Abstract
In recent years, drug-facilitated crime (DFC) has become an increasing problem. A minimum list of 80 analytes to be monitored in such cases has been proposed by the Society of Forensic Toxicologists (SOFT) including the recommended minimum performance limits (RMPL). In the present study, two liquid chromatography-tandem mass spectrometry-based screening procedures, one in positive (method I) and one in negative (method II) electrospray ionization mode were developed and validated. Gradient elution was performed on a ZORBAX Eclipse XDB-C18 column after protein precipitation of the urine samples. Detection was carried out in the scheduled multiple reaction monitoring (MRM) mode monitoring two transitions per compound. A total of 100 analytes (91 basic in method I and nine acidic in method II) could be identified using the described procedure. No interferences were observed in 30 tested blank urine samples. The RMPLs were achieved for all analytes and ranged from 1 ng/mL for fentanyl to 10 μg/mL for γ-hydroxybutyrate (GHB). Matrix effects (ME) were evaluated using the same 30 urine samples and ranged from −90 % for tetrazepam to >6,000 % for the 11-nor-9-carboxy-tetrahydrocannabinol (THC-COOH). The relative standard deviations of ME were below 25 % for the vast majority of analytes. Results for urine specimens from nine authentic DFC cases were always negative with exception of drugs prescribed to the victims. Reanalysis with the developed procedure of 24 urine samples, with a positive screening result during routine clinical toxicology analysis, confirmed the routine findings. In an excretion study after a single oral doxylamine dose (30 mg), the parent drug and its nor metabolite could be detected in urine specimens from a young female volunteer for 10 days. The developed procedure allows a selective and sensitive screening of urine samples for almost all recommended analytes relevant in DFC cases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent years, the problem of the so-called drug-facilitated crimes (DFC), i.e., criminal offenses in which the victims’ control over their own actions and/or their ability to resist are compromised by drug effects, have received increasing attention among forensic experts as well as the public media. By far, the most notorious DFC is drug-facilitated sexual assault (DFSA). It is defined as a nonconsensual sexual act whereby the victim is incapacitated or unconscious due to the effects of alcohol and/or drugs [1] and often occurs in a “date-rape” setting. Precise epidemiologic data do not exist, and the number of unreported cases is estimated to be high [2]. Many victims do not report the incidents to the police or a physician because of anxiety, feelings of shame and guilt, and/or anterograde amnesia [3]. In an epidemiologic study in Great Britain in 2002, a total of 1,014 suspected DFSA cases were examined, but DFSA could only be verified in 21 of these cases (2 %) [4]. For Germany, data exist, for example, for the Institute of Forensic Medicine in Bonn, where 40 to 50 suspected DFSA cases per year were registered in the mid-2000s [5]. Benzodiazepines, sedative agents, and antihistamines were the most common substances detected in this study.
The drugs relevant in the context of DFC/DFSA are often referred to as “knock-out drugs.” They can be divided into sedative-hypnotic and stimulating substances. Sedative-hypnotic drugs cause drowsiness or unconsciousness, impairment of judgment, and a change of the victims’ behavior [2], leaving them in a helpless situation exploited by the offender. Depending on the administered substance, victims describe symptoms like dizziness, confusion, hypotension, muscle relaxation, nausea, and vomiting [2]. A further relevant effect of sedative-hypnotic knock-out drugs in DFC/DFSA is a dose-dependent anterograde amnesia starting with the onset of action of such drugs [2, 3] that is not necessarily associated with the unconsciousness of the victim [6]. In contrast to sedative-hypnotic substances, stimulating drugs such as cocaine, marijuana, amphetamine, and ecstasy lead to disinhibition and elevate the victim’s sexual desire [2, 4].
Besides alcohol [7], the drugs that are most often mentioned in the context of DFC/DFSA are γ-hydroxybutyrate (GHB), flunitrazepam (Rohypnol®), and ketamine, but there is a great variety of other substances misused for this purpose as well, especially for DFSA [4]. These can be benzodiazepines, so-called Z-drugs (zolpidem, zopiclone, zaleplone), H1-antihistamines, antipsychotics, opiates, common drugs of abuse, or central muscle relaxants. Toxicological analysis in DFC/DFSA cases must consider that the analyte concentrations in biological samples may be very low, because of the high potency and/or short elimination half-lives of some potential knock-out drugs as well as the time delay of often many hours or even days between incident and sampling. Mostly blood and urine are chosen as sample matrices and to be obtained as soon as possible after the incident [7]. For screening, the collection of at least 10 mL of blood, citrate-free, within 24 h has been recommended [7]. For urine samples, the detection windows are generally much longer than that in blood and may range up to 96 h [8]. Furthermore, urine may contain both the parent drug and its metabolites and can be collected noninvasively [9]. Therefore, the combination of blood and urine specimens should be considered. If there is a very long time delay between the incident and sampling or a suspicion of chronic abuse, the analysis of hair has been recommended [10]. The Society of Forensic Toxicologists (SOFT) DFSA Committee has published a list with 80 analytes including drugs and metabolites relevant in DFC/DFSA cases with the recommended minimum performance limits (RMPLs) for urine specimens [11].
