Abstract
In vitro and in vivo studies indicate that scutellarin (SCU) exerts anti-inflammatory effects in the central nervous system (CNS) and inhibits microglia activation. This study investigated the anti-neuroinflammation molecular mechanisms exerted by scutellarin in LPS-induced BV-2 cells. The results showed that production of TNF-α, IL-1β, IL-6, and NO and TNF-α, IL-1β, IL-6, and iNOS mRNA were inhibited by scutellarin, which was independent of cytotoxicity as assessed by a CCK8 assay. Western blot analysis indicated that NF-κB-p65 phosphorylation was suppressed by scutellarin via inhibition of IκB degradation and IKKβ activation, which coincided with blockage of nuclear translocation of NF-κB as shown by immunofluorescent staining. Consistent with the inhibition of NF-κB, scutellarin inhibited the phosphorylation of p38, JNK, and AKT without affecting phosphorylation of ERK1/2 or PI3K in LPS-induced BV-2 cells. Overall, the present study suggests that scutellarin inhibits the production of pro-inflammatory mediators via inhibition of the IKK-dependent NF-κB and p38/JNK signaling pathway, which inhibits microglia activation and exerts anti-inflammation, indicating its potential therapeutic effect for neurodegenerative and cerebrovascular diseases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neuroinflammation plays a crucial role in the pathogenesis of ischemic stroke, which is associated with an increased rate of morbidity and mortality worldwide (Tuttolomondo et al. 2008; Wu et al. 2016). In the CNS, neuroinflammation is regulated by microglia, resident innate immune cells which play a dual role, both neuroprotective and neurotoxic, in mediating inflammatory responses in the developing brain (Block and Hong 2005; Glass et al. 2010). After cerebral ischemic injury or other destructive stimulations, microglia are activated and release pro-inflammatory mediators including TNF-α, IL-1β, and NO. These pro-inflammatory mediators also further stimulate the activation of microglia and contribute to the accumulation of pro-inflammatory mediators, which ultimately results in neuronal death and exacerbates cerebral damage (Bhalala et al. 2015; Liu and McCullough 2013; Shukla et al. 2017; Vidale et al. 2017). NF-κB, a crucial transcription factor in the inflammatory response, is located in the cytoplasm bound to its inhibitor protein IκB in resting conditions (Shih et al. 2011). Once microglia are activated, NF-κB is phosphorylated, translocates to the nucleus, and binds to inflammation-related genes, resulting in the production of pro-inflammatory mediators (Bosman et al. 2016; Luo et al. 2017).
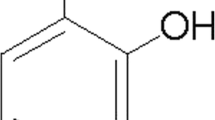
Scutellarin, a flavone glucuronide, is extracted as a monomeric compound from the traditional Chinese medicine plant Erigeron breviscapus (vant.) Hand. Mazz., which has been made into numerous preparations and is widely used for the clinical treatment of cardiovascular and cerebrovascular diseases (Lin et al. 2007). Previous studies have demonstrated significant neuroprotective effects of scutellarin such as anti-oxidant (Guo et al. 2011; Sang et al. 2015), anti-inflammatory (Guo et al. 2011; Sung et al. 2015; Yuan et al. 2014), and anti-apoptotic (Zhang et al. 2009) activities in ischemic cerebrovascular disease. More specifically, scutellarin has been reported to decrease infarct size, activate microglia in the brains of middle cerebral artery occlusion (MCAO) rats, and inhibit the activation of microglia via the Notch pathway (Yuan et al. 2015, 2014). Moreover, recent studies have demonstrated that scutellarin suppresses the activation of TLR4 and NF-κB in the brains of hypertensive rats and attenuates the inflammatory response in LPS-induced BV-2 microglia by inhibiting activation of NF-κB (Chen et al. 2013; Guo et al. 2011). Several intracellular inflammation-associated pathways, including PI3K/AKT and mitogen-activated protein kinase (MAPK), are involved in the activation of microglia (Jiamvoraphong et al. 2017). Therefore, inhibition of aberrant microglia activation is considered an efficient therapeutic strategy for neurodegenerative diseases. Thus, the current study aimed to explore whether scutellarin is able to exert anti-inflammatory activity via PI3K/AKT and MAPK signaling in neuroinflammation.
