Abstract
Rationale
Amphetamine enhances dopamine (DA) transmission and induces psychotic states or exacerbates psychosis in at-risk individuals. Amphetamine sensitization of the DA system has been proposed as a rodent model of schizophrenia-like symptoms. In humans, excessive nonphysiologic drinking or primary polydipsia is significantly associated with a diagnosis of schizophrenia. In rodents, nonphysiologic drinking can be induced by intermittent presentation of food in the presence of a drinking spout to a hungry animal; this phenomenon is termed, “schedule-induced polydipsia” (SIP).
Objective
This study aims to determine the effects of amphetamine sensitization on SIP.
Methods
We injected rats with amphetamine (1.5 mg/kg) daily for 5 days. Following 4 weeks of withdrawal, animals were food restricted and exposed to the SIP protocol (noncontingent fixed-time 1-min food schedule) for daily 2-h sessions for 24 days.
Results
Results showed that previously amphetamine-injected animals drank more in the SIP protocol and drank more than controls when the intermittent food presentation schedule was removed.
Conclusions
These findings suggest that hyperdopaminergia associated with schizophrenia may contribute to the development of polydipsia in this population. Whether animals that develop SIP have DA dysfunction or aberrant activity of other circuits that modulate DA activity has yet to be clearly defined.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Schizophrenia, a disease affecting approximately 1 % of the global population (Jablensky 1997), is characterized by subtle neurological abnormalities that result in disordered perception, cognition, and emotion. Schizophrenia is debilitating, often requiring short term and sometimes permanent hospitalization or institutional living. Of psychiatric inpatients and outpatients with a diagnosis of schizophrenia, up to 20 % (de Leon et al. 1994; Iftene et al. 2013) have been observed to also have primary polydipsia, i.e., either chronic or intermittent excessive drinking without homeostatic or physiologic cause. Comorbid polydipsia can have clinically significant physical complications (Illowsky and Kirch 1988) and continually ingesting large amounts of fluid increases mortality in this population (Hawken et al. 2009).
The pathophysiology underlying polydipsia associated with schizophrenia is largely unknown but dopamine (DA) has been implicated. The role for DA in the etiology of psychosis, a clinical hallmark of schizophrenia, is primarily based on evidence that dopamine D2 receptors are the pharmacological target of all antipsychotic drug treatments (Seeman et al. 1975; Meltzer and Stahl 1976; Seeman 1987; Nord and Farde 2011). Secondly, DA direct and indirect agonists (e.g., amphetamine [AMPH]) can produce symptoms that mimic an acute psychotic state in nonschizophrenic people and exacerbate positive symptoms in individuals with schizophrenia (Angrist and Gershon 1970; Angrist et al. 1974; Lieberman et al. 1987; Friedman and Sienkiewicz 1991). Recent evidence for a relationship between observed hyperactivity of subcortical DA pathways and schizophrenia comes from human imaging studies (Laruelle et al. 1996, 1999; Laruelle 2000; Abi-Dargham et al. 2009; Kegeles et al. 2010). It has been postulated that it is this hyperdopaminergia of schizophrenia that facilitates excessive drinking in polydipsic patients (Illowsky and Kirch 1988; Fukunaka et al. 2007). The evidence comes in part from reports of an associated increase in polydipsic behaviors during psychotic episodes that then abate when the psychosis remits (for reviews, see Illowsky and Kirch 1988; Mittleman et al. 1994). More direct evidence comes from Matsumoto et al. (2005) who demonstrated that polymorphisms in the D2 receptor gene confer susceptibility to polydipsia in schizophrenia. Increases in levels of antipsychotic medication or adding the atypical antipsychotic clozapine (a “broad-spectrum” antagonist; Naheed and Green 2001) may reduce symptom severity as well as the incidence of polydipsia (Zink et al. 2004; for review, see Bersani et al. 2007). Together, this suggests a similar mechanism may underlie psychosis and polydipsia (Raskind et al. 1975; Smith and Clark 1980; Illowsky and Kirch 1988).
