Abstract
Rationale
Ketamine is a non-competitive N-methyl-d-aspartate (NMDA) receptor antagonist which interferes with the action of excitatory amino acids (EAAs) including glutamate and aspartate. The use of ketamine at subanaesthetic doses has increased because of its psychotomimetic properties. However, long-term ketamine abuse may interfere with memory processes and inhibit the induction of long-term potentiation (LTP) in the hippocampus, an effect probably mediated by its NMDA antagonist action. Neurotrophins such as brain-derived neurotrophic factor (BDNF) and nerve growth factor (NGF) serve as survival factors for selected populations of central nervous system neurons, including cholinergic and dopaminergic neurons. In addition, neurotrophins, particularly BDNF, may regulate LTP in the hippocampus and influence synaptic plasticity.
Objectives
The purpose of this study was to test the hypothesis that ketamine use in humans is associated with altered serum levels of neurotrophins.
Methods
We measured by enzyme-linked immunosorbent assay the NGF and BDNF serum levels in two groups of subjects: frequent ketamine users and healthy subjects.
Results
Our data show that BDNF serum levels were increased in chronic ketamine users as compared to healthy subjects, while NGF levels were not affected by ketamine use.
Conclusion
These findings suggest that chronic ketamine intake is associated with increases in BDNF serum levels in humans. Other studies are needed to explore the pharmacological and molecular mechanism by which ketamine, and/or other NMDA antagonists, may induce modification in the production and utilization of BDNF and alter normal brain function.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ketamine is a non-competitive N-methyl-d-aspartate (NMDA) receptor antagonist which interferes with the action of excitatory amino acids (EAAs) including glutamate and aspartate (Anis et al. 1983). Initially used as a dissociative anaesthetic, the non-medical use of ketamine has increased because of its psychotomimetic properties. The diverse subjective experiences of ketamine include the sensation of light through the body; novel experiences concerning ‘body consistency’ (e.g. being made of wood or rubber); grotesque distortion of shape or size of body parts; visions, hallucinations; sensations of melting together with people or things in the environment; and ‘out of body’ experiences (Hansen et al. 1988; Curran and Morgan 2000a, b). Other studies have shown that ketamine, at subanaesthetic doses, disrupts attentional function and explicit memory (Ghoneim et al. 1985; Krystal et al. 1994; Harborne et al. 1996; Malhotra et al. 1996; Adler et al. 1998; Newcomer et al. 1999). Moreover, ketamine inhibits the induction of long-term potentiation (LTP) in the hippocampus (Harris et al. 1984), an effect probably mediated by its NMDA antagonist action (Muller et al. 1988; Zhang and Levy 1992).
Neurotrophins such as brain-derived neurotrophic factor (BDNF) and nerve growth factor (NGF) serve as survival factors for selected populations of central nervous system (CNS) neurons, including cholinergic and dopaminergic neurons (Lad et al. 2003; Hyman et al. 1991; Ha et al. 1999). In addition, neurotrophins, particularly BDNF, may regulate LTP in the hippocampus (Minichiello 2009) and influence synaptic plasticity (Verpelli et al. 2010). Thus, deficits in the production and utilization of these proteins can lead to a variety of CNS dysfunctions (Connor and Dragunow 1998), including those elicited by psychoactive compounds (Meredith et al. 2002; Angelucci et al. 2007a). Supporting this idea in human studies, we found that chronic use of drugs, such as heroin and cocaine and cannabis, is associated with decreased serum concentrations of both NGF and BDNF (Angelucci et al. 2007b, 2008, 2009).
Studies performed in rats showed that prolonged exposure to ketamine may increase neurodegeneration and BDNF levels in developing brains (Ibla et al. 2009), while expression of messenger RNA of neurotrophins and their receptors were found to be altered after subchronic ketamine treatment used as a model of schizophrenia (Becker et al. 2008). These findings suggest that ketamine use in humans may be associated with altered serum levels of neurotrophins. To test this hypothesis, in this study, we measured by enzyme-linked immunosorbent assay (ELISA) the NGF and BDNF serum levels in two groups of subjects: frequent ketamine users and healthy subjects.