Materials and methods
Cell culture and treatment
The BV-2 cell line was purchased from the China Center for Type Culture Collection (CCTCC) (Wuhan, Hubei). BV-2 cells were cultured in RPMI 1640 medium (HyClone Laboratories, South Logan, UT, USA) supplemented with 10% fetal bovine serum (Gibco, Gaithersburg, MD, USA), 100 U/ml penicillin, and 100 μg/ml streptomycin. Cells were incubated at 37 °C in an atmosphere of 5% CO2 and checked for mycoplasma contamination once a month using Hoechst 33258 Staining. Scutellarin (Sigma-Aldrich, St. Louis, MO, USA) was dissolved in DMSO as a stock solution (100 mg/ml). LPS (Escherichia coli O111:B4) (Sigma-Aldrich) was dissolved in phosphate buffered saline (PBS) (Thermo Fisher Scientific, Waltham, MA, USA) as a stock solution (5 mg/ml). BV-2 cells were treated with varying concentrations of scutellarin (10, 20, or 40 μg/ml) in the presence or absence of 1 μg/ml LPS for 3, 12, or 24 h.
Cell viability
BV-2 cells (8 × 104 cells/ml) were seeded into a 96-well plate and treated with scutellarin at varying concentrations with or without LPS for 24 h. Then, 10 μl of Cell Counting Kit-8 (CCK-8) (Engreen Biosystem Ltd., Beijing, China) reagent was added into each well and incubated at 37 °C for 4 h. The CCK-8 reagent contains a novel highly water-soluble tetrazolium salt which is reduced by dehydrogenase activities in cells to generate a yellow water-soluble formazan dye, and the amount of the formazan dye is directly proportional to the number of viable cells. After incubation, OD values were measured at 450 nm using a Model 680 microplate reader (Bio-Rad, Hercules, CA, USA).
Measurement of pro-inflammatory mediators
BV-2 cells (5 × 105 cells/ml) were seeded into 12-well plates and routinely cultured until surface adherence was achieved. Cells were treated with scutellarin (10, 20, or 40 μg/ml) and co-cultured with LPS for 12 h. Cells with no treatment were included as a control. Cell-free supernatants were collected. Levels of TNF-α, IL-1β, and IL-6 were measured by ELISA (Shenzen DAKEWEI, Shenzen, Guangdong, China) following the manufacturer’s instructions and OD values were read at 450 nm. Levels of NO were measured by Griess reagent (Beyotime Institute of Biotechnology, Haimen, Jiangsu, China) following the manufacturer’s instructions and OD values were read at 570 nm.
Real-time RT-PCR
BV-2 cells were treated with scutellarin and co-cultured with LPS as mentioned above, then total RNA was extracted with the RNAsimple Total RNA Kit (TIANGEN Biotech, Beijing, China) and evaluated at 260 and 280 nm. Total RNA was reverse-transcribed using the RevertAid First Strand cDNA Synthesis Kit (Thermo Fisher Scientific). The initial cDNA was used as a PCR template for real-time PCR amplification with the KAPA SYBR FAST qPCR Kit (Kapa Biosystems, Wilmington, MA, USA) in a BIO-RAD CFX96 touch q-PCR system (Bio-Rad). PCR primer sequences were as follows (forward primer and reverse primer, respectively): β-actin (Xia et al. 2015): 5′-GACCTGACTGACTACCTC-3′, 5′-GACAGCGAGGCCAGGATG-3′; iNOS (Xia et al. 2015): 5′-TCCCAGCCTGCCCCTTCAAT-3′, 5′-CGGATCTCTCTCCTCCTGGG-3′; TNF-α (Li et al. 2016): 5′-TCTCATTCCTGCTTGTGGCA-3′, 5′-GGTGGTTTGCTACGACGTGG-3′; IL-6 (Li et al. 2016): 5′-TCTTGGGACTGATGCTGGTG-3′, 5′-TGCCATTGCACAACTCTTTTCT-3′; IL-1β (Li et al. 2016): 5′-CCAAAAGATGAAGGGCTGCTT-3′, 5′-GAAAAGAAGGTGCTCATGTCCTC-3′. PCR amplification was performed with initial denaturation for 3 min at 95 °C and 40 cycles of 10 s at 95 °C, 30 s at 60 °C, and 30 s at 72 °C.
