective. Prog Brain Res 161:3–9. doi:10.1016/S0079-6123(06)61001-7
Roozenbeek B, Maas AI, Menon DK (2013) Changing patterns in the epidemiology of traumatic brain injury. Nat Rev Neurol 9:231–236
Rowe RK, Harrison JL, Thomas TC, Pauly JR, Adelson PD, Lifshitz J (2013) Using anesthetics and analgesics in experimental traumatic brain injury. Lab Anim (NY) 42:286–291
Rowe RK, Harrison JL, O’Hara BF, Lifshitz J (2014a) Recovery of neurological function despite immediate sleep disruption following diffuse brain injury in the mouse: clinical relevance to medically untreated concussion sleep. Sleep 37:743–752
Rowe RK, Striz M, Bachstetter AD, Van Eldik LJ, Donohue KD, O’Hara BF, Lifshitz J (2014b) Diffuse brain injury induces acute post-traumatic sleep. PLoS ONE 9:e82507. doi:10.1371/journal.pone.0082507
Schmidt OI, Heyde CE, Ertel W, Stahel PF (2005) Closed head injury—an inflammatory disease? Brain Res Brain Res Rev 48:388–399
Semple BD, Bye N, Rancan M, Ziebell JM, Morganti-Kossmann MC (2010) Role of CCL2 (MCP-1) in traumatic brain injury (TBI): evidence from severe TBI patients and CCL2−/− mice. J Cereb Blood Flow Metab 30:769–782
Setnik L, Bazarian JJ (2007) The characteristics of patients who do not seek medical treatment for traumatic brain injury. Brain Inj 21:1–9
Thau-Zuchman O, Shohami E, Alexandrovich AG, Trembovler V, Leker RR (2012) The anti-inflammatory drug carprofen improves long-term outcome and induces gliogenesis after traumatic brain injury. J Neurotrauma 29:375–384
Theeler B, Lucas S, Riechers RG 2nd, Ruff RL (2013) Post-traumatic headaches in civilians and military personnel: a comparative, clinical review. Headache 53:881–900. doi:10.1111/head.12123
Vane JR (1971) Inhibition of prostaglandin synthesis as a mechanism of action for aspirin-like drugs. Nat New Biol 231:232–235
Wang KK, Larner SF, Robinson G, Hayes RL (2006) Neuroprotection targets after traumatic brain injury. Curr Opin Neurol 19:514–519
Werner C, Engelhard K (2007) Pathophysiology of traumatic brain injury. Br J Anaesth 99:4–9. doi:10.1093/bja/aem131
Woodcock T, Morganti-Kossmann MC (2013) The role of markers of inflammation in traumatic brain injury. Front Neurol 4:18. doi:10.3389/fneur.2013.00018
Ziebell JM, Morganti-Kossmann MC (2010) Involvement of pro- and anti-inflammatory cytokines and chemokines in the pathophysiology of traumatic brain injury. Neurotherapeutics 7:22–30
Ziebell JM, Bye N, Semple BD, Kossmann T, Morganti-Kossmann MC (2011) Attenuated neurological deficit, cell death and lesion volume in Fas-mutant mice is associated with altered neuroinflammation following traumatic brain injury. Brain Res 1414:94–105
Acknowledgments
Research reported in this publication was supported, in part, by National Institute of Neurological Disorders and Stroke of the National Institutes of Health under award number R01NS065052, R01NS065052-S, R21NS072611, and KSCHIRT 10-5A.
Author information
Authors and Affiliations
Corresponding author
Additional information
Jordan L. Harrison and Rachel K. Rowe contributed equally to the design, execution, and interpretation of the study.
Rights and permissions
About this article
Cite this article
Harrison, J.L., Rowe, R.K., O’Hara, B.F. et al. Acute over-the-counter pharmacological intervention does not adversely affect behavioral outcome following diffuse traumatic brain injury in the mouse. Exp Brain Res 232, 2709–2719 (2014). https://doi.org/10.1007/s00221-014-3948-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00221-014-3948-3