Many different approaches to toxicological analysis, using gas chromatography-mass spectrometry (GC-MS), liquid chromatography-(tandem) mass spectrometry (LC-MS(/MS)) or immunoassays [12], in cases of suspected DFC/DFSA cases have been described in the literature. Immunoassays usually include only a small number of substances relevant in the context of DFC/DFSA, mainly benzodiazepines, cannabinoids, opiates, amphetamine, and cocaine. Positive immunoassay results have to be confirmed with other specific methods [13]. Furthermore, many commercially available immunoassays are not sufficiently sensitive to reliably detect the potentially low drug concentrations in this context. Several LC-MS(/MS)-based screening procedures for the analysis of urine samples have been described [14–17]. The advantage of using LC-MS(/MS) is the possibility for a direct determination of the analytes without chemical derivatization and the lower temperatures as needed in GC-based methods [17]. The methods of Birkler et al. [18], including 46 medicinal drugs, and of Vincenti et al. [19], analyzing 88 pharmaceutical drugs and metabolites, were developed using ultra-performance liquid chromatography-time of flight-MS and LC-MS/MS, respectively, for the analysis of blood. Ishida et al. analyzed 43 benzodiazepines, their metabolites, zolpidem, and zopiclone in plasma samples using LC-MS [20], but other drugs relevant in DFC/DFSA cases were not included in their method. A great number of 128 date-rape drugs in urine specimens using GC-electron ionization (EI)-MS has been published by Adamowicz and Kala [21], but the limits of detection (LODs) were in part well above the RMPLs recommended by the SOFT DFSA Committee [11]. Juhascik et al. [22] developed a GC-MS screening for urine samples for 30 substances of the list of the SOFT DFSA Committee. The remaining analytes had to be analyzed by another screening procedure. Finally, a review article by Brown et al. [9] summarized in detail several analytical methods employing different biological matrices, but the analyte spectrum covered was limited to club drugs.
The above overview shows that the analytical methods currently available in the literature either use blood instead of the recommended matrix urine, only cover a subset of the analytes relevant in the context of DFC/DFSA, or are not sufficiently sensitive to reliably detect the analytes at the RMPLs recommended by the SOFT DFSA Committee. Therefore, the aim of the presented study was the development and validation of a simple, sensitive, and selective LC-MS/MS procedure for simultaneous screening of a total of 100 analytes relevant in DFC/DFSA cases in urine. The analyte spectrum was supposed to include the list of the SOFT DFSA Committee and additional drugs and metabolites relevant in DFC/DFSA cases in Germany.
Experimental
Chemicals
With exception of nordoxylamine, the drug and metabolite standards were obtained from EDQM (Strasbourg, France), LGC Standards (Wesel, Germany), Lipomed (Weil am Rhein, Germany), Pfizer Deutschland (Berlin, Germany), Sigma-Aldrich Chemie (Steinheim, Germany), and Sigma-Aldrich Laborchemikalien (Seelze, Germany). Nordoxylamine was produced by in vitro biotransformation of doxylamine using the fungus Cunninghamella elegans [23]. The enzyme β-glucuronidase from E. coli K (150 U/mg at 35 °C and pH 7) was obtained from Roche Deutschland (Grenzach-Wyhlen, Germany). Water (for chromatography), methanol (for gas chromatography), acetonitrile (gradient grade for liquid chromatography), and formic acid 98–100 % (ACS Reag. Ph. Eur., for analysis) were obtained from Merck (Darmstadt, Germany). Ammonium formate was ordered from Sigma-Aldrich Chemie (Steinheim, Germany).
Liquid chromatography-mass spectrometry
The samples were analyzed using an ABSciex QTrap 4000 tandem mass spectrometer (Darmstadt, Germany) coupled to a LC-20 liquid chromatography system including a degaser, autosampler, column oven, two binary pumps, and a communication bus module (Shimadzu, Jena, Germany). The LC-MS/MS system was controlled by the Software Analyst 1.5.
Separation was performed on a ZORBAX Eclipse XDB-C18 column (4.6 × 150 mm, 5 μm) from Agilent (Böblingen, Germany). The mobile phase consisted of 50 mM ammonium formate buffer plus 0.75 % formic acid (eluent A) and acetonitrile plus 0.1 % formic acid (eluent B). The column oven was set to 40 °C, and the autosampler temperature was 10 °C. Two gradient methods were developed, one for analytes detected in positive ionization mode (method I) and one for analytes detected in negative ionization mode (method II). Column equilibration was performed with starting conditions for 1 min for each method. Flow and gradient conditions were as follows.
For method I, the flow rate was kept constant at 1.4 mL/min throughout the run. Starting conditions were 10 % eluent B held until 2.0 min, 2.0–4.5 min to 15 % B, 4.5–6.0 min hold at 15 % B, 6.0–10.0 min up to 25 % B, held for 5 min, 15.0–28.0 min up to 30 % B, 28.0–40.0 min up to 72 % B, and 40.0–40.5 min to 90 % B. Column flushing was performed in an additional method (4.5 min), leading to a total run time of 45 min for one sample. For column flushing, gradient elution was performed starting with 90 % eluent B for 2.0 min. The amount of eluent B was decreased to 10 % in 0.5 min and kept for 2.0 min. The injection volume was 10 μL.
For method II, a flow gradient was applied starting with 1.4 mL/min. After 5 min, the flow was reduced to 1.0 mL/min in 0.1 min and was kept until the end. The gradient was programmed as follows: starting conditions 0 % B, 0–5.0 min up to 2.5 % B, 5.0–18.5 min to 55 % B, and 18.5–25.0 min to 90 % B, held for 1 min. Column flushing was performed in an additional method (4.0 min), leading to a total run time of 30 min for one sample. For column flushing, gradient elution was performed starting with 90 % eluent B for 1.5 min. The amount of eluent B was decreased to 0 % in 0.5 min and held for 2.0 min. The injection volume was 20 μL. The injector needle was purged after every injection for 60 s with a mixture of water and methanol of 50:50 (v/v).
