Abstract
Rationale
It has been suggested that corticosteroid-serotonin interactions are central to the pathophysiology of depression. These interactions have been investigated in healthy and depressed humans, primarily using neuroendocrine techniques.
Objectives
To review the evidence regarding the nature of these interactions in healthy and depressed humans.
Methods
Electronic searches were performed for relevant papers, employing MEDLINE and Web of Science. To focus the review, we selected only those articles involving (i) assessment of serotonergic function following experimental manipulation of the HPA axis in healthy volunteers; and (ii) assessment of both serotonergic and HPA axis function in clinically depressed subjects.
Results
Pre-treatment with hydrocortisone, both acutely and sub-acutely attenuates the GH response to GHRH in healthy subjects. This complicates the interpretation of 5-HT neuroendocrine studies employing GH output as a measure. In depression there is evidence that reduced availability of l-tryptophan impairs HPA axis feedback. There is also evidence that depressed and healthy subjects may adapt differently both to low tryptophan and hypercortisolaemic challenges. There is no consistent evidence of a simple relationship between HPA axis function and 5-HT function in depression.
Conclusions
The putative reduction in central 5-HT function has not been shown to be a direct consequence of hypercortisolaemia. Rather, the 5-HT system and HPA axis have complex inter-relationships. Challenges to either system, such as stress or reduced dietary tryptophan, may perturb the other and subjects vulnerable to depression may fail to adapt to such challenges.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hypothalamic pituitary adrenal (HPA) axis abnormalities are well established in major depression (Steckler et al. 1999). Abnormalities of the serotonin (5-HT) system also appear to be important although evidence is less consistent (Cowen 1996). The most consistent neuroendocrine evidence in depression suggests a reduction in 5-HT1A receptor function (Lesch et al. 1990; Power and Cowen 1992; Meltzer and Maes 1995; Riedel et al. 2002a; Shapira et al. 2000) and number (Drevets et al. 1999; Sargent et al. 2000). It has also been suggested that 5-HT2 function is increased in depression. Studies investigating platelet 5-HT2 binding suggest an upregulation of 5-HT2 receptors as do some studies using putative 5-HT2 challenge strategies (5-HTP, m-CPP) (Koyama and Meltzer 1986; Maes et al. 1987a; Riedel et al. 2002a). However, there are also negative studies (Heninger et al. 1990; Kahn et al. 1990).
It has been postulated, on the basis of this and extensive animal evidence (Chaouloff 1993, 2000), that the abnormalities of these two systems are linked and that this link is an important aetiological mechanism in depression (Dinan 1994; McAllister-Williams et al. 1998). In particular, it has been suggested that hypercortisolaemia reduces 5-HT1A receptor function (McAllister-Williams et al. 1998) and increases 5-HT2 receptor function or numbers (Maes and Meltzer 1995). Both of these changes may then act to dysregulate HPA axis function further. This article reviews the human evidence for interactions between corticosteroids and the 5-HT system, both in healthy volunteers and in subjects with major depression.
Search strategy
Electronic database searches were carried out for relevant papers, utilising MEDLINE and Web of Science. In the initial search, the terms: “serotonin” or “5-HT” and “HPA axis”, “cortisol”, “ACTH”, “corticotropin” or “CRH” were used. To enable the inclusion of more recent articles, ScienceDirect was also searched using these keywords in the “abstract, title, keywords” field. To focus the review, we selected only those articles involving (i) assessment of serotonergic function following experimental manipulation of the HPA axis in healthy volunteers; and (ii) assessment of both serotonergic and HPA axis function in clinically depressed subjects. All were limited to English language publications and human subjects.
Methodologies
Two methods have commonly been used to investigate the relationship between HPA axis function and 5-HT function in humans, and in particular in depression. The first is to manipulate HPA axis or 5-HT function and observe the effects on the other system. The advantage of this is that if other factors are well controlled, causality can be attributed to the manipulation. However, neither the manipulation used nor the response to it may accurately reflect the situation in depression. The second method is to measure HPA axis function and 5-HT function and to examine correlations between the two in depressed patients. This method does not prove causality, but has the advantage of investigating the actual situation in depressed subjects.
Measurement of baseline HPA axis function
The methods used to examine 5-HT function are complex and discussed in the relevant sections. The method of measurement of HPA axis function also influences results. While it is beyond the scope of this review to examine in detail the validity of these methods, some preliminary points are as follows.
Two distinct methods have been used to investigate HPA axis function in depression: (a) measurement of hormonal output and (b) measurement of feedback. Measures of cortisol output estimate the amount of cortisol to which 5-HT targets are exposed and, if repeated measures are made, the circadian pattern of this exposure. Measures of feedback estimate the function of glucocorticoid receptors, which may modulate 5-HT function. This may correlate with cortisol output. The commonly used measures of HPA axis feedback are the dexamethasone suppression test (DST) and combined dexamethasone/corticotrophin releasing hormone test (dex/CRH) (Heuser et al. 1994). The latter has not been used to investigate the relationship between the HPA axis and 5-HT system.
There is debate about the best measure of HPA axis function and in large clinical populations it is rarely possible to use more than one measure. Rubin et al. (1987) investigated the correlations between 24-h urinary cortisol before and after dexamethasone, and serum cortisol levels taken at various points both before and after dexamethasone administration. The study clearly demonstrated that average 24-h serum cortisol concentration correlated well with mean post-dexamethasone cortisol measures. The correlations among measures worsened as the measure taken became further removed from the average 24-h serum cortisol concentration, i.e. if a smaller segment of the 24-h serum profile was taken. The measure that correlated least well with results was a single plasma cortisol measure. Repeated basal cortisol measures therefore correlate with DST output and allow examination of diurnal rhythm. Twenty-four hour urinary free cortisol (UFC) does not measure diurnal rhythm and in the study of Rubin et al. (1987) did not correlate well with average 24-h serum cortisol. Saliva sampling, which was used in a number of the studies reviewed below allows repeated measurements of steroid hormones from large numbers of subjects and yields data on diurnal variation of secretion of these hormones. It is particularly useful when subjects are ambulant. Salivary levels of cortisol correlate well with serum levels and these correlate well with CSF levels (Guazzo et al. 1996). Only unbound cortisol is able to pass into the saliva and cross the blood-brain barrier. It has therefore been suggested that salivary cortisol is a better measure of brain exposure to cortisol than plasma cortisol (Vining et al. 1983).
Experimental manipulations of the HPA axis
Studies have investigated reduction of cortisol levels by administration of steroid synthesis inhibitors such as metyrapone or ketoconazole (which inhibit 11 β-hydroxylase, preventing the conversion of 11-deoxycortisol to cortisol). This has the disadvantage that these treatments interfere with other aspects of steroid hormone synthesis and cause accumulation of 11-deoxycortisol, which itself is psychoactive. In addition, producing hypocortisolaemia does not necessarily have the opposite effect to the hypercortisolaemia seen in depression.
More commonly, corticosteroids have been administered in an effort to mimic aspects of the hypercortisolaemia seen in depression. Most frequently used have been dexamethasone, a potent glucocorticoid receptor (GR) agonist, and hydrocortisone, which is essentially indistinguishable from cortisol (the corticosteroid present in highest concentrations in humans), which has high affinity for mineralocorticoid receptors (MRs) and considerably less affinity for GRs (Reul et al. 1990). These differences in receptor binding profile are important for their effects on 5-HT function, as is the marked difference in their ability to penetrate the brain. Dexamethasone is actively pumped out of the brain across the blood-brain barrier by the mdr1a p-glycoprotein (Meijer et al. 1998). It is difficult therefore to predict the degree to which a particular dose of dexamethasone will enter the brain, making studies investigating pre-treatment with dexamethasone difficult to interpret.
Schedules of pre-treatment with hydrocortisone have generally involved either administration of a single dose the night before testing 5-HT function (acute) or a smaller dose taken twice a day (b.d.) for 4–10 days prior to testing (subacute). These schedules have generally been compared with pre-treatment with placebo, in a double-blind, counterbalanced design. Young et al. (1998) found, in healthy males, that a sub-chronic schedule of administration (20 mg b.d. for 10 days) elevated 24-h UFC into the range seen in depression. Newcomer et al. (1999) administered 100 mg at 7 a.m. and 60 mg at 7 p.m. to healthy males and found that 4 p.m. plasma levels were on average 700–800 nmol/l compared with 250 nmol/l in subjects treated with 25 mg at 7 a.m. and 15 mg at 7 p.m. and 120 nml/l in subjects who had taken placebo. This compares with 828–1104 nmol/l following major abdominal surgery (Chernow et al. 1987) and an average 1–4 pm plasma concentration for depressed DST non-suppressors of 310 nmol/l (Rubin et al. 1987). Equal doses morning and evening have been used in most studies on the basis of evidence that the diurnal variation in cortisol secretion is reduced in depression (Sachar et al. 1973; Deuschle et al. 1997). Recent animal work has suggested that a manipulation that does not alter corticosterone levels but does flatten circadian rhythm, does affect 5-HT1A function in rats (Leitch et al. 2003). However, in healthy volunteers, twice-daily administration of hydrocortisone results in a sharp evening and morning peak of cortisol with a negative feedback induced lowering of cortisol levels in the middle of the day (Hearn et al. 2002). Therefore this schedule actually creates two peaks with an exaggerated decline in the hours following them. This manipulation therefore creates a situation that in terms of the pattern of cortisol secretion does not really mimic what is seen in depression.
