Abstract
The interplay between gait and specific cognitive faculties, in particular executive function (EF) and dual tasking abilities, has been described in healthy adults and in patients with Parkinson’s disease (PD). There is, however, little direct evidence on the relationship between cognitive function, gait, and fall risk in PD, especially in the “ON” state (i.e., under the influence of the anti-parkinsonian medications). To address this issue, we evaluated cognitive function and gait under usual walking and dual-task conditions in 30 patients with PD in the ON state of the medication cycle. Subjects were classified as fallers or non-fallers based on their history. A computerized battery quantified cognitive function. Gait was assessed under three conditions: (1) Usual walking, (2) While subtracting serial 3 s, and (3) While subtracting serial 7 s. The EF and attention scores were lower in the fallers, compared to non-fallers (P ≤ 0.037), but general measures of cognition, e.g., memory, (P = 0.341) were not. Gait speed, variability, and the bilateral coordination of gait were worse in the fallers in all conditions. The DT effects on gait variability and bilateral coordination were larger in the fallers (P = 0.044, P = 0.061, respectively). These results suggest that patients with PD who have a high risk of falling are more sensitive to DT effects, perhaps as a result of relatively poor EF. These cognitive and motor deficits may increase the likelihood of loss of balance during everyday attention-demanding tasks among patients with PD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Falls are one of the most common negative consequences of Parkinson’s disease (PD). Patients with PD fall frequently, two to three times that seen in the general elderly population (Bloem et al. 2004; Pickering et al. 2007). Falls in PD significantly impact on psychological and physical function in many ways. They often bring about the development of fear of falling (Adkin et al. 2003), loss of independence, increased admission to nursing home (Hely et al. 1999), injuries, reduced mobility, and weakness (Sato et al. 1998). Given the profound and widespread negative impact of falls, it is not surprizing that recently published guidelines suggest that neurologists inquire about fall status at every clinical visit (Cheng et al. 2010).
Fall risk factors among patients with PD include disease severity, motor function, and level of mobility (Kerr et al. 2010). Recent studies also identified cognitive impairment as an independent contributing factor (Latt et al. 2009a; Allcock et al. 2009). This association between cognitive impairment and falls in PD parallels findings in older adults and in a variety of neurological patient populations (Alexander and Hausdorff 2008; Bootsma-van der et al. 2003; Rochester et al. 2005; Springer et al. 2006; van Iersel et al. 2008; Yogev-Seligmann et al. 2008). In those populations, the ability to walk while performing another task, i.e., dual tasking (DT), has specifically been associated with fall risk (Bootsma-van der et al. 2003; Springer et al. 2006; Sheridan and Hausdorff 2007; Plummer-D’Amato et al. 2008; Yang et al. 2007; Kalron et al. 2010). Patients with PD share many of the fall risk factors of the general elderly population and, while clearly not identical, the profiles of the motor and cognitive deficits overlap (Bloem et al. 2004; Hausdorff et al. 2006; Yogev et al. 2007). While the negative impact of DT on gait among patients with PD has also been documented (Camicioli et al. 1998; Yogev-Seligmann et al. 2008; Yogev et al. 2005, 2007; Hausdorff et al. 2003a), it remains to be seen if a reduced DT performance is associated with an increased fall risk among patients with PD. To more fully understand the factors that contribute to fall risk in PD, it is important to determine the possible role of DT gait in fall risk.
To our knowledge, however, no studies have yet to directly compare the effects of DT among PD fallers and non-fallers. The purpose of the present report was to begin to evaluate the relationship between DT gait abilities and fall risk in patients with PD. Given the study by Allcock et al. (2009) and the findings in other populations, we hypothesized that the effects of DT on gait would be larger among PD fallers, compared to PD non-fallers. More specifically, since in the elderly population, gait variability increased in DT conditions among fallers (Springer et al. 2006), we hypothesized that the DT effect would be larger among PD fallers, compared to PD non-fallers. We also evaluated the effects of DT on other measures of gait (e.g., bilateral coordination of gait) to determine whether these features responded differently in fallers and non-fallers. A secondary objective was to evaluate which executive functions are more impaired among PD fallers, compared to PD non-fallers. To accomplish these aims we re-examined a database that was recently analyzed for other purposes (Plotnik et al. 2011). Since many falls occur in the “ON” medication state, when patients are generally more mobile and exposed to circumstances that often lead to falls (Kerr et al. 2010), we focused on gait during the “ON” state.
Materials and methods
Subjects
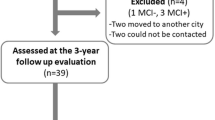
The analyses described herein are based on a data set previously reported (Plotnik et al. 2011). The study participants were subjects with idiopathic PD (n = 30), as defined by the UK Brain Bank criteria (Gelb et al. 1999).
