Abstract
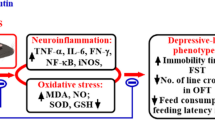
This study was designed to evaluate the effect of quercetin, a natural flavonoid, on behavioral alterations, brain oxidative stress, and immune dysregulation caused by a chemotherapeutic agent, Adriamycin (ADR; 7 mg/kg of body weight). Different subsets of male Wistar rats were used to determine the benefit of quercetin on ADR-related depression-like and anxiety-like behaviors in the forced swim test, open field, and elevated plus maze, respectively. Quercetin (60 mg/kg of body weight) was administered 24, 5, and 1 h before the test session of forced swim test (FST) or at the same time points before the elevated plus maze/open field (EPM/OF) tests. Other subsets of rats were sacrificed after quercetin injections to assess the plasma corticosterone level, the brain oxidative status, and the immune cell count. Our results indicate that quercetin alleviated the anxio-depressive-like behavior, attenuated the brain oxidative stress, and suppressed the corticosterone excess that appeared following ADR treatment. The ADR-induced immune disturbance was slightly diminished after quercetin administration, especially for the lymphocyte count. This study suggests that quercetin can mitigate the neurobehavioral and immunological impairments that manifest in ADR-treated rats. Therefore, the combination of quercetin treatment with the chemotherapeutic regimen seems to be beneficial against chemotherapy-related complications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Among anthracyclines, Adriamycin (ADR) is a powerful antineoplastic agent, widely used for the treatment of human’s solid tumors by blocking the process of replication in the malignant cells (Cutts et al. 2003). However, the clinical use of ADR is compromised by the development of life-threatening adverse effects, such as myelosuppression, fatigue, and cognitive impairments (Jansen et al. 2008). Recently, ADR-related neurobehavioral changes have been indicated using established rodent models (Liedke et al. 2009; Merzoug et al. 2011).
Several investigations have revealed that chemotherapeutic agents, including ADR, are responsible for brain tissue injury (Ahles and Saykin 2007). ADR modulates endogenous levels of cytokines, such as tumor necrosis factor alpha (TNF-α), leading to reactive oxygen and/or nitrogen species (ROS/RNS) production which results in brain oxidative stress (Joshi et al. 2005, 2007; Tangpong et al. 2006, 2007). It was also reported that ADR-mediated free radicals generation in the brain tissue increases lipid peroxidation and protein oxidation and alters the antioxidant defense system which can enhance the oxidative stress (Joshi et al. 2005, 2007, 2010) leading to neuropsychological changes (Dubovický 2010).
Chemotherapeutic drugs have been reported to induce toxic effects on immune cells in bone marrow and peripheral lymphoid tissues (Park et al. 2009). Interestingly, chemotherapy-associated myelotoxicity and immunosuppression might increase the release of inflammatory cytokines, which cross the blood–brain barrier and activate microglia, resulting in neuroinflammation and subsequent neuropsychiatric and cognitive symptoms (Ahles and Saykin 2007). Nowadays, it is well documented that the central nervous system (CNS) and the immune system (IS) are intimately linked through bidirectional chemical messengers (Banks and Erickson 2010). Importantly, the IS has been implicated in neurodegenerative diseases that accompany CNS injuries (Kipnis et al. 2008). Therein, preliminary experiments revealed that the hypothalamo-pituitary-adrenocortical (HPA) axis is involved in the protection of the rat against chemotherapeutic-induced toxic outcomes. In adrenalectomized or hypophysectomized rats, the lethal effects of anticancer drugs were considerably increased, probably due to the omitted corticosterone release (Navarra and Preziosi 1997). However, it is well known that stressful conditions, such as chemical stresses, result in enhanced HPA axis activity and, thus, lead to increased plasma glucocorticoids released from the adrenal cortex (Heim et al. 2000). Consequently, the behavioral outcomes of stress, such as anxiety and depression, are believed to be mediated by enhanced values of glucocorticoids (Berton and Nestler 2006).
Flavonoids belong to the family of natural polyphenols widely distributed in the plant kingdom, including apples, berries, onion, tea, seeds, and vegetables (Hollman and Kata 1999). Quercetin (Q, 3,5,7,3′,4′-pentahydroxyflavone) is the most abundant bioflavonoid in the human diet (Manach et al. 2004). Whatever the route of administration, a considerable amount of quercetin is metabolized during its first passage through the liver, resulting especially in the formation of methylated metabolites such as isorhamnetin and tamarixetin (van der Woude et al. 2004). Urinary and biliary excretions of either the unchanged form of quercetin or its conjugates were reported in previous pharmacokinetics studies (Gugler et al. 1975). Quercetin has a powerful antioxidant capacity, protecting the body against oxidative stress-related damages (Haleagrahara et al. 2009). With the ability of crossing the blood–brain barrier in vivo, quercetin and its metabolites appear in the brain after several hours of quercetin administration (Paulke et al. 2006), exerting beneficial actions on the CNS such as neuroprotection and anxiolytic and cognitive-enhancing effects (Cho et al. 2006). More recently, several experimental studies have demonstrated the efficacy of quercetin against depressive disorders in rodents. Indeed, it has been noted that quercetin-enriched foods, such as freeze-dried onion powder and Ginkgo biloba leaves, are regarded to possess an antidepressant-like activity in the forced swimming test (Rojas et al. 2011; Sakakibara et al. 2008), a behavioral paradigm for the assessment of antidepressant drugs efficacy. Moreover, it was reported that quercetin inhibits the corticotrophin releasing factor (CRF)-induced anxiety- and depression-like behaviors in mice and rats (Bhutada et al. 2010; Kawabata et al. 2010).
Fruits and vegetables rich in quercetin are believed to protect the brain tissue from oxidative stress-related neurodegenerative diseases (Heo and Lee 2004; Youdim et al. 2004). Importantly, quercetin prevented stress-induced oxidative damage in neurons by inhibiting hydroperoxide formation, scavenging free radicals, and preserving antioxidant enzymes (Dok-Go et al. 2003; Haleagrahara et al. 2009). Quercetin also attenuated neuronal damage in rodents’ hippocampus following cerebral ischemia in vivo (Cho et al. 2006; Pu et al. 2007), and it is therefore suggested to be of therapeutic benefit in the treatment of Alzheimer’s and Parkinson’s diseases (Choi et al. 2012; Haleagrahara et al. 2011).
Previous investigations highlighted the immunostimulatory effects of quercetin by enhancing lymphocyte activation and/or secretion of the multipotent cytokine interferon-γ (Cherng et al. 2008), neutrophil chemotaxis and oxidative burst activity (Akbay et al. 2003), macrophage stimulation (Oršolić and Bašić 2005), and natural killer cell activity (Yu et al. 2010). Other studies have shown that quercetin inhibits the production of pro-inflammatory cytokines (Cho et al. 2003; Min et al. 2007) through inhibition of neuroendocrine signaling pathways (Spencer 2007), which may lead to normalization of stressor-mediated overactive HPA axis.
In this respect, the current study was aimed to investigate the possible beneficial effect of quercetin against ADR-related anxio-depressive-like behavior, plasma corticosterone hyperactivity, brain oxidative stress, and immune alterations in male Wistar rats.