We know of no studies which have followed cortisol levels through the night following acute pre-treatment with hydrocortisone and can therefore only speculate on the likely effects of the acute schedule. The half-life of hydrocortisone is approximately 90 min (Rang and Dale 1991) and Kasuya et al. (1995) demonstrated that 5 mg hydrocortisone increased levels to 55 nmol/l 30 min after administration (during the day). Extraolating from this, 100 mg would produce a peak of approximately 1100 nmol/l at 11:30 p.m. Since endogenous levels of cortisol at night are low, feedback inhibition of endogenous cortisol secretion is unlikely to have a significant impact on cortisol levels and we could therefore expect levels to decline at a rate in keeping with the biological half-life. Therefore at 4 a.m. (i.e. at 3 half lives or 4.5 h after peak) levels would have declined to be equivalent to having taken 12.5 mg hydrocortisone orally. Endgenous cortisol secretion at this time will be beginning to rise and may be restrained by the hydrocortisone present in the system. The following morning, cortisol levels appear to be significantly lower (Porter et al. 1998). Therefore, the effect of this manipulation is likely to be to increase cortisol levels dramatically at a time when they would normally have been low, during the nocturnal trough, with a compensatory reduction in the morning. Once again, it could be argued that this mimics to some extent the situation in depression, although it is likely that the concentrations reached using a dose of 100 mg (Porter et al. 1998) or even 50 mg (Bhagwagar et al. 2002a) are far higher than in most depressed patients at night. An important point is that MRs are largely occupied at all phases of the circadian cycle except at the nocturnal nadir. If they are occupied at this time (in depression or following pre-treatment with hydrocortisone), this is likely to affect their overall function since receptors which are permanently fully occupied are unlikely to function efficiently.
Other aspects of HPA axis dysregulation that may be present in people with depression or vulnerability to depression cannot be manipulated. It is possible, for instance, that the effects of increased cortisol are different in depression because of dysfunctional GRs (Holsboer et al. 1995) or MRs (although a recent study does not suggest impaired MR function in depression; Young et al. 2003). Furthermore, hydrocortisone administration in healthy volunteers is likely to inhibit CRH release, while in depressed subjects CRH release may be increased (Nemeroff 1996). CRH has important direct effects on GH release (Steiger and Holsboer 1997) and on the 5-HT system (Price et al. 1998b). Potentially, GR function could be manipulated using RU-486 and MR function using spironolactone. As far as we know the effects of such manipulations on 5-HT function have not been investigated.
Effects of corticosteroids on GH and PRL release
Studies investigating the 5-HT system have generally employed neuroendocrine techniques. Most of these measure pituitary hormone responses, primarily adrenocorticotropic hormone (ACTH), growth hormone (GH), prolactin (PRL) and (from the adrenal) cortisol, to a serotonergic probe. However, cortisol inhibits its own secretion and that of ACTH by negative feedback. There is also evidence that pituitary release of ACTH in response to CRH is reduced in depression (Gold et al. 1986) and that this correlates inversely with baseline cortisol levels (Holsboer et al. 1984). These measures are therefore unlikely to give a good indication of independent effects of HPA axis hormones on 5-HT function. HPA axis hormones may also directly affect GH and PRL release from the pituitary in a serotonin independent manner. The evidence regarding modulation of pituitary release of GH and PRL by HPA axis hormones is therefore reviewed below.
In vitro and animal studies suggest complex interactions between corticosteroids and the somatotrophic axis (see Thakore and Dinan 1994 for review). In humans, naturalistic studies have shown that long-term hypercortisolaemia, as seen in Cushing’s disease, is associated with reduced growth and GH levels (Wajchenberg et al. 1996). Dexamethasone has been used in a number of studies examining this effect. The time lag between administration of the corticosteroid and measurement of GH is of significance; dexamethasone has an initial stimulatory and a later inhibitory effect on GHRH induced GH release (Casanueva et al. 1988). Using pre-treatment with the physiological corticosteroid hydrocortisone, Frantz and Rabkin (1964) demonstrated a reduced GH response to insulin-induced hypoglycaemia. GHRH induced GH release is reduced in a dose dependant manner by acute pre-treatment with cortisone acetate (Giustina et al. 1990) while stimulated (insulin and arginine) GH release is enhanced in states of chronic hypocortisolaemia and reversed by corticosteroid replacement (Giustina et al. 1989). Studies using metyrapone to reduce cortisol levels in healthy volunteers have shown both an enhanced response (Dinan et al. 1994) and no significant effect (Burguera et al. 1990).
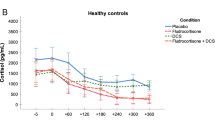
We investigated the effects of two different schedules of administration of hydrocortisone on GHRH mediated GH release (Watson et al. 2000). The GH response to GHRH was significantly reduced by pre-treatment with both the chronic (20 mg b.d. for 7 days) and acute (100 mg, 11 h before testing) schedules. Baseline levels of GH were unaffected by either schedule.
The GHRH test has been extensively investigated in depression and in other conditions (see Skare et al. 1994 for review). Studies divide roughly equally into those which show blunting, enhancement and no difference in GH response to GHRH in depressed compared with control subjects. Lesch (1989a) investigated the relationship between the GH response to GHRH and the ACTH and cortisol responses to CRH in depression. There was no correlation. Data regarding the correlation between baseline cortisol secretion and GH response was not reported. Birmaher (2000) investigated adolescents at high risk of major depressive disorder according to family history, but with no past or current history of depression. There was a significantly lower GH response to GHRH in these subjects compared with controls and no correlation between various measures of cortisol secretion and the GH response to GHRH (Birmaher et al. 2002).
Data on GH response to various 5-HT agents is reviewed below, but studies have also investigated the correlation between GH response to other agents and HPA axis measures. Dolan (1986) found a significant negative correlation between the GH response to clonidine and urinary free cortisol levels in 14 depressed patients. Matussek (1980) and Amsterdam (1990) have also found a negative correlation between basal measures of plasma or urinary cortisol and GH release in response to clonidine. Mokrani (1997) found that DST non-suppressors had a significantly lower GH response to clonidine than suppressors. Therefore, there is reasonably consistent evidence that increased cortisol secretion and/or impaired feedback reduces the GH response to clonidine. Whether this is mediated at the pituitary level or not is unclear at present.
In vitro, there is evidence that sub-chronic hydrocortisone reduces pituitary synthesis of PRL (Dannies and Tashjian 1973). In healthy humans, acute (24 h) reduction of cortisol levels by metyrapone increased the PRL response to TRH (in six healthy subjects) and the PRL response to d-fenfluramine (n=5) and enhanced the nocturnal surge of PRL secretion (Dinan and Scott 1996). Treatment for 24 h with hydrocortisone (n=6) abolished the nocturnal rise in PRL secretion and reduced the PRL response to d-fenfluramine (see Table 1). Although there was no data regarding the effects of hydrocortisone on PRL response to TRH the authors interpreted the latter finding as likely to be secondary to direct suppression at the pituitary.
Dexamethasone has been shown to blunt the PRL response to TRH (Sowers et al. 1977). In Cushing’s disease, PRL secretory dynamics are altered but there is no difference in the PRL response to TRH (Caufriez et al. 1981). Furthermore, pre-treatment with a chronic schedule of hydrocortisone (see Table 1) had no effect on the PRL response to TRH in healhy volunteers (Porter et al. 2002a).
Two studies have investigated both the PRL response to TRH and the PRL response to a 5-HT challenge in depression (Golden et al. 1990; Anderson et al. 1992). Both showed reduced PRL response to clomipramine but no difference in PRL response to TRH, in depressed subjects compared with healthy controls. In the study of Golden et al. (1990), the two challenges were carried out in the same group of patients. The data suggest that the response to TRH is unimpaired in depression therefore the blunting of PRL responses to 5-HT challenges are not mediated by dysfunction in PRL production or release from lactotrophs.
Serotonergic control of HPA axis function
Serotonin precursors
In humans, the 5-HT precursors 5-HTP and l-TRP stimulate ACTH and cortisol release, as does the 5-HT releasing agent fenfluramine and the 5-HT1A agonists ipsapirone and buspirone (Fuller 1992). However, this does not mean that serotonergic activation is physiologically necessary for cortisol secretion, either basally or during stress.
Human studies have investigated the effects of manipulation of the 5-HT system on HPA axis feedback. Maes et al. (1991a) demonstrated that in DSM-III “major depressives” but not “minor depressives” 5-HTP either augmented existing dexamethasone non-suppression or caused escape from suppression in previous non-suppressors. In a further study, this was confirmed (Maes et al. 1995), with the further finding that 5-HTP stimulated escape from suppression not only of cortisol but also of ACTH. The authors suggest that upregulation of 5-HT2 receptors in depression may mediate this effect. However, neuroendocrine challenges with large doses of 5-HTP are unphysiological and do not necessarily add evidence regarding the likely effects of more subtle fluctuations in 5-HT function. Furthermore 5-HTP may have significant catecholaminergic effects (van Praag et al. 1987).
Longer-term administration at lower doses (3.5–7 g per day for 1–2 weeks) of l-TRP in 20 depressed patients (Nuller and Ostroumova 1980) increased dexamethasone suppression of cortisol. The likely mechanism in this case is unclear. A related issue is that there is some evidence that l-TRP has antidepressant properties at least as an augmentation agent (Barker et al. 1987).
Antidepressants
In healthy volunteers and depressed subjects, acute 5-HT stimulation by various antidepressants, as with 5-HT precursors (see above), leads to an acute stimulation of ACTH and cortisol release (Laakmann 1990; Bhagwagar et al. 2002b).
