Abstract
Evidence shows that the N-methyl-d-aspartate (NMDA) antagonist MK801 reduces the development of morphine (Mor) tolerance. The paraventricular nucleus of the thalamus (PVT) comprises the highest levels of μ-opioid receptors in the thalamus and is involved in pain modulation. The present study examined whether blocking NMDA receptors by administration of MK801 in the PVT nucleus could affect the nociceptive behavioral manifestations caused by the formalin in Mor-dependent rats. Male Wistar rats weighing 250–300 g were dependent on Mor by subcutaneously (s.c.) injection (6, 16, 26, 36, 46, 56, and 66 mg/kg, 2 ml/kg) at an interval of 24 h for 7 days. Animals were randomized into four experimental groups in which the NMDA receptor antagonist, MK801 (20 mM in 0.1 ml), or its vehicle were injected into the PVT nucleus for 7 days before each Mor injection. On day 8, the formalin test was carried out. Results showed that repetitive Mor administration prompted antinociception in interphase and phase II of formalin test. Also, inhibition of NMDA receptors decreased formalin-induced nociceptive behaviors in all phases of the test in Mor-dependent rats. Our findings suggested that continuous co-administration of MK801 into PVT with Mor could enhance the antinociceptive effect of Mor and reduce the nociceptive behaviors prompted by formalin in Mor-dependent rats.
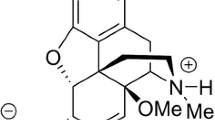
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The thalamus is one of the places that receive projections from multiple ascending pain pathways. This structure is involved in the processing of nociceptive information before conveying the information to different parts of the cortex [1, 34]. The PVT in humans and rats comprises the primary levels of μ-opioid receptors in the thalamus [10, 24] and comprises a high aggregation of thalamic fibers with the endogenous μ-opioid receptor ligands [36]. Following noxious stimulation, the initiation of c-fos expression has been revealed in the thalamic PVT nucleus [7, 8, 12]. Mor enhances basal PVT neuronal firing. The intrinsic excitability of PVT neurons is increased by Mor [27]. Initiation of the μ-opioid receptor activity in PVT diminishes physical pain and may also control social pain. The firing of PVT neurons is inhibited by the activation of μ-opioid receptors in this nucleus [5]. Furthermore, it is revealed that frequent Mor injection enhances the spontaneous firing of PVT neurons along with augmentation of PVT neuronal excitability and excitatory synaptic glutamatergic transmission [27].
It is known that the PVT consists primarily of glutamatergic neurons [9, 30]. Evidence has shown that NMDA receptors are implicated in nociceptive transmission in the thalamus [11, 33]. Though NMDA receptor subunits have been detected in the medial thalamus [6] and NMDA inactivation has a significant role in drug addiction, the inhibition of NMDA receptors on nociception in the PVT nucleus has not been established and needs further investigation. Therefore, our attention was attracted by the question of whether intra-PVT administration of NMDA antagonism has a significant effect on nociceptive behaviors in Mor-dependent rats.
Materials and methods
Animals
Male Wistar rats, weighing 250–300 g were purchased from the Iran University of Medical Sciences and kept in plexiglass breeding cages with free access to water and food. Animals were kept in a colony room at constant room temperature and 12 h dark and light cycles. All experiments were carried out at 7–9 a.m. to evade any bias induced by circadian rhythm.
Ethics declarations
The current research was achieved based on the ethical rules of Iran University of Medical Sciences Ethics Committee, Tehran, Iran, which is based on the NIH Guide for the Care and Use of Laboratory Animals.
Stereotaxic surgery and cannulation
The rats anesthetized by ketamine (100 mg/kg, i.p.) and xylazine (10 mg/kg, i.p.). then, bregma was identified as the coordinates taken from Paxinos and Watson’s rat brain atlas by a stereotaxic device [31]. The coordinates for the PVT were 3.1 mm posterior to bregma, 1.3 mm lateral to the midline, and 4.0 mm ventral to the skull, with the incisor bar set at 3.3 mm below the intraaural line [23]. Then, a stainless-steel guide cannula (23-gauge needle) was unilaterally placed at the depth of 1 mm above the PVT and was fixed by means of dental acrylic cement and two screws [2]. Animals were allowed to recover after the operation for 7 days.
