Abstract
Rationale
The neurosteroids pregnenolone sulfate (PREGS), dehydroepiandrosterone sulfate (DHEAS) and allopregnanolone (3α,5α THPROG) have been implicated as powerful modulators of memory processes and sleep states in young and aged subjects with memory impairment. As these processes depend on the integrity of cholinergic systems, a specific effect of neurosteroids on these systems may account for their effects on sleep and memory.
Objective
To review the evidence for a specific and differential effect of neurosteroids on cholinergic systems.
Methods
We carried out keyword searches in “Medline” to identify articles concerning (1) the effects of neurosteroids on cholinergic systems, sleep and memory processes, and (2) changes in neurosteroid concentrations during aging. Few results are available for humans. Most data concerned rodents.
Results
Peripheral and central administrations of PREGS, DHEAS, and 3α,5α THPROG modulate the basal forebrain and brainstem projection cholinergic neurons but not striatal cholinergic interneurons. Local administration of neurosteroids to the basal forebrain and brainstem cholinergic neurons alters sleep and memory in rodents. There are a few conflicting reports concerning the effects of aging on neurosteroid concentrations in normal and pathological conditions.
Conclusions
The specific modulation of basal forebrain and brainstem cholinergic systems by neurosteroids may account for the effects of these compounds on sleep and memory processes. To improve our understanding of the role of neurosteroids in cholinergic systems during normal and pathological aging, we need to determine whether there is specific regionalization of neurosteroids, and we need to investigate the relationship between neurosteroid concentrations in cholinergic nuclei and age-related sleep and memory impairments.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Several studies have suggested that the neurosteroids pregnenolone sulfate (3β-hydroxy-5-pregnen-20-one-3 sulfate; PREGS), dehydroepiandrosterone sulfate (5-androstene-3β-ol-17-one sulfate; DHEAS) and allopregnanolone (3α,5α tetrahydroxyprogesterone; 3α,5α THPROG) may play a critical role in age-related neuropsychiatric disorders in humans and animals, and in the disruption of sleep and memory processes in particular (Vallée et al. 1997, 2001; Maurice 2001; Racchi et al. 2001; Weill-Engerer et al. 2002a; Mayo et al. 2003; Schumacher et al. 2003). There is little direct evidence of a pathophysiological relationship between neurosteroid concentrations in specific cerebral structures and age-related sleep and memory impairments (Vallée et al. 1997; Weill-Engerer et al. 2002b), but many studies have demonstrated that these neurosteroids affect sleep and memory processes in young subjects. Indeed, the peripheral or central administration of PREGS, DHEAS and 3α,5α THPROG induces robust changes in memory performances and sleep states (Flood et al. 1992; Frye 1995; Isaacson et al. 1995; Meziane et al. 1996; Lancel et al. 1997; Darnaudery et al. 1999a,b; Ladurelle et al. 2000; Damianisch et al. 2001; Matthews et al. 2002; Johansson et al. 2002; Turkmen et al. 2004). There are several lines of evidence suggesting that cholinergic systems may mediate these effects. Firstly, the integrity of cholinergic systems is critical for sleep and memory processes (Everitt and Robbins 1997), and these systems are known to degenerate during aging (Bartus et al. 1982; Perry et al. 1999; Sarter and Bruno 2004). Secondly, although little is known about the anatomic distribution of neurosteroid enzymes in discrete cerebral structures in adults, the key regulator of neurosteroid synthesis, the steroidogenic acute regulatory protein (StAR) (King et al. 2002; Sierra et al. 2003) and neurosteroid synthesis enzymes are produced in cholinergic systems (Rajkowski et al. 1997; Mellon et al. 2001). Thirdly, cholinergic neurons receive numerous γ-aminobutyric acid(GABA)ergic and glutamatergic modulatory afferences, and it is known that the neurosteroids PREGS, DHEAS and 3α,5α THPROG exert their pharmacological effects by modulating GABA receptors (GABAA) and glutamate receptors [-amino-3-hydroxy-5-methyl-4-isoxazole propionic acid (AMPA), kainate and N-methyl-d-aspartate (NMDA)].
In this review, we will consider anatomical and functional aspects of cholinergic systems and analyze the effects of administering PREGS, DHEAS and 3α,5α THPROG (mainly in rodents) on cholinergic neurotransmission. We will then describe how specific effects of neurosteroids on cholinergic systems may account for the modulation of sleep and memory processes. Finally, we will discuss the potential pathophysiological implications for age-related sleep and memory impairments and suggest future lines of research to confirm the existence of interactions between neurosteroids and cholinergic systems.
Cholinergic systems
Definitions
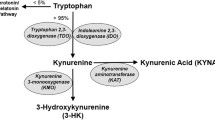
Two main neuronal systems have been identified—the basal forebrain cholinergic system (BFCS) and the brainstem cholinergic system (BCS)—based on the nomenclature of central cholinergic pathways proposed by Mesulam et al. 1983a,b for rats and primates (Mesulam et al. 1983a) (Fig. 1). The BFCS includes the medial septal nucleus (MS or Ch1), the vertical (vdB or Ch2) and horizontal (hdB or Ch3) limb nuclei of the diagonal band of Broca and the nucleus basalis magnocellularis (NBM or Ch4), the rodent equivalent of the nucleus basalis of Meynert in primates. The BCS, located in the brainstem and part of the reticular formation, encompasses the pedunculopontine tegmental (PPT) nucleus and the laterodorsal tegmental (LDT) nucleus, corresponding to the Ch5 and Ch6 groups described by Mesulam et al. 1983a,b. In addition to these cholinergic projection neurons, several interneurons have been identified in the striatum and nucleus accumbens, olfactory tubercle and islands of Calleja complex (Woolf and Butcher 1981; Houser et al. 1983; Satoh et al. 1983).
Schematic diagram of cholinergic systems in a rodent brain, adapted from Woolf (1991). The two major cholinergic systems composed of projection neurons are represented, the basal forebrain cholinergic system (BFCS) and the brainstem cholinergic system (BCS), together with the cholinergic interneurons of the striatum. The BFCS and the BCS encompass the Ch1-4 and Ch5–6 groups, respectively
Basal forebrain cholinergic system
Anatomical organization
In rat, BFCS cholinergic neurons form a constellation of neurons ranging from the anterior medial septal nucleus rostrally to the lateral hypothalamus caudally (Butcher et al. 1992; Oh et al. 1992). Most, if not all, of these cholinergic cells are projection neurons. The medial septum-vertical limb of the diagonal band of Broca (Ch1 and Ch2) innervates the hippocampus, dentate gyrus, entorhinal, perirhinal and retrosplenial cortex and interpeduncular nucleus (Woolf 1991). These neurons receive excitatory/inhibitory afferents from the hippocampus and enthorinal cortex (Dutar et al. 1985; Jakab and Leranth 2005). They are also innervated by afferents from the hypothalamus, ventral tegmental area, LDT, dorsal and median raphe and locus coeruleus (Woolf 1991). The horizontal limb of the diagonal band of Broca (Ch3) is responsible for cholinergic innervation of the olfactory bulb.
The nucleus basalis cholinergic projection (Ch4) is the single most substantial regulatory afferent system of the cerebral cortex in rat (Mesulam 1995). These cortical projections are topographically organized (Mesulam et al. 1983a; Rye et al. 1984; Saper and Chelimsky 1984; Saper 1984; Woolf et al. 1984). NBM neurons also send projections to the basolateral nucleus of the amygdala (Carlsen et al. 1985), the thalamus and the hypothalamus (Mesulam et al. 1983a). Cholinergic neurons of the NBM are interspersed with other non-cholinergic magnocellular corticopetal neurons, mainly GABAergic (Brashear et al. 1986; Zaborszky et al. 1986; Fisher et al. 1988). These GABAergic neurons are twice as numerous as the cholinergic cells (Gritti et al. 1993). Major afferences to the NBM include projections from the amygdala, nucleus accumbens, hypothalamus, ventral tegmentum, PPT, locus coeruleus and raphe nucleus. Terminals containing GABA (Perez et al. 1981), serotonin (Steinbusch and Nieuwenhuys 1981), glutamate (Davies et al. 1984), aspartate (Fuller et al. 1987) and substance P (Haber and Elde 1981) have been described among these afferences.