Studies of both serotonergic and noradrenergic antidepressants suggest that successful treatment normalises the DST, dex/CRH and other measures of HPA axis function in depressed subjects (Greden et al. 1983; Holsboer-Trachsler et al. 1991; Inder et al. 2001). It has been suggested that this is central to their antidepressant activity (Barden et al. 1995; Holsboer and Barden 1996), something that is supported by studies suggesting that relapse is likely if HPA axis activity is not normalised (Zobel et al. 2001). Whether they do this primarily by acting on the 5-HT system or by a common activity on a cellular level is unclear (Duman et al. 1997).
Whether antidepressants with 5-HT activity affect HPA axis function in healthy subjects is not as clear although there is abundant evidence that they do this in animals (Holsboer and Barden 1996). Heuser et al. (1996) found no effect of amitriptyline on basal cortisol/ACTH or the dex/CRH test in healthy elderly subjects and Kathol et al. (1991) failed to find an effect of imipramine on HPA axis responses to insulin induced hypoglycaemia after 10 days (n=6). In contrast, Michelson et al. (1997) found that while 6 weeks treatment with imipramine did not affect basal hormones, responses to ovine CRH and arginine vasopressin (AVP) were reduced in healthy volunteers (n=14). A recent study investigated activated HPA axis function by measuring the increase in salivary cortisol that occurs in the hour following waking. While neither reboxetine nor citalopram influenced basal salivary cortisol in healthy volunteers, 6 days of treatment with citalopram significantly enhanced the increase in cortisol produced by waking while reboxetine had no effect. This argues against the hypothesis that the effect of all antidepressants is mediated via the HPA axis, suggesting that this is selective to serotonergic antidepressants (Harmer et al. 2003).
Acute tryptophan depletion
Studies using the technique of acute tryptophan depletion (ATD) have investigated the effects of reduced 5-HT transmission on HPA axis function. ATD induced an increase in cortisol levels in patients with seasonal affective disorder, which was associated with depressive relapse (Hesselmann et al. 1997). In currently depressed patients, ATD induced no change in cortisol levels (Price et al. 1997b, 1998a). Porter et al. (2002b) investigated the effects of ATD on salivary and plasma cortisol in patients with Alzheimer’s disease and healthy elderly subjects. This study also used a battery of cognitive tests that gave rise to a small rise in cortisol levels presumably secondary to the stress of testing. However, there was no effect of ATD on cortisol at any point. Miller et al. (2000) investigated the effects of ATD on cortisol in patients with panic disorder and healthy controls and found no effect of ATD on cortisol even when patients had panic attacks induced by CO2 inhalation. This procedure, however, did not raise cortisol. Sobczak et al. (2002) investigated the effects of ATD on stress induced cortisol release in 1st degree relatives of patients both with bipolar I and bipolar II disorder and in healthy volunteers. The stressor was a stress inducing speech task, which induced a robust increase in cortisol greater than that seen in the study of Porter et al. (2002b). This was attenuated by ATD in the subjects with a family history but not in control subjects. However, a report of a larger number of control subjects did suggest a reduction of stress induced cortisol secretion by ATD (Riedel et al. 2002b).
Thus stress induced cortisol release may be dependent on 5-HT transmission in humans as in animals (Joseph and Kennett 1983). This may be exaggerated by 5-HT vulnerability in subjects suffering from or with a family history of affective disorder.
Summary of effects of the 5-HT system on HPA axis function
There is some evidence that reduced l-TRP availability impairs the cortisol response to stress. This may be exaggerated in subjects with an underlying vulnerability to affective disorder. Basal secretion of cortisol appears unaffected by ATD in healthy subjects and patient groups including currently depressed subjects. No studies have specifically investigated the effects of experimental reduction of 5-HT function on HPA axis feedback rather than output. Antidepressants and administration of l-TRP may normalise HPA axis feedback in depressed subjects. Whether this is by a direct 5-HT effect is unknown.
HPA axis effects on 5-HT function
Studies using experimental HPA axis manipulations
Tryptophan availability
The synthesis of 5-HT is directly dependent on the amount of l-TRP in the brain. In animals, the main metabolising enzyme of l-TRP, TRP 2,3-dioxygenase is induced by hydrocortisone (Badawy et al. 1995). This may mediate a reduction in l-TRP availability in response to hypercortisolaemia. There is no direct evidence regarding the effects of steroids on TRP 2,3-dioxygenase in man. Central l-TRP availability is mediated by entry of l-TRP into the brain which occurs via a transport mechanism in competition with five other large neutral amino acids (LNAAs) (Wurtman 1982). Glucocorticoid treatment induces hepatic and brain tyrosine aminotransferase which is the major tyrosine degrading enzyme (Hirota et al. 1985) therefore tyrosine levels may also be altered by changes in glucocorticoid levels. Tyrosine is one of the competing LNAAs and is important in the synthesis of noradrenaline and dopamine; therefore, it is useful to measure the ratio and not only l-TRP levels.
Maes (1990a) examined TRP and TYR availability after administration of 1 mg dexamethasone to patients with major depression (n=50) and controls (n=16). TRP and TYR were measured at 8:00 a.m. after administration of the dexamethasone the night before. In healthy controls, baseline amino acid levels were measured before dexamethasone testing while in depressed subjects they were measured 3 days later when residual effects on HPA axis regulation were possible. Patients with melancholia and/or psychotic features had significantly lower baseline values of l-TRP and l-TRP/LNAA compared with controls and other depressed subjects. Dexamethasone significantly reduced l-TRP and TRP/LNAA ratio and TYR and TYR/LNAA ratio. However, there was no group by treatment interaction, i.e. no differential effect in any group. In a further study, in 26 depressed patients, administration of dexamethasone also reduced availability of both TRP and TYR (Maes 1990b) (see Table 1). In contrast, two studies (Traskman-Bendz et al. 1986; Porter et al. 1999) showed no effect of dexamethasone on l-TRP levels in healthy controls. However, these studies were smaller and did not measure other LNAA levels. One study (Bhagwagar et al. 2002a) suggests an effect of administration of hydrocortisone on l-TRP levels both in healthy controls and recovered depressed subjects but our own studies do not (Porter et al. 1998, 2002a).
Responses to d-fenfluramine
d-Fenfluramine (d-FEN) causes acute release of 5-HT from presynaptic terminals and also blocks 5-HT reuptake into presynaptic terminals (Newman et al. 1998). There is further evidence that the PRL response to fenfluramine reflects release of a “functional” pool of newly synthesised 5-HT (Coccaro et al. 1998). The PRL response to d-FEN is seen as an indicator of the responsiveness of postsynaptic 5-HT2A/2C subtype receptors (Goodall et al. 1993; Coccaro et al. 1996a, 1996b) and of the general integrity of the 5-HT system. Challenge with the racemic mixture dl-fenfluramine may be contaminated by significant catecholaminergic effects (Smythe and Mitchell 1992) because l-fenfluramine releases dopamine and noradrenalin (Invernizzi et al. 1986).
Young et al. (1998) found no attenuation in d-fenfluramine induced PRL release following hydrocortisone pre-treatment for 10 days (20 mg b.d.) compared with placebo. In contrast, following acute pre-treatment with hydrocortisone (10 mg t.i.d. over 24 h), Dinan (1996) found the PRL response to be attenuated, while pre-treatment with metyrapone enhanced the response. However, metyrapone also enhanced the response to TRH, suggesting a direct effect at the pituitary level (see above).
Response to buspirone
Buspirone is a direct 5-HT1A receptor agonist, administration of which gives rise to a hypothermic response and GH and PRL responses. There is debate regarding whether pre or postsynaptic 5-HT1A receptors mediate the hypothermic response to buspirone. 5-HT1A mediated hypothermia is generally thought to be mediated by pre-synaptic receptors in animals. However, in humans, the technique of acute tryptophan depletion does not attenuate the hypothermic response (Blier et al. 2002), suggesting a direct post-synaptic action. Other problems in interpretation of neuroendocrine responses to buspirone are that it also acts as a dopamine-D2 receptor antagonist (Gregory et al. 1990; Meltzer et al. 1992), has a pharmacologically active metabolite 1-pyrimidinylpiperazine (1-PP) (Mahmood and Sahajwalla 1999), and may have 5-HT1A partial agonist properties. Furthermore, the neuroendocrine findings in depressed patients with this drug have been inconsistent (Power and Cowen 1992).
Young (1994) investigated the effects on responses to buspirone of treatment with hydrocortisone, 20 mg twice a day for 1 week, in 11 healthy volunteers. There was no blunting of GH or PRL responses following hydrocortisone compared with placebo. However, there was blunting of the hypothermic response. A possible explanation is that hormonal responses are mediated by post-synaptic 5-HT1A receptors while hypothermia is mediated by pre-synaptic receptors and that the function of these is attenuated by sub-acute hydrocortisone. As discussed above, the origin of the hypothermic response is still unclear.
Responses to ipsapirone
Ipsapirone is a partial 5-HT1A agonist. It appears to have negligible affinity for the 5-HT1D, 5-HT2 or 5-HT3 subtypes (Peroutka 1988). At doses of 0.3 mg/kg it induces a hypothermic response that is blocked by pindolol (a 5-HT1A antagonist and β-adreno receptor antagonist). There is also an ACTH, cortisol and GH response in normal human subjects but not a reliable PRL response (Lesch et al. 1989b). The origin of the hypothermic response (whether pre- or post-synaptic) is not entirely clear.
Price et al. (1997a) investigated the effects of administration of the cortisol synthesis-inhibitor, ketoconazole (1000 mg over 24 h prior to neuroendocrine testing with ipsapirone, in a double-blind, placebo controlled study) to healthy controls and depressed subjects. In neither group were the non-HPA responses enhanced. As expected, the cortisol response was inhibited while the ACTH response was enhanced (presumably a result of reduced negative feedback).
