Abstract
Sepsis is a life-threatening organ dysfunction condition response resulting in acute lung injury. Urotensin II (UII), an endogenous vasoactive peptide, is widely distributed in pulmonary, cardiovascular, central nervous, renal and metabolic systems, and especially in inflammatory regions. This study aimed to investigate whether urotensin II (UII) and UII receptor (UTR) antagonists play a role in the inflammatory response to sepsis-induced lung damage and they are possible therapeutic targets. In the study, 78 male Balb-c mice were used. A cecal ligation and puncture (CLP)-induced polymicrobial sepsis model was applied, and the effects of human urotensin II (agonist) and urantide and palosuran (antagonists) were investigated on lung tissues. Glutathione and malondialdehyde levels and SOD activity of lung tissues were investigated in addition to TNF-α, IL-1β, IL-6, NF-κB, and UTR mRNA levels. Also, lung sections were histopathologically evaluated. Urantide and palosuran, UII receptor antagonists, decreased proinflammatory cytokines such as TNF-α, IL-1β, IL-6, NF-κB, and also decreased oxidative stress parameters in lung tissue, which are markers of damage. UTR mRNA expression was increased in septic lungs, and both antagonists significantly decreased the elevated receptor level. Also, histopathological examination showed beneficial effects of both agonists on lung tissue. The results of this study help to understand the inflammatory and therapeutic contribution of the UII/UTR system on sepsis-induced lung damage. We can suggest that UTR receptor antagonists may be evaluated as a potential drug which reduces sepsis-induced lung damage in the future.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sepsis is a life-threatening organ dysfunction condition caused by the complex inflammatory response of a host to infection (Singer et al. 2016) followed by hemorrhage, trauma, or abdominal surgery that can result in multiple organ dysfunction such as acute respiratory distress syndrome (ARDS), acute lung injury, systemic inflammatory response syndrome (SIRS), and progress to septic shock, even death (Cavaillon and Annane 2006; Ozdulger et al. 2003; Polat et al. 2017). The inflammatory cytokines are among the reasons of sepsis-related injuries such as multiple organ dysfunctions and systemic inflammatory response syndrome (SIRS) (Bhan et al. 2016). In addition, it is shown that oxidative stress may play a significant role in mortality and organ damages caused by sepsis (Cadirci et al. 2011; Petronilho et al. 2016; Prauchner 2017). But it is considered that starting and worsening of both cytokine response and oxidative damage are originated from endothelium damage (Opal and Poll 2015).
Urotensin-II (UII) is one of the main endothelial originated mediator and a somatostatin-like cyclic vasoactive peptide that contains 11 amino acids (Onan et al. 2004; Ross et al. 2010). UII is originally isolated from goby fish (Onan et al. 2004; Ross et al. 2010). It has been shown later that UII is widely distributed in cardiovascular, pulmonary, central nervous, renal and metabolic systems, and especially in inflammatory regions (Cadirci et al. 2016; Ong et al. 2005; Segain et al. 2007; Vaudry et al. 2010). UII exerts its effects through a specific affinity receptor of urotensin (UTR), transduced by orphan-G-coupled receptor 14 (GPR14) (Ames et al. 1999; Davenport and Maguire 2000). Much research has shown that there is an interaction between UII/UTR and inflammatory, immune condition. UII can stimulate expression of specific cytokines such as IL-6, IL-1β, and inflammatory adhesion molecules and tissue factor (TF) by endothelial cells (Johns et al. 2004; Park et al. 2013). The other study has shown that the level of specific cytokines such as IL-1β and IL-6 is increased by stimulation of UII. This effect of UII is inhibited by UTR blocker (You et al. 2012). According to the recent research, the urotensin antagonist urantide might be helpful in preventing from sepsis (Liu et al. 2015a, 2015b). In addition to this finding, in our previous study, we investigated the effect of urotensin agonist (HU-II) and antagonist (palosuran) on sepsis in diabetic mice (Ugan et al. 2018). Diabetes is a chronic metabolic disease that damages endothelial tissue, and some studies have identified a greater infection risk in diabetic patients compared to healthy individuals and found that septic lung injury is more severe in diabetes (Uyanik et al. 2012). It has also been reported that endothelial damage is more severe when diabetes and sepsis occur together (Schuetz et al. 2011). It is known that UII performs various biological actions under both pathophysiological and physiological conditions that are both endothelium-independent vasoconstriction through a direct effect on vascular smooth muscle cells and endothelium-dependent vasorelaxation through the release of nitric oxide (Vaudry et al. 2010). Our previous study showed beneficial effects of urotensin receptor antagonist palosuran in diabetic mice with damaged endothelial tissue; however, that study did not investigate the role of these receptors in sepsis of mice with no underlying endothelial damage. We hypothesized that effects of urotensin receptors can be different in sepsis alone.
In light of these findings, this study aimed to investigate the effects of UII and UTR antagonists (urantide and palosuran) in cecal ligation and puncture (CLP)-induced polymicrobial sepsis model of healthy mice and to observe the effects of UII and UTR antagonists’ administration on sepsis-induced acute lung injury without any accompanying disorder.
Materials and methods
Animals
In the study, 78 male Balb-c mice that were each weighed from 22 to 25 g and 5–7 weeks of age were obtained from Ataturk University’s Experimental Animal Laboratory of Medicinal and Experimental Application and Research Center and were used for all experiments. Animal experiments and procedures were performed by the national guidelines for the use and care of laboratory animals and approved by Ataturk University’s local animal care committee. Mice were housed in standard plastic cages on sawdust bedding in an air-conditioned room at 22 ± 1 °C under lighting controls (14 h light/10 h dark cycle). Standard mice chow and tap water were given ad libitum.
Experimental design
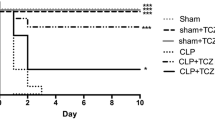
The mice were randomly divided into five groups.
