Abstract
Rationale
The only systematic in vivo studies comparing antipsychotic (AP) effects on nucleus accumbens (NAc) shell and core dopamine (DA) transmission are voltammetric studies performed in pargyline-pretreated, halothane-anaesthetized rats. Studies in freely moving rats not pretreated with pargyline are not available. This study was intended to fill this gap by the use of in vivo microdialysis in freely moving rats.
Methods
Male Sprague-Dawley rats were implanted with microdialysis probes in the NAc shell and core and medial prefrontal cortex (PFCX). The next day, rats were administered intravenously with two or three doses of APs, and dialysate DA was monitored in 10-min samples. Some rats were pretreated with pargyline (75 mg/kg i.p.) and after 1 h were given clozapine or risperidone.
Results
Clozapine, risperidone, quetiapine, raclopride, sulpiride and amisulpride increased DA preferentially in the NAc shell. Such preferential effect on shell DA was not observed after haloperidol, chlorpromazine and olanzapine. In contrast to voltammetric studies, a preferential effect on NAc core DA was not observed after any dose of AP. Pargyline pretreatment did not reduce but actually amplified the preferential effect of clozapine and risperidone on NAc shell DA.
Conclusions
Apart from raclopride and olanzapine, the APs with lower extrapyramidal effects could be distinguished from typical APs on the basis of their ability to preferentially stimulate DA transmission in the NAc shell. There was no relationship between stimulation of PFCX DA and atypical APs profile. The differences between this study and voltammetry studies were not attributable to pargyline pretreatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In spite of the vast number of studies made in the attempt to identify a unitary mechanism for the lower extrapyramidal symptom (EPS) liability of clozapine and second-generation antipsychotics (APs), no consensus has been reached (Abi-Dargham and Laruelle 2005; Arnt and Skarsfeldt 1998; Ginovart and Kapur 2012; Meltzer 1991). Thus, after a period of hot debate, the field has undergone a phase of resigned agnosticism. What is clear is that, depending on the specific AP, different mechanisms might concur to a low EPS profile. Among pharmacodynamic mechanisms are fast off-rate of binding to D2 receptors (Kapur and Seeman 2001) and interactions with non-dopamine (DA) receptors (e.g. 5HT2A, alpha2 adrenergic, muscarinic receptors) (Arnt and Skarsfeldt 1998; Meltzer 1991). Among pharmacokinetic mechanisms is the slow rate of transfer into the brain by simple diffusion and carrier-mediated efflux out of the brain (e.g. P-glycoprotein) (Hartter et al. 2003; Linnet and Ejsing 2008).
Since the seminal studies by Carlsson (1974) (Carlsson and Lindqvist 1963), APs are known to increase all presynaptic indices of DA transmission, including synthesis, metabolism and release of DA and DA neuron firing activity (Anden et al. 1970; Bunney 1988; Imperato and Di Chiara 1985).
Along this line, an early explanation of the low EPS liability of clozapine is that of a “limbic specificity”, i.e. the ability of activating DA turnover preferentially in the nucleus accumbens (NAc) as compared to the dorsal striatum (Anden and Stock 1973; Bartholini 1976; White and Wang 1983).
The NAc, however, is a heterogeneous area and has been distinguished into a ventromedial shell and a dorsolateral core that differ in terms of neurochemical composition, input and output connections, physiological and pharmacological responses and behavioural functions (Deutch and Cameron 1992; Di Chiara 2002; Heimer et al. 1997; Zahm 2000).
Clozapine and most second-generation antipsychotics stimulate to a larger extent Fos-like immunoreactivity in the NAc shell than in the dorsolateral striatum and in the core, while the opposite applies to first-generation APs (Deutch et al. 1992; Dilts et al. 1993; Robertson and Fibiger 1992). Another property of APs like clozapine, risperidone and olanzapine that block 5HT2A receptors is the ability to increase extracellular DA in the medial prefrontal cortex (PFCX) (Ichikawa et al. 1998, 2001; Imperato and Angelucci 1989; Kuroki et al. 1999; Moghaddam and Bunney 1990). This property has been related to their low EPS liability and/or the ability to control negative symptoms (Abi-Dargham et al. 2002; Knable and Weinberger 1997).
In spite of the interest of a shell vs core dichotomy for the action of APs, the only available comparative studies on the acute in vivo effects of APs on extracellular DA in the NAc shell and core are those of Marcus et al. (1996, 2000, 2002) and Franberg et al. (2008) who utilized differential normal pulse voltammetry in halothane-anaesthetized rats pretreated with pargyline, in order to avoid the interfering influence of DOPAC. It is notable that, in the same studies, brain microdialysis was utilized to monitor extracellular DA in the whole NAc, without distinguishing between shell and core. This is also the case of the studies by Volonte et al. (1997) and Kuroki et al. (1999). The only exception is the study by Shilliam and Dawson (2005) dealing exclusively with clozapine.
Therefore, no systematic in vivo study in freely moving rats not pretreated with pargyline is available. In order to fill this gap, we decided to embark in a systematic comparative microdialysis study of the acute effects of AP on extracellular DA in the NAc shell and core and medial prefrontal cortex (PFCX). Such a study might have predictive translational value, due to the high degree of concordance between microdialysis and PET as a means to monitor extracellular DA dynamics in specific brain areas (Morris et al. 2008; Narendran et al. 2014).
AP representative of different pharmacological categories were selected, namely haloperidol and chlorpromazine (high to intermediate D2R affinity and EPS liability), clozapine and quetiapine (low D2R, high to intermediate 5HT2A affinity and low EPS liability), amperozide (high 5HT2A, low D2R affinity and weak AP activity), risperidone and olanzapine (high D2R and 5HT2A affinity and mild EPS liability), raclopride (a benzamide with high D2R affinity, fast plasma-brain equilibration and high EPS liability) and, finally, (S)-sulpiride and amisulpride (benzamides with high D2R affinity, slow plasma-brain equilibration and low EPS liability) (Cassano et al. 1975; Csernansky et al. 1994; Harnryd et al. 1984; Leucht et al. 2013; Mauri et al. 1996; Rummel-Kluge 2010).
Methods and materials
Animals
Male Sprague-Dawley rats (Harlan Laboratories, Italy) weighing 250 to 275 g at arrival in the animal facility were kept under standard conditions of temperature and humidity, in an artificial light dark cycle (light on 08.00 a.m., off 08.00 p.m.) and were housed six per cage (cage size, 40 × 70 × 20 cm) for at least 1 week before microdialysis surgery procedures. They had free access to food and water, except during microdialysis testing procedures. All procedures and experiments were carried out in an animal facility according to Italian (D.L. 116/92 and 152/06) and European Council directives (609/86 and 63/2010) and in compliance with the approved animal policies by the Ethical Committee for Animal Experiments (CESA, University of Cagliari) and the Italian Department of Health.
Probe preparation
Concentric dialysis probes (dialysing portion 1.5 mm for NAc and 3.0 mm for PFCX) were prepared with AN69 fibres (310 μm o.d., 220 μm i.d., Gambro Hospal, Italy) by a modification of the method described by Tanda and Di Chiara (1998).
Surgery
Rats were anaesthetized with Equitesin (2.5 mg/kg i.p.), placed in a stereotaxic apparatus and implanted with two dialysis probes aimed at the NAc shell on one side and at the NAc core or at the PFCX on the other side, according to the rat brain atlas of Paxinos and Watson (1998) (uncorrected coordinates: PFCX, anterior = +3.5, L = ±0.6, from bregma; vertical = 5.0 from dura; NAc shell, A = +2.0, L = 0.9, V = 8.0; NAc core, A = +1.6, L = 1.5, V = 7.6).
In order to perform intravenously (i.v.) drug administration, a catheter (Silastic, Dow Corning Corporation, Michigan, USA) was inserted in the right jugular vein according to the technique previously described (Lecca et al. 2006).