Responses to l-TRP
In humans, intravenous infusion of 7 g l-TRP over 20 min causes a robust increase in GH and PRL (Charney and Heninger 1982). The GH response has been shown to be particularly sensitive to blockade by the 5-HT1A antagonist, pindolol (Smith et al. 1991) and hence is likely to be mediated by the 5-HT1A receptor. The PRL response is less blunted by pindolol, suggesting an additional component. It is, however, abolished by metergoline (McCance et al. 1987). This may suggest that a receptor other than the 5-HT1A receptor plays a role in the response. Since l-TRP competes with tyrosine for transport across the blood-brain barrier (Wurtman 1982) infusion may reduce dopamine synthesis by reducing brain tyrosine. Evidence suggests that loading with LNAAs other than tyrosine selectively reduces dopamine rather than noradrenalin function (McTavish et al. 2001). That this occurs during IV infusion of l-TRP is supported by evidence that an infusion of 5 g l-TRP causes a reduction in post-probenecid cerebrospinal fluid (CSF) concentrations of the dopamine metabolite homovanillic acid (HVA) (van Praag et al. 1987). The PRL response to l-TRP may therefore be mediated, in part, by a reduction in dopamine synthesis, which releases PRL secretion from tonic inhibition by dopamine.
In healthy volunteers, pre-treatment 10 h before infusion with dexamethasone (1 mg) compared with placebo, resulted in a significantly greater PRL response, but no effect on GH response (Traskman-Bendz et al. 1986). In contrast, 5 mg dexamethasone in healthy volunteers (11 h before infusion) reduced the PRL response even when an increased baseline PRL was taken into account (Porter et al. 1999). The degree of entry of dexamethasone into the brain at different doses is not known. A possible interpretation of the difference in these studies is that 5 mg is sufficient to enter the brain and bind to GRs to a significant extent, while 1 mg is not.
We found a reduction in GH but not PRL response to l-TRP in healthy volunteers following pre-treatment with hydrocortisone (100 mg) 11 h before infusion (Porter et al. 1998). A similar result was found with the sub-chronic schedule (20 mg b.d. for 1 week) (Porter et al. 2002a). Both can be interpreted as an effect at the pituitary level, given the finding of a similar effect of the same pre-treatments on GHRH mediated GH release (Watson et al. 2000).
Bhagwagar (2002a) used a similar acute pre-treatment schedule to investigate subjects who had recovered from depression and had a history of at least two episodes, compared with healthy controls. Hydrocortisone (50 mg orally) compared with placebo 10.5 h before IV l-TRP, reduced GH release in the recovered depressives, but not significantly, and significantly increased GH release in controls.
There was a reduction of peripheral tryptophan in both groups following treatment with hydrocortisone. Plasma TRP after infusion was significantly lower in the depressed patients than the control subjects. This is surprising given the very large and equal amounts of IV l-TRP given to both groups. Baseline measures of cortisol were taken only immediately prior to the infusion and there were no differences between groups following either placebo or hydrocortisone. A possible interpretation of the findings of the increased GH responses after pre-treatment with hydrocortisone in controls but not recovered depressives is that healthy control subjects were able to up-regulate 5-HT1A function in response to hydrocortisone, while recovered depressed subjects were unable to mount such a response. It could also be that the results reflect a failure of adaptation of pituitary mediated GH release in response to hydrocortisone pre-treatment in depressed subjects. A further interpretation is that the treatment altered cortisol rhythms in a different way in recovered depressed subjects compared with control subjects and that this is the origin of the difference in response to l-TRP rather than there being a different adaptive response to an equal change in cortisol levels.
5-HT1A receptor binding
Animal studies suggest that both function and numbers of post synaptic 5-HT1A receptors are affected by alterations in HPA axis function. For example, postsynaptic 5-HT1A receptor binding is increased following adrenalectomy, an effect that is reversed by administration of corticosterone (de Kloet et al. 1986; Martire et al. 1989; Mendelson and McEwen 1992a; Kuroda et al. 1994). Chronic administration of corticosterone causes a reduction in the expression of post-synaptic 5-HT1A receptor mRNA (Meijer and de Kloet 1994) and binding to 5-HT1A receptors (Mendelson and McEwen 1992b).
In humans, Montgomery et al. (2001), using PET scanning techniques, showed no reduction in 5-HT1A binding following pre-treatment with hydrocortisone (100 mg taken 11.5 h before testing) compared with placebo (the study was specifically designed to be analogous to Porter et al. 1998). In addition, a small group of patients on chronic prednisone therapy and a single patient with Cushing’s disease were tested and found to have no difference in 5-HT1A binding compared with age matched controls.
EEG measures of 5-HT function
McAllister-Williams and Massey have demonstrated that buspirone and pindolol administration to healthy subjects engenders a shift in the EEG frequency spectrum and suggest that this may reflect somatodendritic 5-HT1A receptor function (McAllister-Williams and Massey 2003). This group has recently demonstrated that this effect is significantly attenuated by pre-treatment with a sub-acute schedule of hydrocortisone for 7 days (Fairchild et al. 2003).
Studies in depression correlating HPA axis measures with 5-HT function
Tryptophan availability
In three separate studies, Maes et al. (1987b, 1988, 1990c) investigated the relationship between post-dexamethasone cortisol and TRP/LNAA ratio in depression. Cortisol responses to dexamethasone were significantly and negatively associated with availability of l-TRP in all three studies (Table 2). However, in Maes et al. (1990c) there was no correlation between TRP/LNAA ratio and basal plasma cortisol (8:00 a.m.) and three further studies have failed to find a correlation between TRP/LNAA ratio and measures of basal cortisol output. Maes et al. (1990b), in a relatively small study (26 patients), found no correlation with 24-h urinary cortisol and Mulder et al. (2003) in 100 depressed subjects found no correlation between baseline plasma cortisol (average of three morning measures) and TRP/LNAA ratio (data regarding this correlation not reported in the original report: but see Table 2). Strickland et al. (2002) found no correlation between salivary cortisol throughout the day and l-TRP availability in depressed and healthy women (P. Strickland, personal communication). In a group of carers of patients with dementia, Da Roza Davis and Cowen (2001) did demonstrate raised cortisol secretion as measured by midday and 10:00 p.m. salivary cortisol and reduced total plasma tryptophan but there was no correlation between the two measures. Several other studies have measured tryptophan levels or availability and HPA axis function in depression but not reported on correlations between the two that may therefore be lacking (Cowen and Charig 1987; Price et al. 1991).
In summary, there appears to be a degree of consistency of a finding of a negative correlation between HPA axis activity and l-TRP availability when measures of HPA axis feedback rather than cortisol output are used. A possible interpretation of this is that rather than high cortisol levels reducing l-TRP availability, low l-TRP availability leads to impaired glucocorticoid mediated inhibitory feedback on the HPA axis and therefore resistance to dexamethasone suppression. Based on animal evidence (Budziszewska et al. 1995), it has been suggested that reduced activation of 5-HT1A receptors in the hippocampus may be responsible for impaired feedback at this level which in turn leads to activation of the HPA axis (McAllister-Williams et al. 1998).
Response to 5-HTP
Evidence suggests that the PRL response to 5-HTP is mediated by 5-HT1A receptors, while the cortisol response is not (Meltzer and Maes 1994). Interpretation of responses to 5-HTP may be complicated by a lack of 5-HT specificity. 5-HT is taken up by catecholaminergic as well as 5-HT neurones (Fuxe et al. 1971) and may thus release dopamine and noradrenalin by displacement. There is evidence that at the doses used in challenge tests there are significant catecholaminergic effects in humans (van Praag et al. 1987).
Maes (1990c), in 64 depressed females, showed that the cortisol response to 5-HTP was not related to l-TRP availability or to post-dexamethasone cortisol. They do not report on the relationship with the PRL response. Meltzer et al. (1984) also failed to find a relationship between cortisol response to 5-HTP and post-dexamethasone cortisol in depressed patients. However, there was a significant negative correlation between baseline cortisol and cortisol response to 5-HTP in healthy controls. The degree to which the cortisol response depends on the feedback status of the HPA axis rather than effects of cortisol on 5-HT function is not clear.
Responses to d-fenfluramine
Mitchell and Smythe (1990) found a negative correlation between the PRL response to dl-fenfluramine and baseline cortisol (average of three measures 9–10 a.m.). This correlation was found in a combined group of 27 depressed patients and 14 healthy controls (presumably there was no interaction between diagnostic group and baseline cortisol in the ANCOVA, although this is not explicitly stated), but this was only significant when one outlying depressed patient was excluded. Rajewska et al. (2003) found an inverse relationship between the PRL and cortisol responses to d-fenfluramine and baseline cortisol in a combined group of post-menopausal depressed women (n=60) and controls (n=30).
In contrast, Park et al. (1996) found no correlation between baseline cortisol and PRL or cortisol response to d-fenfluramine in either 31 depressed or 29 control subjects and Duval et al. found no correlation between hormonal responses to d-fenfluramine and cortisol levels (basal or post-DST) in 71 drug-free depressed and 34 hospitalised healthy control subjects (Duval et al. 2001). Maes et al. (1991b) found no relationship between 8:00 a.m. post-dexamethasone cortisol and responses to d-fenfluramine in controls, minor depressives, simple major and melancholic depressives (DSM-III; American Psychiatric Association 1980).