Ionization was performed using the Turbo V ion spray source. Nitrogen was used as collision gas, and dried and cleaned air was used as curtain gas as well as source gas 1 and 2. Positive and negative ionization was used in methods I and II, respectively. The MS conditions for method I were as follows: curtain gas, 20 psi (138 kPa); collision gas, high; ion spray voltage, 5,500 V; source temperature, 450 °C; ion source gas 1, 55 psi (379 kPa); ion source gas 2, 50 psi (345 kPa); interface heater, on; and resolution of Q1 and Q3, 0.7 amu. For method II, the MS conditions were as follows: curtain gas, 20 psi (138 kPa); collision gas, high; ion spray voltage, −4,300 V; source temperature, 350 °C; ion source gas 1, 40 psi (276 kPa); ion source gas 2, 50 psi (345 kPa); interface heater, on; and resolution of Q1 and Q3, 0.7 amu. For both methods, the mass spectrometer was operated in scheduled multiple reaction monitoring (MRM) mode with a detection window of 120 s for each transition. The target scan time for method I was 5 s (486 cycles per run) and for method II, 1 s (1,560 cycles per run). The monitored transitions and their particular settings, declustering potential, entrance potential, collision energy, and collision exit potential were optimized for each analyte. They were determined using a 10 ng/mL (positive ionization) or 50 ng/mL (negative ionization) solution of the respective analytes in a 50:50 mixture (v/v) of eluents A and B. The analyte solutions were infused into ion spray source by a syringe pump, and settings were obtained using the automatic compound optimization feature of the software. The results were compared with those obtained manually. Two MRM transitions were chosen based on their intensity and structural information. The most abundant MRM transition was used as a target and qualifier 1 transition, and the other, as qualifier 2 transition. For the deuterated internal standards, only one MRM transition was monitored in compliance with reference [24]. All MRM transitions, analyte-specific settings, and retention times are summarized in Table 1 for the analytes detected with method I and in Table 2 for analytes of method II. For data evaluation Analyst 1.5 was used.
For analyte identification, both monitored transitions were required to be present with a signal-to-noise ratio (S/N) ≥3. In addition, the acceptance criteria for relative retention times and ratios of the monitored transitions as proposed by the Gesellschaft für Toxikologische und Forensische Chemie (GTFCh) [24] were applied.
Preparation of stock solutions
Stock solutions in appropriate concentrations (1 to 100 μg/mL) were prepared in methanol. Working solutions for the validation experiments were prepared by adding the appropriate amount of the corresponding stock solution to volumetric flasks to obtain concentrations ten times higher than the corresponding RMPLs.
Urine samples
The screening method was developed using urine from drug-abstinent male and female volunteers. Urine specimens from suspected DFSA/DFC cases and urine samples from clinical toxicology cases, which had been submitted to the authors’ laboratory for toxicological analysis, were used for applicability experiments. All samples were stored at −20 °C.
Sample preparation
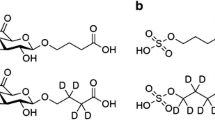
Sample preparation was performed with both nonhydrolyzed and hydrolyzed urine samples. For enzymatic hydrolysis, 20 μL of β-glucuronidase was added to 400 μL of urine. The resulting mixture was thoroughly mixed and incubated at 55 °C for 30 min. For method I, 100 μL of hydrolyzed or nonhydrolyzed urine, 10 μL of internal standard solution (morphine-d3, 100 ng/mL; zolpidem-d6, 100 ng/mL; and cyproheptadine, 100 ng/mL), and 500 μL acetonitrile were added. The mixture was thoroughly mixed, shaken on a rotary shaker for 2 min, and centrifuged for 3 min at 10,400 rpm. Afterwards, 500 μL of the supernatant was transferred into a glass vial and evaporated to dryness with nitrogen at 45 °C. The residue was redissolved in 50 μL of a mixture of eluents A and B at 80:20 (v/v) [25].
For method II, 250 μL of hydrolyzed or nonhydrolyzed urine, 25 μL of internal standard solution (GHB-d6, 100 μg/mL; secobarbital-d5, 200 ng/mL; THC-COOH-d3, 100 ng/mL), and 500 μL of acetonitrile were added. The mixture was thoroughly mixed, shaken on a rotary shaker for 2 min, and centrifuged for 3 min at 10,400 rpm. Afterwards, 700 μL of the supernatant was transferred into a glass vial and evaporated to dryness with nitrogen at 45 °C. The residue was redissolved in 30 μL of eluent A according to reference [25] with modifications.
Assay validation
The methods were validated with regard to selectivity, matrix effects (ME), process efficiencies (PE), and recovery (RE). Furthermore, the identification of all analytes at the respective RMPLs was tested.
Selectivity
For each method, selectivity was tested by using 30 nonhydrolyzed and hydrolyzed blank urine specimens, of which 15 urine specimens were from drug-free volunteers. The other 15 urine specimens were from routine clinical toxicology cases and had yielded negative GC-MS screening results during routine clinical toxicology analysis. Potential interference of the internal standards on the analyte detection was tested by two blank samples spiked with internal standards only.
Matrix effects, process efficiencies, and recovery
ME, PE, and RE were performed at the RMPLs according to the simplified approach described by Matuszewski et al. [26]. For sample set 1, 10 and 25 μL of spiking solutions were evaporated to dryness and reconstituted as described above for methods I and II, respectively. Ten replicate samples of set 1 were injected for each method.
For sample set 2, 10 and 25 μL methanol, respectively, were added to 100 and 250 μL of nonhydrolyzed blank urine specimens (30 different urines) and were worked up according to method I and method II, respectively. However, prior to evaporation, 10 and 25 μL of the spiking solution were added to the samples for method I and method II, respectively.
For sample set 3, 100 and 250 μL of the nonhydrolyzed blank urine specimens (30 different urines) were spiked with 10 and 25 μL of the respective spiking solution for methods I and II, respectively. Thereafter, the samples were worked up as described above.
