Abstract
Rationale
Asenapine is a novel psychopharmacologic agent being developed for the treatment of schizophrenia and bipolar disorder.
Materials and methods
The present study was undertaken to investigate the effects of asenapine using animal models predictive of antipsychotic efficacy (conditioned avoidance response [CAR]) and extrapyramidal side effects (EPS; catalepsy). In parallel, the effects of asenapine on regional dopamine output using in vivo microdialysis in freely moving rats, dopamine output in the core and shell subregions of nucleus accumbens (NAc) using in vivo voltammetry in anesthetized rats, and N-methyl-d-aspartate (NMDA)-induced currents in pyramidal neurons of the medial prefrontal cortex (mPFC) using the electrophysiological technique intracellular recording in vitro were assessed.
Results
Asenapine (0.05–0.2 mg/kg, subcutaneous [s.c.]) induced a dose-dependent suppression of CAR (no escape failures recorded) and did not induce catalepsy. Asenapine (0.05–0.2 mg/kg, s.c.) increased dopamine efflux in both the mPFC and the NAc. Low-dose asenapine (0.01 mg/kg, intravenous [i.v.]) increased dopamine efflux preferentially in the shell compared to the core of NAc, whereas at a higher dose (0.05 mg/kg, i.v.), the difference disappeared. Finally, like clozapine (100 nM), but at a considerably lower concentration (5 nM), asenapine significantly potentiated the NMDA-induced responses in pyramidal cells of the mPFC.
Conclusions
These preclinical data suggest that asenapine may exhibit highly potent antipsychotic activity with very low EPS liability. Its ability to increase both dopaminergic and glutamatergic activity in rat mPFC suggests that asenapine may possess an advantageous effect not only on positive symptoms in patients with schizophrenia, but also on negative and cognitive symptoms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Schizophrenia is a devastating brain disease characterized by positive, negative, and cognitive symptoms. The classical dopamine (DA) hypothesis of schizophrenia suggests an overall hyperdopaminergic state in the brain (Carlsson 1978). However, the current hypothesis suggests a hyperdopaminergic state in subcortical areas, leading to psychotic symptoms, while negative and cognitive symptoms may be related to hypofunctioning of both dopaminergic and glutamatergic neurotransmission in the prefrontal cortex (PFC; see, e.g., Svensson 2003a). In support of this notion, it has been shown that the prevalence of the DA metabolizing enzyme catechol-O-methyltransferase (COMT) Val allele is higher in families afflicted by schizophrenia (Egan et al. 2001; Weinberger et al. 2001). Specifically, this COMT polymorphism, primarily affecting DA catabolism in the PFC, predicts cognitive deficits and indicates an impaired prefrontal dopaminergic transmission in patients with schizophrenia. Furthermore, it has been found that the N-methyl-d-aspartate (NMDA) receptor antagonist phencyclidine can produce schizophrenia-like symptoms (Jentsch and Roth 1999), and mutant mice expressing 5% of normal NMDA receptor 1 (NR1) subunit exert a schizophrenia-like state that can be improved when treated with antipsychotic drugs (APDs; Mohn et al. 1999). Clinical data have also shown a significant reduced phosphorylation of the NR1 subunit of the NMDA-receptor in the PFC and hippocampus, indicating an involvement of NMDA-receptor dysfunction in schizophrenia (Emamian et al. 2004).
Clozapine is the prototype of the atypical APDs, possessing superior efficacy in treatment-resistant schizophrenia and shows better effect than typical APDs on negative and cognitive symptoms (Kane et al. 1988; Meltzer and McGurk 1999; Davis et al. 2003). Neurochemically, atypical APDs, such as clozapine, but not typical APDs, such as haloperidol, enhance DA efflux not only in subcortical areas but also in the medial PFC (mPFC; Moghaddam and Bunney 1990; Nomikos et al. 1994; Kuroki et al. 1999). The enhanced prefrontal dopaminergic transmission is thought to improve negative and also cognitive symptoms in schizophrenia, an effect mediated via stimulation of D1 receptors (Castner et al. 2000; Goldman-Rakic et al. 2000). This notion is underlined by studies showing that the enhanced NMDA response in mPFC induced by clozapine is mediated by DA via D1 receptors (Chen and Yang 2002; Ninan and Wang 2003). Moreover, clinical data have reported a downregulation of DA D1 receptors in both drug-naive and drug-medicated patients with schizophrenia (Sedvall and Farde 1995). In addition, D1 antagonists have not been shown to possess antipsychotic efficacy in patients with schizophrenia, and in a substantial proportion of the patients, even deterioration was seen (Karlsson et al. 1995; Gessa et al. 1991). Against this background, both enhanced prefrontal dopaminergic and glutamatergic transmission are thought to be involved in the effect of clozapine in patients with schizophrenia.
In addition, other biochemical differences in the brain may to some extent indicate an atypical or typical profile of the APDs. When studying the two subdivisions of NAc, i.e., the core and shell, regions associated with motor control and limbic function, respectively (Deutch and Cameron 1992; Deutch 1993), atypical APDs, such as clozapine, preferentially increase DA output in the shell of NAc, whereas typical APDs, e.g., haloperidol, increase the DA output preferentially in the core region (Marcus et al. 1996, 2000, 2002). These findings are supported by studies comparing activity in the core and shell regions by measuring regional c-fos expression by APDs (Deutch et al. 1992; Robertson and Fibiger 1992).
In contrast to haloperidol, clozapine has a multi-target profile, and both preclinical and clinical studies suggest that, in addition to blockade of D2 receptors, its affinity to several other receptors, such as for example serotonin (5-HT)2A and α2-adrenergic receptors, may contribute to explain its superior clinical effectiveness, as well as the absence of extrapyramidal side effects (EPS) and its cognition-enhancing action (Svensson 2003b). Interestingly, preclinical experiments show that 5-HT2A receptor antagonism by M100907 together with haloperidol-induced D2 antagonism potentiate both the antipsychotic-like effect and the prefrontal DA output (Wadenberg et al. 2001a; Liégeois et al. 2002). In similarity, adjunct treatment with an α2 receptor antagonist (idazoxan) to APDs that lack appreciable α2-adrenoceptor blocking properties enhances both preclinical and clinical antipsychotic effect and the prefrontal DA efflux in rat (Litman et al. 1996; Hertel et al. 1999; Wadenberg et al. 2007).
Preclinically, the conditioned avoidance response (CAR) test is a behavioral test of antipsychotic activity that has shown high predictive validity, and all effective APDs share the ability to selectively suppress avoidance behavior in rats (Wadenberg and Hicks 1999). Studies using the selective D2/3 receptor antagonist raclopride show that about 70–75% D2 occupancy is necessary to suppress CAR with a magnitude that predicts sufficient antipsychotic activity, whereas catalepsy, an experimental measure of EPS liability, usually appears at about 80% D2 occupancy (Wadenberg et al. 2000, 2001b). This corresponds well to clinical data where a striatal D2 receptor occupancy of 70% is required, to obtain a sufficient antipsychotic effect with typical APDs (i.e., haloperidol) and whereas the risk of EPS becomes very high at an occupancy of 80% (Farde et al. 1988). Clozapine, on the other hand, needs a D2 receptor occupancy of only about 45% for both preclinical and clinical antipsychotic effect (Wadenberg et al. 1993; Nordström et al. 1995; Marcus et al. 2005).
With clozapine, EPS are virtually absent, but there is a risk of agranulocytosis which reduces its usefulness (Tandon 2002). Other substantial side effects of this APD include, for example, substantial weight gain and sedation. Therefore, the development of APDs with similar clinical efficacy but with minimal side effect profile is crucial for improving the pharmacological treatment of schizophrenia.
