Abstract
Dual task-related changes in gait are considered as a sensitive and a specific marker of adverse effects of cognitive impairment on the highest levels of gait control. No study has examined the longitudinal association between gait performance while dual tasking and the occurrence of cognitive decline. This study aims to examine the association of stride time parameters (i.e., mean value and coefficient of variation (CoV)) during single and dual tasking with the occurrence of cognitive decline in non-demented older community dwellers. A total of 56 non-demented community dwellers were recruited in a longitudinal prospective cohort study. Mini-Mental Status Examination (MMSE) scores at baseline assessment and at 5-year follow-up assessment, and mean value and CoV of stride time at self-selected usual pace, while usual walking and dual tasking (i.e., counting backward and verbal fluency task) at baseline assessment were recorded. Variation (i.e., delta) of MMSE score from baseline to follow-up assessment as well as of stride time parameters from single to dual task was used as outcomes. Worse stride time values were reported while dual tasking compared to single tasking (P < 0.03). An increase of mean value, CoV, and delta of CoV of stride time was associated with an increased delta MMSE while performing verbal fluency task (P < 0.05). Worsening stride time parameters while performing a verbal fluency task at baseline assessment was associated with decline in MMSE score during the 5-year follow-up period in this sample of older community dwellers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the past 10 years, an accumulation of data highlights the evidence that a strong relationship exists between gait and cognition in two specific ways (Beauchet et al. 2016; Allali et al. 2016; Seidler et al. 2010). First, an association has been identified with the changes in gait performance while dual tasking (Zijlstra et al. 2008; Chu et al. 2013; Montero-Odasso et al. 2012). The principle of dual task gait paradigm is to compare performance under routine conditions (i.e., walking without distractions) with performance under a challenging dual task condition (i.e., simultaneously executing an attention-demanding task) (Zijlstra et al. 2008). Changes in gait performance while dual tasking are usually interpreted as the interference due to competing demands for cognitive resources needed for both tasks (Montero-Odasso et al. 2012; Beauchet et al. 2009). Individuals with early cognitive decline such as mild cognitive impairment (MCI) have demonstrated high stride time variability, particularly under dual task conditions (Montero-Odasso et al. 2014; Beauchet et al. 2014). Second, a recent meta-analysis reported that low gait performance predicts the occurrence of dementia (Beauchet et al. 2016). The uniqueness of the association between gait and cognition is that it does not rely on a complex neuropsychological evaluation or laboratory investigations. Thus, it is easy to apply gait measure to predict outcomes in clinical scenarios while maintaining low costs among large populations. It also provides new perspectives in the field of secondary prevention of dementia, which is key to developing public health-related policies to counter the impressive growth of dementia.
No study has examined the longitudinal association between gait performance while dual tasking and the occurrence of cognitive decline. Dual task-related changes in gait are considered as a sensitive and a specific marker of adverse effects of cognitive impairment on the highest levels of gait control (Zijlstra et al. 2008; Chu et al. 2013; Montero-Odasso et al. 2012; Beauchet et al. 2009). Increased stride time (i.e., gait cycle duration) variability is also considered as the best biomarker to detect the consequences of cognitive impairment on the highest levels of gait control, high variability reflecting abnormal control and gait instability (Montero-Odasso et al. 2012; Beauchet et al. 2014; Montero-Odasso et al. 2014). Thus, we hypothesized that an increased stride time variability while dual tasking could be associated with the occurrence of cognitive decline in non-demented older adults. This study aims to examine the association of stride time parameters (i.e., mean value and coefficient of variation (CoV)) during single and dual tasking with the occurrence of cognitive decline in non-demented older community dwellers. Establishing the predictive value of gait parameters for cognitive decline could have various clinical implications in terms of prevention and management of dementia, and will improve our understanding of the cognitive substrates of the highest level of gait control.
Material and methods
Participants
A total of 56 non-demented older community dwellers (mean age 68.9 ± 0.5 years; 46.4% female) from the “PROgnostic indicator OF cardiovascular and cerebrovascular events” (PROOF) cohort were included in this prospective observational cohort study after having given their written informed consent for research. Sampling and data collection procedures of the PROOF study have been described elsewhere in details (Barthelemy et al. 2007). The subset of participants included in the current study was participants who received a baseline gait analysis and who had a 5-year follow-up assessment after the initial gait analysis. Inclusion criteria for the present analysis were at PROOF baseline assessment: age ≥ 65 years; absence of chronic conditions influencing gait variability (e.g., extrapyramidal rigidity of the upper limbs, neurological and psychiatric diseases, severe medical conditions affecting walking, inability to walk 15 min unassisted), no dementia; and Mini-Mental Status Examination (MMSE) score at baseline and at 5-year follow-up assessment (mean 4.8 ± 0.7 years). The number of participants required for this study has been calculated using a free sample size calculator (http://www.sample-size.net/) and using the following characteristics: type I error α (two-tailed) = 0.050, type II error β = 0.20 and standard deviation S(Δ) = 1.30. The calculated number of participants was n = 53.