Functional role
The functional role of the BFCS has been extensively investigated over the last 20 years because this system is profoundly modified in neurodegenerative diseases classically associated with cognitive and sleep disorders (for review, see Everitt and Robbins 1997; Perry et al. 1999). As the main projection of medial septal neurons is the hippocampus, we would expect the functions of these neurons to be closely related to those of the hippocampus (Everitt and Robbins 1997). Hippocampal lesions are known to induce spatial learning and memory defects, and excitotoxic or electrolytic lesions of the medial septum have been reported to induce severe deficits in spatial memory tasks in rats (Hagan et al. 1988; Marston et al. 1993; Kelsey and Vargas 1993). Indeed, the cholinergic projection from the medial septum to the hippocampus may be involved in short-term memory, as suggested by reported deficits in contextual stimulus trace conditioning (McAlonan et al. 1995). Discrete excitotoxic lesions of the vertical limb of the diagonal band of Broca have been reported to lead to small but significant cholinergic depletions in the cingulate cortex and to impair the delayed retention of conditional discrimination performance in rats (Muir et al. 1996). Many experiments on excitotoxic/electrolytic lesions in rodents carried out from the 1980s onwards revealed that the NBM was involved in the regulation of cognitive processes, including attention, learning and memory, in particular, and in the regulation of sleep states (for review, see Everitt and Robbins 1997; Wenk 1997).
The precise role of cholinergic neurons remains a matter of debate. Cholinergic neurons are intermingled with a significant population of GABAergic neurons, and the lack of a selective toxin targeting cholinergic neurons was a recurrent problem in studies. Experiments involving the use of a specific cholinergic toxin (192 immunoglobulin G (IgG)–saporin) for lesioning basal forebrain cholinergic neurons have suggested that even if cholinergic neurons are involved in some memory processes, they seem to play a more important role in attentional processes (Muir et al. 1992, 1995; Berger-Sweeney et al. 1994; Torres et al. 1994; Baxter et al. 1995; Sarter and Bruno 1997). These results suggest that cholinergic projections from the BFCS (MS, vdB and NBM) are primarily involved in the modulation of attentional and memory processes.
The NBM may also be seen as a ventral extrathalamic relay from the brainstem reticular activating system to the cerebral cortex for the modulation of sleep/wake states (Shute and Lewis 1963; Krnjevic and Silver 1965; Moruzzi and Magoun 1995). Briefly, sleep/wake states include (1) wakefulness, characterized by a low-amplitude desynchronized electroencephalogram (EEG) and high muscular tone; (2) non-rapid eye movement (non-REM) sleep, characterized by a high-amplitude synchronized EEG mainly in the delta (0–4 Hz) and spindle (12–15 Hz) bands; and (3) REM sleep, characterized by a low-amplitude desynchronized EEG without muscular tone. More acetylcholine (ACh) is released in the neocortex during waking and REM sleep than during non-REM sleep (Phillis 1968; Jasper and Tessier 1971). Consistent with this finding, the discharge rates of NBM neurons have been shown to be maximal during waking and REM sleep in cats (Detari et al. 1984), and the basal forebrain has been shown to be deactivated during non-REM sleep in humans (Maquet 2000). Furthermore, lesioning of the NBM abolishes both REM and non-REM sleep (Szymusiak and McGinty 1986) and alters EEG synchronization (Buzsaki et al. 1988; Riekkinen et al. 1991). The state-dependent pattern of activity of NBM neurons may be partly regulated by changes in GABA-mediated inhibition. Indeed, cholinergic NBM neurons receive substantial GABAergic inputs, including local interneurons (Zaborszky et al. 1986; Ingham et al. 1988), and the infusion of GABA agonists or antagonists into the NBM alters the sleep-/wakefulness-related pattern of discharge of these neurons (Szymusiak et al. 2000). Interestingly, some authors have suggested that much of the variation in discharge of NBM neurons during waking and sleep may reflect changes in the activity of brainstem afferents (Szymusiak et al. 2000).
The BFCS therefore (1) modulates sleep/wake states, favoring arousal, via its projections to the neocortex and (2) enhances memory consolidation during wakefulness and/or sleep via projections to the amygdala and hippocampus.
Brainstem cholinergic system
Anatomical organization
The BCS comprises mostly large cholinergic neurons and, as for the cholinergic groups of the basal forebrain, brainstem cholinergic neurons form an integral part of the BCS (Armstrong et al. 1983; Rye et al. 1987; Jones 1990; Steininger et al. 1997) and are intermingled with a variety of other neurons such as GABAergic (Ford et al. 1995; Bevan and Bolam 1995; Torterolo et al. 2001) and glutamatergic neurons (Clements and Grant 1990; Charara et al. 1996). The BCS receives numerous projections from the surrounding area, including the ventral tegmental area, substantia nigra, raphe nucleus and locus coeruleus, and from other distal structures such as the hypothalamus, subthalamic nucleus and amygdala (Rye et al. 1987; Steininger et al. 1997). The main ascending projections from the BCS are the thalamic nuclei, basal forebrain, and brainstem nuclei (ventral tegmental area, raphe nucleus and locus coeruleus) (Fig. 1; Rye et al. 1987; Steininger et al. 1997). There are also some descending projections to the deep cerebellar nuclei, medioventral medulla and pontomedullary reticular nuclei (Fig. 1). BCS neurons are regulated primarily by serotonergic, noradrenergic, GABAergic and glutamatergic inputs originating from the pontomesen cephalic reticular formation and the PPT itself (Steckler et al. 1994; Rye 1997). These cholinergic neurons are also regulated by the autocrine/paracrine release of nitric oxide (NO) (Datta et al. 1997; Leonard and Lydic 1997).
Functional role
Several studies have demonstrated that the electrical activity of BCS neurons depends on sleep–wake state (Saito et al. 1977; el Mansari et al. 1989; Steriade et al. 1990; Kayama et al. 1992; Datta and Siwek 2002). It has been shown that the BCS contains at least two classes of neurons in animals: the REM-ON neurons, which display preferential discharge activity during REM sleep, and the wake/REM-ON neurons, which show preferential discharge activity during wakefulness and REM sleep. Wake/REM-ON neuronal activity increases the release of ACh into the pons and thalamus, leading to the electroencephalographic desynchronization seen in the wake and REM sleep states (Dingledine and Kelly 1977; Steriade et al. 1990; Datta 1997; Datta and Siwek 1997). As some BCS neurons are also strictly involved in the initiation of REM sleep, the BCS is now considered to be a key structure in the control of REM–nonREM sleep transitions (Hobson and Pace-Schott 2002; Pace-Schott and Hobson 2002).
Although the role of the BCS in sleep regulation has been extensively investigated, the role of this system in cognitive processes, and particularly in memory, has received little attention. However, the data reported suggest that the BCS may be involved in memory processes. In rodents, excitotoxic/electrolytic lesions of the BCS have been shown to impair contextual memory acquisition in numerous tasks (Fujimoto et al. 1989, 1992; Dellu et al. 1991; Satorra-Marin et al. 2001; Keating et al. 2002; Mitchell et al. 2002; Taylor et al. 2004). However, it is impossible to conclude that cholinergic neurons of the BCS are entirely responsible for these memory effects due to the lack of specific cholinergic-targeted toxins for the induction of lesions in the BCS.
Sleep and memory processes may be seen as independent functions, but recent studies suggest that these two functions may be linked, with the BCS underlying both. Indeed, the cholinergic activation of phasic pontine-wave generator cells in the brainstem improves memory consolidation and prevents REM sleep-deprivation-induced memory impairment in the active avoidance task (Mavanji and Datta 2003; Datta et al. 2004), suggesting that the BCS may play a key role in sleep-dependent memory consolidation.
Modulation of cholinergic transmission by PREGS, DHEAS and THPROG
Septo-hippocampal projection neurons
Several studies based on microdialysis coupled with high-performance liquid chromatography (HPLC) have shown that neurosteroids modulate the release of ACh in freely moving rats. The intraperitoneal (i.p.) administration of various doses of DHEAS (25–250 μmol/kg) increases ACh release in the hippocampus (Rhodes et al. 1996). The highest dose was found to increase ACh release by a factor of more than 4 with respect to treatment with saline. Similarly, the intracerebroventricular (i.c.v.) administration (12–192 nmol/5 μl) of PREGS induces a dose-dependent increase in ACh release into the hippocampus (Vallée et al. 1997; Darnaudery et al. 2000). The administration of 12 or 48 nmol of PREGS induces a transient (20 min) increase in the release of ACh, with a maximum around 120% above baseline. The administration of 96- and 192-nmol doses induced a longer-lasting (80 min) increase that peaked around 300% above baseline. This DHEAS-/PREGS-induced hippocampal ACh release was also observed indirectly, following daily i.p. administration of the non-steroidal steroid sulfatase inhibitor (p-O-sulfamoyl)-N-tetradecanoyl tyramine (DU-14) for 15 days (Rhodes et al. 1997), at a dose sufficient to increase plasma sulfated steroid concentrations by up to 88%. Consistent with these results, local infusion of PREGS (12 pmol/0.5 μl) into the MS induces a transient (30 min) 50% increase in ACh release in the hippocampus over baseline levels (Darnaudery et al. 2002). This result, obtained following local infusion into the MS, is similar to that obtained after i.c.v. administration of 12 and 48 nmol of PREGS, suggesting that the PREGS-induced release of ACh in the hippocampus depends primarily on a specific effect on the MS (Fig. 2). In contrast to the increase in ACh release observed after the administration of DHEAS and PREGS, the i.c.v. administration of 3α,5α THPROG (15–45 nmol/5 μl) decreases basal ACh release in the hippocampus in a dose-dependent manner (Dazzi et al. 1996). Doses of 30 and 45 nmol decrease ACh release by 20 and 55%, respectively, with respect to baseline (Fig. 4a). At a dose of 30 nmol, 3α,5α THPROG completely prevented the increase in ACh release induced by footshock stress, suggesting that the neurosteroid modulation of cholinergic systems could be of physiological importance. Thus, the i.p. or i.c.v. infusion of neurosteroids can modulate hippocampal ACh release, probably through a specific effect on MS cholinergic neurons. However, the regional specificity of neurosteroids remains to be clearly demonstrated using control infusions in other afferent structures to the hippocampus and the hippocampus itself. These results also highlight the opposite effects of DHEAS/PREGS and 3α,5α THPROG on ACh release in the hippocampus (Fig. 4a).