In rodents, drinking is in part modulated by DA neurotransmission: intermittent administration of DA-releasing drugs like AMPH or the D2-like receptor agonist quinpirole increases drinking in the hours following injection (Rowland et al. 1981; Fraioli et al. 1997; Cioli et al. 2000). Animals pretreated subchronically with N-methyl-d-aspartate glutamate receptor antagonist MK-801 have also been reported to show spontaneous polydipsia (Hawken et al. 2013a). Excessive drinking behavior in rats has also been examined in a schedule-induced polydipsia (SIP) protocol, where food-restricted animals will drink large quantities of water when presented with intermittent food delivery (Falk 1961). Integrity of the DA systems is implicated in the development of this “adjunctive” behavior (Robbins and Koob 1980; Wallace et al. 1983; Weissenborn et al. 1996); both D1- and D2-like receptor agonists and antagonists disrupt the acquisition of SIP (Todd et al. 1992; for review, see Mittleman et al. 1994). Furthermore, animals that develop SIP show increased DA turnover (Hooks et al. 1994), and increased D2-like and decreased D1-like receptor binding throughout the nucleus accumbens, medial prefrontal cortex, amygdala, and ventral tegmental areas (Pellón et al. 2011) suggesting that an imbalance of DA receptor activation may facilitate SIP behavior.
Repeated AMPH treatment, termed “AMPH sensitization”, followed by a period of AMPH withdrawal produces a chronic and self-sustaining hyperdopaminergic state in rodents (for review, see Robinson and Becker 1986; Paulson and Robinson 1995; Lodge and Grace 2012) that may model some of the neurochemical and behavioral abnormalities associated with the psychotic aspects of schizophrenia (Akbarian et al. 1995; Peleg-Raibstein et al. 2008; for reviews, see Tenn et al. 2003; Yin et al. 2012). Here, we tested the hypothesis that an AMPH sensitization model of schizophrenia-like symptoms augments SIP in rats. We found (like Mittleman and Vallenstein 1985) following AMPH sensitization SIP behavior increased. Additionally, we demonstrated that SIP behavior may, in part, be a learned phenomenon.
Methods
Subjects
Twenty-four male Sprague–Dawley rats weighing 200–225 g (Charles River, QC, Canada) were housed separately in clear Plexiglas cages (45 × 23 × 20 cm deep). The floors were lined with bedding (Beta Chip, NEPCO, Warrenburg, NY, USA) and the cages were located in a climate-controlled colony room (21 ± 1 °C; humidity, 40–70 %) on a reversed 12-h light/dark schedule (lights off at 0700 hours). Animals initially had free access to both food (LabDiet rodent feed #5001,PMI Nutrition International, Brentwood, MO, USA) and water but were later food restricted (see next section). Rats were treated in accordance with the guidelines of the Canadian Council on Animal Care, and the Queen's University Animal Care Committee approved the experimental protocol.
Drug treatment
One week following arrival in the facility, animals were randomly assigned to either receive once daily intraperitoneal injections of d-amphetamine sulfate (Sigma, Oakville, ON, Canada) dissolved in saline at a dose of 1.5 mg/kg or saline (1 ml/kg) for five consecutive days. A 28-day washout period followed the last injection. During this time, animals were food (but not water) restricted, i.e., they were allowed free access to food for 2 h per day. Food restriction was continued for the duration of the study.
Apparatus
Four commercially built (Med Associate Inc., St. Albans, VT, USA) experimental chambers (30.5 × 24.1 × 21 cm) were housed inside sound-attenuating cabinets that contained an electric fan for ventilation that ran throughout the experiment. The boxes were made of polycarbonate with aluminum panels and steel grid flooring. A light was illuminated in the box for the duration of the session. Each reward consisted of one 45-mg dustless precision food pellet (Bio-serv, Frenchtown, NJ, USA), released into the recessed dispenser tray (5 × 8 × 4 cm). On the opposite wall of the pellet dispenser and sitting between two inactive levers was a metal drinking spout containing a ball bearing. The drinking spout was freely available the entire session. A photo beam sensor was positioned across the mouth of the drinking spout to measure head entries. Inactive levers recorded lever presses. The experimental chambers were controlled by a computer running MED-PC IV (Med Associates Inc.).
Behavioral testing
All animals completed 24 days of testing. Prior to each testing session, 22-h home-cage drinking (by weighing home-cage water bottles) and animal weights were recorded. For the first two 2-h testing sessions, all animals received 120 pellets freely available in a dish at the start of the session (free feed [FF]). On day 3, experimental animals (AMPH, n = 6; saline, n = 6) were then tested: for each session, the test box automatically dispensed a pellet every min for a total of 120 pellets over 120 min. Control animals (AMPH, n = 6; saline, n = 6) did not receive a scheduled delivery of pellets but instead had FF. On day 24, all groups again received FF. Animals were tested in squads of four in daily morning and afternoon sessions. The amount of water consumed in each test session was recorded by measuring the before and after weights of the water bottles. Following testing, the animals were returned to their home cages and allowed free access to food for 2 h.