Asenapine is a psychopharmacologic agent with a unique human receptor binding profile being developed for the treatment of schizophrenia and bipolar disorder. Relative to its D2 receptor activity, it possesses higher affinity for an ensemble of serotonergic (5-HT2A, 5-HT2C, 5-HT6, 5-HT7), noradrenergic (α2A, α2B, α2C), and dopaminergic (D3, D4) receptors (Shahid et al. 2007b). There exist some previously published data on asenapine, also called Org 5222, using a set of preclinical behavioral methods (see, e.g., Costall et al. 1990; Broekkamp et al. 1990; Hoffman and Donovan 1995), suggesting that asenapine possesses an antipsychotic-like effect with an atypical profile. Judging from emerging clinical results, asenapine provides improvement of positive, negative, and cognitive symptoms in schizophrenia with low EPS liability and few if any other severe side effects, such as weight gain, increased prolactin secretion, or agranulocytosis (Potkin et al. 2006, 2007).
Against the above background, the present experimental study was undertaken to examine the antipsychotic efficacy of asenapine using CAR, as well as its EPS liability using a catalepsy test. In parallel neurochemical studies, using microdialysis in awake and freely moving animals, the effects of asenapine on regional DA output in rat brain were assessed. Moreover, the effects of asenapine on DA output in two subdivisions of NAc, the core and shell, were examined using in vivo voltammetry in anesthetized rats. Finally, by means of intracellular recordings in pyramidal neurons of the mPFC, its putative enhancement of prefrontal glutamatergic transmission, i.e., NMDA-induced response, was evaluated in vitro.
Materials and methods
Animals
Adult male Wistar rats (BK Universal, Sollentuna, Sweden) with an average weight of 200–250 g upon arrival were used for the behavioral and microdialysis experiments, whereas male Sprague–Dawley rats (BK Universal) with an average weight of approximately 70 and 270 g upon arrival were used for in vitro electrophysiological and in vivo voltammetry experiments, respectively. The animals were housed three to four per cage (Makrolon® IV, BK Universal AS, Nittedal, Norway) under standard laboratory conditions with a temperature of 21.0 ± 0.4°C and relative humidity of 55–65%. Food (R34, Ewos, Södertälje, Sweden) and tap water were available ad libitum. For the microdialysis, voltammetry, and electrophysiological experiments, the animals were kept on a 12:12 h light/dark cycle (lights on at 6:00 a.m.), whereas for the behavioral tests, animals were maintained on a reversed 12:12 h light/dark cycle (lights off at 6:00 a.m.). The animals were acclimatized for at least 5 days before experiments. All experiments were performed between 8:00 a.m. and 6:00 p.m.
All experiments were approved by, and conducted in accordance with, the local Animal Ethics Committee, Stockholm North, and the Karolinska Institutet, Sweden.
Conditioned avoidance response
Rats were trained in conventional shuttle boxes (530 × 250 × 225 mm), divided into two compartments of equal size by a partition with an opening, as described previously (Salmi et al. 1994). The apparatus was equipped with photocells, automatically registering the position of the rat in relation to the opening, and a grid floor connected to a high resistance power supply. Upon presentation of the 80-dB white noise (white noise generator; Lafayette Instruments, Lafayette, IN, USA) conditioned stimulus (CS), the rats had 10 s to move from one compartment of the shuttle box into the other. If the rat remained in the same compartment for more than 10 s, an intermittent electric shock (intershock interval 2.5 s, shock duration 0.5 s) of approximately 0.3 mA (the unconditioned stimulus [UCS]) was presented to the grid floor until an escape was performed. If the rat did not respond within 50 s, the trial was terminated (escape failure).
The position of the rat was automatically transferred to the computer, and the following behavioral variables were recorded: (1) avoidance (response to CS within 10 s); (2) escape (response to CS + UCS); (3) escape failure (failure to respond within 50 s); and (4) inter-trial crosses (movement between compartments between trials).
The animals were transferred from the animal quarters to the laboratory 1 h before behavioral experiments were started and were housed in a ventilated cabinet between observations. The animals were trained for five consecutive days, each session lasting 15 min per animal and day. Experimental manipulations were always preceded by a pretest and experiment sessions, lasting 10 min, were conducted 20, 90, and 240 min after injection of the drug or vehicle. Experimental days were always separated by at least two nonexperimental days. The animals were tested in a counterbalanced change-over design serving as their own controls (Li 1964).
Catalepsy
Catalepsy was observed in a dimly lit room by placing the animals on an inclined grid (60°) for a maximum of 2.25 min. The animals were allowed 30 s of adaptation on the grid before observations started. The catalepsy was scored from 0 to 5, according to the time (square root transformation) the rat remained immobile (minutes): 0 = 0.00–0.08; 1 = 0.09–0.35; 2 = 0.36–0.80; 3 = 0.81–1.42; 4 = 1.43–2.24; 5 ≥ 2.25, i.e., if the rat remained immobile for 0.08 min, it was scored as 0, etc. (Ahlenius and Hillegaart 1986). The animals were transferred from the animal quarters to the laboratory 1 h before behavioral experiments were started and were housed in a ventilated cabinet between observations. Observations were performed 30, 60, and 120 min after drug or vehicle injection. Each animal received only one treatment.
In vivo microdialysis
Probe implantation and dialysis procedures, as well as the biochemical analysis, were similar to those previously described (e.g., Schilström et al. 1998). Rats were anesthetized with a cocktail of Hypnorm® (0.315 mg/ml fentanyl citrate and 10 mg/ml fluanisone; Janssen-Cilag, Saunderton, UK) and Dormicum® (5 mg/ml midazolam; Roche AB, Stockholm, Sweden), diluted in distilled water (1:1:2; 5 ml/kg, intraperitoneal [i.p.]), mounted in a stereotaxic frame, and implanted with dialysis probes in the mPFC, NAc, or lateral striatum (STR; anteroposterior [AP] = +2.8, +1.4, +0.7; mediolateral [ML] = −0.6, −1.4, −3.5; DL: −5.2, −8.2, −6.2), respectively, relative to bregma and dural surface (in millimeters) in accordance with the atlas of Paxinos and Watson (1998). Dialysis occurred through a semipermeable membrane (Filtral AN69 Hospal Industrie, Meyzieu, France) with an active surface length of 4 mm for mPFC, 2.25 mm for NAc, and 3 mm for STR. Dialysis experiments were conducted approximately 48 h after surgery in awake and freely moving rats. The dialysis probe was perfused with a physiological perfusion solution (147 mM NaCl, 3.0 mM KCl, 1.3 mM CaCl2, 1.0 mM MgCl2, and 1.0 mM NaHPO4, pH 7.4, Apoteksbolaget, Solna, Stockholm) at a rate of 2.5 μl/min, set by a microinfusion pump (Harvard Apparatus, Holliston, MA, USA). Dialysate samples were collected over 30- or 15-min intervals for mPFC or NAc and STR, respectively. Online quantification of DA and metabolites in the dialysate was accomplished by high-performance liquid chromatography (HPLC) coupled to electrochemical detection (ESA Bioscience, Chelsford, MA, USA), with a detection limit of approximately 0.2 fmol/min. The loading and injection modes of the injector (Valco Instruments, Houston, TX, USA) were directed by a computerized system with Totalcrom WS version 6.3 software (Perkin Elmer, Wellesley, MA, USA). Separation of DA, dihydroxyphenylacetic acid (DOPAC), homovanillic acid (HVA), and 5-hydroxyindoleacetic acid (5-HIAA) was achieved by reversed phase liquid chromatography. The mobile phase for DA detection consisted of a 55-mM sodium acetate buffer, pH 4.0 (adjusted with glacial acetic acid), with 12% methanol and 0.55 mM octanesulfonic acid. It was delivered by an HPLC pump (Model 2150, Pharmacia LKB, Sweden) on a C-18 column (Nucleocil 150/75 × 4.6 mm, 5 μm) at a flow rate of 0.8 ml/min. After separation, the analysate was passed through a guard cell with an applied oxidizing potential of 50 mV to reduce baseline noise from other electroactive compounds. Samples were then quantified by sequential oxidation and reduction in a high sensitive analytical cell (model 5011; ESA Bioscience) that was controlled by a potentiostat (Coulochem II model 5200; ESA Bioscience) with applied potentials of 400 and −200 mV for detection of metabolites and DA, respectively, in NAc and STR and 250 and −300 mV for detection of metabolites and DA in mPFC, respectively. Chromatograms were both printed on a two-pen chart recorder (Kipp & Sonen, Delft, The Netherlands) and recorded by the computer.