Effects of intracerebroventricular (icv; 48 nmol) and intra-medial septum (intra-MS; 12 pmol) PREGS infusions on the release of acetylcholine in the hippocampus, as assessed by microdialysis coupled to HPLC in freely moving rats. Note that the enhancement of cholinergic release in the hippocampus observed after icv infusion is reproduced following local infusion into the MS. Data represent the mean expressed as fold changes vs baseline. Adapted from Vallée et al. (1997) and Darnaudery et al. (2002)
Basalo-cortical and basalo-amygdalar projection neurons
Most of the cholinergic sources of the frontal cortex and amygdala come from the BFCS and the NBM. The release of ACh in the frontal cortex induced by i.c.v. administration of PREGS (0, 12, 48, 96 and 192 nmol/5 μl) was investigated by Darnaudery et al. (1998) using intracerebral microdialysis in freely moving rats. Extracellular ACh levels in the cortex were found to increase in a dose-dependent manner. The highest doses (96 and 192 nmol) tripled ACh release, the intermediate dose of 48 nmol doubled ACh release, and 12 nmol PREGS had no effect on extracellular levels of ACh. The increase in cortical ACh concentration was maximal 30 min after administration for all active doses. These data suggest that the cholinergic projections of the NBM require higher concentrations of PREGS (48 nmol) than the cholinergic projections of the MS (12 nmol) to increase ACh release in the corresponding terminals. Pallares et al. (1998) confirmed the effect of PREGS on the cholinergic projection neurons of the NBM (Fig. 3). They showed that the infusion of PREGS (12 pmol/0.5 μl) directly into the NBM induces a long-lasting release (130 min) of ACh in the frontal cortex and amygdala. In contrast, i.c.v. administrations (30–45 nmol/5 μl) of 3α,5α THPROG decrease ACh release in the frontal cortex of rats (Dazzi et al. 1996) (Fig. 4b). Thus, as for septo-hippocampal projection neurons, PREGS and 3α,5α THPROG act in opposite manners on basalo-cortical and basalo-amygdalar projection neurons, suggesting that basal cholinergic release may be controlled by a balance between these two steroids. Similarly, as for septo-hippocampal projection neurons, the regional specificity of neurosteroids remains to be clearly demonstrated using control infusions in other afferent structures to the cortex and amygdala.
Effects of intracerebroventricular (icv; 48 nmol) and intra-nucleus basalis magnocellular (intra-NBM; 12 pmol) PREGS infusions on the release of acetylcholine in the frontal cortex, as assessed by microdialysis coupled to HPLC in freely moving rats. Note that the enhancement of cholinergic release in the frontal cortex observed after icv infusion is reproduced following local infusion into the NBM. Data represent the mean expressed as fold changes vs baseline. Adapted from Darnaudery et al. (1998) and Pallares et al. (1998)
Summary of the changes in cholinergic transmission observed following icv infusions of PREGS and THPROG, as assessed by microdialysis coupled to HPLC in freely moving rats. Note that PREGS (black) and THPROG (gray) exert opposite effects on the release of ACh in the hippocampus (a) and frontal cortex (b) but have no effect on striatal cholinergic release (c). Data represent the mean expressed as fold changes vs baseline against time after injection. Adapted from Dazzi et al. (1996), Vallée et al. (1997) and Darnaudery et al. (1998)
Striatal interneurons
Cholinergic interneurons of the striatum account for only 1–3% of all neurons in the striatum, but their extensive axonal/dendritic arborization in the striatum is critical for the integration of information in the striatum. Neurosteroids seem to have no effect on striatal cholinergic interneurons in rat. Indeed, the i.c.v. administration of PREGS at the doses (0, 12, 48, 96 and 192 nmol/5 μl) active in other cholinergic systems has absolutely no effect on striatal ACh release as measured by microdialysis in freely moving rats (Darnaudery et al. 1998) (Fig. 4c). Similarly, i.c.v. administration (15–45 nmol/5 μl) of 3α,5α THPROG (Dazzi et al. 1996) has no effect on striatal cholinergic transmission (Fig. 4c). Thus, either striatal cholinergic interneurons require higher concentrations of neurosteroids for changes in ACh release or neurosteroids are not involved in the physiological regulation of cholinergic release in the striatum.
The results described above demonstrate that neurosteroids have a strong influence on cholinergic transmission. The modulation of this transmission is specific to cholinergic projections (MS, NBM and PPT) because neurosteroids have no effect on striatal cholinergic interneurons. The differential effects of neurosteroids on the BFCS, BCS and on striatal cholinergic systems may result from differences in the composition of GABAA receptor subunits in these systems, as the effects of neurosteroids on GABAA receptors depend on subunit composition. In particular, the presence of the δ subunit has been shown to increase the sensitivity of GABAA receptors to neurosteroids (Lambert et al. 2003). In line with this, neurons in the BFCS and BCS produce mostly the α1, β2, γ1, γ3, ɛ, δ and α3, γ3, δ subunits, respectively, whereas those in the striatum produce mostly the α3, α5, β1 and β2 subunits, but these are devoid of δ subunits (Moragues et al. 2000, 2002; Pirker et al. 2000). For a full evaluation of the effects of neurosteroids on cholinergic systems, further studies are required to demonstrate the effects of neurosteroids on cholinergic transmission from the BCS.
Modulation of cholinergic-related functions by PREGS, DHEAS and THPROG
Memory processes
Many studies have investigated the pharmacological effects of peripheral and central administrations of PREGS, DHEAS and 3α,5α THPROG on memory processes in rats. PREGS and DHEAS have been shown to improve memory, whereas 3α,5α THPROG has been shown to impair memory. These effects have been observed for several memory-related tasks such as the active and passive avoidance task (Flood et al. 1992; Isaacson et al. 1995), appetitively reinforced go–no go visual discrimination task (Meziane et al. 1996), the Y-maze (Ladurelle et al. 2000), a spatial version of the water-maze task (Frye and Lacey 1999; Matthews et al. 2002; Johansson et al. 2002; Turkmen et al. 2004) and a spatial recognition task (Darnaudery et al. 1999b, 2000). The memory-enhancing effect of i.c.v. administration of PREGS is correlated with a parallel increase in ACh release in the hippocampus (Darnaudery et al. 2000), suggesting that PREGS acts on the BFCS. These findings were confirmed after local infusions of PREGS into the BFCS. Local infusion into the MS (12 pmol/0.5 μl) and the NBM (12 pmol/0.5 μl) improves spatial memory and increases ACh release in the corresponding projection structures: hippocampus, amygdala and frontal cortex (Pallares et al. 1998; Darnaudery et al. 2002). Consistent with the opposite actions of PREGS and 3α,5α THPROG on cholinergic transmission from the BFCS, these two neurosteroids have opposite effects on spatial memory performance. Mayo et al. (1993) found that PREGS (12 pmol/0.5 μl) infusion in the NBM enhanced spatial performance in the Y-maze recognition task, whereas the infusion of 3α,5α THPROG (0.6–6 pmol/0.5 μl) in the NBM impaired performance in this task (Fig. 5). PREGS and DHEAS have been shown to enhance memory in physiological conditions in young subjects, and PREGS and DHEAS have been shown to reverse memory impairments in various rodent models of amnesia (Mathis et al. 1994, 1996; Meziane et al. 1996; Urani et al. 1998; Zou et al. 2000), suggesting that these neurosteroids may be of therapeutic value for the memory impairments observed during aging.
