Abstract
Rationale
Previous research investigating the effects of stimulants, such as methylphenidate (MPH), on children with attention deficit/hyperactivity disorder (AD/HD) has rarely included autonomic measures of arousal.
Objective
Our aim was to clarify the effects of MPH on central and autonomic measures in AD/HD children during a continuous performance task (CPT) using a naturalistic open-label study.
Method
Thirty-six boys (18 AD/HD and 18 control) participated in a CPT over two trial periods, allowing a more valid estimate of the effects of medication, rather than assuming that retesting per se has no substantial impact. MPH was administered to the AD/HD group 1 h prior to the second trial. Errors and reaction time (RT) were recorded as measures of performance, electrodermal activity as an autonomic nervous system measure and event-related potentials (ERPs) as an index of central nervous system activity.
Results
AD/HD children made more errors than controls in the first session, but no group differences were found after medication. No significant differences were observed for RT. Skin conductance level was found to be lower in AD/HD children than controls, but this difference was also ameliorated after medication. Conversely, mean skin conductance response to target stimuli was found not to differ between groups during the initial test phase but became significantly different in phase 2. ERP data showed topographic differences between groups in N1, P2, N2 and P3 at the initial test phase, which were reduced at the second test.
Conclusion
Stimulant medication ameliorated some of the dysfunctions in AD/HD children, which are reflected in behavioural and ERP measures. These results, in combination with general differences in electrodermal activity, support a hypoarousal model of AD/HD, which can explain the action of MPH in these children.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Attention deficit/hyperactivity disorder (AD/HD) is a prevalent and persistent developmental syndrome, estimated to affect 7.5% of 6- to 17-year olds in Australia (Graetz et al. 2001), c.f. 3–5% in the USA (American Psychiatric Association 1994). For more than half a century, AD/HD has been treated using stimulant medications, including methylphenidate (MPH) and dexamphetamine. While the effectiveness of this is well documented, it is still not clear how these effects are achieved. Several theories attribute the effectiveness of psychostimulants to their ability to enhance levels of arousal in the central nervous system (CNS) and autonomic nervous system (ANS), assuming that children with AD/HD are typically underaroused (see Satterfield and Cantwell 1974; Sergeant et al. 1999). This model also accounts for the seemingly paradoxical effect of stimulant medications on the behaviours of AD/HD children; in small doses, stimulants act to increase their arousal to normal levels, which results in reduction of the problem behaviours. In a recent review, Oades (2005) reports biochemical support for the concept of hypoarousal in AD/HD from measures of adrenaline and phenylethylamine. Previous research has shown that adrenaline levels tend to be low in urine samples from AD/HD children, and accordingly, the adrenergic response to stress is reduced (Hanna et al. 1996). Treatment with MPH and other amphetamines has been shown to increase adrenaline levels (e.g. McCracken et al. 1990), supporting their low levels of arousal becoming partially normalised through treatment with stimulant medications.
Event-related potentials (ERPs) have been used to gain insight into brain functioning in AD/HD by investigating attentional, inhibitory and preparatory processing. ERPs reliably discriminate between children with AD/HD and controls (Klorman et al. 1979; Strandburg et al. 1996; see review in Barry et al. 2003). Importantly, the electrophysiological abnormalities associated with AD/HD are concurrent with performance deficits on psychometric instruments such as the continuous performance task (CPT), a group of paradigms for the evaluation of attention and response inhibition. The basic paradigm for the CPT involves selective attention or vigilance for an infrequently occurring target and is characterised by the rapid presentation of continuously changing stimuli with a designated target stimulus or pattern (Riccio et al. 2001).
ERP studies investigating AD/HD and control children using CPTs typically find reduced amplitudes in AD/HD groups for the early negative components N1 and N2 (Prichep et al. 1976; Klorman et al. 1979; Holcomb et al. 1985, 1986; Satterfield et al. 1990; Strandburg et al. 1996; Overtoom et al. 1998). Further, reduced P2 and P3 amplitudes have been reported for AD/HD children in studies using the CPT-AX task (O'Toole et al. 1997; Overtoom et al. 1998; Okazaki et al. 2002) and variations (Michael et al. 1981; Strandburg et al. 1996; Sunohara et al. 1999; Seifert et al. 2003). Findings for ERP latencies in CPTs are less consistent, with delayed components reported for AD/HD in some studies (Klorman et al. 1990; Strandburg et al. 1996; Sunohara et al. 1999) but not others (Klorman et al. 1979; Michael et al. 1981).
Electrophysiological and behavioural research suggests that administration of psychostimulants to children with AD/HD reduces differences from controls in terms of both arousal and performance measures. Michael et al. (1981) reported reduced errors and reaction time (RT) in a CPT after MPH, a result replicated using variations of the CPT (Klorman et al. 1979, 1983; O'Toole et al. 1997; Sunohara et al. 1999; Okazaki et al. 2002). Conversely, Satterfield et al. (1974) found that while overall performance improved after psychostimulants, RT increased, suggesting that stimulant medications result in slower responding when it is more appropriate in terms of task demands.
MPH has been found to ameliorate electrophysiological differences between AD/HD and control groups in attentional tasks (Prichep et al. 1976; Klorman et al. 1979, 1990; Jonkman et al. 2000) and specifically CPT paradigms (Klorman et al. 1981, 1983; Zillesen et al. 2001; Okazaki et al. 2002; Seifert et al. 2003), although several studies report no effect of MPH on the P3 component in terms of amplitude or latency (Jonkman et al. 1999, 2000), while others have found amplitude but not latency effects (Michael et al. 1981).