-
Control group: healthy group (6 mice)
-
CLP group: CLP control group (18 mice)
-
CLP + HU-II group: CLP operation + human urotensin II 10 nmol/kg i.p. (per hour) (18 mice)
-
CLP + urantide group: CLP operation + urantide 1.2 mg/kg i.p. (18 mice)
-
CLP + palosuran group: CLP operation + palosuran 100 mg/kg i.p. (18 mice)
Chemicals
Human urotensin receptor agonist (HU-II) and urotensin receptor peptide antagonist (urantide) were obtained from Sigma Chemical Company (Germany). Urotensin receptor non-peptide antagonist (palosuran) was taken from DC Chemicals (Shanghai, China). Metamizole sodium (Novalgin 500 mg/ml injectable preparation) was obtained from Sanofi-Aventis.
CLP induced Polymicrobial Sepsis model
A CLP polymicrobial sepsis model was applied to the mice induced by cecal ligation and a two-hole puncture (Albayrak et al. 2013; Starr et al. 2015; van Griensven et al. 2002). Anesthesia was induced through the intraperitoneal administration of a combination of ketamine at 100 mg/kg and xylazine at 15 mg/kg. The mice’s abdomens were shaved, and the peritoneum was opened making about 1 cm midline abdominal incisions after disinfection of the abdominal wall using povidone iodine. Once the abdominal organs were exposed, the cecum was isolated and ligated with a 3/0 silk ligature distal to the ileocecal valve. Two punctures were made twice (four punctures in total) on the opposite side of the mesentery with a 21-gauge needle through the cecum distal to the point of ligation, and the cecum was returned to the peritoneal cavity. The abdominal incision was then closed with a 4/0 sterile synthetic absorbable suture in two layers. Normal saline (0.5 ml) was subcutaneously given to all animals at the time of surgery as fluid resuscitation. To protect the mice from hypothermia, the mice were placed on heating pads to keep them warm during the surgery and also after the surgery. To prevent postoperative pain, a peritoneal injection of metamizole sodium (150 mg/kg) that has no anti-inflammatory effect was applied at the beginning of the procedure.
The drugs were administered 1 h after sepsis was performed. Administration of HU-II was repeated each hour because of the short half-life of urotensin was a physiologic matter.
At 6 h, 12 h, and 18 h, six randomly selected mice from each group were sacrificed with an overdose of a general anesthetic through the IP administration of a combination of ketamine and xylazine. Whole blood samples were taken via the intracardiac method. The lungs were then quickly removed from all of the mice and washed in ice-cold saline. Half of the lung was applied snap-frozen and then kept at − 80 °C for biochemical and molecular analyses, the other half of the lung was fixed in a 10% formalin solution for histopathological analyses.
Biochemical investigation of lung tissues
After the surgical procedures, the mice tissues were snap frozen and then stored at − 80 °C. All tissue samples from each mouse were initially perfused with PBS/heparin and then grounded in liquid nitrogen using a Tissue Lyser II (Qiagen) grinding jars set. Approximately 20 mg of the tissue was homogenized in 1 ml of PBS homogenate buffer in an Eppendorf tube using the Tissue Lyser II. They were then centrifuged. SOD (Sun et al. 1988), glutathione (GSH) (Sedlak and Lindsay 1968), and malondialdehyde (MDA) (Ohkawa et al. 1979) levels from each sample supernatant and standards were measured at room temperature in duplicate via modified methods with an enzyme-linked immunosorbent assay (ELISA) reader. The average absorbance of each sample and standard were calculated. A standard curve was plotted, and the equation was obtained from the absorbance of the standards. The linear SOD, GSH, and MDA concentrations were calculated according to this equation. The SOD, GSH, and MDA levels in the tissues were expressed as unit per milligram of protein, nanomoles per milligram of protein, and nanomoles per milligram of protein, respectively. All data were presented as the mean ± standard deviation results based on 1 mg of protein.
Total RNA extraction and cDNA synthesis
All tissues from each group were pooled among themselves and were stabilized in RNA Stabilization Reagent (RNAlater, Qiagen) and then disrupted using the Tissue Lyser II (2 × 2 min, Qiagen). Total RNA was purified using RNA easy Mini Kit Qiagen according to the manufacturer’s instructions in Qiaqube (Qiagen). The RNA samples were reverse-transcribed into complementary DNA by High-Capacity cDNA Reverse Transcription Kit (Applied Biosystem). From 10 μl, total RNA was treated with 2 μl 10× RT Buffer, 0.8 μl 25× dNTPs mix, 2 μl 10× RT Random Primers, 1 μl MultiScribe Reverse Transcriptase, and 4.2 μl DEPC-H2O. Reverse transcription was carried out at 25 °C for 10 min, followed by 120 min at 37 °C, and finally 85 °C for 5 min using the Veriti 96 Well Thermal Cycler (Applied Biosystem). The cDNA concentration and quality were assessed and quantified by using the Epoch Spectrophotometer System and Take3 Plate (Biotek).
Relative quantification of gene expression of mice tissues
Relative UTR, TNF-α, IL-1β, IL-6, and NF-κB expression analyses were performed with StepOne Plus Real-Time PCR System technology (Applied Biosystem) using cDNA synthesized from mouse lung RNAs (Table 1). Results are expressed as relative fold compared to control animals. Expression data of β-actin in each tissue were used as endogenous control. For each tissue, triplicate determinations were performed in a 96-well optical plate for both targets using 9 μl of cDNA (100 ng), 1 μl of Primer Perfect Probe mix, and 10 μl of QuantiTect Probe PCR Master mix (Qiagen, Hilden, Germany) in each 20 μl reaction. The plates were heated for 2 min at 50 °C and 10 min at 95 °C, and subsequently, 40 cycles of 15 s at 94 °C and 60 s at 60 °C were applied. All data are expressed as fold-change in expression compared to the expression in other animal groups, using the 2−ΔΔCt method (Livak and Schmittgen 2001).