Statistical analysis
All analyses were performed using SPSS version 17.0 (Chicago, IL, USA). Control data were used to determine if the SIP protocol was successfully established. Animals were deemed to have developed SIP when they consumed at least 15 ml of water per 2-h session for three consecutive days (Hawken et al. 2011). Amount of water drunk during the testing sessions was also compared to 22-h home-cage water consumption (percent of home-cage drinking). Drinking more in the 2-h session than that consumed daily is a reported definition of polydipsia (Flory 1971). Acquisition (testing days, 3–23) and expression (testing days, 2 and 24) were analyzed between the protocol (experimental × control) and the treatment (AMPH × saline) conditions across days using repeated measures analysis of variance (ANOVA). Tests of simple effects were used to examine significant interactions. For repeated measures ANOVA, trend analyses (contrasts) were performed. Neither sphericity of variance nor a significant main effect of the within-subject variable is an assumption of running trend analysis (Glass and Hopkins 1996).
Results
SIP acquisition
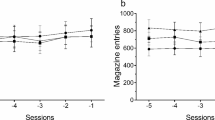
The AMPH experimental groups that received intermittent food presentation drank substantially more during daily 2-h sessions than the other groups; there was some evidence of a greater increase in drinking in the saline experimental group in later sessions (Fig. 1; three-way ANOVA revealed a significant main effect of day (F[1, 20] = 10.9, p = 0.004), day × protocol interaction (F[1, 20] = 4.74, p = 0.042), treatment (F[1, 20] = 11.7, p = 0.003), protocol (F[1, 20] = 14.7, p = 0.001), and a significant treatment x protocol interaction (F[1, 20] = 9.08, p = 0.007)). Two-way ANOVA examining the within-protocol effects of treatment on daily session drinking revealed significantly more drinking in the AMPH group compared to the saline controls within the experimental protocol (main effect of day (F[1, 10] = 8.47, p = 0.016) and treatment (F[1, 10] = 14.0, p = 0.004)). The AMPH control group failed to drink more than the saline control group (Fig. 1). AMPH-treated animals in the experimental protocol gradually increased drinking over the days.
Five injections of amphetamine (AMPH) given weeks earlier significantly increased drinking in the schedule-induced polydipsia protocol across days. Daily mean (±SEM) water drinking (in milliliter) during the 2-h testing session for AMPH and saline groups in experimental and control protocols are shown. Free feeding (FF) sessions demonstrated AMPH-treated animals learned to drink more in the SIP protocol. *ANOVA revealed a significant effect of AMPH (p < 0.05)
Animals in the experimental protocol increased weight over the days (F[1, 10] = 83.0, p < 0.001), but weight gain across the two groups (AMPH and saline) was not significantly different (data not shown). Thus, increased drinking was not due to differences in body weight.
In the experimental protocol, two rats in the AMPH group developed SIP (three consecutive days consuming at least 15 ml) and two more nearly developed SIP (two consecutive days consuming at least 15 ml), compared to none of the saline-treated rats. At the end of the 21 days of testing, two of the six AMPH-treated rats drank more in the daily 2-h drinking sessions than they drank in 22-h in their home cages. None of the rats in the saline group achieved this. Control animals not subjected to the 1-min schedule of pellet delivery did not develop SIP. That is, control animals failed to drink more than 15 ml on three consecutive days and also failed on any day to drink more than their daily 22-h water consumption.
Home-cage drinking increased over days for all rats (Fig. 2; F[1, 20] = 40.3, p < 0.001) and was not different between protocols or drug conditions. When the amount of water consumed in each daily testing session was expressed as a percentage of home-cage drinking (data not shown), only the AMPH treatment group in the experimental protocol showed an across-day pattern of drinking a larger proportion of their daily intake during testing sessions (three-way ANOVA showed a significant day × protocol interaction (F[1, 20] = 6.09, p = 0.023) and significant effects for protocol (F[1, 20] = 12.9, p = 0.002), treatment (F[1, 20] = 8.67, p = 0.008), and a protocol × treatment interaction (F[1, 20] = 7.30, p = 0.014)). Two-way ANOVA confirmed the treatment effect was largest for the AMPH-treated rats in the experimental protocol (significant main effect of day (F[1, 10] = 5.14, p = 0.042) and treatment (F[1, 10] = 9.60, p = 0.011)).