Surprisingly, there is a paucity of research concurrently measuring effects of MPH on arousal and activation in the ANS during tasks requiring performance despite its immediate relevance. Electrodermal activity is commonly utilised to illustrate arousal differences, with skin conductance level (SCL) reflecting tonic arousal and the skin conductance response (SCR) indicating phasic changes associated with task-related activation. We consider arousal as a state variable reflecting current energetic factors and have shown close connections between SCL and electroencephalogram (EEG) measures (Barry et al. 2004). This approach is generally compatible with Pribram and McGuiness (1975, 1992), who identified arousal and activation systems with different neural substrates. Satterfield and Dawson (1971) found lower levels of skin conductance in hyperkinetic children than controls, interpreting these results to indicate underarousal of the reticular activating system, but others have reported no difference (Cohen and Douglas 1972; Rapoport et al. 1980). Several studies have reported smaller amplitude SCRs in AD/HD (Cohen and Douglas 1972; Spring et al. 1974; Zahn et al. 1975; Shibigaki et al. 1993). Satterfield and Dawson (1971), using SCL as a measure, found psychostimulants elevated abnormally low arousal levels in AD/HD. Cohen et al. (1971) reported a higher resting SCL after medication but no change in SCRs. Conversely, Spring et al. (1974) found increased SCRs but no difference in SCL with medication. Similarly, Rapoport et al. (1980) reported no variation in skin conductance after stimulant medication—smaller SCRs were obtained in some tasks. These contradictory results emphasise the need for further investigation.
The current study aimed to investigate the effects of psychostimulants in children with AD/HD during a CPT. We examined behavioural and physiological indices of attention (ERPs) in children with AD/HD and controls while simultaneously investigating changes in arousal (SCL) and activation (SCR), specifically after MPH administration in children with AD/HD (the effects of psychostimulants in control subjects cannot be tested due to ethical limitations). As far as we know, such a combination of measures has not been explored in relation to medication effects in AD/HD.
We tested both groups in two phases, comparing AD/HD children with controls in each session, rather than assuming that retesting per se has no substantial impact. This approach has been rarely used previously, with most studies assuming that test repetition has little effect (e.g. Jonkman et al. 2000; Okazaki et al. 2002; Seifert et al. 2003). There is no evidence to support this assumption; indeed, children of this age range may quickly habituate to the laboratory situation, resulting in substantial attentional and motivational shifts between sessions.
We expected that children with AD/HD would perform more poorly than control children and show typical electrophysiological indices of an attention deficit (e.g. generally smaller ERP amplitudes, often associated with atypical topography, such as a more anterior P3) and lower levels of arousal (lower SCLs) in the initial test phase. It was further expected that the administration of MPH to children with AD/HD would reduce these differences between the groups in the second test session.
Method
Subjects
Participants were 18 male Caucasian children with AD/HD of the combined type, aged between 8 years 3 months and 13 years 4 months (mean=11 years 4 months, SD=2 years 1 month), and 18 controls individually matched on sex and age. The AD/HD group was recruited from a private paediatric practice in Sydney and via a local newspaper advertisement. Participants in the control group were also recruited via the newspaper advertisement. Children with AD/HD had been previously diagnosed by a paediatrician and psychologist according to Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition criteria and had not presented with any co-morbid disorders. Two of the controls were medicated for asthma (combinations of Ventolin, Pulmicort and Seretide), and all of the AD/HD group were taking MPH for this disorder, with daily doses ranging from 10 to 40 mg (mean=24.4, SD=9.2 mg). All children abstained from their MPH for 24 h prior to testing.
In addition to a clinical interview, the AD/HD and control groups were assessed using the Child Behaviour Checklist (CBCL; Achenbach and Edelbrock 2001) completed by the parent, two subtests of the Stanford Binet Intelligence Scale (Vocabulary and Quantitative), the South Australian Spelling Test (SAST) and the Neale Analysis of Reading–Revised (Neale 1999). Children in the control group were screened to ensure that no symptoms of AD/HD or other developmental delays/disorders were present. For participants to be included, an IQ score ≥85 was required. Children consuming any stimulants (e.g. caffeine) prior to the test session were excluded. All children reported no vision or hearing problems, had English as their first language and were currently attending school. For the AD/HD group, 17 children were right-handed and 1 was left-handed; all controls were right-handed.
Physiological recording
The continuous scalp EEG was recorded using electrodes at 19 sites (Fp1, Fp2, F3, Fz, F4, F7, F8, C3, Cz, C4, T3, T4, T5, T6, P3, Pz, P4, O1, O2) of the international 10–20 system. Electro-oculogram (EOG) was recorded using tin cup electrodes situated 1 cm above and below the left eye [vertical EOG (vEOG)] and on the outer canthi of the left and right eyes (horizontal EOG). Cap electrodes were referenced to linked ears, and ear and eye electrodes were affixed with tape. Impedance levels were below 3 kΩ for ear and eye electrodes and 5 kΩ for cap electrodes. Subjects were grounded by an electrode located midway between the Fpz and Fz sites. The EEG was amplified 19× with a 0.5-Hz high-pass filter, a 70-Hz low-pass filter, sampled using a 22 bit A/D converter and recorded at 500 Hz by Neuroscan software. The EEG data were later low-pass filtered down 3 dB at 30 Hz.