Clinical assessment
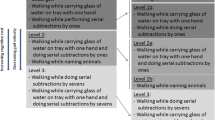
A full-standardized medical examination and quantitative gait assessment were performed in all participants at baseline and 5 years later (mean 4.8 ± 0.7 years). Mean value and CoV (CoV = (standard deviation/mean) × 100) of stride time were recorded at self-selected usual pace, while usual walking and dual tasking, using the SMTEC® footswitches system (SMTEC®, Sport & Medical Technologies SA, Nyon Switzerland). This system is highly reliable for measuring gait in non-demented and demented older adults (Beauchet et al. 2011; Beauchet et al. 2008). It includes a pair of innersoles fitted inside the participant’s shoes. Each innersole contains two independent footswitches, one placed at the heel and another at the toe, which are linked to a portable data recorder worn at the waist. Two different cognitive tasks were used: an arithmetic task (i.e., counting backward out loud starting from 50) and a verbal fluency task (i.e., enumerating out loud as many animal names as possible). These two tasks are attention-demanding tasks but involve different cognitive domains. The verbal fluency task relies on the semantic memory, whereas the counting backward task depends on working memory (Beauchet et al. 2005). The semantic and working memory domains may be affected separately or together at the onset of cognitive impairment caused by dementia likely Alzheimer disease or vascular dementia (Waldemar et al. 2007). Furthermore, it has been reported that the counting backward and verbal fluency tasks may worsen gait performances differently in cognitively healthy individuals, counting backward having a greater impact on gait variability compared to verbal fluency (Beauchet et al. 2005). There is no previous study that had examined, which changes in gait due to these two cognitive tasks are related to cognitive decline. Gait assessment was performed according to the European guidelines for spatio-temporal gait analysis in older adults (Kressig and Beauchet 2006). Briefly, participants were asked to walk at in a quiet, well-lit corridor wearing their own footwear. The participants performed one trial per walking condition. To avoid acceleration and deceleration effects, participants started walking one meter before reaching the 20-m walkway and completed their walk 1 m beyond it. The range of the time of ambulation was between 17 and 22 s (walking speed ranges between 0.9 and 1.2 m/s), and number of steps was between 9 and 14. Age, sex, height (cm), weight (kg), the number of drugs taken daily and educational level evaluated with the number of years of schooling and categorized by high school level (i.e., yes or not) were recorded.
Ethics
Participants in the study were included after having given their written informed consent for research. The study was conducted in accordance with the ethical standards set forth in the Helsinki Declaration (1983). Saint-Etienne local Ethical Committee, France, approved the study protocol.
Statistics
The participants’ characteristics were summarized using means and standard deviations or frequencies and percentages, as appropriate. For the current analysis, variation in MMSE score, called delta MMSE, was calculated from the formula (MMSE at baseline − MMSE at 5-year follow-up period / (MMSE at baseline + MMSE at 5-year follow-up period) / 2) × 100. Similar methods were used to calculate the variation (i.e., delta) of stride time parameters from single to dual task: (dual task − single task / (dual task + single task) / 2) × 100. Comparisons were performed with non-parametric Wilcoxon test. Uni- and multivariable linear regressions were performed to examine the association between change in MMSE score (i.e., delta MMSE used as dependent variable); and each stride time parameter (i.e., mean value, CoV, and delta used as independent variable) while usual walking and while dual tasking, adjusted on participant’s baseline characteristics. P values less than 0.05 were considered as statistically significant. All statistics were performed using SPSS (version 23.0; SPSS, Inc., Chicago, IL).