Western blotting
BV-2 cells (1 × 106 cells/ml) were seeded into 6-well plates and treated with scutellarin (10, 20, or 40 μg/ml) in the presence or absence of LPS for 12 h. Cells were washed twice with cold PBS before lysing with the RIPA lysis Kit (Beyotime) containing 1 mM phenylmethanesulfonyl fluoride (PMSF) (Beyotime). The BCA protein assay kit (Takara, Kusatsu, Shiga, Japan) was used for determining the protein concentration of samples. Equal amounts of protein were separated on 10–12% SDS-PAGE and then electrophoretically transferred to nitrocellulose membranes (Amersham Biosciences, UK). Membranes were blocked with 5% bull serum albumin (BSA) (Sigma-Aldrich) for 2 h and then incubated at 4 °C overnight with primary antibodies including anti-p-Ikkα/β, anti-Ikkβ, anti-Ikkα, anti-p-IκBα, anti-IκBα, anti-p-p65, anti-p65, anti-p-PI3K, anti-PI3K, anti-p-AKT, anti-AKT, anti-p-JNK, anti-JNK, anti-p-p38, anti-p38, anti-p-ERK1/2, anti-ERK1/2, and anti-β-actin (1:1000 dilution in TBS with 0.05% Tween-20 [TBST]). All antibodies were acquired from Cell Signaling Technology (Danvers, MA, USA). Following incubation with primary antibody, membranes were washed three times with TBST and incubated with HRP-conjugated secondary antibody (1:2000) (Cell Signaling Technology) for 1 h at room temperature. Blots were then washed with TBST and developed using an ECL detection reagent (Bio-Rad). The optical density was measured using a FluorChem 8000 system (AlphaInnotech, San Leandro, CA, USA).
Immunofluorescent staining
BV-2 cells (5 × 105 cells/ml) were seeded into 6-well plates with sterilized coverslips and treated with 20 μg/ml scutellarin with or without LPS for 3 h. Cells were then fixed in 4% paraformaldehyde for 30 min and washed three times with PBS. Cells were permeabilized using 0.5% Triton X-100 for 10 min and then blocked with 5% BSA for 1 h at room temperature. Cells were then incubated with anti-NFκB-p65 primary antibody (1:400) (Cell Signaling Technology) for 1 h at 37 °C, washed three times with PBS, and subsequently incubated with Alexa Fluor 488 conjugated Anti-Rabbit IgG secondary antibody (1:1000) (Cell Signaling Technology). After washing three times with PBS containing 0.05% Tween-20, cells were stained with DAPI (1 μg/ml) (Biosharp, HF, China) for 5 min and washed again three times with PBS. The coverslips with cells were sealed using 90% glycerinum and visualized using a fluorescence microscope (Olympus, Japan).
Statistical analysis
All experiments were independently repeated three times with at least three replicates for each independent assay. Then, data are expressed as mean ± standard deviation (SD). Statistical significance of data was analyzed by ANOVA using IBM SPSS Statistics 24.0 (IBM, Armonk, NY). A p value < 0.05 was considered statistically significant.
Results
BV-2 cell viability assay with scutellarin
The effects of scutellarin on BV-2 cell viability in the absence or presence of LPS were examined by CCK8 assay. The viability of BV-2 cells was not significantly inhibited by scutellarin at concentrations below 40 μg/ml in the absence or presence of LPS (1 μg/ml) as compared to the control group. However, when treated with 80 μg/ml scutellarin, cell viability decreased to 87.64% in the absence of LPS and 80.98% in the presence of LPS for 24 h. The inhibitory effect exerted by scutellarin was statistically significant as compared to the control group (p < 0.01) (Fig. 1). Since lower doses of scutellarin in the presence of LPS (1 μg/ml) had no inhibitory effect on the viability of BV-2 cells, concentrations of 10, 20, or 40 μg/ml scutellarin were chosen for subsequent experiments.
Effect of scutellarin on the viability of BV-2 cells. BV-2 cells were treated with scutellarin (0–80 μg/ml) in the absence or presence of LPS for 24 h and the cell viability was measured by CCK8 assay. Results are expressed as the mean of three independent experiments. *p < 0.05, **p < 0.01 vs control
Scutellarin downregulates pro-inflammatory mediators in LPS-induced BV-2 cells
To evaluate the anti-inflammatory effects of scutellarin on LPS-induced BV-2 cells, the levels of TNF-α, IL-1β, IL-6, and NO and TNF-α, IL-1β, IL-6, and iNOS mRNA were evaluated. Compared with the control group, the production of TNF-α, IL-1β, IL-6, and NO (Fig. 2a–d) and the levels of TNF-α, IL-1β, IL-6, and iNOS mRNA (Fig. 2e–h) were significantly increased following stimulation with LPS (p < 0.01). However, pretreatment with scutellarin decreased the production of TNF-α, IL-1β, IL-6, and NO and the levels of TNF-α, IL-1β, IL-6, and iNOS mRNA in LPS-induced BV-2 cells, and the inhibitory effects were statistically significant at all concentrations compared to the LPS group (p < 0.05, p < 0.01) (Fig. 2).