For calculation of the ME, the analyte peak areas in the samples of set 2 were compared to the average peak area of the respective analytes in the set 1 samples. PE was determined accordingly by comparing the analyte peak areas of set 3 samples to the average peak area of the respective analytes in set 1 samples, whereas RE was assessed by comparison of analyte peak areas from sample sets 2 and 3.
Recommended minimum performance limits
The performance of the methods at the RMPLs was checked by using the abovementioned 30 nonhydrolyzed and hydrolyzed urine specimens spiked with all substances at the RMPLs. All samples were worked up and analyzed as described above. The acceptance criterion was a S/N ratio above 3:1 for both monitored transitions for each analyte. The RMPLs for all substances of method I and method II are shown in Tables 1 and 2, respectively.
Applicability
The applicability of the developed screening procedure was tested by the analysis of urine from nine suspected DFC/DFSA cases. Furthermore, 24 urine samples with a positive screening result for at least one of the analytes during routine clinical toxicology analysis were analyzed by the presented methods to check if the findings could be confirmed. Twenty-two of the urine specimens were analyzed using method I. With method II, three urine samples were tested. One urine specimen was tested with both methods. After the analysis, the intensities of the peak areas of the corresponding analytes in hydrolyzed and nonhydrolyzed urine samples were compared.
Excretion study with doxylamine
Additionally, an excretion study with doxylamine was performed. For this purpose, 43 urine samples were collected from a 24-year-old female after administration of a single oral dose of 30 mg of doxylamine (Schlafsterne®) and analyzed to examine how long the substance and its nor metabolite are detectable above the RMPL and in total. After ingestion of the doxylamine tablet, the total volume of each urine void was determined, and a 10-mL urine specimen was stored at −20 °C. The urine samples were analyzed using method I regarding doxylamine and its metabolite nordoxylamine. Creatinine was determined photometrically (at 505 nm after the Jaffé reaction with picric acid) using a Roche/Hitachi 902 analyzer. The peak areas of doxylamine and nordoxylamine were normalized to the corresponding creatinine concentrations. Furthermore, endogenous GHB was determined with method II and compared with the 10-μg/mL cutoff proposed in reference [27, 28].
Results and discussion
Liquid chromatography-mass spectrometry procedure
As this procedure was developed for a broad screening of analytes relevant in DFSA/DFC cases, another 22 drugs of potential relevance in DFC/DFSA cases in Germany, mainly benzodiapepines, antipsychotics, and opioids, were added to the 80 analytes recommended by the SOFT DFSA Committee [11]. All included analytes are given in Tables 1 and 2, respectively. The additional analytes are marked in italics.
For nordoxylamine, no reference substance was commercially available at the time of this study. Therefore, it was produced by in vitro biotransformation of doxylamine using the fungus C. elegans which is able to N-dealkylate doxylamine to nordoxylamine. The incubation procedure and identification of nordoxylamine was carried out as described by Martinez-Ramirez et al. [23]. Since the in vitro production of doxylamine by C. elegans was not quantitative, it could not be used for evaluation of the “quantitative” validation parameters ME, RE, and PE. However, MRM transitions, potentials, and retention times could be established for this analyte.
With exception of ethanol and valproic acid, all analytes proposed by the SOFT DFSA committee were included in the screening procedure. Alcohol is routinely tested in the authors’ laboratory by an accredited headspace GC method. Valproic acid could not be detected with this screening procedure, although precursor and fragment ions were detectable when directly injecting the drug into the MS/MS interface with a syringe pump. It therefore seems likely that poor chromatography is the reason for this phenomenon rather than MS detection. In fact, of the published analytical methods for determination of valproic acid in urine and plasma [29–32], two employed mobile-phase systems based on ammonium acetate and methanol [30, 33].
For tramadol, only one transition with sufficient abundance could be obtained (m/z 264 to m/z 58) which is in line with findings of Allen [34]. For this reason, a pseudoMRM transition (m/z 264 to m/z 264) was chosen as qualifier 2. For the initially selected MRM transitions of brompheniramine, chlordiazepoxide, and norsertraline, interfering peaks were observed in blank urine samples. Therefore, the respective MRM transitions based on isotopes of chlorine and bromine were selected which were free of interferences..
As concentrations of knock-out drugs can be very low in urine specimen, the SOFT DFSA Committee suggested minimum performance limits for procedures to be applied for the analysis of these compounds in DFC/DFSA cases. The respective RMPLs are listed in Tables 1 and 2. The RMPLs for the additional analytes were according to those suggested for analytes from the same drug class by the SOFT Committee. Therefore, the RMPLs of the included benzodiapepines, antipsychotics, and opioids were set to 5 ng/mL. The RMPL of topiramate was defined as 25 ng/mL, like for the other antiepileptics included in the recommendations of the SOFT DFSA committee.
The original aim to cover all analytes in a single procedure proved to be unfeasible due to the very different physicochemical properties of the analytes. The latter were therefore divided into an alkaline and an acidic group analytes that were covered by two different methods. Method I allowed the simultaneous analysis of 91 basic substances of different indication groups, mainly benzodiazepines, antipsychotics, antihistamines, central muscle relaxants, and common drugs of abuse. Cyproheptadine, morphine-d3, and zolpidem-d6 were chosen as internal standards, because they represent different extraction and ionization properties and because their retention times are distributed over the chromatogram. Figure 1 shows the MRM chromatograms recorded with method I from a urine specimen spiked with the 90 analytes (without nordoxylamine) at the RMPLs and the internal standards. The numbering of the analytes corresponds to that in Table 1.
