Abstract
Rationale
Formalin-induced pain is reduced in sigma-1 (σ1) receptor knockout mice; therefore, we hypothesized that haloperidol and its metabolites I and II, which have affinity for σ1 receptors, may modulate formalin-induced pain.
Results
Intraplantar administration of formalin (2.5%) to CD-1 mice produced a biphasic period of pain. Haloperidol (0.03–1 mg/kg, s.c.) and reduced haloperidol (metabolite II, 0.25–8 mg/kg, s.c.) dose-dependently inhibited both phases of formalin-induced pain. Haloperidol metabolite I (4–128 mg/kg, s.c.) also produced dose-dependent antinociception in the second phase of the formalin test, but was less potent and effective against first-phase pain. Haloperidol metabolite III (16 and 128 mg/kg) and (−)sulpiride (200 mg/kg), which have no affinity for σ1 receptors, did not produce significant antinociception in either phase of the formalin test. The order of potency of the drugs to produce their antinociceptive effect [haloperidol > metabolite II > metabolite I ≫ metabolite III= (−)sulpiride=inactive] correlated with their affinity for σ1 receptors, but not with their affinity for σ2 or dopamine D2 receptors. Naloxone (1 mg/kg, s.c.) did not antagonize the antinociception induced by haloperidol and its metabolites. None of the antinociceptive drugs in the formalin test produced any antinociception in the tail flick test.
Conclusion
These results suggest that the antinociceptive effect of haloperidol and its metabolites in the formalin test is not due to unspecific/generalised inhibition of nociception or modulation of opioid receptors, and that it may be related, at least partially, to the ability of these drugs to interact with σ1 receptors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Haloperidol is a widely used drug for the treatment of acute and chronic psychosis; its antipsychotic activity and many other of its pharmacological effects result, at least in part, from its ability to act as an antagonist at dopamine D2 receptors (Marder 1998). Haloperidol shows similar affinity for D2 and sigma (σ) receptors (Walker et al. 1990; Bowen et al. 1990), but the consequences of its binding to σ receptors are less well known. Two major metabolic pathways have been identified for haloperidol in animals and humans (see Bowen et al. 1990 for references). One is a reversible reductive pathway that produces 4-(4-chlorophenyl)-α-(4-fluorophenyl)-4-hydroxy-1-piperidinebutanol (also called reduced haloperidol or metabolite II). The other is an oxidative N-dealkylation pathway that leads to two products: 4-(4-chlorophenyl)-4-hydroxypiperidine (metabolite I) and 3-(4-fluorobenzoyl)propionic acid (metabolite III). In comparison to haloperidol, reduced haloperidol has high affinity for σ receptors but shows much lower affinity for D2 receptors (Bowen et al. 1990; Jaen et al. 1993). Metabolite I has a lower affinity for σ receptors than haloperidol and reduced haloperidol, but no affinity for D2 receptors, whereas metabolite III has no affinity for either σ or D2 receptors (Bowen et al. 1990; Matsumoto and Pouw 2000).
Sigma receptors have a unique pharmacological profile that includes interactions with some antipsychotics, (+)enantiomers of opioid drugs and some neurosteroids, among other drugs (Walker et al. 1990; Maurice et al. 2001). The σ receptors have been classified into two distinct subtypes called σ1 and σ2, which differ in their affinities for σ ligands and their tissue distribution (Quirion et al. 1992; Maurice et al. 2001; Guitart et al. 2004). The σ1 receptors have been cloned in several species including the mouse, and their amino acid sequence does not resemble that of any other mammalian protein (Hanner et al. 1996; Seth et al. 1997; Pan et al. 1998). These receptors have a wide but specific distribution throughout the central nervous system, including areas of great importance in pain control such as the superficial layers of the spinal cord dorsal horn and the periaqueductal gray matter (Alonso et al. 2000; Kitaichi et al. 2000). The role of σ1 receptors in acute pain modulation is substantiated by the fact that agonists of σ1 receptors, such as (+)pentazocine, antagonize the antinociception induced by agonists of mu (μ), delta (δ) and kappa (κ)-opioid receptors in a tail flick test (Chien and Pasternak 1994; Mei and Pasternak 2002), whereas treatment with σ1 receptor antagonists such as haloperidol or with σ1 receptor antisense oligodeoxynucleotides enhances the antinociception induced by agonists of these opioid receptors (Chien and Pasternak 1994; King et al. 1997; Pan et al. 1998; Mei and Pasternak 2002). These data suggest that there is an endogenous σ1 system that is tonically active, antagonizing opioid-induced antinociception and facilitating pain perception (Chien and Pasternak 1994; King et al. 1997; Pan et al. 1998; Mei and Pasternak 2002). In support of this notion, we recently found that formalin-induced pain is reduced in σ1 receptor knockout animals (Cendan et al. 2005). These findings suggest the hypothesis that σ1 receptor antagonists can produce antinociception in the formalin test.