Effects of scutellarin on production of pro-inflammatory mediators in LPS-induced BV-2 cells. BV-2 cells were treated with 10, 20, or 40 μg/ml scutellarin with or without 1 μg/ml LPS for 12 h. The levels of a TNF-α, b IL-1β, c IL-6, and d NO and e TNF-α, f IL-1β, g IL-6, and h iNOS mRNA were measured. Results are expressed as the mean of three independent experiments. #p < 0.05, ##p < 0.01 vs control group; and *p < 0.05,**p < 0.01 vs LPS group
Scutellarin inhibits NF-κB activation in LPS-induced BV-2 cells
NF-κB plays a crucial role in regulating the transcription of iNOS genes and the inflammatory response. To evaluate whether scutellarin inhibited the activation of NF-κB in LPS-induced BV-2 cells, we examined NF-κB pathway-related protein expression using western blots and the nuclear translocation of NF-κB using immunofluorescent staining. As shown in Fig. 3a, the phosphorylation of IKKα/β, IκBα, and p65 levels were markedly upregulated compared to those of the control group (p < 0.01), and the expression of IκBα was markedly downregulated compared to that of the control group (p < 0.01) in LPS-induced BV-2 cells. Scutellarin significantly downregulated the phosphorylation of these proteins compared to the LPS group (p < 0.01, p < 0.05) and upregulated the expression of IκBα in LPS-induced BV-2 cells from a concentration of 20 μg/ml onward compared to the LPS group (p < 0.05). The expression of IKKβ was significantly downregulated in LPS-induced BV-2 cells compared to LPS group (p < 0.01, p < 0.05), but the expression of p65 and IKKα was not affected by scutellarin. According to the results obtained by immunofluorescent staining, NF-κB-p65 in the control group was mostly cytoplasmic and translocated to the nucleus when treated with LPS. However, when treated with scutellarin in the presence of LPS, the nuclear translocation was blocked (Fig. 3b). Taken together, these data suggest that scutellarin may inhibit the activation of NF-κB by suppressing the phosphorylation of p65, degradation of IκB, and expression of IKKβ in LPS-induced BV-2 cells.
Scutellarin regulates activation of the NF-κB pathway. a Scutellarin inhibited phosphorylation of IKKα/β, IκBα, p65, and expression of IKKβ, and promoted the expression of IκBα. b Scutellarin blocked translocation of NF-κB-p65 (× 200, green) into the nucleus in LPS-induced BV-2 cells. Results are expressed as the mean of three independent experiments. #p < 0.05, ##p < 0.01 vs control group; and *p < 0.05, **p < 0.01 vs LPS group
Scutellarin inhibits the phosphorylation of p38, JNK, and AKT in LPS-induced BV-2 cells
The PI3K/AKT pathway and MAPKs play an important role in the inflammatory response. To further investigate whether scutellarin inhibits neuroinflammation via the PI3K/AKT and MAPK pathway, levels of related proteins were evaluated. The phosphorylation of PI3K and AKT were significantly upregulated by LPS compared to the control group (p < 0.01), and the phosphorylation of AKT was slightly downregulated following treatment with scutellarin as compared to the LPS group (p < 0.05). However, the phosphorylation of PI3K was not affected (Fig. 4a). Similarly, the phosphorylation of p38, JNK, and ERK1/2 were significantly upregulated in LPS-induced BV-2 cells compared to those of the control group (p < 0.01) while scutellarin downregulated the phosphorylation of p38 and JNK in LPS-induced BV-2 cells compared to LPS group (p < 0.01, p < 0.05). However, the phosphorylation of ERK1/2 was seemingly unchanged (Fig. 4a). Scutellarin appears to inhibit the phosphorylation of p38 and JNK but not affect phosphorylation of the ERK1/2 in LPS-induced BV-2 cells.
