Abstract
We developed a method for the analysis of creatinine in dried blood spot (DBS) samples to facilitate monitoring of renal function in combination with TDM of immunosuppressive drugs for transplant patients outside the hospital. An 8-mm disc of the DBS was punched, extracted and followed by LC–MS/MS analysis. The haematocrit proved to have a significant influence on the analysis of creatinine in DBS samples. As potassium is a suitable marker for haematocrit, we implemented a method for measuring potassium in DBS and correct the creatinine for haematocrit. For both creatinine and K+ in DBS analytical and DBS, validation was performed, both components met the validation criteria and no other influences beside the haematocrit were detected. To assess the haematocrit correction, samples were compared to the ‘golden’ standard and plotted before and after correction. The correction showed a great improvement in agreement between the DBS assay and venous blood assay.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Creatinine (CRT) is a degradation product of the muscles generated at a constant rate, which is influenced by age, sex, race, muscle mass, weight and diet. CRT serum concentrations are used to estimate glomular filtration rates which is a parameter of the renal function. Monitoring of the CRT level is therefore mandatory when monitoring immunosuppressive drugs because acute rejection of a transplanted kidney or kidney damage caused by high levels of immunosuppressive drugs are of great medical importance and may also influence drug clearance. Information on the CRT plasma concentration along with the immunosuppressive drug concentrations is necessary for medical decision making. For this reason, the goal was to analyse CRT in the same analytical run as the earlier developed assay for immunosuppressive drugs [1].
Part of the method validation for CRT in dried blood spot (DBS) is the validation of DBS parameters, such as punch location, blood spot volume and haematocrit (HT). The HT influence was severe and could not be corrected by standardizing the HT of the calibration standards. This standardization is performed by calculation of the average HT of the patient pool and the preparation of the standards at this HT. With this method, the HT influence is also averaged and naturally the deviation should not exceed 15 %. This is the easiest and most used method to correct for the HT influence. The use of K+ to determine the HT was described by Capiau et al. [2]. As a marker, K+ is highly suitable; it is a stable endogenous component, easy to analyse and it is predominantly found in erythrocytes. The concentration of K+ in erythrocytes is approximately 30 times higher than in serum or plasma; the measured K+ is therefore directly proportional to the concentration of erythrocytes. In this paper, we describe the analysis of CRT in DBS and the necessary correction for HT by measurement of K+ as a marker in DBS samples.
Experimental
Chemicals
Creatinine (>98 %) and ammonium formate (AMF) (pro-analysis) were purchased from Sigma-Aldrich (Zwijndrecht, the Netherlands). Trifluoretic acid (TFA) (for synthesis), potassium chloride (for analysis) and ethanol (EtOH) (absolute for analysis) were purchased from Merck (Darmstadt, Germany). Methanol (MeOH) (HPLC Gradient) was purchased from Biosolve (Valkenswaard, the Netherlands). Creatinine-D3 was purchased from Bio-Connect (Huissen, the Netherlands). Reagents for potassium measurement: sample diluent, reference solution, calibration serum and cleaning fluid were all obtained from Abbott Diagnostics (Hoofddorp, the Netherlands). Surplus heparin whole blood was used to prepare K+ calibrators and quality control (QC) samples. Calibrators and QCs for CRT were prepared in Bio-Rad blank lyophilized serum and concentrated erythrocytes. The DBS paper was Whatman 903 sampling paper (Protein Saver Cards) and was purchased from GE Healthcare (Diegem, Belgium).