Chromatograms of qualifier 1 transitions in selected retention time windows in a urine sample spiked with the analytes (except nordoxylamine) at the respective RMPLs and internal standards. Analyte numbers as given Table 1
Nine substances with acidic character, including GHB, topiramate, 11-nor-9-carboxy-tetrahydrocannabinol (THC-COOH), and six barbiturates, could be more effectively detected using the negative ESI mode (method II). The better detection of these analytes was also due to a different sample preparation with a greater sample volume of urine and a lower reconstitution volume resulting in a stronger concentration of the analytes in the final sample. As internal standards GHB-d6, secobarbital-d5, and THC-COOH-d6 were selected. The MRM chromatograms recorded with method II from a urine specimen spiked with the nine analytes at the respective RMPLs and the internal standards are displayed in Fig. 2. The numbering of the analytes corresponds to that in Table 2.
Chromatograms of qualifier 1 transitions in selected retention time windows in a urine sample spiked with the analytes at the respective RMPLs and internal standards. Analyte numbers as given Table 2
An important challenge was the chromatographic separation of substances with the same nominal molecular masses. Many of these substances had different chemical compositions and could be easily separated by the chromatographic conditions, for example, tramadol and nortriptyline (M r 263 u) with retention times of 9.9 and 27.6 min, respectively. The chromatographic separation of clobazam, norclomipramine, and temazepam (M r 300 u) proved to be more difficult. However, their retention times differed by at least 0.6 min in the final method. Furthermore, the isobaric pair morphine and hydromorphone (M r 285 u) was fully separated with retention times of 1.8 and 2.3 min, respectively. Separation of amobarbital and pentobarbital which differ only in the position of a methyl group in one of the alkyl side chains was the most difficult chromatographic problem encountered during method development. Both substances shared identical mass transitions, so that a full chromatographic resolution was essential. Under the current chromatographic conditions, both substances are separated with a time difference of 0.2 min, as shown enlarged in Fig. 2.
A total chromatographic resolution of all substances could not be achieved. However, this was not considered essential because of the qualitative character of this method. Moreover, the combination of analyte retention time and two MRM transitions per substance allowed unambiguous identification of all analytes. In DFC/DFSA cases, reliable identification of the drugs in question is more important than quantification.
For the screening procedure, a simple and unselective sample preparation was chosen because of the great range of analytes with different chemical and physical properties. The larger sample volumes in method II were necessary to account for lower sensitivity in the negative ESI mode.
Validation
Selectivity
No relevant interferences were observed in the 30 tested blank urine samples. Additionally, two urine samples, which were collected after consumption of poppy seeds the day before, were analyzed and showed signals for morphine, codeine, and hydrocodone. Minor matrix peaks were observed at the retention times of some analytes (alprazolam qualifier 2, chlordiazepoxide qualifier 1, cocaine qualifier 2, nitrazepam qualifier 1, oxymorphone qualifier 1, tramadol qualifier 2) in method I. However, these were always markedly (3 to 50 times) lower than those in samples containing the respective analytes at the RMPL. Figure 3 shows MRM chromatograms of a representative blank urine sample analyzed by method I (top) and method II (bottom).
The endogenous GHB concentrations of the 30 tested blank urines and the 43 urines of the excretion study were always below the proposed 10 μg/mL cutoff proposed for differentiation between endogenous and exogenous GHB [27]. The peak areas were markedly lower than those of the urine controls spiked with GHB at its RMPL of 10 μg/mL.
Matrix effects, process efficiencies, and recovery
The mean values and relative standard deviations (RSDs) for ME, PE, and RE are listed in the Electronic Supplementary Material that accompanies the online version of this article, Tables S1 and S2. For method I, the ME of the qualifier 1 ranged from 8 % (RSD 98 %) for tetrazepam to 996 % (RSD 48 %) for morphine, with a mean of 171 %, and a median of 126 %. The PE for qualifier 1 varied from 8 % (RSD 121 %) for tetrazepam to 970 % (RSD 50 %) for morphine, with a mean of 164 % and a median of 121 %. The RE for qualifier 1 varied between 58 % (RSD 52 %) for norpropoxyphene to 116 % (RSD 24 %) for zopiclone, with a mean of 95 % and a median of 95 %.
Furthermore, for method II, the ME for qualifier 1 ranged from 158 % (RSD 24 %) for GHB to 6,268 % (RSD 98 %) for THC-COOH, with a mean of 897 % and a median of 225 %. The PE for qualifier 1 varied from 146 % (RSD 25 %) for GHB to 4,852 % (RSD 112 %) for THC-COOH, with a mean of 720 % and a median of 205 %. The RE for qualifier 1 varied between 83 % (RSD 44 %) for THC-COOH 93 % to (RSD 23 %) for phenytoin, with a mean of 90 % and a median of 90 %.
ME and PE data of both methods varied greatly. For method I, the majority of analytes showed a large enhancement of the analyte signal. Only tetrazepam showed a strong suppression of the analyte signals by the matrix. For method I, it is obvious that there is a large enhancement of the analyte signal of morphine, oxymorphone, and hydromorphone and a large variation of the analyte signals between the tested urine samples. These analytes elute within the first 3 min. The most important cause of the great enhancement is certainly the high amount of co-eluting substances within the first minutes. Furthermore, the analyte signal of pregabalin is greatly increased because of an overlapping endogenous peak. It is also notable that the analyte signal of tetrazepam was strongly suppressed in urine samples and that this suppression showed considerable variability between samples. Nevertheless, tetrazepam was detectable at its RMPL in all of the 30 samples tested, indicating that this compound tetrazepam can be screened for with the described method despite intense and variable matrix effects.