Microdialysis
Experiments were performed 24 h after probe implant on freely moving rats. Ringer’s solution (147.0 mM NaCl, 2.2 mM CaCl2 and 4.0 mM KCl) was pumped through the dialysis probes at a constant rate of 1 μl/min. Collection of samples started after 30 min. After stabilization of dialysate DA (i.e. after about 1 h), rats were administered with drugs or saline.
Analytical procedure
Dialysate samples (10 μl) were taken every 10 min and injected without purification into an HPLC apparatus equipped with a reverse-phase column (C8 3.5 μm, Waters, Mildford Massachusetts) and a coulometric detector (ESA Coulochem II, Bedford, MA) to quantify DA. The oxidation and reduction electrodes of the analytical cell (5014B, ESA, Bedford, MA) were set at +130 mV and −175 mV, respectively. The mobile phase, containing 50 mM NaH2PO4, 0.1 mM Na2EDTA, 0.5 mM n-octyl sulfate and 15 % (v/v) methanol (pH adjusted to 5.5 with Na2HPO4), was pumped with a Jasco pump at 1.0 ml/min. Assay sensitivity for DA was 5 fmol per sample.
Histology
At the end of the experiment, rats were transcardially perfused with 100 ml saline and 500 ml of 4 % formaldehyde, 1 % calcium acetate and 100 mM NaCl solution. Probes were removed, and brains were cut on a vibratome in serial coronal slices oriented according to the atlas Paxinos and Watson (Paxinos and Watson 1998). Sections were processed in order to identify the location of the probes in relation to the PFCX and shell and core subdivisions of the NAc (Fig. 1).
Schematic localization of microdialysis probe dialysing portion within the PFCX, the NAc shell (sh) and core (co) according to Paxinos and Watson (1998)
Drugs
Haloperidol, chlorpromazine, olanzapine, sulpiride (obtained from commercial sources), amperozide hydrochloride (Tocris Bioscience, UK), risperidone and pargyline hydrochloride (Sigma-Aldrich, Italy) were dissolved in 0.9 % NaCl. Clozapine and amisulpride (Tocris Bioscience, UK), raclopride (Sigma-Aldrich, Italy) and quetiapine (kindly provided by Astra Zeneca) were all dissolved in a minimal amount of acetic acid and 0.9 % NaCl buffered to pH 7.4 with 1 N NaOH.
All drugs were administered i.v. except for pargyline that was given i.p. Drug doses were selected on the basis of the results of previous studies from our laboratory (Imperato and Di Chiara 1985) and of pilot experiments intended to identify the threshold dose for maximal increase of dialysate DA (that for APs corresponds to twice the basal values) in the most sensitive area of the accumbens (either shell or core). Once this dose was identified, a lower, and in some cases, a higher dose, was also studied. The higher dose level of clozapine and risperidone was taken from the study by Marcus et al. (1996) in order to compare the effect of these drugs in control and pargyline-pretreated rats. In the case of amperozide, we selected a dose about seven times higher, on a milligramme per kilogramme basis, than the total daily dose (20 mg) utilized in the study by Axelsson et al. (1991).
Three dose levels (in mg/kg) were studied for haloperidol (0.006, 0.0125, 0.025), clozapine (1.0, 2.0, 5.0), olanzapine (0.125, 0.25, 0.50), risperidone (0.05, 0.1, 1.0), quetiapine (2.5, 5.0, 20.0) and amisulpride (1.0, 2.0, 4.0). Two dose levels were studied for chlorpromazine (0.25, 0.5), raclopride (0.025, 0.075), sulpiride (10.0, 18.0) and amperozide (1.0, 2.0). A posteriori, taking into account that in the present study drugs were given i.v., the range of doses selected compares favourably, on a milligramme per kilogramme basis, with individual doses of intramuscular and oral APs utilized in the clinic (Gardner et al. 2010).
Statistics
Three-way repeated measures ANOVA with brain area, drug dose (vehicle and two or three doses, depending on the group) and time as factors were applied to the data obtained from serial assays of DA. Four-way ANOVA (factors: area, pretreatment, treatment) for repeated measures over time was carried out for the analysis of data obtained from pargyline experiments. For graphical purposes, data were normalized as percentage of basal DA values. For clarity, vehicle time course has been omitted from the figures but was included in the analysis. Basal DA values were means of three consecutive samples differing no more than 10 %. Results from treatments showing overall changes were subjected to post hoc Tukey’s test with significance at p < 0.05.
Results
Basal dialysate dopamine
Basal values of DA (fmoles/10 min sample ± SEM) in the three brain areas under study were PFCX, 9.6 ± 1.3 (N = 146); NAc shell, 48.6 ± 7.8 (N = 168); and NAc core, 53.5 ± 8.5 (N = 164).
No significant differences between treatment groups were found for each brain area.
Effect of antipsychotics on NAc shell and core and prefrontal cortex dopamine
Haloperidol (6.0, 12.5 and 25.0 μg/kg) dose-dependently increased dialysate DA in the NAc shell and core and to a lesser extent in the PFCX (Fig. 2). The time course of shell DA after 12.5 and 25.0 μg/kg was biphasic with a peak followed by a lower shoulder. In the core, no initial peak but only a progressive increase to a plateau was observed. Saline administration in control group did not modify dialysate DA in the PFCX, shell and core (data not shown). Three-way ANOVA revealed a main effect of dose [F (3,40) = 82.33; p < 0.001], area [F (2,40) = 29.25; p < 0.001] and time [F (18,720) = 14.59, p < 0.001] and an interaction of area × dose [F (6,40) = 4.78, p < 0.001], area × time [F (36,720) = 2.88; p < 0.001] and dose × time [F (54,720) = 3.76; p < 0.001]. Post hoc analysis showed that haloperidol increased dialysate DA to a greater extent in the NAc shell and core than in the PFCX without differences between shell and core. Analysis of NAc shell and core data alone for all the doses by three-way ANOVA or for each dose of haloperidol also failed to reveal post hoc differences between shell and core.
Effect of haloperidol (6, 12.5 and 25 μg/kg i.v.; saline not shown) on NAc shell (circles), NAc core (squares) and PFCX (triangles) dialysate DA. Results are expressed as mean ± SEM of dialysate DA levels expressed as percentage of basal values. Solid symbols: p < 0.05 vs the respective basal values; *p < 0.05 NAc shell vs PFCX; #p < 0.05 NAc core vs PFCX; §p < 0.05 NAc shell vs NAc core; $p < 0.05 NAc shell vs the corresponding time point of saline group; +p < 0.05 NAc core vs the corresponding time point of saline group; °p < 0.05 PFCX vs the corresponding time point of saline group (NAc shell, N = 17; NAc core, N = 18; PFCX, N = 17)
Chlorpromazine(0.25 and 0.5 mg/kg), like haloperidol, dose-dependently increased dialysate DA in the NAc shell, in the core and to a lesser extent, in the PFCX (Fig. 3). The time course of the effect of 0.5 mg/kg chlorpromazine on shell DA was characterized, like that of haloperidol, by a sharp peak followed by a shoulder. In contrast, after the same dose, DA increased in the core to a plateau without an initial peak. Saline administration in control group did not modify dialysate DA in the PFCX, shell and core (data not shown). Three-way ANOVA revealed a main effect of dose [F (2,27) = 58.40, p < 0.001], area [F (2,27) = 11.64; p < 0.001] and time [F (18,486) = 36.56, p < 0.001] and an interaction of area × dose [F (4,27) = 3.31, p < 0.05], area × time [F (36,486) = 5.83, p < 0.001], dose × time [F (36,486) = 11.49, p < 0.001] and area × dose × time [F (72,486) = 2.89, p < 0.001]. Post hoc analysis showed a larger increase of dialysate DA in the NAc shell and in the core as compared to the PFCX but no differences between shell and core. No differences on post hoc test were obtained by three-way ANOVA of the shell and core data alone for all the doses or for each dose of chlorpromazine.