Mulder et al. (2003), in a study of 108 outpatients with DSM-III-R major depression, showed an interaction between baseline cortisol (three single morning measurements) and DSM-III-R melancholic sub-type of depression. Non-melancholic patients showed a positive correlation and melancholic patients a negative correlation between the PRL response to fenfluramine and basal cortisol levels. A possible interpretation of these results is that there is a difference between melancholic and non-melancholic subjects in their ability to alter sensitivity of 5-HT2C receptors in response to alterations in cortisol levels. Thus, non-melancholic subjects appear to increase 5-HT2C receptor function in response to high cortisol while the opposite is the case for melancholic subjects. It should be noted that this study used the less selective racemic mixture dl-fenfluramine and may be contaminated by noradrenergic effects.
A recent study by Strickland et al. (2002) demonstrated an increased response to d-fenfluramine in depressed women compared with large numbers of control women. The study employed a placebo control and co-varied for d-fenfluramine and baseline PRL levels and was therefore particularly methodologically robust. However, the depression was relatively mild, only eight of 20 women meeting DSM-IV criteria for depression (20 in total met ICD-10 criteria). The same group had a reduced average morning serum cortisol compared with non-depressed subjects. Baseline plasma cortisol was not a significant covariate in analysis of the PRL response to fenfluramine and there was no correlation between salivary cortisol levels over the preceding days and PRL response to fenfluramine (P. Strickland, personal communication).
Responses to 5-HT1A receptor agonists
Pichot (2001) used neuroendocrine challenge with the specific 5-HT1A receptor agonist flesinoxan, in 21 depressed in-patients. There was no relationship between cortisol, ACTH, PRL and hypothermic responses and post-dexamethasone cortisol. Although the authors go on to report a significant difference in ACTH response between DST suppressors and non-suppressors (suppressors had a significantly higher response), none of the other responses were significantly different between these groups. Shapira et al. (2000) showed an inverse correlation between cortisol response to ipsapirone and baseline plasma cortisol. Correlations with the GH or hypothermic responses are not reported. In both studies, responses could have been inhibited by negative feedback by cortisol at the pituitary level.
In 50 healthy volunteers, buspirone-induced PRL response was highly negatively correlated with a single morning measure of plasma cortisol (Dinan et al. 2001).
Responses to l-TRP
Four studies have investigated the relationship between HPA axis function and hormonal responses to IV l-TRP. Deakin et al. (1990) found that increased baseline cortisol levels were associated with reduced PRL responses, but there was no association with GH responses. Cowen and Charig (1987) found that DST non-suppressors had greater PRL responses than DST suppressors but there was no difference in GH response. Price et al. (1991) showed a negative correlation between post-dexamethasone cortisol and GH response, but no correlation with PRL response. Porter et al. (2003) found an increased PRL response to IV l-TRP in depressed patients compared with control subjects. Across both groups, there was an inverse correlation between PRL response and total salivary cortisol secretion (measured at 8:00 a.m., midday, 4:00 p.m. and 8:00 p.m. over 3 days prior to testing). Depressed subjects did not, in this study, secrete more cortisol than control subjects. Our preferred interpretation of this finding is that it reflects an effect of cortisol secretion, within a normal physiological range, on dopamine function rather than on 5-HT1A function.
Summary
Both acute and sub-acute treatment with hydrocortisone reduce GHRH mediated GH release. This is therefore likely to be an important factor in alterations in GH release in response to 5-HT neuroendocrine challenge agents following treatment with hydrocortisone. This is less likely to be the case when PRL is used as a measure. It is unlikely that measuring HPA axis hormonal output (cortisol and ACTH) following 5-HT stimulation will give rise to useful data regarding the relationship between the two systems.
Effects of manipulations of corticosteroids on other responses are inconsistent, although generally there is no effect especially following sub-acute manipulations. This probably reflects the ability of healthy subjects to compensate for such manipulations. The study of Bhagwagar et al (2002a) suggests that healthy subjects may up-regulate 5-HT1A receptor function in response to acute pre-treatment with hydrocortisone while subjects with a recurrent depressive illness do not. This is of interest since the study of Smith et al. (2000) suggests that subjects with previous depression are less able to up-regulate 5-HT1A receptor function in response to low TRP than healthy controls. These two challenges may be linked, since studies in depressed subjects have suggested that TRP availability correlates with measures of HPA axis feedback. That this is the case while there is no good evidence of a correlation between l-TRP availability and measures of cortisol output suggests that the link may be via control of HPA axis feedback by the 5-HT system.
Apart from the relationship between l-TRP availability and HPA axis feedback noted above, studies investigating correlations between HPA axis measures and 5-HT measures are inconsistent. This is perhaps not surprising given the inconsistent evidence regarding abnormalities of 5-HT neuroendocrine challenge tests in depression. The most consistent findings have been of reduced responses (GH and/or PRL) to IV l-TRP thought to reflect reduced 5-HT1A function in depression. Much animal research has focused on corticosteroid effects on the 5-HT1A receptor, which is believed to mediate these responses. However, there is no consistent evidence of a relationship between HPA axis function and these responses to IV l-TRP
One study (Mulder et al. 2003) suggests that there may be a difference in the ability of the 5-HT system to adapt to altered cortisol levels between melancholic and non-melancholic patients. Whether this reflects a distinct abnormality in melancholia or a one end of a spectrum of failure of homeostatic mechanisms in depression is not clear.
Future research
Animal studies have convincingly demonstrated bi-directional interactions between the HPA axis and the serotonin system. In humans, existing neuroimaging methods are able to examine only structural rather than functional changes and the validity of newer methods of examining brain function has not yet been proven. There are methodological difficulties inherent in examining these systems using traditional neuroendocrine methods. Data from existing neuroendocrine research needs to be considered in light of these and non-neuroendocrine models of receptor function such as EEG measures of 5-HT function (McAllister-Williams and Massey 2003) may be more suited to investigate this further. Future studies might also use more sophisticated methods of manipulating and measuring the HPA axis and 5-HT system, for instance flattening the diurnal cortisol rhythm using the model piloted in laboratory rats by Leitch et al. (2003) and using more selective serotonergic agonists. Further investigation of the effects of low l-TRP availability on HPA axis function is also likely to be useful.
References
American Psychiatric Association (1980) Diagnostic and statistical manual of mental disorders DSM-III, 3rd edn. American Psychiatric Association, Arlington, Va.
Amsterdam JD, Maislin G (1990) Comparison of growth hormone response after clonidine and insulin hypoglycemia in affective illness. Biol Psychiatry 28:308–314
Anderson IM, Ware CJ, da Roza Davis JM, Cowen PJ (1992) Decreased 5-HT-mediated prolactin release in major depression. Br J Psychiatry 160:372–378
Badawy AA, Morgan CJ, Lovett JW, Bradley DM, Thomas R (1995) Decrease in circulating tryptophan availability to the brain after acute ethanol consumption by normal volunteers: implications for alcohol-induced aggressive behaviour and depression. Pharmacopsychiatry 28:93–97
Barden N, Reul JM, Holsboer F (1995) Do antidepressants stabilize mood through actions on the hypothalamic-pituitary-adrenocortical system? Trends Neurosci 18:6–11
Barker WA, Scott J, Eccleston D (1987) The Newcastle chronic depression study: results of a treatment regime. Int Clin Psychopharmacol 2:261–272
Bhagwagar Z, Hafizi S, Cowen PJ (2002a) Cortisol modulation of 5-HT-mediated growth hormone release in recovered depressed patients. J Affect Disord 72:249–255
Bhagwagar Z, Whale R, Cowen PJ (2002b) State and trait abnormalities in serotonin function in major depression. Br J Psychiatry 180:24–28