Methods
Animals and housing
Sixty-eight adult male Wistar rats were obtained from Pasteur Institute (Algiers, Algeria) and individually housed in transparent cages in a temperature-controlled facility room (23 ± 1 °C). Rats were maintained on a 12-h/12-h light cycle (lights on at 07:30 a.m.) with access to standard rodents chow and tap water ad libitum. The experimental protocol was carried out according to the NIH revised Guidelines for the Care and Use of Laboratory Animals (No. 80-23, 1996).
Drugs
Adriamycin (doxorubicin hydrochloride) and quercetin (quercetin dihydrate) were purchased from Sigma-Aldrich Co. (Steinheim, Germany). Both ADR (7 mg/kg of body weight) and quercetin (60 mg/kg of body weight) were dissolved in saline solution (0.9 %) and injected intraperitoneally (i.p.) in a volume of 1 ml/kg of body weight according to the experimental procedure detailed below. Seven milligrams per kilogram of body weight of ADR was chosen based on our previous study, in which this dose has been indicated to induce anxiety-like behavior and locomotor anomalies with a concomitant brain oxidative injury and immune depletion (Merzoug et al. 2011). In many rodent studies, it was reported that the most effective physiological dose of quercetin is 60 mg/kg of body weight (Filho et al. 2008; Song et al. 2002).
Experimental procedure
The entire study includes three experiments in parallel. The 68 rats were randomly divided into four groups: vehicle-treated control (C) rats, ADR-treated rats (ADR), quercetin (Q)-treated rats, and quercetin-injected rats pretreated with ADR (ADR + Q). Animals received a single i.p. injection of saline (groups C and Q) or ADR (groups ADR and ADR + Q). A treatment with saline (groups C and ADR) or quercetin (groups Q and ADR + Q) was therefore conducted at specific time points in order to evaluate the ability of this flavonoid to reverse ADR-related neurobehavioral and immune disorders according to the procedure of each experiment (Fig. 1).
Experiment 1
This experiment aimed at investigating the effect of quercetin on ADR-induced depression-like behavior in the forced swim test (FST). Seventy-two hours post-ADR injection, 24 rats (n = 6) were individually subjected to the first session of FST (i.e., the pretest session) as described below. Quercetin (groups Q and ADR + Q) or saline (groups C and ADR) injections were performed 24, 5, and 1 h before the second session of FST (i.e., the test session) during which the animals’ behavior was evaluated (Fig. 1). These time points of quercetin treatment are based on the method described by Porsolt et al. (1977) for the evaluation of antidepressant effects. It is interesting to note that the cumulative dose (i.e., 180 mg/kg of body weight) has no toxicological effects in rats (Russo et al. 2012).
Experiment 2
The second experiment aimed at evaluating the effect of quercetin on ADR-induced anxiety-like behavior. Seventy-two hours post-ADR injection, animals (n = 6) directly received quercetin (groups Q and ADR + Q) or saline (groups C and ADR) injections at the same time points as described in the experiment 1, then behaviorally tested in the open field (OF) and the elevated plus maze (EPM) tasks instead of the second FST session (Fig. 1).
Experiment 3
During the third experiment, the rats (n = 5) directly received quercetin injections at the same time points as described in the experiment 1, then sacrificed by decapitation without being tested in the FST, the OF, nor the EPM (Fig. 1). Blood samples were collected into ethylenediaminetetraacetic acid (EDTA)-coated tubes to quantify white blood cells (WBCs), lymphocytes (LYM), monocytes (MONO), and granulocytes (GRAN) using an automatic cell counter (ERMA Inc., Model PCE-210, Tokyo, Japan). Plasma samples were used to determine corticosterone concentrations in duplicate using a commercially available RIA kit according to the manufacturer’s instructions (Sigma, USA). Immediately after sacrifice, the brains were dissected out and rinsed with ice-cold isotonic saline. Brain samples were prepared with ice-cold 0.1 mol/l phosphate buffer (pH 7.4) to obtain 1:10 (w/v) homogenates, and then centrifuged at 10,000 g (4 °C) for 15 min. The supernatant aliquots were used for assessing the oxidative stress parameters spectrophotometrically (UV/Vis spectrophotometer, Optizen 2120 UV, Mecasys Co., Ltd, Korea).
Behavioral assessment
The rats’ behavior in all tests was videotaped and analyzed using ANYmaze™ computer software (Stoelting Co., USA).
Forced swim test
The FST is a well-established behavioral paradigm used to test the efficacy of antidepressant drugs. In our study, the FST was conducted according to the method of Porsolt et al. (1977). The behavioral apparatus was a clear glass aquarium (height, 54.0 cm; length, 34.0 cm; width 60.0 cm) filled with water to a depth of 40.0 cm maintained at 24.0 ± 1 °C (Molina-Hernández et al. 2004). Rats were forced to swim for 15 min (pretest). Twenty-four hours later, they were reinforced to swim for a 5-min period (test) during which the time spent in immobility, swimming, or struggling was measured. The number of defecations as a sign of emotional reactivity was also registered. The rats were judged to be immobile whenever they remained passively floating in a slightly hunched but upright position with their heads being just above the water surface. The struggling behavior was registered when the animals made active and exaggerated movements with their forepaws in an attempt to escape the stressful situation. They were considered to be in a swimming position when they made active swimming or circular movements (Cryan et al. 2002). After each session, the rats were removed from the water, dried with towels, and placed in a warmed enclosure for 20 min before being returned to their home cages. The aquarium was emptied and cleaned with an alcoholic solution between rats.
Open field test
Spontaneous locomotor activity of rats was tested in an OF, which consisted of a gray square Plexiglas arena (70 cm × 70 cm × 40 cm) divided into a 35 × 35 cm central zone and the surrounding peripheral one. The room was illuminated by a red bulb (25 W) located 130 cm above the center of the apparatus (Sáenz et al. 2006). The rats were individually placed in the center of the arena and allowed to freely explore for 5 min. The following behavioral parameters were measured: the locomotive distance, the number of rearings, the time spent in central zone, and the time spent in peripheral zone. After each test, the animals were returned to their home cages, and the apparatus was cleaned with an alcoholic solution followed by wet and dry paper towels.
Elevated plus maze test
As previously described (Patin et al. 2005), the elevated plus maze consisted of four arms (50 cm × 10 cm) extending from a central platform (10 cm × 10 cm). Two opposing arms were closed-in by 45-cm high Plexiglas walls, while the other two arms were open with 3–5 mm high railing around the perimeter to prevent the rat from falling. The entire apparatus was elevated to 50 cm above the ground level. The test room was lit by a 60-W electric bulb placed directly 175 cm above the central area of the apparatus (Estanislau and Morato 2005). Rats were individually placed in the center of the maze facing an open arm, and their activity over the entire 5-min test period was evaluated. The following behavioral parameters were measured: the number of entries into and the time spent in open arms, and the number of entries into and the time spent in closed arms. After each test, the animals were returned to their home cages, and the apparatus was cleaned with an alcoholic solution followed by wet and dry paper towels.