Materials and methods
Subjects
This study was performed at the Department of Clinical and Behavioural Neurology, IRCCS Santa Lucia Foundation and at the Psychiatry Division of the Catholic University (Policlinico Gemelli), Rome, Italy. The characteristics of the experimental groups are summarized in Table 1. Participants were recruited using a ‘snowball’ sampling technique (Solowij et al. 1992) and only frequent ketamine users (defined as subjects taking ketamine at least four times/week) were included in the study (Curran and Morgan 2000a, b). Urine samples were also analysed (Medscreen, London, UK) to confirm the inclusion criteria in the group of ketamine users. Drug screening tests were also performed to ascertain the use of other psychoactive compounds: among ketamine users, ten subjects assumed at irregular intervals cannabis and three subjects other psychostimulants such as cocaine and amphetamine (see Table 1).
Ketamine users fulfilled DSM-IV criteria for ketamine dependence at the time of the study. The diagnosis was determined in a consensus procedure using clinical material and the Mini International Neuropsychiatric Interview for psychiatric disorders (First et al. 1997). The psychopathological status of the ketamine and control groups was assessed by a trained physician using the 21-item Hamilton Depression Rating Scale (Hamilton 1960) for depression and the Hamilton Anxiety Rating Scale (Hamilton 1959) for anxiety. Cognitive status was evaluated with the Mini Mental State Examination (Folstein et al. 1975). Drug users were required to abstain from psychotropic drug use for at least 15 h prior to testing, to have no history of head injury or organic brain damage. Control subjects had neither self-reported personal or familial psychiatric history nor medication history. The study was approved by the institutional ethics committee and all subjects gave written informed consent.
Blood sampling
Venous blood was collected into sampling tubes that were centrifuged within 20 min after sampling at 2,000×g for 20 min. Serum was then aliquoted and stored at −80°C until analysis.
Determination of NGF and BDNF content in serum
BDNF and NGF were detected in sandwich ELISAs according to the manufacturer’s instructions (R & D Systems, Minneapolis, MN, USA). These sandwich ELISAs are set in order to measure natural and recombinant human mature BDNF and NGF in cell culture medium and serum. All assays were performed on F-bottom 96-well plates (Nunc, Wiesbaden, Germany).
Tertiary antibodies were conjugated to horseradish peroxidase. Wells were developed with tetramethylbenzidine and measured at 450/570 nm. Neurotrophin content was quantified against a standard curve calibrated with known amounts of protein. The detection limits were 15 pg/ml for BDNF and 8 pg/ml for NGF. Measurements were performed in duplicate and are expressed as nanogram per millilitre (BDNF) or picogram per millilitre (NGF). Cross-reactivity to related neurotrophins (NT-3, NT-4) was less than 3%.
Statistical analysis
Student’s t test was used with experimental groups (ketamine users and healthy subjects) as variables. The statistical significance level was set at P < 0.05.
Results
Demographic characteristics of ketamine users and control subjects
The demographic characteristics of the two groups are shown in Table 1. No differences in age, sex or years of education were found. Also, no evidence for age and gender differences in circulating neurotrophin levels was found. Therefore, data were pooled for subsequent analysis.
BDNF serum levels in ketamine users and controls
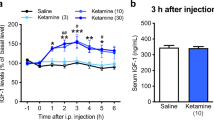
Figure 1 shows the levels of circulating BDNF in ketamine users and healthy subjects. Student’s t test showed that circulating BDNF levels were significantly higher (DF = 1, 26; F value = 12.6; P value = 0.0015) in ketamine users than in healthy subjects (12.70 ± 1.33 ng/ml ketamine; 6.159 ± 0.97 ng/ml control).
NGF serum levels in ketamine users and controls
NGF serum levels in ketamine users and controls are also shown in Fig. 1. As assessed by Student’s t test, NGF levels in ketamine users were comparable to those of healthy subjects (DF = 1, 26; F value = 0.022; P value = 0.884) (100 ± 46.1 pg/ml ketamine; 110.7 ± 55.4 pg/ml control).
Discussion
This study was performed in order to elucidate the effect of chronic ketamine intake on serum levels of neurotrophins in human subjects. The results demonstrated that BDNF serum levels were increased in chronic ketamine users as compared to healthy subjects, while NGF levels were not affected by ketamine use.