Electrodermal activity was recorded from Ag/AgCl electrodes secured on the distal volar surfaces of digits 2 and 3 of the non-dominant hand, using an electrolyte of 0.05 M NaCl in an inert viscous ointment base. Skin conductance was sampled at 10 Hz using a constant voltage device (UFI Bioderm model 2701) set at 0.5 V. This system was used to separately record a tonic DC-coupled SCL and AC-coupled (1-s time constant) fluctuations in skin conductance (SCR), both measured in microSiemens (μS).
For each subject, mean SCL was taken as the average from onset of the first stimulus to the end of the block in each session. Mean phasic response to correct target stimuli was obtained by averaging the SCRs at each point in the data stream over 10-s epochs time-locked to target onset, analogous to ERP averaging, following the procedure used by Barry and O'Gorman (1989). In accordance with Barry (1990), the mean SCR was identified as the amplitude of this ERP-style response within this epoch commencing in a 1–3-s latency window after stimulus onset.
The ERP epoch was defined as 200 ms pre-stimulus to 800 ms post-stimulus onset. Epochs containing amplitudes greater than ±150 μV at any non-frontal site were excluded from averaging. Additionally, an ocular artefact reduction procedure (Semlitsch et al. 1986) based on vEOG was used. Averages were then calculated for the target ERPs at each site. N1, P2, N2 and P3 peaks were quantified by means of an automatic peak picking program based on slope changes in defined latency ranges, with visual confirmation, to determine individual amplitudes and latencies for each component.
Procedure
Parents provided written consent for their child to participate, and children provided assent. Children were then fitted with an Electro-cap, ear, eye and skin conductance electrodes and seated in an air-conditioned, sound-attenuated booth. Each child performed two tasks: a CPT and an auditory cued ‘go/no-go’ task, included as part of another study (task order was rotated across subjects). The CPT was similar to the vigilance task of the Gordon Diagnostic System (Gordon 1986). Stimuli were presented on a 15-in. computer monitor positioned at eye level, 1 m from where the participant was seated. The A–X version of the CPT consisted of the numbers 0, 1, 2, 3, 4, 5, 6, 7, 8 and 9. The numbers were white on a black background and 4 cm in height. Stimuli remained on the screen for 200 ms with an 800-ms inter-stimulus interval.
The task included a practice block of 15 stimulus presentations followed by two blocks of 180 sequentially displayed stimuli (360 stimuli in total) for 6 min. Children performed the task on two occasions, so two forms of the task were used to avoid practice effects; the order was counterbalanced between groups and trials.
In one version, the target sequence was a 1 followed by a 9. The alternative version used a 3 followed by a 5. Both tasks included 15 randomly presented paired target stimuli per 3-min block, with 30 paired targets presented during a single task. Participants responded to target stimuli using a button pressed with the index finger of their dominant hand. Responses to target stimuli which followed a cue (i.e. 1 then 9 or 3 then 5) within 1,000 ms of target onset were deemed correct. Other responses, including those to target stimuli not preceded by a cue, cues not followed by a target and distractors, were considered incorrect but were recorded to calculate number of errors, RT and for general assessment of task performance.
AD/HD and control children participated in two sessions separated by a 1-h interval. AD/HD children were administered their prescribed dosage of MPH immediately after test session 1, allowing 1 h for the medication to take effect. This time-frame was deemed adequate for MPH to metabolise and was compatible with the methodology of similar studies (O'Toole et al. 1997; Clarke et al. 2002; Okazaki et al. 2002; Seifert et al. 2003). During this interval, children were taken to an adjacent room for a psychometric assessment, lasting approximately 45 min. The time which had elapsed during these tests ensured the absorption rate of the medication for the AD/HD group and was unaffected by food consumption. The children then completed the ‘go/no-go’ and the alternative form of the CPT-AX task for test session 2. This research protocol was approved by the joint Illawarra Area Health Service/University of Wollongong Human Research Ethics Committee.
Data analysis
Demographic and psychometric data were analysed using analysis of variance. Electrodermal (SCL and SCR) and behavioural (errors and RT) data were analysed with multivariate analysis of variance (MANOVA) with group as a between-subjects factor (AD/HD and control), and separate analyses run for test periods 1 and 2.
While EEG was recorded from 19 sites, analyses of the ERP data were restricted to nine sites (F3, Fz, F4, C3, Cz, C4, P3, Pz, P4) to cover the major effects expected. N1, P2, N2 and P3 amplitudes and latencies to target stimuli were examined using separate MANOVAs for test period 1 and 2, with group (AD/HD and control) as a between-subjects factor and lateral [left (F3, C3, P3), midline (Fz, Cz, Pz), right (F4, C4, P4)] and sagittal [frontal (F3, Fz, F4), central (C3, Cz, C4), posterior (P3, Pz, P4)] as within-subjects site factors. Within site, contrasts compared the frontal region with the posterior region, and their mean with the central region; the left hemisphere was compared with the right hemisphere, and their mean with the midline, allowing optimal clarification of site effects within the regions studied. As the contrasts were planned and there were no more of them than the degrees of freedom for effect, no Bonferroni-type adjustment to α was necessary (Tabachnick and Fidell 1989). Further, these single degree of freedom contrasts preclude the problems of nonsphericity often encountered with repeated measures analyses, thus avoiding the need for their control using Greenhouse–Geisser type epsilon adjustments. Degrees of freedom for all effects are 1,34 unless otherwise stated.
Results
Group differences
Table 1 presents the means and statistical results for demographic and behavioural variables. The AD/HD and control groups did not differ on age, IQ, reading or spelling ability. Children with AD/HD had higher scores than controls on all subscales of the CBCL, and this difference was significant on most subscales.
