Abstract
Rationale
Clozapine inhibits sympathetic outflow to the cutaneous vascular bed. Clozapine reverses hyperthermia and cutaneous vasoconstriction induced by 3,4-methylenedioxymethamphetamine (MDMA, Ecstasy) or by lipopolysaccharide (LPS). Clozapine also reverses cutaneous vasoconstriction elicited by exposure to cold. These actions distinguish clozapine from haloperidol. Clozapine could also inhibit sympathetic cutaneous vasomotor alerting responses (SCVARs), vasoconstrictor episodes that reflect emotional/psychological function, and this property might also distinguish clozapine from haloperidol.
Objectives
Experiments in rats determined whether clozapine and haloperidol inhibit SCVARs, and whether SR46349B (a 5HT2A receptor antagonist), 8-OH-DPAT (a 5-HT1A agonist), L741,626 (a dopamine D2 antagonist) or SCH23390 (a dopamine D1 antagonist) have clozapine-like effects on SCVARs.
Methods
Mean level and pulse amplitude of the tail artery Doppler flow signal were recorded in conscious freely moving rats before and after alerting stimuli (e.g. tapping the cage), and expressed as a SCVAR index (fall to zero flow implies SCVAR index of 100%, no fall implies 0%).
Results
Clozapine (0.0625–1.0 mg/kg, s.c.) dose-dependently increased resting tail blood flow. After 1 mg/kg, the SCVAR index was 18±1%, compared with 83±2% after vehicle. SR46349B (0.01–1.0 mg/kg) and 8-OH-DPAT (0.25 mg/kg) had similar but less potent effects on cutaneous blood flow and on SCVARs. Haloperidol (0.005–0.5 mg/kg) and L741,626 (1 mg/kg) had no or little effect on these variables. SCH23390 mildly inhibited SCVARs.
Conclusions
Clozapine, but not haloperidol, increases resting cutaneous blood flow and decreases SCVARs. Antagonism at 5-HT2A receptors and agonism at 5-HT1A receptors could contribute to these actions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Clozapine, a drug of major theoretical and practical importance in the treatment of schizophrenia (Meltzer 2002; Meltzer et al. 2003; Tauscher et al. 2004), lowers body temperature (Heh et al. 1988; Millan et al. 1995; Oerther and Ahlenius 2000; Salmi and Ahlenius 1996; Salmi et al. 1994). Clozapine interacts as an agonist or as an antagonist at a range of neurotransmitter receptors (Arnt and Skarsfeldt 1998), so that mechanisms underlying clozapine's hypothermic action have not been easy to identify. Similarly, there is no consensus on the receptor mechanisms underlying clozapine's psychotherapeutic action. Because the drug “remains unique in its efficiency in the treatment of refractory schizophrenia” (Tauscher et al. 2004), elucidation of mechanisms underlying any identifiable physiological actions of clozapine is an important task.
Body temperature is a composite variable, reflecting a balance between the processes of heat production and heat loss, and these are themselves net summations of more basic physiological processes. Cutaneous blood flow is one such process. Variations in cutaneous blood flow modulate heat transfer to the environment. By measuring cutaneous blood flow in conscious freely moving rabbits (ear pinna blood flow) and rats (tail blood flow), and by direct recordings from sympathetic cutaneous vasomotor nerves in anesthetized animals, our laboratory has demonstrated that lowering of body temperature by clozapine is at least partially mediated by its remarkable ability to inhibit sympathetic outflow to the cutaneous vascular bed. Clozapine and olanzapine (a clozapine-like antipsychotic drug) reverse sympathetically mediated cutaneous vasoconstriction and hyperthermia elicited by MDMA (Blessing et al. 2003; Pedersen and Blessing 2001). Clozapine's cutaneous sympathoinhibitory action is so robust that it reverses cutaneous vasoconstriction induced physiologically by exposure to a cold environment; in this situation, clozapine-treated animals can no longer conserve heat and body temperature falls (Blessing 2004b). Clozapine and olanzapine also reverse cutaneous vasoconstriction and hyperthermia occurring as part of the acute febrile response elicited by lipopolysaccharide (LPS) (Blessing 2004b). Haloperidol (a conventional antipsychotic drug) does not affect cutaneous blood flow or body temperature in these situations (Blessing 2004b; Schmidt et al. 1990).
Sympathetic outflow to the cutaneous vascular bed is suddenly and selectively activated when the individual detects salient, potentially dangerous or stressful, alerting environmental events, so that the resulting sudden falls in cutaneous blood flow are linked to the onset of alerting-arousal rhythms in the hippocampal EEG (Yu and Blessing 1997). I propose that these specifically patterned autonomic events be called SCVARs (sympathetic cutaneous vasomotor alerting responses). If SCVARs occurred in a sustained fashion, especially during a period of increased heat production, they could contribute to a rise in body temperature. Apart from the general concept of “stress-induced hyperthermia”, any rationale for a link between body temperature and psychological function has previously been obscure. SCVARs could provide the rationale for this link (see Discussion section).
Experiments reported in the present study determined whether clozapine and/or haloperidol inhibit SCVARs, assessed by measuring sudden alerting-related changes in blood flow in the tail artery bed of the conscious unrestrained rat. Further similarly designed experiments examined the cutaneous blood flow and SCVAR effects of drugs that interact with 5-hydroxytryptamine (5-HT) receptors, particularly the specific 5-HT1A receptor agonist 8-OH-DPAT (Arvidsson et al. 1987) and the specific 5-HT2A receptor antagonist SR46349B (Rinaldi-Carmona et al. 1992). This pattern of 5-HT receptor interaction is considered important in the manner whereby atypical antipsychotics exert their effects on dopaminergic neurotransmission (Meltzer et al. 2003). Finally, the cutaneous blood flow and SCVAR effects of dopamine D1 and D2 receptor antagonism were assessed using SCH23390 (Faunt and Crocker 1987; Hartman et al. 1996) and L741,626 (Kulagowski et al. 1996), respectively. Results from these studies might be relevant to the controversy concerning the role of D1 and D2 receptor interactions in the psychotherapeutic actions of clozapine in comparison with haloperidol (Kapur and Seeman 2001; Meltzer 2002; Tauscher et al. 2004).
