Abstract
Rationale
Preclinical studies suggest that the GABAB receptor is a potential target for treatment of substance use disorders. However, recent clinical trials report adverse effects in patients treated with the GABAB receptor agonist baclofen and even question efficacy. How can the discrepancy between preclinical and clinical findings be explained?
Objective
To test efficacy and adverse effects of baclofen and the novel GABAB positive allosteric modulator (PAM) CMPPE in rat addiction models, which were developed in accordance with DSM.
Methods
We used a well-characterized rat model of long-term alcohol consumption with repeated deprivation phases that result in compulsive alcohol drinking in a relapse situation, and a rat model of long-term intravenous cocaine self-administration resulting in key symptoms of addictive behavior. We tested repeated baclofen (0, 1, and 3 mg/kg; i.p.) and CMPPE doses (0, 10, and 30 mg/kg; i.p.) in relapse-like situations, in either alcohol or cocaine addicted-like rats.
Results
Baclofen produced a weak anti-relapse effect at the highest dose in alcohol addicted-like rats, and this effect was mainly due to the treatment-induced sedation. CMPPE had a better profile, with a dose-dependent reduction of relapse-like alcohol drinking and without any signs of sedation. The cue-induced cocaine-seeking response was completely abolished by both compounds.
Conclusion
Positive allosteric modulation of the GABAB receptor provides efficacy, and no observable side effects in relapse behavior whereas baclofen may cause, not only sedation, but also considerable impairment of food intake or metabolism. However, targeting GABAB receptors may be effective in reducing certain aspects of addictive-like behavior, such as cue-reactivity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The GABAB receptor, a member of the G protein-coupled receptor family, has recently received significant attention in preclinical and clinical studies as a potential target for treatment of substance use disorders. In rats, activation of this receptor by baclofen has been shown to block acquisition of alcohol drinking, reduce motivation to self-administer alcohol, and lower both voluntary alcohol consumption and relapse-like drinking behavior (Colombo et al. 2002, 2003, 2006; Maccioni et al. 2012). This compound also attenuated the acute rewarding effect of cocaine measured as elevated brain reward thresholds (Slattery et al. 2005), decreased cocaine self-administration, and reduced cue-induced reinstatement of cocaine seeking behavior (Roberts et al. 1996; Brebner et al. 1999; Xi and Stein 1999; Di Ciano and Everitt 2003). Baclofen was found effective in reducing self-administration of other drugs, such as heroin (Di Ciano and Everitt 2003), nicotine (Paterson et al. 2004), and amphetamine (Brebner et al. 2005). Similarly, activation of positive allosteric modulators (PAMs) of the GABAB receptor attenuated the rewarding properties of cocaine in the intracranial self-stimulation paradigm (Slattery et al. 2005), reduced self-administration, seeking, and conditioned place preference of different drugs (for review see Filip et al. 2015). In the described preclinical studies, effective doses of baclofen were devoid of any sedative effects, since neither water consumption, food intake, body weight nor spontaneous locomotor activity was affected by this treatment (for review see Agabio and Colombo 2014). However, in clinical studies, effective doses of baclofen induce undesirable side effects in most of the patients, and especially substantial fatigue/sleepiness is reported (Kiel et al. 2015; Pelissier et al. 2017). Most worrying, in July 2017 ANSM, the French National Drug and Health Products Safety Agency, released a warning regarding the use of high-dose baclofen in alcoholic patients due to observed increase in numbers of hospitalization and premature death by off-label use of baclofen (ANSM 2017). It is therefore surprising that adverse side effects have not been reported in preclinical studies. However, acute or sub-chronic treatment schedules of baclofen, brief instrumental training procedures, or the use of non-dependent animals might be contributing to the lack of adverse side effects in preclinical studies. Laboratory animals that only have a short-lasting drug experience are less likely to develop side effects, partly because of their young age but mostly because of the negligible impact of a short drug exposure on the organism. In humans, development of addictive behavior is linked to chronic drug use. This is accompanied by prominent alterations in the function of the central nervous system and by multiple secondary problems, such as brain and organ damage.
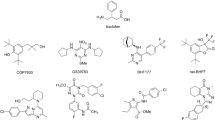
Hence, the aim of this study was to examine whether baclofen and the GABAB positive allosteric modulator CMPPE (2-{1-[2-(4-chlorophenyl)-5-methylpyrazolo[1,5-a]pyrimidin-7-yl]-2-piperidinyl}ethanol) (Perdona’ et al. 2011) will be able to reduce alcohol and cocaine relapse, without inducing adverse side effects such as pronounced sedation, in two rat models of either alcohol or cocaine addiction. Both models are based on long-term drug intake and were developed in accordance with the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV/5) and provide good face, construct, and predictive validity (Spanagel 2017). The DSM-based rat model of alcoholism incorporates long-term voluntary alcohol drinking with repeated deprivation phases. Following repeated deprivation phases, rats lose control over drinking behavior. This is characterized by an increased motivation to consume alcohol and a shift towards drinking more concentrated alcohol solutions, compulsive drinking despite aversive consequences, loss of interest in alternative rewards, and loss of circadian drinking patterns (Spanagel 2017; Spanagel and Hölter 1999; Vengeliene et al. 2009, 2013, 2014). The rat model of cocaine addiction integrates similar behavioral sub-dimensions of addiction: (i) the inability to refrain from drug-seeking and taking, (ii) high motivation to self-administer cocaine, and (iii) maintenance of cocaine use despite negative consequences (Deroche-Gamonet et al. 2004; Cannella et al. 2013). Both models have been repeatedly employed to study the neurobiological mechanisms underlying the transition from controlled to compulsive drug use and for testing novel abstinence-promoting compounds (e.g., Cannella et al. 2013, 2018; Kasanetz et al. 2010; Spanagel 2009, 2017; Vengeliene et al. 2016; Takahashi et al. 2017).