When duration of time spent at the drinking spout was averaged across the 21 test days into 5-s bins (Fig. 3), AMPH and saline animals in the experimental protocol showed the postprandial pattern of drinking characteristic of SIP. Spout time for the experimental groups increased after pellet delivery to a maximum in the sixth 5-s bin and then declined to control levels toward the end of the 60-s interval. AMPH-treated animals in the experimental protocol showed the longest duration of drinking throughout most of the interpellet interval. Control animals spent a consistently low amount of time at the spout (Fig. 3). This is further evidence that the SIP protocol was successfully established in the experimental groups.
The experimental (intermittent food presentation) protocol increased time spent at the drinking spout. Mean (±SEM) duration (s) at the drinking spout during the inter-pellet interval (1 min; measured in 5-s bins) over 21 days for amphetamine (AMPH) and saline experimental and control groups is shown
SIP expression
Following 21 days of SIP or control training, in a final day of testing all animals (regardless of protocol) received a dish of 120 pellets (FF) during the their daily 2-h session (Fig. 1). The AMPH experimental group drank more in spite of no longer receiving intermittent food. A three-way ANOVA comparing drinking under FF conditions averaged for the two FF days prior to training and the FF day that followed training revealed a significant effect of day (F[1, 20] = 61.0, p < 0.001), nearly significant day × protocol interaction (F[1, 20] = 4.32, p = 0.051), and a significant day × treatment × protocol interaction (F[1, 20] = 9.02, p = 0.007). Further analysis of the experimental protocol groups by a two-way ANOVA revealed a significant day × treatment interaction (F[1, 10] = 5.09, p = 0.048) and a trend toward significance for treatment (F[1, 10] = 4.61, p = 0.057) suggesting that animals that experienced intermittent food presentation learned to drink more independently of the food schedule. One-way ANOVA for FF prior to SIP training showed no differences between AMPH and saline groups; however, following SIP training AMPH-treated animals drank significantly more during FF than saline-treated controls (F[1, 11] = 7.18, p = 0.023) demonstrating conditioning. This was not true in the control protocol where animals were not exposed to SIP training and did not show increased drinking following 21 days of FF exposure.
Discussion
We examined possible excessive drinking in the context of an AMPH sensitization model of schizophrenia-like symptoms. Animals exposed to a 5-day repeated treatment regimen of the DA-releasing agent AMPH drank significantly more weeks later in a schedule-induced polydipsia protocol than those that received saline alone. Furthermore, AMPH pretreated animals also drank more following the SIP protocol in the absence of an intermittent food schedule. These findings suggest a hyperdopaminergic animal model of polydipsia associated with schizophrenia akin to that observed in the human population.
A moderate amount of SIP was successfully established in our animals as demonstrated through both comparisons to home cage water consumption and control groups not exposed to the intermittent food delivery schedule (Falk 1961, 1969; Flory 1971). In humans, not all individuals with schizophrenia go on to develop polydipsia. The setup reported here produces SIP rates (roughly 30 %) comparable to the frequency of polydipsia reported in schizophrenia populations (approximately 20 %; de Leon et al. 1994).
Excessive drinking in the SIP protocol happens only after repeated pairing of intermittent food with access to a drinking spout. SIP cannot develop in the absence of intermittent food delivery (Falk 1971) and also fails to develop if water is introduced after animals have received a schedule of intermittent food presentation without concurrent water availability or a schedule that is paired with wheel running (Williams et al. 1992). Over the course of days, repeated acute AMPH treatments in the home cage cause increased drinking (Rowland et al. 1981) initially in the presence of food but over time food availability is no longer necessary to sustain the increased intake of water. It appears that eventually, the animals learn to drink in excess of need. We demonstrated this in the SIP protocol and postulate that over time polydipsia in humans may also become a learned pattern of behavior facilitated by a hyperdopaminergic state (for review, see Murray et al. 2008). For instance, in susceptible patients (i.e., acutely psychotic) schedules of institutional living may trigger unregulated drinking behavior that over time, becomes habitual, free of the routine that elicited the behavior in the first place. In SIP, further experiments are necessary to test if this learned behavior is sustained.