Materials and methods
Experiments, conducted according to protocols approved by the Flinders University Animal Welfare Committee, were performed on Sprague–Dawley rats (300–500 g), instrumented (halothane general anesthesia) with a chronically implanted Doppler ultrasonic flow probe (Iowa Doppler Products, Iowa, USA) around the base of the tail artery (Garcia et al. 2001). Probe wires were passed subcutaneously and attached to a head socket. A telemetric temperature probe (Data Sciences International, St Paul, MN USA) was positioned in the peritoneal cavity. After at least a 1-week recovery period, tail artery blood flow and body temperature were measured in conscious unrestrained animals, which were placed in a special cage (cubic wooden box, 40 cm sides, fitted with a swivel device, light-proof, not sound-proof). The animal was kept in this cage (temperature 22–24°C) overnight before an experiment. An hour before an experiment, temperature was increased to 24–29°C by means of an internal light and a heating pad. Tail artery blood flow Doppler signal, body and cage temperature were continuously recorded, digitized and displayed on a Macintosh computer with PowerLab and Chart (ADInstruments, Sydney, Australia).
Tail Doppler blood flow signal for the 20-min period immediately preceding injection of vehicle or drug was used as a control. The cage was then opened and either vehicle (0.5 ml of acidified Ringer) or drug was injected either s.c. or i.p. The animal was then left undisturbed for 30 min and the tail Doppler flow signal from the last 20 min of this period was selected for analysis of resting flow parameters (see below).
The rat was then subjected to a series of six standardized alerting stimuli, administered at approximately 5-min intervals, in the same order for each animal. Alerting stimuli were delivered at a time when the tail Doppler flow signal was at a reasonably high baseline level. A flexible plastic rod, suddenly released from a restraint, tapped the side of the cage. A 0.5-s, 90-dB, 2000-Hz sound was played just outside the box. The cage was suddenly dropped 1 cm by removal of a support. The cage was suddenly moved 5 cm sideways. A cover over a transparent 20×20 cm window in the front door of the cage was suddenly removed. Finally, the door of the cage was opened, and the animal was pricked once on the back with a 20-ga. needle. The timing of each stimulus was recorded using a vibration detector device attached to the outside of the cage and connected to PowerLab.
Experimental design and statistical analysis
Experiments were conducted in stages, with different rats used in each stage, up to four treatments in each stage, and at least 3 days' interval between experiments on the same rat. Treatments at each stage were administered in rotating order to control for habituation and/or other serial effects. First stage: vehicle, clozapine 0.0625, clozapine 0.25 and clozapine 1 mg/kg. Second stage: vehicle, haloperidol 0.005, haloperidol 0.05 and haloperidol 0.5 mg/kg. Third stage: vehicle, SR46349B 0.01 mg/kg, SR46349B 0.1 mg/kg, SR46349B 1.0 mg/kg. Fourth stage: L741,626 1 mg/kg, SCH23390 0.1 mg/kg, 8-OH-DPAT 0.25 mg/kg with the dose repeated 10 min before commencement of alerting stimuli, 8-OH-DPAT 0.25 mg/kg preceded 30 min before by the specific 5-HT1A antagonist WAY-100635 0.5 mg/kg (Cryan et al. 1999; Forster et al. 1995). When technical failure (usually Doppler probe signal failure) meant that all doses could not be completed, a new animal was substituted. Some rats (approximately 10% of animals) had very low (0–5 cm/s) tail flow Doppler signals, either before or after injection of vehicle or before injection of drug, and data from these animals were excluded from all analyses.
In the case of experiments using SR46349B (0.01, 0.1 and 1 mg/kg), after alerting stimuli had been presented, the rat was treated with 100 μg/kg s.c. of the 5-HT2A agonist (±)-1-(2,5-dimethoxy-4-iodophenyl)-2-aminopropane (DOI), and tail blood flow was measured for the period 30–50 min after the DOI injection (Blessing and Seaman 2003). Results were used to confirm the effectiveness of SR46349B as a 5-HT2A antagonist.
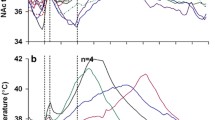
Data were analysed with Chart, IgorPro (WaveMetrics, Lake Oswega, OR, USA) and Statview (SAS Institute, Cary, NC, USA) software. For each rat, the mean Doppler flow signal and the coefficient of variation of the signal (averaged over 1 s periods to eliminate the pulsatile component) for the defined 20 min pre- and post-injection periods were calculated. For analysis of the response to alerting stimuli, a 3-s control period of the pulsatile Doppler signal just before the stimulus, and a 3-s period from approximately 7 to 10 s after the stimulus were selected (see Fig. 1). The overall mean level of flow signal for each 3-s period was calculated, as well as the mean of the amplitude of individual pulses (see Fig. 1). The SCVAR index was calculated, as shown in Fig. 1, so that if alerting stimulus caused flow and pulse amplitude to fall to zero values the SCVAR index was 100%, and no tail flow effect of an alerting stimulus yielded an index of 0%. The SCVAR index was calculated for each of the six individual alerting stimuli for each rat and an overall single combined SCVAR index was obtained for all rats in each drug treatment condition.