To test this hypothesis, we evaluated the effect of haloperidol and its metabolites (metabolites I and II), which have affinity for σ1 receptors (Jaen et al. 1993; Matsumoto and Pouw 2000), on pain induced by formalin in mice and compared their effects with that of (−)sulpiride, a drug with affinity for D2 receptors (Freedman et al. 1994) but not for σ receptors (Matsumoto and Pouw 2000), and haloperidol metabolite III, a drug devoid of affinity for either σ or D2 receptors (Bowen et al. 1990; Matsumoto and Pouw 2000). Moreover, to test whether the antinociceptive effects of the drugs evaluated in the formalin test (a model of tonic pain induced by a chemical stimulus) are also seen in other types of nociception, we evaluated the effect of these drugs in the tail flick test (a model of acute pain induced by a thermal stimulus).
In mice lacking μ- and δ-opioid receptor genes, the duration of formalin-induced pain is longer (Martin et al. 2003), and intrathecal treatment with antiserum against leu-enkephalin or dynorphin A (1–17) enhances the pain induced by formalin (Wu et al. 2002). These results suggest that endogenous opioids tonically modulate formalin-induced pain. Since haloperidol enhances the antinociception induced by agonists of μ-, δ- and κ-opioid receptors in thermal tests (Chien and Pasternak 1994, 1995), its antinociceptive activity in the formalin test might be due to enhancement of the effect of endogenous opioid peptides. To test this hypothesis, we studied the effect of naloxone, an antagonist of μ-, δ- and κ-opioid receptors (Dhawan et al. 1996), on the antinociception induced by haloperidol and its metabolites in the formalin test. As a positive control, we also evaluated the effect of naloxone on morphine-induced antinociception in this test.
Materials and methods
Animals
Female CD-1 mice (Charles River, Spain) weighing 25–30 g were used. The animals were housed in colony cages with free access to food and water prior to the experiments. They were maintained in temperature- and light-controlled rooms (22±1°C, lights on at 0800 hours and off at 2000 hours, air replacement every 20 min). Testing took place during the light phase (from 0900 to 1500 hours). Mice were handled in accordance with EEC Council Directive 86/609 and with current guidelines for the investigation of experimental pain with conscious animals (Zimmermann 1983). The experimental procedure was approved by the University of Granada Ethical Committee on Animal Research.
Drugs and drug administration
The drugs used (and their providers) were haloperidol, haloperidol metabolites I, II and III, (−)sulpiride, naloxone HCl (Sigma-Aldrich Química S.A., Spain) and morphine HCl (General Directorate of Pharmacy and Drugs, Spanish Ministry of Health). Morphine and naloxone were dissolved in saline, whereas all the other drugs were administered in a 5% gum arabic suspension in ultrapure water. An equal volume of the solvent was used in the control group. The drug under study (or its solvent) was injected subcutaneously (s.c.) into the interscapular zone in a volume of 5 ml/kg and was administered 30 min before formalin injection or immediately after the basal tail flick latency was recorded (see below). When naloxone was associated to any of the other drugs under study, the animals first received an injection of naloxone solution in the subcutaneous space above the left scapula and, immediately thereafter, another s.c. injection of the drug under study solution (morphine, haloperidol or its metabolite) or its solvent in the space above the right scapula. Thirty minutes after the second s.c. injection, the animals received an intraplantar injection of the formalin solution as explained below. Diluted formalin was prepared from a stock solution of 38% formaldehyde (Panreac, S.A., Spain) with the addition of physiological saline (0.9% NaCl in water) to obtain the appropriate concentration of formalin (2.5%).
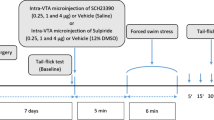
Formalin test
Formalin tests were performed as previously described (Shibata et al. 1989) with small modifications. In all the experiments, 20 μl of a 2.5% formalin solution was injected into the dorsal surface of the right hind paw of the mouse, using a Hamilton microsyringe with a 301/2-gauge needle. Immediately thereafter, the animal was put into a glass cylinder and the observation period started. A small mirror was placed behind the glass cylinder to allow clear observation of the paws. The time spent in licking or biting the injected paw during 45 min (divided into nine periods of 5 min each) after the injection was measured as an indicator of the pain response in mice non-treated (naive) and treated with the solvent of the drugs. Because a similar biphasic response was observed in both groups (see Results and Fig. 1), we decided to record two different periods of licking/biting of the injected paw in drug-treated animals. The first period was recorded 0–5 min after the injection of formalin and was considered indicative of first-phase pain. The second period was recorded 15–35 min after formalin injection and was considered indicative of second-phase pain. The duration of the formalin-induced response in naive and solvent-treated animals was similar in both the first phase (89.91±6.79 vs 86.5±9.19 s, respectively) and the second phase (202.73±29.48 vs 188.25±36.79 s, respectively) of pain.
Time course of the pain response (duration of licking or biting of the treated paw) induced by the intraplantar injection of 2.5% formalin to non-treated (naive) (○) and solvent-treated (•) mice. Each point and vertical line represents the mean±SEM of values obtained in at least eight animals. No statistically significant differences between the two groups were observed in any observation period (ANOVA)
Tail flick test
The test was performed as previously described by us (Moncada et al. 2003). Briefly, the animals were restrained in a Plexiglas tube and placed on the tail flick apparatus (LI 7100, Letica, S.A., Spain). A noxious beam of light was focussed on the tail about 4 cm from the tip, and the tail flick latency was recorded automatically to the nearest 0.1 s. The intensity of the radiant heat source was adjusted to yield baseline latencies between 3 and 5 s; this intensity was never changed and any animal whose baseline latency was outside the pre-established limits was excluded from the experiments. In order to minimise injury in the animals, a cut-off time of 10 s was used. Baseline tail flick latencies were recorded 10 min and immediately before drug administration; the mean value of the two measurements was considered the basal tail flick latency. Once baseline latencies were obtained, the animals received an s.c. injection of the drug under study (or the solvent), and tail flick latencies were measured again at 30, 60, 90, 120 and 150 min after drug administration.