Histopathological study
At the end of the experiment, the lungs of the mouse were removed, fixed in 10% formalin solution for 48–55 h, dehydrated by an increasing-concentration alcohol series, and cleared by xylene series. After histological processing, the tissues were embedded in paraffin and sectioned to a thickness of 5 mm using a microtome (Leica RM2235, Leica Instruments, Nussloch, Germany) with disposable metal microtome blade (Leica 819, Leica Instruments, Nussloch, Germany). Sections were stained with hematoxylin and eosin (H&E) and observed under a light microscope. In addition, photomicrographs were obtained.
Inflammation scoring
Sections were obtained systematically, sampled randomly, and then scored independently in a double-blinded way by two pathologists depending on the degree of inflammation in the perivascular area as follows:
-
0: No inflammatory cells (ICs)
-
1: A few ICs
-
2: Many ICs in the peripheral parts of the perivascular area
-
3: Numerous ICs in the perivascular area
Statistical analyses
We used the SPSS 20.0 software for statistical analysis. Results were presented as means ± standard deviation (SD). Comparisons between the groups were performed using a one-way ANOVA, the Tukey’s test. Significance was accepted at p < 0.05.
Results
Biochemical parameters
GSH and MDA levels and SOD activity of lung tissues
The SOD activity (Fig. 1) and GSH levels (Fig. 2) decreased, whereas the levels of MDA (Fig. 3) significantly increased in the lung of the sepsis group when compared to the control group at 6 h, 12 h, and 18 h. In the sepsis + palosuran and sepsis + urantide groups, the SOD activity and GSH level increased, and the MDA level decreased when compared to the sepsis group at 6 h, 12 h, and 18 h. There was no significance for the MDA, GSH level, and the SOD activity in the sepsis + HU-II group for the SOD and GSH. There was a significant increase in the sepsis + HU-II group 18 h for the MDA.
SOD activity in groups underwent CLP induced septic lung injury at 6 h, 12 h, and 18 h. Statistical comparisons were made using one-way ANOVA followed by Tukey’s test. The healthy control group was compared with the other groups; *p < 0.05, **p < 0.01, and ***p < 0.001 marks were used. The sepsis group was compared with the other groups; #p < 0.05, ##p < 0.01, and ###p < 0.001 marks were used. Values represented as mean ± S.D.
GSH level in groups underwent CLP induced septic lung injury at 6 h, 12 h, and 18 h. Statistical comparisons were made using one-way ANOVA followed by Tukey’s test. The healthy control group was compared with the other groups; *p < 0.05, **p < 0.01, and ***p < 0.001 marks were used. The sepsis group was compared with the other groups; #p < 0.05, ##p < 0.01, and ###p < 0.001 marks were used. Values represented as mean ± S.D.
MDA level in groups underwent CLP induced septic lung injury at 6 h, 12 h, and 18 h. Statistical comparisons were made using one-way ANOVA followed by Tukey’s test. The healthy control group was compared with the other groups; *p < 0.05, **p < 0.01, and ***p < 0.001 marks were used. The sepsis group was compared with the other groups; #p < 0.05, ##p < 0.01, and ###p < 0.001 marks were used. Values represented as mean ± S.D.
Molecular parameters
TNF-α, IL-1β, IL-6 NF-κB, and UTR mRNA levels in lung tissues
TNF-α mRNA expression (Fig. 4) increased in the sepsis group (respectively 6.83, 8.67, 21.08-fold) compared with the control group (p < 0.001) at 6 h, 12 h, and 18 h. The decreased TNF-α levels in the sepsis + urantide (respectively 4.34, 3.86, 2.86-fold) (p < 0.001) and the sepsis + palosuran (respectively 5.45-fold (p < 0.01), 3.95, 8.49-fold (p < 0.001)) groups were significant when compared to the sepsis group at 6 h, 12 h, and 18 h. There was not a significant difference in the sepsis + HU-II groups at 6 h and 12 h when compared to the sepsis group (respectively 6.35, 8.65). There was a significant increase in the sepsis + HU-II groups at 18 h when compared to the sepsis group (23.52) (p < 0.05).
TNF-α mRNA expressions in CLP-induced lung injury at 6 h, 12 h, and 18 h. Gene expression was detected by quantitative real-time PCR analysis. Results were normalized to beta-actin (housekeeping gene control). The relative expression levels were indicated as “fold change” compared with the healthy control group. Statistical comparisons were made using one-way ANOVA followed by Tukey’s test. The healthy control group was compared with the other groups; *p < 0.05, **p < 0.01, and ***p < 0.001 marks were used. The sepsis group was compared with the other groups; #p < 0.05, ##p < 0.01, and ###p < 0.001 marks were used. Values represented as mean ± S.D.
IL-6 mRNA level (Fig. 5) significantly increased in the sepsis group (respectively 265.5, 164.9, 162.6-fold) compared to the control group (p < 0.001) at 6 h, 12 h, and 18 h. Compared to the sepsis group, there was a significant decrease in the sepsis + urantide group (respectively 100.5, 84.9, 88.2-fold) (p < 0.001) at 6 h, 12 h, and 18 h. In addition to the sepsis + urantide group, there was a significant decrease in sepsis + palosuran which was another treatment group at 6 h, 12 h and 18 h (respectively 159.8, 74.9, 69.9-fold) (p < 0.001) when compared to the control group. There was no meaningful difference between the sepsis + HU-II group and the sepsis group at 6 h and 12 h (respectively 247.5, 173.1-fold) and increase in the sepsis + HU-II groups at 18 h when compared to the sepsis group (183.4-fold) (p < 0.05).