For method II, THC-COOH showed a large enhancement of the analyte peak area in urine samples. Apart from extensive ion enhancement, increased solubility or reduced adsorption of THC-COOH in the presence of urine matrix compared to neat samples could be potential explanations for this finding. However, the ME, PE, and RE values for method II vary widely. Nevertheless, all acidic substances are currently qualitative identifiable.
The vast majority of analytes had recovery values of around 95 % for method I and 90 % for method II, respectively. The correspondence with the theoretically achievable values (82 % for method I and 90 % for method II) is acceptable. For tetrazepam, ziprasidone and zopiclone marked deviations of the average values was observed in single samples for recovery data, which were found to be statistically significant outliers (Grubbs’ test, P < 0.05). For this qualitative assay, the RSDs below 25 % for the majority of the analytes are also acceptable.
Recommended minimum performance limits
All compounds could be detected in the 30 tested urine samples at the RMPLs with a S/N ratio above 3:1. The RMPLs, shown in Tables 1 and 2 respectively, were achieved for all analytes as recommended by the SOFT DFSA Committee and also for the additionally included substances. The RMPLs ranged from 1 ng/mL for fentanyl to 10 μg/mL for GHB.
Applicability
Suspected DFC/DFSA cases
For applicability, nine suspected DFC/DFSA cases were examined. All analyses were carried out using the developed LC-MS/MS procedure. Seven of the nine alleged victims were female. The age ranged from 16 to 39 years. With exception of one case where robbery and extortion had been claimed, DFSA was suspected in all cases. Apart from the prescribed medication, knock-out drugs could not be detected. All results are shown in Table 3.
In case #7, pregabalin and duloxetine, both part of the presumed victim’s medication, were detected at concentrations significantly exceeding the respective RMPLs. In cases #6 and #7, the time delay between incident and sampling within 36 to 63 h was probably too long to detect many knock-out drugs, especially such with short half-lives. In the remaining cases, the time delay was in an appropriate range to detect the vast majority of knock-out drugs in urine specimens. In cases #1, #4, and #5, the main cause of unconsciousness and the symptoms described in Table 3 was probably the large amounts of alcohol ingested by the alleged victims. Hence, the symptoms can be explained without additional ingestion of knock-out drugs. In case #2, it turned out that the alleged victim had self-inflicted the injuries, and therefore the credibility of her version of the incidence is highly questionable including the alleged administration of knock-out drugs. In cases #3 and #8, no time span between the event and the specimen collection was documented. By the analysis of case #3, doxepine, part of the alleged victim’s medication, and its metabolite nordoxepine were detected at concentrations considerably above the respective RMPLs. No other knock-out drugs were found. In case #8, zolpidem was detected at a concentration below the RMPL in the urine specimen as shown in Fig. S1. An additional solid-phase extraction of this urine confirmed this result. In the further course, it became known that the alleged victim had been prescribed zolpidem after the incident for calming her down.
Investigation of known positive urine samples from clinical toxicology
To prove the developed screening procedure, some known positive urine samples from clinical toxicology were analyzed. The 24 urine samples investigated had been deliberately chosen. All analytes, previously identified during routine analysis (rapid immunochemical tests, GC-MS with urine hydrolysis, liquid-liquid extraction, and acetylation prior analysis), were observed with the developed procedure. This shows that a recent drug intake can easily be detected. Furthermore, additional substances, mainly amphetamines, opiates, opioids, and benzodiazepines, were detected, which is mainly due to the higher sensitivity of these analytes by using LC-MS/MS techniques. The complete results are given in Table S3. The observed concentrations were always considerably above the RMPLs, which is typical for intoxication or drug of abuse cases. As another result of the investigation, 17 of the 55 detected substances gave a more intense (2 to 100 times) analyte signal in hydrolyzed samples than in nonhydrolyzed samples. These include several benzodiazepines, opiates, and antipsychotics. For the remaining substances, the analyte signals were similar or slightly lower. It showed that a hydrolysis should always be performed additionally to the analysis of nonhydrolyzed samples.
Excretion study with doxylamine
The results of the excretion study after administration of 30 mg doxylamine (Schlafsterne®) are shown in Fig. 4 (concentrations of doxylamine and nordoxylamine are normalized to creatinine). Doxylamine with an elimination half-life of 10 h [35] could be detected above the RMPL for 5 days. This is significantly longer than the generally accepted detection window of 96 h in urine specimens [35]. Taking a S/N ratio above 3:1 as an identification criterion, doxylamine was even detectable for 10 days. Its normetabolite, nordoxylamine, was still detectable with a S/N ratio above 10:1 for 10 days. Nordoxylamine could have been detected well beyond the study time of 11 days with a S/N ratio above 3:1. This study showed that it may be possible to detect certain knock-out drugs despite of a long time delay, when they have long half-lives. This is even more apparent for the metabolites of such substances.
In contrast to existing methods, which are developed for blood and/or cover only subsets of the relevant analytes [18–20, 22], the developed procedure included the analytes suggested by the SOFT DFSA Committee and additional drugs and metabolites relevant in DFC/DFSA cases in Germany. Only ethanol and valproic acid have to be analyzed using other in-house methods. The procedure was developed and validated for urine specimen as suggested by the SOFT DFSA Committee [11] and showed to be selective for all included analytes. Nevertheless, special attention has to be drawn for the identification of opiates, amobarbital, pentobarbital, morphine, and hydromorphone. ME was tested with a remarkable number of 30 different urines samples, which is much more than the recommended for validation by the GTFCh [36]. The test showed that severe matrix effects were detected for some analytes, but were not present in all urine samples and therefore highlight the importance of testing ME with a high number of samples. As all analytes could be detected at the recommended RMPLs, also tested with 30 different urine samples, the procedure is therefore sensitive, in contrast to the method of Adamowicz and Kala [21]. The validation results and the successful application to samples from suspected DFC/DFSA cases and urine samples from clinical toxicology showed that this method is suitable for screening of 100 relevant analytes in urine samples. The long analysis time, resulting from two runs for each of the hydrolyzed and nonhydrolyzed samples, might be considered a limitation during routine application. However, DFC/DFSA cases are not very frequent compared to other routine casework, and analysis of such cases is generally not performed in an emergency toxicology setting. Hence, the total run time of 2.5 h per sample seems acceptable. This method was also successfully used for monitoring doxylamine concentrations in an excretion study.