Data analysis
The degree of antinociception induced by the different treatments in the formalin test was calculated with the following formula: \(\% \,{\text{antinociception = }}{\left[ {{\left( {{\text{LT}}_{{\text{c}}} - {\text{LT}}_{{\text{t}}} } \right)}/{\text{LT}}_{{\text{c}}} } \right]} \times 100\), where LTc and LTt represent the licking time in control (solvent-injected) and treated (drug-injected) animals, respectively. The values of ED50 (dose of drug that produced half of the maximal antinociception) and E max (maximum antinociceptive effect) were calculated from the dose-response curves using non-linear regression analysis, so that the data could be fitted to a sigmoidal equation, with the SigmaPlot 2000 version 6.00 computer program (SPSS Science, USA). The values in the control group were compared against those obtained in the treated groups using one- or two-way analysis of variance (ANOVA) followed by Newman–Keuls test. The differences between the values in naloxone- and naloxone solvent-treated groups were analysed with a Student's t-test. In all cases, the differences between means were considered significant when the value of P was below 0.05. All results are given as the mean±SEM.
Results
Effects of haloperidol and its metabolites in the formalin test
The intraplantar injection of 2.5% formalin produced a biphasic period of intensive licking/biting of the injected paw both in non-treated (naive) and solvent-treated mice (Fig. 1). First-phase pain ensued 0–10 min after formalin injection, whereas second-phase pain was evident from 10 to 45 min. There were no statistically significant differences between the two experimental groups in the time spent licking or biting the injected paw in any observation period (Fig. 1).
Haloperidol (0.25 mg/kg, s.c.) markedly inhibited both phases of formalin-induced pain; by contrast, much higher doses of haloperidol metabolite III (16 and 128 mg/kg, s.c.) and (−)sulpiride (200 mg/kg, s.c.) did not produce significant antinociception in any phase of the formalin test (Fig. 2).
Comparison of the antinociceptive effects induced by the subcutaneous administration of haloperidol (0.25 mg/kg), haloperidol metabolite III (16 and 128 mg/kg) and (−)sulpiride (200 mg/kg) in the formalin test in mice. Each bar and vertical line represents the mean±SEM of the values obtained in at least eight animals. Statistically significant differences between the solvent- and drug-injected groups: **P<0.01 (one-way ANOVA followed by Newman–Keuls test)
To better characterize the effect of haloperidol, a wide range of doses was tested. Haloperidol (0.03–1 mg/kg, s.c.) produced dose-dependent antinociception in both phases of the formalin test, being slightly more potent and efficacious against the second phase (Fig. 3a). The ED50 values were 0.11±0.01 and 0.07±0.004 mg/kg for the first and second phase, respectively, and the E max values were 90.06±4.67% antinociception for the first phase and 98.6±1.52% for the second phase. Haloperidol metabolite II (0.25–8 mg/kg, s.c.) showed a similar pattern of activity to haloperidol in both phases of the formalin test (Fig. 3b). The data were also adjusted to a sigmoid curve, which allowed us to calculate E max values of 83.04±6.55 and 97.08±6.17%, and ED50 values of 1.03±0.19 and 0.61±0.09 mg/kg for the first and second phase, respectively (Table 1).
Antinociceptive effects of subcutaneously administered haloperidol (a), haloperidol metabolite II (b) and haloperidol metabolite I (c), in the first phase (•) and second phase (□) of the formalin test in mice. Each point and vertical line represents the mean±SEM of the values obtained in at least eight animals. Statistically significant differences between the solvent- and drug-injected groups: *P<0.05, **P<0.01 (two-way ANOVA followed by Newman–Keuls test)
Haloperidol metabolite I (4–128 mg/kg, s.c.) produced dose-dependent antinociception in the second phase of the formalin test (Fig. 3c), with an E max of 64.27±3.72% and an ED50 of 10.83±1.79 mg/kg (Table 1). Its antinociceptive effect in the first phase of formalin-induced pain was smaller (Fig. 3c) and only reached statistical significance with the dose of 64 mg/kg, which produced 27.65±9% antinociception.
Effects of naloxone on the antinociception induced by morphine, haloperidol and its metabolites in the formalin test
Naloxone (1 mg/kg, s.c.) did not significantly modify formalin-induced pain in any phase (% antinociception=13.16±10.54 in the first phase and 13.66±6.07 in the second phase, P>0.05 in comparison to control group). Morphine (4 mg/kg, s.c.) produced a marked antinociception in both phases of the formalin test, and its effect was almost abolished when animals also received naloxone (1 mg/kg, s.c.; Fig. 4a,b). On the other hand, the same dose of naloxone did not significantly modify the antinociception induced by haloperidol (0.125 mg/kg, s.c.), haloperidol metabolite II (1 mg/kg, s.c.) or haloperidol metabolite I (16 mg/kg, s.c.) in any phase of the formalin test (Fig. 4a,b).