The findings of this study markedly contradict studies that have administered AMPH shortly before each SIP testing session (either during or after SIP acquisition): in neurologically healthy animals, such treatments have by and large prevented or attenuated SIP behavior (Yoburn and Glusman 1982; for review, see Mittleman et al. 1994; Didriksen and Christensen 1993). Acute treatments of AMPH increase DA activity via various DA-releasing mechanisms that allows DA to accumulate in the synapse of active DA neurons (Sulzer et al. 1995; Kahlig et al. 2005; for review see Fleckenstein et al. 2007) initially augmenting but then occluding the phasic DA signal. This exaggerated DA efflux (enhanced further by food restriction) into the synapse and its behavioral consequences (increased locomotion and other stereotypic behavior) may abolish the opportunity for SIP to develop (Hooks et al. 1991; Mittleman et al. 1994; Cadoni et al. 2003).
Unlike these studies, we administered AMPH in a 5-day period prior to behavioral testing, followed with a period of drug withdrawal after which animals were tested (entirely drug free). In a similar protocol but with higher and more frequent doses (5 mg/kg, twice daily for 5 days), Mittleman and Valenstein (1985) demonstrated that pre-exposing animals to a regimen of repeated AMPH treatments, followed by 7 days of withdrawal before the start of SIP testing augments SIP. Here, we used substantially lower doses (1.5 mg/kg once a day for 5 days) [Lodge and Grace 2008] of AMPH and a much longer withdrawal period (28 days) to achieve a similar result, demonstrating the sustained long-term effects of low-dose exposure to repeated AMPH treatment. AMPH pretreatment also increases DA activity but in a capacity different than that in acute administration by increasing the population of DA neurons that are active (Lodge and Grace 2008). Thus, the phasic DA signal is enhanced but in a way that maintains the integrity of the signal at the synapse. These two treatment protocols (acute versus the repeated treatment protocol used in our study) likely led to the differential behavioral outcomes on SIP development.
While the neuroanatomial and neurochemical mechanisms mediating SIP and its augmentation by subchronic AMPH treatment remain unknown, both studies of acute and subchronic AMPH regimens suggest the hypothesis that predisposition to nonregulatory drinking may be related to some property of the DA system (Mittleman and Valenstein 1985; López-Grancha et al. 2008). These abnormalities of DA neurotransmission may be secondary to a prefrontal (Deutch 1992) or glutamate dysfunction (Weinberger 1987; Grace 1991; Olney and Farber 1995; Lodge and Grace 2008). Furthermore, the effect of amphetamine sensitization on other monoamines, i.e., serotonin and noradrenaline, as a promoter of SIP cannot be ruled out as repeated treatment of AMPH has been reported to increase reactivity of noradrenergic and serotonergic neurons (Tassin 2008) and both serotonin and noradrenaline in turn have been implicated in SIP behavior (Lu et al. 1992; Tung et al. 2008). How these systems contribute to SIP pathophysiology, however, remains to be elucidated.
Conclusion
Repeated AMPH treatment is a model of schizophrenia-like symptoms that focuses on replicating the pathophysiology of schizophrenia and not its etiology (for review, see Tenn et al. 2003). Here, we demonstrate that repeated AMPH increases drinking behavior that may result from a hyperfunctioning of DA systems. This, along with the evidence that subchronic MK-801 treatment and social isolation also increase SIP and other polydipsias in rats (Hawken et al. 2011, a, b) further supports the idea that the pathophysiology of schizophrenia also participates in the development of polydipsia observed in schizophrenic populations. Future studies need to characterize the behavioral changes in rats treated with subchronic AMPH and to dissect the contribution of various brain regions, related circuitry, and neurotransmitter systems that facilitate excessive fluid intake associated with schizophrenia.