Conclusion
The developed screening procedure proved to be selective and sensitive for all analytes included in the list of the SOFT DFSA Committee and the additional compounds, with the exception of ethanol and valproic acid. The procedure had been validated for urine specimens regarding selectivity, ME, PE, RE, and RMPLs. The validation results and the successful application to real DFC/DFSA samples demonstrate that this procedure is suitable for screening of 100 analytes relevant in DFC/DFSA cases.
References
Hall JA, Moore CB (2008) Drug facilitated sexual assault—a review. J Forensic Legal Med 15(5):291–297. doi:10.1016/j.jflm.2007.12.005
Madea B, Musshoff F (2009) Knock-out drugs: their prevalence, modes of action, and means of detection. Dtsch Arztebl Int 106(20):341–347. doi:10.3238/arztebl.2009.0341
Goulle JP, Anger JP (2004) Drug-facilitated robbery or sexual assault: problems associated with amnesia. Ther Drug Monit 26(2):206–210
Scott-Ham M, Burton FC (2005) Toxicological findings in cases of alleged drug-facilitated sexual assault in the United Kingdom over a 3-year period. J Clin Forensic Med 12(4):175–186. doi:10.1016/j.jcfm.2005.03.009
Madea B, Plieger S, Musshoff F (2008) Begutachtung in Fällen von drogenassoziierten Sexualdelikten. Aktuelle Beiträge zur Forensischen und Klinischen Toxikologie Bad Vilbel:116–124
Kauert GF (2008) Pharmakologisches Knocked Out. Ist das Bewusstlosigkeit oder was? Aktuelle Beiträge zur Forensischen und Klinischen Toxikologie Bad Vilbel:107–110
Beynon CM, McVeigh C, McVeigh J, Leavey C, Bellis MA (2008) The involvement of drugs and alcohol in drug-facilitated sexual assault: a systematic review of the evidence. Trauma Violence Abuse 9(3):178–188. doi:10.1177/1524838008320221
Schwartz RH, Milteer R, LeBeau MA (2000) Drug-facilitated sexual assault (‘date rape’). South Med J 93(6):558–561
Brown SD, Melton TC (2011) Trends in bioanalytical methods for the determination and quantification of club drugs: 2000–2010. Biomed Chromatogr: BMC 25(1–2):300–321. doi:10.1002/bmc.1549
Kintz P (2007) Bioanalytical procedures for detection of chemical agents in hair in the case of drug-facilitated crimes. Anal Bioanal Chem 388(7):1467–1474. doi:10.1007/s00216-007-1209-z
SOFT DFSA Committee (2012) Recommended minimum performance limits for common DFSA drugs and metabolites in urine samples. http://soft-tox.org/sites/default/files/SOFT_DFSA_Rec_Det_Limits_3-2012.pdf. Accessed 22 May 2013
LeBeau MA (2008) Guidance for improved detection of drugs used to facilitate crimes. Ther Drug Monit 30(2):229–233. doi:10.1097/FTD.0b013e31816791d7
von Mach MA, Weber C, Meyer MR, Weilemann LS, Maurer HH, Peters FT (2007) Comparison of urinary on-site immunoassay screening and gas chromatography–mass spectrometry results of 111 patients with suspected poisoning presenting at an emergency department. Ther Drug Monit 29(1):27–39. doi:10.1097/FTD.0b013e31802bb2aa
Kintz P, Villain M, Dumestre-Toulet V, Ludes B (2005) Drug-facilitated sexual assault and analytical toxicology: the role of LC-MS/MS A case involving zolpidem. J Clin Forensic Med 12(1):36–41. doi:10.1016/j.jcfm.2004.08.005
Deveaux M, Cheze M, Pepin G (2008) The role of liquid chromatography-tandem mass spectrometry (LC-MS/MS) to test blood and urine samples for the toxicological investigation of drug-facilitated crimes. Ther Drug Monit 30(2):225–228. doi:10.1097/FTD.0b013e3181676186
Parkin MC, Turfus SC, Smith NW, Halket JM, Braithwaite RA, Elliott SP, Osselton MD, Cowan DA, Kicman AT (2008) Detection of ketamine and its metabolites in urine by ultra high pressure liquid chromatography-tandem mass spectrometry. J Chromatogr B Anal Technol Biomed Life Sci 876(1):137–142. doi:10.1016/j.jchromb.2008.09.036
Quintela O, Sauvage FL, Charvier F, Gaulier JM, Lachatre G, Marquet P (2006) Liquid chromatography-tandem mass spectrometry for detection of low concentrations of 21 benzodiazepines, metabolites, and analogs in urine: method with forensic applications. Clin Chem 52(7):1346–1355. doi:10.1373/clinchem.2005.065631
Birkler RI, Telving R, Ingemann-Hansen O, Charles AV, Johannsen M, Andreasen MF (2012) Screening analysis for medicinal drugs and drugs of abuse in whole blood using ultra-performance liquid chromatography time-of-flight mass spectrometry (UPLC-TOF-MS)–toxicological findings in cases of alleged sexual assault. Forensic Sci Int 222(1–3):154–161. doi:10.1016/j.forsciint.2012.05.019
Vincenti M, Cavanna D, Gerace E, Pirro V, Petrarulo M, Di Corcia D, Salomone A (2012) Fast screening of 88 pharmaceutical drugs and metabolites in whole blood by ultrahigh-performance liquid chromatography-tandem mass spectrometry. Anal Bioanal Chem. doi:10.1007/s00216-012-6403-y