This is the first study showing a significant increase in serum BDNF concentrations in subjects with a history of frequent ketamine use. Ketamine is an antagonist of NMDA receptor, while BDNF is a trophic factor and involved in the maintenance of midbrain dopaminergic neurons (Hyman et al. 1991) and in the regulation of synaptic plasticity (Thoenen 1995). Noteworthy, BDNF has been shown to influence, or be influenced by, glutamate signalling. It was demonstrated that elevated glutamate extracellular levels stimulate the production of BDNF in neurons (Marini et al. 1998; Lee et al. 2002). On the other hand, ketamine is able to elevate glutamate levels in the extracellular compartment of the mediofrontal cortex, as shown by an in vivo microdialysis study (Moghaddam et al. 1997). Thus, one possibility is that BDNF levels are increased because of NMDA antagonist action of ketamine. Another option is that increased BDNF levels are the result of adaptive mechanisms to ketamine withdrawal. In fact, drug users were required to abstain from psychotropic drug use for at least 24 h prior to testing. Nonetheless, because of the short time of drug withdrawal and the fact that subjects with withdrawal symptoms were excluded from the study, it is reasonable to believe that altered BDNF levels are a consequence of chronic adaptation to ketamine use, rather than an effect of withdrawal syndrome.
Other studies have shown that non-competitive NMDA receptor antagonists are also able to elevate the concentration of extracellular dopamine (Adams and Moghaddam 1998; Bristow et al. 1993; Carboni et al. 1989; Imperato et al. 1990), and low-dose ketamine may increase dopamine turnover in the nucleus accumbens (Irifune et al. 1991, 1997). A possible link between the effect of dopamine stimulation and BDNF has already been evidenced. In rats, both increased (Meredith et al. 2002) and reduced (Angelucci et al. 2007a) BDNF expression in brain areas after exposure to amphetamine has been reported, while methamphetamine (Kim et al. 2005) and ecstasy (Angelucci et al. 2010) abusers are characterized by increased plasma or serum BDNF levels. Since BDNF supports the function of dopaminergic neurons, these findings may also support the idea that a ketamine-induced BDNF increase could be part of an adaptive response to changes in dopamine turnover.
Interestingly, an antidepressant action of ketamine has been recently described in humans and animal models. More intriguing, other evidences suggest that BDNF is involved in depression, namely the expression of BDNF is decreased in depressed patients (De Oliveira et al. 2009). In addition, chronic, but not acute, antidepressant treatment induces increasing of BDNF expression and BDNF immunoreactive fibres in the hippocampus of rodents (Nibuya et al. 1996; De Foubert et al. 2004). Therefore, the general consensus is that an increase in BDNF is necessary for antidepressant drugs to exert their action (Drzyzga et al. 2009). Clinical studies have shown that acute administration of ketamine (as well as other NMDA antagonists) ameliorates depressive symptoms in major depressed patients (Zarate et al. 2006; Berman et al. 2000). In line with these findings, ketamine induces anxiolytic- and antidepressant-like effects in rodent models of anxiety and depression (Kos et al. 2006; Yilmaz et al. 2002; Silvestre et al. 1997), an effect also associated with an increase in BDNF in the hippocampus (Garcia et al. 2008). Thus, it is possible that the described antidepressant action of ketamine in humans can be mediated by BDNF. Nevertheless, it is important to note that the majority of the above cited studies focused on the acute effect of ketamine, whereas little is known about the effects of long-term ketamine abuse.
A limitation to the interpretation of our data is that we measured the BDNF levels in serum and a direct correlation between central and peripheral neurotrophin levels has not yet been demonstrated. However, some studies reported that neurotrophins are able to cross the blood–brain barrier via a high-capacity saturable transport system (Kastin et al. 1999; Pan et al. 1998). Another limitation of this study is that the majority of ketamine users were also polydrug users. Unfortunately, ‘pure’ ketamine users are very rare and confounding factors caused by the concomitant use of other substances cannot be totally excluded. Nevertheless, our findings may be of interest since we enrolled subjects with prevalent use of ketamine in their lifetime.
In conclusion, this study has shown that chronic ketamine intake increases BDNF serum levels in humans. Whether this effect is a consequence of a direct neurotoxic insult of ketamine is still matter of debate, as well as the possible association with ketamine antidepressant action. Other studies are needed to elucidate the pharmacological and molecular mechanism by which ketamine, and/or other NMDA antagonists, may induce modification in the production and utilization of BDNF and alter normal brain function.