Rats were randomly assigned to four groups (n = 32): Group 1: Animals received a subcutaneous injection of saline at an interval of 24 h for 7 days (Sal, n = 8). Group 2: Animals received a subcutaneous injection of Mor at an interval of 24 h for 7 days (Mor, n = 8). Groups 3 and 4, animals received intra-PVT microinjection of MK801 (20 mM in 0.1 ml, n = 8, MK. Mor), or its vehicle (Sal.Mor, n = 8), respectively, for 7 days before each Mor injection.
Induction of Mor dependence and formalin test
To induce Mor dependence, Mor was injected (6, 16, 26, 36, 46, 56, and 66 mg/kg, 2 ml/kg) for 7 days [18, 32]. On day 8, formalin (50 μL of 2%) was injected and nociceptive behaviors were observed and calculated for 30 min in a transparent plexiglass chamber. Injections were achieved at the same time during the experiments.
Intra-PVT microinjection
The non-NMDA receptor antagonist or dizocilpine hydrogen malate (MK801) (20 mM) solved in 0.1 ml sterile saline (5 µg solved in 1.0-µl sterile saline [18, 35]. The solution was divided into portions and then frozen in − 20 °C. MK801 and its vehicle were injected into PVT prior to each Mor injection through an injection cannula that was connected to hamilton syringes with volume of 1 μl by a 20 cm polyethylene tube (PE-20). A 30-gauge needle, the length of which was 1 mm longer than the guide cannula, was applied for injection. Drugs were microinjected for 60 s, and the microinjection needles were left at the site of injection for a further 60 s before being taken out [25].
MK801 is a selective non-competitive NMDA receptor antagonist. It inhibits NMDA-induced excitation by interacting with open ion channels associated with NMDA receptors [21, 22].
Histological verification
After each test, the correct placement of the cannula tips was verified histologically. For this purpose, animals were deeply anesthetized by urethane (1.5 g/kg, i.p.). Afterward, pontamine sky blue (2%, 0.2 μl) dye was microinjected into the PVT nucleus. Then rats were sacrificed, the brains were removed, and kept in a solution of 10% phosphate-buffered formalin for 24 h. The fixed tissues were sectioned into 300-μm-thick slices and injection sites were verified histologically by the rat brain atlas of Paxinos and Watson [31] (Fig. 1). Rats with misplaced cannula were excluded from the analysis.
Evaluation of nociceptive behaviors in Mor-dependent rat using formalin test
Formalin tests were achieved in the Plexiglas chamber (30 × 30 × 30 cm) with a mirror located below at a 45° angle to provide an unimpeded view of the animals’ paws.
In the current research, initially, rats were acclimatized for 30 min in an acrylic observation chamber. Afterward, 10 to 20 min after the last injection of Mor, formalin (50 μl;s.c.; 2%) was injected subcutaneously through a 25-gauge needle into the plantar surface of the right hind paw.
The stable scores from formalin were ensured by inserting the needle 5 mm under the skin. Subsequently, each rat was immediately returned to the observation box, and behavioral recording was commenced. Pain behaviors were scored as follows: 0 = the injected paw was not favored, 1 = the injected paw had little or no weight placed on it, 2 = the injected paw was increased and not in contact with any surface, and 3 = the injected paw was licked or bitten. Recording of nociceptive behaviors began immediately after formalin injection (time 0) and was continued for 60 min. The length of licking/biting the formalin-injected hind paw during each phase was assessed by a digital time-out stopwatch as an indicator of the pain response. In all groups, the behavioral response of rats during the first phase, interphase, and second phase were separately measured. The behavioral assessment was achieved just once for each animal, i.e., the formalin was never injected into the same animal twice [29, 37].