Ishida T, Kudo K, Hayashida M, Ikeda N (2009) Rapid and quantitative screening method for 43 benzodiazepines and their metabolites, zolpidem and zopiclone in human plasma by liquid chromatography/mass spectrometry with a small particle column. J Chromatogr B Anal Technol Biomed Life Sci 877(25):2652–2657. doi:10.1016/j.jchromb.2009.05.008
Adamowicz P, Kala M (2010) Simultaneous screening for and determination of 128 date-rape drugs in urine by gas chromatography-electron ionization-mass spectrometry. Forensic Sci Int 198(1–3):39–45. doi:10.1016/j.forsciint.2010.02.012
Juhascik M, Le NL, Tomlinson K, Moore C, Gaensslen RE, Negrusz A (2004) Development of an analytical approach to the specimens collected from victims of sexual assault. J Anal Toxicol 28(6):400–406
Martinez-Ramirez JA, Voigt K, Peters FT (2012) Studies on the metabolism of five model drugs by fungi colonizing cadavers using LC-ESI-MS/MS and GC-MS analysis. Anal Bioanal Chem. doi:10.1007/s00216-012-6212-3
Paul LD, Musshoff F (2009) Richtilinie der GTFCh zur Qualitätssicherung bei forensisch-toxikologischen Untersuchungen. Toxichem Krimtech 76(3):142–176
Wissenbach DK, Meyer MR, Remane D, Weber AA, Maurer HH (2011) Development of the first metabolite-based LC-MS(n) urine drug screening procedure-exemplified for antidepressants. Anal Bioanal Chem 400(1):79–88. doi:10.1007/s00216-010-4398-9
Matuszewski BK, Constanzer ML, Chavez-Eng CM (2003) Strategies for the assessment of matrix effect in quantitative bioanalytical methods based on HPLC-MS/MS. Anal Chem 75(13):3019–3030
Yeatman DT, Reid K (2003) A study of urinary endogenous gamma-hydroxybutyrate (GHB) levels. J Anal Toxicol 27(1):40–42
LeBeau MA, Montgomery MA, Morris-Kukoski C, Schaff JE, Deakin A, Levine B (2006) A comprehensive study on the variations in urinary concentrations of endogenous gamma-hydroxybutyrate (GHB). J Anal Toxicol 30(2):98–105
Salomone A, Di Corcia D, Gerace E, Vincenti M (2011) A fatal case of simultaneous ingestion of mirtazapine, escitalopram, and valproic acid. J Anal Toxicol 35(7):519–523
Gao S, Miao H, Tao X, Jiang B, Xiao Y, Cai F, Yun Y, Li J, Chen W (2011) LC-MS/MS method for simultaneous determination of valproic acid and major metabolites in human plasma. J Chromatogr B Anal Technol Biomed Life Sci 879(21):1939–1944. doi:10.1016/j.jchromb.2011.05.022
Jain DS, Subbaiah G, Sanyal M, Shrivastav P (2007) A high throughput and selective method for the estimation of valproic acid an antiepileptic drug in human plasma by tandem LC-MS/MS. Talanta 72(1):80–88. doi:10.1016/j.talanta.2006.09.033
Kim KB, Seo KA, Kim SE, Bae SK, Kim DH, Shin JG (2011) Simple and accurate quantitative analysis of ten antiepileptic drugs in human plasma by liquid chromatography/tandem mass spectrometry. J Pharm Biomed Anal 56(4):771–777. doi:10.1016/j.jpba.2011.07.019
Matsuura K, Ohmori T, Nakamura M, Itoh Y, Hirano K (2008) A simple and rapid determination of valproic acid in human plasma using a non-porous silica column and liquid chromatography with tandem mass spectrometric detection. Biomed Chromatogr 22(4):387–393. doi:10.1002/bmc.944
Allen KR (2006) Interference by venlafaxine ingestion in the detection of tramadol by liquid chromatography linked to tandem mass spectrometry for the screening of illicit drugs in human urine. Clin Toxicol (Phila) 44(2):147–153
Donato JL, Koizumi F, Pereira AS, Mendes GD, De Nucci G (2012) Simultaneous determination of dextromethorphan, dextrorphan and doxylamine in human plasma by HPLC coupled to electrospray ionization tandem mass spectrometry: application to a pharmacokinetic study. J Chromatogr B Anal Technol Biomed Life Sci 899:46–56. doi:10.1016/j.jchromb.2012.05.001
GTFCh (2009) Anhang B zur Richtlinie der GTFCh zur Qualitätssicherung bei forensich-toxikologischen Untersuchenungen. Anforderungen an die Validierung von Analysenmethoden. http://www.gtfch.org/cms/images/stories/files/GTFCh_Richtlinie_Anhang%20B_Validierung_Version%201.pdf. Accessed 22 Jun 2013
Acknowledgments
The authors thank Wiebke Rudolph for proofreading the manuscript and Anita Gabler for performing the creatinine measurements.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 129 kb)
Rights and permissions
About this article
Cite this article
Remane, D., Wetzel, D. & Peters, F.T. Development and validation of a liquid chromatography-tandem mass spectrometry (LC-MS/MS) procedure for screening of urine specimens for 100 analytes relevant in drug-facilitated crime (DFC). Anal Bioanal Chem 406, 4411–4424 (2014). https://doi.org/10.1007/s00216-014-7841-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00216-014-7841-5