Materials and methods
Animals
Fifty 2-month-old male Wistar rats (from our own breeding colony at the CIMH, Germany) were used for the ADE experiments, ten 2-month-old male Wistar rats (State Breeding Farm Rappolovo, Russia) were used for ethanol cue-induced reinstatement experiments, and 62 2-month-old male Sprague-Dawley rats (Charles River, Germany) were used for cocaine cue-induced reinstatement experiments. Statistical power analysis was done for sample size estimation. All rat handling was performed by a person blind to the experimental design. All animals were housed individually in standard rat cages (Ehret, Germany and Tecniplast, Italy) under a 12/12-h artificial light/dark cycle and constant room temperature (22 ± 1 °C). Standard laboratory rat food (Ssniff, Soest, Germany and Laboratorkorm, Russia) and tap water were provided ad libitum throughout the experimental period. All experimental procedures are approved by the Committee on Animal Care and Use (Regierungspräsidium Karlsruhe, Germany) or by Ethics Committee of First Pavlov State Medical University (St. Petersburg, Russia) and were carried out in accordance with the local Animal Welfare Act and the European Communities Council Directive of 22 September 2010 (2010/63/EU).
Drugs
Alcohol drinking solutions were prepared from 96% ethanol (Sigma-Aldrich, Germany) and then diluted with tap water. Cocaine-HCl (Caesar & Loretz GmbH, Germany) was dissolved in sterile water for injections. Baclofen (Sigma-Aldrich, Germany or generously provided by AbbVie, Ludwigshafen, Germany) was dissolved in either saline or polyethylene glycol (PEG, Sigma-Aldrich, Germany) and then diluted with injection water to a final PEG concentration of 10%. CMPPE (generously provided by AbbVie, Ludwigshafen, Germany) was either suspended in 1% hydroxypropyl methylcellulose or dissolved in cremophor (Sigma-Aldrich, Germany) and then diluted with injection water to a final cremophor concentration of 20%. All drugs were freshly prepared and injected intraperitoneally (i.p.) in a volume of 2 ml/kg. The doses of baclofen and CMPPE and the timing of injections were selected according to the previous published research (Perdona’ et al. 2011; Brown et al. 2016).
Long-term voluntary alcohol consumption with repeated deprivation phases
Relapse-like drinking procedure
After 2 weeks of habituation to the animal room, rats were given concurrent ad libitum access to four bottles containing tap water, 5, 10, and 20% ethanol solutions (v/v). Drinking of alcohol and water was monitored daily/weekly by weighing bottles. From these data, water consumption (ml per kg of body weight per day; ml/kg/day) and alcohol consumption (g of pure alcohol per kg of body weight per day; g/kg/day) was calculated. The first 2-week deprivation period was introduced after 8 weeks of continuous alcohol availability. After the deprivation period, rats were given access to alcohol again, and five more deprivation periods were introduced in a random manner. The long-term voluntary alcohol drinking procedure including all deprivation phases lasted for approximately 1 year.
The pharmacological testing was introduced at the end of the sixth alcohol deprivation period (Fig. 1). In order to study the effects of drug treatment on the expression of the alcohol deprivation effect (ADE), rats were divided into groups (n = 8–9 per group) in such a way that the mean baseline total alcohol intake was approximately the same in each group (i.e., 2.5 g/kg/day). Baseline drinking was monitored daily for 1 week. After the last day of baseline measurement, the ethanol bottles were removed from the cages leaving the animals with free access to food and water for 3 weeks. Thereafter, the first three groups of animals were subjected to injections of either baclofen (1 and 3 mg/kg) or its respective vehicle every 12 h for a total of five injections. The other three groups received five injections of either vehicle or CMPPE (10 and 30 mg/kg). The alcohol bottles were reintroduced after the second drug administration and the occurrence of an ADE was determined. Total ethanol (g/kg/day) and water intake (ml/kg/day) were measured daily for a subsequent week.
A timeline for the long-term voluntary alcohol consumption with repeated deprivation phases procedure. The first 2-week deprivation period (D1) was introduced after eight weeks of continuous alcohol and water availability (Alc). After this deprivation period, rats were given access to alcohol again, and five more deprivation periods were introduced in a random manner (D2–D6), i.e., the duration of subsequent drinking and deprivation phases was irregular, 4–6 and 2–4 weeks, respectively. The pharmacological testing (^) was introduced at the end of the sixth alcohol deprivation period. All animals were divided into six groups and were given either baclofen (1 and 3 mg/kg) or CMPPE (10 and 30 mg/kg) or their respective vehicles every 12 h for a total of five injections. All rats were re-exposed to alcohol after the second drug administration
Home cage locomotor activity measurements by the E-Motion system
In order to test for any sedative effects resulting from the drug treatment, home cage locomotor activity was monitored by the use of an infrared sensor connected to a recording and data storing system Mouse-E-Motion (Infra-e-motion, Henstedt-Ulzburg, Germany). A Mouse-E-Motion device was placed above each cage (30 cm from the bottom) so that the rat could be detected at any position inside the cage. The device was sampling every second whether the rat was moving or not, and total number of movements was recorded in 6-min intervals. The sensor could detect body movement of the rat of at least 1.5 cm from one sample point to the successive one. The data measured by each Mouse-E-Motion device were downloaded into a personal computer and processed with Microsoft Excel. Monitoring of locomotor activity started 1 day before drug treatment procedure and was continued for 5 more post-treatment days. The percentage of each rat’s locomotor activity during and after treatment days was calculated by using the “before treatment” activity data as a reference.
Cue-induced reinstatement of ethanol-seeking behavior
Operant ethanol self-administration apparatus
Cue-induced reinstatement of ethanol-seeking was carried out in operant chambers (MED Associates Inc., St. Albans, VT) enclosed in ventilated sound-attenuating cubicles. The chambers were equipped with two nose-poke holes separated by liquid delivery system (a liquid dipper), a house-light and triple cue lights situated above nose-poke holes. Responses in one hole (active) initiated a delivery of 0.05 ml of the fluid. Responses in the other nose-poke hole (inactive) were recorded but had no programmed consequences. An IBM compatible computer controlled the delivery of fluids, presentation of stimuli, and data recording.