Effects of naloxone (1 mg/kg, s.c.) on the antinociception induced by the subcutaneous administration of morphine (4 mg/kg), haloperidol (0.125 mg/kg), haloperidol metabolite II (1 mg/kg) and haloperidol metabolite I (16 mg/kg) in the formalin test in mice. Each bar and vertical line represents the mean±SEM of the values obtained in at least six animals. Statistically significant differences between the solvent- and naloxone-injected group: **P<0.01 (Student's t test)
Effects of haloperidol and its metabolites in the tail flick test
The subcutaneous administration of doses of haloperidol (2 mg/kg), metabolite II (8 mg/kg) and metabolite I (128 mg/kg) that produced maximum antinociception in the formalin test had no antinociceptive effect in the tail flick test (Fig. 5). As a positive control, we used morphine (4–16 mg/kg, s.c.), which produced dose-dependent antinociception in this test (Fig. 5).
Time course of the effects on mice tail flick latency of subcutaneous treatment with solvent, haloperidol (2 mg/kg), haloperidol metabolite I (128 mg/kg), haloperidol metabolite II (8 mg/kg) or different doses of morphine (4–16 mg/kg). Each point and vertical line represents the mean±SEM of the values obtained in at least eight animals. All doses of morphine produced a statistically significant (P<0.01) effect in comparison with solvent at all the times evaluated, whereas none of the other treatments had a significant effect at any time (two-way ANOVA followed by Newman–Keuls test). HAL Haloperidol, MET metabolite, MOR morphine
Discussion
In this study, we found that the subcutaneous administration of haloperidol and two of its metabolites (metabolites I and II) produced dose-dependent antinociception in the formalin test, whereas haloperidol metabolite III and (−)sulpiride did not. We also observed that none of the drugs evaluated (except morphine) produced any antinociceptive effect in the tail flick test, which suggests that the antinociception induced by haloperidol and its metabolites against formalin-induced pain is not due to unspecific or generalised inhibition of nociception. The effect of haloperidol and its metabolites in the formalin test and the lack of effect of haloperidol metabolites in the tail flick test were previously unreported, whereas the absence of effect of haloperidol in the tail flick test is consistent with the results of previous studies (Dykstra and Woods 1986; Chien and Pasternak 1994, 1995).
The neurotransmitters and spinal pathways that modulate tail flick and formalin test responses differ (Fasmer et al. 1985; Ryan et al. 1985; Zimmer et al. 1998), and the two pain models also differ in their sensitivity to different drugs (Millan and Seguin 1994; Correa et al. 1996; Shimoyama et al. 1997). Therefore, the differential effects of haloperidol and its metabolites I and II in these two tests are not unusual and may be due to the different types of pain that each test explores. The tail flick test is a model of nociceptive pain produced by thermal stimuli of very short duration (i.e., phasic pain). This test measures changes in the pain threshold that produces a tail flick response, and this response is mainly a spinal reflex, which is modulated by supraspinal mechanisms (Le Bars et al. 2001). By contrast, the formalin test uses suprathreshold chemical stimuli that produce a much more elaborate response than a spinal reflex, and the pain lasts much longer (i.e., tonic pain) than in the tail flick test (Le Bars et al. 2001). Moreover, formalin injection produces an inflammatory response and sensitization of spinal cord neurons (Le Bars et al. 2001). In view of these differences, our results suggest that haloperidol and its metabolites can be expected to produce more antinociception in models of tonic than phasic pain.
It has been suggested that drugs that produce antinociceptive effects in the second phase of formalin-induced pain are effective in reducing other types of persistent pain in which central sensitization processes are involved (Jett et al. 1997; Vissers et al. 2003), and there are case reports describing the efficacy of haloperidol in the treatment of chronic pain in humans (Raft et al. 1979). Therefore, it seems interesting to investigate the possible antinociceptive effect of haloperidol and its metabolites in models of pain that involve central sensitization and in experimental models of chronic pain.
Naloxone has been reported to enhance (Ossipov et al. 1996), reduce (Vaccarino et al. 1989) or have no effect on (Kocher 1988) formalin-induced pain in mice and rats. The type of nociceptive response measured (flinching vs licking) (Wheeler-Aceto and Cowan 1993) and the strain of mice used (Vaccarino et al. 1988) appear to be key factors that probably account for the differences. In our study, naloxone (1 mg/kg, s.c.) did not modify formalin-induced pain, but completely antagonized the antinociception induced by a dose of morphine that produced a marked antinociceptive effect. These results agree with those of previous studies in CD-1 mice (the strain used in the present study) and other strains of mice and rats (North 1978; Kocher 1988; Vaccarino et al. 1988; Wang et al. 2005). Our results indicate that this dose of naloxone was able to block opioid-receptor-mediated antinociception in the formalin test (since the effect of morphine was antagonized), and that endogenous opioid tone in CD-1 mice is too low to tonically inhibit formalin-induced pain (since naloxone per se was devoid of effect). We also found that naloxone was unable to antagonize the antinociception induced by haloperidol and its metabolites in the formalin test, which suggests that the antinociception induced by these drugs is not due to the activation of opioid receptors or the modulation of the effect of endogenous opioid peptides.