Scutellarin inhibits neuroinflammation via the PI3K/AKT and MAPK pathway. a Scutellarin inhibited the phosphorylation of AKT in LPS-induced BV-2 cells. b Scutellarin inhibited the phosphorylation of p38 and JNK in LPS-induced BV-2 cells. Results are expressed as the mean of three independent experiments. #p < 0.05, ##p < 0.01 vs control group; and *p < 0.05, **p < 0.01 vs LPS group
Discussion
Erigeron breviscapus (Vant.) Hand. Mazz., a famous traditional Chinese herbal medicine, has been used for the treatment of cerebrovascular and cardiovascular diseases for many years (Chu et al. 2005). Scutellarin, the main bioactive flavonoid glycoside isolated from E. breviscapus, exerts efficient neuroprotection through multiple mechanisms (Chu et al. 2005; Liu et al. 2005). In recent years, scutellarin has been reported to have anti-inflammatory effects especially in microglia-mediated neuroinflammation (Guo et al. 2011, 2013; Sung et al. 2015). In this study, we demonstrated the inhibitory effects on neuroinflammation and clarified the molecular mechanism regulated by scutellarin.
Scutellarin had no negative effects on cell viability below 40 μg/ml. We demonstrated that scutellarin suppressed LPS-induced production of NO and downregulated expression of iNOS mRNA, thus suppressing BV-2 cell activation. NO plays a key role in the inflammatory response as a main cytotoxic mediator in activated microglia, and NO production is regulated by iNOS which is expressed at low levels under normal condition and induced in activated microglia (Kim et al. 2013; Rivest 2003; Schwartz and Shechter 2010). Moreover, the transcription of the iNOS gene is activated by pro-inflammatory cytokines such as TNF-α, IL-1β, and IL-6 in activated microglia, which contributes to the development of chronic inflammation (Gebicke-Haerter 2001; Liang et al. 2007; Wang et al. 2003). Consistent with our research, recent studies have reported that scutellarin inhibits TNF-α, IL-1β, and NO production and downregulates the expression of relevant mRNA in activated microglia, as well as in macrophages (Guo et al. 2011; Sung et al. 2015; Wang et al. 2011). In MCAO rats, scutellarin also inhibits TNF-α, IL-1β, and iNOS expression after cerebral ischemic injury (Yuan et al. 2015, 2014). Our results indicate that scutellarin inhibits the production of TNF-α, IL-1β, and IL-6 via downregulating mRNA expression. TNF-α and IL-1β are released in response to neuroinflammation, inducing the expression of chemokines which ultimately exacerbates the damage of neurons (Dheen et al. 2007; Rothwell 2003). Similarly, IL-6 is also considered a vital cytokine in the neuroinflammatory process and microglia activation. Additionally, it is reported that scutellarin is minimally toxic or nontoxic in rodents and did not result in significant changes in biochemical examination under test doses (Yuan et al. 2016). Thus, scutellarin is considered to have little basal effects on BV-2 cells. Our data suggest that scutellarin may inhibit these pro-inflammatory mediators at the transcriptional level without negatively affecting cell viability.
One of the most important intracellular signaling molecules involved in the inflammatory response is NF-κB which targets iNOS, TNF-α, IL-1β, and IL-6. The present study showed that scutellarin inhibited the nuclear translocation of NF-κB, which downregulated expression of the related mRNAs, and subsequently suppressed the release of pro-inflammatory mediators. Our study also demonstrated that scutellarin inhibited the phosphorylation and degradation of IκB, an inhibitor bound to NF-κB in the cytoplasm, which is degraded when activated by noxious stimuli such as LPS, thus liberating NF-κB to translocate to the nucleus (Carayol et al. 2006). Additionally, our results showed that scutellarin inhibited the phosphorylation of signaling molecules upstream of NF-κB including IKK and AKT. As the upstream kinase for IκB, activated IKK phosphorylates IκB resulting in ubiquitination and degradation (Arkan et al. 2005). Both subunits of IKK, IKKα and IKKβ, are required for PI3K/AKT-mediated phosphorylation and the transcription potential of the RelA/p65 subunit of NF-κB, but IKKα is dispensable for IκB degradation and NF-κB translocation. IKKβ plays an essential role in LPS-induced IκB phosphorylation, degradation, and NF-κB liberation (Sizemore et al. 2002; Yang et al. 2003). In line with current research, our results suggest that the inhibition of NF-κB activation is due to the inhibition of IKK phosphorylation by scutellarin. Interestingly, scutellarin also downregulated the expression of IKKβ, which contributed to the attenuation of IKK phosphorylation as well as NF-κB phosphorylation and liberation. In addition to IKKα/β, PI3K/AKT also plays a role in the activation of NF-κB, which targets the trans-activation domain of the RelA/p65 subunit of NF-κB in an IKKβ and p38-dependent manner (Madrid et al. 2001). Furthermore, it was reported not only that AKT activated the IKK complex, but also that IKKβ might potentiate the phosphorylation of AKT creating a feed forward control (Sommermann et al. 2011). Our findings indicate that activation of AKT was suppressed, but PI3K was not, which suggests that suppression of AKT activation by scutellarin might be due to the interaction between AKT and IKKβ but not PI3K activation, and does not predominate in IκB degradation accompanied by the activation of NF-κB. In summary, our present study suggests that scutellarin inhibits IκB degradation and NF-κB activation via suppression of IKKβ activity, which ultimately blocks NF-κB from translocating into the nucleus, binding to DNA, and upregulating the expression of iNOS, TNF-α, IL-1β, and IL-6 mRNA.