Ethanol self-administration conditioning and extinction phase
Before the initiation of ethanol self-administration conditioning phase, all rats were subjected to a voluntary home-cage drinking procedure for a period of 7 weeks. During this period, rats were given a free choice between water and 10% ethanol solution. The individual intake of fluids was measured daily and the body weights were monitored weekly. Thereafter, rats were trained to self-administer 10% ethanol solution in 1 h daily operant conditioning sessions. During the first ten sessions, ethanol solution was delivered using a fixed-ratio 1 (FR1) schedule of reinforcement. Each active nose-poke was followed by the house-light turned off for 15 s and a triple cue light turned on for 3 s (compound stimulus). During the 15-s time-out period, responses were recorded but not reinforced. Then, animals were subjected to six FR2 sessions followed by eight FR3 sessions.
After completing the conditioning phase, rats were subjected to daily 1 h extinction sessions for eight consecutive days; this was sufficient to reach reduced response rates approximating the extinction criterion of 20% of the last three conditioning sessions. Extinction phase was identical to the conditioning phase except that active nose-pokes were not followed by the presentation of the compound stimulus, and water (instead of ethanol) was delivered upon each successful nose-poke.
Ethanol cue-induced reinstatement
Reinstatement testing began the next day after the final extinction session. In this test, rats were exposed to the same conditions as during the conditioning phase, except that ethanol was not made available. Nose-pokes in the active hole under an FR3 schedule of reinforcement were followed by the presentation of both the ethanol-associated compound stimuli and the liquid dipper filled with water. To test the effect of baclofen, animals were subjected to the cue-induced reinstatement test once every fourth day. Between tests, animals were left undisturbed in their home cages. Vehicle, 1 mg/kg of baclofen or 3 mg/kg of baclofen was tested in all rats according to a within-subjects Latin Square design. Drug administration was performed 30 min before the test procedure. In order to test the effect of CMPPE on ethanol cue-induced reinstatement, all animals were reconditioned in 12 FR3 self-administration sessions and extinguished until the extinction criterion was reached. Similarly to baclofen, administration of vehicle, 10 mg/kg of CMPPE or 30 mg/kg of CMPPE was performed 30 min before the reinstatement test. Animals were subjected to this test once every fourth day using a within-subjects Latin Square design. Between tests, animals were left undisturbed in their home cages.
Cue-induced reinstatement of cocaine-seeking behavior
Catheter implantation
A catheter made of polyurethane (internal diameter 0.58 mm, external diameter 0.94 mm) was implanted at the jugular vein under isoflurane anesthesia (~ 2%). The proximal end was placed into the right atrium of the animal’s heart, while the distal end was passed underneath the skin and fixed in the mid scapular region. Rats were given 4–6 days of recovery before the initiation of cocaine self-administration (CSA) training. Catheters were flushed daily with a heparinized solution (100 IU/ml) containing 1 mg/ml of enrofloxacin (Baytril®).
Operant cocaine self-administration apparatus
CSA was carried out in operant chambers (Imetronic, France) enclosed in ventilated sound-attenuating cubicles. Two nose-poke holes were located on the opposite walls, 5 cm above the grid floor. Nose-poke responses were recorded by the interruption of a photo-beam projected across the hole. Poking in the active hole resulted in the delivery of cocaine, whereas poking in the inactive hole had no programmed consequences. The chambers were equipped with a white cue-light located 9.5 cm above the active hole, a green cue-light next to it, a blue cue-light located on the opposite wall 33 cm above the grid floor, and the house light that illuminated the entire chamber. Data was collected using POLY software.
Cocaine self-administration conditioning and extinction phase
CSA was based on the protocol published by Deroche-Gamonet et al. (2004) and Cannella et al. (2013). Briefly, each CSA session was comprised of drug availability periods (drug-ON, 40 min) alternated with NO-drug periods (15 min). During drug-ON periods, blue cue light was lit to indicate the availability of cocaine and a white cue-light was paired with cocaine infusion. During NO-drug periods, the blue and white cue-lights were withdrawn, nose-pokes had no scheduled consequences, and the NO-drug period was indicated by the house light. Animals were trained under FR5 schedule of reinforcement for 0.8 mg/kg/infusion of cocaine. Each cocaine infusion was followed by a 40-s time-out period. Three drug-ON and two NO-drug periods were alternated, resulting to a 2.5-h daily CSA sessions.
Following 50 CSA sessions, animals were tested for the three addiction criteria: motivation to self-administer cocaine, persistence of cocaine-seeking, and resistance to punishment. Motivation was assessed in a break point (BP) test. Blue and white cue lights were lit during the test, and the progressive ratio of reinforcement was 10, 20, 30, 45, 65, 85, 115, 145, 185, 225, 275, 325, 385, 445, 515, 585, 665, 745, 835, 925, 1025, 1125, 1235, 1345, 1465, and 1585. The test ceased either after 5 h or if a ratio could not be completed in a 1-h period. The last completed ratio was used as a break point value. Persistence of cocaine-seeking was measured as the number of active nose-pokes during NO-drug periods in the last three CSA training sessions prior to the BP test. And finally, resistance to punishment was assessed by pairing cocaine infusion with foot shocks (0.2 mA, 1 s). Before this test, animals received four more daily CSA sessions, and the foot shock test lasted for only one 40-min drug-ON period. In addition to the blue and white cue lights, a green cue light was turned on after the first nose-poke to indicate the upcoming shock. After the fourth nose-poke animals received a foot shock, and following the FR5 cocaine infusion, another foot shock was delivered. Percentage of cocaine infusions earned during the foot shock test with respect to the first drug-ON period during the last CSA session was used as a criterion.