Patients were included if they were receiving levodopa treatment and experienced motor response fluctuations, either ‘predictable’ or ‘non-predictable’ (as documented in their routine medical records by the treating neurologist). In addition to levodopa, seven patients were treated with dopamine agonists, ten with amantadine, eight with monoamine oxidase B (MAO-B) inhibitors, and three with catechol-O-methyltransferase (COMT) inhibitors. Subjects were excluded if they had brain surgery in the past, or if they had clinically significant co-morbidities likely to affect gait including diabetes mellitus, rheumatic or orthopedic disease, dementia (score of the Mini Mental State Exam, MMSE < 25), major depression, or history of stroke, as determined by clinical or radiological evaluation. The subjects were characterized with respect to age, gender, height and weight, body mass index (BMI), and disease duration.
To determine if a subject has an increased risk of falling, the following questions were introduced to the patient: (1) Did you fall in the past month?; (2) Did you fall in the past year?; (3) How many times did you fall in the past year?; and (4) Do you fear that you will fall?. For the purpose of the present analyses, the subjects were divided into two groups: (1) Fallers (n = 16) if a subject responded ‘yes’ to question 2 and (2) Non-fallers (n = 14) if a subject responded ‘no’. To further explore the association between DT gait and fall risk, we also compared recurrent fallers (patients who reported at least two falls) to non-fallers. The experimental protocol was approved by the local human studies committee. All subjects provided informed written consent according to the Declaration of Helsinki prior to enrollment in the study.
Experimental procedure
The patients started the testing during their “ON” state of the medication cycle, i.e., approximately 45 min to 1 h after the last intake of anti-parkinsonian medication, after confirming being in a good “ON” state. All testing was performed in the “ON” state to address our primary objective and as is typical in studies of the assessment of cognitive function in patients with PD, minimizing potentially confounding motor effects. If the subject or the examiner reported ‘wearing off’, the patient took the next dose of medication, and when the patient reported returning to “ON”, he/she resumed the examination (only three subjects had to retake their medications). The protocol was performed in this order: the assessment of gait, cognitive function, and clinical symptoms. The protocol lasted about 1.5–2 h.
Clinical evaluation and assessment of falls and group classification
PD status was evaluated using the Unified Parkinson’s Disease Rating Scale (UPDRS) (Fahn et al. 1987) and the Hoehn and Yahr (H&Y) staging (Hoehn and Yahr 1967). The clinical evaluation also included the timed up and go (TUG) test of mobility (Podsiadlo and Richardson 1991). Briefly, for the TUG, the subject was seated in a chair. When told to start, the subject was asked to get up, walk forward a distance of 3 m, turn, go back to the chair, and sit down again. The time required for completion of the task was measured using a stopwatch. Two trials were performed and the second was analyzed. Affect, a potential confounder, was assessed using the Geriatric Depression Scale (GDS; Yesavage et al. 1982) and the Spielberger State and Trait Anxiety Inventory test (Spielberger and Gorusch 1983).
Gait protocol
The subjects wore force-sensitive insoles (Pedar-X, Novel, Germany) that use an array of capacitive sensors (99 in each insole) to measure the ground reaction forces under each foot at a sampling rate of 100 Hz. The data were saved on a portable recording unit and then transferred to a computer for offline analysis (i.e., extracting from the signal temporal parameters of the gait cycles). Prior to the experiment, the subjects received an explanation about the protocol and were introduced to the walking area, a level ~20-m-long and 2-m-wide corridor. Three gait tasks were performed in a random order, with about 5 min of rest between each task: (1) Usual walking: the subject walked back and forth in the corridor covering a distance of ~80 m at his or her self-selected comfortable pace. (2) Dual Tasking (DT): serial three (S3) condition (DT_S3). The subject walked the same path as during Usual-walking, but this time performed serial subtractions of the number three starting from a randomly presented three digit number (e.g., 500, 497, 494…). (3) DT_S7: same as DT_S3, except that the number seven was subtracted. Several studies suggest that serial subtractions is one of the most effective DT paradigms, causing gait changes in healthy subjects and patients with PD (e.g., Springer et al. 2006; Yogev et al. 2005).
Cognitive assessment
“Pen and Paper” tests
To assess executive function (EF) capabilities, we used The Trails Making test (TMT), a classic test of EF test that evaluates visual scanning and task switching. TMT performance has been associated with dual-task abilities and gait impairments (e.g., reduced gait speed) during a complex walking task (Coppin et al. 2006; Herman et al. 2010).
The color version of the test was used. Briefly, the subject has to draw a line connecting numbered circles (1–25) randomly scattered on a page (TMT-A), and then to repeat this task (on a different page) with the additional demand to alternate the path between circles painted in two different colors (TMT-B). Times needed for completing the TMT-A, TMT-B, and the time difference between TMT-B and TMT-A [TMT (B-A)] were recorded.
The second test of EF is the digit span test. Subjects were requested to repeat series of digits that were read by the examiner in the same order (‘forward’) or in reverse order (‘backwards’). The maximum numbers of digits that could be repeated without two mistakes were recorded for the ‘forward’ and ‘backward’ parts. These values were summed and served as the score of this test. This test assesses the domain of working memory.