References
Adams B, Moghaddam B (1998) Corticolimbic dopamine neurotransmission is temporally dissociated from the cognitive and locomotor effects of phencyclidine. J Neurosci 18:5545–5554
Adler CM, Goldberg TE, Malhotra AK, Pickar D, Breier A (1998) Effects of ketamine on thought disorder, working memory, and semantic memory in healthy volunteers. Biol Psychiatry 43:811–816
Angelucci F, Gruber SH, El Khoury A, Tonali PA, Mathé AA (2007a) Chronic amphetamine treatment reduces NGF and BDNF in the rat brain. Eur Neuropsychopharmacol 17:756–762
Angelucci F, Ricci V, Pomponi M, Conte G, Mathé AA, Tonali P, Bria P (2007b) Chronic heroin and cocaine abuse is associated with decreased serum concentrations of the nerve growth factor and brain-derived neurotrophic factor. J Psychopharmacol 21:820–825
Angelucci F, Ricci V, Spalletta G, Pomponi M, Tonioni F, Caltagirone C, Bria P (2008) Reduced serum concentrations of nerve growth factor, but not brain-derived neurotrophic factor, in chronic cannabis abusers. Eur Neuropsychopharmacol 18:882–887
Angelucci F, Ricci V, Spalletta G, Caltagirone C, Mathé AA, Bria P (2009) Effects of psychostimulants on neurotrophins: implications for psychostimulant-induced neurotoxicity. Int Rev Neurobiol 88:1–24
Angelucci F, Ricci V, Martinotti G, Palladino I, Spalletta G, Caltagirone C, Bria P (2010) Ecstasy (MDMA)-addicted subjects show increased serum levels of brain-derived neurotrophic factor, independently from arise of drug-induced psychotic symptoms. Addict Biol 15(3):365–367
Anis NA, Berry SC, Burton NR, Lodge D (1983) The dissociative anaesthetics, ketamine and phencyclidine, selectively decrease excitation of central neurons by N-methyl-d-aspartate. Br J Pharmacol 83:179–185
Becker A, Grecksch G, Schwegler H, Roskoden T (2008) Expression of mRNA of neurotrophic factors and their receptors are significantly altered after subchronic ketamine treatment. Med Chem 4:256–263
Berman RM, Cappiello A, Anand A, Oren DA, Heninger GR, Charney DS, Krystal JH (2000) Antidepressant effects of ketamine in depressed patients. Biol Psychiatry 47:351–354
Bristow LJ, Hutson PH, Thorn L, Tricklebank MD (1993) The glycine/NMDA receptor antagonist, R-(+)-HA-966, blocks activation of the mesolimbic dopaminergic system induced by phencyclidine and dizocilpine (MK-801) in rodents. Br J Pharmacol 108:1156–1163
Carboni E, Imperato A, Perezzani L, Di Chiara G (1989) Amphetamine, cocaine, phencyclidine and nomifensine increase extracellular dopamine concentrations preferentially in the nucleus accumbens of freely moving rats. Neuroscience 28:653–661
Connor B, Dragunow M (1998) The role of neuronal growth factors in neurodegenerative disorders of the human brain. Brain Res Brain Res Rev 27:1–39
Curran HV, Morgan C (2000a) Acute and residual effects of ketamine on recreational users: evidence for persisting cognitive impairments, dissociative and psychotic symptoms. Addiction 95:575–590
Curran HV, Morgan C (2000b) Cognitive, dissociative and psychotogenic effects of ketamine in recreational users on the night of drug use and 3 days later. Addiction 95:575–590
De Foubert G, Carney SL, Robinson CS, Destexhe EJ, Tomlinson R, Hicks CA, Murray TK, Gaillard JP, Deville C, Xhenseval V, Thomas CE, O’Neill MJ, Zetterström TS (2004) Fluoxetine-induced change in rat brain expression of brain-derived neurotrophic factor varies depending on length of treatment. Neuroscience 128:597–604
De Oliveira GS, Ceresér KM, Fernandes BS, Kauer-Sant’Anna M, Fries GR, Stertz L, Aguiar B, Pfaffenseller B, Kapczinski F (2009) Decreased brain-derived neurotrophic factor in medicated and drug-free bipolar patients. J Psychiatr Res 43:1171–1174
Drzyzga ŁR, Marcinowska A, Obuchowicz E (2009) Antiapoptotic and neurotrophic effects of antidepressants: a review of clinical and experimental studies. Brain Res Bull 79:248–257