Method of deriving sympathetic cutaneous vasomotor alerting response (SCVAR) index. Method of deriving SCVAR index. The mean signal amplitude and the mean pulse amplitude were measured for the 3-s periods indicated (a before the alerting stimulus and b after the fall in flow elicited by the alerting stimulus), and the SCVAR index was calculated as shown
Factorial analysis of variance was used to compare corresponding values in vehicle and drug-treated animals. Pre- and post-injection values in a particular vehicle or drug condition were also analysed by repeated-measures analysis of variance. Fisher's protected t test was used to determine significant differences, with the overall significance threshold set at the 0.05 level. Regression analysis (linear regression of log dose) was used to determine dose–response relationships.
Drugs
All drugs were injected in a volume of 0.5 ml. Injections were s.c. except that in the vehicle, and haloperidol study (second stage) injections were s.c. in the first four rats injections and i.p. in the second 4. Clozapine and haloperidol (Sigma, Castle Hill, NSW, Australia) were dissolved in acidified Ringer. 8-OH-DPAT, WAY-100635 and DOI (Sigma) were dissolved in Ringer. L741,626 and SCH23390 (Tocris Cookson Ltd, Avonmouth, UK) were dissolved in 200 μl of DMSO with 300 μl of acidifed Ringer, and in Ringer, respectively. SR46349B, kindly donated by Sanofi-Recherche (Montpellier, France), was dissolved in 200 μl of DMSO and 300 μl of Ringer.
Results
Baseline tail blood flow indices
In individual rats maintained undisturbed in a closed, constant temperature cage (after overnight habituation in the same cage), there were marked variations in pulsatile tail blood flow, with the records displaying sudden decreases in this parameter and gradual return to high levels (SCVARs), without change in body temperature (Figs. 2, 3a–e control periods). SCVARs were sometimes obviously related to a particular environmental event (e.g. the experimenter moving near or touching the cage, or the process of drug injection as is evident in Fig. 3), but sometimes they occurred apparently spontaneously. In vehicle-treated rats, experimentally administered alerting stimuli usually caused SCVARs (Fig. 4a). The time from alerting stimulus to the commencement of the fall in the tail Doppler signal was approximately 2 s and the time to minimum flow was approximately 7 s.
Pulsatile tail blood flow Doppler signals (a, b), and cage temperature and body temperature (c) in a rat in the experimental box just before vehicle injection. Tail blood flow Doppler signal shows apparently spontaneous fluctuations from high to low levels, with sudden diminution of the amplitude of individual pulse waves (see expanded time scale trace in a, corresponding to the trace in b at the arrow), occurring without change in cage or body temperature. These variations in the Doppler signal are not due to recording errors. Rather, they reflect changes in the underlying blood flow, as documented in the conscious rabbit where the correlation coefficient between right and left ear pinna Doppler blood flow signals is greater than 0.97 (Blessing et al. 1998)
Examples of tail artery Doppler signal obtained from rats in the 20-min control period (before arrow under each trace) and during the 30 min after the subcutaneous or intraperitoneal injection. The fall in the signal just before and for some minutes after the arrow in each trace reflects cutaneous vasoconstriction (a sustained SCVAR) elicited by opening the cage and injecting the vehicle or drug. Time bar in d applies to all traces
The mean pre-treatment 20-min baseline tail artery Doppler flow signal from all rats studied was 12±1 cm/s and the mean coefficient of variation for the Doppler flow signal (averaged over 1 s intervals) during the 20-min baseline observation period was 68±3% (n=97 observations in 41 rats).
Effect of vehicle on tail blood flow indices
In individual rats, the 10- to 30-min period after injection of vehicle was compared with the 20-min period prior to the injection procedure. Vehicle caused no change in mean tail blood flow or in the coefficient of variation of flow (Fig. 5a,b). The SCVAR index for vehicle-treated rats was 83±2% (Fig. 5c), so that the flow-pulse amplitude value just after the alerting stimulus was 17% (100−83) of the pre-alerting control value.
Group data (mean±SEM) showing the effects of vehicle or different drug treatments on resting tail blood flow Doppler signal (a) on the coefficient of variation of the Doppler signal averaged over 1-s periods (b) and on the SCVAR index for combined alerting stimuli (c). The unfilled columns in a and b show results from the before treatment (vehicle or drug) 20-min control period. The filled columns in a and b show results from the 20-min period 10–30 min after administration of vehicle or drug. The filled columns in c show results obtained during the subsequent period (approximately 30 min) when controlled alerting stimuli were administered to calculate the SCVAR index. Doses of drugs are given in mg/kg directly under the bars, and numbers of rats in each condition are shown below the drug names. **Significant linear regression, P<0.001. ns Not significantly different from vehicle or from pre-injection control value, P>0.05. ¶Significantly less than vehicle and/or pre-injection control value, P<0.05. ¶¶Significantly less than vehicle and/or pre-injection control value, P<0.01. ‡‡Significantly greater than vehicle and/or pre-injection control value, P<0.01
Effect of clozapine on tail blood flow indices
Clozapine (0.0625, 0.25 and 1 mg/kg) increased baseline tail blood flow, decreased the coefficient of variation of flow, and substantially reduced the SCVAR index, with all three effects being dose-dependent (Figs. 3b–d, 4b,c and 5; Table 1a). As shown in Table 1a, the dose-dependent effect of clozapine on the SCVAR index was also apparent for each individual alerting stimulus. The proportion of the variance (Pearson r 2) due to the effect of clozapine was substantial, ranging from 0.66 to 0.83 (Table 1a). The regression slopes for the relationship between log dose of clozapine and the SCVAR index for individual alerting stimuli were remarkably homogenous, ranging between −45.20 and −52.74 (see Table 1a). A dose of 1 mg/kg of clozapine substantially reduced the vasoconstrictor response to the alerting stimulus, so that the SCVAR index was 18% (Table 1a), meaning that the flow-pulse amplitude just after the stimulus was 82% of the pre-stimulus value, compared with a corresponding value of 17% just after the stimulus in vehicle-treated animals.