Results
Table 1 shows the participant’s baseline characteristics. There was a significant increase in mean value and CoV of stride time while dual tasking (P < 0.001 for backward counting and verbal fluency task) compared to usual walking. There was also a significant increase in mean value and CoV of stride time while performing verbal fluency task (P < 0.001 for mean and P = 0.029 for CoV) compared to counting back. The delta of CoV of stride time while counting backward (P < 0.001) and while performing the verbal fluency task (P < 0.001) was higher compared to the delta of mean value. MMSE score at 5-year follow-up assessment was significantly lower than MMSE score at baseline assessment (P < 0.001). The univariable linear regressions showed that increased CoV of stride time (P = 0.011) and increased delta CoV of stride time (P = 0.037) (i.e., worst gait performance) while performing the verbal fluency task were associated with increased delta MMSE (i.e., worst cognitive performance) (Table 2). The multiple linear regressions showed that increased mean value of stride time (i.e., worst gait performance) was associated with increased delta MMSE (i.e., worst cognitive performance) while usual walking (P = 0.041) and while performing the verbal fluency task (P = 0.049). In addition, while performing the verbal fluency task, increased CoV (P = 0.010) and increased delta CoV of stride time (P = 0.040) (i.e., worse gait performance) were associated with increased delta MMSE.
Discussion
The main findings of this study show that worsening stride time parameters while performing a verbal fluency task at baseline assessment, and in particular CoV of stride time was associated with decline in MMSE score during the 5-year follow-up period in the sample of older community dwellers recruited for the study.
To the best of our knowledge, this study is the first to report that dual task-related increase in stride time mean value and variability predicts cognitive decline. Cognition and locomotion are two human abilities controlled by the brain (Beauchet et al. 2016; Allali et al. 2016; Seidler et al. 2010; Zijlstra et al. 2008). Their decline is highly prevalent with physiological and pathological aging, and is greater than the simple sum of their respective prevalence, suggesting a complex age-related interplay between cognition and locomotion (Beauchet et al. 2016; Allali et al. 2016; Seidler et al. 2010). Both declines in cognition and locomotion are associated and the temporal nature of their association has been unclear for a long time (Beauchet et al. 2016; Seidler et al. 2010). Recently, a systematic review and meta-analysis has provided evidence that poor gait performance predicts dementia, suggesting that low gait performance is the first symptom of dementia (Beauchet et al. 2016). Our results underscore a specific association between increased stride time variability while dual tasking and decline in MMSE score. An increase in stride time variability reflects a poor gait performance and gait instability (Montero-Odasso et al. 2012; Beauchet et al. 2009). For instance, an association with high gait variability and falls in older adults has been previously reported (Maki 1997). Thus, our results are consistent with the recent meta-analysis. However, compared to previous studies, which have only examined gait performance while single tasking (i.e., usual walking), we reported in the present study changes in gait while dual tasking. These dual task-related gait changes underscore that impaired higher levels of gait control, demonstrated with increased gait variability while performing a verbal fluency task, predict cognitive decline. Dual task-related gait changes have previously been identified as a good predictor of adverse clinical outcomes, such as falls (Beauchet et al. 2009). Our study highlights a new aspect, which is related less to gait decline and more to cognitive decline. It suggests that the association of gait and cognitive impairment, which are highly prevalent with physiological and pathological aging, exceed the simple sum of their respective prevalences and evokes a complex age-related interplay between cognition and locomotion.
The second main finding of this study is that worsening of stride time parameters while performing the verbal fluency task at baseline was especially associated with the occurrence of cognitive decline. Two complementary explanations can be suggested. First, verbal fluency task provoked the highest increase in gait variability in the sample of individuals. It could be suggested that it overloads brain capacities due to its higher level of cognitive resources in comparison to counting backwards and, thus, may be more sensitive to detect an early abnormality (Seidler et al. 2010; Zijlstra et al. 2008; Montero-Odasso et al. 2012; Beauchet et al. 2009; Montero-Odasso et al. 2014; Beauchet et al. 2014). The second explanation may be related to the type of cognitive decline. Alzheimer disease (AD) is the main cause of dementia (World Alzheimer Report 2015). It has been previously reported that abnormal performance in this specific task was associated with the occurrence of AD (Fagundo et al. 2008). Thus, we suggested that this cognitive task may be more difficult to perform while walking compared to counting backward in early stages of the disease that leads to greater gait variability. Furthermore, as the highest value of the coefficient of regression, which shows the strength of the association between delta in MMSE and gait performance, has been reported with the CoV of stride time, it could be suggested that this gait characteristic represents the best measure to predict cognitive decline.