First MB, Spietzer RL, Gibbon M, William JBW (1997) Structured clinical interview for DSM-1V axis 1 disorders clinical version. American Psychiatric, Washington
Folstein MF, Folstein SE, McHugh PR (1975) Mini-mental state. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12:189–198
Garcia LS, Comim CM, Valvassori SS, Réus GZ, Barbosa LM, Andreazza AC, Stertz L, Fries GR, Gavioli EC, Kapczinski F, Quevedo J (2008) Acute administration of ketamine induces antidepressant-like effects in the forced swimming test and increases BDNF levels in the rat hippocampus. Prog Neuropsychopharmacol Biol Psychiatry 32:140–144
Ghoneim MM, Hinrichs JM, Mewaldt SP, Petersen RC (1985) Ketamine: behavioural effects of subanaesthetic doses. J Clin Psychopharmacol 5:70–77
Ha DH, Robertson RT, Roshanaei M, Weiss JH (1999) Enhanced survival and morphological features of basal forebrain cholinergic neurons in vitro: role of neurotrophins and other potential cortically derived cholinergic trophic factors. J Comp Neurol 406:156–170
Hamilton M (1959) The assessment of anxiety states by rating. Br J Med Psychol 32:50–55
Hamilton M (1960) A rating scale for depression. J Neurol Neurosurg Psychiatry 23:56–62
Hansen G, Jensen SB, Chandresh L, Hilden T (1988) The psychotropic effect of ketamine. J Psychoactive Drugs 20:419–425
Harborne GC, Watson FL, Healy DT, Groves L (1996) The effects of sub-anaesthetic doses of ketamine on memory, cognitive performance and subjective experience in healthy volunteers. J Psychopharmacol 10:134–140
Harris EW, Ganong AH, Cotman CW (1984) Long term potentiation in the hippocampus involves activation of N-methyl-d-aspartate receptors. Brain Res 323:132–137
Hyman C, Hofer M, Barde YA, Juhasz M, Yancopoulos GD, Squinto SP, Lindsay RM (1991) BDNF is a neurotrophic factor for dopaminergic neurons of the substantia nigra. Nature 350:230–232
Ibla JC, Hayashi H, Bajic D, Soriano SG (2009) Prolonged exposure to ketamine increases brain derived neurotrophic factor levels in developing rat brains. Curr Drug Saf 4:11–16
Imperato A, Scrocco MG, Bacchi S, Angelucci L (1990) NMDA receptors and in vivo dopamine release in the nucleus accumbens and caudatus. Eur J Pharmacol 187:555–556
Irifune M, Shimizu T, Nomoto M (1991) Ketamine-induced hyperlocomotion associated with alteration of presynaptic components of dopamine neurons in the nucleus accumbens of mice. Pharmacol Biochem Behav 40:399–407
Irifune M, Fukuda T, Nomoto M, Sato T, Kamata Y, Nishikawa T, Mietani W, Yokoyama K, Sugiyama K, Kawahara M (1997) Effects of ketamine on dopamine metabolism during anesthesia in discrete brain regions in mice: comparison with the effects during the recovery and subanesthetic phases. Brain Res 763:281–284
Kastin AJ, Pan W, Maness LM, Banks WA (1999) Peptides crossing the blood–brain barrier: some unusual observations. Brain Res 848:96–100
Kim DJ, Roh S, Kim Y, Yoon SJ, Lee HK, Han CS, Kim YK (2005) High concentrations of plasma brain-derived neurotrophic factor in methamphetamine users. Neurosci Lett 388:112–115
Kos T, Popik P, Pietraszek M, Schäfer D, Danysz W, Dravolina O, Blokhina E, Galankin T, Bespalov AY (2006) Effect of 5-HT3 receptor antagonist MDL 72222 on behaviors induced by ketamine in rats and mice. Eur Neuropsychopharmacol 16:297–310
Krystal JH, Karper LP, Seibyl JP, Freeman GK, Delaney R, Bremner JD, Heninger GR, Bowers MB, Charney DS (1994) Subanesthetic effects of the noncompetitive NMDA antagonist, ketamine, in humans. Psychotomimetic, perceptual, cognitive, and neuroendocrine responses. Arch Gen Psychiatry 51:199–214
Lad SP, Neet KE, Mufson EJ (2003) Nerve growth factor: structure, function and therapeutic implications for Alzheimer's disease. Curr Drug Targets CNS Neurol Disord 2:315–334