Haloperidol has high affinity (K i=0.3–3 nM) for D2 and D3 receptors, and reduced haloperidol (metabolite II) also has affinity (K i around 100–250 nM) for these receptors (Table 1; Bowen et al. 1990; Jaen et al. 1993; Freedman et al. 1994). Therefore, their antinociceptive effect in the formalin test may be due to their action on these receptors. However, (−)sulpiride also shows high affinity (K i=6–20 nM) for D2 and D3 receptors (Freedman et al. 1994; Sokoloff et al. 1992), but was devoid of any antinociceptive activity, although it was administered at a dose much higher than those of haloperidol and reduced haloperidol. Furthermore, dopamine D2/D3 receptor agonists (but not antagonists) have been reported to produce antinociception in the formalin test (Morgan and Franklin 1991; Magnuson and Fisher 2000). Therefore, dopamine receptor antagonism seems unlikely to be involved in the antinociceptive effects of haloperidol and reduced haloperidol in the formalin test.
Antagonists of N-methyl-d-aspartate (NMDA) receptors inhibit formalin-induced pain, whereas agonists of these receptors produce the opposite effect (Coderre and Melzack 1992; Chaplan et al. 1997). In particular, NMDA receptors containing NR2B subunits play an important role in the expression of formalin-induced pain, as shown by the finding that transgenic mice with targeted overexpression of the NR2B subunit exhibited an enhanced pain response to formalin injection (Wei et al. 2001), whereas the intrathecal (i.t.) injection of small interfering RNA targeting the NR2B subunit of NMDA receptors abolished formalin-induced pain (Tan et al. 2005). Interestingly, NMDA receptors play a more important role in second- than in first-phase pain induced by formalin (Coderre and Melzack 1992; Chaplan et al. 1997), and in our study, the active drugs were also more potent and more efficacious in inhibiting the second phase of formalin-induced pain. Therefore, a theoretically possible explanation for our results is that haloperidol and its metabolites reduce formalin-induced pain either through direct binding and blockade of the NMDA receptor or through indirect modulation of NMDA-mediated effects.
Haloperidol displaces from neuronal membranes several radioligands that bind to NMDA receptors (such as [3H]TCP] and [3H]ifenprodil) (Yamamoto et al. 1995; Coughenour and Cordon 1997) and is able to block NMDA-induced membrane currents in cultured neurons and in Xenopus oocytes that express NMDA receptors containing NR2B subunits (Ilyin et al. 1996; Whittemore et al. 1997). Moreover, haloperidol and reduced haloperidol, but not sulpiride, displace [125I]MK-801 from native NMDA receptors in neuronal membranes and from HEK cells transfected with NMDA receptors that contain NR2B subunits (Shim et al. 1999). These data suggest that haloperidol and reduced haloperidol block NMDA receptors through direct binding to the receptor; this may explain their ability to reduce formalin-induced pain. However, this does not appear to be a plausible explanation for our results since, as summarized in Table 1, the affinity of haloperidol and reduced haloperidol for NMDA receptors is very low (K i in the μM range) (Whittemore et al. 1997; Coughenour and Cordon 1997) in comparison to their affinity for σ1 receptors, which is 1,000 times higher (nM range) (Bowen et al. 1990; Whittemore et al. 1997; Matsumoto and Pouw 2000). It seems unlikely that micromolar concentrations of any of these drugs were reached in vivo at the doses used in our experiments (the ED50 for second-phase pain was 0.07 mg/kg for haloperidol and 0.61 mg/kg for reduced haloperidol).
An alternative explanation for our results may be that haloperidol and its metabolites inhibit formalin-induced pain through indirect modulation of NMDA receptor-mediated effects. Agonists of the σ1 receptor enhance different effects mediated by NMDA receptors, such as the increase in neuronal firing rate induced by NMDA (Debonnel and Montigny 1996; Bergeron and Debonnel 1997), the enhancement of [3H]noradrenaline release induced by NMDA (Monnet et al. 1992a) and the increase in intracellular calcium concentration induced by the activation of NMDA receptors (Monnet et al. 2003). Haloperidol has a high affinity for σ1 receptors (Table 1; Jaen et al. 1993; Matsumoto and Pouw 2000) and inhibited the enhancement of NMDA effects induced by σ1 receptor agonists in vitro (Debonnel and Montigny 1996; Monnet et al. 1992a, 2003). In addition, an i.v. dose of haloperidol as low as 0.01 mg/kg antagonized the potentiation of NMDA effects induced by agonists of σ1 receptors in vivo (Monnet et al. 1992b, 1994; Bergeron and Debonnel 1997). Therefore, our results might be explained by the modulation of NMDA-mediated effects through an action of the drugs studied here on σ1 receptors. Several facts indirectly support this notion. All the drugs that showed affinity for σ1 receptors (haloperidol, haloperidol metabolites I and II) (Bowen et al. 1990; Jaen et al. 1993; Matsumoto and Pouw 2000) produced antinociception, whereas none of the drugs devoid of affinity for σ1 receptors [haloperidol metabolite III and (−)sulpiride] (Bowen et al. 1990; Matsumoto and Pouw 2000) had any antinociceptive effect (Table 1). Moreover, there was good correlation for the different drugs between potency of the observed antinociceptive effect [haloperidol > metabolite II > metabolite I ≫ metabolite III=(−)sulpiride=inactive] and their affinity for σ1 receptors (but not for σ2 or dopamine D2 receptors; Table 1).