Memory-enhancing and memory-impairing effects in the Y-maze after local infusion of PREGS and THPROG into the BMN. Data are expressed as variation of the recognition index as a percentage of the value for control animals (maximum SEM of control animals indicated by the striped area). Adapted from Mayo et al. (1993)
Sleep states
Few studies have investigated the effects of peripheral administration of PREGS, DHEAS and 3α,5α THPROG on sleep/wake states (Mendelson et al. 1987; Lancel et al. 1997; Darnaudery et al. 1999a; Schiffelholz et al. 2000). The peripheral administration of 3α,5α THPROG leads to robust changes in sleep architecture and cortical activities during sleep in rodents. The i.p. administration of 3α,5α THPROG (24–48 μmol/kg) decreases non-REM sleep latency and EEG power in the delta band (0–4Hz), whereas it increases EEG power in the spindles band (12–15Hz). The peripheral administration of 3α,5α THPROG therefore tends to have a benzodiazepine-like effect, increasing the tendency to fall asleep and promoting non-REM sleep at the expense of REM sleep, which may be transiently abolished at the highest doses (Mendelson et al. 1987; Lancel et al. 1997; Schiffelholz et al. 2000; Damianisch et al. 2001). In contrast, the i.p. administration of PREGS (113 μmol/kg) increases the amount of REM sleep without affecting non-REM sleep in rats (Darnaudery et al. 1999a; Schiffelholz et al. 2000). The opposite effects of PREGS and 3α,5α THPROG on REM sleep are consistent with those obtained following local infusions into the NBM. The infusion of PREGS (12 pmol/0.5 μl) in this structure induces a long-lasting (8 h) increase (+30%) in the amount of REM sleep, whereas the infusion of 3α,5α THPROG (6 pmol/0.5 μl) induces a long-lasting decrease (−25%) in the amount of REM sleep (Darnaudery et al. 1999b).
We have also shown that PREGS administration in the PPT affects sleep–wakefulness states in a dose-dependent manner (Darbra et al. 2004). The infusion in the PPT of a low concentration (12 pmol/0.5 μl) of PREGS, similar to that known to induce a slight increase in REM sleep following infusion into the NBM, produces a robust, transient (90 min) increase in the amount of REM sleep (+200%), with no change in non-REM sleep and wakefulness, suggesting that PPT cholinergic neurons are a primary target of PREGS. Moreover, increasing the dose of PREGS (24–48 pmol/0.5 μl) increases REM sleep and non-REM sleep, and also increases delta power and decreases theta power during wakefulness. Thus, depending on the dose used, PREGS can promote REM sleep alone or the global propensity to fall asleep, impairing the quality of wakefulness. The regulation and the functional role of neurosteroids appear to be radically different in the NBM and the PPT, and the effects of 3α,5α THPROG on these two systems differ: 3α,5α THPROG infusion in the NBM decreases the amount of REM sleep, whereas the same infusion in the PPT induces no change (Fig. 6).
Summary of REM sleep results obtained after local infusions of PREGS and THPROG into the BFCS (BMN) and BCS (PPT). REM sleep is assessed by chronic sleep recording and expressed as a percentage of the control in each experiment (maximum SEM of control animals indicated by the striped area). Note that in the BMN, the two neurosteroids have opposite effects, whereas in the PPT, only PREGS has an effect, inducing a robust increase in REM sleep. Adapted from Darnaudery et al. (1999a,b) and Darbra et al. (2004)
The data described here provide strong evidence for the differential regulation of the BFCS and BCS by neurosteroids. The effects of PREGS and 3α,5α THPROG on these two systems suggest that (1) cholinergic projection neurons of the NBM are controlled by a physiological balance between PREGS and 3α,5α THPROG because in the NBM, these two neurosteroids affect sleep states, memory and cholinergic transmission in opposite manners; (2) cholinergic projection neurons of the PPT are controlled by strong 3α,5α THPROG tonic inhibition that is reversed by exogenous PREGS because 3α,5α THPROG administration has no effect on sleep state. Given that REM sleep is controlled by the BCS, it could be suggested that the infusion of PREGS (but not of 3α,5α THPROG) into the BCS should enhance cholinergic transmission in the thalamus and pons. Confirmation of the hypothesized local and differential actions of these neurosteroids in the BFCS and BCS will require measurements of the concentration of neurosteroids in these regions and analysis of the various mechanisms of neurosteroidogenesis regulation in these two systems.
Pathophysiological implications for age-related sleep and memory disorders
Neurosteroid–cholinergic system interactions are thought to be involved in age-related sleep and memory disorders primarily because a marked change in cholinergic systems is observed during aging (Muir 1997; Mesulam 1998). Such changes take place in both the BFCS and BCS, in which decreases in numbers of ACh neurons and in ACh transmission have been described in aged rodents, primates and humans (Fischer et al. 1992; Kobayashi et al. 1994; Lolova et al. 1996, 1997; Martinez-Serrano and Bjorklund 1998; Ransmayr et al. 2000) and in demented patients (Perry et al. 1995; Arendt et al. 1995a,b, 1997; Herholz et al. 2004). Age-related changes in cholinergic-related functions have been also demonstrated. Although human aging is associated with numerous neuropsychiatric changes that affect daily life, a hallmark of these changes is the higher prevalence of memory and sleep disorders in the elderly population. The dysfunctions of episodic and working memories (Grady and Craik 2000; Nyberg et al. 2002) and the decrease in amplitude of the sleep–wake circadian rhythm associated with a fragmentation of non-REM sleep have critical health outcomes (Rosenberg et al. 1979; Ingram et al. 1982; Stone 1989; Myers and Badia 1995; Van Someren 2000; Dagan 2002; Mignot et al. 2002). For instance, a lack of restful sleep at night results in excessive daytime sleepiness, attention and memory problems, depressed mood, falls, and poor quality of life (Young 2004; Foley et al. 2004). The mechanisms underlying age-related sleep and memory disorders are poorly understood, but numerous correlations have been demonstrated between cholinergic dysfunctions and memory impairments in aged subjects. Published results suggest that changes in neurosteroid concentrations in the BFCS and BCS may mediate these dysfunctions.
Extensive but controversial studies have shown that plasma steroid levels change with age and may be associated with memory deficits in aged humans and demented patients (see for review Vallée et al. 2001, 2004). However, there have been few experimental reports of changes in brain neurosteroids during aging or relationships between brain neurosteroid levels and age-related dysfunctions. Overall decreases in PREGS and 3α,5α THPROG levels in the hippocampus and cerebral cortex, respectively, have been reported in aged rats, with young rats used as the reference group (Vallée et al. 1997; Bernardi et al. 1998), whereas 3α,5α THPROG levels in the hypothalamus have been reported to increase with age (Bernardi et al. 1998). However, Barbaccia et al. (1998) reported no change in 3α,5α THPROG concentration in the cortex during aging (Barbaccia et al. 1998). Interestingly, hippocampal PREGS concentrations have been shown to be negatively correlated with memory impairments in aged rats (Vallée et al. 1997), strongly suggesting that hippocampal PREGS is important for memory processing in aged animals. In humans, changes in brain neurosteroid concentrations have been described in demented patients [Alzheimer’s disease (AD)], with age-matched controls used as the reference group (Weill-Engerer et al. 2002a; Kim et al. 2003; Brown et al. 2003). Weill-Engerer et al. (2002a,b) reported decreases in the concentrations of PREGS and DHEAS in the striatum, hypothalamus (DHEAS only) and cerebellum of demented patients, consistent with the decrease in cerebrospinal fluid (CSF) DHEAS levels observed in patients with AD and vascular dementia (Kim et al. 2003). Moreover, DHEA levels have been shown to be high in the hippocampus, hypothalamus, frontal cortex and CSF in AD patients (Brown et al. 2003). Given the small number and conflicting nature of the results obtained to date, further studies are required to determine the involvement of neurosteroids in age-related sleep and memory dysfunctions in normal aging and pathological aging, as in neurodegenerative disorders.
Conclusions
This review deals with the modulation of cholinergic transmission and cholinergic-related function by neurosteroids. We suggest that neurosteroids play a critical role in sleep and memory processes by selectively modulating the BFCS and BCS, and that the dysregulation of neurosteroid synthesis in these regions may play a key role in sleep and memory disorders during aging. Improvements in our understanding of the role of neurosteroids in these processes in young subjects and in pathological conditions during aging will require a demonstration that neurosteroidogenesis is particularly important in cholinergic systems. Further studies are required (1) to demonstrate the specific cerebral regionalization, particularly in cholinergic structures, of neurosteroids and their associated proteins (steroidogenic enzymes, StaR), (2) to determine whether this cerebral regionalization changes during the subject’s lifetime and (3) to study the relationship between neurosteroid concentrations in cholinergic systems and the sleep/memory impairments observed in some subjects during aging.