Effect of SR46349B on tail blood flow indices
SR46349B (0.01, 0.1 and 1 mg/kg) dose-dependently increased baseline tail blood flow, decreased the coefficient of variation of flow, and reduced the SCVAR index (Table 1b; Figs. 4d, 5). As shown in Table 1b, the dose-dependent effect of SR46349B on the SCVAR index was also apparent for each individual alerting stimulus. For SR46349B, the slope of the dose–response regression line for combined SCVAR index (−14.54±2.17) was significantly less negative (P<0.01) than the corresponding slope for clozapine (−49.73±3.12), indicating that over the dose range employed the effect of SR46349B on the SCVAR index was less potent than that of clozapine. Similarly, the combined SCVAR index for the 1-mg/kg dose of SR46349B (53±3) was greater than the combined SCVAR index for the 1-mg/kg dose of clozapine (18±1), as shown in Table 1.
DOI (100 μg/kg, s.c.) administered after the alerting stimuli reduced tail blood flow (measured during the 30- to 50-min period after DOI) only in rats previously treated with lowest dose (0.01 mg/kg) of SR46349B. Linear regression analysis for the three doses of SR46349B showed a significant negative log dose–response relationship (Pearson r=−0.72, P<0.01), and after the 1-mg/kg dose of SR46349B, the mean 30–50 min post-DOI tail blood flow was not significantly different from the original pre- SR46349B control tail blood flow value (P>0.05, n=7).
Effect of 8-OH-DPAT on tail blood flow indices
8-OH-DPAT (0.25 mg/kg) increased baseline tail blood flow, decreased the coefficient of variation of flow, and reduced the SCVAR index (Fig. 5a–c). These changes were all prevented by prior treatment with WAY-100635 (0.5 mg/kg), as also shown in Fig. 5.
Effect of haloperidol, L741,626 and SCH23390 on tail blood flow indices
Haloperidol (0.005, 0.05 or 0.5 mg/kg) did not change mean tail blood flow or the coefficient of variation of flow (Figs. 3e, 5a,b). With the highest dose of haloperidol, there was a small drop in the combined SCVAR index (Fig. 5c). L741,626 (1 mg/kg) had no effect on resting tail blood flow and no effect on the coefficient of variation of tail blood flow (Fig. 5a,b). The drug slightly but significantly increased the SCVAR index (Fig. 5c). SCH23390 (0.1 mg/kg) substantially reduced resting tail blood flow (Fig. 5a) for the duration of the 10- to 30-min post-injection observation period. After this time tail blood flow increased so that the mean Doppler value for the 30- to 60-min post-injection time was not significantly different from the pre-injection value (15±3 to 21±3 cm/s, P>0.05, n=7). SCH23390 caused a moderate reduction in the SCVAR index (Fig. 5c).
Discussion
SCVARs, a link between sympathetic control of cutaneous blood flow, body temperature, psychological function and schizophrenia
We go pale with fright. Physiological mechanisms mediating this pallor include activation of sympathetic discharge to the cutaneous vessels, as documented in nerve and blood flow recordings in conscious humans (Delius et al. 1972; Hagbarth et al. 1972; Kistler et al. 1998; Macefield and Wallin 1999; Wallin and Fagius 1988). Episodic SCVARs, observed by direct observation in the rabbit ear pinna, were termed “psychic vascular reactions” by Krogh (1922). The vascular response, with near-complete vasoconstriction in the cutaneous vascular bed and little change in renal, mesenteric or skeletal muscle beds, or in cardiac output, commences 2 s after an alerting stimulus induces a burst of theta rhythm in the hippocampal EEG (Blessing et al. 1998; Yu and Blessing 1997). SCVARs thus constitute a patterned autonomic component of the overall bodily response to an alerting, salient or emotionally stressful stimulus.
Sustained SCVARs could interfere with normal heat loss from the body, thereby contributing to stress-induced hyperthermia (Mendoza et al. 1999; Olivier et al. 1994; Pattij et al. 2002; Van der Heyden et al. 1997; Zethof et al. 1995). Untreated schizophrenic patients do tend to have high body temperatures, reversed by antipsychotic treatment (Heh et al. 1988; Shiloh et al. 2001, 2003). In the first half of last century, finger plethysmography was widely used to study cutaneous blood flow in patients with mental illness, and Ackner (1956) documents evidence for vasoconstriction in the cutaneous vascular beds of psychotic patients. Clozapine does reduce alerting-induced vasoconstriction in schizophrenia patients, a response not observed with conventional antipsychotics (Zahn and Pickar 1993).
Clozapine and SR46349B inhibit SCVARs by actions within the CNS, not via peripheral effects on blood vessels or sympathetic ganglia
Systemic administration of clozapine substantially reduces directly measured post-ganglionic cutaneous sympathetic nerve vasomotor discharge (Blessing et al. 2003). There is no inhibition of synaptic transmission through the peripheral sympathetic ganglion or at the neuromuscular junction, as evidenced by the lack of inhibitory effect on clozapine on cutaneous vasoconstriction evoked by electrical stimulation of the cervical sympathetic trunk (Ootsuka et al. 2004). At a dose of 1.5 mg/kg (greater than the maximum amount used in the present study), clozapine has no effect on resting arterial blood pressure in conscious rats (van den Buuse 2003). This evidence is against a generalized peripherally mediated vasodilatory effect of low-dose clozapine, and consistent with the selective effects of clozapine on regional blood flow (Blessing et al. 2003). Similarly, the cutaneous vasomotor effects of 5-HT2A receptor stimulation and inhibition are mediated by actions on CNS neural pathways, not via peripheral actions on the sympathetic ganglion or the vasculature (Blessing and Seaman 2003; Ootsuka and Blessing 2005; Sipe et al. 2004). Therefore, at the doses used in the present study, the SCVAR-inhibiting actions of clozapine and SR46349B are mediated within the central nervous system, not via peripheral effects.