It is also important to consider that the deltas of stride parameters provide additional information regarding the association of the parallel gait and cognitive declines. Actually, only the delta of CoV of stride time, but not of the mean value of stride time, has been associated with the delta of MMSE (β = 0.022 while counting backward and β = 0.021 while performing the verbal fluency task) in our study. This result suggests that the change in CoV is more sensitive to change in cognition than the change in mean value. This finding is another illustration of the interest of studying variability of gait parameters that is considered as a marker of cerebral control of gait (Hausdorff 2005).
Our study also shows that increased mean values of stride time (i.e., worse gait performance) while usual walking were positively associated with increased delta MMSE (i.e., worst cognitive performance). This result may be due to the strong relationship between mean value of stride time and gait speed. As gait speed has been previously related to cognitive decline (Dubost et al. 2006), it could be suggested that mean value of stride time reflects low gait speed and, thus, has the same value in term of prediction of cognitive decline. A similar result has been reported with mean value of stride time while performing the verbal fluency task but this association may be taken with cautious as the P value was at the border of the significance (i.e., 0.049).
Although the strength of this study was designed to specifically examine a strong a priori hypothesis, some limitations need to be considered. First, due to the small number of participants and because this study is the first to demonstrate an association between greater stride time variability (i.e., worse performance) while dual tasking and decline in global cognitive functioning, the results should be taken with caution and confirmed on a higher number of individuals in a following longitudinal study. Second, the duration of the dual task condition was short compared to the duration of a cognitive task performed during a neuropsychological assessment. Indeed, the duration of verbal fluency task ranges between 1 and 2 min. It could be suggested that a shorter time leads to a relative better performance in terms of enumerated animal names or figures compared to the classical condition of testing because the difficulty of task increase with time; that could influence dual task-related gait performance. Third, walking speed may influence gait variability but there is a non-linear relationship between stride time variability and walking speed, with greater variability at slow walking speeds (0.2–0.6 m/s) compared to moderate walking speeds (0.8–1.4 m/s) (Heiderscheit 2000). All participants of our study had a normal walking speed between 0.9 and 1.2 m/s. Thus, the effect of walking speed is unlikely and limited. Fourth, we do not have an extended clinical and/or neuropathological confirmation of the disease status of the participants at 5-year follow-up assessment.
In conclusion, this study found that increased stride time values, and in particular variability while performing a verbal fluency task at baseline assessment, were associated with decline in cognitive performance during the follow-up period. These results confirm the strong relationship between gait and cognitive decline, and thus open new perspective in terms of prediction of dementia.
References
Allali G, Annweiler C, Blumen HM, Callisaya ML, De Cock AM, Kressig RW, Srikanth V, Steinmetz JP, Verghese J, Beauchet O (2016) Gait phenotype from mild cognitive impairment to moderate dementia: results from the GOOD initiative. Eur J Neurol 23:527–541
Barthelemy JC, Pichot V, Dauphinot V, Celle S, Laurent B, Garcin A, Kerleroux J, Lacour JR, Kossovsky M, Gaspoz JM, Roche F (2007) Autonomic nervous system activity and decline as prognostic indicators of cardiovascular and cerebrovascular events: the ‘PROOF’ study. Study design and population sample. Associations with sleep-related breathing disorders: the ‘SYNAPSE’ Study Neuroepidemiology 29:18–28
Beauchet O, Dubost V, Aminian K, Gonthier R, Kressig RW (2005) Dual-task-related gait changes in the elderly: does the type of cognitive task matter? J Mot Behav 37:259–264
Beauchet O, Herrmann FR, Grandjean R, Dubost V, Allali G (2008) Concurrent validity of SMTEC footswitches system for the measurement of temporal gait parameters. Gait Posture 27:156–159
Beauchet O, Annweiler C, Dubost V, Allali G, Kressig RW, Bridenbaugh S, Berrut G, Assal F, Herrmann FR (2009) Stops walking when talking: a predictor of falls in older adults? Eur J Neuro l16:786–795