References
Abi-Dargham A, van de Giessen E, Slifstein M, Kegeles LS, Laruelle M (2009) Baseline amphetamine-stimulated dopamine activity are related in drug-naïve schizophrenic subjects. Biol Psychiatry 65:1091–1093
Akbarian S, Kim JJ, Potkin SG, Hagman JO, Tafazzoli A, Bunney WE Jr, Jones EG (1995) Gene expression for glutamic acid decarboxylase is reduced without loss of neurons in prefrontal cortex of schizophrenics. Arch Gen Psychiatry 52:258–266
Angrist BM, Gershon S (1970) The phenomenology of experimentally induced AMPH psychosis—preliminary observation. Biol Psychiatry 2:95–107
Angrist BM, Sathananthan G, Wilk S, Gershon S (1974) AMPH psychosis: behavioral and biochemical aspects. J Psychiatr Res 11:13–23
Bersani G, Pesaresi L, Orlandi V, Gherardelli S, Pancheri P (2007) Atypical antipsychotics and polydipsia: a cause or a treatment? Hum Psychopharmacol 22:103–107
Cadoni C, Solinas M, Valentini V, Chiara GD (2003) Selective psychostimulant sensitization by food restriction: differential changes in accumbens shell and core dopamine. Eur J Neurosci 18:2326–2334
Cioli I, Caricati A, Nencini P (2000) Quinpirole-and AMPH-induced hyperdipsia: influence of fluid palatability and behavioral cost. Behav Brain Res 109:9–18
de Leon JD, Verghese C, Tracy JI, Josiassen RC, Simpson GM (1994) Polydipsia and water intoxication in psychiatric poatients: a review of the epidemiological literature. Biol Psychiatry 35(6):408–419
Deutch AY (1992) The regulation of subcortical dopamine systems by the prefrontal cortex: interactions of central dopamine systems and pathogenesis of schizophrenia. J Neural Transm Suppl 36:61–89
Didriksen M, Christensen AV (1993) The attenuation of schedule-induced polydipsia by dopamine blockers is not an expression of extrapyramidal side effect liability. Behav Pharmacol 4:517–522
Falk JL (1961) Production of polydipsia in normal rats by an intermittent food schedule. Science 133:195–196
Falk JL (1969) Conditions producing psychogenic polydipsia in animals. Ann N Y Acad Sci 157:569–593
Falk JL (1971) The nature and determinants of adjunctive behavior. Physiol Behav 6:577–588
Fleckenstein AE, Volz TJ, Riddle EL, Gibb JW, Hanson GR (2007) New insights into the mechanism of action of AMPHs. Annu Rev Pharmacol Toxicol 47:681–698
Flory RK (1971) The control of schedule-induced polydipsia: frequency and magnitude of reinforcement. Learn Motiv 2:215–227
Fraioli S, Cioli I, Nencini P (1997) Amphetamine reinstates polydipsia induced by chronic exposure to quinpirole, a dopaminergic D2 agonist, in rats. Behav Brain Res 89:199–215
Friedman A, Sienkiewicz J (1991) Psychotic complications of long-term levodopa treatment of Parkinson's disease. Acta Neurol Scand 84:111–113
Fukunaka Y, Shinkai T, Hwang R, Hori H, Utsunomiya K, Sakata S, Naoe Y, Shimizu K, Matsumoto C, Ohmori O, Nakamura J (2007) The orexin 1 receptor (HCRTR1) gene as a susceptibility gene contributing to polydipsia-hyponatremia in schizophrenia. Neuromolecular Med 9:292–297
Glass GV, Hopkins KD (1996) Statistical methods in psychology and education, 3rd edn. Allyn and Bacon, Maryland
Grace AA (1991) Phasic versus tonic dopamine release and the modulation of dopamine system responsivity: a hypothesis for the etiology of schizophrenia. Neuroscience 41:1–24
Hawken ER, Crookall JM, Reddick D, Millson RC, Milev R, Delva N (2009) Mortality over a 20-year period in patients with primary polydipsia associated with schizophrenia: a retrospective study. Schizophr Res 107:128–133
Hawken ER, Delva NJ, Reynolds JN, Beninger RJ (2011) Increased schedule-induced polydipsia in the rat following subchronic treatment with MK-801. Schizophr Res 125:93–98
Hawken ER, Lister J, Winterborn AN, Beninger RJ (2013a) Spontaneous polydipsia in animals treated subchronically with MK-801. Schizophr Res 143:228–230
Hawken ER, Delva NJ, Beninger RJ (2013b) Increased drinking following social isolation rearing: implications for polydipsia associated with schizophrenia. PLoS One 8:e56105. doi:10.1371/journal.pone.0056105