References
Arendt T, Bruckner MK, Bigl V, Marcova L (1995a) Dendritic reorganisation in the basal forebrain under degenerative conditions and its defects in Alzheimer’s disease. II. Ageing, Korsakoff’s disease, Parkinson’s disease, and Alzheimer’s disease. J Comp Neurol 351:189–222
Arendt T, Bruckner MK, Bigl V, Marcova L (1995b) Dendritic reorganisation in the basal forebrain under degenerative conditions and its defects in Alzheimer’s disease. III. The basal forebrain compared with other subcortical areas. J Comp Neurol 351:223–246
Arendt T, Schindler C, Bruckner MK, Eschrich K, Bigl V, Zedlick D, Marcova L (1997) Plastic neuronal remodeling is impaired in patients with Alzheimer’s disease carrying apolipoprotein epsilon 4 allele. J Neurosci 17:516–529
Armstrong DM, Saper CB, Levey AI, Wainer BH, Terry RD (1983) Distribution of cholinergic neurons in rat brain: demonstrated by the immunocytochemical localization of choline acetyltransferase. J Comp Neurol 216:53–68
Barbaccia ML, Concas A, Serra M, Biggio G (1998) Stress and neurosteroids in adult and aged rats. Exp Gerontol 33:697–712
Bartus RT, Dean RL III, Beer B, Lippa AS (1982) The cholinergic hypothesis of geriatric memory dysfunction. Science 217:408–414
Baxter MG, Bucci DJ, Gorman LK, Wiley RG, Gallagher M (1995) Selective immunotoxic lesions of basal forebrain cholinergic cells: effects on learning and memory in rats. Behav Neurosci 109:714–722
Berger-Sweeney J, Heckers S, Mesulam MM, Wiley RG, Lappi DA, Sharma M (1994) Differential effects on spatial navigation of immunotoxin-induced cholinergic lesions of the medial septal area and nucleus basalis magnocellularis. J Neurosci 14:4507–4519
Bernardi F, Salvestroni C, Casarosa E, Nappi RE, Lanzone A, Luisi S, Purdy RH, Petraglia F, Genazzani AR (1998) Aging is associated with changes in allopregnanolone concentrations in brain, endocrine glands and serum in male rats. Eur J Endocrinol 138:316–321
Bevan MD, Bolam JP (1995) Cholinergic, GABAergic, and glutamate-enriched inputs from the mesopontine tegmentum to the subthalamic nucleus in the rat. J Neurosci 15:7105–7120
Brashear HR, Zaborszky L, Heimer L (1986) Distribution of GABAergic and cholinergic neurons in the rat diagonal band. Neuroscience 17:439–451
Brown RC, Han Z, Cascio C, Papadopoulos V (2003) Oxidative stress-mediated DHEA formation in Alzheimer’s disease pathology. Neurobiol Aging 24:57–65
Butcher LL, Oh JD, Woolf NJ, Edwards RH, Roghani A (1992) Organization of central cholinergic neurons revealed by combined in situ hybridization histochemistry and choline-O-acetyltransferase immunocytochemistry. Neurochem Int 21:429–445
Buzsaki G, Bickford RG, Ponomareff G, Thal LJ, Mandel R, Gage FH (1988) Nucleus basalis and thalamic control of neocortical activity in the freely moving rat. J Neurosci 8:4007–4026
Carlsen J, Zaborszky L, Heimer L (1985) Cholinergic projections from the basal forebrain to the basolateral amygdaloid complex: a combined retrograde fluorescent and immunohistochemical study. J Comp Neurol 234:155–167
Charara A, Smith Y, Parent A (1996) Glutamatergic inputs from the pedunculopontine nucleus to midbrain dopaminergic neurons in primates: Phaseolus vulgaris-leucoagglutinin anterograde labeling combined with postembedding glutamate and GABA immunohistochemistry. J Comp Neurol 364:254–266
Clements JR, Grant S (1990) Glutamate-like immunoreactivity in neurons of the laterodorsal tegmental and pedunculopontine nuclei in the rat. Neurosci Lett 120:70–73
Dagan Y (2002) Circadian rhythm sleep disorders (CRSD). Sleep Med Rev 6:45–54
Damianisch K, Rupprecht R, Lancel M (2001) The influence of subchronic administration of the neurosteroid allopregnanolone on sleep in the rat. Neuropsychopharmacology 25:576–584
Darbra S, George O, Bouyer JJ, Piazza PV, Le Moal M, Mayo W (2004) Sleep–wake states and cortical synchronization control by pregnenolone sulfate into the pedunculopontine nucleus. J Neurosci Res 76:742–747
Darnaudery M, Koehl M, Pallares M, Le Moal M, Mayo W (1998) The neurosteroid pregnenolone sulfate increases cortical acetylcholine release: a microdialysis study in freely moving rats. J Neurochem 71:2018–2022
Darnaudery M, Bouyer JJ, Pallares M, Le Moal M, Mayo W (1999a) The promnesic neurosteroid pregnenolone sulfate increases paradoxical sleep in rats. Brain Res 818:492–498
Darnaudery M, Pallares M, Bouyer JJ, Le Moal M, Mayo W (1999b) Infusion of neurosteroids into the rat nucleus basalis affects paradoxical sleep in accordance with their memory modulating properties. Neuroscience 92:583–588
Darnaudery M, Koehl M, Piazza PV, Le Moal M, Mayo W (2000) Pregnenolone sulfate increases hippocampal acetylcholine release and spatial recognition. Brain Res 852:173–179
Darnaudery M, Pallares M, Piazza PV, Le Moal M, Mayo W (2002) The neurosteroid pregnenolone sulfate infused into the medial septum nucleus increases hippocampal acetylcholine and spatial memory in rats. Brain Res 951:237–242
Datta S (1997) Cellular basis of pontine ponto-geniculo-occipital wave generation and modulation. Cell Mol Neurobiol 17:341–365
Datta S, Siwek DF (1997) Excitation of the brain stem pedunculopontine tegmentum cholinergic cells induces wakefulness and REM sleep. J Neurophysiol 77:2975–2988
Datta S, Siwek DF (2002) Single cell activity patterns of pedunculopontine tegmentum neurons across the sleep–wake cycle in the freely moving rats. J Neurosci Res 70:611–621
Datta S, Patterson EH, Siwek DF (1997) Endogenous and exogenous nitric oxide in the pedunculopontine tegmentum induces sleep. Synapse 27:69–78
Datta S, Mavanji V, Ulloor J, Patterson EH (2004) Activation of phasic pontine-wave generator prevents rapid eye movement sleep deprivation-induced learning impairment in the rat: a mechanism for sleep-dependent plasticity. J Neurosci 24:1416–1427
Davies SW, McBean GJ, Roberts PJ (1984) A glutamatergic innervation of the nucleus basalis/substantia innominata. Neurosci Lett 45:105–110
Dazzi L, Sanna A, Cagetti E, Concas A, Biggio G (1996) Inhibition by the neurosteroid allopregnanolone of basal and stress-induced acetylcholine release in the brain of freely moving rats. Brain Res 710:275–280
Dellu F, Mayo W, Cherkaoui J, Le Moal M, Simon H (1991) Learning disturbances following excitotoxic lesion of cholinergic pedunculo-pontine nucleus in the rat. Brain Res 544:126–132
Detari L, Juhasz G, Kukorelli T (1984) Firing properties of cat basal forebrain neurones during sleep–wakefulness cycle. Electroencephalogr Clin Neurophysiol 58:362–368
Dingledine R, Kelly JS (1977) Brain stem stimulation and the acetylcholine-evoked inhibition of neurones in the feline nucleus reticularis thalami. J Physiol 271:135–154
Dutar P, Lamour Y, Jobert A (1985) Septohippocampal neurons in the rat: an in vivo intracellular study. Brain Res 340:135–142
el Mansari M, Sakai K, Jouvet M (1989) Unitary characteristics of presumptive cholinergic tegmental neurons during the sleep–waking cycle in freely moving cats. Exp Brain Res 76:519–529
Everitt BJ, Robbins TW (1997) Central cholinergic systems and cognition. Annu Rev Psychol 48:649–684
Fisher RS, Buchwald NA, Hull CD, Levine MS (1988) GABAergic basal forebrain neurons project to the neocortex: the localization of glutamic acid decarboxylase and choline acetyltransferase in feline corticopetal neurons. J Comp Neurol 272:489–502
Fischer W, Chen KS, Gage FH, Bjorklund A (1992) Progressive decline in spatial learning and integrity of forebrain cholinergic neurons in rats during aging. Neurobiol Aging 13:9–23