IL-6 mRNA expressions in CLP-induced lung injury at 6 h, 12 h, and 18 h. Gene expression was detected by quantitative real-time PCR analysis. Results were normalized to beta-actin (housekeeping gene control). The relative expression levels were indicated as “fold change” compared with the healthy control group. Statistical comparisons were made using one-way ANOVA followed by Tukey’s test. The healthy control group was compared with the other groups; *p < 0.05, **p < 0.01, and *** p < 0.001 marks were used. The sepsis group was compared with the other groups; #p < 0.05, ##p < 0.01, and ###p < 0.001 marks were used. Values represented as mean ± S.D.
IL-1β gene expression (Fig. 6) increased in the sepsis group (respectively 44.1, 38.8, 36.6-fold) (p < 0.001) compared to the control group at 6 h, 12 h, and 18 h. Compared to the sepsis group, there was a significant decrease in the sepsis + urantide group (respectively 25.6-fold (p < 0.01), 16.1, 9.2-fold (p < 0.001)) at 6 h, 12 h, and 18 h. In addition to the sepsis + urantide group, there was a significant decrease in the sepsis + palosuran which was another treatment group at 6 h, 12 h, and 18 h (respectively 29.6-fold (p < 0.05), 27.6, 8.8-fold (p < 0.001)) when compared to the control group. There was no meaningful difference between the sepsis + HU-II group and the sepsis group at 6 h and 12 h (respectively 33.9, 34.6-fold) and a significant increase in the sepsis + HU-II groups at 18 h when compared to the sepsis group (41.5-fold) (p < 0.05).
IL-1β mRNA expressions in CLP-induced lung injury at 6 h, 12 h, and 18 h. Gene expression was detected by quantitative real-time PCR analysis. Results were normalized to beta-actin (housekeeping gene control). The relative expression levels were indicated as “fold change” compared with the healthy control group. Statistical comparisons were made using one-way ANOVA followed by Tukey’s test. The healthy control group was compared with the other groups; *p < 0.05, **p < 0.01, and ***p < 0.001 marks were used. The sepsis group was compared with the other groups; #p < 0.05, ##p < 0.01, and ###p < 0.001 marks were used. Values represented as mean ± S.D.
In NF-κB expression (Fig. 7), when compared to the control group (respectively 2.53, 2.62, 1.82-fold), there was a significant increase in the sepsis group (p < 0,001) at 6 h, 12 h, and 18 h. Compared to the sepsis group, there was a significant decrease in the sepsis + urantide group (respectively 1.53, 1.7, 0.8-fold (p < 0.001) at 6 h, 12 h, and 18 h). In addition to the sepsis + urantide group, there was a significant decrease in the sepsis + palosuran which was another treatment group at 6 h, 12 h, and 18 h (respectively 1.9, 1.7, 1.5-fold) (p < 0.001) when compared to the control group. There was no meaningful difference between the sepsis + HU-II group and the sepsis group at 6 h and 12 h (respectively 2.3, 2.5-fold) and a significant increase in the sepsis + HU-II groups at 18 h when compared to the sepsis group (2.0-fold) (p < 0.05).
NF-κB mRNA expressions in CLP-induced lung injury at 6 h, 12 h, and 18 h. Gene expression was detected by quantitative real-time PCR analysis. Results were normalized to beta-actin (housekeeping gene control). The relative expression levels were indicated as “fold change” compared with the healthy control group. Statistical comparisons were made using one-way ANOVA followed by Tukey’s test. The healthy control group was compared with the other groups; *p < 0.05, **p < 0.01, and *** p < 0.001 marks were used. The sepsis group was compared with the other groups; #p < 0.05, ##p < 0.01, and ###p < 0.001 marks were used. Values represented as mean ± S.D.
UTR gene expression (Fig. 8) increased in the sepsis group (respectively 2.2, 3.3, 3.2-fold) (p < 0.001) compared to the control group at 6 h, 12 h, and 18 h. Compared to the sepsis group, there was a significant decrease in the sepsis + urantide group (respectively 0.7, 1.13, 0.5-fold (p < 0.001) at 6 h, 12 h, and 18 h. In addition to the sepsis + urantide group, there was a significant decrease in sepsis + palosuran which was another treatment group at 6 h, 12 h and 18 h (respectively 1.7-fold (p < 0.05), 1.4, 1.5-fold (p < 0.001)) when compared to the control group. There was no meaningful difference between the sepsis + HU-II group and the sepsis group at 6 h and 12 h (respectively 2.5, 3.3-fold). There was a significant increase in the sepsis + HU-II groups at 18 h when compared to the sepsis group (3.5-fold) (p < 0.01).
UTR mRNA expressions in CLP-induced lung injury at 6 h, 12 h, and 18 h. Gene expression was detected by quantitative real-time PCR analysis. Results were normalized to beta-actin (housekeeping gene control). The relative expression levels were indicated as ‘fold change’ compared with the healthy control group. Statistical comparisons were made using one-way ANOVA followed by Tukey’s test. The healthy control group was compared with the other groups; *p < 0.05, **p < 0.01, and ***p < 0.001 marks were used. The sepsis group was compared with the other groups, #p < 0.05, ##p < 0.01, and ###p < 0.001 marks were used. Values represented as mean ± S.D.
Histopathological results
Inflammation scoring
Inflammation scoring on histopathological examination was designed according to the grading system in Table 2. When compared to the sepsis group, it was seen at all hours in the sepsis + urantide and sepsis + palosuran groups that polymorphonuclear leukocytes (PMNL), vascular congestion (VK), and edema scoring were lower than the sepsis groups.
