Abstract
Vascular smooth muscle cells (VSMC) are present in arterial intima before atherosclerotic plaques develop and are likely to be exposed to unmodified serum lipids as they enter the vessel wall. We examined the effects of sera from mice on the morphology and function of mouse VSMC. Incubation of a mouse VSMC line (MOVAS) with sera from normocholesterolemic (C57BL/6J) or hypercholesterolemic (APOE−/−) mice caused concentration-dependent increases in lipid accumulation as measured by AdipoRed, with the extent of lipid uptake significantly greater with the latter sera type. Inhibition of c-Jun N-terminal kinases (SP600125), Src kinases (AG1879), and clathrin-dependent endocytosis (monodansylcadaverine) to disrupt scavenger receptor-mediated uptake of lipids had no effect on serum-induced lipid accumulation by VSMC. By contrast, inhibition of macropinocytosis with antagonists of PI-3 kinase (LY294002) and actin (cytochalasin D) markedly reduced lipid accumulation. Serum exposure reduced the expression of the ATP-binding cassette transporter A1, consistent with impaired cholesterol efflux, but had no effect on the expression of markers of VSMC differentiation. Moreover, the expression of several inflammation and foam cell markers was unchanged (CCL2, CCL5, and CD68) by mouse sera. The accumulation of unmodified serum lipids by VSMC involves a macropinocytosis-like uptake pathway and is associated with the downregulation of the ATP-binding cassette transporter. We speculate that VSMC may play an atheroprotective role in arterial intima by acting as a “sink” for unmodified lipids.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The “response to retention” hypothesis posits that the accumulation of unmodified serum lipoproteins in the subendothelial intima is an initiating event in atherosclerotic plaque formation (Williams and Tabas 1995; Tabas et al. 2007). The lipoproteins are then thought to associate with extracellular matrix (ECM) proteoglycans via ionic interactions, causing them to be retained within the intima and also making them more susceptible to oxidation or enzymatic modification (Camejo et al. 1998; Chait and Wight 2000). Such modifications convert lipoproteins from relatively innocuous species into those that promote endothelial activation and chemoattraction of inflammatory cells such as macrophages and T cells (Tabas et al. 2007). Oxidized lipoproteins are also high-affinity ligands for macrophage scavenger receptors, such as CD36, type I (SR-A1) and type II (SR-A2) class A scavenger receptors, and lectin-like oxidized low-density lipoprotein (LDL) receptor-1 (LOX-1), and are thus avidly taken up by these cells (Webb and Moore 2007). Excessive uptake of lipids by macrophages causes their transformation into foam cells, the major constituents of fatty streaks (Webb and Moore 2007). Furthermore, owing to their pro-inflammatory properties and propensity to undergo apoptosis, foam cells contribute to the ongoing development of more complex atherosclerotic lesions and their ultimate rupture (Bobryshev 2006).
Although the majority of foam cells within atherosclerotic plaques are derived from macrophages, immunohistochemical studies on lesions from humans and nonhuman primates indicate that at least some of the lipid-laden cells are vascular smooth muscle cells (VSMC) (Takebayashi et al. 1972; Goldfischer et al. 1975; Stary et al. 1994). VSMC express several cholesterol uptake receptors, including the LDL receptor, CD36, SR-A1, SR-A2, and CXCL16/SR-PSOX (Matsumoto et al. 2000; Wagsater et al. 2004; Lim et al. 2006; Ruan et al. 2006). Moreover, exposure of VSMC to inflammatory cytokines, such as interleukin-1β (IL-1β), tumor necrosis factor-α (TNF-α), and interferon-γ, causes upregulation of these receptors and increased uptake of LDL that has been modified by acetylation, oxidation, or enzymatically (Li et al. 1995; Wagsater et al. 2004; Ruan et al. 2006). This causes VSMC to assume a foam cell-like morphology characterized by the presence of lipid-filled vacuoles, downregulation of VSMC differentiation markers, upregulation of macrophage markers, and increased production of pro-inflammatory cytokines (Rong et al. 2003; Barlic et al. 2007; Sima et al. 2010; Sun and Chen 2010).