Rats that showed responses above the 60th percentile of the population distribution received a score of 1 in each of the assessed addiction criteria. Therefore, the total score of each rat spanned from 0 to 3 criteria. In this model, animals that meet all 3 criteria are classified as addicted-like. Twelve animals in our study were classified as addicted-like and were used for pharmacological assessments.
Extinction training started after 1 week of additional CSA sessions. During extinction sessions, nose-poking did not result in either the administration cocaine or the presentation of response-contingent cues. Extinction training continued for nine 2-h daily sessions, which in total was sufficient to reach reduced response rates approximating the extinction criterion of 20% of the last conditioning sessions.
Cocaine cue-induced reinstatement
Reinstatement testing of 1 h was performed on the next day after the final extinction session. In this test, rats were exposed to the same conditions as during the conditioning phase, except that the cocaine was not made available. Operant chamber was constantly illuminated by the blue cue light, which served as a contextual stimulus for cocaine availability. Following the required number of nose-pokes in the active hole, the white cue light was illuminated. The number of nose-poking in both the active and inactive holes was recorded throughout the test.
To test the effect of baclofen and CMPPE on the cue-induced reinstatement of cocaine- seeking, animals were divided into groups on the basis of their performance during the last CSA and extinction sessions (n = 7–8 per group). Vehicle, 3 mg/kg of baclofen or 30 mg/kg of CMPPE was administered 30 min before the reinstatement test. Animals were subjected to this test once per week using a within-subjects Latin Square design.
Statistical analysis
ADE measurements (total alcohol intake, water intake) and locomotor activity data were analyzed using recordings from pre- and post-deprivation days by a two-way ANOVA with repeated measures [factors were treatment group and day]. Data analysis regarding the effects of baclofen and CMPPE treatment on the change in the rat body weight was performed using a one-way ANOVA [factor was treatment group]. Data obtained from the cue-induced alcohol-seeking experiments was analyzed by use of a two-way ANOVA with repeated measures [factors were nose-pokes (active vs. inactive) and session (extinction vs. reinstatement)]. Cocaine-seeking experiments were analyzed by use of a three-way ANOVA with repeated measures [factors were treatment group, session (extinction vs. reinstatement), and nose-pokes (active vs. inactive)]. Whenever indicated by ANOVA, Student Newman-Keuls’ post-hoc tests were performed. The chosen level of significance was p < 0.05.
Results
Effect of the administration of baclofen and CMPPE on relapse-like drinking
Following the re-introduction of alcohol solutions after a period of abstinence, the vehicle-treated groups showed a typical increase in alcohol consumption, indicating the occurrence of an ADE. This increase was not different from that observed during the first deprivation periods (data not shown). Hence, a two-way ANOVA for repeated measures revealed a general increase in alcohol intake after a sixth deprivation phase as compared to basal drinking [factor day F(7,154) = 56.2, p < 0.0001 and F(7,154) = 94.9, p < 0.0001 for baclofen and CMPPE treatment groups, respectively] (Fig. 1). Analysis of data also showed that both baclofen and CMPPE treatments significantly reduced alcohol intake during post-abstinence days when compared to intake by vehicle-treated animals [factor treatment group × day interaction effect: F(14,154) = 2.6, p < 0.01 and [F(12,154) = 4.5, p < 0.0001 for baclofen and CMPPE treatment groups, respectively]. The subsequent post-hoc tests demonstrated that treatment of rats with 1 mg/kg of baclofen did not affect post-abstinence drinking, whereas twice daily administration of 3 mg/kg of baclofen significantly reduced alcohol intake during relapse-like drinking days (Fig. 2a). Administration of both doses of CMPPE significantly reduced post-abstinence drinking; however, the alcohol intake was still significantly increased during the first post-deprivation days as compared to the baseline consumption (Fig. 2b). Water intake in baclofen and CMPPE-treated rats was either unchanged or tended to be increased during treatment days when compared to water intake by vehicle-treated animals [factor treatment group × day interaction effect p = 0.19 and p = 0.70 for baclofen and CMPPE-treatment groups, respectively] (data not shown), demonstrating that treatment selectively affected alcohol consumption.
Total ethanol intake (g/kg/day) before (baseline, BL) and after an alcohol deprivation period of 3 weeks. Arrows indicate twice-daily administration of (a) vehicle, 1 mg/kg baclofen, 3 mg/kg of baclofen, and (b) vehicle, 10 mg/kg of CMPPE, 30 mg/kg of CMPPE (n = 8–9 per treatment condition). The alcohol bottles were reintroduced after the second drug administration. Data are presented as means ± S.E.M. * indicates significant differences from the baseline, # indicates significant differences from the control vehicle group, p < 0.05
Locomotor activity data was analyzed using recordings of 12-h post-injection intervals that corresponded to the animals’ active (dark) phase and 1-h post-injection intervals of animals’ active phase. Overall, there was a general reduction in home-cage activity seen in all animal groups, which was likely caused by alcohol intoxication during the first post-abstinence drinking days [factor day for 12-h recordings: F(7,133) = 20.7, p < 0.0001 and F(7,147) = 45.0, p < 0.0001 and for 1-h recordings: F(3,57) = 15.4, p < 0.0001 and F(3,63) = 9.2, p < 0.0001 for baclofen and CMPPE treatment groups, respectively] (Fig. 3). However, a two-way ANOVA revealed that treatment with 3 mg/kg of baclofen had an additional sedative effect on animal home-cage activity [factor treatment group: F(2,19) = 5.4, p < 0.05 and F(2,19) = 5.8, p < 0.05 for 12-h and 1-h recordings, respectively] (Fig. 3a, b). This activity change was temporary and recovered to basal levels immediately after treatment stopped. Locomotor activity changes, induced by CMPPE administration were not significant [factor treatment group: p = 0.72 and p = 0.22 for 12-h and 1-h recordings, respectively] (Fig. 3c, d).