Clozapine's SCVAR inhibitory actions: comparison with haloperidol
Clozapine reduced both spontaneous SCVARs (occurring in response to natural environmental stimuli detected by the animal) and experimentally elicited SCVARs (occurring in response to experimentally controlled alerting stimuli). Effects of clozapine were dose-dependent, robust and substantial. After 1 mg/kg, the blood flow response was reduced to 18% of vehicle control. This dose is at the low end of the doses used in animal cardiovascular, behavioral and neurotransmitter release studies (Chung et al. 2004; Geyer et al. 2001; Meltzer et al. 2003; Rigdon and Weatherspoon 1992; van den Buuse 2003), and less than the usual clinically effective dose in humans (Davis and Chen 2004). Thus inhibition of sympathetic cutaneous vasomotor discharge, with inhibition of SCVARs, reflects a robust, dose-dependent, biologically relevant property of clozapine, one that can readily be measured in experimental animals.
Haloperidol had no effect on the resting level of tail blood flow, no effect on spontaneously occurring SCVARs, and at the highest dose, only a very minor effect on experimentally elicited SCVARs. The 0.5-mg/kg dose of haloperidol is above maximal doses recommended for antipsychotic effects in humans (Davis and Chen 2004), above doses required for cardiovascular and behavioral effects in experimental animals, and at a dosage level associated with non-specific sedative actions (Geyer et al. 2001; Rigdon and Weatherspoon 1992; van den Buuse 2003). By its inability to inhibit sympathetic cutaneous vasomotor outflow, haloperidol thus differs markedly from clozapine.
SCVARs, 5-HT2A receptor antagonism and 5-HT1A agonism
The experiments with DOI, administered after each SR46349B experiment, demonstrate that SR46349B successfully blocked 5-HT2A receptors in a dose-responsive manner. Activation of 5-HT2A receptors has previously been demonstrated to increase body temperature (Gudelsky et al. 1986) and substantially reduce tail blood flow and tail temperature (Blessing and Seaman 2003; Sipe et al. 2004). Agents that stimulate 5-HT2A receptors [including lysergic acid diethylamide (LSD)] are hallucinogens, the observation that originally triggered the idea that 5-HT2A receptor actions might be important in psychotic states (Geyer et al. 2001). There is a remarkable similarity between the molar doses of the different 5-HT2A receptor-stimulating agents that cause hallucinations in humans and the doses causing hyperthermia in experimental animals (Jacob and Lafille 1963). Clozapine, but not haloperidol, blocks the hyperthermic effect of 5-HT2A receptor stimulation (Nash et al. 1988). Given that 5-HT2A receptor antagonism is important in clozapine's psychotherapeutic action, the clozapine-like action of SR46349B in the present experimental model is further evidence for the view that SCVARs are linked with emotional/psychological function.
The slope of the dose–response curve for the effect of SR46349B on the SCVAR index was significantly less negative than the slope for clozapine. SR46349B (1 mg/kg) reduced the SCVAR index to 53%, compared with 18% for the 1-mg/kg dose of clozapine. Thus 5-HT2A antagonism could contribute to, but not account for all of the SCVAR-inhibiting action of clozapine. Clinical trials show that SR46349B, by itself, is helpful for patients with schizophrenia/schizoaffective disorder (Meltzer et al. 2004), so there is a relationship between the ability of 5-HT2A antagonists to inhibit SCVARs and their clinical effects on emotional/psychological function.
Changes induced by 8-OH-DPAT were prevented by pre-treatment with WAY-100635, a selective 5-HT1A antagonist (Forster et al. 1995). 8-OH-DPAT also inhibits thermoregulatory cutaneous vasomotor sympathetic outflow induced physiologically by exposing the animal to a cold environment, and by experimental induction of the febrile response by LPS (Blessing 2004a;Ootsuka and Blessing 2003). Buspirone, a 5-HT1A agonist with anti-anxiety psychotherapeutic actions, lowers body temperature (Martin et al. 1992; Millan et al. 1993; Young et al. 1993), possibly by increasing cutaneous blood flow. Partial agonism at 5-HT1A receptors contributes to the therapeutic action of clozapine, even though the receptor affinity is quite low (Arnt and Skarsfeldt 1998; Bantick et al. 2001; Meltzer et al. 2003; Millan 2000). Stimulation of 5-HT1A receptors has a modest “clozapine-like” action on cutaneous blood flow and on SCVARs, so that activation of these receptors could contribute to clozapine's effects on sympathetic cutaneous vasomotor outflow.
SCVARs and dopamine D2 and D1 receptor antagonism
L741,626 (1 mg/kg), a selective D2 receptor antagonist (Kulagowski et al. 1996), slightly increased the SCVAR index, and had no effect on resting tail blood flow and no effect on the coefficient of variation of tail blood flow. The affinity of haloperidol for dopamine D2 receptors is approximately 50–200 times that of clozapine and the affinity of L741,626 is approximately 30 times that of clozapine (Arnt and Skarsfeldt 1998; Bymaster et al. 1996; Hartman et al. 1996; Kulagowski et al. 1996; Meltzer et al. 2003; Weiner et al. 2001). Thus dopamine D2 receptor blockade, considered a key element of the therapeutic action of haloperidol, is unlikely to contribute to clozapine's SCVAR-reducing inhibition of sympathetic cutaneous vasomotor outflow. Haloperidol has little or no effect on hyperthermia elicited by MDMA (Schmidt et al. 1990), no effect on hyperthermia and cutaneous vasoconstriction elicited by LPS, and no effect on cold-induced cutaneous vasoconstriction (Blessing 2004b).