Injection of formalin induces a biphasic nociceptive and active response, including an early phase (0–5 min), quiescent interphase (5–20), and a second long-lasting phase (20–60 min). To confirm stable scores from formalin, it was required to be sure that the needle was inserted through the skin and run for 5 mm under the skin. Afterward, each rat was directly returned to the observation box, and behavioral recording started. Nociceptive behaviors were scored as follows: 0, the injected paw was not favored;1, the injected paw had little or no weight placed on it; 2, the injected paw was raised up and not in contact with any surface; and 3, the injected paw was licked or bitten. Recording of pain behaviors commenced immediately after formalin injection (time 0) and was sustained for 60 min.
Data analysis
Data were expressed as mean ± SEM and analyzed using unpaired two-tailed Student’s t test for comparison of two groups by prism software. The defined level of statistical significance was p < 0.05.
Results
To study the effect of tolerance to the analgesic effect of Mor, we used the formalin test, the nociceptive score was measured in different phases (phases I, II, and interphase) of the formalin test.
To examine the impact of Mor in the induction of tolerance formalin-induced pain was used. The nociceptive score was evaluated in each phase of the pain evoked by formalin (phase I, interphase, and II). Mor failed to alter pain behaviors evoked by formalin in phase I. In interphase and phase II, Mor could reduce the nociception (analyzed by unpaired t test, Fig. 2).
Formalin-induced nociceptive behaviors following the infusion of Mor. Upper schematic plan demonstrates the experimental protocols used for assessment of nociceptive behaviors in Mor-dependent rats. Bar chart for injection of Mor (Mor) in the formalin-induced pain represents mean of the nociceptive score in each phase: phase 1 (minutes 0–5), interphase (minutes 5–20), and phase 2 (minutes 20–60). Recording of nociceptive behaviors began immediately for 60 min after formalin injection (50 μl, s.c.; 2%) into the hind paw (minute 0). Data are expressed as mean ± SEM. *p < 0.05 in comparison with saline (Sal) group, n = 8 per group
We found that the pain behaviors created by formalin in Mor-treated rats decreased by the chronic application of MK801 in phase I (p < 0.05), interphase (p < 0.01), and phase II (p < 0.0001) (analyzed by unpaired t test, Fig. 3).
Formalin-induced nociceptive behaviors following infusion of MK801. Upper schematic design shows the experimental protocols used for measuring nociceptive behaviors following MK801 injection in Mor-dependent rats. The mean of the nociceptive score for injection of MK801 in the formalin test in each phase: phase 1 (minutes 0–5), interphase (minutes 5–20), and phase 2 (minutes 20–60). Recording of the nociceptive behaviors began immediately after formalin (50 μl, s.c.; 2%) injection into the hind paw (time 0) and was continued for 60 min. Data are analyzed by unpaired t test and expressed as mean ± SEM. *p < 0.05, **p < 0.01, *** p < 0.0001 in comparison with vehicle, n = 8 per group
These results propose that NMDA receptors are important mediators of the development of long-lasting, non-associative Mor effect. The increment of Mor’s antinociceptive influences by MK801 recommends the exciting likelihood that the NMDA receptor activity may exert nociception.
Discussion
The current results displayed that the pain behavior in rats who received repeated Mor failed to have any significant difference compared to the saline-treated rats in phase I of the formalin test. This suggests that the absence of analgesia caused by the long-standing application of Mor in the current study might result from the development of tolerance in phase I. The pain behavior in rats who received repeated Mor exhibited significant reduction compared to the saline-treated rats in interphase and phase II of the formalin test that was consistent with our previous study [19].
Our findings also showed that long-term injection of MK801 into the PVT significantly decreased the nociceptive behaviors in all phases of the formalin test in Mor-dependent rats. Consistent with our study, previous studies have shown that NMDA receptors have a considerable role in the development and expression of opioid physical dependence [3]. It has been demonstrated that MK801 blocks Mor dependence and inhibits the behavioral symptoms of the Mor abstinence syndrome [22].