Injection of asenapine was performed after a stable outflow (<10% variation) of DA (DOPAC, 5-HIAA, HVA). Baseline (100%) was calculated as the average of the last two (mPFC) or four (NAc and STR) pre-injection values.
After completion of dialysis experiment, the animals were killed, and their brains were preserved in a 25% sucrose 4% formaldehyde solution. Each brain was sectioned into 50-μm thick slices on a cryostat (SLEE, Mainz, Germany), Nissl stained and examined microscopically for verification of probe placement. Only animals with correct probe placement were included in the study.
In vivo voltammetry
Rats were pretreated with pargyline (75 mg/kg, i.p., 90–120 min before recording; Sigma-Aldrich, Stockholm, Sweden) and anesthetized with chloral hydrate (CH, 400 mg/kg, i.p.; Merck, Germany). A tracheal catheter, as well as a jugular and a femoral vein catheter were inserted for intravenous (i.v.) administration of drugs and continuous infusion of CH (100 mg kg−1 h−1, i.v.), respectively. The animals were kept under surgical anesthesia throughout the experiment, and normal body temperature was maintained by using a thermostatically controlled electric heating pad. Rats were mounted in a stereotaxic instrument (Unimecanique, France, incisor bar −3 mm to interaural line). The skull was exposed, and a hole was drilled above the NAc. The dura mater was incised, and the pia mater was punctuated by means of a used electrode. Electrodes were inserted into either the core (AP = +1.7 mm, ML = +1.6 mm relative to bregma) or the shell region of NAc (AP = +1.6 mm, ML = +0.8 mm relative to bregma; Paxinos and Watson 1998). Carbon fiber electrodes (active portion 12 μm thick and 500 μM long) were prepared and treated as described by Gonon et al. (1984), except with smaller modifications for the electrochemical treatment (see Marcus et al. 1996). The electrochemical treatment of the electrodes increases their sensitivity for the catechols over ascorbate. The pretreatment of the rats with pargyline is to prevent formation of DOPAC and thus minimizing the interference of DOPAC with the catechol peak (Gonon et al. 1984; Gonon 1988). The tip of the electrode was placed 6.5–7.0 mm below the cortical surface, and the catechol oxidation current was monitored by a pulse voltammetric system (Biopulse, SOLEA Tacusell, France). Differential normal pulse voltammetry was used to record voltammograms every minute with the parameters as described elsewhere (Gonon 1988). The Biopulse system was connected to a computer with a chromatography software and data acquisition system (AZUR version 4.0, Datalys, France) by which the peak area was calculated. The average of ten 1-min samples before the first injection of drug was used as baseline. After a stable baseline had been achieved and subsequently recorded for at least 10 min, the animals received an injection (i.v.) of vehicle to exclude non-drug-specific effects, and 10 min later, the drug was injected. For each experiment, all values were expressed as percent of baseline. The overall DA output was measured as the mean±standard error of the mean (SEM) percent change from baseline over 15 min after drug injection. At the end of each experiment, an electrolytic lesion (5 V, 5 s) was made through the carbon fiber electrode for histological verification of the recording site. After the experiment, the animals were killed, and their brains were stored in a 25% sucrose 4% formaldehyde solution. Each brain was cut in 50-μm thick slices on a cryostat (SLEE), Nissl stained, and examined under a microscope for electrode placement. Only animals with correct electrode placement were included in the study.
Intracellular recording
The procedures for the preparation of the rat slice have been described elsewhere (Arvanov et al. 1997; Arvanov and Wang 1998). Briefly, the rats were decapitated under halothane anesthesia (AstraZeneca AB, Södertälje, Sweden). The brains were then rapidly removed and cooled in ice-cold Ringer’s solution (in millimolars: 126 NaCl, 2.5 KCl, 2.4 CaCl2, 1.3 MgCl2, 1.2 NaH2PO4, 10 d-glucose, 18 NaHCO3, pH 7.4) aerated by 95% O2/5% CO2. The brains were then cut coronally to produce 450-μm slices. The brain slices were removed from the Vibroslice (Campden model MA 752, World Precision Instruments, Sarasota, FL, USA) and kept submerged in aerated Ringer’s solution at room temperature for at least 1 h to allow for recovery. A single slice containing mPFC was then transferred to a recording chamber (32°C), in which it was held submerged between two nylon nets during the electrophysiological recordings. The chamber was continuously perfused by aerated Ringer’s solution at a flow rate of ∼2 ml/min.
Standard intracellular recording was used to record pyramidal cells in layers V and VI of the mPFC in slice preparations (Arvanov et al. 1997; Arvanov and Wang 1998). Electrodes were pulled from borosilicate glass capillaries (Clark Electromedical Instruments, Pangbourne, UK) by using a horizontal electrode puller (Model P-87, Sutter Instruments, San Rafael, CA, USA). Recording electrodes were filled with 2 M KAc (tip resistance 75 ± 3 MΩ; mean ± SEM; n = 44 cells) and used for recording the mPFC neurons with an Axoclamp 2A amplifier (Axon Instruments, Foster City, CA, USA). Single electrode voltage clamp (holding potential −60 mV) was performed in the discontinuous mode with a sampling rate of 5–6.2 kHz. The voltage recordings are acquired using digital/analogue sampling and acquisition software (Clampex version 9.2, Axon Instruments). During the voltage clamp recordings of NMDA-evoked currents, tetrodotoxin (TTX; 0.5 μM, to block the action potentials), glycine (1 μM, to enhance the NMDA-induced responses), and bicuculline (5 μM, to block the γ-aminobutyric acid A responses) were routinely included in the aerated Ringer’s solution. All drugs used were diluted in Ringer’s solution and administered via bath application by perfusion via a three-way tap system. NMDA (7.5–15 μM) was also applied via bath perfusion, to induce inward currents. The effect of the drug on the NMDA-induced current was calculated by dividing the NMDA-induced current after the bath application of the drug by the control NMDA-induced current.
Drugs
Asenapine was provided by Organon Laboratories, Newhouse, UK. The compounds bicuculline methiodide, glycine, and NMDA were all purchased from Sigma, St. Louis, MO, USA. TTX was obtained from Tocris, Bristol, UK.