Further indirect support for a role of σ1 receptors in the antinociceptive effect of haloperidol and its metabolites comes from the fact that the formalin-induced pain is reduced in σ1 receptor knockout mice (Cendan et al. 2005). However, it is important to note that the pain induced by formalin is reduced by approximately 55% in σ1 receptor knockout mice, whereas haloperidol and reduced haloperidol inhibited the effect of formalin by 90% or more. This finding suggests that other mechanisms in addition to σ1 receptor antagonism may be involved in the antinociceptive effect of these drugs in formalin tests. In this context, it should be recalled that σ2 receptor agonists are also able to enhance NMDA-mediated effects (Couture and Debonnel 1998; Gronier and Debonnel 1999), and that haloperidol and reduced haloperidol have affinity for σ2 receptors (Table 1; Matsumoto and Pouw 2000). Consequently, the antagonism of σ2 receptors might also play a role in the antinociceptive effect of these drugs. Moreover, it is tempting to speculate that the lack of effect of haloperidol metabolite I on σ2 receptors (Matsumoto and Pouw 2000) is related with the lower antinociceptive efficacy of this drug in comparison to haloperidol and reduced haloperidol. Obviously, further studies are necessary to evaluate the role of σ1 and σ2 receptors in the antinociception induced by haloperidol and its metabolites in the formalin test.
In conclusion, we found that haloperidol and its metabolites that have affinity for σ receptors dose-dependently inhibited formalin-induced pain, and that there is a good correlation between the affinity of these drugs for σ1 receptors and their potency to inhibit formalin-induced pain. We also conclude that further studies should be done to evaluate the possible antinociceptive effects of these drugs in other types of pain and to characterize the receptors involved in their antinociceptive effect.
References
Alonso G, Phan V, Guillemain I, Saunier M, Legrand A, Anoal M, Maurice T (2000) Immunocytochemical localization of the sigma(1) receptor in the adult rat central nervous system. Neuroscience 97:155–170
Bergeron R, Debonnel G (1997) Effects of low and high doses of selective sigma ligands: further evidence suggesting the existence of different subtypes of sigma receptors. Psychopharmacology (Berl) 129:215–224
Bowen WD, Moses EL, Tolentino PJ, Walker JM (1990) Metabolites of haloperidol display preferential activity at σ receptors compared to dopamine D-2 receptors. Eur J Pharmacol 177:111–118
Cendan CM, Pujalte JM, Portillo-Salido E, Montoliu L, Baeyens JM (2005) Formalin-induced pain is reduced in σ1 receptor knockout mice. Eur J Pharmacol 511:73–74
Chaplan SR, Malmberg AB, Yaksh TL (1997) Efficacy of spinal NMDA receptor antagonism in formalin hyperalgesia and nerve injury evoked allodynia in the rat. J Pharmacol Exp Ther 280:829–838
Chien CC, Pasternak GW (1994) Selective antagonism of opioid analgesia by a sigma system. J Pharmacol Exp Ther 271:1583–1590
Chien CC, Pasternak GW (1995) Sigma antagonists potentiate opioid analgesia in rats. Neurosci Lett 190:137–139
Coderre TJ, Melzack R (1992) The contribution of excitatory amino acids to central sensitization and persistent nociception after formalin-induced tissue injury. J Neurosci 12:3665–3670
Correa CR, Kyle DJ, Chakraverty S, Calixto JB (1996) Antinociceptive profile of the pseudopeptide B2 bradykinin receptor antagonist NPC 18688 in mice. Br J Pharmacol 117:552–558
Coughenour LL, Cordon JJ (1997) Characterization of haloperidol and trifluperidol as subtype-selective N-methyl-d-aspartate (NMDA) receptor antagonists using [3H]TCP and [3H]ifenprodil binding in rat brain membranes. J Pharmacol Exp Ther 280:584–592
Couture S, Debonnel G (1998) Modulation of the neuronal response to N-methyl-d-aspartate by selective sigma2 ligands. Synapse 29:62–71
Debonnel G, de Montigny C (1996) Modulation of NMDA and dopaminergic neurotransmissions by sigma ligands: possible implications for the treatment of psychiatric disorders. Life Sci 58:721–734
Dhawan BN, Cesselin F, Raghubir R, Reisine T, Bradley PB, Portoghese PS, Hamon M (1996) International Union of Pharmacology. XII. Classification of opioid receptors. Pharmacol Rev 48:567–592
Dykstra LA, Woods JH (1986) A tail withdrawal procedure for assessing analgesic activity in rhesus monkeys. J Pharmacol Methods 15:263–269
Fasmer OB, Berge OG, Hole K (1985) Changes in nociception after lesions of descending serotonergic pathways induced with 5,6-dihydroxytryptamine. Different effects in the formalin and tail-flick tests. Neuropharmacology 24:729–734