The reduction of nociceptive behaviors observed in MK801-treated animals during the experiment is consistent with previous ideas that this drug blocks the development of opiate dependence. These results illustrate that the development of opiate dependence, similar to other kinds of plasticity [17, 20] comprises NMDA receptor activation. Gutstein et al. demonstrated that MK801 attenuates the development of Mor dependence at spinal sites [14]. Therefore, NMDA receptors are largely implicated in opiate-induced plasticity and the development of opiate dependency [28].
Current findings propose that NMDA-type glutamate receptor-mediated neurotransmission exhibits important impact on the antinociception induction following continuing opioid administration. In previous studies, it has been shown that the activation of NMDA receptors has been accompanying with hyperalgesia, neuropathic pain, and reduced functionality of opioid receptors [4]. Hyperalgesia may induced by augmented spinal neuron sensitization, resulting in an increment of pain [16]. Furthermore, in another study, the essential role of NMDA receptor in the central sensitization of spinal cord dorsal horn has been demonstrated [15]. This assumption is consistent with evidence that showed an augmentation of intracellular calcium concentration by NMDA receptor activation. Increased intracellular calcium and calcium-calmodulin dependent kinases activity can cause uncoupling of receptor-G-protein implicated in sensitization of mu-opioid receptor [13]. Furthermore, the continued analgesia by co-use of Mor and an NMDA antagonist demonstrated the prolongation of the analgesic effect of an opioid [26].
Conclusion
In conclusion, current findings demonstrated that NMDA receptors in the PVT nucleus seem to act either directly or indirectly on the signaling pathways of Mor to exhibit a reasonable path for the development of Mor dependence and demonstrate an innovative potential therapeutic goal in the treatment of pain. Therefore, it may be concluded that NMDA receptors has the capability to block the non-associative opiate tolerance at the thalamus level. Indeed, MK801 might have changed the development of dependence and enhance the analgesic effect of Mor when administered along with each Mor injection. Nevertheless, additional in vitro and in vivo studies are required to clarify how the NMDA receptors play a role in pain modification.
Data availability
Data will be made available upon request.
References
Ab Aziz, C. B. and A. H. Ahmad (2006). “The role of the thalamus in modulating pain”. The Malaysian journal of medical sciences: MJMS 13(2): 11.
Babaie, F., M. Kourosh-Arami and M. Farhadi (2022). “Administration of orexin-A into the rat thalamic paraventricular nucleus enhances the naloxone induced morphine withdrawal”. Drug Research 72(04): 209-214.
Bell, J. A. and C. L. Beglan (1995). “Co-treatment with MK-801 potentiates naloxone-predpitated morphine withdrawal in the isolated spinal cord of the neonatal rat”. European journal of pharmacology 294(1): 297-301.
Bennett, G. J. (2000). “Update on the neurophysiology of pain transmission and modulation: focus on the NMDA-receptor”. Journal of pain and symptom management 19(1): 2-6.
Brunton, J. and S. Charpak (1998). “μ-Opioid peptides inhibit thalamic neurons”. Journal of Neuroscience 18(5): 1671-1678.
Buller, A. L., H. C. Larson, B. E. Schneider, J. A. Beaton, R. A. Morrisett and D. T. Monaghan (1994). “The molecular basis of NMDA receptor subtypes: native receptor diversity is predicted by subunit composition”. Journal of Neuroscience 14(9): 5471-5484.
Bullitt, E. (1989). “Induction of c-fos-like protein within the lumbar spinal cord and thalamus of the rat following peripheral stimulation”. Brain research 493(2): 391-397.
Ceccarelli, I., A. Scaramuzzino, C. Massafra and A. M. Aloisi (2003). “The behavioral and neuronal effects induced by repetitive nociceptive stimulation are affected by gonadal hormones in male rats”. Pain 104(1-2): 35-47.