Performance data
Total errors were subject to a square-root transformation to reduce the skew commonly associated with the small numbers of errors during simple RT tasks. This reduced the skew over all data points and subjects from 2.02 to 0.20. At time 1, the AD/HD group committed more errors than the control group (2.50>1.81, F=4.83, p<0.05), a difference not present at time 2 (1.55∼1.56, F<1; see Table 1).
No significant group differences were found for RTs to target stimuli in either test session (Table 1).
Electrodermal activity
Skin conductance level
During the initial session, children in the AD/HD group had lower SCL than controls (AD/HD 9.63 μS<control 12.83 μS, F=7.41, p<0.05). This difference was no longer present in the second session, where AD/HD children showed an increased SCL (AD/HD 10.51 μS∼control 12.24 μS, F<1).
Skin conductance response
Following Barry and Sokolov (1993), SCRs were subjected to a square-root transformation to reduce the skew commonly associated with small responses in the electrodermal field. This reduced the skew over all data points and subjects from 1.44 to 0.21. At time 1, no significant differences were observed in SCRs (AD/HD 0.26 √μS vs controls 0.27 √μS, F<1). At time 2, AD/HD children showed reduced SCRs relative to control children (0.20 √μS vs 0.26 √μS, F=5.19, p<0.05).
Event-related potentials
Waveform morphology
Figure 1 illustrates the major components (N1, P2, N2 and P3) for AD/HD and control groups at all sites for the grand mean ERPs to target stimuli.
N1 amplitude
As shown in Fig. 2A, the N1 component (largest negativity in the 100–190 ms range) for the initial test phase showed a strong frontal maximum (frontal>parietal F=20.68, p<0.001; frontal/parietal>central F=9.96, p<0.005). In the lateral dimension, a larger N1 was found in the right than left hemisphere (F=16.25, p<0.001) and in the hemispheres than the midline (F=5.60, p<0.001). The latter effect was less at frontal than posterior sites (F=4.55, p<0.05). This Lateral × Sagittal interaction differed between the groups, with the lateral difference being similar at frontal and posterior sites in the AD/HD group compared with the large posterior difference in the control group (F=3.59, p=0.066). Figure 2A indicates the existence of an atypical frontal midline reduction of N1 in the AD/HD group.
In the second phase, Fig. 2B shows that the frontal maximum was maintained (frontal>parietal F=33.19, p<0.001; frontal/parietal>central F=15.80, p<0.001). Laterally, greater N1 persisted in the right hemisphere than left (F=23.61, p<0.001), and N1 was larger in the hemispheres than the midline (F=38.95, p<0.001). A Lateral × Sagittal interaction was also observed, with enhancement of frontal N1 relative to posterior sites greater in the right than left hemisphere (F=5.72, p<0.05). The previous Group × Lateral × Sagittal interaction shown in Fig. 2A did not remain significant.
P2 amplitude
During the first test period, the P2 component (largest positivity in the 190–250 ms range) showed a centro-parietal maximum (parietal>frontal F=13.63, p<0.001; central>frontal/parietal F=64.22, p<0.001). In the lateral dimension, P2 was larger in the left hemisphere than the right (F=15.70, p<0.001) and larger along the midline than the hemispheres (F=46.57, p<0.001). Additionally, there was a Lateral × Sagittal interaction with a greater midline enhancement of P2 at parietal than frontal sites (F=15.93, p<0.001). A Group × Sagittal interaction was found for this component, with a smaller increase in P2 at parietal than frontal sites in AD/HD children compared to controls (F=5.95, p<0.05). Figure 3A illustrates the reduced parietal P2 in the AD/HD group. There was also a Group × Lateral × Sagittal interaction which approached significance—the central enhancement of P2 was greater in the midline than the hemispheres for both AD/HD and control groups, but the extent of this difference was smaller for AD/HD children than control children (F=3.69, p=0.063).
At time 2, P2 sustained its centro-parietal maximum (parietal>frontal F=28.63, p<0.001; central>frontal/parietal F=40.63, p<0.001). In the lateral dimension, P2 remained larger in the left than right hemisphere (F=17.30, p<0.001) and along the midline relative to the hemispheres (F=56.95, p<0.001; see Fig. 3B). The Lateral × Sagittal interaction persisted, with an enhancement of midline P2 greater at parietal than frontal sites (F=25.10, p<0.001). Further, there was a Group × Lateral interaction—a smaller elevation in midline P2 relative to the hemispheres for children with AD/HD compared to the control group (F=6.63, p<0.05). There was also a Group × Lateral × Sagittal interaction which approached significance—midline enhancement of P2 was greater parietally than frontally, but the extent of this parietal elevation was smaller for the AD/HD than control group (F=3.61, p=0.066). Overall, the pattern of topographic difference between the groups was similar to the initial test period, although differences were less significant.
N2 amplitude
At time 1, the N2 component (largest negativity between 200 and 300 ms) was maximal frontally (frontal>parietal F=9.93, p<0.005; frontal/parietal>central F=74.75, p<0.001). Laterally, N2 was larger in the right hemisphere than the left (F=10.77, p<0.005) and in the hemispheres than the midline (F=27.23, p<0.001). There was also a Lateral × Sagittal interaction with the midline N2 reduction greater at parietal than frontal sites (F=22.07, p<0.001). In terms of group differences, Fig. 4A demonstrates a Group × Sagittal interaction, with the AD/HD group showing a diminished frontal N2 relative to the control group (F=6.63, p<0.05). Further, there was a Group × Sagittal × Lateral interaction, in that the central decrease in N2 was greater in the left hemisphere than the right for the AD/HD group, with this reversed in the control group (F=7.45, p<0.01).