Locomotor activity during and after twice-daily administration of (a, b) vehicle, 1 mg/kg of baclofen, 3 mg/kg of baclofen, and (c, d) vehicle, 10 mg/kg of CMPPE, 30 mg/kg of CMPPE (n = 7–9 per treatment condition). Locomotor activity is shown as (a, c) 12 h- and (b, d) 1-h post-injection intervals of animals’ active (dark) phase. The percentage of each rat’s locomotor activity during and after treatment days was calculated with respect to basal (BL) activity prior to treatment (dashed line). Injection days are marked as “^”. The alcohol bottles were reintroduced after the second drug administration. Data are presented as means ± S.E.M. * indicates significant differences from the control vehicle group, p < 0.05
Treatment with either baclofen or CMPPE led to significant changes in the animals’ body weight, demonstrating that both drugs altered food intake and/or metabolism. Body weight changes during the treatment days were most apparent in baclofen-treated animals, and 3 mg/kg caused significant loss of body weight [vehicle +1.3%, 1 mg/kg of baclofen +0.8%, and 3 mg/kg of baclofen − 1.4%, factor treatment group F(2,22) = 10.0, p < 0.001]. CMPPE treatment did not cause loss of body weight; however, animals from the 30 mg/kg of CMPPE treatment group did not gain as much of body weight as the vehicle-treated rats [vehicle + 1.8%, 10 mg/kg of CMPPE + 2.0% and 30 mg/kg of CMPPE + 0.6%, factor treatment group F(2,22) = 21.3, p < 0.0001].
Effects of the administration of baclofen and CMPPE on cue-induced reinstatement of ethanol-seeking behavior
Daily ethanol intake by the end of the free-choice ethanol drinking phase was approximately 3.4 g of pure ethanol/kg of body weight per day. At the end of the conditioning phase, rats exhibited 124 ± 15 ethanol-associated nose-pokes (this resulted to 0.4 g of pure ethanol intake per kg of body weight) and 2.3 ± 0.5 inactive nose-pokes. The number of operant responses progressively faded away across eight extinction sessions. Thus, during the last two extinction sessions, active nose-pokes dropped down to 16 ± 3, and inactive pokes were 1.5 ± 0.4.
Two-way ANOVA revealed that the number of responses during the ethanol cue-induced reinstatement testing increased significantly when compared to the last extinction sessions [factor session: F(3,54) = 10.1, p < 0.0001 and F(3,54) = 6.1, p < 0.01 for baclofen and CMPPE treatment groups, respectively] (Fig. 4a, c). Post-hoc analysis demonstrated that this increase was caused by the higher responses in the active hole in the vehicle-treated condition. Treatment with both doses of baclofen and CMPPE abolished reinstatement of ethanol-seeking behavior (Fig. 4a, c). Hence, responding in the active hole during the reinstatement test in the drug-treated condition was significantly lower compared to the vehicle condition and did not differ from that during the last extinction sessions. Responding in the inactive hole was too low to be used as a measure of sedative effects of treatment (Fig. 4b, d).
The effect of (a) vehicle, 1 mg/kg of baclofen, 3 mg/kg of baclofen, and (b) vehicle, 10 mg/kg of CMPPE, 30 mg/kg of CMPPE (n = 10 per treatment condition) on ethanol cue-induced reinstatement. Data are shown as the average number of pokes in the active and inactive holes during the last extinction sessions and as the number of nose-pokes after the presentation of stimuli previously paired with ethanol. Data are presented as means ± S.E.M. # indicates significant differences to the extinction nose-pokes; * indicates significant differences from the control vehicle group, p < 0.05
Effects of the administration of baclofen and CMPPE on cue-induced reinstatement of cocaine-seeking behavior
At the end of the conditioning phase, 12 addicted-like animals exhibited 477 ± 56 of cocaine-associated nose-pokes and 53 ± 19 inactive nose-pokes. The number of operant responses progressively faded away across nine extinction sessions, reaching 39 ± 9 active nose-pokes and 30 ± 5 inactive nose-pokes. Cue-induced reinstatement was carried out on the next day after the extinction criteria was achieved. Three-way ANOVA for baclofen vs. vehicle treatment revealed significant difference between extinction and reinstatement sessions [factor session: F(1,24) = 7.5, p < 0.01] and significant effect of baclofen treatment [factor session × treatment interaction F(1,24) = 7.1, p < 0.01, and factor session × treatment × nose-poke interaction F(1,24) = 6.5, p < 0.05]. Post-hoc analysis indicated that baclofen treatment abolished cue-induced cocaine-seeking behavior (Fig. 5a). Similarly, analysis of vehicle vs. CMPPE data showed significant difference between extinction and reinstatement sessions [F(1,26) = 5.9, p < 0.05]. As in the case of baclofen, administration of 30 mg/kg of CMPPE abolished cue-induced cocaine-seeking [factor session × treatment interaction F(1,26) = 5.0, p < 0.05, and factor session × treatment × nose-poke interaction F(1,26) = 4.3, p < 0.05] (Fig. 5c). Post-hoc analysis indicated that nose-pokes in the inactive-hole were not significantly different in both baclofen- and CMPPE-treated groups (Fig. 5b, d).
The effect of either vehicle or 3 mg/kg of baclofen (a, b) and vehicle or 30 mg/kg of CMPPE (c, d) (n = 7–8 per treatment condition) on cocaine cue-induced reinstatement. Data are shown as the average number of active (a, c) and inactive (b, d) nose-pokes during the last extinction sessions and as the number of pokes after the presentation of stimuli previously paired with cocaine. Data are presented as means ± S.E.M. * indicates significant differences to the extinction nose-pokes; # indicates significant differences from the control vehicle group, p < 0.05
Discussion
The present study demonstrates that both baclofen and CMPPE caused a significant reduction of relapse-like excessive alcohol intake during the post-abstinence drinking days in a DSM-based rat model of alcohol addiction. Water consumption in baclofen and CMPPE treated rats was slightly increased during post-abstinence days compared to vehicle-treated animals, showing the selectivity of these compounds towards alcohol. Whereas CMPPE produced a dose-dependent reduction in relapse-like drinking behavior, only the highest dose of baclofen produced a weak anti-relapse effect. The highest does of baclofen also caused sedation and significant loss of body weight. These side effects were not observed in CMPPE-treated rats. This demonstrates, not only the efficacy of the GABAB PAM CMPPE in alcohol relapse behavior, but that the therapeutic safety of CMPPE is within acceptable limits, whereas baclofen has questionable efficacy and may cause both sedation and considerable impairment of food intake or changed metabolism.