Apparatus
Analysis of DBS K+ was performed on the Architect Plus C4000 immunoassay analyser from Abbott (Hoofddorp, the Netherlands). System control and data acquisition and processing were performed with Architect software version 8.10. Analysis of CRT and its internal standard CRT-D3 in DBS samples was performed on a LC–MS/MS consisting of a 2795 Separation Module and a Quattro Micro Tandem Mass Spectrometer, both from Waters (Watford, UK). System control and data acquisition and processing were performed with MassLynx version 4.1 software. The CRT in plasma was determined at the Clinical Chemistry Laboratory (CCL), using the Modular P800 from Roche Diagnostics (Almere, the Netherlands). The HT in whole blood was also measured at the CCL, using a Cell-Dyn from Abbott. A Millipore® Synergy UV purifying system was used to obtain purified water (Millipore S.A.S., Molsheim, France). The hole puncher was developed for DBS analysis by the Department of Mechatronics Engineering of the Leiden University Medical Center (Leiden, the Netherlands). The Branson 3510 ultrasonic water-bath was purchased from VWR (Amsterdam, the Netherlands).
Architect C4000, Modular P800 and Cell-Dyn Sapphire
The Integrated Chip Technology (ICT) module of the Architect C4000 is capable of measuring Na+, K+ and Cl−. An electrical potential is measured by an ion-selective electrode utilizing ion-specific membranes.
The Modular P800 uses an enzymatic assay for the measurement of CRT. Creatinine is turned into creatine using creatininase. The creatine is then converted to sarcosin and ureum by creatinase. Through oxidizing the sarcosin, hydrogen peroxide is formed. The hydrogen peroxide is then mixed in a cuvette with reagents to form a coloured solution which is measured photometrically at a fixed wavelength.
The HT at the Cyll-Dyn is measured by determining the electrical impedance. Two electrodes are each placed at a side of an opening through which erythrocytes pass. With each cell passing the electrical current changes between the two electrodes. By counting the electric pulses, the amount of cells is registered.
LC–MS/MS analysis
Isocratic elution was obtained with a mixture of 35 % mobile phase A containing 0.02 % TFA and 5 mM AMF in purified water and 65 % mobile phase B containing 0.02 % TFA and 5 mM AMF in MeOH. The mixture was run at a flow rate of 0.5 mL/min on an XSelect™ HSS T3 XP analytical column, 3.0 × 100 mm, 2.5 μm which was kept at 50 °C. Total runtime was 4 min.
Mass spectrometric detection was performed in positive electrospray mode. The capillary voltage was 1.70 kV; the collision energy was 15 and 20 eV for CRT and CRT-D3, respectively. The (quantifier) mass transitions were m/z 114.0 → 85.9 and (qualifier) m/z 114.0 → 43.9 for CRT. The mass transition of CRT-D3 was m/z 117.0 → 46.9 for CRT-D3.
Standard and QC preparation
The standards and QCs for the K+ measurement were prepared by concentrating and diluting surplus heparin blood from daily routine analysis. The heparin blood was three times centrifuged during 10 min at 3000g. After centrifuging, the supernatant was removed and replaced with PBS buffer. After the third time, the concentrated erythrocytes were diluted with Bio-Rad blank serum to a specific HT. The HT of the standards and QCs was then measured in duplicate at the CCL with the Cell-Dyn Sapphire analyser. The concentrations of the standards were 0.18, 0.27, 0.31, 0.35, 0.40 and 0.44. The concentrations of the QCs were 0.16 (QC low), 0.33 (QC medium) and 0.44 (QC high). Different batches of pure substance were used to prepare standards and QCs for CRT. Favourably, the matrix of the standards and QCs is close to the matrix of patient samples. The use of surplus blood or blood from volunteers is therefore a common practice; however, this also means that it is difficult to obtain blood completely free of CRT because it is a endogenous component. Most of the CRT was removed from the erythrocytes with the washing procedure mentioned above and Bio-Rad blank serum was chosen to dilute the concentrated erythrocytes. Stock solutions for CRT were prepared in methanol, at concentrations of 4256 and 8258 μmol/L. Stock solution was added to the Bio-Rad blank serum to obtain concentrations of 20, 39, 77, 118, 239 and 478 μmol/L. For both CRT and K+, the lowest standard was used to determine the lower limit of quantification. The internal standard was prepared in methanol; the stock solution had a concentration of 431 μmol/L and was further diluted to a concentration of 4.31 μmol/L.