For time 2, N2 again showed a frontal maximum (frontal>parietal F=11.33, p<0.005; frontal/parietal>central F=57.64, p<0.001). In the lateral dimension, N2 remained greater in the right than left hemisphere (F=6.59, p<0.05) and in the hemispheres than the midline (F=28.14, p<0.001). There was also a Lateral × Sagittal interaction in the second test period with midline N2 enhanced in the frontal region and reduced in the parietal region (F=45.18, p<0.001). As shown in Fig. 4B, the Group × Sagittal interaction present at time 1 was no longer significant at time 2. The Group × Lateral × Sagittal interaction present in the initial test period—a greater decrease in central N2 in the left than right hemisphere for the AD/HD group and the reverse of this in the control group—was somewhat weaker at the second test (F=5.39, p<0.05).
P3
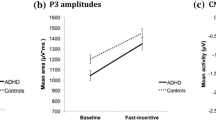
P3 amplitude
At time 1, the P3 component (greatest positivity between 300 and 450 ms) showed a centro-parietal maximum (parietal>frontal F=11.04, p<0.005; central>frontal/parietal F=14.97, p<0.001). In the lateral dimension, P3 was greater in the left than right hemisphere (F=8.21, p<0.01) and greater in the midline than the hemispheres (F=14.9, p<0.001). The parietal enhancement was larger in the midline than the hemispheres (F=32.77, p<0.001). There was a significant Group × Sagittal interaction, with the AD/HD group demonstrating a reduced posterior P3 compared to controls (F=10.90, p<0.005; see Fig. 5A). Further, a Group × Sagittal × Lateral interaction was observed, with little effect in the AD/HD group and a central enhancement of the midline P3 relative to the hemispheres apparent in the control group (F=4.33, p<0.05); this is primarily due to reduced parietal P3 in the hemispheres in AD/HD.
At time 2, the centro-parietal maximum was maintained (parietal>frontal F=15.18, p<0.001; central>frontal/parietal F=25.95, p<0.001). Laterally, the difference between left and right hemispheres was no longer present, although greater P3 was still apparent in the midline relative to the hemispheres (F=15.15, p<0.001). The pattern of parietal enhancement was also maintained, with greater P3 at the midline than the hemispheres (F=47.90, p<0.001). A significant difference was observed between groups, with the AD/HD group showing a smaller P3 than controls across the scalp (F=16.06, p<0.001). There was also a Group × Sagittal interaction which approached significance. Figure 5B shows that the AD/HD group's reduced posterior P3 relative to the control group was somewhat normalised in this period (F=4.03, p=0.053). The Group × Sagittal × Lateral interaction observed at time 1 was not present at time 2.
Latencies for P3 and other components
For the P3 latency at time 1, there was a Group × Sagittal interaction, with AD/HD children showing shorter latencies frontally than parietally and control children, the opposite (AD/HD, frontal 421.0 ms<parietal 426.0 ms; control, parietal 381.6 ms<frontal 402.8 ms, F=5.54, p<0.05). Further, there was a Group × Sagittal × Lateral interaction—for the AD/HD group, shorter latencies were seen frontally in both hemispheres, although the parietal increase in latency was greater in the right hemisphere than the left (left: frontal 422.1 ms<parietal 427.0 ms; right: frontal 419.3 ms<parietal 427.8 ms); for the control group, shorter latencies were observed at frontal than parietal sites in the left hemisphere, with the opposite pattern observed in the right hemisphere (left: frontal 393.7 ms<parietal 396.9 ms; right: frontal 404.0 ms>parietal 364.3 ms, F=5.18, p<0.05). No latency differences between the groups were found for any other components.
At time 2, no group differences were found for P3 latency or the latencies of any other component.
Discussion
Task performance data indicated that boys in the AD/HD group initially committed more errors than controls, but after medication, this difference was no longer present. We consider that these findings, and others here, can be readily generalised to children of both genders, and thus, we refer to “children” rather than “boys” in the following. Previous literature supports the notion that behavioural data obtained using CPTs indicate poorer performance in children with AD/HD (e.g. Klorman et al. 1979; Michael et al. 1981; Overtoom et al. 1998; Jonkman et al. 2000; Okazaki et al. 2002) and that stimulant medication reduces these performance deficits (e.g. Klorman et al. 1979, 1983; Michael et al. 1981; Okazaki et al. 2002). No significant group differences were found for RT to target stimuli, consistent with several previous studies (Jonkman et al. 1999, 2000; Karayanidis et al. 2000; Okazaki et al. 2002). Specifically, no change was observed for the AD/HD group after MPH—a finding not without precedent (e.g. Jonkman et al. 1999, 2000; Sunohara et al. 1999; Okazaki et al. 2002). These findings suggest MPH may not necessarily improve response speed but rather demonstrates efficacy by enhancing attention and concentration, illustrated by improved accuracy and task performance of AD/HD children in the second session.