Beauchet O, Freiberger E, Annweiler C, Kressig RW, Herrmann FR, Allali G (2011) Test-retest reliability of stride time variability while dual tasking in healthy and demented adults with frontotemporal degeneration. J Neuroeng Rehabil 8:37
Beauchet O, Allali G, Montero-Odasso M, Sejdić E, Fantino B, Annweiler C (2014) Motor phenotype of decline in cognitive performance among community-dwellers without dementia: population-based study and meta-analysis. PLoS One 9:e99318
Beauchet O, Annweiler C, Callisaya ML, De Cock AM, Helbostad JL, Kressig RW, Srikanth V, Steinmetz JP, Blumen HM, Verghese J, Allali G (2016) Poor gait performance and prediction of dementia: results from a meta-analysis. J Am Med Dir Assoc 17:482–490
Chu YH, Tang PF, Peng YC, Chen HY (2013) Meta-analysis of type and complexity of a secondary task during walking on the prediction of elderly falls. Geriatr Gerontol Int 13:289–97
Dubost V, Kressig RW, Gonthier R, Herrmann FR, Aminian K, Najafi B, Beauchet O (2006) Relationships between dual-task related changes in stride velocity and stride time variability in healthy older adults. Hum Mov Sci 25:372–82
Fagundo AB, López S, Romero M, Guarch J, Marcos T, Salamero M (2008) Clustering and switching in semantic fluency: predictors of the development of Alzheimer’s disease. Int J Geriatr Psychiatry 23:1007–1013
Hausdorff JM (2005) Gait variability: methods, modeling and meaning. J Neuroeng Rehabil 2:19
Heiderscheit BC (2000) Movement variability as a clinical measure for locomotion. J Appl Biomech 16:419–427
Kressig RW, Beauchet O (2006) Guidelines for clinical applications of spatio-temporal gait analysis in older adults. Aging Clin Exp Res 18:174–176
Maki BE (1997) Gait changes in older adults: predictors of falls or indicators of fear. J Am Geriatr Soc 45:313–320
Montero-Odasso M, Verghese J, Beauchet O, Hausdorff JM (2012) Gait and cognition: a complementary approach to understanding brain function and the risk of falling. J Am Geriatr Soc 60:2127–2136
Montero-Odasso M, Oteng-Amoako A, Speechley M, Gopaul K, Beauchet O, Annweiler C, Muir-Hunter SW (2014) The motor signature of mild cognitive impairment: results from the gait and brain study. J Gerontol A Biol Sci Med Sci 69:415–421
Seidler RD, Bernard JA, Burutolu TB, Fling BW, Gordon MT, Gwin JT, Kwak Y, Lipps DB (2010) Motor control and aging: links to age-related brain structural, functional, and biochemical effects. Neurosci Biobehav Rev 34:721–733
Waldemar G, Dubois B, Emre M, Georges J, McKeith IG, Rossor M, Scheltens P, Tariska P, Winblad B, EFNS (2007) Recommendations for the diagnosis and management of Alzheimer’s disease and other disorders associated with dementia: EFNS guideline. Eur J Neurol 14:e1–26
World Alzheimer Report 2015 The global impact of dementia: an analysis of prevalence, incidence, cost and trends Alzheimer: https://www.alz.co.uk/research/WorldAlzheimerReport2015.pdf
Zijlstra A, Ufkes T, Skelton DA, Lundin-Olsson L, Zijlstra W (2008) Do dual tasks have an added value over single tasks for balance assessment in fall prevention programs? A mini-review. Gerontology 54:40–49
Acknowledgments
The PROOF study group would like to thank all persons who took part in this study, in particular Mr. Gabin Ntougou Assoumou, Mrs. Judith Kerleroux, and Mrs. Magali Saint Martin. This study was supported by a grant from the French Minister of Health (Cellule Projet Hospitalier de Recherche Clinique National, Direction interrégionale de la Recherche Clinique, CHU Saint-Etienne; Appel d’Offre 1998 and Appel d’Offre 2002) and by Associations SYNAPSE and ONDAINE.
Author information
Authors and Affiliations
Contributions
Conceived and designed the experiments: OB, FR, and GA. Performed the experiments: OB, JCB, and FR. Analyzed the data: OB, CPL, and GA. Contributed reagents/materials/analysis tools: OB, JCB, FR, CLP, and AG. Wrote the paper: OB, CPL, JBC, FR, JC, EJL, and GA.
Corresponding author
Ethics declarations
Participants in the study were included after having given their written informed consent for research. The study was conducted in accordance with the ethical standards set forth in the Helsinki Declaration (1983). Saint-Etienne local Ethical Committee, France, approved the study protocol.
Conflict of interest
The authors declare that they have no conflicts of interest.
About this article
Cite this article
Beauchet, O., Launay, C.P., Sekhon, H. et al. Association of increased gait variability while dual tasking and cognitive decline: results from a prospective longitudinal cohort pilot study. GeroScience 39, 439–445 (2017). https://doi.org/10.1007/s11357-017-9992-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11357-017-9992-8