Flood JF, Morley JE, Roberts E (1992) Memory-enhancing effects in male mice of pregnenolone and steroids metabolically derived from it. Proc Natl Acad Sci U S A 89:1567–1571
Foley D, Ancoli-Israel S, Britz P, Walsh J (2004) Sleep disturbances and chronic disease in older adults: results of the 2003 National Sleep Foundation Sleep in America survey. J Psychosom Res 56:497–502
Ford B, Holmes CJ, Mainville L, Jones BE (1995) GABAergic neurons in the rat pontomesencephalic tegmentum: codistribution with cholinergic and other tegmental neurons projecting to the posterior lateral hypothalamus. J Comp Neurol 363:177–196
Frye CA (1995) The neurosteroid 3 alpha, 5 apha-THP has antiseizure and possible neuroprotective effects in an animal model of epilepsy. Brain Res 696:113–120
Frye CA, Lacey EH (1999) The neurosteroids DHEA and DHEAS may influence cognitive performance by altering affective state. Physiol Behav 66:85–92
Fujimoto K, Yoshida M, Ikeguchi K, Niijima K (1989) Impairment of active avoidance produced after destruction of pedunculopontine nucleus areas in the rat. Neurosci Res 6:321–328
Fujimoto K, Ikeguchi K, Yoshida M (1992) Impaired acquisition, preserved retention and retrieval of avoidance behavior after destruction of pedunculopontine nucleus areas in the rat. Neurosci Res 13:43–51
Fuller TA, Russchen FT, Price JL (1987) Sources of presumptive glutamergic/aspartergic afferents to the rat ventral striatopallidal region. J Comp Neurol 258:317–338
Grady CL, Craik FI (2000) Changes in memory processing with age. Curr Opin Neurobiol 10:224–231
Gritti I, Mainville L, Jones BE (1993) Codistribution of GABA- with acetylcholine-synthesizing neurons in the basal forebrain of the rat. J Comp Neurol 329:438–457
Haber S, Elde R (1981) Correlation between met-enkephalin and substance P immunoreactivity in the primate globus pallidus. Neuroscience 6:1291–1297
Hagan JJ, Salamone JD, Simpson J, Iversen SD, Morris RG (1988) Place navigation in rats is impaired by lesions of medial septum and diagonal band but not nucleus basalis magnocellularis. Behav Brain Res 27:9–20
Herholz K, Weisenbach S, Zundorf G, Lenz O, Schroder H, Bauer B, Kalbe E, Heiss WD (2004) In vivo study of acetylcholine esterase in basal forebrain, amygdala, and cortex in mild to moderate Alzheimer disease. Neuroimage 21:136–143
Hobson JA, Pace-Schott EF (2002) The cognitive neuroscience of sleep: neuronal systems, consciousness and learning. Nat Rev Neurosci 3:679–693
Houser CR, Crawford GD, Barber RP, Salvaterra PM, Vaughn JE (1983) Organization and morphological characteristics of cholinergic neurons: an immunocytochemical study with a monoclonal antibody to choline acetyltransferase. Brain Res 266:97–119
Ingham CA, Bolam JP, Smith AD (1988) GABA-immunoreactive synaptic boutons in the rat basal forebrain: comparison of neurons that project to the neocortex with pallidosubthalamic neurons. J Comp Neurol 273:263–282
Ingram DK, London ED, Reynolds MA (1982) Circadian rhythmicity and sleep: effects of aging in laboratory animals. Neurobiol Aging 3:287–297
Isaacson RL, Varner JA, Baars JM, De Wied D (1995) The effects of pregnenolone sulfate and ethylestrenol on retention of a passive avoidance task. Brain Res 689:79–84
Jakab RL, Leranth C (2005) Septum. In: Paxinos G (ed) The rat nervous system. Academic, London, pp 405–442
Jasper HH, Tessier J (1971) Acetylcholine liberation from cerebral cortex during paradoxical (REM) sleep. Science 172:601–602
Johansson IM, Birzniece V, Lindblad C, Olsson T, Backstrom T (2002) Allopregnanolone inhibits learning in the Morris water maze. Brain Res 934:125–131
Jones BE (1990) Immunohistochemical study of choline acetyltransferase-immunoreactive processes and cells innervating the pontomedullary reticular formation in the rat. J Comp Neurol 295:485–514
Kayama Y, Ohta M, Jodo E (1992) Firing of ‘possibly’ cholinergic neurons in the rat laterodorsal tegmental nucleus during sleep and wakefulness. Brain Res 569:210–220
Keating GL, Walker SC, Winn P (2002) An examination of the effects of bilateral excitotoxic lesions of the pedunculopontine tegmental nucleus on responding to sucrose reward. Behav Brain Res 134:217–228
Kelsey JE, Vargas H (1993) Medial septal lesions disrupt spatial, but not nonspatial, working memory in rats. Behav Neurosci 107:565–574
Kim SB, Hill M, Kwak YT, Hampl R, Jo DH, Morfin R (2003) Neurosteroids: cerebrospinal fluid levels for Alzheimer’s disease and vascular dementia diagnostics. J Clin Endocrinol Metab 88:5199–5206
King SR, Manna PR, Ishii T, Syapin PJ, Ginsberg SD, Wilson K, Walsh LP, Parker KL, Stocco DM, Smith RG, Lamb DJ (2002) An essential component in steroid synthesis, the steroidogenic acute regulatory protein, is expressed in discrete regions of the brain. J Neurosci 22:10613–10620
Kobayashi K, Miyazu K, Seki M, Fukutani Y, Hayashi M, Aoki T, Muramori F, Yamaguchi N (1994) Age-related changes in nerve growth factor receptor immunoreactive neurons in the magnocellular basal forebrain system in rat brain—an immunocytochemical and morphometric study. Dementia 5:57–61
Krnjevic K, Silver A (1965) A histochemical study of cholinergic fibres in the cerebral cortex. J Anat 99:711–759
Ladurelle N, Eychenne B, Denton D, Blair-West J, Schumacher M, Robel P, Baulieu E (2000) Prolonged intracerebroventricular infusion of neurosteroids affects cognitive performances in the mouse. Brain Res 858:371–379
Lambert JJ, Belelli D, Peden DR, Vardy AW, Peters JA (2003) Neurosteroid modulation of GABAA receptors. Prog Neurobiol 71:67–80
Lancel M, Faulhaber J, Schiffelholz T, Romeo E, Di Michele F, Holsboer F, Rupprecht R (1997) Allopregnanolone affects sleep in a benzodiazepine-like fashion. J Pharmacol Exp Ther 282:1213–1218
Leonard TO, Lydic R (1997) Pontine nitric oxide modulates acetylcholine release, rapid eye movement sleep generation, and respiratory rate. J Neurosci 17:774–785
Lolova IS, Lolov SR, Itzev DE (1996) Changes in NADPH-diaphorase neurons of the rat laterodorsal and pedunculopontine tegmental nuclei in aging. Mech Ageing Dev 90:111–128
Lolova IS, Lolov SR, Itzev DE (1997) Aging and the dendritic morphology of the rat laterodorsal and pedunculopontine tegmental nuclei. Mech Ageing Dev 97:193–205
Maquet P (2000) Functional neuroimaging of normal human sleep by positron emission tomography. J Sleep Res 9:207–231
Marston HM, Everitt BJ, Robbins TW (1993) Comparative effects of excitotoxic lesions of the hippocampus and septum/diagonal band on conditional visual discrimination and spatial learning. Neuropsychologia 31:1099–1118
Martinez-Serrano A, Bjorklund A (1998) Ex vivo nerve growth factor gene transfer to the basal forebrain in presymptomatic middle-aged rats prevents the development of cholinergic neuron atrophy and cognitive impairment during aging. Proc Natl Acad Sci U S A 95:1858–1863
Mathis C, Paul SM, Crawley JN (1994) The neurosteroid pregnenolone sulfate blocks NMDA antagonist-induced deficits in a passive avoidance memory task. Psychopharmacology (Berl) 116:201–206
Mathis C, Vogel E, Cagniard B, Criscuolo F, Ungerer A (1996) The neurosteroid pregnenolone sulfate blocks deficits induced by a competitive NMDA antagonist in active avoidance and lever-press learning tasks in mice. Neuropharmacology 35:1057–1064
Matthews DB, Morrow AL, Tokunaga S, McDaniel JR (2002) Acute ethanol administration and acute allopregnanolone administration impair spatial memory in the Morris water task. Alcohol Clin Exp Res 26:1747–1751
Maurice T (2001) Beneficial effect of the [sigma]1 receptor agonist PRE-084 against the spatial learning deficits in aged rats. Eur J Pharmacol 431:223–227