Effect of chlorpromazine (0.25 and 0.5 mg/kg i.v.; saline not shown) on NAc shell (circles), NAc core (squares) and PFCX (triangles) dialysate DA. Results are expressed as mean ± SEM of dialysate DA levels expressed as percentage of basal values. Solid symbols: p < 0.05 vs the respective basal values; *p < 0.05 NAc shell vs PFCX; #p < 0.05 NAc core vs PFCX; §p < 0.05 NAc shell vs NAc core; $p < 0.05 NAc shell vs the corresponding time point of saline group; +p < 0.05 NAc core vs the corresponding time point of saline group; °p < 0.05 PFCX vs the corresponding time point of saline group (NAc shell, N = 12; NAc core, N = 12; PFCX, N = 12)
Raclopride (25 and 75 μg/kg) increased dialysate DA in the NAc shell and to a lesser extent in the core and in the PFCX (Fig. 4). The time course of raclopride effect in the shell consisted of a sharp increase peaking 20–30 min post-drug. Saline administration in control group did not modify dialysate DA in the PFCX, shell and core (data not shown). Three-way ANOVA revealed a main effect of dose [F (2,30) = 32.27, p < 0.001], area [F (2,30) = 8.98, p < 0.001] and time [F (18,540) = 67.01, p < 0.001] and an interaction of area × dose [F (4,30) = 7.97, p < 0.001], area × time [F (36,540) = 7.94, p < 0.001], dose × time [F (36,540) = 16.72, p < 0.001] and area × dose × time [F (72,540) = 3.19, p < 0.001]. Post hoc analysis showed that raclopride induced a greater increase of dialysate DA in the shell as compared to the core and PFCX.
Effect of raclopride (25 and 75 μg/kg i.v.; saline not shown) on NAc shell (circles), NAc core (squares) and PFCX (triangles) dialysate DA. Results are expressed as mean ± SEM of dialysate DA levels expressed as percentage of basal values. Solid symbols: p < 0.05 vs the respective basal values; *p < 0.05 NAc shell vs PFCX; §p < 0.05 NAc shell vs NAc core; $p < 0.05 NAc shell vs the corresponding time point of saline group; +p < 0.05 NAc core vs the corresponding time point of saline group; °p < 0.05 PFCX vs the corresponding time point of saline group (NAc shell, N = 13; NAc core, N = 13; PFCX, N = 13)
Clozapine (1.0 and 2.0 mg/kg) increased dialysate DA in the PFCX to a larger extent than in the NAc shell but not in the core (Fig. 5). Saline administration in control group did not modify dialysate DA in the PFCX, shell and core (data not shown). Three-way ANOVA revealed a main effect of dose [F (2,33) = 23.98, p < 0.001], area [F (2,33) = 26.96, p < 0.001] and time [F (18,594) = 56.87, p < 0.001] and an interaction of area × dose [F (4,33) = 6.94, p < 0.001], area × time [F (36,594) = 17.38, p < 0.001], dose × time [F (36,594) = 18.34, p < 0.001] and area × dose × time [F (72,594) = 5.00, p < 0.001]. Post hoc analysis showed that clozapine elicited a greater increase of dialysate DA in the PFCX as compared to the shell and core. Three-way ANOVA and post hoc test on the NAc shell and core data showed that clozapine elicited a greater increase of dialysate DA in the shell as compared to the core [F (1,25) = 47.36, p < 0.001].
Effect of clozapine (1 and 2 mg/kg i.v.; saline not shown) on NAc shell (circles), NAc core (squares) and PFCX (triangles) dialysate DA. Results are expressed as mean ± SEM of dialysate DA levels expressed as percentage of basal values. Solid symbols: p < 0.05 vs the respective basal values; *p < 0.05 NAc shell vs PFCX; #p < 0.05 NAc core vs PFCX; §p < 0.05 NAc shell vs NAc core; $p < 0.05 NAc shell vs the corresponding time point of saline group; °p < 0.05 PFCX vs the corresponding time point of saline group (NAc shell, N = 14; NAc core, N = 13; PFCX, N = 15)
Risperidone (50 and 100 μg/kg) increased dialysate DA in the PFCX more than in the NAc shell and core and more in the shell as compared to the core after the higher dose (Fig. 6). The time course of DA showed an early peak in the shell and a plateau in the core after the lower dose. Saline administration in control group did not modify dialysate DA in the PFCX, shell and core (data not shown). Three-way ANOVA revealed a main effect of dose [F (2,30) = 127.20, p < 0.001], area [F (2,30) = 22.71, p < 0.001] and time [F (18,540) = 83.57, p < 0.001] and an interaction of area × dose [F (4,30) = 10.43, p < 0.001], area × time [F (36,540) = 9.60, p < 0.001], dose × time [F (36,540) = 22.00, p < 0.001] and area × dose × time [F (72, 540) = 3.60, p < 0.001]. Post hoc test showed that risperidone induced a greater increase of dialysate DA in the PFCX as compared to the shell and core and a greater increase of dialysate DA in the shell as compared to the core.
Effect of risperidone (50 or 100 μg/kg i.v.; saline not shown) on NAc shell (circles), NAc core (squares) and PFCX (triangles) dialysate DA. Results are expressed as mean ± SEM of dialysate DA levels expressed as percentage of basal values. Solid symbols: p < 0.05 vs the respective basal values; *p < 0.05 NAc shell vs PFCX; #p < 0.05 NAc core vs PFCX; §p < 0.05 NAc shell vs NAc core; $p < 0.05 NAc shell vs the corresponding time point of saline group; +p < 0.05 NAc core vs the corresponding time point of saline group; °p < 0.05 PFCX vs the corresponding time point of saline group (NAc shell, N = 13; NAc core, N = 13; PFCX, N = 13)
Olanzapine (0.125, 0.25 and 0.5 mg/kg) increased dialysate DA in the PFCX to a greater extent than in the shell and core, but no differences were obtained between shell and core (Fig. 7). The time course of DA showed an early peak in the shell and a plateau in the core after the intermediate dose tested. Saline administration in control group did not modify dialysate DA in the PFCX, shell and core (data not shown). Three-way ANOVA revealed a main effect of dose [F (3,38) = 79.41, p < 0.001], area [F (2,38) = 18.81, p < 0.001] and time [F (18,684) = 111.91, p < 0.001] and an interaction of area × dose [F (6,38) = 3.96, p < 0.001], area × time [F (36,684) = 16.8, p < 0.001], dose × time [F (54,684) = 16.1, p < 0.001] and area × dose × time [F(108,684) = 5.87, p < 0.001]. Post hoc analysis showed that olanzapine increased to a greater extent dialysate DA in the PFCX as compared to the shell and core of the NAc, but no differences were obtained between shell and core. Analysis of NAc shell and core data alone for all the doses by three-way ANOVA or for each dose of olanzapine also failed to reveal post hoc differences between shell and core (Fig. 7).
Effect of olanzapine (0.125, 0.25 and 0.5 mg/kg i.v.; saline not shown) on NAc shell (circles), NAc core (squares) and PFCX (triangles) dialysate DA. Results are expressed as mean ± SEM of dialysate DA levels expressed as percentage of basal values. Solid symbols: p < 0.05 vs the respective basal values; *p < 0.05 NAc shell vs PFCX; #p < 0.05 NAc core vs PFCX; §p < 0.05 NAc shell vs NAc core; $p < 0.05 NAc shell vs the corresponding time point of saline group; +p < 0.05 NAc core vs the corresponding time point of saline group; and °p < 0.05 PFCX vs the corresponding time point of saline group (NAc shell, N = 17; NAc core, N = 17; PFCX, N = 16)
Quetiapine (2.5, 5.0 and 20.0 mg/kg) increased dialysate DA in the NAc shell but not in the core. DA increased in the PFCX only after the highest dose (Fig. 8). Saline administration in control group did not modify dialysate DA in the PFCX, shell and core (data not shown). Three-way ANOVA revealed a main effect of dose [F(3,51) = 23.36, p < 0.001] and time [F (18,918) = 21.16, p < 0.001] and an interaction of area × dose [F (6,51) = 2.78, p < 0.05], area × time [F (36,918) = 1.97, p < 0.001] and dose × time [F (54,918) = 4.61, p < 0.01]. Three-way ANOVA of only shell and core values showed that quetiapine elicited a greater increase of dialysate DA in the shell as compared to the core [F(1,31) = 4.65, p < 0.05].