Birmaher B, Dahl RE, Williamson DE, Perel JM, Brent DA, Axelson DA, Kaufman J, Dorn LD, Stull S, Rao U, Ryan ND (2000) Growth hormone secretion in children and adolescents at high risk for major depressive disorder. Arch Gen Psychiatry 57:867–872
Birmaher B, Dahl RE, Ryan ND, Williamson DE (2002) The role of hypothalamic-pituitary-adrenal axis dysfunction in the attenuated growth hormone response in adolescents with familial loading for affective disorder: in reply. Arch Gen Psychiatry 59:187
Blier P, Seletti B, Gilbert F, Young SN, Benkelfat C (2002) Serotonin 1A receptor activation and hypothermia in humans: Lack of evidence for a presynaptic mediation. Neuropsychopharmacology 27:301–308
Budziszewska B, Siwanowicz J, Przegaliski E (1995) Role of the serotoninergic system in the regulation of glucocorticoid and mineralocorticoid receptors in the rat hippocampus. Pol J Pharmacol 47:299–304
Burguera B, Muruais C, Penalva A, Dieguez C, Casanueva FF (1990) Dual and selective actions of glucocorticoids upon basal and stimulated growth hormone release in man. Neuroendocrinology 51:51–58
Casanueva FF, Burguera B, Tome MA, Lima L, Tresguerres JA, Devesa J, Dieguez C (1988) Depending on the time of administration, dexamethasone potentiates or blocks growth hormone-releasing hormone-induced growth hormone release in man. Neuroendocrinology 47:46–49
Caufriez A, Desir D, Szyper M, Robyn C, Copinschi G (1981) Prolactin secretion in Cushing’s disease. J Clin Endocrinol Metab 53:843–846
Chaouloff F (1993) Physiopharmacological interactions between stress hormones and central serotonergic systems. Brain Res Brain Res Rev 18:1–32
Chaouloff F (2000) Serotonin, stress and corticoids. J Psychopharmacol 14:139–151
Charney DS, Heninger GR (1982) The effect of IV l-tryptophan on prolactin, growth hormone, and mood in healthy subjects. Psychopharmacology 78:38–43
Chernow B, Alexander HR, Smallridge RC, Thompson WR, Cook D, Beardsley D, Fink MP, Lake CR, Fletcher JR (1987) Hormonal responses to graded surgical stress. Arch Int Med 147:1273–1278
Cleare AJ, Murray RM, O’Keane V (1996) Reduced prolactin and cortisol responses to d-fenfluramine in depressed compared to healthy matched control subjects. Neuropsychopharmacology 14:349–354
Coccaro EF, Kavoussi RJ, Cooper TB, Hauger R (1996a) 5-HT3 receptor antagonism by ondansetron does not attenuate prolactin response to d-fenfluramine challenge in healthy human subjects. Psychopharmacology 127:108–112
Coccaro EF, Kavoussi RJ, Oakes M, Cooper TB, Hauger R (1996b) 5-HT2A/2C receptor blockade by amesergide fully attenuates prolactin response to d-fenfluramine challenge in physically healthy human subjects. Psychopharmacology 126:24–30
Coccaro EF, Kavoussi RJ, Cooper TB, Hauger R (1998) Acute tryptophan depletion attenuates the prolactin response to d-fenfluramine challenge in healthy human subjects. Psychopharmacology 138:9–15
Cowen PJ (1996) The serotonin hypothesis: necessary but not sufficient. In: Feighner J, Boyer W (eds) Selective serotonin reuptake inhibitors. Wiley, Chichester, pp 63–86
Cowen PJ, Charig EM (1987) Neuroendocrine responses to intravenous tryptophan in major depression. Arch Gen Psychiatry 44:958–66
Da Roza Davis JM, Cowen PJ (2001) Biochemical stress of caring. Psychol Med 31:1475–1478
Dannies PS, Tashjian AR Jr (1973) Effects of thyrotropin-releasing hormone and hydrocortisone on synthesis and degradation of prolactin in a rat pituitary cell strain. J Biol Chem 248:6174–9
de Kloet ER, Sybesma H, Reul HM (1986) Selective control by corticosterone of serotonin1 receptor capacity in raphé-hippocampal system. Neuroendocrinology 42:513–521
Deakin JF, Pennell I, Upadhyaya AJ, Lofthouse R (1990) A neuroendocrine study of 5HT function in depression: evidence for biological mechanisms of endogenous and psychosocial causation. Psychopharmacology 101: 85–92
Deuschle M, Schweiger U, Weber B, Gotthardt U, Korner A, Schmider J, Standhardt H, Lammers CH, Heuser I (1997) Diurnal activity and pulsatility of the hypothalamus-pituitary-adrenal system in male depressed patients and healthy controls. J Clin Endocrinol Metab 82:234–238
Dinan TG (1994) Glucocorticoids and the genesis of depressive illness. A psychobiological model Br J Psychiatry 164:365–371
Dinan TG, Scott LV (1996) The influence of cortisol on spontaneous and 5HT stimulated prolactin release in man. J Basic Clin Physiol Pharmacol 7:45–56
Dinan TG, Thakore J, V OK (1994) Lowering cortisol enhances growth hormone response to growth hormone releasing hormone in healthy subjects. Acta Physiol Scand 151:413–416
Dinan TG, Scott LV, Thakore J, Naesdal J, Keeling PW (2001) Impact of cortisol on buspirone stimulated prolactin release: a double-blind placebo-controlled study. Psychoneuroendocrinology 26:751–756
Dolan RJ, Calloway SP (1986) The human growth hormone response to clonidine: relationship to clinical and neuroendocrine profile in depression. Am J Psychiatry 143:772–774
Drevets WC, Frank E, Price JC, Kupfer DJ, Holt D, Greer PJ, Huang Y, Gautier C, Mathis C (1999) PET imaging of serotonin 1A receptor binding in depression. Biol Psychiatry 46:1375–1387
Duman RS, Heninger GR, Nestler EJ (1997) A molecular and cellular theory of depression. Arch Gen Psychiatry 54:597–606
Duval F, Mokrani MC, Correa H, Bailey P, Valdebenito M, Monreal J, Crocq MA, Macher JP (2001) Lack of effect of HPA axis hyperactivity on hormonal responses to d-fenfluramine in major depressed patients: implications for pathogenesis of suicidal behaviour. Psychoneuroendocrinology 26:521–537
Fairchild GF, Massey AE, Hsu FC, McAllister-Williams RH (2003) Repeated cortisol administration attenuates 5HT1A autoreceptor function in humans. J Psychopharmacol 17:A76
Frantz AG, Rabkin JG (1964) Clinical Measurement, response to hypoglycaemia and suppression by corticosteroids. N Engl J Med 271:1375–1381
Fuller RW (1992) The involvement of serotonin in regulation of pituitary-adrenocortical function. Front Neuroendocrinol 13:250–270
Fuxe K, Butcher LL, Engel J (1971) dl-5-Hydroxytryptophan-induced changes in central monoamine neurons after peripheral decarboxylase inhibition. J Pharm Pharmacol 23:420–424
Giustina A, Romanelli G, Candrina R, Giustina G (1989) Growth hormone deficiency in patients with idiopathic adrenocorticotropin deficiency resolves during glucocorticoid replacement. J Clin Endocrinol Metab 68:120–124
Giustina A, Doga M, Bodini C, Girelli A, Legati F, Bossoni S, Romanelli G (1990) Acute effects of cortisone acetate on growth hormone response to growth hormone-releasing hormone in normal adult subjects. Acta Endocrinol 122:206–210
Gold PW, Loriaux DL, Roy A, Kling MA, Calabrese JR, Kellner CH, Nieman LK, Post RM, Pickar D, Gallucci W (1986) Responses to corticotropin-releasing hormone in the hypercortisolism of depression and Cushing’s disease. Pathophysiologic and diagnostic implications. N Engl J Med 314:1329–1335
Golden RN, Ruegg R, Brown TM, Haggerty J, Jr., Garbutt JC, Pedersen CA, Evans DL (1990) Abnormal neuroendocrine responsivity to clomipramine in depression. Psychopharmacol Bull 26:317–320
Goodall EM, Cowen PJ, Franklin M, Silverstone T (1993) Ritanserin attenuates anorectic, endocrine and thermic responses to d-fenfluramine in human volunteers. Psychopharmacology 112:461–466
Greden JF, Gardner R, King D, Grunhaus L, Carroll BJ, Kronfol Z (1983) Dexamethasone suppression tests in antidepressant treatment of melancholia. The process of normalization and test-retest reproducibility. Arch Gen Psychiatry 40:493–500
Gregory CA, Anderson IM, Cowen PJ (1990) Metergoline abolishes the prolactin response to buspirone. Psychopharmacology 100:283–284
Guazzo EP, Kirkpatrick PJ, Goodyer IM, Shiers HM, Herbert J (1996) Cortisol, dehydroepiandrosterone (DHEA), and DHEA sulfate in the cerebrospinal fluid of man: relation to blood levels and the effects of age. J Clin Endocrinol Metab 81:3951–3960
Harmer CJ, Bhagwagar Z, Shelley N, Cowen PJ (2003) Contrasting effects of citalopram and reboxetine on waking salivary cortisol. Psychopharmacology 167:112–114
Heninger GR, Charney DS, Price L, Delgado P, Woods S, Goodman W (1990) Neuroendocrine effects of serotonin agonists in rhesus monkeys, healthy humans and patients with depression or anxiety disorders: effects of anti-depressant treatment. In: Paoletti R, Vanhoutte PM, Brunello N, Maggi FM (eds) Serotonin: cell biology to pharmacology and therapeutics. Kluwer Acadmic, Dordrecht, pp 559–563
Hesselmann B, Neumeister A, Praschak-Rieder N, Vitouch O, Kasper S (1997) Cortisol concentration during tryptophan depletion in depressed and remitted patients with seasonal affective disorder (SAD) 6th World Congress of Biological Psychiatry, Nice, pp 39–123
Heuser I, Yassouridis A, Holsboer F (1994) The combined dexamethasone/CRH test: a refined laboratory test for psychiatric disorders. J Psychiatr Res 28:341–356
Heuser IJ, Schweiger U, Gotthardt U, Schmider J, Lammers CH, Dettling M, Yassouridis A, Holsboer F (1996) Pituitary-adrenal-system regulation and psychopathology during amitriptyline treatment in elderly depressed patients and normal comparison subjects. Am J Psychiatry 153:93–99