For all in vivo experiments, asenapine was dissolved in saline (0.9% NaCl). Control animals received injections with saline (0.9% NaCl). Systemic administration was performed by subcutaneous (s.c.) injections at a volume of 1.0 ml/kg or i.v. injections at a maximum volume of 0.2 ml/kg. For the in vitro experiments, asenapine was dissolved in purified water.
Statistics
Statistical evaluation of behavioral data was performed by Friedman two-way analysis of variance (ANOVA), followed by Wilcoxon matched pairs signed ranks test (CAR) or the Kruskal–Wallis one-way ANOVA, followed by Mann–Whitney U test (catalepsy; Siegel and Castellan 1988). Statistical evaluation of microdialysis data over time was performed by means of a two-way (treatment × time) ANOVA for repeated measures followed by a planned comparison test, whereas overall effects presented as area under the curve (AUC) were statistically evaluated by means of a one-way (treatment) or a two-way (treatment × area) ANOVA for multiple categorial variables followed by Neuman–Keuls test. Voltammetry data were statistically evaluated by a t-test for dependent samples. Statistical evaluation of the intracellular recording data was performed with the software GraphPad Prism version 4.0 (GraphPad Software, San Diego, CA, USA) using a paired t-test, measuring significant different from the control NMDA-induced currents, or a Student’s t-test, measuring significant different from clozapine’s effect on the NMDA-induced currents. All other statistical evaluations were performed by using the software Statistica version 7.1 (StatSoft, Tulsa, OK, USA). In all statistical measures, a p value less than 0.05 (p < 0.05) was considered significant.
Results
Effects of asenapine on CAR behavior
The dose–response relationship for the antipsychotic-like effect of asenapine using the CAR method was established. As shown in Fig. 1, asenapine (0.05, 0.1, and 0.2 mg/kg, s.c., n = 8) produced suppression of CAR [20 min: χ 2(3)=20.84, p < 0.001; 90 min: χ 2(3)=14.12, p < 0.05] in a dose-dependent manner. Asenapine 0.05 mg/kg had a small but not significant effect, while the doses 0.1 and 0.2 mg/kg produced a significant suppression of CAR at both 20 and 90 min after administration (p < 0.05). The results show that the dose needed for antipsychotic effect, i.e., about 80% suppression of CAR (Wadenberg et al. 2001b), is between 0.1–0.2 mg/kg (ED50 = 0.12 mg/kg). All animals were back to normal performance at 480 min after asenapine administration (data not shown). No escape failures were recorded under any treatment condition or time; that is, a decrease in avoidance responses was always accompanied by a corresponding increase in escape responses.
Effects of asenapine (0.05, 0.1, and 0.2 mg/kg, s.c.) on conditioned avoidance response behavior in rats at 0 to 240 min after administration. The results are represented as median (avoidance%) ± semi-interquartile range. Animals (n = 8) were serving as their own controls in a change-over design (Li 1964). No escape failures were recorded. + p < 0.05 for saline- vs. asenapine-treated animals
Effects of asenapine in the catalepsy test
Asenapine (0.1, 0.2, 0.5, 1.0, 2.0 mg/kg, s.c.) was tested in the catalepsy test [30 min: χ 2(5)=26.16, p < 0.001; 60 min: χ 2(5)=30.00, p < 0.001; 90 min: χ 2(5)=16.78, p < 0.01]. As shown in Table 1, asenapine 0.1 and 0.2 mg/kg did not at any time interval studied reach a score of 2, the level at which catalepsy is considered to begin according to previous studies (Wadenberg et al. 2001b). The scores for animals treated with asenapine 0.5, 1.0, and 2.0 mg/kg were 2–3.5, which were statistically significant for 0.5 mg/kg both at 60 and 120 min and for 1.0 and 2.0 at all time points (30, 60, and 120 min; p < 0.05–0.001). However, none of these higher doses reached 5, the maximal score for the test.
Effects of asenapine on regional extracellular DA concentrations
The mean ± SEM basal DA levels in the mPFC, NAc, and STR were 0.36 ± 0.24 fmol/min (n = 26), 3.18 ± 1.67 fmol/min (n = 29), and 6.42 ± 3.59 fmol/min (n = 24), respectively. No statistically significant differences between mean baseline concentrations of DA were found between different treatment groups within the same brain region studied. Vehicle injections had no effect on extracellular DA output in any of the areas investigated.
Administration of asenapine (0.05, 0.1, 0.2 mg/kg, s.c.) induced a significant increase in mPFC DA efflux [F(treatment × time)21,154=3.25, p < 0.001; Fig. 2a]. Compared to vehicle, asenapine (0.05, 0.1, 0.2 mg/kg, s.c.) elevated the extracellular DA concentrations at 60–120 and 210 min (p < 0.05–0.01), 60–210 min (p < 0.01–0.001), and 60–210 min (p < 0.05–0.001), respectively. There was no significant difference in overall DA output (AUC) between the different doses of asenapine.
When measured in NAc, a significant increase in DA output was observed after asenapine administration [F(treatment × time)42,350=2.16, p < 0.001; Fig. 2b]. Compared to vehicle, asenapine (0.05, 0.1, 0.2 mg/kg, s.c.) elevated extracellular DA concentrations at 60 and 90 min (p < 0.05), 15–210 min (p < 0.05–0.001), and 15–210 min (p < 0.05–0.001), respectively. There was a significant difference in overall DA output between 0.05 and 0.1 mg/kg (p < 0.05), as well as between 0.05 and 0.2 mg/kg (p < 0.05).
Asenapine also caused a significant increase in extracellular DA concentration in STR [F(treatment × time) 42,280=5.30, p < 0.001; Fig. 2c]. All doses (0.05, 0.1, 0.2 mg/kg, s.c.) were found to elevate extracellular DA concentrations (p < 0.05–0.001, p < 0.001, and p < 0.001, respectively) at all time points (15–210 min). There was a significant difference in overall DA output between 0.05 and 0.1 mg/kg (p < 0.01), as well as between 0.05 and 0.2 mg/kg (p < 0.05).
Effects of asenapine on overall regional monoamine biochemistry
For comparison of the overall biochemical effects of asenapine (0–210 min) between the different brain regions studied (mPFC, NAc, STR), the dose 0.2 mg/kg s.c. was selected, corresponding to an antipsychotic-like effect in the CAR test. Vehicle injections had no effect on extracellular DA, DOPAC, HVA, or 5-HIAA of HVA output in any of the areas investigated.
Statistical evaluation of the overall effects of asenapine on DA and its metabolite DOPAC in all three brain areas investigated revealed a statistically significant interaction effect [F(treatment × area)2,30 = 8.17, p < 0.01; F(treatment × area)2,30 = 4.00, p < 0.05; Fig. 3]. For the DA metabolite HVA, a treatment effect was found [F(treatment)1,20 = 149.74 p < 0.001], whereas there were no area or interaction effects. Furthermore, the 5-HT metabolite 5-HIAA indicated a significant treatment [F(treatment)1,30 = 8.96, p < 0.01] and area [F(area)2,30 = 3.72, p < 0.05] effect, while no interaction effect was found.
Overall output of asenapine 0.2 mg/kg s.c. on dialysate concentrations of DA, DOPAC, HVA, and 5-HIAA from mPFC (open bars), NAc (solid bars), and STR (hatched bars). Bars represent mean ± SEM percent of baseline level over 210 min after asenapine administration. The dotted line represents the baseline value (100%). ++ p < 0.01, +++ p < 0.001 saline- vs. asenapine-treated animals. *p < 0.05, **p < 0.01, ***p < 0.001 between dialysis regions
As shown in Fig. 3, post hoc evaluation revealed that asenapine (0.2 mg/kg) increased DA concentrations in all brain regions studied (mPFC, NAc, and STR; p < 0.001), most extensively in STR compared to mPFC and NAc (p < 0.001). Asenapine was also found to enhance DA metabolism in all regions, as indicated by DOPAC and HVA (HVA not measured in mPFC; p < 0.001). In similarity with the DA release, the asenapine-induced elevation of DOPAC was most extensive in STR compared to mPFC and NAc (p < 0.05–0.001). In contrast, there was a small but significant increase in the 5-HT metabolite 5-HIAA in the mPFC compared to NAc (p < 0.01).