Oxidative stress analyses
Glutathione-S-transferase assay
The glutathione-S-transferase activity was estimated at 37 °C according to the method of Habig et al. (1974). The reaction mixture (1 ml) contained 0.334 ml of 100 mM phosphate buffer (pH 6.5), 0.033 ml of 30 mM 1-chloro-2-4-di-nitrobenzene (CDNB), and 0.033 ml of reduced glutathione. After preincubating the mixture for 2 min, 0.01 ml of supernatant was added, and the absorbance was measured for three consecutive minutes at 340 nm. The activity of GST is expressed as nanomole per min per milligram of protein, using an extinction coefficient of 9.6/Mm/cm.
Reduced glutathione assay
Reduced glutathione (GSH) concentration was determined as described earlier by Ellman (1959). A 1.0 ml supernatant was precipitated with 1.0 ml of 4 % sulfosalicylic acid and cold digested at 4 °C for 1 h. The samples were centrifuged at 1,200 g for 15 min at 4 °C. To 1 ml of this supernatant, 2.7 ml of 0.1 M phosphate buffer (pH 8.0) and 0.2 ml of 5-5′-dithio-bis-2-nitrobenzoic acid (DTNB) were added. The yellow color developed was immediately read at 412 nm. The results were expressed as nanomole of GSH per milligram of protein.
Lipid peroxidation assay
The malondialdehyde (MDA) levels were assayed as a product of lipid peroxidation (Draper and Hadley 1990). Briefly, 2.5 ml of 10 % trichloroacetic acid (TCA) was added to 0.5 ml of samples in each centrifuge tube and boiled in a water bath for 15 min. After cooling, the tubes were centrifuged at 1,000 g for 10 min, and 2.0 ml of the supernatant was added to 1.0 ml of 0.67 % thiobarbituric acid (TBA) solution and then boiled in a water bath for 15 min. After cooling, the absorbance of the TBA-MDA reaction was measured at 532 nm. Results were expressed as nanomole MDA per milligram of protein, using an extinction coefficient of 1.56 × 105/cm/M.
Brain protein assay
The brain protein content was measured according to the method of Bradford (1976) using bovine serum albumin (BSA) as standard. The Bradford reagent was diluted in deionized water (1:4). Twenty microliters of the protein extract was mixed with 1 ml of the diluted reagent, and the blue color formed was spectrophotometrically measured at 595 nm. A standard curve was determined using a serial dilution series (0.1–1.0 mg/ml) of BSA dissolved in phosphate buffer (0.1 mol/l, pH 7.4).
Statistical analysis
Results are presented as the mean ± standard error of the mean (SEM). One-way analysis of variance (ANOVA) was used to compare key variable between groups, followed by the post-hoc Tukey–Kramer’s test when necessary. Additionally, an analysis of covariance (ANCOVA) was applied on FST, EPM, and OF measures to check for statistical relationships among the parameters of each behavioral test. Statistical significance was considered with a p < 0.05. All statistical analyses were performed using the Minitab software (version 15.1.1.0, Minitab Inc., USA).
Results
Body weight
One-way ANOVA registered significant differences among groups’ body weight change [F(3, 16) = 92.73, p < 0.001]. ADR-treated rats showed a significant decrease in body weight gain (p < 0.001) as compared to vehicle-treated ones. Moreover, treatment with quercetin in ADR-injected animals significantly alleviated body weight decrease (p < 0.001) when compared to that in ADR group (data not shown).
Depression-like behavior in the forced swim test
Animals’ behavior in the FST is presented in Fig. 2. One-way ANOVA indicated a significant difference among the groups in respect of immobility [F(3, 36) = 653.20; p < 0.001], swimming [F(3, 36) = 129.30, p < 0.001], struggling [F(3, 36) = 506.96, p < 0.001], and defecation [F(3, 36) = 21.23, p < 0.001]. When compared to C group, ADR injection significantly increased FST-related immobility (p < 0.001; Fig. 2a). Quercetin-injected rats exhibited a significant decrease in immobility time (p < 0.001) as compared to C rats and ADR-treated ones. Quercetin treatment in ADR-injected animals significantly reduced immobility time (p < 0.001) when compared to C and ADR groups. As shown in Fig. 2b, both ADR and quercetin treatments enhanced significantly the swimming time (p < 0.001) as compared to vehicle-treated rats, with further increase in quercetin-injected animals (p < 0.001) when compared to ADR-treated ones. Interestingly, the swimming time increased significantly in Q-injected rats pretreated with ADR (p < 0.001) when compared to that in vehicle- and ADR-injected ones, while decreased significantly (p < 0.01) as compared to Q group. ADR treatment significantly declined the struggling time (p < 0.001) when compared to C group (Fig. 2c). On the contrary, Q-injected rats spent longer time in struggling behavior as compared to vehicle- and ADR-injected ones. The struggling time in Q-injected rats pretreated with ADR decreased significantly (p < 0.001) as compared to that in C and Q groups, while enhanced significantly (p < 0.001) in comparison with ADR-injected animals. In addition, no significant difference was registered in respect to the number of fecal boli between ADR and C groups (Fig. 2d). Quercetin treatment alone suppressed FST-related defecation (p < 0.001) when compared to all other groups. An ANCOVA was applied to determine if the time spent immobile is influenced by the overall activity. When this activity (either the swimming time or the struggling time) was defined as a covariate, there was no change in significance (p ˂ 0.001) for the time of immobility, indicating that ADR-injected rats showed a depressive-like behavior.
Anxiety-like behavior in the open field test
Figure 3 shows the rats’ behavior in the OF. One-way ANOVA revealed significant differences among the groups in terms of the locomotive distance [F(3, 20) = 6.21, p < 0.01], the number of rearings [F(3, 20) = 6.96, p < 0.01], the central zone time [F(3, 20) = 36.46, p < 0.001], and the peripheral zone time [F(3, 20) = 36.54, p < 0.001]. Indeed, ADR-treated animals traveled lesser distance (p < 0.01; Fig. 3a) when compared to vehicle-treated ones. Quercetin administration in untreated and ADR-treated rats significantly enhanced the distance traveled in the apparatus (p < 0.001 and p < 0.05, respectively) as compared to that in ADR group. When compared to C animals, the number of rearings decreased significantly in ADR and ADR + Q groups (p < 0.001 and p < 0.001, respectively; Fig. 3b). Quercetin-injected rats showed greater number of rearings (p < 0.05) as compared to ADR-injected ones. ADR-treated rats spent shorter time in central area and longer time in peripheral one (p < 0.001; Fig. 3c, d) as compared to vehicle-treated animals. When compared to ADR group, Q-treated rats spent longer time in the central area and shorter time in the peripheral one (p < 0.001). Q-injected rats pretreated with ADR spent less time in the central zone and more time in the peripheral one as compared to C and Q groups (p < 0.01 and p < 0.05 respectively), while they spent longer time in the central area and shorter time in the peripheral one (p < 0.001) when compared to ADR-treated animals. An ANCOVA was performed to demonstrate that the behavioral responses of ADR-injected rats were due to the anxiety disorders rather than the fatigue. Taking the locomotive distance as a covariate, there was no change in significance (p < 0.001), indicating that the difference in the time spent in both central and peripheral zones among all the groups did not depend on the difference observed for the traveled distance.