Computerized battery of cognitive tests
Computerized cognitive tests were performed with the Mindstreams system (NeuroTrax, Corp., Newark, NJ). This consists of software that resides on a local testing computer and serves as the platform for interactive cognitive tests (Dwolatzky et al. 2003, 2004). The following cognitive capacities were studied and quantified as individual indices: EF, attention, information processing speed, memory, and visual–spatial orientation. Familiarization with the testing environment and with each individual test was accomplished through practice sessions. The scoring system has been elaborately described elsewhere (Doniger et al. 2005, 2006; Dwolatzky et al. 2003, 2004; Yogev et al. 2005). Briefly, the performance of each cognitive domain is compared to a normal distribution of values based on data collected from healthy control subjects with the same age and gender as the subject. A score of 100 represents the mean of each cognitive domain for healthy control subjects. Scores of 85 and 115 are one standard deviation below or above the age and education adjusted mean, respectively. Performance on these computerized cognitive tests were previously associated with fall risk in older adults (Herman et al. 2010; Springer et al. 2006) and with the effects of therapeutic interventions and DT on gait among patients with PD (Yogev et al. 2005). The Mini Mental State Exam (MMSE; Folstein et al. 1975) was used as a screen for dementia and as a gross measure of cognitive function.
Gait analysis
For each leg, the time series of the force profile (sum of the forces sampled by each of the individual sensors) were analyzed by computer software that automatically detects the times of the heel strike and the toe-off of each gait cycle, as previously described (Hausdorff et al. 1998, 2003b). In order to focus on the assessment of undisturbed continuous walking, the collected data were pre-processed and strides belonging to 180° turns (i.e., at the end of the corridor) were excluded from the analysis, as detailed elsewhere (Hausdorff et al. 2003b). Gait outcome measures representing general mobility, gait variability, and bilateral function of gait were calculated for each walking condition: Mobility measures: (1) Gait speed- Average gait speed was determined using a stopwatch by measuring the average time the subject walked the middle fifteen meters of the walking path; (2) Stride length- Average stride length was determined by the product of the average gait speed and the average stride time (see below). Gait variability measures: (1) Stride time variability (i.e., the coefficient of variation (CV) of the stride time, left and right stride times, i.e., L_str and R_str, respectively); (2) Swing time variability- the CV of the swing time- left and right (LSW_CV and RSW_CV, respectively). Since stride and swing time values and stride and swing time variability values were highly correlated between the left and the right leg during all walking conditions (0.79 ≤ R ≤ 1.00; P < 0.001), we report here data from the left leg only (i.e., L_str and L_CV, L_SW, and LSW_CV). Gait variability measures have been shown to be associated with parkinsonian gait from early stages of the disease (Baltadjieva et al. 2006), may even be a bio-marker of PD (Mirelman 2011), and have been associated with fall risk in PD (Hausdorff 2009). Swing time variability was found especially sensitive to DT in PD (Yogev et al. 2005).
Finally, the following measures assessed bilateral function of gait:
-
1.
Gait Asymmetry (GA): Calculation of GA is performed according to the relationship:
This measure has been described in healthy subjects and in patients with PD (Plotnik et al. 2005; Yogev et al. 2007). The natural logarithm was applied to take into account the skewed nature of the data.
-
2.
Phase Coordination Index (PCI): The coordination of left–right stepping was assessed using a recently described measure, i.e., the PCI. A full description and derivation of the PCI metric is detailed elsewhere (Plotnik et al. 2007). Lower PCI values reflect a more consistent and more accurate phase generation.
Data handling and statistical analysis
Descriptive statistics are reported as mean ± standard deviation (SD). Demographic and clinical parameters were compared between the fallers and the non-fallers based on the Student’s t test. Since age was significantly higher for the fallers (see Table 1), scores on cognitive tests were compared between the groups using univariate analysis of variance (U-ANOVA) entering GROUP (i.e., fallers, non-fallers) as a fixed factor. For the ‘pen and paper’ tests, age was entered as a covariate to the model, but not for the computerized test battery for which the scores are already normalized with respect to age. Gait variables were checked for normality and pair wise exclusion of outliers was performed if needed. Only in the case of PCI and GA, one data point was excluded in some of the walking conditions. Statistical significance was considered if P < 0.05. If 0.1 < P < 0.05, the results were considered marginally significant.
To address the primary objective of the study, a general linear model (GLM) with repeated measures was applied to evaluate how DT affected gait variability. Similar analyses were applied for each of the different gait parameters (i.e., gait speed, stride length, GA, PCI). Each gait parameter was assessed as within-subject variable with three levels (i.e., TASK: usual walking, DT_S3, DT_S7). The GROUP parameter (i.e., fallers, non-fallers) was the between-subject variable and age was fed into the model as a covariate. The Group X Task interaction assessed any differential effect of DT.