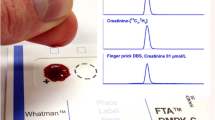
Sample preparation procedure
The sample preparation was derived from the earlier published sample preparation procedure for the analysis of immunosuppressive drugs in dried blood spots. In short, 250 μL EtOH and 250 μL IS was added to an 8-mm punched out disc. After short vortexing, the Eppendorf cups were placed in an ultrasonic water-bath for 10 min at 65 °C. The supernatant was then transferred to clean cups and evaporated at room temperature under dried nitrogen gas. The dried samples were reconstituted in 100 μL mobile phase v/v% 50/50. For the analysis of CRT, the dissolvation step was changed to 200 μL volume instead of 100 μL to enhance peak shape and linearity. A volume of 2 μL was injected on the LC–MS/MS. For the measurement of K+, 50 μL of the final sample volume was used. To obtain a concentration approximately in the middle of the validated range, the standard addition method was used. A solution with 5 mmol/L K+ was prepared and 100 μL of this solution was added to the 50 μL sample volume.
Validation
Both assays, LC–MS/MS and immunoassay, were validated according to our internal validation parameters. These parameters are derived from FDA guidelines for bioanalytical method validation, published work regarding matrix effects and published work regarding DBS validation (see also our earlier published work [1]).
Linearity
Linearity was determined by preparing three calibration curves and analysing the obtained data according ANOVA statistics, using regression software (BOSS Regres, Groningen). Data was first corrected for blank samples.
Matrix effects
The matrix effects were assessed according Matuszewski et al.; the slopes of post-extracted calibration curves were compared with neat calibration curves. The experiment was performed with six different batches of blank material. Any matrix effect should not exceed the 10.0 % limit and variation should not be more than 5.0 %.
Within- and between-run accuracy and precision
The experiment was performed by repeated (n = 6) analysis of the QCs. For the within-run accuracy and precision, analysis was performed during one analytical run. The between-run accuracy and precision were determined during six analytical runs. The obtained data was then tested for outliers with Dixon’s Q test. Per QC, level not more than one outlier should be detected. The accuracy and precision should be 85–115 % for QC low, medium and high. The accuracy and precision of the LLOQ had to be within 80–120 %.
Stability
The stability of the samples was tested for autosampler stability and long-term stability. The autosampler stability was determined by analysing the QC low and QC high in triplicate at t = 0 h; at the chosen time intervals, a new calibration curve was prepared and the QCs from t = 0 h were reanalysed. For K+, the samples remained in the sample area which is at room temperature; the CRT samples remained in the autosampler which was kept at 15 °C.
The long-term stability for K+ was determined by preparing fresh QC low and QC high samples; these QCs were than analysed and compared to the stored calibration curve. To determine the long-term stability of CRT, a fresh calibration curve was prepared after preparation of a fresh stock solution. Stored QC samples were then prepared and compared to the fresh calibration curve. For all stability tests, deviation of the nominal value should not exceed 15 %. Both CRT and K+ were stored in the refrigerator at a temperature of 4 °C.
Spot volume
The influence of the spot volume was tested by pipetting different volumes of blood on the paper and analysing the punched out discs from the centre. The chosen concentrations were at QC low and QC high levels, 70 and 174 mmol/L, respectively. The influence was accepted when the accuracy was within 85–115 %.
Punch location
This parameter was validated by pipetting 50 μL on the paper and punching out near the perimeter and in the centre of the formed spot. The influence was accepted when the accuracy was within 85–115 %; the concentrations of the samples were at QC low and QC high levels, 70 and 174 mmol/L, respectively.
HT influence
Analysis of this influence was performed by preparing samples with concentrations of 40 and 80 mmol/L at a variable HT. The HT values were chosen in accordance with the average, lowest and highest HT of the patient population as described in earlier published work [1]. The QC samples were analysed and compared with the QC sample with a HT of 0.35. The accuracy of all samples should be within 85–115 %.