Faunt and Crocker (1987) reported that 0.1 mg/kg of SCH23390 caused an initial small rise in body temperature followed by a small fall, a change that could reflect reduced, then increased, heat loss via the tail vascular bed. Salmi and colleagues (1993, 1994), Oerther and Ahlenius (2000) and Chaperon et al. (2003) reported no change in body temperature with SCH23390. Salmi et al. (1994), Salmi and Ahlenius (1996) and Oerther and Ahlenius (2000) reported that the hypothermic action of clozapine (but not that of olanzapine) was entirely prevented by prior administration of SCH23390. However, Salmi et al. (1993) and Faunt and Crocker (1987) noted that the partial dopamine D1 agonist SKF 38393 has no effect on body temperature when administered alone, and Salmi et al. (1993) noted that A68930, a high-affinity D1 agonist, has a rather modest temperature lowering action. There are no previous reports of the effects of SCH23390 on cutaneous blood flow. Pre-treatment with SCH23390 does not prevent clozapine-induced increases in tail blood flow (Blessing, unpublished data).
Conclusion
Clozapine, by actions within the central nervous system, robustly inhibits sympathetic outflow to the thermoregulatory cutaneous vascular bed, thereby substantially reducing sympathetic cutaneous vasomotor alerting responses (SCVARs) and increasing cutaneous blood flow. Haloperidol does not have these effects and neither do specific dopamine D1 or D2 antagonists. Activation of 5-HT1A receptors or blockade of 5-HT2A receptors reduces SCVARs and increases baseline cutaneous blood flow, so that these receptor actions could contribute to clozapine's inhibition of cutaneous sympathetic vasomotor outflow, but the actual receptor mechanisms mediating the effects of clozapine remain to be elucidated. Clozapine's inhibition of cutaneous vasomotor sympathetic outflow, with resulting cutaneous vasodilatation and SCVAR inhibition, is a physiological action that clearly differentiates the drug from haloperidol. Studies utilizing this newly described biological property of clozapine may elucidate mechanisms underlying its therapeutic actions.
References
Ackner B (1956) Emotions and the peripheral vasomotor system. J Psychosom Res 1:3–20
Arnt J, Skarsfeldt T (1998) Do novel antipsychotics have similar pharmacological characteristics? A review of the evidence. Neuropsychopharmacology 18:63–101
Arvidsson LE, Johansson AM, Hacksell U, Nilsson JL, Svensson K, Hjorth S, Magnusson T, Carlsson A, Andersson B, Wikstrom H (1987) (+)-cis-8-Hydroxy-1-methyl-2-(di-n-propylamino)tetralin: a potent and highly stereoselective 5-hydroxytryptamine receptor agonist. J Med Chem 30:2105–2109
Bantick RA, Deakin JF, Grasby PM (2001) The 5-HT1A receptor in schizophrenia: a promising target for novel atypical neuroleptics? J Psychopharmacol 15:37–46
Blessing WW (2004a) 5-Hydroxytryptamine 1A receptor activation reduces cutaneous vasoconstriction and fever associated with the acute inflammatory response in rabbits. Neuroscience 123:1–4
Blessing WW (2004b) Clozapine and olanzapine, but not haloperidol, reverse cold-induced and lipopolysaccharide-induced cutaneous vasoconstriction. Psychopharmacology (Berl) 175:487–493
Blessing WW, Seaman B (2003) 5-Hydroxytryptamine(2A) receptors regulate sympathetic nerves constricting the cutaneous vascular bed in rabbits and rats. Neuroscience 117:939–948
Blessing WW, Arnolda LF, Yu YH (1998) Cutaneous vasoconstriction with alerting stimuli in rabbits reflects a patterned redistribution of cardiac output. Clin Exp Pharmacol Physiol 25:457–460
Blessing WW, Seaman B, Pedersen NP, Ootsuka Y (2003) Clozapine reverses hyperthermia and sympathetically-mediated cutaneous vasoconstriction induced by MDMA (Ecstasy) in rabbits and rats. J Neurosci 23:6385–6391
Bymaster FP, Calligaro DO, Falcone JF, Marsh RD, Moore NA, Tye NC, Seeman P, Wong DT (1996) Radioreceptor binding profile of the atypical antipsychotic olanzapine. Neuropsychopharmacology 14:87–96
Chaperon F, Tricklebank MD, Unger L, Neijt HC (2003) Evidence for regulation of body temperature in rats by dopamine D2 receptor and possible influence of D1 but not D3 and D4 receptors. Neuropharmacology 44:1047–1053
Chung YC, Li Z, Dai J, Meltzer HY, Ichikawa J (2004) Clozapine increases both acetylcholine and dopamine release in rat ventral hippocampus: role of 5-HT1A receptor agonism. Brain Res 1023:54–63
Cryan JF, Kelliher P, Kelly JP, Leonard BE (1999) Comparative effects of serotonergic agonists with varying efficacy at the 5-HT(1A) receptor on core body temperature: modification by the selective 5-HT(1A) receptor antagonist WAY 100635. J Psychopharmacol 13:278–283
Davis JM, Chen N (2004) Dose response and dose equivalence of antipsychotics. J Clin Psychopharmacol 24:192–208
Delius W, Hagbarth K-E, Hongell A, Wallin BG (1972) Manoeuvres affecting sympathetic outflow in human skin nerves. Acta Physiol Scand 84:177–186