Anxiety-like behavior in the elevated plus maze test
The rats’ behavior in the elevated plus maze is presented in Fig. 4. One-way ANOVA among all groups indicated a significant effect of treatment on the number of entries into [F(3, 20) = 12.02, p < 0.001] and the time spent in [F(3, 20) = 65.58, p < 0.001] the open arms, and the number of entries into [F(3, 20) = 18.54, p < 0.001] and the time spent in [F(3, 20) = 147.44, p < 0.001] the closed arms. Interestingly, ADR treatment decreased significantly the number of entries into and the time spent in the open arms (p < 0.001; Fig. 4a, b) as compared to C group. Q-treated rats exhibited lower number of entries into the open arms (p < 0.05) when compared to vehicle-treated ones, while they showed greater number of entries into (p < 0.05) and longer time spent in the open arms (p < 0.001) as compared to ADR-treated rats. When compared to C group, Q-injected rats pretreated with ADR showed lower number of entries into and less time spent in the open arms (p < 0.001). In addition, the time they spent in the open arms was longer than that registered in the ADR group (p < 0.001) and shorter than that noted in Q-treated animals (p < 0.001). On the other hand, ADR treatment significantly increased the number of entries into (p < 0.05) and the time spent in the closed arms (p < 0.001; Fig. 4c, d) when compared to controls. Q-injected rats showed lower number of entries into the closed arms as compared to C group. Moreover, they exhibited lower number of entries into and longer time spent in the closed arms (p < 0.001) when compared to ADR group. Q-injected animals pretreated with ADR indicated longer time spent in the closed arms (p < 0.001) as compared to controls. In addition, they showed lower number of entries into (p < 0.05) and longer time spent in the closed arms (p < 0.001) when compared to ADR-treated rats, with greater number of entries into and longer time spent in the closed arms (p < 0.001) when compared to Q-treated rats. An ANCOVA was applied to determine if the time spent in arms is influenced by the overall movement. When controlling for both open and closed arms entries, there was no change in significance (p ˂ 0.001) for the time spent in these arms.
Corticosterone changes
One-way ANOVA revealed a significant effect of treatment on corticosterone level between groups [F(3, 16) = 18.98, p < 0.001]. Plasma corticosterone concentration significantly increased post-ADR injection (p < 0.05; Fig. 5) as compared to C and Q groups. Quercetin treatment in ADR-pretreated rats resulted in a significant reduction of corticosterone level when compared to that in C, ADR (p < 0.001), and Q (p < 0.01) groups.
Brain oxidative biomarkers
One-way ANOVA revealed significant differences for the GST activity [F(3,16) = 109.50, p < 0.001], GSH level [F(3,16) = 14.90, p < 0.001], and lipid peroxidation [F(3,16) = 40.34, p < 0.001]. When compared to controls, ADR and ADR + Q groups exhibited a significant increase in the GST activity (p < 0.001; Fig. 6a). Quercetin administration in saline- or ADR-pretreated rats significantly reduced the GST activity (p < 0.001) as compared to ADR-treated ones. In addition, ADR + Q group showed a significant increase in GST activity (p < 0.001) when compared to Q-injected animals. On the other hand, GSH level was significantly depleted in ADR and ADR + Q (p < 0.001 and p < 0.05 respectively; Fig. 6b), as compared to that in vehicle-injected ones. Quercetin treatment significantly enhanced GSH content in Q and ADR + Q groups (p < 0.001 and p < 0.01, respectively) when compared to that in ADR-treated animals. Furthermore, ADR + Q showed a significant decrease in GSH level (p < 0.05) in comparison to Q-treated ones. A significant increase in lipid peroxidation was registered in ADR and ADR + Q groups (p < 0.001 and p < 0.01, respectively; Fig. 6c) as compared to saline-injected rats. Quercetin injection in Q and ADR + Q significantly reduced lipid peroxidation (p < 0.001 and p < 0.01, respectively) in comparison to that in ADR-treated ones. Lipid peroxidation was significantly enhanced in ADR + Q (p < 0.01) when compared to that in Q-injected ones.
Hematological changes
Total leukocyte counts and WBC relative counts (%) are presented in Table 1. One-way ANOVA revealed significant differences between groups in respect of total leukocytes [F(3, 16) = 6.02, p < 0.01], number and percentage of lymphocytes [F(3, 16) = 43.07; F(3, 16) = 53.52, p < 0.001] and monocytes [F(3, 16) = 9.92; F(3, 16) = 33.03, p < 0.001], and only the percentage of granulocytes [F(3, 16) = 11.22, p < 0.001]. ADR injection significantly decreased the WBC count (p < 0.01) as compared to vehicle-treated animals. Q and ADR + Q groups showed an increase in the total number of leukocytes (p < 0.05) when compared to ADR-treated rats. Furthermore, a significant lymphopenia was registered in the ADR and ADR + Q groups (p < 0.001) as compared to that in the controls. When compared to the ADR-treated rats, a significant increase in lymphocyte number (p < 0.001) and percentage (p < 0.001 and p < 0.05, respectively) was noticed in the Q and ADR + Q groups. On the other hand, the mean monocyte levels (p < 0.01) and the percentage of monocytes in leukocytes increased significantly in the ADR and ADR + Q groups (p < 0.001) as compared to those in the controls. When compared to ADR group, Q-injected animals showed lower monocyte values (p < 0.01) and relative count of monocytes in leukocytes (p < 0.001). The ADR + Q exhibited a significant decline in the percentage of monocytes (p < 0.05) as compared to the ADR-treated rats, while they had higher monocyte levels (p < 0.01) and relative monocyte counts (p < 0.001) when compared to the Q group. Moreover, the granulocyte relative counts were significantly enhanced in the ADR and ADR + Q (p < 0.001 and p < 0.01, respectively) as compared to those in the vehicle-injected group. The Q rats exhibited lower percentage of granulocytes (p < 0.01) as compared to the ADR-treated group. Furthermore, the Q-injected rats pretreated with ADR had higher granulocyte values and granulocyte relative counts (p < 0.05) when compared to the Q-treated rats.
Discussion
In the present study, we investigated the ability of quercetin to reverse the effects of a single i.p. injection of ADR (7 mg/kg) on neurobehavioral and immune aspects in male rats. The behavioral part of our experiments indicated that ADR treatment enhanced immobility and swimming with the struggling time being decreased, revealing that ADR administration could be associated with a mild depressive-like behavior. Quercetin treatment following ADR injection reduced the immobility time in the FST, suggesting that it produces a powerful antidepressant-like effect in rats. Interestingly, quercetin per se decreased the emotional reactivity in response to stress conditions, as indicated by the suppression of defecation during the test. Quercetin administered per os (10, 20, or 40 mg/kg) dose dependently reduced the immobility time in mice which were submitted to FST 60 min later (Bhutada et al. 2010). Moreover, quercetin (50 and 100 mg/kg, i.p.) dose dependently reduced the immobility during the FST in diabetic mice (Anjaneyulu et al. 2003). Rojas et al. (2011) have also reported that Ginkgo biloba extract (EGb761; 10 mg/kg, i.p.), a quercetin-enriched medicinal plant, manifests an antidepressant-like effect in the FST when administered for 17 consecutive days in mice.