In our long-term voluntary alcohol drinking rats, baclofen and CMPPE reduced alcohol intake during the ADE. However, relapse-like drinking was not entirely abolished by these compounds. Alcohol intake during the first post-abstinence days was still significantly elevated compared to baseline drinking. This indicates that relapse-like drinking is not entirely under the control of GABAB receptors, and contribution of other receptor systems have a crucial impact on this behavior as well (Vengeliene et al. 2008). This finding differs from the studies performed with non-addicted rats (Colombo et al. 2003, 2006), where baclofen abolished the ADE at a dose as low as 1 mg/kg. However, our data agree with some clinical studies, which have reported low efficacy of baclofen in prolonging abstinence period of individuals with alcohol use disorders at very high doses of this agonist (Beraha et al. 2016; Braillon and Naudet 2017; Reynaud et al. 2017). On the other hand, baclofen seems to have a very different efficacy in alcohol-addicted patients, which could be caused by distinct factors, such as history of drug use, genetic background, and dependence severity. This was also demonstrated in animal studies. For instance, Walker and Koob (2007) have shown that baclofen was more efficacious in reducing motivation to self-administer alcohol in alcohol vapor-exposed rats during acute withdrawal phase compared to control air-exposed animals. Hence, different drinking history in our study may explain the discrepancy between our findings and previous reports by Colombo et al. (2003, 2006).
Clinical studies have been consistent in reporting systemic side effects of baclofen. Similarly, we have found that baclofen treatment produced substantial side effects including induced hypolocomotion, measured as reduced home-cage activity, and significant loss of body weight. Sedative effect of baclofen has been demonstrated in animals administered with higher doses of baclofen (Munzar et al. 2000; Besheer et al. 2004), which may explain self-poisoning reports with baclofen by alcohol-dependent patients (Kiel et al. 2015; Pelissier et al. 2017). However, it has also been shown that repeated baclofen administration led to rapid pharmacological tolerance (Lehmann et al. 2003; Gjoni and Urwyler 2008; Beveridge et al. 2013). Tolerance to sedative effect of drug treatment (e.g., acamprosate) has also been demonstrated in our animal model of alcoholism (Vengeliene et al. 2010); however, the sedative effect of baclofen was only getting stronger after each successive drug administration.
PAMs of GABAB receptors are emerging as a novel class of drugs, which increase the GABAB receptor activity and show fewer side effects than full agonists (Perdona’ et al. 2011). In addition, GABAB PAMs do not appear to provoke development of pharmacological tolerance because PAMs act synergistically with agonists by enhancing activation of the receptor (Lehmann et al. 2003; Gjoni and Urwyler 2008). Hence, many different GABAB PAMs have been synthetized in recent years, and, although similar, they have slightly different mechanisms of action. CMPPE appears to have higher effectiveness compared to the other PAMs, such as CGP7930 and GS39783, as it was shown that CMPPE was also able to stimulate [35S]GTPγS binding to membranes overexpressing GABAB receptors similar to the full agonist GABA (Perdona’ et al. 2011). In our model of alcohol addiction, CMPPE significantly reduced the excessive alcohol consumption during the post-abstinence days, compared to the baseline drinking. However, like baclofen, it did not abolish the ADE. These findings confirm that GABAB receptors may not be fully responsible for relapse-like drinking behavior. Furthermore, we found no significant reduction of locomotor activity or loss of body weight after repeated CMPPE administration, demonstrating that GABAB PAM CMPPE may be a better alternative for the treatment of drug addiction than the full agonist baclofen.
Both alcohol- and cocaine-seeking were abolished by administration of either baclofen or CMPPE in alcohol addicted-like and cocaine addicted-like rats. Hence, activation of GABAB receptors seems to be sufficient and a very effective approach to reduce cue-induced drug-seeking behavior. In agreement, the study of Young et al. (2014) demonstrated that cocaine cue-induced neuronal activation of the ventral striatum, ventral pallidum, amygdala, and orbitofrontal cortex measured in cocaine-dependent participants was prevented by baclofen treatment. Our data is in line with other studies performed in animals subjected to short-term alcohol or cocaine self-administration protocols (Colombo et al. 2003; Filip and Frankowska 2007; Agabio and Colombo 2014; Filip et al. 2015; Froger-Colléaux and Castagné 2016), suggesting that effectiveness of GABAB compounds on drug-seeking responses does not depend on whether an animal is drug dependent or not.
In conclusion, we have demonstrated that both baclofen and CMPPE blocked the drug-seeking behavior in the cue-induced reinstatement paradigm, as well as reduced alcohol drinking during the post-abstinence days in the alcohol addicted-like rats. Our data also showed that the GABAB allosteric modulator CMPPE produced fewer side effects compared to the GABAB full agonist baclofen. Activation of GABAB receptors by either baclofen or CMPPE did not abolish alcohol relapse, indicating that GABAB activation is not sufficient to reduce relapse behavior in alcohol addicted-like animals. Individual differences and the severity of addiction may influence the efficacy of GABAB agonists or PAMs to achieve a positive treatment effect. Furthermore, targeting GABAB receptors may be more effective in reducing certain aspects of addictive-like behavior, such as cue-reactivity, and not as effective in interfering with relapse-like alcohol consumption.