Csaki, A., K. Kocsis, B. Halasz and J. Kiss (2000). “Localization of glutamatergic/aspartatergic neurons projecting to the hypothalamic paraventricular nucleus studied by retrograde transport of [3H] D-aspartate autoradiography”. Neuroscience 101(3): 637-655.
Ding, Y. Q., T. Kaneko, S. Nomura and N. Mizuno (1996). “Immunohistochemical localization of μ-opioid receptors in the central nervous system of the rat”. Journal of Comparative Neurology 367(3): 375-402.
Dougherty, P. M., Y.-J. Li, F. Lenz, L. Rowland and S. Mittman (1996). “Evidence that excitatory amino acids mediate afferent input to the primate somatosensory thalamus”. Brain research 728(2): 267-273.
Erdos, B., Z. Lacza, I. E. Toth, E. Szelke, T. Mersich, K. Komjati, M. Palkovits and P. Sandor (2003). “Mechanisms of pain-induced local cerebral blood flow changes in the rat sensory cortex and thalamus”. Brain research 960(1-2): 219-227.
Garzón, J., M. Rodríguez-Muñoz and P. Sánchez-Blázquez (2008). “Do pharmacological approaches that prevent opioid tolerance target different elements in the same regulatory machinery?” Current drug abuse reviews 1(2): 222-238.
Gutstein, H. B. and K. A. Trujillo (1993). “MK-801 inhibits the development of morphine tolerance at spinal sites”. Brain research 626(1-2): 332-334.
Inturrisi, C. (2005). “The role of N-methyl-D-aspartate (NMDA) receptors in pain and morphine tolerance”. Minerva anestesiologica 71(7-8): 401-403.
Jamero, D., A. Borghol, N. Vo and F. Hawawini (2011). “The emerging role of NMDA antagonists in pain management”. US Pharm 36(5).
Komaki A, S. Shahidi, A. Sarihi, P. Hasanein, R. Lashgari, A. Haghparast, I. Salehi, M. K. Arami (2013). Effects of neonatal C-fiber depletion on interaction between neocortical short-term and long-term plasticity. Basic and clinical neuroscience 4(2): 136.
Kourosh-Arami, M., M. Javan and S. Semnanian (2020). “Inhibition of orexin receptor 1 contributes to the development of morphine dependence via attenuation of cAMP response element-binding protein and phospholipase Cβ3”. Journal of Chemical Neuroanatomy 108: 101801.
Kourosh-Arami, M., M.-T. Joghataei, A. Komaki, M. Gholami, Z. Najafi and M. Lavaie (2021). “Persistent effects of the orexin-1 receptor antagonist SB-334867 on naloxone precipitated morphine withdrawal symptoms and nociceptive behaviors in morphine dependent rats”. International Journal of Neuroscience 132(1): 67-76.
Kourosh-Arami, M., A. Komaki and M. Gholami (2022). “Addiction-induced plasticity in underlying neural circuits”. Neurological Sciences 43(3): 1605-1615.
Kourosh-Arami M., M. Soleimani, M. T. Joghataei, F. Mosleh, P. Hayatand A. Komaki (2022). Upregulation of connexins in the rat hippocampal and cortical neurons following blockade of NMDA receptors during postnatal development. Protein and Peptide Letters.
Koyuncuoǧlu, H., Y. Dizdar, F. Aricioǧlu and Ü. Sayin (1992). “Effects of MK 801 on morphine physical dependence: attenuation and intensification”. Pharmacology Biochemistry and Behavior 43(2): 487-490.
Li, Y., S. Li, C. Wei, H. Wang, N. Sui and G. J. Kirouac (2010). “Orexins in the paraventricular nucleus of the thalamus mediate anxiety-like responses in rats”. Psychopharmacology 212(2): 251-265.
Majidinezhad, M., H. Amirteymouri, S. Karimi-Haghighi, M. Kourosh-Arami and A. Haghparast (2022). “Orexin system in the ventral tegmental area is implicated in the rewarding properties of methamphetamine”. European Journal of Pharmacology 930: 175170.