Conventional light microscopic examination
Figure 9 shows the lung histology obtained using the HE staining under light microscopy with an original magnification of × 40. In the control groups, a section of all structures of the lung had normal appearances at 6 h, 12 h, and 18 h (Fig. 9(A), 6 h, 12 h, 18 h). In sepsis groups (Fig. 9(B), 6 h, 12 h, 18 h), which is induced with CLP, dense inflammatory cell infiltrations with diffuse and nodular form were remarkable findings at first glance at 6 h, 12 h, and 18 h. The inflammation consisted of several PMNL in sepsis groups, especially at 12 h and 18 h. When histopathological changes were evaluated in both the sepsis + urantide (Fig. 9(D), 6 h, 12 h, 18 h) and the sepsis + palosuran groups (Fig. 9(E), 6 h, 12 h,18 h), the inflammatory cell infiltrations were seen decreased when compared to the sepsis group at 6 h, 12 h, and 18 h. There was no significant decrease in PMNL and VK degree of the sepsis + HU-II groups (Fig. 9(C), 6 h,12 h,18 h), according to the sepsis groups.
Discussion
Recent research has suggested that the UII/UTR signaling pathway is related to proinflammatory responses via mediating proinflammatory cytokine expression (Liang et al. 2013; Liu et al. 2015b; Yang et al. 2016). UII plasma level is associated with the pathogenesis of vascular endothelial dysfunction and tissue injury (Watanabe et al. 2009). In addition, in our previous study, we investigated the effects of urotensin agonist and antagonist on septic rats with underlying diabetes and endothelium damage. We observed that the cytokine levels were increased by diabetes and sepsis and were completely decreased by urotensin receptor antagonist: palosuran. HU-II exerted partial beneficial responses at a low dose and completed harmful responses at high doses (Ugan et al. 2018). This result might derive from the endothelium-dependent biphasic effect of urotensin under diabetic mice with damaged endothelial tissue. So, in this study, we have applied a high dose HU-II and two different UII antagonists (palosuran and urantide) and found a time-dependent relationship between UII/UT and cytokine levels on the lung injury which was induced by polymicrobial sepsis (cecal ligation and puncture—CLP) in healthy mice with no underlying endothelial damage.
CLP-induced sepsis model, a commonly used animal model (Albayrak et al. 2013; Starr et al. 2015; van Griensven et al. 2002), and this model mimic the clinical situation of bowel perforation and bacterial infection (Dejager et al. 2011) that causes acute lung injury in patients (Cadirci et al. 2013; Mukherjee and Hanidziar 2018). In our study, uncontrolled propagation of proinflammatory cytokines such as TNF-α and IL-6 has been activated in the lungs of mice during CLP-induced sepsis in line with previous studies (Akpinar et al. 2014; Cadirci et al. 2010). The NF-κB signaling pathway plays a significant role in activating and regulating the expression and the transcription of proinflammatory cytokines in the immune response and inflammation reaction (DiDonato et al. 2012; 2012; Hoesel and Schmid 2013). As shown in the previous research, UII contributes to the activation of proinflammatory cytokines by acting as cytokines in many diseases (Ong et al. 2008). The studies also found that the expression of the proinflammatory cytokines such as TNF-α, IL-1β, IL-6, and NF-κB was increased by the administration of UII agonist (Johns et al. 2004), while the administration of UII antagonist decreased the cytokines (Liang et al. 2013; Liu et al. 2015b). Another research (Liang et al. 2013) indicated that the inhibition of UII/UTR system by the administration of urantide relieved the acute inflammation of liver through preventing the activation of TNF-α, IL-1β proinflammatory cytokines, and NF-κB pathway. In this study, we researched the effect of UII/UTR systems on the NF-κB pathway and demonstrated that urantide and palosuran significantly inhibited the NF-κB expression. This result suggested that the inflammatory activation in the CLP-induced lung damage depends on the NF-κB activation, and it also indicated that the UII/UTR system is associated with the NF-κB pathway. The findings of the current study are consistent with the previous study showing that the agonist application stimulating the UTR did not increase the inflammation (Cadirci et al. 2016). Our results suggest that the urotensin system plays a strong role in the disease states compared to the healthy state, and also this system operates the inflammatory response.
In addition to this cytokine storm, reactive oxygen species (ROS) also increased during the inflammation. Physiologically, there is a balance between ROS and antioxidant defense mechanism in the body. However, this balance is impaired by ROS in the presence of some diseases. Consequently, an imbalance occurs between oxidant and antioxidant and the resulting free radicals begin to damage (Naito et al. 1998). In the present study, we found that MDA levels, which are end products of lipid peroxidation, increased with sepsis, but they were not changed by the administration of HU-II according to sepsis group at 6 h, 12 h, and increased at the 18 h. We observed that increased MDA levels were reduced at all times (6, 12, 18 h) by the application of urotensin antagonists. In addition, the SOD activity and the GSH level increased with sepsis; the HU-II administration did not change these parameters when compared to sepsis group. Application of urotensin antagonists also decreased these parameters when compared to sepsis. Previous studies found the similar results supporting our present study; the activity of the SOD and GSH levels decreased while the MDA levels increased in the CLP-induced sepsis group (Akpinar et al. 2014; Coskun et al. 2011). Various studies showed that the SOD activity and GSH levels decreased during sepsis (Cadirci et al. 2011; Polat et al. 2013). Association of the UII/UTR system with oxidative stress has been previously investigated. In our previous research, the SOD activity, and GSH levels decreased, and the MDA levels increased in the UII agonist given group compared to the carrageenan edema group. However, urantide given group when compared to the carrageenan edema group, the SOD activity and GSH levels increased, and the MDA levels decreased (Cadirci et al. 2016). Another research also showed that the SOD activity and GSH levels increased, and the MDA levels decreased in the palosuran administered group compared to the sepsis group (Ugan et al. 2018).