In the OF test, ADR-treated animals traveled lesser distance and showed a reduced number of rearings in the apparatus, suggesting that ADR affects the locomotor and exploratory activities and thereby promotes the sickness behavior (Konat et al. 2008; Liedke et al. 2009). This hypolocomotion was accompanied with a shorter time in the central area and a longer time in the peripheral one, meaning that these animals tend to remain close to the apparatus walls. This finding is considered as an index of thigmotaxis (Simon et al. 1994). Meanwhile, the EPM test indicated that ADR treatment reduced the number of entries into and the time spent in the open arms, while enhanced the number of entries into and the time spent in the closed arms. These later results suggest that ADR-treated rats had an anxiety-like behavior. Indeed, we have recently reported that a single i.p. injection of ADR at 7 mg/kg reduced the locomotive activity and enhanced the anxiety in the OF and EPM tests 72 h post-treatment (Merzoug et al. 2011). It was also reported that prenatal exposure to ADR dose dependently increased anxiety and affected the emotional behavior in 3-month-old C57BL/6 J-mice (Van Calsteren et al. 2009). Our findings demonstrate that quercetin attenuates the ADR-related anxiety-like behavior and locomotor impairment in both OF and EPM tasks, except for the vertical exploration (i.e., the number of rearings). This anxiolytic effect has been found in rats at a dose of 300 mg/kg after oral or intranasal administration (Priprem et al. 2008). Quercetin has also been shown to ameliorate the time spent in and the number of entries into the open arms of EPM after a sub-chronic treatment in male rats (Wattanathorn et al. 2007). Using an animal model of aging, Sun et al. (2007) indicated that the long-term intake of quercetin attenuates the ambulatory impairment. Specifically, our findings suggest that the behavioral impairment following ADR treatment could be conferred to the significant increase in corticosterone levels, suggesting further that ADR is a chemical stress that activates the HPA axis. Then, the alleviating effect of quercetin may be related to its ability to restore the corticosterone level in ADR-exposed animals. It has been noted that quercetin supplementation attenuated the stress-induced behavioral depression by inhibiting the corticotrophin-releasing factor (CRF) mRNA expression in the hypothalamus (Kawabata et al. 2010). More recently, a sub-acute oral treatment with quercetin (50 mg/kg for 6 days) was found to be anxiolytic in predator-stressed pregnant rats when tested in the EPM and OF paradigms, an effect that was partially attributed to the blockade of corticosterone hypersecretion (Toumi et al. 2013).
The anxio-depressive-like behavior in ADR-injected rats was associated with a pronounced brain oxidative stress. Indeed, ADR exposure enhanced the GST activity and lipid peroxidation (i.e., increased MDA level) while depleted the GSH level. MDA is the most commonly studied product of lipid peroxidation for quantifying the level of oxidative stress in vivo and in vitro (Del Rio et al. 2005). It has been reported that lipid peroxidation exerts cytotoxic effects on a wide range of organs including the brain, contributing therefore to cognitive disorders and neurodegenerative diseases (Sultana et al. 2006). The reduction in GSH level may be involved in neuronal death (Bains and Shaw 1997) and neurobehavioral and cognitive deficits in rats (Cruz-Aguado et al. 2001). In addition, the elevation of GST activity following ADR injection could be related to its protective role against oxidative injury in the brain. Interestingly, it was noted that GST can detoxify toxins and transport them away from axons and myelin sheaths (Sagara and Sugita 2001). Our findings corroborate the prior investigations indicating that ADR exposure generates lipid peroxides and alters the activity of antioxidant enzymes in cerebral tissues (Joshi et al. 2005, 2007, 2010). Quercetin is a well-known antioxidant flavonoid that protects brain cells against ROS-induced damage. Our data show that quercetin improved the brain oxidative status in ADR-treated rats. This effect of quercetin could be associated with its ability to stabilize high levels of GSH while scavenging lipid peroxides within the brain tissue (Sun et al. 2007). A neuroprotective activity of quercetin through ROS elimination has also been reported in isolated rat cortical cells that were exposed to H2O2 (Dok-Go et al. 2003). In addition, quercetin alleviated d-galactose-induced neuron damage in mice by scavenging oxygen radicals and increasing the activity of antioxidant enzymes such as superoxide dismutase (Lu et al. 2006). Interestingly, the antioxidant effect of quercetin in our study might in part be responsible for the behavioral improvement in OF and EPM tests. In fact, Singh et al. (2003) reported that a chronic treatment of mice with this flavonoid reverses their cognitive deficits due to ethanol intoxication and aging by ameliorating the forebrain level of GSH and activity of superoxide dismutase and catalase.
ADR treatment has been previously considered as immunosuppressive and myelosuppressive (Grant et al. 1991). In the current study, ADR injection reduced total WBC and the number and the percentage of lymphocytes, while it enhanced the number and the percentage of monocytes and only the percentage of granulocytes. We have previously demonstrated that the acute ADR treatment at the same dose is associated with immune alterations in rats (Merzoug et al. 2011). It has been noticed that ADR dose dependently depleted leukocytes and lymphocyte numbers in the spleen, thymus, lymph nodes, and peripheral blood of healthy mice (Pourtier-Manzanedo et al. 1995). Interestingly, ADR-associated lymphopenia might be due to the elimination of lymphocyte precursors and the destruction of mature lymphocyte populations leading to immunodeficiency (Steele 2002). Moreover, Asmis et al. (2006) have revealed that intravenous injections of ADR in female mice increased blood monocytes. ADR-induced monocytosis may contribute to T cell immunosuppression by the production of suppressive factors that inhibit T cell function (Mackall 2000). On the other hand, ADR has been indicated to cause pronounced marrow depression with peripheral blood granulocytopenia (Falkson et al. 1985), which may result in increased susceptibility to infections (Tsang et al. 2007). The IS has been reported to be involved in neurodegenerative conditions that accompany CNS injuries (Weiner and Cohen 2002). Recent investigations have revealed that an injection of T cells from wild-type donors into immune-depleted mice restored their cognitive functions (Kipnis et al. 2008), supporting the hypothesis that neurobehavioral diseases could be related to chemotherapy-mediated immunodeficiency (Ahles and Saykin 2007; Kipnis et al. 2008). The high level of corticosterone is likely to play a role in the obtained immune disturbance in ADR-injected rats, as corticosterone is thought to inhibit the cell-mediated immunity (CMI) and modulate monocyte and granulocyte counts (Song et al. 1994; Woiciechowsky et al. 1999). Quercetin treatment reversed leucopenia and slightly attenuated lymphopenia and monocytosis in ADR-exposed rats, while no effect was noted in respect of granulocytosis. The hematologic benefits of quercetin could be related to its potent ability to stabilize cell membranes by reducing lipid peroxidation (Chaudhuri et al. 2007) and DNA oxidative damage in human lymphocytes (Sato et al. 1997). Furthermore, quercetin has been indicated to enhance WBCs in X ray-exposed mice and human lymphocytes after radiotherapy (Fahlman and Krol 2009). The immune-stimulating effect of quercetin might also be due to its blockade of ADR-mediated HPA axis hyperactivation, a possible mechanism that was recently highlighted (Toumi et al. 2013).