Additionally, another group of signaling molecules, MAPKs, of which members include p38, JNK, and ERK1/2, is also involved in the production of pro-inflammatory mediators and modulation of NF-κB (Kim et al. 2006). The activation of MAPK and NF-κB is induced by TLR4 activation when stimulated by LPS. Then, the MAPK signaling cascade triggers the transcription of cellular inflammatory response-associated genes mediated by NF-κB and the synthesis of pro-inflammatory mediators (Cuenda and Rousseau 2007; Imajo et al. 2006). Accordingly, suppression of only NF-κB is insufficient for inhibiting the inflammatory response. Our study further indicated that scutellarin suppressed the phosphorylation of p38 and JNK but had no effect on the phosphorylation of ERK1/2 induced by LPS. Previous studies reported that p38 and JNK are activated by stress reactions and cytokines, which mediate the differentiation and death of cells, and are thus regarded as stress-activated MAPKs. However, ERK1/2 is mostly associated with growth factors and cell proliferation (Rincón et al. 2000). Hence, the results suggested that scutellarin might inhibit the phosphorylation of p38 and JNK via inhibiting the upstream kinase.
In conclusion, the present study demonstrates that scutellarin may inhibit the production of pro-inflammatory mediators by blocking the activation of NF-κB via suppression of IKKβ activity and IκB degradation, accompanied by blocking of AKT, p38, and JNK activation without affecting PI3K and ERK1/2 in order to exert anti-inflammatory action in LPS-induced BV-2 cells. Taken together, our findings clarify, at least in part, the anti-neuroinflammation mechanism of scutellarin in LPS-induced BV-2 cells and provide a theoretical basis for its success in the clinical treatment of neurodegenerative and cerebrovascular diseases.
References
Arkan MC, Hevener AL, Greten FR, Maeda S, Li Z-W, Long JM, Wynshaw-Boris A, Poli G, Olefsky J, Karin M (2005) IKK-β links inflammation to obesity-induced insulin resistance. Nat Med 11:191–198
Bhalala US, Koehler RC, Kannan S (2015) Neuroinflammation and neuroimmune dysregulation after acute hypoxic-ischemic injury of developing brain. Front Pediatr 2:144
Block ML, Hong J-S (2005) Microglia and inflammation-mediated neurodegeneration: multiple triggers with a common mechanism. Prog Neurobiol 76:77–98
Bosman MC, Schuringa JJ, Vellenga E (2016) Constitutive NF-kappaB activation in AML: causes and treatment strategies. Crit Rev Oncol Hematol 98:35–44
Carayol N, Chen J, Yang F, Jin T, Jin L, States D, Wang CY (2006) A dominant function of IKK/NF-kappaB signaling in global lipopolysaccharide-induced gene expression. J Biol Chem 281:31142–31151
Chen X, Shi X, Zhang X, Lei H, Long S, Su H, Pei Z, Huang R (2013) Scutellarin attenuates hypertension-induced expression of brain toll-like receptor 4/nuclear factor kappa B. Mediat Inflamm 2013:432623
Chu Q, Wu T, Fu L, Ye J (2005) Simultaneous determination of active ingredients in Erigeron breviscapus (Vant.) Hand-Mazz. by capillary electrophoresis with electrochemical detection. J Pharm Biomed Anal 37:535–541
Cuenda A, Rousseau S (2007) p38 MAP-kinases pathway regulation, function and role in human diseases. Biochim Biophys Acta 1773:1358–1375
Dheen ST, Kaur C, Ling EA (2007) Microglial activation and its implications in the brain diseases. Curr Med Chem 14:1189–1197
Gebicke-Haerter PJ (2001) Microglia in neurodegeneration: molecular aspects. Microsc Res Tech 54:47–58
Glass CK, Saijo K, Winner B, Marchetto MC, Gage FH (2010) Mechanisms underlying inflammation in neurodegeneration. Cell 140:918–934