Children with AD/HD were found to have a lower SCL than controls, consistent with several studies (e.g. Satterfield and Dawson 1971; Cohen and Douglas 1972; Satterfield and Cantwell 1974; Satterfield et al. 1974; Shibigaki and Yamanaka 1990) and compatible with models of underarousal (Sergeant et al. 1999; Satterfield and Dawson 1971). Several studies have reported MPH to increase SCL in children with AD/HD, ameliorating the difference between AD/HD and control groups (Cohen et al. 1971; Satterfield and Cantwell 1974; Satterfield et al. 1974). Consistent with this, AD/HD children showed an increased SCL here after MPH administration, resulting in no significant group differences.
While no significant group differences were found for SCR in the initial test period, in the second test session, the difference between the groups became significant due to a reduction in the SCRs of children in the AD/HD group. This decrease may be indicative of the action of stimulants. Rapoport et al. (1980) reported that hyperactive children showed decreased SCRs after psychostimulant administration. Satterfield and Dawson (1971) suggested that stimulants result in slower responding when it is more appropriate to do so in terms of the demands of a task. Thus, it is possible that the decreased amplitudes of SCRs post MPH are indicative of maintenance of arousal at a level most effective for accurate decision making based on task demands or, alternatively, that children with AD/HD find it easier to respond adequately to task demands when medicated.
For the current study, negative ERP components (N1 and N2) were found to have significantly different topographic distributions for the AD/HD group relative to controls. For both components, diminished amplitudes were found frontally in the AD/HD group, compatible with previous research investigating negativities across several attentional paradigms (e.g. Prichep et al. 1976; Klorman et al. 1979; Holcomb et al. 1985, 1986; Satterfield et al. 1990; Oades et al. 1996; Strandburg et al. 1996; Overtoom et al. 1998; Johnstone et al. 2001). Importantly, a change in these topographies was observed in the second test period—the differences between AD/HD and control groups were reduced. In particular, N1 amplitude differences between groups were not significant in the second test session, indicating that the action of MPH had normalised the amplitudes of the AD/HD group, in keeping with the findings of previous medication studies (e.g. Klorman et al. 1990).
For P2, AD/HD children were observed to have decreased amplitudes parietally, a pattern which remained in the second test period, although slight increases in amplitude were observed which may be attributed to MPH. Similarly, P3 amplitudes were found to be decreased in the AD/HD group during the initial test session. Reduced P3 amplitudes have been reported in numerous visual CPT paradigms (e.g. Klorman et al. 1979; Overtoom et al. 1998) and have been suggested to indicate attentional problems (Overtoom et al. 1998; Karayanidis et al. 2000), diminished evaluation and processing capacities (Klorman 1991; Frank et al. 1994) and deficient central resource allocation (Holcomb et al. 1986; Humphreys and Kramer 1994; Kok 2001). For the second test period, the P3 amplitudes were somewhat normalised for the AD/HD group. Notably, this normalisation coincided with MPH administration, a finding reported in other research utilising CPTs (Klorman et al. 1979; Zillesen et al. 2001; Seifert et al. 2003) and other paradigms (e.g. Prichep et al. 1976; Klorman et al. 1990; Jonkman et al. 2000).
For P3 latency, a significant difference was observed between groups in terms of topography, although these differences were not significant in the second test session due to changes in the AD/HD group, again, indicating an ameliorating affect of MPH. These findings correspond with most other studies of AD/HD children (e.g. Taylor et al. 1993; Oades et al. 1996) and some which have investigated the effects of stimulant medication (e.g. Holcomb et al. 1985; Winsberg et al. 1997).
In summary, MPH ameliorated some group differences between AD/HD children and controls, as reflected by ERP and behavioural measures. In combination with general differences in electrodermal activity, these data lend support to models of hypoarousal (e.g. Satterfield and Cantwell 1974), explaining the action of MPH in children with AD/HD and the effectiveness of stimulant medications in treating the performance deficits associated with this disorder. Future research may attempt to clarify these findings through the use of a balanced double-blind medication design with the AD/HD children, although ethical limits preclude stimulant medication testing with the controls. It may also be useful to employ methodologies which account for attentional fluctuation during tasks (such as recent CPT variants, e.g. Teicher et al. 2004) to maximise potential differences existing between AD/HD and control groups. In this study, we tested both experimental and control children on two occasions rather than making the common experimental assumption that repeated testing itself has no substantial effect. Thus, the effects reported here strengthen previous findings. This relatively novel approach, together with adding electrodermal measures to ERPs and behavioural indices, has demonstrated its value in clarifying the effects of medication in AD/HD children. The results argue for the value of this approach in future work.