Effect of quetiapine (2.5, 5.0 and 20.0 mg/kg i.v.; saline not shown) on NAc shell (circles), NAc core (squares) and PFCX (triangles) dialysate DA. Results are expressed as mean ± SEM of dialysate DA levels expressed as percentage of basal values. Solid symbols: p < 0.05 vs the respective basal values; *p < 0.05 NAc shell vs PFCX; #p < 0.05 NAc core vs PFCX; §p < 0.05 NAc shell vs NAc core; $p < 0.05 NAc shell vs the corresponding time point of saline group; °p < 0.05 PFCX vs the corresponding time point of saline group (NAc shell, N = 21; NAc core, N = 19; PFCX, N = 27)
Amisulpride (1.0, 2.0 and 4.0 mg/kg) slowly and lastingly increased dialysate DA in the NAc shell and core but not in the PFCX (Fig. 9), and this effect was more pronounced in the shell than in the core. Saline administration in control group did not modify dialysate DA in the PFCX, shell and core (data not shown). Three-way ANOVA revealed a main effect of dose [F (3,51) = 13.8, p < 0.0001], area [F (2,51) = 43.74, p < 0.0001] and time [F (24,1224) = 7.63, p < 0.0001] and an interaction of area × dose [F (6,51) = 8.01, p < 0.0001], area × time [F (48,1224) = 8.99, p < 0.0001], dose × time [F (72,1224) = 1.90, p < 0.0001] and area × dose × time [F (144,1224) = 1.92, p < 0.0001]. Post hoc analysis showed that amisulpride elicited a greater stimulation of dialysate DA in the NAc shell and core as compared to the PFCX.
Effect of amisulpride (1, 2.0 and 4.0 mg/kg i.v.; saline not shown) on NAc shell (circles), NAc core (squares) and PFCX (triangles) dialysate DA. Results are expressed as mean ± SEM of dialysate DA levels expressed as percentage of basal values. Solid symbols: p < 0.05 vs the respective basal values; *p < 0.05 NAc shell vs PFCX; #p < 0.05 NAc core vs PFCX; §p < 0.05 NAc shell vs NAc core; $p < 0.05 NAc shell vs the corresponding time point of saline group; +p < 0.05 NAc core vs the corresponding time point of saline group (NAc shell, N = 21; NAc core, N = 20; PFCX, N = 21)
(S)-sulpiride (10 and 18 mg/kg) elicited a slow and long-lasting increase of dialysate DA in the NAc shell and core but not in the PFCX (Fig. 10). Saline administration in control group did not modify dialysate DA in the PFCX, shell and core (data not shown). Three-way ANOVA revealed a main effect of dose [F (2,30) = 18.76, p < 0.001], area [F (2,30) = 13.85, p < 0.01] and time [F (24,720) = 9.70, p < 0.001] and an interaction of area × dose [F (4,30) = 4.58, p < 0.01], area × time [F (48,720) = 2.51, p < 0.001] and dose × time [F (48,720) = 3.47, p < 0.001]. Post hoc analysis showed that sulpiride increased to a larger extent dialysate DA in the NAc shell and core as compared to the PFCX, but no differences were observed between shell and core. Three-way ANOVA and post hoc test of dialysate DA in the NAc shell and core confirmed the lack of shell vs core differences obtained in the analysis that included PFCX values. However, analysis of data for each dose showed that the highest dose of sulpiride elicited a greater increase of dialysate DA in the shell as compared to the core [F(2,12) = 18.17, p < 0.001].
Effect of (S)-sulpiride (10 and 18.0 mg/kg i.v.; saline not shown) on NAc shell (circles), NAc core (squares) and PFCX (triangles) dialysate DA. Results are expressed as mean ± SEM of dialysate DA levels expressed as percentage of basal values. Solid symbols: p < 0.05 vs the respective basal values; *p < 0.05 NAc shell vs PFCX; §p < 0.05 NAc shell vs NAc core; $p < 0.05 NAc shell vs the corresponding time point of saline group; +p < 0.05 NAc core vs the corresponding time point of saline group (NAc shell, N = 15; NAc core, N = 14; PFCX, N = 20)
Amperozide (1.0 and 2.0 mg/kg) increased dialysate DA in the PFCX but not in the NAc shell and core (Fig. 11). Saline administration in control group did not modify dialysate DA in the PFCX, shell and core (data not shown). Three-way ANOVA revealed a main effect of dose [F (2,27) = 58.31, p < 0.001], area [F (2,27) = 72.39, p < 0.001] and time [F (18,486) = 41.00, p < 0.001] and an interaction of area × dose [F (4,27) = 38.41, p < 0.001], area × time [F (36,486) = 29.73, p < 0.001], dose × time [F (36,486) = 16.83, p < 0.001] and area × dose × time [F (72, 486) = 15.80, p < 0.001]. Post hoc analysis showed that amperozide increased to a greater extent dialysate DA in the PFCX as compared to the shell and core of the NAc.
Effect of amperozide (1.0 and 2.0 mg/kg i.v.; saline not shown) on NAc shell (circles), NAc core (squares) and PFCX (triangles) dialysate DA. Results are expressed as mean ± SEM of dialysate DA levels expressed as percentage of basal values. Solid symbols: p < 0.05 vs the respective basal values; *p < 0.05 NAc shell vs PFCX; #p<0.05 NAc core vs PFCX;°p < 0.05 PFCX vs the corresponding time point of saline group (NAc shell, N = 12; NAc core, N = 12; PFCX, N = 12)
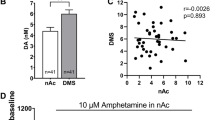
Effects of pargyline pretreatment on the effect of clozapine and risperidone on NAc shell and core dopamine
Pargyline (75 mg/kg i.p.) increased dialysate DA in shell and core to about 280 % (data not shown). Pretreatment with pargyline 1 h before clozapine (5 mg/kg, Fig. 12a) and risperidone (1 mg/kg, Fig. 12b) strongly potentiated the increase of dialysate DA induced in normal animals. In rats pretreated with pargyline, the increase of DA in the shell vs core was larger than that observed in normal rats. In Fig. 12a, four-way ANOVA revealed a main effect of pretreatment (saline or pargyline) [F (1,23) = 102.01, p < 0.001], treatment (saline or clozapine) [F (1,23) = 72.93, p < 0.001], area [F(1,23) = 177.33, p < 0.01] and time [F (18,414) = 31.828, p < 0.001] and an interaction of pretreatment × treatment × area [F (1,23) = 23.69, p < 0.001] and pretreatment × treatment × area × time [F (18,414) = 1.62, p < 0.05]. Post hoc analysis showed that pargyline potentiated clozapine effect in the NAc shell and core, and this effect was higher in the shell vs core. In Fig. 12a four-way ANOVA revealed a main effect of pretreatment (saline or pargyline) [F (1,26) = 14.27, p < 0.001], treatment (saline or risperidone) [F (1,26) = 27.45, p < 0.001], area [F (1,26) = 4.54, p < 0.05] and time [F (18,468) = 12.62, p < 0.001] and an interaction of area × treatment [F (1,26) = 4.5, p < 0.05], treatment × time [F (18,468) = 10.12, p < 0.001], pretreatment × treatment × time [F (18,468) = 4.21, p < 0.01] and area × treatment × time [F (18,468) = 2.88, p < 0.01]. Post hoc analysis showed that pargyline potentiated risperidone effect in the NAc shell but not in the core.