When we evaluated our results in a time-dependent manner, we observed that cytokine levels decreased at 6 h, 12 h, and 18 h in both of the antagonist groups, but we found that urantide is more effective than palosuran at the 6th hour. We also observed that HU-II did not alter proinflammatory levels increased by sepsis at 6 h and 12 h but increased the proinflammatory levels further to at 18 h. Based on these results, we thought that HU-II not only contributes the inflammation and tries to maintain balance at the beginning but also mediates to increase the damage in the later stage. The peptide structure of urantide is seen to be more effective in regulating the inflammation and oxidation which develops due to sepsis to compare the non-peptide structure of palosuran at the 6 h. We can conclude that the palosuran is more effective at the 12 h and 18 h than the 6 h because the half-life is moderately longer (20 h) (Sidharta et al. 2009). As for that peptide structure of urantide, it may have allowed it to reach faster where it affects and to act more efficiently.
In this study, we observed that the UTR expression increased in the sepsis group, but it did not change at 6 h and 12 h and increased at 18 h in the HU-II group. When we applied urotensin antagonists, we found that the UTR expression decreased at all-time intervals, as well as urantide was more effective at 6 h. The results of our UTR expression are similar to those of cytokine and oxidative stress parameters results, and we can suggest that these receptors play roles in the pathophysiology of sepsis, and the urotensin receptors may play an active role in the development or treatment of the sepsis-related damage. Because of the increased amount of urotensin due to lung damage at 6 h and 12 h with sepsis, when given HU-II, the UTR expression may not have shown an increasing effect. But it contributed to the increase of the UTR expression associated with enhancing of damage at 18 h. We can conclude that HU-II contributing endothelial damage in lungs occurs in time-dependent manned during sepsis and both of the antagonists can reverse in this damage.
Liu et al. (2015a) also found that the time-dependent expression of UII challenged by LPS increased significantly and reached a peak from 0.5 to 2 h and remained high till 6 h. At the end of 6 h, the UII levels began to degrade but remained high. They found that the time-dependent expression of TNF-α by challenged LPS increased significantly and peaked at 1 h and 2 h. In our study, UII induced the increase in the expression of proinflammatory cytokines at all-time intervals. Liu et al. (2015a) also found that the time-dependent expression of IL-1β level peaked at the end of the 6 h, but there was not any increase until 6 h. TNF-α plays a private role in the inflammation to induce the release of IL-6 (Cunha et al. 2005). There is a strong interaction between the IL-6 and inflammation (Xing et al. 1994). In the present study, the increase of the TNF-α level and upregulation of UII-induced secretion of IL-6 is similar to the results of the previous study (Johns et al. 2004). This time-dependent modification according to our results and also as it is known before, UII-induced tight junction between endothelial cell function and inflammation (Imhof and Aurrand-Lions 2006) showed a relation between UII and other proinflammatory cytokines.
According to our histopathological results, in our sepsis group, which was induced with CLP, high vascular congestion, edema, and polymorphonuclear leukocytes were remarkable findings. Urantide and palosuran treatment ameliorate the inflammatory cells that accumulate in the lung and result in lung injury in septic mice while administration of HU-II increases histopathological changes like vascular congestion, edema, and polymorphonuclear leukocytes depending on time. In addition, previous research demonstrated urotensin II increases macrophage cell functions and mediates inflammatory responses in different conditions such as atherosclerosis (Wang et al. 2014; Zhao et al. 2015). Both histopathological findings and cytokine mRNA expression results support each other and also show the protective effect of urantide and palosuran on the lungs during sepsis.
As a conclusion, this study demonstrated the roles of the UII/UTR system in sepsis-induced lung damage. UII can trigger releasing proinflammatory cytokines in CLP-induced septic mice. Urantide and palosuran, UII receptor antagonists, showed beneficial effects on lung tissues by preventing releases of proinflammatory cytokines such as TNF-α, IL-1β, IL-6, NF-κB, and also decreasing oxidative stress, which are markers of damage. UII and UTR may provide the experimental foundation, and these antagonists may be evaluated as a potential drug that reduces sepsis in the future.
References
Akpinar E, Halici Z, Cadirci E, Bayir Y, Karakus E, Calik M, Topcu A, Polat B (2014) What is the role of renin inhibition during rat septic conditions: preventive effect of aliskiren on sepsis-induced lung injury. Naunyn Schmiedeberg’s Arch Pharmacol 387:969–978. https://doi.org/10.1007/s00210-014-1014-0
Albayrak A, Halici Z, Polat B, Karakus E, Cadirci E, Bayir Y, Kunak S, Karcioglu SS, Yigit S, Unal D, Atamanalp SS (2013) Protective effects of lithium: a new look at an old drug with potential antioxidative and anti-inflammatory effects in an animal model of sepsis. Int Immunopharmacol 16:35–40