Freedman SB, Patel S, Marwood R, Emms F, Seabrook GR, Knowles MR, McAllister G (1994) Expression and pharmacological characterization of the human D3 dopamine receptor. J Pharmacol Exp Ther 268:417–426
Gronier B, Debonnel G (1999) Involvement of σ receptors in the modulation of the glutamatergic/NMDA neurotransmission in the dopaminergic systems. Eur J Pharmacol 368:183–196
Guitart X, Codony X, Monroy X (2004) Sigma receptors: biology and therapeutic potential. Psychopharmacology (Berl) 174:301–319
Hanner M, Moebius FF, Flandorfer A, Knaus HG, Striessnig J, Kempner E, Glossmann H (1996) Purification, molecular cloning, and expression of the mammalian sigma1-binding site. Proc Natl Acad Sci U S A 93:8072–8077
Ilyin VI, Whittemore ER, Guastella J, Weber E, Woodward RM (1996) Subtype-selective inhibition of N-methyl-d-aspartate receptors by haloperidol. Mol Pharmacol 50:1541–1550
Jaen JC, Caprathe BW, Pugsley TA, Wise LD, Akunne H (1993) Evaluation of the effects of the enantiomers of reduced haloperidol, azaperol, and related 4-amino-1-arylbutanols on dopamine and σ receptors. J Med Chem 36:3929–3936
Jett MF, McGuirk J, Waligora D, Hunter JC (1997) The effects of mexiletine, desipramine and fluoxetine in rat models involving central sensitization. Pain 69:161–169
King M, Pan YX, Mei J, Chang A, Xu J, Pasternak GW (1997) Enhanced κ-opioid receptor-mediated analgesia by antisense targeting the σ1 receptor. Eur J Pharmacol 331:R5–R6
Kitaichi K, Chabot JG, Moebius FF, Flandorfer A, Glossmann H, Quirion R (2000) Expression of the purported sigma1 (σ1) receptor in the mammalian brain and its possible relevance in deficits induced by antagonism of the NMDA receptor complex as revealed using an antisense strategy. J Chem Neuroanat 20:375–387
Kocher L (1988) Systemic naloxone does not affect pain-related behaviour in the formalin test in rat. Physiol Behav 43:265–268
Le Bars D, Gozariu M, Cadden SW (2001) Animal models of nociception. Pharmacol Rev 53:597–652
Magnusson JE, Fisher K (2000) The involvement of dopamine in nociception: the role of D1and D2 receptors in the dorsolateral striatum. Brain Res 855:260–266
Marder SR (1998) Antipsychotic medications. In: Schatzberg AF, Nemeroff CH (eds) The American Psychiatric Press textbook of psychopharmacology, 2nd edn. American Psychiatric Press Inc, Washington, pp 309–321
Martin M, Matifas A, Maldonado R, Kieffer BL (2003) Acute antinociceptive responses in single and combinatorial opioid receptor knockout mice: distinct mu, delta and kappa tones. Eur J Neurosci 17:701–708
Matsumoto RR, Pouw B (2000) Correlation between neuroleptic binding to σ1 and σ2 receptors and acute dystonic reactions. Eur J Pharmacol 401:155–160
Maurice T, Urani A, Phan VL, Romieu P (2001) The interaction between neuroactive steroids and the σ1 receptor function: behavioral consequences and therapeutic opportunities. Brain Res Rev 37:116–132
Mei J, Pasternak GW (2002) σ1 receptor modulation of opioid analgesia in the mouse. J Pharmacol Exp Ther 300:1070–1074
Millan MJ, Seguin L (1994) Chemically-diverse ligands at the glycine B site coupled to N-methyl-d-aspartate (NMDA) receptors selectively block the late phase of formalin-induced pain in mice. Neurosci Lett 178:139–143
Moncada A, Cendan CM, Baeyens JM, Del Pozo E (2003) Effects of serine/threonine protein phosphatase inhibitors on morphine-induced antinociception in the tail flick test in mice. Eur J Pharmacol 465:53–60
Monnet FP, Blier P, Debonnel G, de Montigny C (1992a) Modulation by sigma ligands of N-methyl-d-aspartate-induced [3H]noradrenaline release in the rat hippocampus: G-protein dependency. Naunyn-Schmiedeberg's Arch Pharmacol 346:32–39
Monnet FP, Debonnel G, de Montigny C (1992b) In vivo electrophysiological evidence for a selective modulation of N-methyl-d-aspartate-induced neuronal activation in rat CA3 dorsal hippocampus by sigma ligands. J Pharmacol Exp Ther 261:123–130
Monnet FP, Debonnel G, Bergeron R, Gronier B, de Montigny C (1994) The effects of sigma ligands and of neuropeptide Y on N-methyl-d-aspartate-induced neuronal activation of CA3 dorsal hippocampus neurones are differentially affected by pertussin toxin. Br J Pharmacol 112:709–715
Monnet FP, Morin-Surun MP, Leger J, Combettes L (2003) Protein kinase C-dependent potentiation of intracellular calcium influx by σ1 receptor agonists in rat hippocampal neurons. J Pharmacol Exp Ther 307:705–712
Morgan MJ, Franklin KB (1991) Dopamine receptor subtypes and formalin test analgesia. Pharmacol Biochem Behav 40:317–322
North MA (1978) Naloxone reversal of morphine analgesia but failure to alter reactivity to pain in the formalin test. Life Sci 22:295–302