Effect of 1-h pretreatment with pargyline (75 mg/kg i.p.) on a clozapine- (5 mg/kg iv; saline not shown) or b risperidone- (1 mg/kg iv; saline not shown) induced dialysate DA increase in the NAc shell and core. Diamond and triangle: shell and core of pargyline-pretreated groups, respectively; circle and square: shell and core of saline-pretreated groups, respectively. Results are expressed as mean ± SEM of dialysate DA levels expressed as percentage of basal values. In pargyline-pretreated rats, basal values correspond to the mean of the last three samples of 1-h pargyline pretreatment. Solid symbols: p < 0.05 vs the respective basal values. Referred to pargyline-pretreated groups, § p < 0.05 NAc shell vs NAc core; $p < 0.05 NAc shell vs the corresponding time point of saline group; +p < 0.05 NAc core vs the corresponding time point of saline group; #p < 0.05 vs the corresponding saline-pretreated group. (a NAc shell, N = 16; NAc core, N = 15; b NAc shell, N = 17; NAc core, N = 18)
Discussion
The present report is, to our knowledge, the first systematic comparative microdialysis study of the acute effect of APs on extracellular DA in NAc shell and core and medial PFCX of freely moving rats. Clozapine, quetiapine, risperidone, sulpiride, amisulpride and raclopride increased, at least at one dose level, dialysate DA preferentially in the shell vs core while haloperidol, chlorpromazine and olanzapine failed to do so at any dose tested. Clozapine, risperidone, quetiapine and olanzapine increased DA also in the PFCX, but this property was not always associated to a preferential DA increase in the shell, as sulpiride and amisulpride did not show it.
All APs, with the exception of sulpiride and amisulpride, showed a prominent shell DA peak on the first hour post-drug, followed by a shoulder. No DA peak, but a progressive increase to a plateau, was observed in the core. The early shell DA peak would result from fast distribution of lipophilic AP to the highly perfused brain compartment (Balant-Gorgia and Balant 1987; Byerly and DeVane 1996; Jann et al. 1993; Javaid 1994; Johnson et al. 2011; Nord and Farde 2011; Verghese et al. 1991). This interpretation is consistent with the observation that amisulpride and sulpiride, which slowly distribute to the brain, lack the initial peak (Mauri et al. 1996; Rosenzweig et al. 2002).
The reason for such a different temporal profile of the response of dialysate DA to APs in the shell and in the core might derive in part from different DA dynamics related to a more efficient DA uptake in the core. Due to this, changes in burst firing activity of DA neurons would induce larger changes in extracellular DA in the shell than in the core (Calipari et al. 2012; Jones et al. 1996; Wu et al. 2001).
Among the three areas investigated, the effect common to all antipsychotics was the ability to increase dialysate DA in the NAc shell, consistent with an important role of this effect in the action of APs.
Raclopride’s preferential effect in the shell might be due to the short duration of action of this AP and to the rapid plasma/brain equilibration of its concentrations, generating a prominent early DA peak in the NAc that, given the short half-life of the drug, dominates the picture and drives the overall effect of the drug (see below).
The observation that APs that block 5HT2A receptors with high affinity preferentially increase dialysate DA in the shell might suggest that blockade of 5HT2A receptors specifically potentiates the stimulatory influence of D2 receptor blockade on DA release in the NAc shell. However, while Andersson et al. (1995) reported that ritanserin, a 5HT2A/2C antagonist, potentiates the DA stimulant properties of raclopride in the NAc, Liegeois et al. (2002) reported that ML100907, a selective 5HT2A antagonist, partially prevents the increase of dialysate DA induced by haloperidol in the NAc. However, both these studies did not differentiate shell from core in the NAc and therefore cannot be compared with our study.
The observation that sulpiride and amisulpride preferentially activate in vivo DA transmission in the shell was unexpected, in view of their high affinity and selectivity for D2 receptors that makes them quite different from clozapine. Although amisulpride has been reported to preferentially stimulate DA metabolism in the NAc as compared to the caudate-putamen, again no distinction has been made between shell and core (Schoemaker et al. 1997). These drugs being highly selective for D2 receptors, a pharmacodynamic mechanism for their preferential shell effect is unlikely. We would rather suggest a pharmacokinetic mechanism related to their slow accumulation into the brain.
As far as the voltammetric studies by Marcus et al. (1996, 2000, 2002) are concerned, many discrepancies are found. According to their studies, clozapine and risperidone increase DA preferentially in the shell after lower doses and in the core after higher doses. Instead, we consistently observed a selective (clozapine) or a preferential (risperidone) increase of DA in the shell. In general, we failed to observe a preferential increase of DA in the core even after haloperidol and chlorpromazine. These discrepancies cannot be accounted for by differences in the sensitivity of microdialysis vs voltammetry since results refer to relative (% of basal) rather than absolute differences between shell and core.
In order to shed light on this issue, we set to test the effect of clozapine and risperidone at the same doses utilized by Marcus et al. (1996) in rats pretreated with pargyline. In contrast to Marcus et al. (1996), pargyline pretreatment did not induce a preferential core increase of extracellular DA but actually amplified the preferential effect on the shell induced by clozapine and risperidone in rats not pretreated with pargyline. These observations indicate that the discrepancies between our observations and those of Marcus et al. (2000, 2002) are not due to pargyline pretreatment but, eventually, to the voltammetric technique itself and/or to the use of anaesthetized instead of freely moving rats. Indeed halothane anaesthesia has been reported to reduce the increase of striatal dialysate DA induced by haloperidol and to increase that elicited by clozapine (Adachi et al. 2003) while fluothane anaesthesia has been reported to attenuate the effect of clozapine and risperidone (Adachi et al. 2008).
Amperozide is a case of its own and deserves a separate discussion. In our hands, amperozide, given i.v. at doses (on a mg/kg basis) about seven times the total daily oral dose given to patients in the study by Axelsson et al. (1991), failed to increase DA in dialysates from the NAc shell, in agreement with some reports (Hertel et al. 1996; Kuroki et al. 1999) but at variance with others (Ichikawa and Meltzer 1992, 2000; Marcus et al. 1996; Nomikos et al. 1994). However, in the present study, 2.0 mg/kg i.v. of amperozide increased to 400 % dialysate DA in the PFCX and at 6 mg/kg i.p. up to 300 % in the bed nucleus stria terminalis (Carboni et al. 2000). Amperozide is a weak D2 ligand but a strong 5HT2A receptor ligand (Svartengren and Simonsson 1990). Early reports suggested that amperozide had antipsychotic efficacy and low EPS (Axelsson et al. 1991). Subsequent clinical experience, however, did cast doubt on its effectiveness as an antipsychotic, leading to interruption of its development (Breier 1995). Thus, the amperozide case illustrates the relationship between the ability to increase DA in the NAc shell and the effectiveness of a drug as an AP.
APs increase NAc shell Fos-like immunoreactivity and this effect has been related to their antipsychotic activity (Robertson et al. 1994). Typical APs also increase Fos-like immunoreactivity in the dorsal caudate-putamen and this effect has been related to EPS liability (Robertson et al. 1994). In principle, stimulation of D1 receptors by DA released as a result of D2/D3 blockade might contribute to Fos-like immunoreactivity induced by APs. However, Fos activation in the dorsolateral striatum by typical APs is resistant to D1 blockade by SCH 23390 (Dragunow et al. 1990; Wirtshafter and Osborn 2005). No information is available on the effect of D1 blockade on Fos activation by APs in the NAc shell.