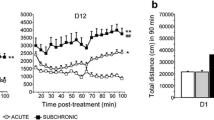
Effects of asenapine on extracellular DA output in the shell and core of the nucleus accumbens
At the lowest dose of asenapine (0.002 mg/kg, i.v.), the overall change from baseline was statistically significant in the shell [t(6)=4.69, p < 0.01], but not in the core (Fig. 4). However, the difference between the DA release in the shell and the core was not statistically significant. The effects of asenapine at 0.01 mg/kg (i.v.) compared to baseline were statistically significant in both the shell [t(6)=5.20, p < 0.01] and the core [t(4)=4.61, p < 0.01]. Asenapine also induced a statistically significant greater increase in DA output in the shell compared to the core [t(10)=2.42, p < 0.05]. At the highest dose (0.05 mg/kg, i.v.), the changes were statistically significant in the shell [t(6)=5.79, p < 0.01] and the core [t(4)=4.24, p < 0.05] compared to baseline. The overall DA output was slightly higher in the core than in the shell; however, the difference was not statistically significant.
Overall effects of asenapine (0.002, 0.01, and 0.05 mg/kg, i.v.) on extracellular concentration of DA in the shell (open bars, n = 7) and core (solid bars, n = 4–5) subregion of the NAc. Data are presented as mean±SEM percent of baseline values during 15 min after drug injection. The dotted line represents the baseline value (100%). + p < 0.05, ++ p < 0.01 shell/core vs. baseline, *p < 0.05 shell vs. core
Effects of asenapine on NMDA-induced currents in pyramidal cells of the rat mPFC
Intracellular voltage clamp recordings were performed in pyramidal cells in layer V and VI of the rat mPFC in slice preparations. The electrophysiological criteria for distinguishing pyramidal from non-pyramidal neurons have been described previously (Arvanov et al. 1997; Arvanov and Wang 1998; Konradsson et al. 2006). Briefly, the presumed pyramidal cells of the mPFC have relatively long spike duration (1–3 ms at half-maximum spike amplitude) and show a pronounced spike-frequency adaptation in response to constant-current depolarization pulses. In Ringer’s solution, the presumed pyramidal cells of the mPFC exhibited a mean resting membrane potential of −75 ± 2 mV (mean±SEM; n = 45 cells), an action potential amplitude of 71 ± 3 mV (n = 45), a spike half-width of 2.8 ± 0.3 ms (n = 25), and an after-hyperpolarization potential of 6.1 ± 0.6 mV (n = 41). These results are comparable to those previously published (Arvanov et al. 1997; Konradsson et al. 2006).
Bath perfusion with 5 nM (n = 4) asenapine significantly potentiated the NMDA-induced currents in pyramidal cells of the mPFC (see Fig. 5a; p < 0.01). The concentration–response curve of the effect of asenapine (0.05, 0.5,1, 5, 7.5, 10, 100 nM; n = 3–6) on the NMDA-induced currents was in similarity with clozapine and risperidone (Ninan et al. 2003; Konradsson et al. 2006), biphasic (Fig. 5a). As presented in Fig. 5b, the effect of 5 nM asenapine was significantly lower than the effect of 100 nM (n = 5) clozapine (p < 0.05), but did not differ from that of 20 nM (n = 6) risperidone.
a Asenapine potentiated the NMDA-induced currents in the pyramidal neurons of rat mPFC, yielding a biphasic concentration–response curve. b A bar graph illustrating the maximal effect of clozapine, risperidone, and asenapine on the NMDA-induced currents in the mPFC. + p < 0.05, ++ p < 0.01, +++ p < 0.001 (significantly different from the control NMDA-induced currents; paired t-test), *p < 0.05 (significantly different from clozapine’s effect on the NMDA-induced currents; Student’s t-test). Each point represents the mean ± SEM percent of control
Discussion
The major findings of this preclinical study demonstrate that asenapine produced an antipsychotic-like effect in doses that did not generate high risk of EPS, indicating an atypical-like profile. Furthermore, asenapine induced a marked enhancement of DA efflux preferentially in the shell region of the NAc compared to the core region, sharing a profile similar to that reported for atypical APDs. Finally, as assessed by means of microdialysis and electrophysiological techniques, asenapine was found to potentiate prefrontal dopaminergic as well as glutamatergic transmission, respectively. Taken together, our data indicate that asenapine can produce an antipsychotic effect with low EPS liability. Its facilitating effect on prefrontal dopaminergic and glutamatergic transmission may contribute to improvement of negative and cognitive symptoms in schizophrenia (see, e.g., Potkin et al. 2006, 2007).
In the present study, after acute administration, asenapine at 0.2 mg/kg s.c. produced a major suppression of CAR, i.e., about 80–100%, while no catalepsy was induced. These preclinical data suggest that asenapine may exhibit a highly potent antipsychotic activity without inducing EPS (Wadenberg et al. 2000). The lowest dose of asenapine producing significant catalepsy was 0.5 mg/kg, i.e., 2.5 times the dose needed to produce an antipsychotic-like effect in the CAR test. Thus, the dose that produced an antipsychotic effect did not generate catalepsy. Although the higher doses of asenapine (i.e., 0.5, 1.0 and 2.0 mg/kg) showed some catalepsy, it did not generate the maximal score of this test, i.e., 5. Our results on asenapine with regard to catalepsy and CAR are congruent with previously published data, although the methods used are not directly comparable (c.f., “Introduction”). As known from previous studies, clozapine generates a robust suppression of CAR (5 mg/kg) with no escape failures, but induces no catalepsy even at very high doses (>160 mg/kg; see, e.g., Wadenberg et al. 1993). Other atypical drugs such as risperidone and olanzapine are more similar to asenapine in this regard, with an antipsychotic-like effect in CAR (0.8 and 2.5–5 mg/kg, respectively) and cataleptogenic effect (2 and 5 mg/kg, respectively; Wadenberg et al. 2001b). In contrast, previous findings showed that, although a low dose of haloperidol (0.1 mg/kg) induces a comparable suppression of CAR, catalepsy was near maximal at this dose. Even at 0.025 mg/kg, which generated a significant, but not sufficient, suppression of CAR, haloperidol induced catalepsy 120 min after administration (Wadenberg et al. 2007), emphasizing a quantitative, but not qualitative, difference between the effects of low and high doses of haloperidol (Marcus et al. 2002).