Malakouti, S. M., M. Kourosh Arami, A. A. R. Sarihi, S. Hajizadeh, G. Behzadi, S. Shahidi, A. R. KOMAKI, B. Heshmatian, and M. Vahabian (2008). “Reversible inactivation and excitation of nucleus raphe magnus can modulate tail blood flow of male wistar rats in response to hypothermia” 237-240.
Manning, B. H., J. Mao, H. Frenk, D. D. Price and D. J. Mayer (1996). “Continuous co-administration of dextromethorphan or MK-801 with morphine: attenuation of morphine dependence and naloxone-reversible attenuation of morphine tolerance”. Pain 67(1): 79-88.
McDevitt, D. S. and N. M. Graziane (2019). “Timing of morphine administration differentially alters paraventricular thalamic neuron activity”. Eneuro 6(6): e0377-19.
Mendez, I. A. and K. A. Trujillo (2008). “NMDA receptor antagonists inhibit opiate antinociceptive tolerance and locomotor sensitization in rats”. Psychopharmacology 196(3): 497-509.
Mobarakeh, J. I., K. Takahashi, S. Sakurada, S. Nishino, H. Watanabe, M. Kato and K. Yanai (2005). “Enhanced antinociception by intracerebroventricularly and intrathecally-administered orexin A and B (hypocretin-1 and-2) in mice”. Peptides 26(5): 767-777.
Myers, B., C. M. Dolgas, J. Kasckow, W. E. Cullinan and J. P. Herman (2014). “Central stress-integrative circuits: forebrain glutamatergic and GABAergic projections to the dorsomedial hypothalamus, medial preoptic area, and bed nucleus of the stria terminalis”. Brain Structure and Function 219(4): 1287-1303.
Paxinos, G. and C. Watson (1998). “A stereotaxic atlas of the rat brain”. New York: Academic.
Rezaei, Z., M. Kourosh-Arami, H. Azizi and S. Semnanian (2020). “Orexin type-1 receptor inhibition in the rat lateral paragigantocellularis nucleus attenuates development of morphine dependence”. Neuroscience Letters 724: 134875.
Salt, T. and S. Eaton (1989). “Function of non-NMDA receptors and NMDA receptors in synaptic responses to natural somatosensory stimulation in the ventrobasal thalamus”. Experimental brain research 77(3): 646-652.
Samani, F. and M. K. Arami (2022). “Repeated administration of orexin into the thalamic paraventricular nucleus inhibits the development of morphine-induced analgesia”. Protein and Peptide Letters 29(1): 57-63.
St-Pierre, J. and P. Bedard (1994). “Intranigral but not intrastriatal microinjection of the NMDA antagonist MK-801 induces contralateral circling in the 6-OHDA rat model”. Brain research 660(2): 255-260.
Uroz, V., L. Prensa and J. M. Giménez-Amaya (2004). “Chemical anatomy of the human paraventricular thalamic nucleus”. Synapse 51(3): 173-185.
Zarmehri, H. A., S. Semnanian, Y. Fathollahi, E. Erami, R. Khakpay, H. Azizi and K. Rohampour (2011). “Intra-periaqueductal gray matter microinjection of orexin-A decreases formalin-induced nociceptive behaviors in adult male rats”. The Journal of Pain 12(2): 280-287.
Acknowledgements
This work is supported by the Neuroscience Research Center of the Iran University of Medical Sciences.
Author information
Authors and Affiliations
Contributions
FS, MKA, and MF were responsible for the study concept and design. FS performed the experiments. MKA was responsible for provision of study materials and equipment, study validation, and supervision. MKA and MF assisted with data analysis and interpretation of findings. MKA drafted the manuscript. All authors critically reviewed content and approved final version for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Samani, F., Arami, M.K. & Farhadi, M. Role of NMDA receptors blockade in the thalamic paraventricular nucleus in morphine dependent rat model of formalin-induced pain. Neurosci Behav Physi 53, 670–677 (2023). https://doi.org/10.1007/s11055-023-01343-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11055-023-01343-6