Faunt JE, Crocker AD (1987) The effects of selective dopamine receptor agonists and antagonists on body temperature in rats. Eur J Pharmacol 133:243–247
Forster EA, Cliffe IA, Bill DJ, Dover GM, Jones D, Reilly Y, Fletcher A (1995) A pharmacological profile of the selective silent 5-HT1A receptor antagonist, WAY-100635. Eur J Pharmacol 281:81–88
Garcia JN, Pedersen NP, Nalivaiko E, Blessing WW (2001) Tail artery blood flow measured by chronically implanted Doppler ultrasonic probes in unrestrained conscious rats. J Neurosci Methods 104:209–213
Geyer MA, Krebs-Thomson K, Braff DL, Swerdlow NR (2001) Pharmacological studies of prepulse inhibition models of sensorimotor gating deficits in schizophrenia: a decade in review. Psychopharmacology (Berl) 156:117–154
Gudelsky GA, Koenig JI, Meltzer HY (1986) Thermoregulatory responses to serotonin (5-HT) receptor stimulation in the rat. Evidence for opposing roles of 5-HT2 and 5-HT1A receptors. Neuropharmacology 25:1307–1313
Hagbarth K-E, Hallin RG, Hongell A, Torebjörk HE, Wallin BG (1972) General characteristics of sympathetic activity in human skin nerves. Acta Physiol Scand 84:164–172
Hartman D, Monsma F, Civelli O (1996) Interaction of antipsychotic drugs with dopamine receptor subtypes. In: Csernansky JG (ed) Handbook of experimental pharmacology. Springer, Berlin Heidelberg New York, pp 43–75
Heh CW, Herrera J, DeMet E, Potkin S, Costa J, Sramek J, Hazlett E, Buchsbaum MS (1988) Neuroleptic-induced hypothermia associated with amelioration of psychosis in schizophrenia. Neuropsychopharmacology 1:149–156
Jacob J, Lafille C (1963) Charactérisation et detection pharacologiques des substances hallucinogènes. Arch Int Pharmacodyn 145:528–545
Kapur S, Seeman P (2001) Does fast dissociation from the dopamine d(2) receptor explain the action of atypical antipsychotics? A new hypothesis. Am J Psychiatry 158:360–369
Kistler A, Mariauzouls C, von Berlepsch K (1998) Fingertip temperature as an indicator for sympathetic responses. Int J Psychophysiol 29:35–41
Krogh A (1922) The anatomy and physiology of capillaries, 2nd edn. Yale University Press, New Haven, CT
Kulagowski JJ, Broughton HB, Curtis NR, Mawer IM, Ridgill MP, Baker R, Emms F, Freedman SB, Marwood R, Patel S, Ragan CI, Leeson PD (1996) 3-((4-(4-Chlorophenyl)piperazin-1-yl)-methyl)-1H-pyrrolo-2,3-b-pyridine: an antagonist with high affinity and selectivity for the human dopamine D4 receptor. J Med Chem 39:1941–1942
Macefield VG, Wallin BG (1999) Respiratory and cardiac modulation of single sympathetic vasoconstrictor and sudomotor neurones to human skin. J Physiol 516(Pt 1):303–314
Martin KF, Phillips I, Hearson M, Prow MR, Heal DJ (1992) Characterization of 8-OH-DPAT-induced hypothermia in mice as a 5-HT1A autoreceptor response and its evaluation as a model to selectively identify antidepressants. Br J Pharmacol 107:15–21
Meltzer HY (2002) Commentary on “clinical studies on the mechanism of action of clozapine; the dopamine–serotonin hypothesis of schizophrenia” (Psychopharmacology (1989) 99:S18–S27). Psychopharmacology (Berl) 163:1–3
Meltzer HY, Li Z, Kaneda Y, Ichikawa J (2003) Serotonin receptors: their key role in drugs to treat schizophrenia. Prog Neuro-Psychopharmacol Biol Psychiatry 27:1159–1172
Meltzer HY, Arvanitis L, Bauer D, Rein W (2004) Placebo-controlled evaluation of four novel compounds for the treatment of schizophrenia and schizoaffective disorder. Am J Psychiatry 161:975–984
Mendoza DL, Bravo HA, Swanson HH (1999) Antiaggresive and anxiolytic effects of gepirone in mice, and their attenuation by WAY 100635. Pharmacol Biochem Behav 62:499–509
Millan MJ (2000) Improving the treatment of schizophrenia: focus on serotonin (5-HT1A) receptors. J Pharmacol Exp Ther 295:853–861
Millan MJ, Rivet JM, Canton H, Le Marouille-Girardon S, Gobert A (1993) Induction of hypothermia as a model of 5-hydroxytryptamine1A receptor-mediated activity in the rat: a pharmacological characterization of the actions of novel agonists and antagonists. J Pharmacol Exp Ther 264:1364–1376
Millan MJ, Audinot V, Melon C, Newman-Tancredi A (1995) Evidence that dopamine D3 receptors participate in clozapine-induced hypothermia. Eur J Pharmacol 280:225–229
Nash JF, Meltzer HY, Gudelsky GA (1988) Antagonism of serotonin receptor mediated neuroendocrine and temperature responses by atypical neuroleptics in the rat. Eur J Pharmacol 151:463–469
Oerther S, Ahlenius S (2000) Atypical antipsychotics and dopamine D(1) receptor agonism: an in vivo experimental study using core temperature measurements in the rat. J Pharmacol Exp Ther 292:731–736
Olivier B, Molewijk E, van Oorschot R, van der Poel G, Zethof T, van der Heyden J, Mos J (1994) New animal models of anxiety. Eur Neuro-Psychopharmacol 4:93–102