Ossipov MH, Kovelowski CJ, Wheeler-Aceto H, Cowan A, Hunter JC, Lai J, Malan TP Jr, Porreca F (1996) Opioid antagonists and antisera to endogenous opioids increase the nociceptive response to formalin: demonstration of an opioid kappa and delta inhibitory tone. J Pharmacol Exp Ther 277:784–788
Pan YX, Mei J, Xu J, Wan BL, Zuckerman A, Pasternak GW (1998) Cloning and characterization of a mouse σ1 receptor. J Neurochem 70:2279–2285
Quirion R, Bowen WD, Itzhak Y, Junien JL, Musacchio JM, Rothman RB, Su TP, Tam SW, Taylor DP (1992) A proposal for the classification of sigma binding sites. Trends Pharmacol Sci 13:85–86
Raft D, Toomey T, Gregg JM (1979) Behavior modification and haloperidol in chronic facial pain. South Med J 72:155–159
Ryan SM, Watkins LR, Mayer DJ, Maier SF (1985) Spinal pain suppression mechanisms may differ for phasic and tonic pain. Brain Res 334:172–175
Seth P, Leibach FH, Ganapathy V (1997) Cloning and structural analysis of the cDNA and the gene encoding the murine type 1 sigma receptor. Biochem Biophys Res Commun 241:535–540
Shibata M, Ohkubo T, Takahashi H, Inoki R (1989) Modified formalin test: characteristic biphasic pain response. Pain 38:347–352
Shim SS, Grant ER, Singh S, Gallagher MJ, Lynch DR (1999) Actions of butyrophenones and other antipsychotic agents at NMDA receptors: relationship with clinical effects and structural considerations. Neurochem Int 34:167–175
Shimoyama N, Shimoyama M, Davis AM, Inturrisi CE, Elliott KJ (1997) Spinal gabapentin is antinociceptive in the rat formalin test. Neurosci Lett 222:65–67
Sokoloff P, Andrieux M, Besancon R, Pilon C, Martres MP, Giros B, Schwartz JC (1992) Pharmacology of human dopamine D3 receptor expressed in a mammalian cell line: comparison with D2 receptor. Eur J Pharmacol 225:331–337
Tan PH, Yang LC, Shih HC, Lan KC, Cheng JT (2005) Gene knockdown with intrathecal siRNA of NMDA receptor NR2B subunit reduces formalin-induced nociception in the rat. Gene Ther 12:59–66
Vaccarino AL, Tasker RA, Melzack R (1988) Systemic administration of naloxone produces analgesia in BALB/c mice in the formalin pain test. Neurosci Lett 84:103–107
Vaccarino AL, Tasker RA, Melzack R (1989) Analgesia produced by normal doses of opioid antagonists alone and in combination with morphine. Pain 36:103–109
Vissers K, Hoffmann V, Geenen F, Biermans R, Meert T (2003) Is the second phase of the formalin test useful to predict activity in chronic constriction injury models? A pharmacological comparison in different species. Pain Pract 3:298–309
Walker JM, Bowen WD, Walker FO, Matsumoto RR, De Costa B, Rice KC (1990) Sigma receptors: biology and function. Pharmacol Rev 42:355–402
Wang Y, Su DM, Wang RH, Liu Y, Wang H (2005) Antinociceptive effects of choline against acute and inflammatory pain. Neuroscience 132:49–56
Wei F, Wang GD, Kerchner GA, Kim SJ, Xu HM, Chen ZF, Zhuo M (2001) Genetic enhancement of inflammatory pain by forebrain NR2B overexpression. Nat Neurosci 4:164–169
Wheeler-Aceto H, Cowan A (1993) Naloxone causes apparent antinociception and pronociception simultaneously in the rat paw formalin test. Eur J Pharmacol 236:193–199
Whittemore ER, Ilyin VI, Woodward RM (1997) Antagonism of N-methyl-d-aspartate receptors by σ site ligands: potency, subtype-selectivity and mechanisms of inhibition. J Pharmacol Exp Ther 282:326–338
Wu HE, Hung KC, Mizoguchi H, Nagase H, Tseng LF (2002) Roles of endogenous opioid peptides in modulation of nocifensive response to formalin. J Pharmacol Exp Ther 300:647–654
Yamamoto H, Yamamoto T, Sagi N, Klenerova V, Goji K, Kawai N, Baba A, Takamori E, Moroji T (1995) Sigma ligands indirectly modulate the NMDA receptor–ion channel complex on intact neuronal cells via σ1 site. J Neurosci 15:731–736
Zimmer A, Zimmer AM, Baffi J, Usdin T, Reynolds K, Konig M, Palkovits M, Mezey E (1998) Hypoalgesia in mice with a targeted deletion of the tachykinin 1 gene. Proc Natl Acad Sci U S A 95:2630–2635
Zimmermann M (1983) Ethical guidelines for investigations of experimental pain in conscious animals. Pain 16:109–110
Acknowledgements
This study was supported in part by a grant from the Junta de Andalucía (CTS 109). We thank K. Shashok for revising the English style of the manuscript and Anke Kröner (visiting scientist from the Faculty of Medical Sciences of Groningen University) for her help in obtaining some of the data.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cendán, C.M., Pujalte, J.M., Portillo-Salido, E. et al. Antinociceptive effects of haloperidol and its metabolites in the formalin test in mice. Psychopharmacology 182, 485–493 (2005). https://doi.org/10.1007/s00213-005-0127-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-005-0127-z