HT correction for the analysis of CRT
To assess the potential of the HT correction, an experiment was set up with surplus heparin blood from TDM. The surplus heparin blood was divided into three portions; the first two portions were used to determine the CRT and HT in whole blood at the CCL. The third and last portion was used to prepare DBS samples at our own laboratory. The DBS sample is used to analyse the CRT in DBS on the LC–MS/MS and the HT in DBS, using K+ as a marker on the Architect C4000. To analyse the exact deviation per HT, a calibration curve with a fixed CRT concentration, but with an increasing HT, was determined on the LC–MS/MS. This calibration curve had a CRT concentration of 79.4 μmol/L. The increasing HT was 0.18, 0.27, 0.31, 0.35, 0.40 and 0.44. The HT–CRT calibration curve was then used to calculate the percentage deviation at the determined HT in DBS. The obtained correction factor was used to correct the determined CRT in DBS.
The corrected CRT in DBS was compared to the ‘golden standard’, the CRT and HT in whole blood. The data (n = 20) was tested for outliers using Grubb’s test; homoscedasticity was tested with a mountain plot, and assay agreement was tested using Passing & Bablok and Bland–Altman plots.
Results and discussion
Results analytical validation
The results of the analytical validation are all within the desired limits as shown in Table 1. The CRT and K+ both proved to be linear, as shown by the GOF and LOF. In Table 1, the calculated GOF and LOF (GOFexp and LOFexp) are presented with the corresponding degrees of freedom (ν) between brackets. The matrix effect was also within limits due to the deuterized internal standard which eluted at the same time as CRT. The within- and between-run accuracy and precision were for both components well within limits. The autosampler stability for K+ was determined by preparing a calibration curve and QC samples (QC low and QC high) at t =0 h and immediate analysis. Both standards and QCs remained in the sampling area of the Architect C4000 and were reanalysed with a fresh prepared calibration curve. This process was performed after 3.5 and 23 h; results from these tests showed a maximum autosampler stability of 3.5 h. The recovery of the QC samples prepared at t = 0 h compared to the fresh prepared calibration curve was admittedly around 200 % (data not shown), but compared to the calibration curve, also prepared at t = 0 h, the recovery was well within limits. The increased recovery after 3.5 h can be explained by evaporation of the samples because the autosampler area is not cooled. Though 3.5 h is a short period, analysis of K+ requires little time (minutes) and is more than enough for multiple reanalysis if necessary. The autosampler stability of CRT was determined after 5 h. Both QC low and QC high were within the desired limits, compared to a fresh prepared calibration curve.
The long-term stability was determined after 200 days for K+ and 382 days for CRT. For both components, the long-term stability was within the desired limits.
Results DBS validation
The results of the DBS validation are shown in Table 2. Both the spot volume and punch location did not prove to have influence on the assay accuracy. For both, all results are well within 90–110 %. The influence of the HT however was significant. Deviation from the nominal value was more than 15 %, especially at the low HT.
Results method comparison
The results of the method comparison are shown in Table 3 and Fig. 1. The results in Table 3 show that the analysis of the HT in DBS and blood are highly comparable. The confidence interval (CI) of both the slope and intercept is in accordance to there respective limits. The Bland–Altmann showed that HT measured in DBS is slightly higher than measured in whole blood. It is not clear how this difference is caused.