Ames RS, Sarau HM, Chambers JK, Willette RN, Aiyar NV, Romanic AM, Louden CS, Foley JJ, Sauermelch CF, Coatney RW, Ao Z, Disa J, Holmes SD, Stadel JM, Martin JD, Liu WS, Glover GI, Wilson S, McNulty DE, Ellis CE, Elshourbagy NA, Shabon U, Trill JJ, Hay DWP, Ohlstein EH, Bergsma DJ, Douglas SA (1999) Human urotensin-II is a potent vasoconstrictor and agonist for the orphan receptor .GPR14. Nature 401:282–286
Bhan C, Dipankar P, Chakraborty P, Sarangi PP (2016) Role of cellular events in the pathophysiology of sepsis. Inflamm Res 65:853–868
Cadirci E, Altunkaynak BZ, Halici Z, Odabasoglu F, Uyanik MH, Gundogdu C, Suleyman H, Halici M, Albayrak M, Unal B (2010) Alpha-lipoic acid as a potential target for the treatment of lung injury caused by cecal ligation and puncture-induced sepsis model in rats. Shock 33:479–484. https://doi.org/10.1097/SHK.0b013e3181c3cf0e
Cadirci E, Halici Z, Odabasoglu F, Albayrak A, Karakus E, Unal D, Atalay F, Ferah I, Unal B (2011) Sildenafil treatment attenuates lung and kidney injury due to overproduction of oxidant activity in a rat model of sepsis: a biochemical and histopathological study. Clin Exp Immunol 166:374–384
Cadirci E, Halici Z, Bayir Y, Albayrak A, Karakus E, Polat B, Unal D, Atamanalp SS, Aksak S, Gundogdu C (2013) Peripheral 5-HT7 receptors as a new target for prevention of lung injury and mortality in septic rats. Immunobiology 218:1271–1283. https://doi.org/10.1016/j.imbio.2013.04.012
Cadirci E, Halici Z, Yayla M, Toktay E, Bayir Y, Karakus E, Topcu A, Buyuk B, Albayrak A (2016) Blocking of urotensin receptors as new target for treatment of carrageenan induced inflammation in rats. Peptides 82:35–43
Cavaillon J-M, Annane D (2006) Invited review: compartmentalization of the inflammatory response in sepsis and SIRS. J Endotoxin Res 12:151–170
Coskun AK, Yigiter M, Oral A, Odabasoglu F, Halici Z, Mentes O, Cadirci E, Atalay F, Suleyman H (2011) The effects of Montelukast on antioxidant enzymes and proinflammatory cytokines on the heart, liver, lungs, and kidneys in a rat model of cecal ligation and puncture-induced sepsis. Sci World J 11:1341–1356
Cunha TM, Verri W, Silva J, Poole S, Cunha F, Ferreira S (2005) A cascade of cytokines mediates mechanical inflammatory hypernociception in mice. Proc Natl Acad Sci U S A 102:1755–1760
Davenport AP, Maguire JJ (2000) Urotensin II: fish neuropeptide catches orphan receptor. Trends Pharmacol Sci 21:80–82
Dejager L, Pinheiro I, Dejonckheere E, Libert C (2011) Cecal ligation and puncture: the gold standard model for polymicrobial sepsis? Trends Microbiol 19:198–208
DiDonato JA, Mercurio F, Karin M (2012) NF-κB and the link between inflammation and cancer. Immunol Rev 246:379–400
van Griensven M, Kuzu M, Breddin M, Böttcher F, Krettek C, Pape H-C, Tschernig T (2002) Polymicrobial sepsis induces organ changes due to granulocyte adhesion in a murine two hit model of trauma. Exp Toxicol Pathol 54:203–209
Hoesel B, Schmid JA (2013) The complexity of NF-κB signaling in inflammation and cancer. Mol Cancer 12:86
Imhof BA, Aurrand-Lions M (2006) Angiogenesis and inflammation face off. Nat Med 12:171–172
Johns DG, Ao Z, Naselsky D, Herold CL, Maniscalco K, Sarov-Blat L, Steplewski K, Aiyar N, Douglas SA (2004) Urotensin-II-mediated cardiomyocyte hypertrophy: effect of receptor antagonism and role of inflammatory mediators. Naunyn Schmiedeberg’s Arch Pharmacol 370:238–250
Liang D-y et al (2013) Inhibition of UII/UTR system relieves acute inflammation of liver through preventing activation of NF-κB pathway in ALF mice. PLoS One 8:e64895
Liu L-M, Zhao L, Liang D-Y, Yu F-P, Ye C-G, Tu W-J, Zhu T (2015a) Effects of urotensin-II on cytokines in early acute liver failure in mice. World J Gastroenterol: WJG 21:3239–3244
Liu LM, Liang DY, Ye CG, Tu WJ, Zhu T (2015b) The UII/UT system mediates upregulation of proinflammatory cytokines through p38 MAPK and NF-κB pathways in LPS-stimulated Kupffer cells. PLoS One 10:e0121383
Livak KJ, Schmittgen TD (2001) Analysis of relative gene expression data using real-time quantitative PCR and the 2(T)(−Delta Delta C) method. Methods 25:402–408. https://doi.org/10.1006/Meth.2001.1262
Mukherjee S, Hanidziar D (2018) More of the gut in the lung: how two microbiomes meet in ARDS. Yale J Biol Med 91:143–149
Naito Y, Yoshikawa T, Yoshida N, Kondo M (1998) Role of oxygen radical and lipid peroxidation in indomethacin-induced gastric mucosal injury. Dig Dis Sci 43:30S–34S
Ohkawa H, Ohishi N, Yagi K (1979) Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal Biochem 95:351–358
Onan D, Hannan RD, Thomas WG (2004) Urotensin II: the old kid in town. Trends Endocrinol Metab 15:175–182
Ong KL, Lam KS, Cheung BM (2005) Urotensin II: its function in health and its role in disease. Cardiovasc Drugs Ther 19:65–75
Ong KL, Wong LY, Cheung BM (2008) The role of urotensin II in the metabolic syndrome. Peptides 29:859–867
Opal S, Poll T (2015) Endothelial barrier dysfunction in septic shock. J Intern Med 277:277–293
Ozdulger A, Cinel I, Koksel O, Cinel L, Avlan D, Unlu A, Okcu H, Dikmengil M, Oral U (2003) The protective effect of N-acetylcysteine on apoptotic lung injury in cecal ligation and puncture-induced sepsis model. Shock 19:366–372
Park SL, Lee BK, Kim Y-A, Lee BH, Jung Y-S (2013) Inhibitory effect of an urotensin II receptor antagonist on proinflammatory activation induced by urotensin II in human vascular endothelial cells. Biomol Ther 21:277–283