The behavioral effects of asenapine were accompanied by an increased DA release in all brain regions studied, i.e., the mPFC, the NAc, and the STR, as assessed by in vivo microdialysis. The effects of asenapine on the release of the DA metabolites DOPAC and HVA (not measured in the mPFC), respectively, showed the same response pattern, while there was a subtle, but significant, increase in levels of the 5-HT metabolite 5-HIAA in the mPFC compared to the NAc. The increase in DA output in the investigated brain regions did not differ between asenapine at 0.1 and 0.2 mg/kg. However, there was a substantial difference in the suppression of avoidance between 0.1 and 0.2 mg/kg of asenapine. The specific mechanisms by which asenapine produces its antipsychotic effect remains to be clarified, but as there was a prominent enhancement of the antipsychotic-like effect without any difference in DA release between asenapine 0.1 and 0.2 mg/kg, this may reflect activity at neurotransmitter receptors other than the DA D2 receptor, given its multi-target profile (Shahid et al. 2007b). Although the data indicate a facilitating effect of asenapine on the DA release in all brain regions studied, there was a larger effect in the STR, yet at doses which did not produce catalepsy. However, clozapine preferentially influences the mesocortical DA projection, with less effect on the DA levels in the STR (Moghaddam and Bunney 1990; Hertel et al. 1996). Furthermore, the release of DA induced by asenapine also differs from that of APDs with high affinity for the DA D2 receptor, e.g., haloperidol and raclopride, which preferentially enhance DA activity in STR and NAc with only minor effects in the mPFC.
The effect of asenapine on DA release in the two subdivisions of NAc, i.e., the core and shell, associated with motor control and limbic function, respectively (Deutch and Cameron 1992; Deutch 1993), was further investigated with in vivo voltammetry, which enables studies with higher spatial and temporal resolution compared to in vivo microdialysis. A low dose of asenapine (0.01 mg/kg, i.v.) produced a significant and preferential increase in DA release in the shell compared to the core region, supporting an atypical profile of asenapine. In fact, our previous studies demonstrate that atypical APDs, e.g., clozapine, preferentially augment extracellular concentrations of DA in the shell of NAc, whereas typical APDs, e.g., haloperidol, preferentially increase extracellular DA concentration in the core region (Marcus et al. 1996), an effect seen even at extremely low doses of haloperidol (Marcus et al. 2002). The preferential effect of asenapine in the shell has also been observed in experiments examining effects on regional activation using introduction of c-fos mRNA as a marker of aggregate neuronal activity (Shahid et al. 2007a). These data also support the atypical-like profile of asenapine.
In similarity with some atypical APDs, such as clozapine and olanzapine (Moghaddam and Bunney 1990; Nomikos et al. 1994; Wadenberg et al. 2007), asenapine produced a substantial release of DA in mPFC. In contrast, the typical APD haloperidol (0.1 and 1.0 mg/kg) had no or only minor such effects (Moghaddam and Bunney 1990; Kuroki et al. 1999). Increased prefrontal DA concentration per se appears to improve antipsychotic effect, which has been shown by administration of l-dopa together with low dose of raclopride (Eltayb et al. 2005). As mentioned previously, the α2 receptor is also believed to contribute to the superior clinical effects of clozapine. Indeed, adjunct treatment with an α2 receptor antagonist to a selective D2/3 antagonist, which markedly enhances the antipsychotic-like and cognitive effects, also enhances cortical DA efflux (Hertel et al. 1999; Marcus et al. 2005). Further studies, both preclinical and clinical, using addition of an α2-adrenoceptor blocking agent to other APDs that lack appreciable α2-adrenoceptor blocking properties also support this notion (Litman et al. 1996; Wadenberg et al. 2007).
As mentioned previously, cognitive dysfunction in schizophrenia might be associated with both an impaired prefrontal DA release and a reduced glutamatergic transmission (c.f., “Introduction”). Atypical APDs, such as clozapine, but not typical APDs, facilitate prefrontal glutamatergic transmission, an effect mediated via DA and subsequent activation of DA D1 receptors (Chen and Yang 2002; Ninan and Wang 2003). In the present study using in vitro intracellular recording, asenapine was found to potentiate the NMDA-induced response in pyramidal neurons of the mPFC at a concentration in the lower nanomolar range. When comparing asenapine with the two atypical APDs clozapine and risperidone, asenapine potentiated the prefrontal glutamatergic transmission at a lower concentration compared to both these drugs, whereas the maximum effect produced by asenapine was similar to that of risperidone but lower than that of clozapine. Thus, the present study shows that clozapine and asenapine quantitatively and qualitatively may differ in their effects on glutamatergic transmission in the mPFC, indicating that clozapine’s unique pharmacological multireceptor binding profile may allow for an optimal effect on prefrontal glutamatergic transmission. On the other hand, compared to clozapine, asenapine was found to cause a significant effect on the glutamatergic transmission at a much lower concentration (5 vs 100 nM), which may suggest that a low dose treatment with asenapine could enhance cognitive dysfunction, tentatively even without any concomitant antipsychotic activity.
Asenapine possesses higher affinity for an ensemble of serotonergic (5-HT2A, 5-HT2C, 5-HT6, 5-HT7), noradrenergic (α2A, α2B, α2C), and dopaminergic (D3, D4) receptors, relative to its D2 receptor activity (Shahid et al. 2007b), offering some insight into the relative value of these targets in the complex action of this multi-target agent. This is intriguing, as preclinical and clinical studies indicate that the activity of clozapine at non-dopaminergic receptors contributes to its superior clinical effectiveness, both as regard its antipsychotic action, the absence of EPS, and its cognition-enhancing action (Svensson 2003a). Unlike clozapine, asenapine does not possess differentially higher affinity for histamine H1 and muscarinic M1–4 receptors relative to D2 receptors. Like asenapine, some atypical APDs have relatively high affinity for the 5-HT6, i.e., clozapine and olanzapine, and 5-HT7 receptors, i.e., clozapine and risperidone (Roth et al. 1994; Schotte et al. 1996). In contrast, risperidone has very low affinity for 5-HT6 receptors. Interestingly, there has recently been an increasing interest in the role of the 5-HT6, 5-HT7, and DA D3 receptors in schizophrenia (Thomas and Hagan 2004; Woolley et al. 2004; Joyce and Millan 2005; Sokoloff et al. 2006). Although more studies are needed to elucidate the pharmacological mechanisms of asenapine, its action on these receptors may potentially also be involved in its clinical profile.
Taken together, our results provide new insight in the complex mechanism of action of asenapine. These data enable comparison with well-established APDs and indicate that asenapine possesses not only some features similar to atypical APDs but also differences that might contribute to a unique profile. Our data propose that asenapine may generate a highly potent antipsychotic action with low EPS liability. Furthermore, its ability to increase both dopaminergic and glutamatergic activity in rat mPFC suggests that asenapine may have an advantageous effect not only on positive symptoms in schizophrenia, but also on negative and cognitive symptoms. The ratio between the dose required for effective antipsychotic-like activity and that causing catalepsy makes asenapine appear like an atypical APD. However, the very low concentrations of asenapine required to facilitate cortical glutamatergic transmission, which are much lower than those of clozapine in this model, suggests that asenapine may provide a superior cognitive-enhancing action.