The stimulatory properties of APs on PFCX DA differentiate a class of APs, namely clozapine, risperidone, olanzapine and quetiapine, that, at clinically effective doses, blocks 5HT2A receptors. This observation, in turn, is consistent with previous studies (Ichikawa et al. 1998, 2001; Imperato and Angelucci 1989; Kuroki et al. 1999; Moghaddam and Bunney 1990). However, this effect is not a marker of low EPS liability as amisulpride and sulpiride, drugs without 5HT2A receptor affinity, do not increase PFCX DA. This observation suggests that blockade of 5HT2A receptors is not a prerequisite for low EPS liability.
The association of low EPS liability and preferential activation of NAc shell vs core DA transmission might be due to the fact that these two properties share some pharmacodynamic and pharmacokinetic determinants. During the initial phase of drug distribution, when most of the drug is still in the blood, highly lipophilic APs, like clozapine, quetiapine, haloperidol and chlorpromazine, rapidly equilibrate with the highly perfused brain compartment (Balant-Gorgia and Balant 1987; Byerly and DeVane 1996; Jann et al. 1993; Javaid 1994; Johnson et al. 2011; Nord and Farde 2011; Verghese et al. 1991). In this phase, distribution to the less perfused peripheral compartments has not yet taken place. As a result of this, APs with a slow k-off rate, as haloperidol and chlorpromazine (Kapur and Seeman 2001), would remain tightly bound to D2 receptors in spite of the subsequent decrease of brain drug levels, as distribution to peripheral compartments takes place. This long-lasting and high occupancy of NAc core D2 receptors would allow a steady activation of DA transmission in the core after peak DA activation, reflecting initial drug distribution, has taken place in the shell.
In the case of clozapine and quetiapine, fast dissociation (k-off) from D2 receptors (Kapur and Seeman 2001) would allow the reduction of receptor occupancy in parallel with the decrease of brain drug concentrations due to its distribution to peripheral compartments. Under these conditions, the level and duration of D2 receptor occupancy, while sufficient for fully increasing DA transmission in the shell, would not be sufficient for activating core DA.
Less lipophilic drugs like amisulpride and sulpiride, which slowly enter the brain (Mauri et al. 1996; Rosenzweig et al. 2002), or like risperidone, which is rapidly converted into the less liposoluble 9-hydroxy metabolite, paliperidone (Mannens et al. 1993; Muly et al. 2012), given in appropriate doses, increase DA preferentially in shell because the absence of the initial overshoot allows titration of the drug to doses that preferentially activate DA in the shell, an area with higher responsivity of DA transmission compared to the core due to a lower level of DA transporter (Calipari et al. 2012; Wu et al. 2001). However, once NAc shell DA has reached its maximal stimulation, higher doses would further increase DA in the core, with loss of preferential shell DA activation.
For two drugs, raclopride and olanzapine, the relationship of differential shell vs core pattern and EPS liability did not hold. Raclopride might be a false positive since its short action makes the initial DA shell peak to dominate the overall time course and result in a preferential shell pattern. Olanzapine, instead, might be a false negative, its low EPS liability being independent of a differential shell vs core pattern, but related instead to its powerful in vivo antimuscarinic properties, superimposable to those of clozapine (Bymaster et al. 2003; Chew et al. 2006). In fact, olanzapine has nanomolar affinity for D2 receptors and rapid blood/brain equilibration that makes it more similar to chlorpromazine than to clozapine (Jones et al. 1996).
We therefore hypothesize that the shell/core differences in the responsiveness of DA transmission to APs are related to differences in the dynamics of DA and in the temporal and fractional scaling of D2 occupancy by APs necessary for shell vs core activation of DA transmission.
Although the relationship between shell vs core DA activation pattern and APs EPS liability can be understood as essentially indirect, being due to sharing of some common determinants, a more direct relationship can be envisioned. Thus, Shilliam and Dawson (2005) have reported that chronic exposure to clozapine results in reversal, from stimulation to inhibition, of its effect on dialysate shell DA. This reversal is not observed in the core. This pattern of change has been interpreted as due to depolarization inactivation of ventrotegmental area neurons projecting to the shell (Shilliam and Dawson 2005). Selective depolarization inactivation of DA neurons to the shell with sparing of DA neurons projecting to the neostriatum has been proposed as the basis for the low EPS liability of clozapine and second-generation antipsychotics (Chiodo and Bunney 1983; Grace et al. 1997). Therefore, the differential responsiveness of shell vs core DA transmission to acute APs might be the premise for depolarization inactivation of shell DA neurons and sparing of DA neurons to the core and dorsal caudate-putamen after chronic APs. If this is the case, the differential responsiveness of shell vs core DA might be relevant for AP therapeutic effectiveness and EPS liability. Chronic studies relating acute to chronic AP effects will be needed to clarify these issues.
References
Abi-Dargham A, Laruelle M (2005) Mechanisms of action of second generation antipsychotic drugs in schizophrenia: insights from brain imaging studies. Eur Psychiatr J Assoc Eur Psychiatrists 20:15–27
Abi-Dargham A, Mawlawi O, Lombardo I, Gil R, Martinez D, Huang Y, Hwang DR, Keilp J, Kochan L, Van Heertum R, Gorman JM, Laruelle M (2002) Prefrontal dopamine D1 receptors and working memory in schizophrenia. J Neurosci Off J Soc Neurosci 22:3708–3719
Adachi YU, Aramaki Y, Satomoto M, Higuchi H, Watanabe K (2003) Halothane attenuated haloperidol and enhanced clozapine-induced dopamine release in the rat striatum. Neurochem Int 43:113–119
Adachi YU, Yamada S, Satomoto M, Higuchi H, Watanabe K, Kazama T, Mimuro S, Sato S (2008) Isoflurane anesthesia inhibits clozapine- and risperidone-induced dopamine release and anesthesia-induced changes in dopamine metabolism was modified by fluoxetine in the rat striatum: an in vivo microdialysis study. Neurochem Int 52:384–391
Anden NE, Stock G (1973) Effect of clozapine on the turnover of dopamine in the corpus striatum and in the limbic system. J Pharm Pharmacol 25:346–348
Anden NE, Butcher SG, Corrodi H, Fuxe K, Ungerstedt U (1970) Receptor activity and turnover of dopamine and noradrenaline after neuroleptics. Eur J Pharmacol 11:303–314
Andersson JL, Nomikos GG, Marcus M, Hertel P, Mathe JM, Svensson TH (1995) Ritanserin potentiates the stimulatory effects of raclopride on neuronal activity and dopamine release selectivity in the mesolimbic dopaminergic system. Naunyn Schmiedeberg’s Arch Pharmacol 352:374–385
Arnt J, Skarsfeldt T (1998) Do novel antipsychotics have similar pharmacological characteristics? A review of the evidence. Neuropsychopharmacol Off Publ Am Coll Neuropsychopharmacol 18:63–101