References
Agabio R, Colombo G (2014) GABAB receptor ligands for the treatment of alcohol use disorder: preclinical and clinical evidence. Front Neurosci 8:140
ANSM (2017) Le Baclofène en vie réelle en France entre 2009 et 2015. Usages, persistance et sécurité, et comparaison aux traitements des problèmes d’alcool ayant une autorisation de mise sur le marché. Rapport – 25th of July, 2017 - www.ansm.sante.fr
Beraha EM, Salemink E, Goudriaan AE, Bakker A, de Jong D, Smits N, Zwart JW, Geest DV, Bodewits P, Schiphof T, Defourny H, van Tricht M, van den Brink W, Wiers RW (2016) Efficacy and safety of high-dose baclofen for the treatment of alcohol dependence: a multicentre, randomised, double-blind controlled trial. Eur Neuropsychopharmacol 26:1950–1959
Besheer J, Lepoutre V, Hodge CW (2004) GABA(B) receptor agonists reduce operant ethanol self-administration and enhance ethanol sedation in C57BL/6J mice. Psychopharmacology 174:358–366
Beveridge TJ, Smith HR, Porrino LJ (2013) Differential development of tolerance to the functional and behavioral effects of repeated baclofen treatment in rats. Pharmacol Biochem Behav 106:27–32
Braillon A, Naudet F (2017) Baclofen and alcohol use disorders: from miracle to mirage. Eur Neuropsychopharmacol 27:691–692
Brebner K, Froestl W, Andrews M, Phelan R, Roberts DC (1999) The GABA(B) agonist CGP 44532 decreases cocaine self-administration in rats: demonstration using a progressive ratio and a discrete trials procedure. Neuropharmacology 38:1797–1804
Brebner K, Ahn S, Phillips AG (2005) Attenuation of d-amphetamine self-administration by baclofen in the rat: behavioral and neurochemical correlates. Psychopharmacology 177:409–417
Brown JW, Moeller A, Schmidt M, Turner SC, Nimmrich V, Ma J, Rueter LE, van der Kam E, Zhang M (2016) Anticonvulsant effects of structurally diverse GABA(B) positive allosteric modulators in the DBA/2J audiogenic seizure test: comparison to baclofen and utility as a pharmacodynamic screening model. Neuropharmacology 101:358–369
Cannella N, Halbout B, Uhrig S, Evrard L, Corsi M, Corti C, Deroche-Gamonet V, Hansson AC, Spanagel R (2013) The mGluR2/3 agonist LY379268 induced anti-reinstatement effects in rats exhibiting addiction-like behavior. Neuropsychopharmacology 38:2048–2056
Cannella N, Cosa-Linan A, Büchler E, Falfan-Melgoza C, Weber-Fahr W, Spanagel R (2018) In vivo structural imaging in rats reveals neuroanatomical correlates of behavioral sub-dimensions of cocaine addiction. Addict Biol 23:182–195
Colombo G, Serra S, Brunetti G, Atzori G, Pani M, Vacca G, Addolorato G, Froestl W, Carai MA, Gessa GL (2002) The GABA(B) receptor agonists baclofen and CGP 44532 prevent acquisition of alcohol drinking behaviour in alcohol-preferring rats. Alcohol Alcohol 37:499–503
Colombo G, Serra S, Brunetti G, Vacca G, Carai MA, Gessa GL (2003) Suppression by baclofen of alcohol deprivation effect in Sardinian alcohol-preferring (sP) rats. Drug Alcohol Depend 70(1):105–108
Colombo G, Serra S, Vacca G, Carai MA, Gessa GL (2006) Baclofen-induced suppression of alcohol deprivation effect in Sardinian alcohol-preferring (sP) rats exposed to different alcohol concentrations. Eur J Pharmacol 550:123–126
Deroche-Gamonet V, Belin D, Piazza PV (2004) Evidence for addiction-like behavior in the rat. Science 305:1014–1017
Di Ciano P, Everitt BJ (2003) The GABA(B) receptor agonist baclofen attenuates cocaine- and heroin-seeking behavior by rats. Neuropsychopharmacology 28:510–518
Filip M, Frankowska M (2007) Effects of GABA(B) receptor agents on cocaine priming, discrete contextual cue and food induced relapses. Eur J Pharmacol 571:166–173
Filip M, Frankowska M, Sadakierska-Chudy A, Suder A, Szumiec L, Mierzejewski P, Bienkowski P, Przegaliński E, Cryan JF (2015) GABAB receptors as a therapeutic strategy in substance use disorders: focus on positive allosteric modulators. Neuropharmacology 88:36–47
Froger-Colléaux C, Castagné V (2016) Effects of baclofen and raclopride on reinstatement of cocaine self-administration in the rat. Eur J Pharmacol 777:147–155
Gjoni T, Urwyler S (2008) Receptor activation involving positive allosteric modulation, unlike full agonism, does not result in GABA B receptor desensitization. Neuropharmacology 55:1293–1299
Kasanetz F, Deroche-Gamonet V, Berson N, Balado E, Lafourcade M, Manzoni O, Piazza PV (2010) Transition to addiction is associated with a persistent impairment in synaptic plasticity. Science 328:1709–1712
Kiel LB, Hoegberg LC, Jansen T, Petersen JA, Dalhoff KP (2015) A nationwide register-based survey of baclofen toxicity. Basic Clin Pharmacol Toxicol 116:452–456
Lehmann A, Mattsson JP, Edlund A, Johansson T, Ekstrand AJ (2003) Effects of repeated administration of baclofen to rats on GABA B receptor binding sites and subunit expression in the brain. Neurochem Res 28:387–393
Maccioni P, Zaru A, Loi B, Lobina C, Carai MA, Gessa GL, Capra A, Mugnaini C, Pasquini S, Corelli F, Hyytiä P, Lumeng L, Colombo G (2012) Comparison of the effect of the GABAΒ receptor agonist, baclofen, and the positive allosteric modulator of the GABAB receptor, GS39783, on alcohol self-administration in 3 different lines of alcohol-preferring rats. Alcohol Clin Exp Res 36:1748–1766