For any gait parameter that this interaction was significant or marginally significant, we applied a secondary analysis in order to determine if the different extent of the DT effect on gait was associated with the DT_S3 effect as compared with the usual walking, and also (or exclusively) with the DT_S7 effect in comparison with the performance in the DT_S3. Therefore, additional post hoc analyses were applied two more times, this time with only two TASK levels: (1) Usual walking and DT_S3 and (2) DT_S3 and DT_S7 (Bonferroni corrected, K = 2).
For any gait parameter for which a significant GROUP effect was found by the GLM, in the case of significant Group X Task interaction, additional post hoc comparisons between the two groups, for each task independently. This was done using three U-ANOVA models with GROUP as a fixed factor and AGE as a covariate (for usual walking, DT_S3 and DT_S7). The statistical significance level was adjusted using the Bonferroni method (K = 3). Within-group DT effects were assessed for each gait parameter using multiple paired t test procedures (i.e., comparing Usual walking with DT_S3 and DT_S7 and comparing DT_S3 with DT_S7) for each group separately, with the statistical significance level adjusted using the Bonferroni method (K = 3).
Results
Demographic and clinical characteristics of the fallers and non-fallers are described in Table 1. The mean age of the fallers was approximately 6 years higher than the non-fallers (fallers: 68.6 ± 6.7 years; non-fallers: 62.8 ± 6.8 years; P = 0.026), and their BMI was significantly lower (fallers: 24.6 ± 4.0 kg/m2; non-fallers: 28.9 ± 4.1 kg/m2; P = 0.008). Disease duration, Hoehn & Yahr staging, UPDRS total score, and the score of UPDRS motor part (part III) did not differ significantly between the groups (P ≥ 0.178). The fallers had significantly higher TUG values (fallers: 10.1 ± 3.2 s; non-fallers: 8.3 ± 2.2 s; P = 0.029). Anxiety, depressive symptoms, and fear of falling were not statistically different between the groups (P ≥ 0.285). Univariate analysis of variance (U-ANOVA) with ‘age’ as a covariate suggested that BMI group differences was not affected by age and that the level of statistical significance for group differences in TUG values decreases after adjusting for age (F 1,27 = 2.993; P = 0.095).
Cognitive evaluation
Table 2 depicts the results of the computerized battery of cognitive tests and the ‘pen and paper’ tests for each group. No significant group differences in the performance of the ‘pen and paper’ tests were observed (F 1,27 ≤ 2.018; P ≥ 0.167). On the computerized cognitive test battery, fallers had lower EF and attention scores (F 1,27 ≥ 4.180; P ≤ 0.037) and visual spatial performance also tended to be worse among the fallers (F 1,28 = 3.195; P = 0.085).
Differential effects of cognitive loading on gait for fallers and non-fallers
Figure 1 describes the mean values of each of the gait measures in each walking condition for each group. For both groups, DT had a detrimental effect for all gait measures. Gait became slower (Fig. 1a), stride length became shorter (Fig. 1b), and gait pacing became more variable (Fig. 1c, d). In addition, gait became less coordinated in terms of the left–right stepping phasing (i.e., increased PCI, Fig. 1e) and more asymmetric (Fig. 1f; see the figure legend for details on within-group statistical comparisons).
Effect of DT on gait measures. Across all panels, ** represent statistical significance level of 0.01 < P < 0.05 for between subjects comparisons. Error bars reflect the SEM, within group comparisons between conditions were performed by paired t test. a Gait speed- for both groups gait speed decreased significantly from usual to DT_S3 and from DT_S3 to DT_S7 conditions (P < 0.001). b Stride length- for both groups stride length decreased significantly from usual to DT_S3 conditions (P < 0.001). The additional decrease from DT_S3 to DT_S7 was significant for non-fallers (P < 0.01) and for the fallers (P < 0.05). c Stride time variability- increased for fallers from usual to the DT conditions (P < 0.05), but not for the change between DT_S3 and DT_S7 (P > 0.552). For non-fallers, the increase of stride time variability from usual to DT_S3 condition was marginally significant (0.05 < P < 0.10) and not significant between DT_S3 and DT_S7 (P > 0.10). d Swing time variability- for the fallers swing time variability increased significantly between DT_S3 and usual walking (P < 0.01), but not between DT_S3 and DT_S7 (P > 0.9). For non-fallers, this increase from usual to DT_S3 condition was not significant (P > 0.2). The increase in between DT_S3 and DT_S7 was significant (P < 0.05). e PCI- for the fallers PCI increased significantly from usual to DT_S3 (P < 0.01), but not between DT_S3 and DT_S7 (P > 0.67). Similar results were seen for the non-fallers (P < 0.01 and P > 0.144, respectively). f GA-. for the fallers and for the non-fallers, none of the within-subject paired comparisons between gait conditions was statistically significant (P > 0.215)
The GLM models did not identify significant Group X Task interactions (F 2,26 ≤ 1.228; P ≥ 0.301) for DT-related changes of gait speed (Fig. 1a), stride length (Fig. 1b), stride time variability (Fig. 1c), or GA (Fig. 1f). Statistically significant and marginally significant Group X Task interactions were found for swing time variability (F 2,26 = 3.301; P = 0.044; Fig. 1d) and for PCI (F 2,25 = 3.234; P = 0.061, Fig. 1e), respectively. Post hoc group comparisons (with ‘age’ as a covariate, and Bonferroni corrected) revealed that for PCI and swing time variability group differences, only the DT_S3 condition significantly differentiated between the groups (F 2,25 ≥ 8.561; P < 0.05; 1D and 1E).