References
Ahlenius S, Hillegaart V (1986) Involvement of extrapyramidal motor mechanisms in the suppression of locomotor activity by antipsychotic drugs: a comparison between the effects produced by pre- and post-synaptic inhibition of dopaminergic neurotransmission. Pharmacol Biochem Behav 24:1409–1415
Arvanov VL, Wang RY (1998) M100907, a selective 5-HT2A receptor antagonist and a potential antipsychotic drug, facilitates N-methyl-d-aspartate-receptor mediated neurotransmission in the rat medial prefrontal cortical neurons in vitro. Neuropsychopharmacology 18:197–209
Arvanov VL, Liang X, Schwartz J, Grossman S, Wang RY (1997) Clozapine and haloperidol modulate N-methyl-d-aspartate- and non-N-methyl-d-aspartate receptor-mediated neurotransmission in rat prefrontal cortical neurons in vitro. J Pharmacol Exp Ther 283:226–234
Broekkamp CL, De Graaf JS, van Delft AM (1990) Behavioural pharmacology of trans-5-chloro-2-methyl-2,3,3a,12b-tetrahydro-1H-dibenz[2,3:6,7]oxepino-[4,5-c]pyrrolidine maleate, a compound interacting with dopaminergic and serotonergic receptors. Arzneimittelforschung 40(5):544–549
Carlsson A (1978) Antipsychotic drugs, neurotransmitters, and schizophrenia. Am J Psychiatry 135:165–173
Castner SA, Williams GV, Goldman-Rakic PS (2000) Reversal of antipsychotic-induced working memory deficits by short-term dopamine D1 receptor stimulation. Science 287:2020–2022
Chen L, Yang CR (2002) Interaction of dopamine D1 and NMDA receptors mediates acute clozapine potentiation of glutamate EPSPs in rat prefrontal cortex. J Neurophysiol 87:2324–2336
Costall B, Domeney AM, Kelly ME, Naylor RJ, Tomkins DM (1990) Actions of ORG 5222 as a novel psychotropic agent. Pharmacol Biochem Behav 35(3):607–615
Davis JM, Chen N, Glick ID (2003) A meta-analysis of the efficacy of second-generation antipsychotics. Arch Gen Psychiatry 60:553–564
Deutch AY (1993) Prefrontal cortical dopamine systems and the elaboration of functional corticostriatal circuits: implications for schizophrenia and Parkinson’s disease. J Neural Transm Gen Sect 91:197–221
Deutch AY, Cameron DS (1992) Pharmacological characterization of dopamine systems in the nucleus accumbens core and shell. Neuroscience 46:49–56
Deutch AY, Lee MC, Iadarola MJ (1992) Regionally specific effects of atypical antipsychotic drugs on striatal fos expression: The nucleus accumbens shell as a locus of antipsychotic action. Mol Cell Neurosci 46:49–56
Egan MF, Goldberg TE, Kolachana BS, Callicott JH, Mazzanti CM, Straub RE, Goldman D, Weinberger DR (2001) Effect of COMT Val108/158 Met genotype on frontal lobe function and risk for schizophrenia. Proc Natl Acad Sci USA 98:6917–6922
Eltayb A, Wadenberg ML, Svensson TH (2005) Enhanced cortical dopamine output and antipsychotic-like effect of raclopride with adjunctive low-dose l-dopa. Biol Psychiatry 58:337–343
Emamian ES, Karayiorgou M, Gogos JA (2004) Decreased phosphorylation of NMDA receptor type 1 at serine 897 in brains of patients with Schizophrenia. J Neurosci 24:1561–1564
Farde L, Wiesel FA, Halldin C, Sedvall G (1988) Central D2-dopamine receptor occupancy in schizophrenic patients treated with antipsychotic drugs. Arch Gen Psychiatry 45:71–76
Gessa GL, Canu A, Del Zompo M, Burrai C, Serra G (1991) Lack of acute antipsychotic effect of Sch 23390, a selective dopamine D1 receptor antagonist. Lancet 6;337(8745):854–855
Goldman-Rakic PS, Muly EC, Williams GV (2000) D(1) receptors in prefrontal cells and circuits. Brain Res Brain Res Rev 31:295–301
Gonon FG (1988) Nonlinear relationship between impulse flow and dopamine released by rat midbrain dopaminergic neurons as studied by in vivo electrochemistry. Neuroscience 24:19–28
Gonon F, Buda M, Pujol JF (1984) Treated carbon fibre electrodes for measuring catechols and ascorbic acid. In: Marsden CA (ed) Measurement of neurotransmittor release in vivo. Wiley, Chichester, UK, pp 153–171
Hertel P, Nomikos GG, Iurlo M, Svensson TH (1996) Risperidone: regional effects in vivo on release and metabolism of dopamine and serotonin in the rat brain. Psychopharmacology (Berl) 124:74–86
Hertel P, Fagerquist MV, Svensson TH (1999) Enhanced cortical dopamine output and antipsychotic-like effects of raclopride by alpha2 adrenoceptor blockade. Science 286:105–107
Hoffman DC, Donovan H (1995) Catalepsy as a rodent model for detecting antipsychotic drugs with extrapyramidal side effect liability. Psychopharmacology 120(2):128–133
Jentsch JD, Roth RH (1999) The neuropsychopharmacology of phencyclidine: from NMDA receptor hypofunction to the dopamine hypothesis of schizophrenia. Neuropsychopharmacology 20:201–225
Joyce JN, Millan MJ (2005) Dopamine D3 receptor antagonists as therapeutic agents. Drug Discov Today 10:917–925
Kane J, Honigfeld G, Singer J, Meltzer H (1988) Clozapine for the treatment-resistant schizophrenic. A double-blind comparison with chlorpromazine. Arch Gen Psychiatry 45:789–796
Karlsson P, Smith L, Farde L, Härnryd C, Sedvall G, Wiesel F-A (1995) Lack of apparent antipsychotic effect of the D1-dopamine receptor antagonist SCH39166 in acutely ill schizophrenic patients. Psychopharmacology 121:309–316
Konradsson A, Marcus MM, Hertel P, Svensson TH, Jardemark KE (2006) Inhibition of the glycine transporter GlyT-1 potentiates the effect of risperidone, but not clozapine, on glutamatergic transmission in the rat medial prefrontal cortex. Synapse 60:102–108
Kuroki T, Meltzer HY, Ichikawa J (1999) Effects of antipsychotic drugs on extracellular dopamine levels in rat medial prefrontal cortex and nucleus accumbens. J Pharmacol Exp Ther 288:774–781
Li C (1964) Introduction to experimental statistics. McGraw-Hill, New York, USA, pp 207–226
Liégeois JF, Ichikawa J, Meltzer HY (2002) 5-HT(2A) receptor antagonism potentiates haloperidol-induced dopamine release in rat medial prefrontal cortex and inhibits that in the nucleus accumbens in a dose-dependent manner. Brain Res 947:157–165
Litman RE, Su TP, Potter WZ, Hong WW, Pickar D (1996) Idazoxan and response to typical neuroleptics in treatment-resistant schizophrenia. Comparison with the atypical neuroleptic, clozapine. Br J Psychiatry 168:571–579
Marcus MM, Nomikos GG, Svensson TH (1996) Differential actions of typical and atypical antipsychotic drugs on dopamine release in the core and shell of the nucleus accumbens. Eur Neuropsychopharmacol 6:29–38
Marcus MM, Nomikos GG, Svensson TH (2000) Effects of atypical antipsychotic drugs on dopamine output in the shell and core of the nucleus accumbens: role of 5-HT(2A) and alpha(1)-adrenoceptor antagonism. Eur Neuropsychopharmacol 10:245–253
Marcus MM, Malmerfelt A, Nyberg S, Svensson TH (2002) Biochemical effects in brain of low doses of haloperidol are qualitatively similar to those of high doses. Eur Neuropsychopharmacol 12:379–386
Marcus MM, Jardemark KE, Wadenberg ML, Langlois X, Hertel P, Svensson TH (2005) Combined alpha2 and D2/3 receptor blockade enhances cortical glutamatergic transmission and reverses cognitive impairment in the rat. Int J Neuropsychopharmacol 8:315–327