References
Achenbach TM, Edelbrock C (eds) (2001) Manual for the Child Behaviour Checklist and revised child behaviour profile. University of Vermont, Burlington, VT
American Psychiatric Association (1994) DSM-IV Diagnostic and statistical manual of mental disorders, 4th edn. American Psychiatric Association, Washington, DC
Barry RJ (1990) Scoring criteria for response latency and habituation in electrodermal research: a study in the context of the OR. Psychophysiology 27:94–100
Barry RJ, O'Gorman JG (1989) Methods and mechanisms in electrodermal studies of omission responding. Biol Psychol 28:271–277
Barry RJ, Sokolov EN (1993) Habituation of phasic and tonic components of the orienting reflex. Int J Psychophysiol 15:39–42
Barry RJ, Johnstone S, Clarke AR (2003) A review of electrophysiology in attention-deficit/hyperactivity disorder: II. Event-related potentials. Clin Neurophysiol 114:184–198
Barry RJ, Clarke AR, McCarthy R, Selikowitz M, Rushby JA, Ploskova E (2004) EEG differences in children as a function of resting-state arousal level. Clin Neurophysiol 115:402–408
Clarke A, Barry RJ, McCarthy R, Selikowitz M, Croft RJ (2002) EEG differences between good and poor responders to methylphenidate in boys with the inattentive type of attention-deficit/hyperactive disorder. Clin Neurophysiol 113:1191–1198
Cohen NJ, Douglas VI (1972) Characteristics of the orienting response in hyperactive and normal children. Psychophysiology 9:238–245
Cohen NJ, Douglas VI, Morgenstern G (1971) The effect of methylphenidate on attentive behaviour and autonomic activity in hyperactive children. Psychopharmacologica 22:282–294
Frank Y, Seiden JA, Napolitano B (1994) Event-related potentials to an “oddball” auditory paradigm in children with learning disabilities with or without attention deficit hyperactivity disorder. Clin Electroencephalogr 25:136–141
Gordon M (1986) How is a computerised attention test used in the diagnosis of attention deficit disorder? J Child Contemp Soc 19:53–64
Graetz BW, Sawyer MG, Hazell PL, Arney F, Baghurst P (2001) Validity of DSM-IV ADHD subtypes in a nationally representative sample of Australian children and adolescents. J Am Acad Child Adolesc Psych 40:1410–1418
Hanna GL, Ornitz EM, Hariharan M (1996) Urinary epinephrine excretion during intelligence testing in attention-deficit hyperactivity disorder and normal boys. Biol Psychiatry 40:553–555
Holcomb PJ, Ackerman PT, Dykman R (1985) Cognitive event-related brain potentials in children with attention and reading deficits. Psychophysiology 22:656–667
Holcomb PJ, Ackerman PT, Dykman R (1986) Auditory event-related potentials in attention and reading disabled boys. Int J Psychophysiol 3:263–273
Humphreys DG, Kramer AF (1994) Toward a psychophysiological assessment of dynamic changes in mental workload. Hum Factors 36:3–26
Johnstone SJ, Barry RJ, Anderson JW (2001) Topographic distribution and developmental timecourse of auditory event-related potentials in two subtypes of attention-deficit hyperactivity disorder. Int J Psychophysiol 42:73–94
Jonkman LM, Kemner C, Verbaten MN, Van Engeland H, Kenemans JL, Camfferman G et al (1999) Perceptual and response interference in children with attention-deficit hyperactivity disorder, and the effects of methylphenidate. Psychophysiology 36:419–428
Jonkman LM, Kemner C, Verbaten MN, Van Engeland H, Camfferman G, Buitelaar JK et al (2000) Attentional capacity, a probe ERP study: differences between children with attention-deficit hyperactivity disorder and normal control children and effects of methylphenidate. Psychophysiology 37:337–346
Karayanidis F, Robaey P, Bourassa M, De Koning D, Geoffroy G, Pelletier G (2000) ERP differences in visual attention processing between attention-deficit hyperactivity disorder and control boys in the absence of performance differences. Psychophysiology 37:319–333
Klorman R (1991) Cognitive event-related potentials in attention deficit disorder. J Learn Disabil 24:130–140
Klorman R, Salzman LF, Pass HL, Borgstedt AD, Dainer KB (1979) Effects of methylphenidate on hyperactive children's evoked response during passive and active attention. Psychophysiology 16:23–29
Klorman R, Salzman LF, Borgstedt AD, Dainer KB (1981) Normalising effects of methylphenidate on hyperactive children's vigilance performance and evoked potentials. Psychophysiology 18:665–677
Klorman R, Salzman LF, Bauer LO, Coons HW, Borgstedt AD, Halpern WI (1983) Effects of two doses of methylphenidate on cross-situational and borderline hyperactive children's evoked potentials. Electroencephalogr Clin Neurophysiol 56:169–185
Klorman R, Brumaghim JF, Salzman LF, Strauss J, Borgstedt AD, McBride MC, Loeb S (1990) Effects of methylphenidate on processing negativities in patients with attention-deficit hyperactivity disorder. Psychophysiology 27:328–337
Kok A (2001) On the utility of P3 amplitude as a measure of processing capacity. Psychophysiology 38(3):557–577
McCracken JT, Hinshaw SP, Henker B, Whalen CK, Zupran B (1990) Urinary catecholamine differences in ADHD versus normal children and effects of methylphenidate. Society for Research in Child and Adolescent Psychopathology, Los Angeles
Michael RL, Klorman R, Salzman LF, Borgstedt AD, Dainer KB (1981) Normalising effects of methylphenidate on hyperactive children's vigilance performance and evoked potentials. Psychophysiology 18:665–677
Neale MD (1999) Neale analysis of reading ability manual, 3rd edn. Australian Council for Educational Research Limited, Melbourne, Victoria
Oades RD (2005) The roles of norepinephrine and serotonin in attention deficit hyperactivity disorder. In: Gozal D, Molfese DL (eds) Attention deficit hyperactivity disorder: from genes to patients. Humana Press Inc, Totowa, New Jersey, pp 97–130