Diffuse intimal thickening (DIT) is evident in human arteries before the appearance of atherosclerotic plaques (Stary et al. 1992; Nakashima et al. 2002). VSMC are the major cellular constituents of DIT (Stary et al. 1992; Nakashima et al. 2002) and are, thus, likely to be exposed to serum lipoproteins that enter the vessel wall before they undergo modification. However, to our knowledge, no studies have examined the impact of exposure of VSMC to unmodified serum lipoproteins. Hence, we examined the effect of exposure of mouse VSMC to unmodified lipoproteins present in mouse serum in the belief that these studies may provide insights into the events that lead to the initiation of plaque formation. We demonstrate that VSMC in culture have a high capacity to take up and store the lipids that are present in sera from both normocholesterolemic (C57BL/6J) and hypercholesterolemic (apolipoprotein E-deficient [APOE−/−]) mice. However, unlike previous studies in which the uptake of modified LDL was shown to be dependent on the activity of scavenger receptors and to cause induction of a pro-inflammatory, macrophage-like phenotype, we show that the accumulation of unmodified serum lipids is the result of a macropinocytosis-like uptake pathway and is associated with the downregulation of the cholesterol efflux transporter, ATP-binding cassette transporter A1 (ABCA1). Importantly, the accumulation of serum lipids was not associated with a loss of VSMC differentiation markers or increased expression of pro-inflammatory cytokines. Based on these observations, we propose that the VSMC may act as a sink for unmodified serum lipoproteins. We further speculate that this action of VSMC within DIT and early atherosclerotic lesions may serve an atheroprotective function by preventing the interaction of lipoproteins with ECM proteoglycans and thereby limiting their oxidation.
Materials and methods
Cell culture
MOVAS (ATCC®CRL-2797) (Afroze et al. 2003) is a continuous mouse aortic VSMC line that has been demonstrated to retain a VSMC-like phenotype, including a spindle cell morphology and the expression of VSMC-specific markers such as smooth muscle α-actin and SM22-α. MOVAS were cultured in Dulbecco's modified Eagle's medium (DMEM) supplemented with 10 % heat-inactivated fetal calf serum (FCS) and 2 mM l-glutamine. For experiments, cells were seeded into white 96-well ViewPlates™ or clear 24-well plates as appropriate.
Sera collection
Mouse sera used in this study were obtained from male C57BL/6J wild-type (WT) or APOE−/− mice (all aged 8–12 weeks) that had been fed a normal chow or Western-style diet (21 % fat and 0.22 % cholesterol), respectively, from 5 weeks of age (Specialty Feeds, Australia). FCS was obtained commercially (JRH Biosciences). For serum collection, mice were euthanized using isoflurane inhalation anesthetic (Baxter Healthcare, Australia). Whole blood was collected from the inferior vena cava using a sterile 26-gauge hypodermic needle (Terumo, Australia) and 1 mL tuberculin syringe (Terumo, Australia) before being transferred into a sterile 1.5 mL microcentrifuge tube. Blood was left to clot for 45 min at room temperature before centrifugation at 16,100×g for 8 min at 4 °C. The serum was collected, transferred into a fresh sterile microcentrifuge tube, and stored at −80 °C until use. All sera used for experiments were non-heat-inactivated.