Mavanji V, Datta S (2003) Activation of the phasic pontine-wave generator enhances improvement of learning performance: a mechanism for sleep-dependent plasticity. Eur J Neurosci 17:359–370
Mayo W, Dellu F, Robel P, Cherkaoui J, Le Moal M, Baulieu EE, Simon H (1993) Infusion of neurosteroids into the nucleus basalis magnocellularis affects cognitive processess in the rat. Brain Res 607:324–308
Mayo W, George O, Darbra S, Bouyer JJ, Vallee M, Darnaudery M, Pallares M, Lemaire-Mayo V, Le Moal M, Piazza PV, Abrous N (2003) Individual differences in cognitive aging: implication of pregnenolone sulfate. Prog Neurobiol 71:43–48
McAlonan GM, Wilkinson LS, Robbins TW, Everitt BJ (1995) The effects of AMPA-induced lesions of the septo-hippocampal cholinergic projection on aversive conditioning to explicit and contextual cues and spatial learning in the water maze. Eur J Neurosci 7:281–292
Mellon SH, Griffin LD, Compagnone NA (2001) Biosynthesis and action of neurosteroids. Int Meet Rep Steroids Nerv Syst 78:7–8
Mendelson WB, Martin JV, Perlis M, Wagner R, Majewska MD, Paul SM (1987) Sleep induction by an adrenal steroid in the rat. Psychopharmacology (Berl) 93:226–229
Mesulam MM (1995) The cholinergic contribution to neuromodulation in the cerebral cortex. Semin Neurosci 7:297–307
Mesulam MM (1998) Some cholinergic themes related to Alzheimer’s disease: synaptology of the nucleus basalis, location of m2 receptors, interactions with amyloid metabolism, and perturbations of cortical plasticity. J Physiol (Paris) 92:293–298
Mesulam MM, Mufson EJ, Wainer BH, Levey AI (1983a) Central cholinergic pathways in the rat: an overview based on an alternative nomenclature (Ch1–Ch6). Neuroscience 10:1185–1201
Mesulam MM, Mufson EJ, Levey AI, Wainer BH (1983b) Cholinergic innervation of cortex by the basal forebrain: cytochemistry and cortical connections of the septal area, diagonal band nuclei, nucleus basalis (substantia innominata), and hypothalamus in the rhesus monkey. J Comp Neurol 214:170–197
Meziane H, Mathis C, Paul SM, Ungerer A (1996) The neurosteroid pregnenolone sulfate reduces learning deficits induced by scopolamine and has promnestic effects in mice performing an appetitive learning task. Psychopharmacology (Berl) 126:323–330
Mignot E, Taheri S, Nishino S (2002) Sleeping with the hypothalamus: emerging therapeutic targets for sleep disorders. Nat Neurosci 5(Suppl):1071–1075
Mitchell AS, Dalrymple-Alford JC, Christie MA (2002) Spatial working memory and the brainstem cholinergic innervation to the anterior thalamus. J Neurosci 22:1922–1928
Moragues N, Ciofi P, Lafon P, Odessa MF, Tramu G, Garret M (2000) cDNA cloning and expression of a gamma-aminobutyric acid A receptor epsilon-subunit in rat brain. Eur J Neurosci 12:4318–4330
Moragues N, Ciofi P, Tramu G, Garret M (2002) Localisation of GABA(A) receptor epsilon-subunit in cholinergic and aminergic neurones and evidence for co-distribution with the theta-subunit in rat brain. Neuroscience 111:657–669
Moruzzi G, Magoun HW (1995) Brain stem reticular formation and activation of the EEG. 1949. J Neuropsychiatry Clin Neurosci 7:251–267
Muir JL (1997) Acetylcholine, aging, and Alzheimer’s disease. Pharmacol Biochem Behav 56:687–696
Muir JL, Dunnett SB, Robbins TW, Everitt BJ (1992) Attentional functions of the forebrain cholinergic systems: effects of intraventricular hemicholinium, physostigmine, basal forebrain lesions and intracortical grafts on a multiple-choice serial reaction time task. Exp Brain Res 89:611–622
Muir JL, Everitt BJ, Robbins TW (1995) Reversal of visual attentional dysfunction following lesions of the cholinergic basal forebrain by physostigmine and nicotine but not by the 5-HT3 receptor antagonist, ondansetron. Psychopharmacology (Berl) 118:82–92
Muir JL, Bussey TJ, Everitt BJ, Robbins TW (1996) Dissociable effects of AMPA-induced lesions of the vertical limb diagonal band of Broca on performance of the 5-choice serial reaction time task and on acquisition of a conditional visual discrimination. Behav Brain Res 82:31–44
Myers BL, Badia P (1995) Changes in circadian rhythms and sleep quality with aging: mechanisms and interventions. Neurosci Biobehav Rev 19:553–571
Nyberg L, Persson J, Nilsson LG (2002) Individual differences in memory enhancement by encoding enactment: relationships to adult age and biological factors. Neurosci Biobehav Rev 26:835–839
Oh JD, Woolf NJ, Roghani A, Edwards RH, Butcher LL (1992) Cholinergic neurons in the rat central nervous system demonstrated by in situ hybridization of choline acetyltransferase mRNA. Neuroscience 47:807–822
Pace-Schott EF, Hobson JA (2002) The neurobiology of sleep: genetics, cellular physiology and subcortical networks. Nat Rev Neurosci 3:591–605
Pallares M, Darnaudery M, Day J, Le Moal M, Mayo W (1998) The neurosteroid pregnenolone sulfate infused into the nucleus basalis increases both acetylcholine release in the frontal cortex or amygdala and spatial memory. Neuroscience 87:551–558
Perez DLM, Possani LD, Tapia R, Teran L, Palacios R, Fuxe K, Hokfelt T, Ljungdahl A (1981) Demonstration of central gamma-aminobutyrate-containing nerve terminals by means of antibodies against glutamate decarboxylase. Neuroscience 6:875–895
Perry EK, Morris CM, Court JA, Cheng A, Fairbairn AF, McKeith IG, Irving D, Brown A, Perry RH (1995) Alteration in nicotine binding sites in Parkinson’s disease, Lewy body dementia and Alzheimer’s disease: possible index of early neuropathology. Neuroscience 64:385–395
Perry E, Walker M, Grace J, Perry R (1999) Acetylcholine in mind: a neurotransmitter correlate of consciousness? Trends Neurosci 22:273–280
Phillis JW (1968) Acetylcholine release from the cerebral cortex: its role in cortical arousal. Brain Res 7:378–389
Pirker S, Schwarzer C, Wieselthaler A, Sieghart W, Sperk G (2000) GABA(A) receptors: immunocytochemical distribution of 13 subunits in the adult rat brain. Neuroscience 101:815–850
Racchi M, Govoni S, Solerte SB, Galli CL, Corsini E (2001) Dehydroepiandrosterone and the relationship with aging and memory: a possible link with protein kinase C functional machinery. Brain Res Brain Res Rev 37:287–293
Rajkowski KM, Robel P, Baulieu EE (1997) Hydroxysteroid sulfotransferase activity in the rat brain and liver as a function of age and sex. Steroids 62:427–436
Ransmayr G, Faucheux B, Nowakowski C, Kubis N, Federspiel S, Kaufmann W, Henin D, Hauw JJ, Agid Y, Hirsch EC (2000) Age-related changes of neuronal counts in the human pedunculopontine nucleus. Neurosci Lett 288:195–198
Rhodes ME, Li PK, Flood JF, Johnson DA (1996) Enhancement of hippocampal acetylcholine release by the neurosteroid dehydroepiandrosterone sulfate: an in vivo microdialysis study. Brain Res 733:284–286
Rhodes ME, Li PK, Burke AM, Johnson DA (1997) Enhanced plasma DHEAS, brain acetylcholine and memory mediated by steroid sulfatase inhibition. Brain Res 773:28–32
Riekkinen P Jr, Aaltonen M, Riekkinen P (1991) Tetrahydroaminoacridine inhibits high voltage spindle activity in aged rats after acute and chronic treatment. Psychopharmacology (Berl) 103:265–267
Rosenberg RS, Zepelin H, Rechtschaffen A (1979) Sleep in young and old rats. J Gerontol 34:525–532
Rye DB (1997) Contributions of the pedunculopontine region to normal and altered REM sleep. Sleep 20:757–788
Rye DB, Wainer BH, Mesulam MM, Mufson EJ, Saper CB (1984) Cortical projections arising from the basal forebrain: a study of cholinergic and noncholinergic components employing combined retrograde tracing and immunohistochemical localization of choline acetyltransferase. Neuroscience 13:627–643