Hirota T, Hirota K, Sanno Y, Tanaka T (1985) A new glucocorticoid receptor species: relation to induction of tryptophan dioxygenase by glucocorticoids. Endocrinology 117:1788–1795
Holsboer F, Barden N (1996) Antidepressants and hypothalamic-pituitary-adrenocortical regulation. Endocrine Rev 17:187–205
Holsboer F, Von Bardeleben U, Gerken A, Stalla GK, Muller OA (1984) Blunted corticotropin and normal cortisol response to human corticotropin-releasing factor in depression. N Engl J Med 311:1127
Holsboer F, Lauer CJ, Schreiber W, Krieg JC (1995) Altered hypothalamic-pituitary-adrenocortical regulation in healthy subjects at high familial risk for affective disorders. Neuroendocrinology 62:340–347
Holsboer-Trachsler E, Stohler R, Hatzinger M (1991) Repeated administration of the combined dexamethasone-human corticotropin releasing hormone stimulation test during treatment of depression. Psychiatry Res 38:163–171
Inder WJ, Prickett TC, Mulder RT, Donald RA, Joyce PR (2001) Reduction in basal afternoon plasma ACTH during early treatment of depression with fluoxetine. Psychopharmacology 156:73–78
Invernizzi R, Berettera C, Garattini S, Samanin R (1986) d- and l-isomers of fenfluramine differ markedly in their interaction with brain serotonin and catecholamines in the rat. Eur J Pharmacol 120:9–15
Joseph MH, Kennett GA (1983) Corticosteroid response to stress depends upon increased tryptophan availability. Psychopharmacology 79:79–81
Kahn RS, Wetzler S, Asnis GM, Papolos D, Van Praag HM (1990) Serotonin receptor sensitivity in major depression. Biol Psychiatry 28:358–362
Kasuya Y, Iwano M, Shibasaki H, Furuta T (1995) Pharmacokinetic studies of cortisol after oral administration of deuterium-labelled cortisol to a normal human subject. Rapid Commun Mass Spectrom Spec No: S29–34
Kathol RG, Jaeckle R, Wysham C, Sherman B (1991) Imipramine effect on the hypothalamic-pituitary-adrenal axis response to hypoglycemia. Psychiatry Res 41:2–52
Koyama T, Meltzer H (1986) A biochemical and neuroendocrine study of the serotonergic system in depression. In: Hippius H et al. (eds) New results in depression research. Springer, Berlin, Heidelberg, New York, pp 169–188
Kuroda Y, Watanabe Y, Albeck DS, Hastings NB, McEwen BS (1994) Effects of adrenalectomy and type I or type II glucocorticoid receptor activation on 5-HT1A and 5-HT2 receptor binding and 5-HT transporter mRNA expression in rat brain. Brain Res 648:157–61
Laakmann G (1990) Psychopharmacoendocrinology and depression research. Springer-Verlag, Berlin, Heidelberg, New York
Leitch MM, Ingram CD, Young AH, McQuade R, Gartside SE (2003) Flattening the corticosterone rhythm attenuates 5HT1A autoreceptor function in the rat: relevance for depression. Neuropsychopharmacology 28:119–125
Lesch KP, Muller U, Rupprecht R, Kruse K, Schulte HM (1989a) Endocrine responses to growth hormone-releasing hormone, thyrotropin-releasing hormone and corticotropin-releasing hormone in depression. Acta Psychiatr Scand 79:597–602
Lesch KP, Rupprecht R, Poten B, Muller U, Sohnle K, Fritze J, Schulte HM (1989b) Endocrine responses to 5-hydroxytryptamine-1A receptor activation by ipsapirone in humans. Biol Psychiatry 26:203–205
Lesch KP, Disselkamp-Tietze J, Schmidtke A (1990) 5-HT1A receptor function in depression: effect of chronic amitriptyline treatment. J Neural Transm [Gen Sect] 80:157–161
Maes M, Meltzer HY (1995) The serotonin hypothesis of major depression. In: Bloom FE, Kupfer DJ (eds) Psychopharmacology: the fourth generation of progress. Raven Press, New York, pp 933–944
Maes M, De Ruyter M, Claes R, Bosma G, Suy E (1987a) The cortisol responses to 5-hydroxytryptophan, orally, in depressive inpatients. J Affect Disord 13:23–30
Maes M, De Ruyter M, Hobin P, Suy E (1987b) Relationship between the dexamethasone suppression test and the l-tryptophan/competing amino acids ratio in depression. Psychiatry Res 21:323–335
Maes M, De Ruyter M, Claes R, Suy E (1988) Sex-related differences in the relationships between self-rated depression and biological markers. J Affect Disord 15:119–25
Maes M, Jacobs MP, Suy E, Minner B, Leclercq C, Christiaens F, Raus J (1990a) Suppressant effects of dexamethasone on the availability of plasma l-tryptophan and tyrosine in healthy controls and in depressed patients. Acta Psychiatr Scand 81:19–23
Maes M, Schotte C, Scharpe S, Martin M, Blockx P (1990b) The effects of glucocorticoids on the availability of l-tryptophan and tyrosine in the plasma of depressed patients. J Affect Disord 18:121–127
Maes M, Vandewoude M, Schotte C, Maes L, Martin M, Scharpe S, Blockx P (1990c) The relationships between the cortisol responses to dexamethasone and to l-5-HTP, and the availability of l-tryptophan in depressed females. Biol Psychiatry 27:601–608
Maes M, D’Hondt P, Martin M, Claes M, Schotte C, Vandewoude M, Blockx P (1991a) l-5-Hydroxytryptophan stimulated cortisol escape from dexamethasone suppression in melancholic patients. Acta Psychiatr Scand 83:302–306
Maes M, D’Hondt P, Suy E, Minner B, Vandervorst C, Raus J (1991b) HPA-axis hormones and prolactin responses to dextro-fenfluramine in depressed patients and healthy controls. Prog Neuropsychopharmacol Biol Psychiatry 15:781–790
Maes M, Meltzer HY, P DH, Cosyns P, Blockx P (1995) Effects of serotonin precursors on the negative feedback effects of glucocorticoids on hypothalamic-pituitary-adrenal axis function in depression. Psychoneuroendocrinology 20:149–167
Mahmood I, Sahajwalla C (1999) Clinical pharmacokinetics and pharmacodynamics of buspirone, an anxiolytic drug. Clin Pharmacokinet 36:277–287
Martire M, Pistritto G, Preziosi P (1989) Different regulation of serotonin receptors following adrenal hormone imbalance in the rat hippocampus and hypothalamus. J Neural Transm 78:109–120
Matussek N, Ackenheil M, Hippius H, Muller F, Schroder HT, Schultes H, Wasilewski B (1980) Effect of clonidine on growth hormone release in psychiatric patients and controls. Psychiatry Res 2:25–36
McAllister-Williams RH, Massey AE (2003) EEG effects of buspirone and pindolol: a method of examining 5-HT1A receptor function in humans. Psychopharmacology 166:284–293
McAllister-Williams RH, Ferrier IN, Young AH (1998) Mood and neuropsychological function in depression: the role of corticosteroids and serotonin. Psychol Med 28:573–584
McCance SL, Cowen PJ, Waller H, Grahame-Smith DG (1987) The effects of metergoline on endocrine responses to l-tryptophan. J Psychopharmacol 2:90–94
McTavish SFB, McPherson MH, Harmer CJ, Clark L, Sharp T, Goodwin GM, Cowen PJ (2001) Antidopaminergic effects of dietary tyrosine depletion in healthy subjects and patients with manic illness. Br J Psychiatry 179:356–360
Meijer OC, de Kloet ER (1994) Corticosterone suppresses the expression of 5-HT1A receptor mRNA in rat dentate gyrus. Eur J Pharmacol 266:255–261
Meijer OC, de Lange EC, Breimer DD, de Boer AG, Workel JO, de Kloet ER (1998) Penetration of dexamethasone into brain glucocorticoid targets is enhanced in mdr1A P-glycoprotein knockout mice. Endocrinology 139:1789–1793
Meltzer HY, Maes M (1994) Effect of pindolol on the l-5-HTP-induced increase in plasma prolactin and cortisol concentrations in man. Psychopharmacology 114:635–643
Meltzer HY, Maes M (1995) Effects of ipsapirone on plasma cortisol and body temperature in major depression. Biol Psychiatry 38:450–457
Meltzer HY, Umberkoman-Wiita B, Robertson A, Tricou BJ, Lowy M, Perline R (1984) Effect of 5-hydroxytryptophan on serum cortisol levels in major affective disorders. I. Enhanced response in depression and mania. Arch Gen Psychiatry 41:366–374
Meltzer HY, Hong Shick L, Nash Jr JF, Coccaro EF, Gabriel S, Mahon T, Macaluso J, Siever LJ (1992) Effect of buspirone on prolactin secretion is not mediated by 5-HT1A receptor stimulation. Arch Gen Psychiatry 49:163–164
Mendelson SD, McEwen BS (1992a) Autoradiographic analyses of the effects of adrenalectomy and corticosterone on 5-HT1A and 5-HT1B receptors in the dorsal hippocampus and cortex of the rat. Neuroendocrinology 55:444–450
Mendelson SD, McEwen BS (1992b) Quantitative autoradiographic analyses of the time course and reversibility of corticosterone-induced decreases in binding at 5-HT1A receptors in rat forebrain. Neuroendocrinology 56:881–888
Michelson D, Galliven E, Hill L, Demitrack M, Chrousos G, Gold P (1997) Chronic imipramine is associated with diminished hypothalamic-pituitary-adrenal axis responsivity in healthy humans. J Clin Endocrinol Metab 82:2601–2606
Miller HE, Deakin JF, Anderson IM (2000) Effect of acute tryptophan depletion on CO2-induced anxiety in patients with panic disorder and normal volunteers. Br J Psychiatry 176:182–188
Mitchell P, Smythe G (1990) Hormonal responses to fenfluramine in depressed and control subjects. J Affect Disord 19:43–51
Mokrani MC, Duval F, Crocq MA, Bailey P, Macher JP (1997) HPA axis dysfunction in depression: correlation with monoamine system abnormalities. Psychoneuroendocrinology 22: S63–S68