In conclusion, we have demonstrated that quercetin administration attenuates ADR-associated behavioral disorders, corticosterone increase, brain oxidative injury, and immune cell count alteration in male Wistar rats. Further experimental studies are needed to clarify the potential effect of quercetin on chemotherapy-mediated cognitive and physiological impairments.
Abbreviations
- ADR:
-
Adriamycin
- EPM:
-
Elevated plus maze
- FST:
-
Forced swim test
- OF:
-
Open field
- Q:
-
Quercetin
References
Ahles TA, Saykin AJ (2007) Candidate mechanisms for chemotherapy-induced cognitive changes. Nat Rev Cancer 7:192–201, PMID: 17318212
Akbay P, Basaran AA, Undeger U, Basaran N (2003) In vitro immunomodulatory activity of flavonoid glycosides from Urtica dioica L. Phytother Res 17:34–37, PMID: 12557244
Anjaneyulu M, Chopra K, Kaur I (2003) Antidepressant activity of quercetin, a bioflavonoid, in streptozotocin-induced diabetic mice. J Med Food 6(4):391–395, PMID: 14977450
Asmis R, Qiao M, Rossi RR, Cholewa J, Xu L, Asmis LM (2006) Adriamycin promotes macrophage dysfunction in mice. Free Radic Bio Med 41:165–174, PMID: 16781464
Bains JS, Shaw CA (1997) Neurodegenerative disorders in humans: the role of glutathione in oxidative stress-mediated neuronal death. Brain Res Rev 25:335–358, PMID: 9495562
Banks WA, Erickson MA (2010) The blood-brain barrier and immune function and dysfunction. Neurobiol Dis 37:26–32, PMID: 19664708
Berton O, Nestler EJ (2006) New approaches to antidepressant drug discovery: beyond monoamines. Nat Rev Neurosci 7:137–151, PMID: 16429123
Bhutada P, Mundhada Y, Bansod K, Ubgade A, Quazi M, Umathe S, Mundhada D (2010) Reversal by quercetin of corticotrophin releasing factor induced anxiety- and depression-like effect in mice. Prog Neuropsychopharmacol Biol Psychiatry 34(6):955–960, PMID: 20447436
Bradford MM (1976) A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem 72:248–254, PMID: 942051
Chaudhuri S, Banerjee A, Basu K, Sengupta B, Sengupta PK (2007) Interaction of flavonoids with red blood cell membrane lipids and proteins: antioxidant and antihemolytic effects. Int J Biol Macromol 41:42–48, PMID: 17239435
Cherng JM, Chiang W, Chiang LC (2008) Immunomodulatory activities of common vegetables and spices of Umbelliferae and its related coumarins and flavonoids. Food Chem 106:944–950. doi:10.1016/j.foodchem.2007.07.005
Cho JY, Kim IS, Jang YH, Kim AR, Lee SY (2006) Protective effect of quercetin, a natural flavonoid against neuronal damage after transient global cerebral ischemia. Neurosci Lett 404:330–335. doi:10.1016/j.neulet.2006.06.010
Cho SY, Park SJ, Kwon MJ, Jeong TS, Bok SH, Choi WY, Jeong WI, Ryu SY, Do SH, Lee CS, Song JC, Jeong KS (2003) Quercetin suppresses proinflammatory cytokines production through MAP kinases and NF-κB pathway in lipopolysaccharide-stimulated macrophage. Mol Cell Biochem 243:153–160, PMID:12619901
Choi GN, Kima JH, Kwak JH, Jeong CH, Jeong HR, Lee U, Heo HJ (2012) Effect of quercetin on learning and memory performance in ICR mice under neurotoxic trimethyltin exposure. Food Chem 132:1019–1024. doi:10.1016/j.foodchem.2011.11.089
Cruz-Aguado R, Almaguer-Melian W, Díaz CM, Lorigados L, Bergado J (2001) Behavioral and biochemical effects of glutathione depletion in the rat brain. Brain Res Bull 55(3):327–333, PMID:11489339
Cryan JF, Markou A, Lucki I (2002) Assessing antidepressant activity in rodents: recent developments and future needs. Trends Pharmacol Sci 23:238–345, PMID:12008002
Cutts SM, Swift LP, Rephaeli A, Nudelman A, Phillips DR (2003) Sequence specificity of adriamycin-DNA adducts in human tumor cells. Mol Cancer Ther 2:661–670, PMID:12883039
Del Rio D, Stewart AJ, Pellegrini N (2005) A review of recent studies on malondialdehyde as toxic molecule and biological marker of oxidative stress. Nutr Metab Cardiovasc Dis 15:316–328, PMID:16054557
Dok-Go H, Lee KH, Kim HJ, Lee EH, Lee J, Song YS (2003) Neuroprotective effects of antioxidative flavonoids, quercetin, (+)-dihydroquercetin and quercetin 3-methyl ether, isolated from Opuntia ficus-indica var. saboten. Brain Res 965:130–136, PMID:12591129
Draper HH, Hadley M (1990) Malondialdehyde determination as index of lipid peroxidation. Meth Enzymol 186:421–431, PMID:2233309
Dubovický M (2010) Neurobehavioral manifestations of developmental impairment of the brain. Interdiscip Toxicol 3(2):59–67, PMID:21217874
Ellman GL (1959) Tissue sulfhydryl groups. Arch Biochem Biophys 82(486):70–77, PMID:13650640
Estanislau C, Morato S (2005) Prenatal stress produces more behavioral alterations than maternal separation in the elevated plus-maze and in the elevated T-maze. Behav Brain Res 163:70–77, PMID:15941599
Fahlman BM, Krol ES (2009) UVA and UVB radiation-induced oxidation products of quercetin. Photochem Photobiol B 97:123–131, PMID:19782575
Falkson G, Klein B, Falkson H (1985) Hematological toxicity: experience with anthracyclines and anthracenes. Exp Hematol 13(Suppl 16):64–71, PMID:3857185
Filho AW, Filho VC, Olinger L, de Souza MM (2008) Quercetin: further investigation of its antinociceptive properties and mechanisms of action. Arch Pharm Res 31(6):713–721. doi:10.1007/s12272-001-1217-2
Grant LD, Kaesberg PR, Ershler WB (1991) Immunologic effects of cancer chemotherapy. In: Powis G, Hacker MP (eds) The toxicity of anticancer drugs. Pergamon Press, New York, pp 167–197
Gugler R, Loschik M, Dengler MJ (1975) Disposition of quercetin in man after single oral and intravenous doses. Eur J Clin Pharmacol 9:229–235, PMID: 1233267
Habig WH, Pabst MJ, Jakoby WB (1974) Glutathione S-transferase, the first enzymatic step in mercapturic acid formation. J Biol Chem 249:7130–7139, PMID:4436300
Haleagrahara N, Radhakrishnan A, Lee N, Kumar P (2009) Flavonoid quercetin protects against swimming stress-induced changes in oxidative biomarkers in the hypothalamus of rats. Eur J Pharmacol 621:46–52, PMID:19744476