Further inspection suggests that for PCI. The Group X Task interaction is significant in the case of usual walking and DT_S3 conditions (F 1,26 = 8.561; P < 0.01), but not for the incremental deterioration between DT_S3 and DT_S7 conditions (F 1,26 = 0.811; >0.378). Similarly, there was a trend for the increase in swing time variability to be higher in fallers when compared to non-fallers between usual walking and DT_S3 (F 1,27 = 5.553; 0.05 < P < 0.1), but not between DT_S3 and DT_S7 (F 1,27 = 5.553; P > 0.119).
Effect of recurrent falls
To further explore the association between DT gait and fall risk, we repeated the analyses evaluating the DT effects among recurrent fallers (patients who reported at least two falls; n = 7, mean age: 70.9 ± 5.7 years). In general, the Group X Task interactions were even stronger than that observed when including all of the fallers. For example, among the recurrent fallers, the mean values (±SD) of swing time variability were 6.55 ± 2.22%, 10.96 ± 3.24%, and 10.64 ± 2.1% for the usual walking, DT_S3 and DT_S7 conditions, respectively (compare with Fig. 1d; for example, during DT_S7, swing time variability only increased to 5.58 and 8.47% among non-fallers and fallers, respectively). The Group X Task interaction when comparing recurrent fallers to non-fallers was highly significant (F 2,17 = 10.524; P = 0.001).
Discussion
This study joins previous investigations that demonstrated the strong detrimental effect of DT on the quality of gait among patients with PD (e.g., Yogev et al. 2007). Here, we show, presumably for the first time, that the DT effect is stronger in patients with PD who have a tendency to lose postural stability and fall, when compared to other patients with PD who do not. In particular, the findings support the hypothesis that DT differentially effects gait variability among PD fallers, compared to non-fallers. Our results also indicate that specific cognitive capacities, i.e., executive function and attention, are impaired among subjects with PD who tend to fall. The DT effects on gait were observed during the optimal “ON” stage of the medication cycle. The significant DT effect seen even during this relatively optimal motor state underscores how difficult it is for these patients to maintain stable gait patterns when encountering concurrent demands on cognitive resources.
In the present study, relatively decreased executive function and attention capacities were observed among the PD fallers, but cognition in general was not. For example, MMSE scores were similar in fallers and non-fallers (recall Table 2). This finding is consistent with that reported earlier among the general elderly (without PD; Herman et al. 2010). Among subjects with PD, lower executive function and attention scores were previously associated with increased gait variability (Yogev et al. 2005), a gait measure that has been related to fall risk (Hausdorff et al. 2001; Hausdorff 2009; Verghese et al. 2009). The present results also point to a trend, similar to that seen in the general elderly population e.g., by Menant et al. (Menant et al. 2010), that visual spatial deficits are associated with fall risk in PD, at least among patients with relatively advanced disease (i.e., suffering from motor response fluctuations). Together, this constellation of findings suggests that specific cognitive deficits exacerbate the risk of falls among patients with PD.
Differential effect of dual tasking on gait in fallers
Almost without exception, gait measures were worse among the fallers when compared to non-fallers across all walking conditions (recall Fig. 1). These differences did not always reach statistically significant levels, perhaps due to the conservative statistical approach we employed (i.e., Bonferroni adjustments) and the relatively small number of subjects in each group, which limited the statistical power of the study. At the same time, even with these constraints, the differential effect of DT on fallers stood out and was expressed as a relatively stronger deterioration of bilateral coordination of gait already in the DT_S3 condition (Fig. 1e). A significant Group X Task interaction was also seen for gait variability measures (i.e., Swing_CV) when comparing the usual walking with the DT_S3 conditions. Further inspection of Fig. 1 suggests that in fallers, but not in non-fallers, there is a trend for relatively stronger expression in of the DT effect already in the DT_S3 trial. Even when the concurrent cognitive task becomes more difficult (i.e., S7 vs. S3), only minimal further deterioration in gait features occurs in the fallers. For the non-fallers, on the other hand, gait continues to deteriorate between the DT_S3 and the DT_S7 conditions. One of the limitations of this study, that restricts our ability to fully interpret this observation, is that the performance of the concurrent cognitive task was not recorded and scored (e.g., number of counts, number of errors). Nonetheless, this paradoxical finding, i.e., that among fallers, the extent to which gait measures are altered in DT is apparently fully expressed in the ‘easier’ task (i.e., DT_S3) suggests that non-fallers seem to ‘restrain’ the level of gait deterioration with respect to the level of the concurrent cognitive load, exhibiting higher flexibility of the central nervous system to negotiate the DT conditions and to allocate compensatory resources to the competing tasks. Fallers, on the other hand, lack this flexibility. Without a healthy control group, we cannot unambiguously determine whether this observation is unique among PD fallers. Still, a previous study in which different levels of DT difficulty were introduced to elderly subjects (fallers vs. non-fallers) did not observe this ‘saturation’ of the DT effect in older adult fallers (Springer et al. 2006). While not definitive, this comparison suggests that specifically PD fallers inappropriately respond to the relatively simple DT.