Montgomery AJ, Bench CJ, Young AH, Hammers A, Gunn RN, Bhagwagar Z, Grasby PM (2001) PET measurement of the influence of corticosteroids on serotonin-1A receptor number. Biol Psychiatry 50:668–676
Mulder RT, Porter RJ, Joyce PR (2003) The prolactin response to fenfluramine in depression—the effects of melancholia and baseline cortisol. J Psychopharmacol 17:97–102
Nemeroff CB (1996) The corticotropin-releasing factor (CRF) hypothesis of depression: new findings and new directions. Mol Psychiatry 1:336–342
Newcomer JW, Selke G, Melson AK, Hershey T, Craft S, Richards K, Alderson AL (1999) Decreased memory performance in healthy humans induced by stress level cortisol treatment. Arch Gen Psychiatry 56:527–533
Newman M, Shapira B, Lerer B (1998) Evaluation of central serotonergic function in affective and related disorders by the fenfluramine challenge test : a critical review. Int J Neuropsychopharmacol 1:49–69
Nuller JL, Ostroumova MN (1980) Resistance to inhibiting effect of dexamethasone in patients with endogenous depression. Acta Psychiatr Scand 61:169–177
Park SB, Williamson DJ, Cowen PJ (1996) 5-HT neuroendocrine function in major depression: prolactin and cortisol responses to d-fenfluramine. Psychol Med 26:1191–1196
Peroutka SJ (1988) 5-Hydroxytryptamine receptor subtypes. Annu Rev Neurosci 11:45–60
Pichot W, Herrera C, Ansseau M (2001) HPA axis dysfunction in major depression: relationship to 5-HT1A receptor activity. Neuropsychobiology 44:74–77
Porter RJ, McAllister-Williams RH, Lunn BS, Young AH (1998) 5-Hydroxytryptamine receptor function in man is reduced by acute administration of hydrocortisone. Psychopharmacology 139:243–250
Porter RJ, McAllister-Williams RH, Jones S, Young AH (1999) Effects of dexamethasone on neuroendocrine and psychological responses to l-tryptophan infusion. Psychopharmacology 143:64–71
Porter RJ, Gallagher P, Watson S, Lunn B, Young AH (2002a) The effects of sub-chronic administration of hydrocortisone on hormonal and psychological responses to l-tryptophan in normal male volunteers. Psychopharmacology 163:68–75
Porter RJ, Marshall EF, O”Brien JT (2002b) Effects of rapid tryptophan depletion on salivary and plasma cortisol in Alzheimer”s disease and the healthy elderly. J Psychopharmacol 16:73–78
Porter RJ, Gallagher P, Watson S, Smith MS, Young AH (2003) Elevated prolactin responses to l-tryptophan infusion in medication-free depressed patients. Psychopharmacology 169: 77–83
Power AC, Cowen PJ (1992) Neuroendocrine challenge tests: assessment of 5-HT function in anxiety and depression. Mol Aspects Med 13:205–20
Price LH, Charney DS, Delgado PL, Heninger GR (1991) Serotonin function and depression: neuroendocrine and mood responses to intravenous l-tryptophan in depressed patients and healthy comparison subjects. Am J Psychiatry 148:1518–1525
Price LH, Cappiello A, Malison RT, McDougle CJ, Pelton GH, Schollnhammer G, Heninger GR (1997a) Effects of antiglucocorticoid treatment on 5-HT1A function in depressed patients and healthy subjects. Neuropsychopharmacology 17:246–257
Price LH, Malison RT, McDougle CJ, McCance-Katz EF, Owen KR, Heninger GR (1997b) Neurobiology of tryptophan depletion in depression: effects of m-chlorophenylpiperazine (mCPP). Neuropsychopharmacology 17:342–350
Price LH, Malison RT, McDougle CJ, Pelton GH, Heninger GR (1998a) The neurobiology of tryptophan depletion in depression: effects of intravenous tryptophan infusion. Biol Psychiatry 43:339–347
Price ML, Curtis AL, Kirby LG, Valentino RJ, Lucki I (1998b) Effects of corticotropin-releasing factor on brain serotonergic activity. Neuropsychopharmacology 18:492–502
Rajewska J, Rybakowski JK (2003) Depression in premenopausal women: gonadal hormones and serotonergic system assessed by d-fenfluramine challenge test. Prog Neuropsychopharmacol Biol Psychiatry 27:705–709
Rang HP, Dale MM (1991) Pharmacology, 2nd edn. Churchill Livingstone, Edinburgh, New York
Reul JM, de Kloet ER, van Sluijs FJ, Rijnberk A, Rothuizen J (1990) Binding characteristics of mineralocorticoid and glucocorticoid receptors in dog brain and pituitary. Endocrinology 127:907–915
Riedel W, Klaassen T, Griez E, Honig A, Menheere P, Van Praag HM (2002a) Dissociable hormonal, cognitive and mood responses to neuroendocrine challenge: evidence for receptor-specific serotonergic dysregulation in depressed mood. Neuropsychopharmacology 26:358–367
Riedel WJ, Sobczak S, Nicolson N, Honig A (2002b) Stress, cortisol and memory as markers of serotonergic vulnerability. Acta Neuropsychiatrica 14:186–191
Rubin R, Poland R, Lesser I, Winston R, Blodgett N (1987) Neuroendocrine aspects of primary endogenous depression, cortisol secretory dynamics in patients and matched controls. Arch Gen Psychiatry 44:328–336
Sachar EJ, Hellman L, Roffwarg HP, Halpern FS, Fukushima DK, Gallagher TF (1973) Disrupted 24-hour patterns of cortisol secretion in psychotic depression. Arch Gen Psychiatry 28:19–24
Sargent PA, Kjaer KH, Bench CJ, Rabiner EA, Messa C, Meyer J, Gunn RN, Grasby PM, Cowen PJ (2000) Brain serotonin1A receptor binding measured by positron emission tomography with [11C]WAY-100635: effects of depression and antidepressant treatment. Arch Gen Psychiatry 57:174–180
Shapira B, Newman ME, Gelfin Y, Lerer B (2000) Blunted temperature and cortisol responses to ipsapirone in major depression: lack of enhancement by electroconvulsive therapy. Psychoneuroendocrinology 25:421–438
Skare SS, Dysken MW, Billington CJ (1994) A review of GHRH stimulation test in psychiatry. Biol Psychiatry 36:249–265
Smith CE, Ware CJ, Cowen PJ (1991) Pindolol decreases prolactin and growth hormone responses to intravenous l-tryptophan. Psychopharmacology 103:140–142
Smith KA, Williams C, Cowen PJ (2000) Impaired regulation of brain serotonin function during dieting in women recovered from depression. Br J Psychiatry 176:72–75
Smythe GA, Mitchell PB (1992) Endocrine and amine responses to d,l-fenfluramine in normal subjects. Am J Psychiatry 149:851–2
Sobczak S, Honig A, Nicholson N, Riedel W (2002) Effects of acute tryptophan depletion on mood and cortisol release in first-degree relatives of type I and type II bipolar patients and healthy matched controls. Neuropsychopharmacology 27:834–842
Sowers JR, Hershman JM, Showsky WR, Carlson HE, Park J (1977) Osmotic control of the release of prolactin and thyrotropin in euthyroid subjects and patients with pituitary tumors. Metabolism 26:187–192
Steckler T, Holsboer F, Reul JMH (1999) Glucocorticoids and depression. Bailliere’s Best Pract Res Clin Endocrinol Metab 13:597–614
Steiger A, Holsboer F (1997) Neuropeptides and human sleep. Sleep 20:1038–1052
Strickland PL, Deakin JF, Percival C, Dixon J, Gater RA, Goldberg DP (2002) Bio-social origins of depression in the community. Interactions between social adversity, cortisol and serotonin neurotransmission. Br J Psychiatry 180:168–173
Thakore JH, Dinan TG (1994) Growth hormone secretion: the role of glucocorticoids. Life Sci 55:1083–1099
Traskman-Bendz L, Haskett RF, Zis AP (1986) Neuroendocrine effects of l-tryptophan and dexamethasone. Psychopharmacology 89:85–88
van Praag HM, Lemus C, Kahn R (1987) Hormonal probes of central serotonergic activity: do they really exist? Biol Psychiatry 22:86–98
Vining RF, McGinley RA, Maksvytis JJ, Ho KY (1983) Salivary cortisol: a better measure of adrenal cortical function than serum cortisol. Ann Clin Biochem 20:329–335
Wajchenberg BL, Liberman B, Neto DG, Morozimato MY, Semer M, Bracco LO, Salgado LR, Knoepfelmacher M, Borges MHS, Pinto ACAR, Kater CE, Lengyel AMJ (1996) Growth hormone axis in Cushing’s syndrome. Horm Res 45:99–107
Watson S, Porter RJ, Young AH (2000) Effect of hydrocortisone on the pituitary response to growth hormone releasing hormone. Psychopharmacology 152:40–46
Hearn AJ, Gallagher P, Owen BM, Smith MS, Watson S, Young AH (2004) Effect of sub-chronic hydrocortisone on responses to amphetamine in normal male volunteers. Psychopharmacology 171:458–464
Wurtman RJ (1982) Nutrients that modify brain function. Sci Am 246:50–59
Young AH, Sharpley AL, Campling GM, Hockney RA, Cowen PJ (1994) Effects of hydrocortisone on brain 5-HT function and sleep. J Affect Disord 32:139–146
Young AH, Rue J, Odontiadis J, Cowen PJ (1998) Lack of effect of hydrocortisone treatment on d-fenfluramine-mediated prolactin release. Psychopharmacology 136:198–200
Young EA, Lopez JF, Murphy-Weinberg V, Watson SJ, Akil H (2003) Mineralocorticoid receptor function in major depression. Arch Gen Psychiatry 60:24–28
Zobel AW, Nickel T, Sonntag A, Uhr M, Holsboer F, Ising M (2001) Cortisol response in the combined dexamethasone/CRH test as predictor of relapse in patients with remitted depression: a prospective study. J Psychiatr Res 35:83–94
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Porter, R.J., Gallagher, P., Watson, S. et al. Corticosteroid-serotonin interactions in depression: a review of the human evidence. Psychopharmacology 173, 1–17 (2004). https://doi.org/10.1007/s00213-004-1774-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-004-1774-1