Ootsuka Y, Blessing WW (2003) 5-Hydroxytryptamine 1A receptors inhibit cold-induced sympathetically-mediated cutaneous vasoconstriction in rabbits. J Physiol 552.1:303–314
Ootsuka Y, Blessing W (2005) Activation of slowly conducting medullary raphé-spinal neurons, including serotonergic neurons, increases cutaneous sympathetic vasomotor in rabbit. Am J Physiol 288:R909–R918
Ootsuka Y, Nalivaiko E, Blessing WW (2004) Spinal 5-HT2A receptors regulate cutaneous sympathetic vasomotor outflow in rabbits and rats; relevance for cutaneous vasoconstriction elicited by MDMA (3,4-methylenedioxymethamphetamine, “Ecstasy”) and its reversal by clozapine. Brain Res 1014:34–44
Pattij T, Groenink L, Hijzen TH, Oosting RS, Maes RA, van der Gugten J, Olivier B (2002) Autonomic changes associated with enhanced anxiety in 5-HT(1A) receptor knockout mice. Neuropsychopharmacology 27:380–390
Pedersen NP, Blessing WW (2001) Cutaneous vasoconstriction contributes to hyperthermia induced by 3,4-methylenedioxymethamphetamine (ecstasy) in conscious rabbits. J Neurosci 21:8648–8654
Rigdon GC, Weatherspoon JK (1992) 5-Hydroxytryptamine 1a receptor agonists block prepulse inhibition of acoustic startle reflex. J Pharmacol Exp Ther 263:486–493
Rinaldi-Carmona M, Congy C, Santucci V, Simiand J, Gautret B, Neliat G, Labeeuw B, Le Fur G, Soubrie P, Breliere JC (1992) Biochemical and pharmacological properties of SR 46349B, a new potent and selective 5-hydroxytryptamine2 receptor antagonist. J Pharmacol Exp Ther 262:759–768
Salmi P, Ahlenius S (1996) Further evidence for clozapine as a dopamine D1 receptor agonist. Eur J Pharmacol 307:27–31
Salmi P, Jimenez P, Ahlenius S (1993) Evidence for specific involvement of dopamine D1 and D2 receptors in the regulation of body temperature in the rat. Eur J Pharmacol 236:395–400
Salmi P, Karlsson T, Ahlenius S (1994) Antagonism by SCH 23390 of clozapine-induced hypothermia in the rat. Eur J Pharmacol 253:67–73
Schmidt CJ, Black CK, Abbate GM, Taylor VL (1990) Methylenedioxymethamphetamine-induced hyperthermia and neurotoxicity are independently mediated by 5-HT2 receptors. Brain Res 529:85–90
Shiloh R, Weizman A, Epstein Y, Rosenberg SL, Valevski A, Dorfman-Etrog P, Wiezer N, Katz N, Munitz H, Hermesh H (2001) Abnormal thermoregulation in drug-free male schizophrenia patients. Eur Neuropsychopharmacol 11:285–288
Shiloh R, Portuguese S, Bodinger L, Katz N, Sigler M, Hermesh H, Munitz H, Weizman A (2003) Increased corneal temperature in drug-free male schizophrenia patients. Eur Neuropsychopharmacol 13:49–52
Sipe K, Leventhal L, Burroughs K, Cosmi S, Johnston GH, Deecher DC (2004) Serotonin 2A receptors modulate tail-skin temperature in two rodent models of estrogen deficiency-related thermoregulatory dysfunction. Brain Res 1028:191–202
Tauscher J, Hussain T, Agid O, Verhoeff NP, Wilson AA, Houle S, Remington G, Zipursky RB, Kapur S (2004) Equivalent occupancy of dopamine D1 and D2 receptors with clozapine: differentiation from other atypical antipsychotics. Am J Psychiatry 161:1620–1625
van den Buuse M (2003) Acute effects of antipsychotic drugs on cardiovascular responses to stress. Eur J Pharmacol 464:55–62
Van der Heyden JA, Zethof TJ, Olivier B (1997) Stress-induced hyperthermia in singly housed mice. Physiol Behav 62:463–470
Wallin BG, Fagius J (1988) Peripheral sympathetic neural activity in conscious humans. Annu Rev Physiol 50:565–576
Weiner DM, Burstein ES, Nash N, Croston GE, Currier EA, Vanover KE, Harvey SC, Donohue E, Hansen HC, Andersson CM, Spalding TA, Gibson DF, Krebs-Thomson K, Powell SB, Geyer MA, Hacksell U, Brann MR (2001) 5-hydroxytryptamine2A receptor inverse agonists as antipsychotics. J Pharmacol Exp Ther 299:268–276
Young AH, McShane R, Park SB, Cowen PJ (1993) Buspirone-induced hypothermia in normal male volunteers. Biol Psychiatry 34:665–666
Yu YH, Blessing WW (1997) Cutaneous vasoconstriction in conscious rabbits during alerting responses detected by hippocampal theta-rhythm. Am J Physiol 272:R208–R216
Zahn TP, Pickar D (1993) Autonomic effects of clozapine in schizophrenia: comparison with placebo and fluphenazine. Biol Psychiatry 34:3–12
Zethof TJ, Van der Heyden JA, Tolboom JT, Olivier B (1995) Stress-induced hyperthermia as a putative anxiety model. Eur J Pharmacol 294:125–135
Acknowledgements
Supported by The National Health and Medical Research Council of Australia. I thank Melissa Blair, Candice Morgan and Robyn Flook for technical assistance. Dr. Eugene Nalivaiko made helpful suggestions concerning the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Blessing, W.W. Clozapine increases cutaneous blood flow and reduces sympathetic cutaneous vasomotor alerting responses (SCVARs) in rats: comparison with effects of haloperidol. Psychopharmacology 181, 518–528 (2005). https://doi.org/10.1007/s00213-005-0012-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-005-0012-9