Hooks MS, Jones GH, Neill DB, Justice JB (1991) Individual differences in AMPH sensitization: dose-dependent effects. Pharmacol Biochem Behav 41:203–210
Hooks MS, Jones GH, Junos JL, Neill DB, Justice JB (1994) Individual differences in schedule-induced and conditioned behaviors. Behav Brain Res 60:199–209
Iftene F, Bowie C, Milev R, Hawken E, Talikowska-Szymczak E, Potopsingh D, Hanna S, Mulroy J, Groll D, Millson R (2013) Identification of primary polydipsia in a severe and persistent mental illness outpatient population: a prospective observational study. Psychiatry Res. doi:10.1016/j.psychres.2013.04.011
Illowsky BP, Kirch DG (1988) Polydipsia and hyponatremia in psychiatric patients. Am J Psychiatry 145:675–683
Jablensky A (1997) The 100-year epidemiology of schizophrenia. Schizophr Res 28:111–125
Kahlig KM, Binda F, Khoshbouei H, Blakely RD, McMahon DG, Javitch JA, Galli A (2005) Amphetamine induces dopamine efflux through a dopamine transporter channel. Proc Natl Acad Sci U S A 102:3495–3500
Kegeles LS, Abi-Dargham A, Frankle G, Gil R, Cooper TB, Slifstein M, Hwang DR, Huang Y, Haber SN, Laruelle M (2010) Increased synaptic dopamine function in associative regions of the striatum in schizophrenia. Arch Gen Psychiatry 67:231–239
Laruelle M (2000) The role of endogenous sensitization in the pathophysiology of schizophrenia: implications from recent brain imaging studies. Brain Res Brain Res Rev 31:371–384
Laruelle M, Abi-Dargham A, van Dyck CH, Gil R, D'Souza CD, Erdos J, McCance E, Rosenblatt W, Fingado C, Zoghbi SS, Baldwin RM, Seibyl JP, Krystal JH, Charney DS, Innis RB (1996) Single photon emission computerized tomography imaging of AMPH-induced dopamine release in drug-free schizophrenic subjects. Proc Natl Acad Sci U S A 93:9235–9240
Laruelle M, Abi-Dargham A, Gil R, Kegeles L, Innis R (1999) Increased dopamine transmission in schizophrenia: relationship to illness phases. Biol Psychiatry 46:56–72
Lieberman JA, Kane JM, Alvir J (1987) Provocative tests with psychostimulant drugs in schizophrenia. Psychopharmacology (Berl) 91:415–433
Lodge DJ, Grace AA (2008) Amphetamine activation of hippocampal drive of mesolimbic dopamine neurons: a mechanism of behavioral sensitization. J Neurosci 28:7876–7882
Lodge DJ, Grace AA (2012) Divergent activation of ventromedial and ventrolateral dopamine systems in animal models of AMPH sensitization and schizophrenia. Int J Neuropsychopharmacol 15:69–76
López-Grancha M, Lopez-Crespo G, Sanchez-Amate MC, Flores P (2008) Individual differences in schedule-induced polydipsia and the role of GABAergic and dopaminergic systems. Psychopharmacology (Berl) 197:487–498
Lu CC, Tseng CJ, Wan FJ, Yin TH, Tung CS (1992) Role of locus coeruleus and serotonergic drug actions on schedule-induced polydipsia. Pharmacol Biochem Behav 43:255–261
Matsumoto C, Shinkai T, Luca VD, Hwang R, Hori H, Lanktree M, Ohmori O, Kennedy JL, Nakamura J (2005) Association between three functional polymorphisms of the dopamine D2 receptor gene and polydipsia in schizophrenia. Int J Neuropsychopharmacol 8:245–253
Meltzer HY, Stahl SM (1976) The dopamine hypothesis of schizophrenia: a review. Schizophr Bull 2:19–76
Mittleman G, Valenstein ES (1985) Individual differences in non-regulatory ingestive behavior and catecholamine systems. Brain Res 348:112–117
Mittleman G, Rosner AL, Schaub CL (1994) Polydipsia and dopamine: behavioral effects of dopamine D1 and D2 receptor agonists and antagonists. J Pharmacol Exp Ther 271:638–650
Murray RM, Lappin J, Di Forti M (2008) Schizophrenia: from developmental deviance to dopamine dysregulation. Eur Neuropsychopharmacol 18(Suppl 3):S129–S134
Naheed M, Green B (2001) Focus on clozapine. Curr Med Res Opin 17:223–229
Nord M, Farde L (2011) Antipsychotic occupancy of dopamine receptors in schizophrenia. CNS Neurosci Ther 17:97–103
Olney JW, Farber NB (1995) Glutamate receptor dysfunction and schizophrenia. Arch Gen Psychiatry 52:998–1007
Paulson PE, Robinson TE (1995) AMPH-induced time-dependent sensitization of dopamine neurotransmission in the dorsal and ventral striatum: a microdialysis study in behaving rats. Synapse 19:56–65