Haleagrahara N, Siew CJ, Mitra NK, Kumari M (2011) Neuroprotective effect of bioflavonoid quercetin in 6-hydroxydopamine-induced oxidative stress biomarkers in the rat striatum. Neurosci Lett 500:139–143, PMID:21704673
Heim C, Newport DJ, Heit S, Graham YP, Wilcox M, Bonsall R, Miller AH, Nemeroff CB (2000) Pituitary-adrenal and autonomic responses to stress in women after sexual and physical abuse in childhood. J Am Med Assoc 284:592–597, PMID:10918705
Heo HJ, Lee CY (2004) Protective effects of quercetin and vitamin C against oxidative stress-induced neurodegeneration. J Agric Food Chem 52(25):7514–7517, PMID:15675797
Hollman PC, Kata MB (1999) Dietary flavonoids: intake, health effects and bioavailability. Food Chem Toxicol 37(9–10):937–942, PMID:10541448
Jansen CE, Dodd MJ, Miaskowski CA, Dowling GA, Kramer J (2008) Preliminary results of a longitudinal study of changes in cognitive function in breast cancer patients undergoing chemotherapy with doxorubicin and cyclophosphamide. Psycho-Oncol 17:1189–1195, PMID:18506671
Joshi G, Aluise CD, Cole MP, Sultana R, Pierce WM, Vore M, St Clair DK (2010) Butterfield DA (2010) Alterations in brain antioxidant enzymes and redox proteomic identification of oxidized brain proteins induced by the anti-cancer drug adriamycin: implications for oxidative stress-mediated chemobrain. Neuroscience 166(3):796–807, PMID:20096337
Joshi G, Hardas S, Sultana R, St Clair DK, Vore M, Butterfield DA (2007) Glutathione elevation by gamma-glutamyl cysteine ethyl ester as a potential therapeutic strategy for preventing oxidative stress in brain mediated by in vivo administration of adriamycin: implication for chemobrain. J Neurosci Res 85:497–503, PMID:17171703
Joshi G, Sultana R, Tangpong J, Cole MP, St Clair DK, Vore M, Estus S, Butterfield DA (2005) Free radical mediated oxidative stress and toxic side effects in brain induced by the anti cancer drug adriamycin: insight into chemobrain. Free Radic Res 39:1147–1154, PMID:16298740
Kawabata K, Kawai Y, Terao J (2010) Suppressive effect of quercetin on acute stress-induced hypothalamic–pituitary–adrenal axis response in Wistar rats. J Nutr Biochem 21:374–380, PMID:19423323
Kipnis J, Derecki NC, Yang C, Scrable H (2008) Immunity and cognition: what do age-related dementia, HIV-dementia and ‘chemo-brain’ have in common? Trends Immunol 29(10):455–463, PMID:18789764
Konat GW, Kraszpulski M, James I, Zhang HT, Abraham J (2008) Cognitive dysfunction induced by chronic administration of common cancer chemotherapeutics in rats. Metab Brain Dis 23:325–333, PMID:18690526
Liedke PE, Reolon GK, Kilpp B, Brunetto AL, Roesler R, Schwartsmann G (2009) Systemic administration of doxorubicin impairs aversively motivated memory in rats. Pharmacol Biochem Behav 94(2):239–243, PMID:19747935
Lu J, Zheng YL, Luo L, Wu DM, Sun DX, Feng YJ (2006) Quercetin reverses D-galactose induced neurotoxicity in mouse brain. Behav Brain Res 171:251–260, PMID:16707173
Mackall CL (2000) T-cell immunodeficiency following cytotoxic antineoplastic therapy: a review. Stem Cells 18:10–18, PMID:10661568
Manach C, Scalbert A, Morand C, Rémésy C, Jiménez L (2004) Polyphenols: food sources and bioavailability. Am J Clin Nutr 79:727–747, PMID: 15113710
Merzoug S, Toumi ML, Boukhris N, Baudin B, Tahraoui A (2011) Adriamycin-related anxiety-like behavior, brain oxidative stress and myelotoxicity in male Wistar rats. Pharmacol Biochem Behav 99:639–647, PMID:21703296
Min YD, Choi CH, Bark H, Son HY, Park HH, Lee S, Park JW, Park EK, Shin HI, Kim SH (2007) Quercetin inhibits expression of inflammatory cytokines through attenuation of NF-κB and p38 MAPK in HMC-1 human mast cell line. Inflamm Res 56:210–215, PMID:17588137
Molina-Hernández M, Tellez-Alcántara NP, Garcí JP, Lopez JIO, Jaramillo MT (2004) Synergistic interaction between ketoconazole and several antidepressant drugs with allopregnanolone treatments in ovariectomized Wistar rats forced to swim. Prog Neuropsychopharmacol Biol Psychiatry 28(8):1337–1345, PMID:15588761
Navarra P, Preziosi P (1997) Disruptions of the hypothalamo-pituitary-adrenal axis increase anticancer drug lethality in the rat. Toxicol Lett 91:219–227, PMID:9217242
Oršolić N, Bašić I (2005) Water-soluble derivative of propolis and its polyphenolic compounds enhance tumoricidal activity of macrophages. J Ethnopharmacol 102:37–45, PMID:16054317
Park JY, Jang MJ, Chung YH, Kim KY, Kim SS, Lee WB, You S, Choi YS, Hur DY, Kim D (2009) Doxorubicin enhances CD4+ T-cell immune responses by inducing expression of CD40 ligand and 4-1BB. Int Immunopharmacol 9:1530–1539, PMID:19778641
Patin V, Lordi B, Vincent A, Caston J (2005) Effects of prenatal stress on anxiety and social interactions in adult rats. Dev Brain Res 160:265–274, PMID:16290208
Paulke A, Schubert-Zsilavecz M, Wurglics M (2006) Determination of St. John’s wort flavonoid-metabolites in rat brain through high performance liquid chromatography coupled with fluorescence detection. J Chromatogr B Anal Technol Biomed Life Sci 832:109–113, PMID:16434241
Porsolt RD, Le Pichon M, Jalfre M (1977) Depression: a new animal model sensitive to antidepressant treatments. Nature 266:730–732, PMID:559941
Pourtier-Manzanedo A, Didier A, Froidevaux S, Loor F (1995) Lymphotoxicity and myelotoxicity of doxorubicin and SDZ PSC 833 combined chemotherapies for normal mice. Toxicology 99:207–217, PMID:7610467
Priprem A, Watanatorn J, Sutthiparinyanont S, Phachonpai W, Muchimapura S (2008) Anxiety and cognitive effects of quercetin liposomes in rats. Nanomedicine 4:70–78, PMID:18249157
Pu F, Mishima K, Irie K, Motohashi K, Tanaka Y, Orito K, Egawa T, Kitamura Y, Egashira N, Iwasaki K, Fujiwara M (2007) Neuroprotective effects of quercetin and rutin on spatial memory impairment in an 8-arm radial maze task and neuronal death induced by repeated cerebral ischemia in rats. J Pharmacol Sci 104:329–334, PMID:17666865