Axelsson R, Nilsson A, Christensson E, Bjork A (1991) Effects of amperozide in schizophrenia. An open study of a potent 5-HT2 receptor antagonist. Psychopharmacology 104:287–292
Balant-Gorgia AE, Balant L (1987) Antipsychotic drugs. Clinical pharmacokinetics of potential candidates for plasma concentration monitoring. Clin Pharmacokinet 13:65–90
Bartholini G (1976) Differential effect of neuroleptic drugs on dopamine turnover in the extrapyramidal and limbic system. J Pharm Pharmacol 28:429–433
Breier A (1995) Serotonin, schizophrenia and antipsychotic drug action. Schizophr Res 14:187–202
Bunney BS (1988) Effects of acute and chronic neuroleptic treatment on the activity of midbrain dopamine neurons. Ann N Y Acad Sci 537:77–85
Byerly MJ, DeVane CL (1996) Pharmacokinetics of clozapine and risperidone: a review of recent literature. J Clin Psychopharmacol 16:177–187
Bymaster FP, Felder CC, Tzavara E, Nomikos GG, Calligaro DO, McKinzie DL (2003) Muscarinic mechanisms of antipsychotic atypicality. Prog Neuro-Psychopharmacol Biol Psychiatry 27:1125–1143
Calipari ES, Huggins KN, Mathews TA, Jones SR (2012) Conserved dorsal-ventral gradient of dopamine release and uptake rate in mice, rats and rhesus macaques. Neurochem Int 61:986–991
Carboni E, Rolando MT, Silvagni A, Di Chiara G (2000) Increase of dialysate dopamine in the bed nucleus of stria terminalis by clozapine and related neuroleptics. Neuropsychopharmacol Off Publ Am Coll Neuropsychopharmacol 22:140–147
Carlsson A (1974) Antipsychotic drugs and catecholamine synapses. J Psychiatr Res 11:57–64
Carlsson A, Lindqvist M (1963) Effect of chlorpromazine or haloperidol on formation of 3-methoxytyramine and normetanephrine in mouse brain. Acta Pharmacol Toxicol 20:140–144
Cassano GB, Castrogiovanni P, Conti L, Bonollo L (1975) Sulpiride versus haloperidol in schizophrenia: a double-blind comparative trial. Curr Ther Res Clin Exp 17:189–201
Chew ML, Mulsant BH, Pollock BG, Lehman ME, Greenspan A, Kirshner MA, Bies RR, Kapur S, Gharabawi G (2006) A model of anticholinergic activity of atypical antipsychotic medications. Schizophr Res 88:63–72
Chiodo LA, Bunney BS (1983) Typical and atypical neuroleptics: differential effects of chronic administration on the activity of A9 and A10 midbrain dopaminergic neurons. J Neurosci Off J Soc Neurosci 3:1607–1619
Csernansky JG, Newcomer JW, Jackson K, Lombrozo L, Faull KF, Zipursky R, Pfefferbaum A, Faustman WO (1994) Effects of raclopride treatment on plasma and CSF HVA: relationships with clinical improvement in male schizophrenics. Psychopharmacology 116:291–296
Deutch AY, Cameron DS (1992) Pharmacological characterization of dopamine systems in the nucleus accumbens core and shell. Neuroscience 46:49–56
Deutch AY, Lee MC, Iadarola MJ (1992) Regionally specific effects of atypical antipsychotic drugs on striatal Fos expression: the nucleus accumbens shell as a locus of antipsychotic action. Mol Cell Neurosci 3:332–341
Di Chiara G (2002) Nucleus accumbens shell and core dopamine: differential role in behavior and addiction. Behav Brain Res 137:75–114
Dilts RP Jr, Helton TE, McGinty JF (1993) Selective induction of Fos and FRA immunoreactivity within the mesolimbic and mesostriatal dopamine terminal fields. Synapse 13:251–263
Dragunow M, Robertson GS, Faull RL, Robertson HA, Jansen K (1990) D2 dopamine receptor antagonists induce Fos and related proteins in rat striatal neurons. Neuroscience 37:287–294
Franberg O, Wiker C, Marcus MM, Konradsson A, Jardemark K, Schilstrom B, Shahid M, Wong EH, Svensson TH (2008) Asenapine, a novel psychopharmacologic agent: preclinical evidence for clinical effects in schizophrenia. Psychopharmacology 196:417–429
Gardner DM, Murphy AL, O’Donnell H, Centorrino F, Baldessarini RJ (2010) International consensus study of antipsychotic dosing. Am J Psychiatry 167:686–693
Ginovart N, Kapur S (2012) Role of dopamine D(2) receptors for antipsychotic activity. Handb Exp Pharmacol 27–52
Grace AA, Bunney BS, Moore H, Todd CL (1997) Dopamine-cell depolarization block as a model for the therapeutic actions of antipsychotic drugs. Trends Neurosci 20:31–37
Harnryd C, Bjerkenstedt L, Bjork K, Gullberg B, Oxenstierna G, Sedvall G, Wiesel FA, Wik G, Aberg-Wistedt A (1984) Clinical evaluation of sulpiride in schizophrenic patients—a double-blind comparison with chlorpromazine. Acta Psychiatr Scand Suppl 311:7–30
Hartter S, Huwel S, Lohmann T, Abou El Ela A, Langguth P, Hiemke C, Galla HJ (2003) How does the benzamide antipsychotic amisulpride get into the brain?—An in vitro approach comparing amisulpride with clozapine. Neuropsychopharmacol Off Publ Am Coll Neuropsychopharmacol 28:1916–1922
Heimer L, Alheid GF, de Olmos JS, Groenewegen HJ, Haber SN, Harlan RE, Zahm DS (1997) The accumbens: beyond the core-shell dichotomy. J Neuropsychiatry Clin Neurosci 9:354–381
Hertel P, Nomikos GG, Iurlo M, Svensson TH (1996) Risperidone: regional effects in vivo on release and metabolism of dopamine and serotonin in the rat brain. Psychopharmacology 124:74–86
Ichikawa J, Meltzer HY (1992) Amperozide, a novel antipsychotic drug, inhibits the ability of d-amphetamine to increase dopamine release in vivo in rat striatum and nucleus accumbens. J Neurochem 58:2285–2291
Ichikawa J, Meltzer HY (2000) The effect of serotonin(1A) receptor agonism on antipsychotic drug-induced dopamine release in rat striatum and nucleus accumbens. Brain Res 858:252–263
Ichikawa J, Kuroki T, Dai J, Meltzer HY (1998) Effect of antipsychotic drugs on extracellular serotonin levels in rat medial prefrontal cortex and nucleus accumbens. Eur J Pharmacol 351:163–171
Ichikawa J, Ishii H, Bonaccorso S, Fowler WL, O’Laughlin IA, Meltzer HY (2001) 5-HT(2A) and D(2) receptor blockade increases cortical DA release via 5-HT(1A) receptor activation: a possible mechanism of atypical antipsychotic-induced cortical dopamine release. J Neurochem 76:1521–1531
Imperato A, Angelucci L (1989) The effects of clozapine and fluperlapine on the in vivo release and metabolism of dopamine in the striatum and in the prefrontal cortex of freely moving rats. Psychopharmacol Bull 25:383–389
Imperato A, Di Chiara G (1985) Dopamine release and metabolism in awake rats after systemic neuroleptics as studied by trans-striatal dialysis. J Neurosci Off J Soc Neurosci 5:297–306
Jann MW, Grimsley SR, Gray EC, Chang WH (1993) Pharmacokinetics and pharmacodynamics of clozapine. Clin Pharmacokinet 24:161–176
Javaid JI (1994) Clinical pharmacokinetics of antipsychotics. J Clin Pharmacol 34:286–295
Johnson M, Kozielska M, Pilla Reddy V, Vermeulen A, Li C, Grimwood S, de Greef R, Groothuis GM, Danhof M, Proost JH (2011) Mechanism-based pharmacokinetic-pharmacodynamic modeling of the dopamine D2 receptor occupancy of olanzapine in rats. Pharm Res 28:2490–2504
Jones SR, O’Dell SJ, Marshall JF, Wightman RM (1996) Functional and anatomical evidence for different dopamine dynamics in the core and shell of the nucleus accumbens in slices of rat brain. Synapse 23:224–231
Kapur S, Seeman P (2001) Does fast dissociation from the dopamine d(2) receptor explain the action of atypical antipsychotics?: a new hypothesis. Am J Psychiatry 158:360–369
Knable MB, Weinberger DR (1997) Dopamine, the prefrontal cortex and schizophrenia. J Psychopharmacol 11:123–131