Rye DB, Saper CB, Lee HJ, Wainer BH (1987) Pedunculopontine tegmental nucleus of the rat: cytoarchitecture, cytochemistry, and some extrapyramidal connections of the mesopontine tegmentum. J Comp Neurol 259:483–528
Saito H, Sakai K, Jouvet M (1977) Discharge patterns of the nucleus parabrachialis lateralis neurons of the cat during sleep and waking. Brain Res 134:59–72
Saper CB (1984) Organization of cerebral cortical afferent systems in the rat. II. Magnocellular basal nucleus. J Comp Neurol 222:313–342
Saper CB, Chelimsky TC (1984) A cytoarchitectonic and histochemical study of nucleus basalis and associated cell groups in the normal human brain. Neuroscience 13:1023–1037
Sarter M, Bruno JP (1997) Cognitive functions of cortical acetylcholine: toward a unifying hypothesis. Brain Res Brain Res Rev 23:28–46
Sarter M, Bruno JP (2004) Developmental origins of the age-related decline in cortical cholinergic function and associated cognitive abilities. Neurobiol Aging 25:1127–1139
Satoh K, Armstrong DM, Fibiger HC (1983) A comparison of the distribution of central cholinergic neurons as demonstrated by acetylcholinesterase pharmacohistochemistry and choline acetyltransferase immunohistochemistry. Brain Res Bull 11:693–720
Satorra-Marin N, Coll-Andreu M, Portell-Cortes I, Aldavert-Vera L, Morgado-Bernal I (2001) Impairment of two-way active avoidance after pedunculopontine tegmental nucleus lesions: effects of conditioned stimulus duration. Behav Brain Res 118:1–9
Schiffelholz T, Holsboer F, Lancel M (2000) High doses of systemic DHEA-sulfate do not affect sleep structure and elicit moderate changes in non-REM sleep EEG in rats. Physiol Behav 69:399–404
Schumacher M, Weill-Engerer S, Liere P, Robert F, Franklin RJ, Garcia-Segura LM, Lambert JJ, Mayo W, Melcangi RC, Parducz A, Suter U, Carelli C, Baulieu EE, Akwa Y (2003) Steroid hormones and neurosteroids in normal and pathological aging of the nervous system. Prog Neurobiol 71:3–29
Shute CC, Lewis PR (1963) Cholinesterase-containing systems of the brain of the rat. Nature 199:1160–1164
Sierra A, Lavaque E, Perez-Martin M, Azcoitia I, Hales DB, Garcia-Segura LM (2003) Steroidogenic acute regulatory protein in the rat brain: cellular distribution, developmental regulation and overexpression after injury. Eur J Neurosci 18:1458–1467
Steckler T, Inglis W, Winn P, Sahgal A (1994) The pedunculopontine tegmental nucleus: a role in cognitive processes? Brain Res Brain Res Rev 19:298–318
Steinbusch HW, Nieuwenhuys R (1981) Localization of serotonin-like immunoreactivity in the central nervous system and pituitary of the rat, with special references to the innervation of the hypothalamus. Adv Exp Med Biol 133:7–35
Steininger TL, Wainer BH, Blakely RD, Rye DB (1997) Serotonergic dorsal raphe nucleus projections to the cholinergic and noncholinergic neurons of the pedunculopontine tegmental region: a light and electron microscopic anterograde tracing and immunohistochemical study. J Comp Neurol 382:302–322
Steriade M, Datta S, Pare D, Oakson G, Curro Dossi RC (1990) Neuronal activities in brain-stem cholinergic nuclei related to tonic activation processes in thalamocortical systems. J Neurosci 10:2541–2559
Stone WS (1989) Sleep and aging in animals. Relationships with circadian rhythms and memory. Clin Geriatr Med 5:363–379
Szymusiak R, McGinty D (1986) Sleep-related neuronal discharge in the basal forebrain of cats. Brain Res 370:82–92
Szymusiak R, Alam N, McGinty D (2000) Discharge patterns of neurons in cholinergic regions of the basal forebrain during waking and sleep. Behav Brain Res 115:171–182
Taylor CL, Kozak R, Latimer MP, Winn P (2004) Effects of changing reward on performance of the delayed spatial win-shift radial maze task in pedunculopontine tegmental nucleus lesioned rats. Behav Brain Res 153:431–438
Torres EM, Perry TA, Blockland A, Wilkinson LS, Wiley RG, Lappi DA, Dunnet SB (1994) Behavioural, histochemical and biochemical consequences of selective immunolesions in discrete regions of the basal forebrain cholinergic system. Neuroscience 63:95–122
Torterolo P, Yamuy J, Sampogna S, Morales FR, Chase MH (2001) GABAergic neurons of the laterodorsal and pedunculopontine tegmental nuclei of the cat express c-fos during carbachol-induced active sleep. Brain Res 892:309–319
Turkmen S, Lundgren P, Birzniece V, Zingmark E, Backstrom T, Johansson IM (2004) 3beta-20beta-dihydroxy-5alpha-pregnane (UC1011) antagonism of the GABA potentiation and the learning impairment induced in rats by allopregnanolone. Eur J Neurosci 20:1604–1612
Urani A, Privat A, Maurice T (1998) The modulation by neurosteroids of the scopolamine-induced learning impairment in mice involves an interaction with sigma1 (sigma1) receptors. Brain Res 799:64–77
Vallée M, Mayo W, Darnaudery M, Corpechot C, Young J, Koehl M, Le Moal M, Baulieu EE, Robel P, Simon H (1997) Neurosteroids: deficient cognitive performance in aged rats depends on low pregnenolone sulfate levels in the hippocampus. Proc Natl Acad Sci U S A 94:14865–14870
Vallée M, Mayo W, Le Moal M (2001) Role of pregnenolone, dehydroepiandrosterone and their sulfate esters on learning and memory in cognitive aging. Brain Res Brain Res Rev 37:301–312
Vallée M, George O, Vitiello S, Le Moal M, Mayo W (2004) New insights into the role of neuroactive steroids in cognitive aging. Exp Gerontol 39:1695–1704
Van Someren EJ (2000) Circadian rhythms and sleep in human aging. Chronobiol Int 17:233–243
Weill-Engerer S, David JP, Sazdovitch V, Liere P, Eychenne B, Pianos A, Schumacher M, Delacourte A, Baulieu EE, Akwa Y (2002a) Neurosteroid quantification in human brain regions: comparison between Alzheimer’s and nondemented patients. J Clin Endocrinol Metab 87:5138–5143
Weill-Engerer S, David JP, Sazdovitch V, Liere P, Eychenne B, Pianos A, Schumacher M, Delacourte A, Baulieu EE, Akwa Y (2002b) Neurosteroid quantification in human brain regions: comparison between Alzheimer’s and nondemented patients. J Clin Endocrinol Metab 87:5138–5143
Wenk GL (1997) The nucleus basalis magnocellularis cholinergic system: one hundred years of progress. Neurobiol Learn Mem 67:85–95
Woolf NJ (1991) Cholinergic systems in mammalian brain and spinal cord. Prog Neurobiol 37:475–524
Woolf NJ, Butcher LL (1981) Cholinergic neurons in the caudate–putamen complex proper are intrinsically organized: a combined Evans blue and acetylcholinesterase analysis. Brain Res Bull 7:487–507
Woolf NJ, Eckenstein F, Butcher LL (1984) Cholinergic systems in the rat brain: I. Projections to the limbic telencephalon. Brain Res Bull 13:751–784
Young TB (2004) Epidemiology of daytime sleepiness: definitions, symptomatology, and prevalence. J Clin Psychiatry 65(Suppl 16):12–16
Zaborszky L, Carlsen J, Brashear HR, Heimer L (1986) Cholinergic and GABAergic afferents to the olfactory bulb in the rat with special emphasis on the projection neurons in the nucleus of the horizontal limb of the diagonal band. J Comp Neurol 243:488–509
Zou LB, Yamada K, Sasa M, Nakata Y, Nabeshima T (2000) Effects of sigma(1) receptor agonist SA4503 and neuroactive steroids on performance in a radial arm maze task in rats. Neuropharmacology 39:1617–1627
Acknowledgments
Supported by INSERM, Université de Bordeaux II, and the European Community (QLK6-CT-2000-00179).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
George, O., Vallée, M., Le Moal, M. et al. Neurosteroids and cholinergic systems: implications for sleep and cognitive processes and potential role of age-related changes. Psychopharmacology 186, 402–413 (2006). https://doi.org/10.1007/s00213-005-0254-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-005-0254-6