Lee J, Duan W, Mattson MP (2002) Evidence that brain-derived neurotrophic factor is required for basal neurogenesis and mediates, in part, the enhancement of neurogenesis by dietary restriction in the hippocampus of adult mice. J Neurochem 82:1367–1375
Malhotra AK, Pinals DA, Weingartner H, Sirocco K, Missar CD, Pickar D, Breier A (1996) NMDA receptor function and human cognition: the effects of ketamine in healthy subjects. Neuropsychopharmacology 14:301–307
Marini AM, Rabin SJ, Lipsky RH, Mocchetti I (1998) Activity-dependent release of brain-derived neurotrophic factor underlies the neuroprotective effect of N-methyl-D-aspartate. J Biol Chem 273:29394–29399
Meredith GE, Callen S, Scheuer DA (2002) Brain-derived neurotrophic factor expression is increased in the rat amygdala, piriform cortex and hypothalamus following repeated amphetamine administration. Brain Res 949:218–227
Minichiello L (2009) TrkB signalling pathways in LTP and learning. Nat Rev Neurosci 10:850–860
Moghaddam B, Adams B, Verma A, Daly D (1997) Activation of glutamatergic neurotransmission by ketamine: a novel step in the pathway from NMDA receptor blockade to dopaminergic and cognitive disruptions associated with the prefrontal cortex. J Neurosci 17:2921–2927
Muller D, Joly M, Lynch G (1988) Contributions of quisqualate and NMDA receptors to the induction and expression of long-term potentiation. Science 242:1694–1697
Newcomer JW, Farber NB, Jevtovic-Todorovic V, Selke G, Melson AK, Hershey T, Craft S, Olney JW (1999) Ketamine-induced NMDA receptor hypofunction as a model of memory impairment and psychosis. Neuropsychopharmacology 20:106–118
Nibuya M, Nestler EJ, Duman RS (1996) Chronic antidepressant administration increases the expression of cAMP response element binding protein (CREB) in rat hippocampus. J Neurosci 16:2365–2372
Pan W, Banks WA, Fasold MB, Bluth J, Kastin AJ (1998) Transport of brain-derived neurotrophic factor across the blood–brain barrier. Neuropharmacology 37:1553–1561
Silvestre JS, Nadal R, Pallares M, Ferré N (1997) Acute effects of ketamine in the holeboard, the elevated-plus maze, and the social interaction test in Wistar rats. Depress Anxiety 5:29–33
Solowij N, Hall W, Lee N (1992) Recreational MDMA use in Sydney: a profile of ‘Ecstasy’ users and their experience with the drug. Br J Addict 87:1161–1172
Thoenen H (1995) Neurotrophins and neuronal plasticity. Science 270:593–598
Verpelli C, Piccoli G, Zanchi A, Gardoni F, Huang K, Brambilla D, Di Luca M, Battaglioli E, Sala C (2010) Synaptic activity controls dendritic spine morphology by modulating eEF2-dependent BDNF synthesis. J Neurosci 30:5830–5842
Yilmaz A, Schulz D, Aksoy A, Canbeyli R (2002) Prolonged effect of an anesthetic dose of ketamine on behavioral despair. Pharmacol Biochem Behav 71:341–344
Zarate CA Jr, Singh JB, Carlson PJ, Brutsche NE, Ameli R, Luckenbaugh DA, Charney DS, Manji HK (2006) A randomized trial of an N-methyl-D-aspartate antagonist in treatment-resistant major depression. Arch Gen Psychiatry 63:856–864
Zhang DX, Levy WB (1992) Ketamine blocks the induction of LTP at the lateral entorhinal cortex–dentate gyrus synapses. Brain Res 593:124–127
Acknowledgements
This work was supported by the Italian Ministry of Health. Experiments comply with the current laws of the country in which they were performed
Conflict of interest
The authors declare no conflicting financial or other competing interests.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ricci, V., Martinotti, G., Gelfo, F. et al. Chronic ketamine use increases serum levels of brain-derived neurotrophic factor. Psychopharmacology 215, 143–148 (2011). https://doi.org/10.1007/s00213-010-2121-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-010-2121-3