Cell treatments
One day after seeding the VSMC, the conventional cell culture media (i.e., containing 10 % heat-inactivated FCS) was replaced with an equivalent volume of media containing either non-heat-inactivated FCS, WT, or APOE−/− mouse serum (10–50 %). Cells were then incubated for up to 48 h. In some experiments, cells were exposed to drugs known to disrupt scavenger receptor-dependent and macropinocytosis-dependent endocytotic pathways for the 3 h prior to exposure to serum and the 48 h during exposure to serum. These included amiloride (3,5-diamino-6-chloro-N-(diaminomethylene)pyrazine-2-carboxamide; 0.1–3.0 mmol/L) (Garcia-Perez et al. 2008); 5-(N-ethyl-N-isopropyl)amiloride (10–300 μmol/L) (Martinez-Argudo and Jepson 2008); LY294002 (2-morpholin-4-yl-8-phenylchromen-4-one; 100 μmol/L) (Kruth et al. 2005; Yao et al. 2009); cytochalasin D (1 μmol/L) (Kruth et al. 2005); monodansylcadaverine (MDC; 10 μmol/L) (Jones and Willingham 1999; Coller and Paulnock 2001); SP600125 (1,9-pyrazoloanthrone; 10 μmol/L) (Rahaman et al. 2006); and AG1879 (4-amino-5-(4-chlorophenyl)-7-(t-butyl)pyrazolo[3,4-d]pyrimidine; 10 μmol/L) (Rahaman et al. 2006). Dimethyl sulfoxide (DMSO; 0.1 %) was the vehicle in each case. To examine whether platelet-derived growth factor (PDGF) in mouse sera stimulated lipid uptake by VSMC, WT and APOE−/− mouse sera (20 %) were incubated with a neutralizing anti-PDGF antibody (40 μg/mL; Millipore) for 1 h at 37 °C, before the treatment of cells for 48 h.
Oil Red O staining
At the time of assay, the cell culture medium was removed and VSMC were fixed with isopropyl alcohol. Cells were stained with Oil Red O (0.5 % in 60 % isopropyl alcohol) for 30 min and then destained with isopropyl alcohol. Cells were visualized at ×20 magnification under bright field on an inverted microscope (PALM MicroBeam Carl Zeiss MicroImaging GmbH, Germany). Images were captured by a digital camera under the control of PALM RoboSoftware v3.1-0106.
Quantitation of VSMC lipid accumulation
Lipid accumulation was measured in VSMC plated in 96-well ViewPlates™ using AdipoRed™ assay reagent (Lonza, Basel, Switzerland), according to the manufacturer's instructions. After incubation of VSMC with FCS or mouse serum for 48 h, the cell culture medium was removed and the cells were rinsed with PBS. A volume of 200 μL of PBS was added to each well, followed by 5 μL of the AdipoRed™ assay reagent. Each plate was incubated at room temperature for 15 min and loaded into a Hidex Chameleon Plate Reader for the detection of fluorescence at wavelengths of 485 nm excitation and 570–590 nm emission. Background was subtracted from relative fluorescence units (RFUs) obtained and calculated as a percentage relative to a control.
Cell viability
Cell viability after serum treatment was assessed using CellTiter 96® AQueous One Solution Reagent (Promega, Madison, WI, USA). The reagent was diluted in PBS at a 1:5 ratio then added to each well, and cells were incubated for 1 h in a humidified, 37 °C, 5 % CO2 incubator. Formazan production by cells, which is directly proportional to the number of viable cells, was determined by measuring absorbance at 485 nm.
Serum lipoprotein sub-fractionation and analysis
FCS and mouse sera (stored at 4 °C) were diluted (1:5) in running buffer (20 mM sodium phosphate buffer, pH 7.8) and subjected to fast protein liquid chromatography (FPLC) (BioLogic DuoFlow, BioRad) using a Superdex 200, 10/300 GL column (GE Healthcare, UK). Plasma proteins were eluted by FPLC at a flow rate of 0.25 mL/min and monitored by measuring absorbance at 280 nm.
Chlamydia pneumoniae infection of VSMC cells
VSMC were infected with 104–106 inclusion forming units (IFU) of C. pneumoniae isolate A-03 (kindly provided by P. Timms, Queensland University of Technology, Australia) or a mock inoculum 1 h prior to the commencement of treatment with mouse serum.
Time-lapse video phase contrast microscopy
One day after seeding, cells in a 24-well plate (Nunc, Denmark) were treated with either non-heat-inactivated FCS or mouse serum (10 and 50 %) diluted in DMEM. After treatment, the plate was immediately placed on the stage of an inverted Leica AF6000 LX Live Cell Imaging Workstation (Leica Microsystems, Germany). Images were captured at 30 min intervals over a period of 48 h at ×400 magnification, while the microscope stage was maintained under conventional cell culture conditions in a temperature-controlled and CO2-controlled chamber (37 °C, 5 % CO2). Video images were collected and assembled using the Leica Application Suite AF Software (version 2.0).