Graphics of the method comparison. Annotations a, c and e show the Passing & Bablok graphs of the HT, DBSuncorrected and DBScorrected measurements. The lighter line, the identity line, is the line which is drawn when two methods do not differ. Panels b, d and f show the Bland and Altmann plots. The bold dotted lines indicate the high and low variance of the results, while the light dotted line represents two methods which do not differ. Panel g is the mountain plot, when two methods are equal the top of the mountain centres over zero. The mountain of the open circles represents the uncorrected data; the mountain of the grey squares represents the corrected data. HT_DBS is the HT measured in DBS samples, HT_CCL and CRT_CCL is the HT or CRT measured at the Clinical Chemistry Laboratory, CRT_DBS uncorr is the CRT measured in DBS samples not corrected for the HT, CRT_DBS corr is the CRT measured in DBS samples corrected for the HT
As can be seen in Table 3, there is a clear difference in slope when the CRT in DBS is corrected for the HT. For both, no constant difference is detected using Passing &Bablok, but without correction, a proportional difference is detected. After correction, the proportional difference is no longer detected and the slope is significantly closer to 1.000. This is also clearly visible in Fig. 1c, e; after correction, the line of the method comparison is much closer to the identity line. In addition, the Bland–Altmann plots show that the mean difference is much smaller when correcting, while the variance in differences remains comparable. Most importantly, the identity line of Fig. 1d is outside the CI, while the identity line of Fig. 1f is inside the CI, meaning there is no significant bias.
The combined mountain plot of the uncorrected and corrected CRT in DBS shows that for both methodologies, the variances are distributed normally. It is also visible that the mountain of the corrected CRT is much more centred over zero than the uncorrected CRT. This means that the correspondence between the two assays is much better when correcting for the HT.
Conclusion
In this paper, we present a method to correct for the HT influence using K+ as a marker. Initially, the assay was developed to be able to measure CRT in DBS to optimize TDM of immunosuppressive drugs. Unfortunately, it was not possible to add the analysis of CRT to the same analytical run as the DBS of the immunosuppressive drugs assay. This was due to a high LLOQ for the immunosuppressive drugs. It is however our expectation that analysis of the immunosuppressive drugs and CRT can be done simultaneously in the future due to developments in LC–MS/MS equipment.
For both CRT and K+, all validation parameters were well within the desired limits. Compared to the assay developed by Capiau et al., the results of the K+ validation are similar. The DBS validation did not show an influence of the punch location and the spotted volume. The only difference is the result of the method comparison; the assay reported in this article has a positive bias for the HT measured in DBS, while Capiau et al. found a negative bias. This was explained by the difference in EDTA whole blood and heparin whole blood. However, the difference reported in our assay is not the same and can therefore not be explained by the difference in blood. It remains unclear how this difference is caused.
Though it is a useful addition when measuring immunosuppressive drugs in DBS, the measurement of CRT in DBS is not yet a common use. As reported by Keevil et al., the correlation between venous blood and fingerprick blood of CRT is high [3]. In spite of these reasons, only Koop et al. have reported an assay for CRT in DBS and tacrolimus in DBS [4]. The results were comparable to the reported assay in this article, although a different type of paper was used; the measured CRT in DBS was overall higher compared to whole blood. Furthermore, no investigation of the influence of the HT was performed, which also resulted in a proportional bias as reported by the authors.
The analytical validation was well within the desired limits as was the DBS validation. The method comparison showed the potential of the HT correction for the measurement of CRT in DBS. Furthermore, compared to the work of Koop et al., the results were highly comparable; a slightly higher CRT in DBS was reported, and without correction, a proportional bias was detected [4].
The developed assay is the first assay where correction for HT by K+ as a marker is implemented and shown to be mandatory for routine analysis when measuring CRT in DBS. For future analysis of DBS, where the influence of the HT is significant, the analysis of K+ is a promising method.
References
den Burger JC, Wilhelm AJ, Chahbouni A, Vos RM, Sinjewel A, Swart EL (2012) Anal Bioanal Chem 404:1803–1811
Capiau S, Stove VV, Lambert WE, Stove CP (2013) Anal Chem 85:404–410
Keevil BG (2011) Clin Biochem 44:110–118
Koop DR, Bleyle LA, Munar M, Cherala G, Al-Uzri A (2013) J Chromatogr B Analyt Technol Biomed Life Sci 926:54–61
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
den Burger, J.C.G., Wilhelm, A.J., Chahbouni, A.C. et al. Haematocrit corrected analysis of creatinine in dried blood spots through potassium measurement. Anal Bioanal Chem 407, 621–627 (2015). https://doi.org/10.1007/s00216-014-8291-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00216-014-8291-9