Petronilho F, Florentino D, Danielski LG, Vieira LC, Martins MM, Vieira A, Bonfante S, Goldim MP, Vuolo F (2016) Alpha-lipoic acid attenuates oxidative damage in organs after sepsis. Inflammation 39:357–365
Polat B, Cadirci E, Halici Z, Bayir Y, Unal D, Bilgin BC, Yuksel TN, Vancelik S (2013) The protective effect of amiodarone in lung tissue of cecal ligation and puncture-induced septic rats: a perspective from inflammatory cytokine release and oxidative stress. Naunyn Schmiedeberg's Arch Pharmacol 386:635–643
Polat G, Ugan RA, Cadirci E, Halici Z (2017) Sepsis and septic shock: current treatment strategies and new approaches. Eurasian J Med 49:53–58
Prauchner CA (2017) Oxidative stress in sepsis: pathophysiological implications justifying antioxidant co-therapy. Burns 43:471–485
Ross B, McKendy K, Giaid A (2010) Role of urotensin II in health and disease. Am J Phys Regul Integr Comp Phys 298:R1156–R1172
Schuetz P, Yano K, Sorasaki M, Ngo L, St Hilaire M, Lucas JM, Aird W, Shapiro NI (2011) Influence of diabetes on endothelial cell response during sepsis. Diabetologia 54:996–1003. https://doi.org/10.1007/s00125-011-2059-y
Sedlak J, Lindsay RH (1968) Estimation of total, protein-bound, and nonprotein sulfhydryl groups in tissue with Ellman’s reagent. Anal Biochem 25:192–205
Segain J-P, Rolli-Derkinderen M, Gervois N, de la Blétière DR, Loirand G, Pacaud P (2007) Urotensin II is a new chemotactic factor for UT receptor-expressing monocytes. J Immunol 179:901–909
Sidharta PN, Giersbergen PL, Dingemanse J (2009) Pharmacokinetics and pharmacodynamics of the urotensin-II receptor antagonist palosuran in healthy male subjects. J Clin Pharmacol 49:1168–1175
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, Bellomo R, Bernard GR, Chiche JD, Coopersmith CM, Hotchkiss RS, Levy MM, Marshall JC, Martin GS, Opal SM, Rubenfeld GD, van der Poll T, Vincent JL, Angus DC (2016) The third international consensus definitions for sepsis and septic shock (sepsis-3). Jama 315:801–810
Starr ME, Takahashi H, Okamura D, Zwischenberger BA, Mrazek AA, Ueda J, Stromberg AJ, Evers BM, Esmon CT, Saito H (2015) Increased coagulation and suppressed generation of activated protein C in aged mice during intra-abdominal sepsis. Am J Phys Heart Circ Phys 308:H83–H91
Sun Y, Oberley LW, Li Y (1988) A simple method for clinical assay of superoxide dismutase. Clin Chem 34:497–500
Ugan RA, Cadirci E, Halici Z, Toktay E, Cinar I (2018) The role of urotensin-II and its receptors in sepsis-induced lung injury under diabetic conditions. Eur J Pharmacol 818:457–469
Uyanik MH et al (2012) Effects of diabetes on cytokines and oxidative organ injury in a rat model of sepsis. Cell Mol Biol (Noisy-le-grand) 58(Suppl):OL1623–OL1631
Vaudry H, Do Rego JC, le Mevel JC, Chatenet D, Tostivint H, Fournier A, Tonon MC, Pelletier G, Michael Conlon J, Leprince J (2010) Urotensin II, from fish to human. Ann N Y Acad Sci 1200:53–66
Wang Y, Wu JF, Tang YY, Zhang M, Li Y, Chen K, Zeng MY, Yao F, Xie W, Zheng XL, Zeng GF, Tang CK (2014) Urotensin II increases foam cell formation by repressing ABCA1 expression through the ERK/NF-kappaB pathway in THP-1 macrophages. Biochem Biophys Res Commun 452:998–1003. https://doi.org/10.1016/j.bbrc.2014.09.030
Watanabe T, Arita S, Shiraishi Y, Suguro T, Sakai T, Hongo S, Miyazaki A (2009) Human urotensin II promotes hypertension and atherosclerotic cardiovascular diseases. Curr Med Chem 16:550–563
Xing Z, Braciak T, Jordana M, Croitoru K, Graham FL, Gauldie J (1994) Adenovirus-mediated cytokine gene transfer at tissue sites. Overexpression of IL-6 induces lymphocytic hyperplasia in the lung. J Immunol 153:4059–4069
Yang Y, Zhang J, Chen X, Wu T, Xu X, Cao G, Li H, Li Y (2016) UII/GPR14 is involved in NF-κB-mediated colonic inflammation in vivo and in vitro. Oncol Rep 36:2800–2806
You Z, Genest J, Barrette P-O, Hafiane A, Behm DJ, D’Orleans-Juste P, Schwertani AG (2012) Genetic and pharmacological manipulation of urotensin II ameliorate the metabolic and atherosclerosis sequalae in mice. Arterioscler Thromb Vasc Biol 32:1809–1816
Zhao S, Li Y, Gao S, Wang X, Sun L, Cheng D, Bai L, Guan H, Wang R, Fan J, Liu E (2015) Autocrine human urotensin II enhances macrophage-derived foam cell formation in transgenic. Rabbits Biomed Res Int 2015:843959–843958. https://doi.org/10.1155/2015/843959
Funding
This study was supported by Turkish Academy of Sciences (TUBA)—The Young Scientist Award Program (GEBIP) with project number “EC/TUBAGEBIP-20135.”
Author information
Authors and Affiliations
Contributions
EC, ZH, and EA conceived and designed research and conducted the experiment. EC, BD, and AG wrote the manuscript. BG performed the histopathological analyses. IC and EC analyzed the data. All authors read and approved the manuscript.
Corresponding author
Ethics declarations
Animal experiments and procedures were performed by the national guidelines for the use and care of laboratory animals and approved by Ataturk University’s local animal care committee.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Cadirci, E., Ugan, R.A., Dincer, B. et al. Urotensin receptors as a new target for CLP induced septic lung injury in mice. Naunyn-Schmiedeberg's Arch Pharmacol 392, 135–145 (2019). https://doi.org/10.1007/s00210-018-1571-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-018-1571-8