Quantitative real-time PCR
Total RNA was harvested from cells using the RNeasy Mini Kit and converted to cDNA with the QuantiTect Reverse Transcription Kit (all from Qiagen, Germany), as per the manufacturer's instructions. Quantitative real-time polymerase chain reaction (PCR) was performed using the following predesigned TaqMan® gene expression assays (Applied Biosystems, USA): smooth muscle α-actin (ACTA2; Mm01546133_m1), ABCA1 (Mm00442663_m1), MCP-1 (CCL2; Mm00441242), RANTES (CCL5; Mm01302428_m1), CD36 (Mm01135198_m1), CD68 (Mm03047343_m1), calponin H1 (CNN1; Mm00487032_m1), Mac-2 (Mm00802901_m1), SR-A1 (MSR1; Mm00446214_m1), and β-actin (4352341E). All real-time PCRs (20 μL) were prepared using diluted cDNA representative of RNA amounts (10–50 ng), 10 μL of 2× Taqman® Universal PCR Master Mix (Applied Biosystems) and 1 μL of the relevant 20× Taqman® Primer/Probe Set. Detection was performed using the CFX 96™ real-time PCR machine (Bio-Rad, Hercules, Germany) using the following thermocycling program: 2 min at 50 °C for optimal Amp® urease activity, initial denaturation 10 min at 95 °C followed by 40 cycles of denaturation 15 s at 95 °C, and annealing and extension for 1 min at 60 °C. All data were normalized to a housekeeping gene (β-actin) and expressed as fold changes relative to a control, using the formula 2−ΔΔCT.
Drugs and their sources
AG1879, amiloride, cytochalasin D, DMSO, EIPA, LY294002, MDC, SP600125, and Oil Red O were all from Sigma-Aldrich. The neutralizing anti-PDGF antibody was from Millipore.
Statistical analysis
All statistical analyses were conducted using the GraphPad Prism software (version 5.03, GraphPad, USA). Where two experimental groups were compared, data were analyzed by Student's unpaired t test. For comparisons across three or more treatment groups, either one-way analysis of variance (ANOVA) followed by Dunnett's post test or two-way ANOVAs followed by Bonferroni post test was used. In all cases, P < 0.05 was considered significant. N values represent the numbers of replicates performed using different cell passages and sera from different mice.
Results
Serum from mice induces lipid accumulation in mouse VSMC
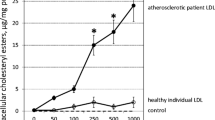
When maintained under our conventional cell culture conditions (i.e., 10 % heat-inactivated FCS in DMEM), murine VSMC displayed an epithelioid appearance, more reminiscent of intimal VSMC than the spindle-shaped VSMC of the medial layer of the vessel wall (Fig. 1a). Incubation of VSMC with serum from either normocholesterolemic (WT) or hypercholesterolemic (APOE−/−) mice for 48 h was associated with profound changes in morphology, most notably the appearance of intracellular vacuoles which stained positively for Oil Red O, indicating the presence of triglycerides and potentially other lipid species (Fig. 1a; see also time-lapse phase contrast videos in Online Supplement Fig. S1). Quantification of lipid accumulation with AdipoRed confirmed the previously described findings (Fig. 1b). Cells exposed to increasing concentrations of FCS displayed minimal lipid uptake (Fig. 1b). By contrast, exposure to serum from WT or APOE−/− mice caused a concentration-dependent increase in lipid accumulation in VSMC. Of note, the lipid content of VSMC exposed to serum from APOE−/− mice was greater than twofold higher than that in cells exposed to WT serum at all concentrations tested (Fig. 1b).