Munzar P, Kutkat SW, Miller CR, Goldberg SR (2000) Failure of baclofen to modulate discriminative-stimulus effects of cocaine or methamphetamine in rats. Eur J Pharmacol 408:169–174
Paterson NE, Froestl W, Markou A (2004) The GABAB receptor agonists baclofen and CGP44532 decreased nicotine self-administration in the rat. Psychopharmacology 172:179–186
Pelissier F, de Haro L, Cardona F, Picot C, Puskarczyk E, Sapori JM, Tournoud C, Franchitto N (2017) Self-poisoning with baclofen in alcohol-dependent patients: national reports to French poison control centers, 2008-2013. Clin Toxicol 55:275–284
Perdona' E, Costantini VJ, Tessari M, Martinelli P, Carignani C, Valerio E, Mok MH, Zonzini L, Visentini F, Gianotti M, Gordon L, Rocheville M, Corsi M, Capelli AM (2011) In vitro and in vivo characterization of the novel GABAB receptor positive allosteric modulator, 2-{1-[2-(4-chlorophenyl)-5-methylpyrazolo[1,5-a]pyrimidin-7-yl]-2-piperidinyl}ethanol (CMPPE). Neuropharmacology 61:957–966
Reynaud M, Aubin HJ, Trinquet F, Zakine B, Dano C, Dematteis M, Trojak B, Paille F, Detilleux M (2017) A randomized, placebo-controlled study of high-dose baclofen in alcohol-dependent patients-the ALPADIR study. Alcohol Alcohol 52:439–446
Roberts DC, Andrews MM, Vickers GJ (1996) Baclofen attenuates the reinforcing effects of cocaine in rats. Neuropsychopharmacology 15:417–423
Slattery DA, Markou A, Froestl W, Cryan JF (2005) The GABAB receptor-positive modulator GS39783 and the GABAB receptor agonist baclofen attenuate the reward-facilitating effects of cocaine: intracranial self-stimulation studies in the rat. Neuropsychopharmacology 30:2065–2072
Spanagel R (2009) Alcoholism: a systems approach from molecular physiology to addictive behavior. Physiol Rev 89:649–705
Spanagel R (2017) Animal models of addiction. Dialogues Clin Neurosci 19(2)
Spanagel R, Hölter SM (1999) Long-term alcohol self-administration with repeated alcohol deprivation phases: an animal model of alcoholism? Alcohol Alcohol 34:231–243
Spanagel R, Durstewitz D, Hansson A, Heinz A, Kiefer F, Köhr G, Matthäus F, Nöthen MM, Noori HR, Obermayer K, Rietschel M, Schloss P, Scholz H, Schumann G, Smolka M, Sommer W, Vengeliene V, Walter H, Wurst W, Zimmermann US, Addiction GWAS Resource Group., Stringer S, Smits Y, Derks EM (2013) A systems medicine research approach for studying alcohol addiction. Addict Biol 18:883–896
Takahashi TT, Vengeliene V, Spanagel R (2017) Melatonin reduces motivation for cocaine self-administration and prevents relapse-like behavior in rats. Psychopharmacology 234:1741–1748
Vengeliene V, Bilbao A, Molander A, Spanagel R (2008) Neuropharmacology of alcohol addiction. Br J Pharmacol 154:299–315
Vengeliene V, Celerier E, Chaskiel L, Penzo F, Spanagel R (2009) Compulsive alcohol drinking in rodents. Addict Biol 14:384–396
Vengeliene V, Leonardi-Essmann F, Sommer WH, Marston HM, Spanagel R (2010) Glycine transporter-1 blockade leads to persistently reduced relapse-like alcohol drinking in rats. Biol Psychiatry 68:704–711
Vengeliene V, Noori HR, Spanagel R (2013) The use of a novel drinkometer system for assessing pharmacological treatment effects on ethanol consumption in rats. Alcohol Clin Exp Res 37:E322–E328
Vengeliene V, Bilbao A, Spanagel R (2014) The alcohol deprivation effect model for studying relapse behavior: a comparison between rats and mice. Alcohol 48:313–320
Vengeliene V, Moeller A, Meinhardt MW, Beardsley PM, Sommer WH, Spanagel R, Bespalov A (2016) The Calpain inhibitor A-705253 attenuates alcohol-seeking and relapse with low side-effect profile. Neuropsychopharmacology 41:979–988
Walker BM, Koob GF (2007) The gamma-aminobutyric acid-B receptor agonist baclofen attenuates responding for ethanol in ethanol-dependent rats. Alcohol Clin Exp Res 31:11–18
Xi ZX, Stein EA (1999) Baclofen inhibits heroin self-administration behavior and mesolimbic dopamine release. J Pharmacol Exp Ther 290:1369–1374
Young KA, Franklin TR, Roberts DC, Jagannathan K, Suh JJ, Wetherill RR, Wang Z, Kampman KM, O'Brien CP, Childress AR (2014) Nipping cue reactivity in the bud: baclofen prevents limbic activation elicited by subliminal drug cues. J Neurosci 34:5038–5043
Acknowledgements
We would like to thank Sabrina Koch and Elena Büchler for the excellent technical assistance.
Funding
Financial support for this work was provided by the Bundesministerium für Bildung und Forschung (e:Med program, FKZ: 01ZX1311A (Spanagel et al. 2013)). TTT was funded by CAPES Foundation, Ministry of Education of Brazil, Brasília – DF 70040-020, Brazil.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Vengeliene, V., Takahashi, T.T., Dravolina, O.A. et al. Efficacy and side effects of baclofen and the novel GABAB receptor positive allosteric modulator CMPPE in animal models for alcohol and cocaine addiction. Psychopharmacology 235, 1955–1965 (2018). https://doi.org/10.1007/s00213-018-4893-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-018-4893-9