Meltzer HY, McGurk SR (1999) The effects of clozapine, risperidone, and olanzapine on cognitive function in schizophrenia. Schizophr Bull 25:233–255
Moghaddam B, Bunney BS (1990) Acute effects of typical and atypical antipsychotic drugs on the release of dopamine from prefrontal cortex, nucleus accumbens, and striatum of the rat: an in vivo microdialysis study. J Neurochem 54:1755–1760
Mohn AR, Gainetdinov RR, Caron MG, Koller BH (1999) Mice with reduced NMDA receptor expression display behaviors related to schizophrenia. Cell 98:427–436
Ninan I, Wang RY (2003) Modulation of the ability of clozapine to facilitate NMDA- and electrically evoked responses in pyramidal cells of the rat medial prefrontal cortex by dopamine: pharmacological evidence. Eur J Neurosci 17:1306–1312
Ninan I, Jardemark KE, Wang RY (2003) Differential effects of atypical and typical antipsychotic drugs on N-methyl-d-aspartate- and electrically evoked responses in the pyramidal cells of the rat medial prefrontal cortex. Synapse 48:66–79
Nomikos GG, Iurlo M, Andersson JL, Kimura K, Svensson TH (1994) Systemic administration of amperozide, a new atypical antipsychotic drug, preferentially increases dopamine release in the rat medial prefrontal cortex. Psychopharmacology (Berl) 115:147–156
Nordström AL, Farde L, Nyberg S, Karlsson P, Halldin C, Sedvall G (1995) D1, D2, and 5-HT2 receptor occupancy in relation to clozapine serum concentration: a PET study of schizophrenic patients. Am J Psychiatry 152:1444–1449
Paxinos G, Watson C (1998) The rat brain in stereotaxic coordinates. Academic, New York, USA
Potkin SG, Fleming K, Binneman B, Keller DS, Alphs L, Panagides J (2006) Asenapine effects on cognitive function during acute episodes of schizophrenia: a randomized placebo- and risperidone-controlled trial. Neuropsychopharmacology 31:251
Potkin SG, Cohen M, Panagides J (2007) Efficacy and tolerability of asenapine in acute schizophrenia: a placebo- and risperidone-controlled trial. J Clin Psychiatry (in press)
Robertson GS, Fibiger HC (1992) Neuroleptics increase c-fos expression in the forebrain: contrasting effects of haloperidol and clozapine. Neuroscience 46(2):315–328
Roth BL, Craigo SC, Choudhary MS, Uluer A, Monsma FJ, Shen Y, Meltzer HY, Sibley DR (1994) Binding of typical and atypical antipsychotic agents to 5-hydroxytryptamine-6 and 5-hydroxytryptamine-7 receptors. J Pharmacol Exp Ther 268:1403–1410
Salmi P, Samuelsson J, Ahlenius S (1994) A new computer-assisted two-way avoidance conditioning equipment for rats: behavioral and pharmacological validation. J Pharmacol Toxicol Methods 32:155–159
Schilström B, Nomikos GG, Nisell M, Hertel P, Svensson TH (1998) N-methyl-d-aspartate receptor antagonism in the ventral tegmental area diminishes the systemic nicotine-induced dopamine release in the nucleus accumbens. Neuroscience 82:781–789
Schotte A, Janssen PF, Gommeren W, Luyten WH, Van Gompel P, Lesage AS, De Loore K, Leysen JE (1996) Risperidone compared with new and reference antipsychotic drugs: in vitro and in vivo receptor binding. Psychopharmacology (Berl) 124:57–73
Sedvall G, Farde L (1995) Chemical brain anatomy in schizophrenia. Lancet 346:743–749
Shahid M, Summer BEH, Wong EHF, Henry B (2007a) Asenapine displays distinctive induction patterns of c-fos mRNA expression in rat forebrain regions. Biol Psychiatry 61(8):256S–256S 826 Suppl. 2
Shahid M, Walker GB, Zorn SH, Wong EHF (2007b) Asenapine: a novel psychopharmacologic agent with a unique human receptor signature. J Psychopharmacol (in press)
Siegel S, Castellan JNJ (1988) Nonparametric statistics for the behavioral sciences. McGraw-Hill, New York, USA
Sokoloff P, Diaz J, Le Foll B, Guillin O, Leriche L, Bezard E, Gross C (2006) The dopamine D3 receptor: a therapeutic target for the treatment of neuropsychiatric disorders. CNS Neurol Disord Drug Targets 5:25–43
Svensson TH (2003a) Preclinical effects of conventional and atypical antipsychotic drugs: defining the mechanisms of action. Clinical Neuroscience Research 3:34–36
Svensson TH (2003b) Alpha-adrenoceptor modulation hypothesis of antipsychotic atypicality. Prog Neuropsychopharmacol Biol Psychiatry 27:1145–1158
Tandon R (2002) Safety and tolerability: how do newer generation “atypical” antipsychotics compare? Psychiatr Q 73:297–311
Thomas DR and Hagan JJ (2004) 5-HT7 receptors. Curr Drug Targets CNS Neurol Disord 3(1):81–90
Wadenberg ML, Ahlenius S, Svensson TH (1993) Potency mismatch for behavioral and biochemical effects by dopamine receptor antagonists: implications for the mechanism of action of clozapine. Psychopharmacology (Berl) 110:273–279
Wadenberg ML, Hicks PB (1999) The conditioned avoidance response test re evaluated: is it a sensitive test for the detection of potentially atypical antipsychotics? Neurosci Biobehav Rev 23:851–862
Wadenberg ML, Kapur S, Soliman A, Jones C, Vaccarino F (2000) Dopamine D2 receptor occupancy predicts catalepsy and the suppression of conditioned avoidance response behavior in rats. Psychopharmacology (Berl) 150:422–429
Wadenberg MG, Browning JL, Young KA, Hicks PB (2001a) Antagonism at 5-HT(2A) receptors potentiates the effect of haloperidol in a conditioned avoidance response task in rats. Pharmacol Biochem Behav 68:363–370
Wadenberg ML, Soliman A, VanderSpek SC, Kapur S (2001b) Dopamine D(2) receptor occupancy is a common mechanism underlying animal models of antipsychotics and their clinical effects. Neuropsychopharmacology 25:633–641
Wadenberg ML, Wiker C, Svensson TH (2007) Enhanced efficacy of both typical and atypical antipsychotic drugs by adjunctive alpha 2 adrenoceptor blockade: experimental evidence. Int J Neuropsychopharmacol 10(2):191–202
Weinberger DR, Egan MF, Bertolino A, Callicott JH, Mattay VS, Lipska BK, Berman KF, Goldberg TE (2001) Prefrontal neurons and the genetics of schizophrenia. Biol Psychiatry 50:825–844
Woolley ML, Marsden CA, Fone KC (2004) 5-HT6 receptors. Curr Drug Targets CNS Neurol Disord 3(1):59–79
Acknowledgements
This research was supported by the Swedish Research Council (grant no. 4747), the Karolinska Institutet, Organon Laboratories and Pfizer. Drs. Kent Jardemark and Björn Schilström were supported by grants from the Scandinavian College of Neuro-Psychopharmacology and the Lundbeck Foundation. We thank Dr. Marie-Louise Wadenberg for valuable discussions and Mrs. Anna Malmerfelt and Mrs. Ann-Chatrine Samuelsson for skillful technical assistance.
All experiments were approved by, and conducted in accordance with, the local Animal Ethics Committee, Stockholm North, and the Karolinska Institutet, Sweden.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Frånberg, O., Wiker, C., Marcus, M.M. et al. Asenapine, a novel psychopharmacologic agent: preclinical evidence for clinical effects in schizophrenia. Psychopharmacology 196, 417–429 (2008). https://doi.org/10.1007/s00213-007-0973-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-007-0973-y