Guo H, Hu LM, Wang SX, Wang YL, Shi F, Li H, Liu Y, Kang LY, Gao XM (2011) Neuroprotective effects of scutellarin against hypoxic-ischemic-induced cerebral injury via augmentation of antioxidant defense capacity. Chin J Physiol 54:399–405
Guo LL, Guan ZZ, Huang Y, Wang YL, Shi JS (2013) The neurotoxicity of beta-amyloid peptide toward rat brain is associated with enhanced oxidative stress, inflammation and apoptosis, all of which can be attenuated by scutellarin. Exp Toxicol Pathol 65:579–584
Imajo M, Tsuchiya Y, Nishida E (2006) Regulatory mechanisms and functions of MAP kinase signaling pathways. IUBMB Life 58:312–317
Jiamvoraphong N, Jantaratnotai N, Sanvarinda P, Tuchinda P, Piyachaturawat P, Thampithak A, Sanvarinda P (2017) Concurrent suppression of NF-kappaB, p38 MAPK and reactive oxygen species formation underlies the effect of a novel compound isolated from Curcuma comosa Roxb. in LPS-activated microglia. J Pharm Pharmacol 69:917–924
Kim HG, Shrestha B, Lim SY, Yoon DH, Chang WC, Shin DJ, Han SK, Park SM, Park JH, Park HI, Sung JM, Jang Y, Chung N, Hwang KC, Kim TW (2006) Cordycepin inhibits lipopolysaccharide-induced inflammation by the suppression of NF-kappaB through Akt and p38 inhibition in RAW 264.7 macrophage cells. Eur J Pharmacol 545:192–199
Kim BW, Koppula S, Hong SS, Jeon SB, Kwon JH, Hwang BY, Park EJ, Choi DK (2013) Regulation of microglia activity by glaucocalyxin-A: attenuation of lipopolysaccharide-stimulated neuroinflammation through NF-kappaB and p38 MAPK signaling pathways. PLoS One 8:e55792
Li Q, Chen Y, Zhang X, Zuo S, Ge H, Chen Y, Liu X, Zhang JH, Ruan H, Feng H (2016) Scutellarin attenuates vasospasm through the Erk5-KLF2-eNOS pathway after subarachnoid hemorrhage in rats. J Clin Neurosci 34:264–270
Liang X, Wu L, Wang Q, Hand T, Bilak M, McCullough L, Andreasson K (2007) Function of COX-2 and prostaglandins in neurological disease. J Mol Neurosci 33:94–99
Lin L, Liu A, Jg YX, Qin L, Su D (2007) Protective effects of scutellarin and breviscapine on brain and heart ischemia in rats. J Cardiovasc Pharmacol 50:327–332
Liu F, McCullough LD (2013) Inflammatory responses in hypoxic ischemic encephalopathy. Acta Pharmacol Sin 34:1121–1130
Liu H, Yang X, Tang R, Liu J, Xu H (2005) Effect of scutellarin on nitric oxide production in early stages of neuron damage induced by hydrogen peroxide. Pharmacol Res 51:205–210
Luo Q, Yan X, Bobrovskaya L, Ji M, Yuan H, Lou H, Fan P (2017) Anti-neuroinflammatory effects of grossamide from hemp seed via suppression of TLR-4-mediated NF-kappaB signaling pathways in lipopolysaccharide-stimulated BV2 microglia cells. Mol Cell Biochem 428:129–137
Madrid LV, Mayo MW, Reuther JY, Baldwin AS Jr (2001) Akt stimulates the transactivation potential of the RelA/p65 subunit of NF-kappa B through utilization of the Ikappa B kinase and activation of the mitogen-activated protein kinase p38. J Biol Chem 276:18934–18940
Rincón M, Flavell RA, Davis RA (2000) The JNK and P38 MAP kinase signaling pathways in T cell–mediated immune responses4. Free Radic Biol Med 28:1328–1337
Rivest S (2003) Molecular insights on the cerebral innate immune system. Brain Behav Immun 17:13–19
Rothwell N (2003) Interleukin-1 and neuronal injury: mechanisms, modification, and therapeutic potential. Brain Behav Immun 17:152–157
Sang Z, Li Y, Qiang X, Xiao G, Liu Q, Tan Z, Deng Y (2015) Multifunctional scutellarin-rivastigmine hybrids with cholinergic, antioxidant, biometal chelating and neuroprotective properties for the treatment of Alzheimer’s disease. Bioorg Med Chem 23:668–680
Schwartz M, Shechter R (2010) Systemic inflammatory cells fight off neurodegenerative disease. Nat Rev Neurol 6:405–410