Oades RD, Dittmann-Balcar A, Schepke R, Eggers C, Zerbin B (1996) Auditory event-related potentials (ERPs) and mismatch negativity (MMN) in healthy children and those with attention deficit or tourette/tic symptoms. Biol Psychol 43:163–185
Okazaki S, Maekawa H, Ozaki H, Futakami S (2002) Topographic changes of ERP during CPT-AX task at pre- and post-medication of methylphenidate in children with ADHD. Int Congr Ser 1232:705–710
O'Toole K, Abramowitz A, Morris R, Dulcan M (1997) Effects of methylphenidate on attention and nonverbal learning in children with attention-deficit hyperactivity disorder. J Am Acad Child Adolesc Psych 36:531–539
Overtoom CE, Verbaten MN, Kemner C, Kenemans JL, van Engeand H, Buitelaar JK, Camfferman G, Koelega HS (1998) Associations between event-related potentials and measures of attention and inhibition in the continuous performance task in children with ADHD and normal controls. J Am Acad Child Adolesc Psych 37:977–986
Pribram KH, McGuiness D (1975) Arousal activation and effort in the control of attention. Psychol Rev 2:116–149
Pribram KH, McGuiness D (1992) Attention and para-attentional processing: event-related brain potentials as tests of a model. In: Friedman D, Bruder GE (eds) Psychophysiology and experimental psychopathology: a tribute to Samuel Sutton, vol. 658. Annals of the New York Academy of Sciences, New York Academy of the Sciences, New York, NY, pp 65–92
Prichep LS, Sutton S, Hakerem G (1976) Evoked potentials in hyperkinetic and normal children under certainty and uncertainty: a placebo and methylphenidate study. Psychophysiology 13:418–428
Rapoport JL, Buchsbaum MS, Weingartner H, Zahn TP, Ludlow C, Mikkelsen EJ (1980) Dextroamphetamine: its cognitive and behavioural effects in normal and hyperactive boys and normal men. Arch Gen Psychiatry 37:933–943
Riccio CA, Reynolds CR, Lowe PA (eds) (2001) Clinical applications of continuous performance tests: measuring attention and impulsive responding in children and adults. Wiley, New York
Satterfield JH, Cantwell DP (1974) CNS function and response to methylphenidate in hyperactive children. Psychopharmacol Bull 10:36–37
Satterfield JH, Dawson ME (1971) Electrodermal correlates of hyperactivity in children. Psychophysiology 8:191–197
Satterfield JH, Satterfield BT, Cantwell DP (1974) Pathophysiology of the hyperactive child syndrome. Arch Gen Psychiatry 31:839–844
Satterfield JH, Schell AM, Nicholas TW, Satterfield BT, Freese TH (1990) Ontogeny of selective attention effects on event-related potentials in attention-deficit hyperactivity disorder and normal boys. Biol Psychiatry 28:879–903
Seifert J, Scheuerpflug P, Zillensen KE, Fallgatter A, Warnke A (2003) Electrophysiological investigation of the effectiveness of methylphenidate in children with and without AD/HD. J Neural Transm 110:821–829
Semlitsch H-V, Anderer P, Schuster P, Presslich O (1986) A solution for reliable and valid reduction of ocular artefact, applied to the P300 ERP. Psychophysiology 23:695–703
Sergeant JA, Oosterlaan J, van der Meere J (1999) Information processing and energetic factors in attention-deficit/hyperactivity disorder. In: Quay HC, Hogan AE (eds) Handbook of disruptive behaviour disorders. Kluver Academic/Plenum, New York, pp 75–104
Shibigaki M, Yamanaka T (1990) Attention of hyperactive preschool children—electrodermal activity during auditory stimulation. Percept Mot Skills 70:235–242
Shibigaki M, Yamanaka T, Furuya T (1993) Attention state in electrodermal activity during auditory stimulation of children with attention-deficit hyperactivity disorder. Percept Mot Skills 77:331–338
Spring C, Greenberg L, Scott J, Hopwood J (1974) Electrodermal activity in hyperactive boys who are methylphenidate responders. Psychophysiology 11:436–442
Strandburg RJ, Marsh J, Brown W, Asarnow RF, Higa J, Harper R et al (1996) Continuous-processing-related event-related potentials in children with attention deficit hyperactivity disorder. Biol Psychiatry 40:964–980
Sunohara GA, Malone MA, Rovet J, Humphries TD, Roberts W, Taylor MJ (1999) Effect of methylphenidate on attention in children with attention deficit hyperactivity disorder (ADHD): ERP evidence. Neuropsychopharmacology 21(2):218–228
Tabachnick BG, Fidell LS (eds) (1989) Using multivariate statistics. Harper Collins, New York
Taylor MJ, Voros JG, Logan WJ, Malone MA (1993) Changes in event-related potentials with stimulant medication in children with attention deficit hyperactivity disorder. Biol Psychol 36:139–156
Teicher MH, Lowen SB, Polcari A, Foley M, McGreenery CE (2004) Novel strategy for the analysis of CPT data provides new insight into the effects of methylphenidate on attentional states in children with ADHD. J Child Adolesc Psychopharmacol 14:219–232
Winsberg BG, Javitt DC, Silipo GS (1997) Electrophysiological indices of information processing in methylphenidate responders. Biol Psychiatry 42:434–445
Zahn TP, Abate F, Little B, Wender PH (1975) Minimal brain dysfunction, stimulant drugs, and autonomic nervous system activity. Arch Gen Psychiatry 32:381–387
Zillesen KE, Scheuerpflug P, Fallgatter AJ, Strik WK, Warnke A (2001) Changes of the brain electrical fields during the continuous performance test in attention-deficit hyperactivity disorder—boys depending on methylphenidate medication. Clin Neurophysiol 112:1166–1174
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lawrence, C.A., Barry, R.J., Clarke, A.R. et al. Methylphenidate effects in attention deficit/hyperactivity disorder: electrodermal and ERP measures during a continuous performance task. Psychopharmacology 183, 81–91 (2005). https://doi.org/10.1007/s00213-005-0144-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-005-0144-y