What increases fall risk in PD?—clinical implications
The pharmacological treatment of patients with PD is aimed at maximizing the time with optimal function (i.e., “ON” state). The significant impact of DT on gait in PD during the “ON” state, especially on gait features that were previously related to falls in PD, e.g., gait rhythmicity (Latt et al. 2009b; Hausdorff 2009), can therefore partially explain the high risk of falling, even in this optimally medicated condition. It seems therefore that these patients function under paradoxical terms. On one hand, they tend to increase their mobility, perhaps with simultaneous additional activities, due to the subjective feeling of “ON”, and on the other hand, the exposure to the effects of DT on stability, in regular or transient conditions, e.g., backward stepping (Hackney and Earhart 2009), increase their risk to fall. This aspect should be considered when developing appropriate treatment plans for fall risk among patients with PD. It appears that patients should be informed, treated, and perhaps specifically instructed how to avoid falls, taking into an account the specific functional disturbances in the “ON” medication state.
In recent years, several therapeutic interventions have been developed to improve gait and postural stability in PD even in the presence of DT (Brauer and Morris 2010; Mirelman et al. 2011; Yogev-Seligmann et al. 2010). These interventions attempt to enhance the patient’s ability to negotiate DT conditions and increase the flexibility in the allocation of the control of resources to the gait and cognitive tasks. While questions remain about the efficacy of these interventions, the present study supports the rationale behind them and suggests that interventions that reduce the DT effects on gait will help to reduce the risk of falls among patients with advanced PD as they carryout their activities of daily living during the “ON” medication state.
The present study has several limitations. For example, inclusion of a healthy control group, a larger sample size, and prospective study would increase the robustness and interpretability of the findings. Nonetheless, the differential DT effects observed when comparing recurrent fallers to non-fallers were highly significant, providing support for the key findings of the study. A larger-scale, prospective study would be helpful for confirming the results. Still, results of the present study suggest that DT gait abilities are associated with an increased risk of falls in patients with PD.
References
Adkin AL, Frank JS, Jog MS (2003) Fear of falling and postural control in Parkinson’s disease. Mov Disord 18:496–502
Alexander NB, Hausdorff JM (2008) Linking thinking, walking, and falling. J Gerontol A Biol Sci Med Sci 63:1325–1328
Allcock LM, Rowan EN, Steen IN, Wesnes K, Kenny RA, Burn DJ (2009) Impaired attention predicts falling in Parkinson’s disease. Parkinsonism Relat Disord 15:110–115
Baltadjieva R, Giladi N, Gruendlinger L, Peretz C, Hausdorff JM (2006) Marked alterations in the gait timing and rhythmicity of patients with de novo Parkinson’s disease. Eur J Neurosci 24:1815–1820
Bloem BR, Hausdorff JM, Visser JE, Giladi N (2004) Falls and freezing of gait in Parkinson’s disease: a review of two interconnected, episodic phenomena. Mov Disord 19:871–884
Brauer SG, Morris ME (2010) Can people with Parkinson’s disease improve dual tasking when walking? Gait Posture 31:229–233
Camicioli R, Oken BS, Sexton G, Kaye JA, Nutt JG (1998) Verbal fluency task affects gait in Parkinson’s disease with motor freezing. J Geriatr Psychiatry Neurol 11:181–185
Cheng EM, Tonn S, Swain-Eng R, Factor SA, Weiner WJ, Bever CT Jr (2010) Quality improvement in neurology: AAN Parkinson disease quality measures: report of the quality measurement and reporting subcommittee of the American academy of neurology. Neurology 75:2021–2027
Coppin AK, Shumway-Cook A, Saczynski JS, Patel KV, Ble A, Ferrucci L, Guralnik JM (2006) Association of executive function and performance of dual-task physical tests among older adults: analyses from the InChianti study. Age Ageing 35:619–624
Doniger GM, Zucker DM, Schweiger A, Dwolatzky T, Chertkow H, Crystal H, Simon ES (2005) Towards practical cognitive assessment for detection of early dementia: a 30-minute computerized battery discriminates as well as longer testing. Curr Alzheimer Res 2:117–124