Peleg-Raibstein D, Knuesel I, Feldon J (2008) AMPH sensitization in rats as an animal model of schizophrenia. Behav Brain Res 191:190–201
Pellón R, Ruiz A, Moreno M, Claro F, Ambrosio E, Flores P (2011) Individual differences in schedule-induced polydipsia: neuroanatomical dopamine divergences. Behav Brain Res 217:195–201
Raskind MA, Orenstein H, Christopher G (1975) Acute psychosis, increased water ingestion, and inappropriate antidiuretic hormone secretion. Am J Psychiatry 132:907–910
Robbins TW, Koob GF (1980) Selective disruption of displacement behaviour by lesions of the mesolimbic dopamine system. Nature 285:409–412
Robinson TE, Becker JB (1986) Enduring changes in brain and behavior produced by chronic AMPH administration: a review and evaluation of animal models of AMPH psychosis. Brain Res 396:157–198
Rowland N, Antelman SM, Kocan D (1981) Elevated water intake in rats treated chronically with AMPH: drinking in excess of need? Appetite 2:51–66
Seeman P (1987) Dopamine receptors and the dopamine hypothesis of schizophrenia. Synapse 1:133–152
Seeman P, Chau-Wong M, Tedesco J, Wong K (1975) Brain receptors for antipsychotic drugs and dopamine: direct binding assays. Proc Natl Acad Sci U S A 72:4376–4380
Smith WO, Clark ML (1980) Self-induced water intoxication in schizophrenic patients. Am J Psychiatry 139:1055–1059
Sulzer D, Chen TK, Lau Y, Kristensen H, Rayport S, Ewing A (1995) Amphetamine redistributes dopamine from synaptic vesicles to the cytosol and promotes reverse transport. J Neurosci 15:4102–4108
Tassin JP (2008) Uncoupling between noradrenergic and serotonergic neurons as a molecular basis of stable changes in behavior induced by repeated drugs of abuse. Biochem Pharmacol 75:85–97
Tenn CC, Fletcher PJ, Kapur S (2003) AMPH-sensitized animals show a sensorimotor gating and neurochemical abnormality similar to that of schizophrenia. Schizophr Res 64:103–114
Todd KG, Beck CH, Martin-Iverson MT (1992) Effects of D1 and D2 receptor antagonists on behavior of polydipsic rats. Pharmacol Biochem Behav 42:381–388
Tung CS, Lu CC, Liu YP, Tseng CJ, Yin TH (2008) Schedule-induced polydipsia increased both mesotelencephalic-dopaminergic and pontine-noradrenergic activities in the rat brain. Chin J Physiol 38:57–63
Wallace M, Singer G, Finlay J, Gibson S (1983) The effect of 6-OHDA lesions of the nucleus accumbens septum on schedule-induced drinking, wheel running and corticosterone levels in the rat. Pharmacol Biochem Behav 18:129–136
Weinberger DR (1987) Implications of normal brain development for the pathogenesis of schizophrenia. Arch Gen Psychiatry 44:660–669
Weissenborn R, Blaha CD, Winn P, Phillips AG (1996) Schedule-induced polydipsia and the nucleus accumbens: electrochemical measurements of dopamine efflux and effects of excitotoxic lesions in the core. Behav Brain Res 75:147–158
Williams SL, Tang M, Falk JL (1992) Prior exposure to a running wheel and scheduled food attenuates polydipsia acquisition. Physiol Behav 52:481–483
Yin DM, Chen YJ, Sathyamurthy A, Xiong WC, Mei L (2012) Synaptic dysfunction in schizophrenia. In: Kreutz MR, Sala C (eds) Synaptic plasticity, advances in experimental medicine and biology. Springer, Wien, pp 493–516
Yoburn BC, Glusman M (1982) Effects of chronic d-AMPH on the maintenance and acquisition of schedule-induced polydipsia in rats. Physiol Behav 28:807–818
Zink M, Sartorius A, Lederbogen F (2004) Remission of polydipsia as antipsychotic effect of clozapine. Eur Psychiatry 19:320–321
Acknowledgments
This research was funded by the Ontario Mental Health Foundation. The authors have full control of the primary data and agree to allow the journal to review that data if requested.
Conflicts of interest
The authors have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hawken, E.R., Beninger, R.J. The amphetamine sensitization model of schizophrenia symptoms and its effect on schedule-induced polydipsia in the rat. Psychopharmacology 231, 2001–2008 (2014). https://doi.org/10.1007/s00213-013-3345-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-013-3345-9