Shih VF, Tsui R, Caldwell A, Hoffmann A (2011) A single NFkappaB system for both canonical and non-canonical signaling. Cell Res 21:86–102
Shukla V, Shakya AK, Perez-Pinzon MA, Dave KR (2017) Cerebral ischemic damage in diabetes: an inflammatory perspective. J Neuroinflammation 14:21
Sizemore N, Lerner N, Dombrowski N, Sakurai H, Stark GR (2002) Distinct roles of the Ikappa B kinase alpha and beta subunits in liberating nuclear factor kappa B (NF-kappa B) from Ikappa B and in phosphorylating the p65 subunit of NF-kappa B. J Biol Chem 277:3863–3869
Sommermann TG, O’Neill K, Plas DR, Cahir-McFarland E (2011) IKKbeta and NF-kappaB transcription govern lymphoma cell survival through AKT-induced plasma membrane trafficking of GLUT1. Cancer Res 71:7291–7300
Sung NY, Kim MY, Cho JY (2015) Scutellarein reduces inflammatory responses by inhibiting Src kinase activity. Korean J Physiol Pharmacol 19:441–449
Tuttolomondo A, Di Raimondo D, di Sciacca R, Pinto A, Licata G (2008) Inflammatory cytokines in acute ischemic stroke. Curr Pharm Des 14:3574–3589
Vidale S, Consoli A, Arnaboldi M, Consoli D (2017) Postischemic inflammation in acute stroke. J Clin Neurol 13:1–9
Wang W, Ji P, Dow KE (2003) Corticotropin-releasing hormone induces proliferation and TNF-alpha release in cultured rat microglia via MAP kinase signalling pathways. J Neurochem 84:189–195
Wang S, Wang H, Guo H, Kang L, Gao X, Hu L (2011) Neuroprotection of scutellarin is mediated by inhibition of microglial inflammatory activation. Neuroscience 185:150–160
Wu MH, Huang CC, Chio CC, Tsai KJ, Chang CP, Lin NK, Lin MT (2016) Inhibition of peripheral TNF-alpha and downregulation of microglial activation by alpha-lipoic acid and etanercept protect rat brain against ischemic stroke. Mol Neurobiol 53:4961–4971
Xia Q, Hu Q, Wang H, Yang H, Gao F, Ren H, Chen D, Fu C, Zheng L, Zhen X, Ying Z, Wang G (2015) Induction of COX-2-PGE2 synthesis by activation of the MAPK/ERK pathway contributes to neuronal death triggered by TDP-43-depleted microglia. Cell Death Dis 6:e1702
Yang F, Tang E, Guan K, Wang CY (2003) IKKβ plays an essential role in the phosphorylation of RelA/p65 on serine 536 induced by lipopolysaccharide. J Immunol 170:5630–5635
Yuan Y, Zha H, Rangarajan P, Ling EA, Wu C (2014) Anti-inflammatory effects of edaravone and scutellarin in activated microglia in experimentally induced ischemia injury in rats and in BV-2 microglia. BMC Neurosci 15:125
Yuan Y, Rangarajan P, Kan EM, Wu Y, Wu C, Ling EA (2015) Scutellarin regulates the Notch pathway and affects the migration and morphological transformation of activated microglia in experimentally induced cerebral ischemia in rats and in activated BV-2 microglia. J Neuroinflammation 12:11
Yuan Y, Fang M, Wu CY, Ling EA (2016) Scutellarin as a Potential Therapeutic Agent for Microglia-Mediated Neuroinflammation in Cerebral Ischemia. Neuromolecular Med 18:264–273
Zhang HF, Hu XM, Wang LX, Xu SQ, Zeng FD (2009) Protective effects of scutellarin against cerebral ischemia in rats: evidence for inhibition of the apoptosis-inducing factor pathway. Planta Med 75:121–126
Funding
This study was supported by China Postdoctoral Science Foundation (no. 2016 M592320), Hubei Provincial Natural Science Foundation of China (no. 2018CFB657), and the National Natural Science Foundation of China (nos. 31570343, 31670341, and 31270405).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
You, P., Fu, S., Yu, K. et al. Scutellarin suppresses neuroinflammation via the inhibition of the AKT/NF-κB and p38/JNK pathway in LPS-induced BV-2 microglial cells. Naunyn-Schmiedeberg's Arch Pharmacol 391, 743–751 (2018). https://doi.org/10.1007/s00210-018-1503-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-018-1503-7