Doniger GM, Dwolatzky T, Zucker DM, Chertkow H, Crystal H, Schweiger A, Simon ES (2006) Computerized cognitive testing battery identifies mild cognitive impairment and mild dementia even in the presence of depressive symptoms. Am J Alzheimers Dis Other Demen 21:28–36
Dwolatzky T, Whitehead V, Doniger GM, Simon ES, Schweiger A, Jaffe D, Chertkow H (2003) Validity of a novel computerized cognitive battery for mild cognitive impairment. BMC Geriatr 3:4
Dwolatzky T, Whitehead V, Doniger GM, Simon ES, Schweiger A, Jaffe D, Chertkow H (2004) Validity of the Mindstreams computerized cognitive battery for mild cognitive impairment. J Mol Neurosci 24:33–44
Fahn S, Elton R, Members of the UPDRS Developmental Committee (1987) Unified Parkinson’s disease rating scale. In: Fahn S (ed) Recent developments in Parkinson’s disease. MacMillan Healthcare Information, Florham Park, pp 153–163
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Gelb DJ, Oliver E, Gilman S (1999) Diagnostic criteria for Parkinson disease. Arch Neurol 56:33–39
Hackney ME, Earhart GM (2009) The effects of a secondary task on forward and backward walking in Parkinson’s disease. Neurorehabil Neural Repair. [Epub ahead of print]
Hausdorff JM (2009) Gait dynamics in Parkinson’s disease: common and distinct behavior among stride length, gait variability, and fractal-like scaling. Chaos 19:026113
Hausdorff JM, Cudkowicz ME, Firtion R, Wei JY, Goldberger AL (1998) Gait variability and basal ganglia disorders: stride-to-stride variations of gait cycle timing in Parkinson’s disease and Huntington’s disease. Mov Disord 13:428–437
Hausdorff JM, Rios D, Edelberg HK (2001) Gait variability and fall risk in community-living older adults: a 1-year prospective study. Arch Phys Med Rehabil 82:1050–1056
Hausdorff JM, Balash J, Giladi N (2003a) Effects of cognitive challenge on gait variability in patients with Parkinson’s disease. J Geriatr Psychiatry Neurol 16:53–58
Hausdorff JM, Schaafsma JD, Balash Y, Bartels AL, Gurevich T, Giladi N (2003b) Impaired regulation of stride variability in Parkinson’s disease subjects with freezing of gait. Exp Brain Res 149:187–194
Hausdorff JM, Doniger GM, Springer S, Yogev G, Giladi N, Simon ES (2006) A common cognitive profile in elderly fallers and in patients with Parkinson’s disease: the prominence of impaired executive function and attention. Exp Aging Res 32:411–429
Hely MA, Morris JG, Traficante R, Reid WG, O’Sullivan DJ, Williamson PM (1999) The sydney multicentre study of Parkinson’s disease: progression and mortality at 10 years. J Neurol Neurosurg Psychiatry 67:300–307
Herman T, Mirelman A, Giladi N, Schweiger A, Hausdorff JM (2010) Executive control deficits as a prodrome to falls in healthy older adults: a prospective study linking thinking, walking, and falling. J Gerontol A Biol Sci Med Sci 65:1086–1092
Hoehn MM, Yahr MD (1967) Parkinsonism: onset, progression and mortality. Neurology 17:427–442
Kalron A, Dvir Z, Achiron A (2010) Walking while talking–difficulties incurred during the initial stages of multiple sclerosis disease process. Gait Posture 32:332–335
Kerr GK, Worringham CJ, Cole MH, Lacherez PF, Wood JM, Silburn PA (2010) Predictors of future falls in Parkinson disease. Neurology 75:116–124
Latt MD, Lord SR, Morris JG, Fung VS (2009a) Clinical and physiological assessments for elucidating falls risk in Parkinson’s disease. Mov Disord 24:1280–1289
Latt MD, Menz HB, Fung VS, Lord SR (2009b) Acceleration patterns of the head and pelvis during gait in older people with Parkinson’s disease: a comparison of fallers and nonfallers. J Gerontol A Biol Sci Med Sci 64:700–706
Menant JC, St George RJ, Fitzpatrick RC, Lord SR (2010) Impaired depth perception and restricted pitch head movement increase obstacle contacts when dual-tasking in older people. J Gerontol A Biol Sci Med Sci 65:751–757
Mirelman A, Gurevich T, Giladi N, Bar-Shira A, Orr-Urtreger A, Hausdorff JM (2011) Gait alterations in healthy carriers of the LRRK2 G2019S mutation. Ann Neurol (in press)
Mirelman A, Maidan I, Herman T, Deutsch J, Giladi N, Hausdorff JM (2011) Virtual reality for gait training: can it induce motor learning to enhance complex walking and reduce fall risk in patients with Parkinson’s disease? J Gerontol Med Sci 66:234–240
Pickering RM, Grimbergen YA, Rigney U, Ashburn A, Mazibrada G, Wood B, Gray P, Kerr G, Bloem BR (2007) A meta-analysis of six prospective studies of falling in Parkinson’s disease. Mov Disord 22:1892–1900