Kuroki T, Meltzer HY, Ichikawa J (1999) Effects of antipsychotic drugs on extracellular dopamine levels in rat medial prefrontal cortex and nucleus accumbens. J Pharmacol Exp Ther 288:774–781
Lecca D, Cacciapaglia F, Valentini V, Gronli J, Spiga S, Di Chiara G (2006) Preferential increase of extracellular dopamine in the rat nucleus accumbens shell as compared to that in the core during acquisition and maintenance of intravenous nicotine self-administration. Psychopharmacology 184:435–446
Leucht S, Cipriani A, Spineli L, Mavridis D, Orey D, Richter F, Samara M, Barbui C, Engel RR, Geddes JR, Kissling W, Stapf MP, Lassig B, Salanti G, Davis JM (2013) Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: a multiple-treatments meta-analysis. Lancet 382:951–962
Liegeois JF, Ichikawa J, Meltzer HY (2002) 5-HT(2A) receptor antagonism potentiates haloperidol-induced dopamine release in rat medial prefrontal cortex and inhibits that in the nucleus accumbens in a dose-dependent manner. Brain Res 947:157–165
Linnet K, Ejsing TB (2008) A review on the impact of P-glycoprotein on the penetration of drugs into the brain. Focus on psychotropic drugs. Eur Neuropsychopharmacol J Eur Coll Neuropsychopharmacol 18:157–169
Mannens G, Huang ML, Meuldermans W, Hendrickx J, Woestenborghs R, Heykants J (1993) Absorption, metabolism, and excretion of risperidone in humans. Drug Metab Dispos Biol Fate Chem 21:1134–1141
Marcus MM, Nomikos GG, Svensson TH (1996) Differential actions of typical and atypical antipsychotic drugs on dopamine release in the core and shell of the nucleus accumbens. Eur Neuropsychopharmacol J Eur Coll Neuropsychopharmacol 6:29–38
Marcus MM, Nomikos GG, Svensson TH (2000) Effects of atypical antipsychotic drugs on dopamine output in the shell and core of the nucleus accumbens: role of 5-HT(2A) and alpha(1)-adrenoceptor antagonism. Eur Neuropsychopharmacol J Eur Coll Neuropsychopharmacol 10:245–253
Marcus MM, Malmerfelt A, Nyberg S, Svensson TH (2002) Biochemical effects in brain of low doses of haloperidol are qualitatively similar to those of high doses. Eur Neuropsychopharmacol J Eur Coll Neuropsychopharmacol 12:379–386
Mauri MC, Bravin S, Bitetto A, Rudelli R, Invernizzi G (1996) A risk-benefit assessment of sulpiride in the treatment of schizophrenia. Drug Saf Int J Med Toxicol Drug Experience 14:288–298
Meltzer HY (1991) The mechanism of action of novel antipsychotic drugs. Schizophr Bull 17:263–287
Moghaddam B, Bunney BS (1990) Acute effects of typical and atypical antipsychotic drugs on the release of dopamine from prefrontal cortex, nucleus accumbens, and striatum of the rat: an in vivo microdialysis study. J Neurochem 54:1755–1760
Morris ED, Normandin MD, Schiffer WK (2008) Initial comparison of ntPET with microdialysis measurements of methamphetamine-induced dopamine release in rats: support for estimation of dopamine curves from PET data. Mol Imaging Biol MIB Off Publ Acad Mol Imaging 10:67–73
Muly EC, Votaw JR, Ritchie J, Howell LL (2012) Relationship between dose, drug levels, and D2 receptor occupancy for the atypical antipsychotics risperidone and paliperidone. J Pharmacol Exp Ther 341:81–89
Narendran R, Jedema HP, Lopresti BJ, Mason NS, Gurnsey K, Ruszkiewicz J, Chen CM, Deuitch L, Frankle WG, Bradberry CW (2014) Imaging dopamine transmission in the frontal cortex: a simultaneous microdialysis and [11C]FLB 457 PET study. Mol Psychiatry 19:302–310
Nomikos GG, Iurlo M, Andersson JL, Kimura K, Svensson TH (1994) Systemic administration of amperozide, a new atypical antipsychotic drug, preferentially increases dopamine release in the rat medial prefrontal cortex. Psychopharmacology 115:147–156
Nord M, Farde L (2011) Antipsychotic occupancy of dopamine receptors in schizophrenia. CNS Neurosci Ther 17:97–103
Paxinos G, Watson C (1998) The rat brain in stereotaxic coordinates, 4th edn. Academic, San Diego
Robertson GS, Fibiger HC (1992) Neuroleptics increase c-Fos expression in the forebrain: contrasting effects of haloperidol and clozapine. Neuroscience 46:315–328
Robertson GS, Matsumura H, Fibiger HC (1994) Induction patterns of Fos-like immunoreactivity in the forebrain as predictors of atypical antipsychotic activity. J Pharmacol Exp Ther 271:1058–1066
Rosenzweig P, Canal M, Patat A, Bergougnan L, Zieleniuk I, Bianchetti G (2002) A review of the pharmacokinetics, tolerability and pharmacodynamics of amisulpride in healthy volunteers. Hum Psychopharmacol 17:1–13
Rummel-Kluge C (2010) Negative symptoms are prevalent in antipsychotic-treated adult outpatients with schizophrenia spectrum disorders. Evid Based Ment Health 13:106
Schoemaker H, Claustre Y, Fage D, Rouquier L, Chergui K, Curet O, Oblin A, Gonon F, Carter C, Benavides J, Scatton B (1997) Neurochemical characteristics of amisulpride, an atypical dopamine D2/D3 receptor antagonist with both presynaptic and limbic selectivity. J Pharmacol Exp Ther 280:83–97
Shilliam CS, Dawson LA (2005) The effect of clozapine on extracellular dopamine levels in the shell subregion of the rat nucleus accumbens is reversed following chronic administration: comparison with a selective 5-HT(2C) receptor antagonist. Neuropsychopharmacol Off Publ Am Coll Neuropsychopharmacol 30:372–380
Svartengren J, Simonsson P (1990) Receptor binding properties of amperozide. Pharmacol Toxicol 66(Suppl 1):8–11
Tanda G, Di Chiara G (1998) A dopamine-mu1 opioid link in the rat ventral tegmentum shared by palatable food (Fonzies) and non-psychostimulant drugs of abuse. Eur J Neurosci 10:1179–1187
Verghese C, Kessel JB, Simpson GM (1991) Pharmacokinetics of neuroleptics. Psychopharmacol Bull 27:551–563
Volonte M, Monferini E, Cerutti M, Fodritto F, Borsini F (1997) BIMG 80, a novel potential antipsychotic drug: evidence for multireceptor actions and preferential release of dopamine in prefrontal cortex. J Neurochem 69:182–190
White FJ, Wang RY (1983) Differential effects of classical and atypical antipsychotic drugs on A9 and A10 dopamine neurons. Science 221:1054–1057
Wirtshafter D, Osborn CV (2005) The atypical dopamine D1 receptor agonist SKF 83959 induces striatal Fos expression in rats. Eur J Pharmacol 528:88–94
Wu Q, Reith ME, Kuhar MJ, Carroll FI, Garris PA (2001) Preferential increases in nucleus accumbens dopamine after systemic cocaine administration are caused by unique characteristics of dopamine neurotransmission. J Neurosci Off J Soc Neurosci 21:6338–6347
Zahm DS (2000) An integrative neuroanatomical perspective on some subcortical substrates of adaptive responding with emphasis on the nucleus accumbens. Neurosci Biobehav Rev 24:85–105
Acknowledgments
This study was supported by the National Research Council of Italy (CNR), by the Ministero dell’Università e della Ricerca (MURST/MIUR) and by the Regione Autonoma della Sardegna (RAS).
Conflict of interest
Authors do not have any conflict of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Additional information
Gianluigi Tanda and Valentina Valentini contributed equally to this work.
Rights and permissions
About this article
Cite this article
Tanda, G., Valentini, V., De Luca, M.A. et al. A systematic microdialysis study of dopamine transmission in the accumbens shell/core and prefrontal cortex after acute antipsychotics. Psychopharmacology 232, 1427–1440 (2015). https://doi.org/10.1007/s00213-014-3780-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-014-3780-2