Rojas P, Serrano-García N, Medina-Campos ON, Pedraza-Chaverri J, Ögren SO, Rojas C (2011) Antidepressant-like effect of a Ginkgo biloba extract (EGb761) in the mouse forced swimming test: role of oxidative stress. Neurochem Int 59:628–636, PMID:21672588
Russo M, Spagnuolo C, Tedesco I, Bilotto S, Russo GL (2012) The flavonoid quercetin in disease prevention and therapy: facts and fancies. Biochem Pharmacol 83:6–15. doi:10.1016/j.bcp.2011.08.010
Sáenz JCB, Villagra OR, Trías JF (2006) Factor analysis of forced swimming test, sucrose preference test and open field test on enriched, social and isolated reared rats. Behav Brain Res 169:57–65, PMID:16414129
Sagara J, Sugita Y (2001) Characterization of cytosolic glutathione S-transferase in cultured astrocytes. Brain Res 902:190–197, PMID:11384612
Sakakibara H, Yoshino S, Kawai Y, Terao J (2008) Antidepressant-like effect of onion (Allium cepa L.) powder in a rat behavioral model of depression. Biosci Biotechnol Biochem 72:94–100, PMID:18175926
Sato M, Miyazaki T, Kambe F, Maeda K, Seo H (1997) Quercetin, a bioflavonoid, inhibits the induction of interleukin 8 and monocyte chemoattractant protein-1 expression by tumor necrosis factor-α in cultured human synovial cells. J Rheumatol 24:1680–1684, PMID:9292787
Simon P, Dupuis R, Costentin J (1994) Thigmotaxis as an index of anxiety in mice. Influence of dopaminergic transmissions. Behav Brain Res 61(1):59–64, PMID:7913324
Singh A, Naidu PS, Kulkarni SK (2003) Reversal of aging and chronic ethanol-induced cognitive dysfunction by quercetin a bioflavonoid. Free Radic Res 37(11):1245–1252, PMID:14703737
Song C, Kelly JP, Leonard BE (1994) The effect of stressful behavioral exposure on endocrine and immune parameters in the rat. Stress Med 10:239–245. doi:10.1002/smi.2460100406
Song J, Kwon O, Chen S, Daruwala R, Eck P, Park JB, Levine M (2002) Flavonoid inhibition of sodium-dependent vitamin C transporter 1 (SVCT1) and glucose transporter isoform 2 (GLUT2), intestinal transporters for vitamin C and glucose. J Biol Chem 277(18):15252–15260. doi:10.1074/jbc.M110496200
Spencer JP (2007) The interactions of flavonoids within neuronal signalling pathways. Genes Nutr 2:257–273, PMID:18850181
Steele TA (2002) Chemotherapy-induced immunosuppression and reconstitution of immune function. Leuk Res 26:411–414, PMID:11839388
Sultana R, Perluigi M, Butterfield DA (2006) Protein oxidation and lipid peroxidation in brain of subjects with Alzheimer’s disease: insights into mechanism of neurodegeneration from redox proteomics. Antioxid Redox Signal 8:2021–2037, PMID:17034347
Sun SW, Yu HQ, Zhang H, Zheng YL, Wang JJ, Luo L (2007) Quercetin attenuates spontaneous behavior and spatial memory impairment in D-galactose-treated mice by increasing brain antioxidant capacity. Nutr Res 27:169–175. doi:10.1016/j.nutres.2007.01.010
Tangpong J, Cole MP, Sultana R, Estus S, Vore M, St Clair W, Ratanachaiyavong S, St Clair DK, Butterfield DA (2007) Adriamycin-mediated nitration of manganese superoxide dismutase in the central nervous system: insight into the mechanism of chemobrain. J Neurochem 100:191–201, PMID:17227439
Tangpong J, Cole MP, Sultana R, Joshi G, Estus S, Vore M, St Clair W, Ratanachaiyavong S, St Clair DK, Butterfield DA (2006) Adriamycin-induced TNF-α-mediated central nervous system toxicity. Neurobiol Dis 23:127–139, PMID:16697651
Toumi ML, Merzoug S, Baudin B, Tahraoui A (2013) Quercetin alleviates predator stress-induced anxiety-like and brain oxidative signs in pregnant rats and immune count disturbance in their offspring. Pharmacol Biochem Behav 107:1–10, PMID:23541492
Tsang YW, Chi KH, Hu CJ, Tseng CL, Tseng FW, Wang YS (2007) Chemotherapy-induced immunosuppression is restored by a fermented soybean extract: a proof of concept clinical trial. Nutr Res 27:679–684. doi:10.1016/j.nutres.2007.09.001
Van Calsteren K, Hartmann D, Van Aerschot L, Verbesselt R, Van Bree R, D’Hooge R, Amant F (2009) Vinblastine and doxorubicin administration to pregnant mice affects brain development and behaviour in the offspring. Neurotoxicology 30:647–657, PMID:19422850
van der Woude H, Boersma MG, Vervoort J, Rietjens IM (2004) Identification of 14 quercetin phase II mono- and mixed conjugates and their formation by rat and human phase II in vitro model systems. Chem Res Toxicol 17(11):1520–1530, PMID:15540950
Wattanathorn J, Phachonpai W, Priprem A, Suthiparinyanont S (2007) Intranasal administration of quercetin liposome decreases anxiety-like behavior and increases spatial memory. Am J Agric Biol Sci 2(1):31–35. doi:10.3844/ajabssp.2007.31.35
Weiner HL, Cohen JA (2002) Treatment of multiple sclerosis with cyclophosphamide: critical review of clinical and immunologic effects. Mult Scler 8:142–154, PMID:11990872
Woiciechowsky C, Schoning B, Lanksch WR, Volk HD, Docke WD (1999) Catecholamine-induced interleukin-10 release: a key mechanism in systemic immunodepression after brain injury. Crit Care 3:R107–R111. doi:10.1186/cc375
Youdim KA, Shukitt-Hale B, Joseph JA (2004) Flavonoids and the brain: interactions at the blood-brain barrier and their physiological effects on the central nervous system. Free Radic Biol Med 37:1683–1693, PMID:15528027
Yu CS, Lai KC, Yang JS, Chiang JH, Lu CC, Wu CL, Lin JP, Liao CL, Tang NY, Wood WG, Chung JG (2010) Quercetin inhibited murine leukemia WEHI-3 cells in vivo and promoted immune response. Phytother Res 24:163–168, PMID:19449452
Acknowledgments
We wish to acknowledge Mr. Mounir Merzoug and Prof. Mohamed Benslama for their experimental and technical support. We are grateful to Prof. Abdellatif Boutefnouchet, Prof. Mohamed Laid Ouakid, and Prof. Abdelmadjid Bairi for their encouragement.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Merzoug, S., Toumi, M.L. & Tahraoui, A. Quercetin mitigates Adriamycin-induced anxiety- and depression-like behaviors, immune dysfunction, and brain oxidative stress in rats. Naunyn-Schmiedeberg's Arch Pharmacol 387, 921–933 (2014). https://doi.org/10.1007/s00210-014-1008-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-014-1008-y