Plotnik M, Giladi N, Balash Y, Peretz C, Hausdorff JM (2005) Is freezing of gait in Parkinson’s disease related to asymmetric motor function? Ann Neurol 57:656–663
Plotnik M, Giladi N, Hausdorff JM (2007) A new measure for quantifying the bilateral coordination of human gait: effects of aging and Parkinson’s disease. Exp Brain Res 181:561–570
Plotnik M, Dagan Y, Gurevich T, Giladi N, Hausdorff JM (2011) Effects of cognitive function on gait and dual tasking abilities in patients with Parkinson’s disease suffering from motor response fluctuations. Exp Brain Res 208:169–179
Plummer-D’Amato P, Altmann LJ, Saracino D, Fox E, Behrman AL, Marsiske M (2008) Interactions between cognitive tasks and gait after stroke: a dual task study. Gait Posture 27:683–688
Podsiadlo D, Richardson S (1991) The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 39:142–148
Rochester L, Hetherington V, Jones D, Nieuwboer A, Willems AM, Kwakkel G, Van Wegen G (2005) The effect of rhythmical cues on walking during a simple and dual functional motor task in a complex environment in people with Parkinson’s disease. Arch Phys Med Rehabil 86:999–1006
Sato Y, Fujimatsu Y, Kikuyama M, Kaji M, Oizumic K (1998) Influence of immobilization on bone mass and bone metabolism in hemiplegic elderly patients with a long-standing stroke. J Neurol Sci 156:205–210
Sheridan PL, Hausdorff JM (2007) The role of higher-level cognitive function in gait: executive dysfunction contributes to fall risk in Alzheimer’s disease. Dement Geriatr Cogn Disord 24:125–137
Spielberger C, Gorusch R (1983) Self-evaluation questionnaire (form Y). Manual for the State-Trait Anxiety Inventory
Springer S, Giladi N, Peretz C, Yogev G, Simon ES, Hausdorff JM (2006) Dual-tasking effects on gait variability: the role of aging, falls, and executive function. Mov Disord 21:950–957
van der Bootsma WA, Gussekloo J, de Craen AJ, van Exel E, Bloem BR, Westendorp RG (2003) Walking and talking as predictors of falls in the general population: the Leiden 85-plus study. J Am Geriatr Soc 51:1466–1471
van Iersel MB, Kessels RP, Bloem BR, Verbeek AL, Olde Rikkert MG (2008) Executive functions are associated with gait and balance in community-living elderly people. J Gerontol A Biol Sci Med Sci 63:1344–1349
Verghese J, Holtzer R, Lipton RB, Wang C (2009) Quantitative gait markers and incident fall risk in older adults. J Gerontol A Biol Sci Med Sci 64:896–901
Yang YR, Chen YC, Lee CS, Cheng SJ, Wang RY (2007) Dual-task-related gait changes in individuals with stroke. Gait Posture 25:185–190
Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, Leirer VO (1982) Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res 17:37–49
Yogev G, Giladi N, Peretz C, Springer S, Simon ES, Hausdorff JM (2005) Dual tasking, gait rhythmicity, and Parkinson’s disease: which aspects of gait are attention demanding? Eur J Neurosci 22:1248–1256
Yogev G, Plotnik M, Peretz C, Giladi N, Hausdorff JM (2007) Gait asymmetry in patients with Parkinson’s disease and elderly fallers: when does the bilateral coordination of gait require attention? Exp Brain Res 177:336–346
Yogev-Seligmann G, Hausdorff JM, Giladi N (2008) The role of executive function and attention in gait. Mov Disord 23:329–342
Yogev-Seligmann G, Rotem-Galili Y, Mirelman A, Dickstein R, Giladi N, Hausdorff JM (2010) How does explicit prioritization alter walking during dual-task performance? Effects of age and sex on gait speed and variability. Phys Ther 90:177–186
Acknowledgments
We thank the patients and staff of the Movement Disorders Unit at the Tel Aviv Sourasky Medical Center for invaluable assistance. We thank Dr. Jennifer Srygley and Mr. Leor Grundlinger for their help with data handling. This study was supported in part by grants from the Tel Aviv Sourasky Medical Center Grant of Excellence, by the Parkinson’s disease Foundation (PDF), the National Parkinson’s Foundation (NPF) and by the Israeli Ministries of Health and Veteran Affairs (Grant #3000004385). M. Plotnik acknowledges Dr. Jay Goldberg for inspiring his scientific work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Plotnik, M., Giladi, N., Dagan, Y. et al. Postural instability and fall risk in Parkinson’s disease: impaired dual tasking, pacing, and bilateral coordination of gait during the “ON” medication state. Exp Brain Res 210, 529–538 (2011). https://doi.org/10.1007/s00221-011-2551-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00221-011-2551-0