Serum from mice induces lipid accumulation in mouse VSMC. a VSMC were treated for 48 h with 10 % (non-heat-inactivated) FCS (control) or with serum from WT or APOE−/− mice before staining for intracellular lipids with Oil Red O. Images are representative of three separate experiments (scale bars = 150 μm). b Lipid accumulation after 48 h incubation with increasing concentrations of FCS, WT, or APOE−/− sera was also quantified in VSMC using the AdipoRed fluorescence assay. Values (mean ± SEM; n = 4–8) are expressed as relative fluorescence units (RFU). c FPLC fractionation of lipoproteins present in FCS, WT, or APOE−/− sera. d Cell numbers/viability of VSMC following 48 h incubation under standard culture conditions (i.e., 10 % heat-inactivated FCS) or in the presence of 20 % FCS, WT, or APOE−/− serum. MTS conversion into its formazan derivative was assessed by measuring light absorbance at 482 nm (n = 3). *P < 0.05 versus control; # P < 0.05 versus WT for two-way ANOVA with Bonferroni post test for 15 comparisons
Reflecting the lipid uptake profiles described previously, FPLC analysis demonstrated that, whereas FCS was more or less devoid of serum lipids, serum from WT and APOE−/− mice contained appreciable amounts of LDL and HDL (Fig. 1c). In addition, APOE−/− sera contained a high content of very-low-density lipoprotein (VLDL) (Fig. 1c). Finally, lipid accumulation and the change in cell morphology following exposure to the different sera did not have a significant impact on cell numbers/viability as revealed by 3-(4,5-dimethylthiazol-2-yl)-5-(3-carboxymethoxyphenyl)-2-(4-sulfophenyl)-2H-tetrazolium (MTS) staining (Fig. 1d).
Effect of pharmacological inhibitors of scavenger receptor-dependent and macropinocytosis-dependent endocytosis on serum-induced lipid uptake in VSMC
Previously, it has been shown that uptake of modified LDL by macrophage CD36 and SR-A scavenger receptors, and the subsequent transformation of macrophages into foam cells, is dependent on signaling pathways involving Src family tyrosine kinases and/or the c-Jun N-terminal kinases, JNK1 and JNK2 (Ricci et al. 2004; Rahaman et al. 2006; Silverstein et al. 2010). However, in the present study, neither a Src kinase inhibitor, AG1879, nor a JNK inhibitor, SP600125, reduced lipid uptake by VSMC exposed to sera from WT or APOE−/− mice (Fig. 2a, b). Lipid uptake by VSMC was also unaffected by MDC (Fig. 2a, b), an inhibitor of clathrin-dependent endocytosis, which is at least partially responsible for the uptake of oxidized and acetylated LDL by macrophages (Jones and Willingham 1999).
Inhibition of macropinocytosis-dependent but not scavenger receptor-dependent endocytosis reduces serum lipid uptake in VSMC. VSMC were treated with pharmacological inhibitors of scavenger receptor-dependent and clathrin-dependent pathways of lipid uptake (a, b) and of macropinocytosis-dependent endocytosis (c, d) for the 3 h prior to and 48 h during exposure to 20 % WT or APOE−/− mouse serum. Lipid accumulation was monitored using the AdipoRed fluorescence assay. Values (mean ± SEM; n = 4–8) are expressed as a percentage of the control group (i.e., cells maintained under normal culture conditions). *P < 0.05 versus vehicle for one-way repeated-measures ANOVA, with Dunnett's post test
Macropinocytosis is an alternative pathway by which macrophages can accumulate lipids, especially lipids that have undergone minimal or no chemical modifications. Macropinocytotic uptake of lipids by macrophages has been shown to be sensitive to treatment with inhibitors of PI-3 kinase and actin polymerization (Araki et al. 1996, Kruth et al. 2005). In the present study, we showed that inhibition of PI-3 kinase with LY294002 markedly reduced lipid accumulation in VSMC exposed to serum from WT or APOE−/− mice (Fig. 2c, d). An actin polymerization inhibitor, cytochalasin D, also inhibited lipid uptake in VSMC exposed to WT serum (Fig. 2c) but had little effect on cells exposed to APOE−/− serum (Fig. 2d). The effects of two additional macropinocytosis inhibitors, amiloride (0.1–3.0 mmol/L), and its analogue 5-(N-ethyl-N-isopropyl)amiloride (10–300 μmol/L), were also examined. However, both of these inhibitors were found to be toxic to VSMC (data not shown) at concentrations previously demonstrated to inhibit macropinocytosis (Garcia-Perez et al. 2008; Martinez-Argudo and Jepson 2008).
Platelet-derived growth factor and C. pneumoniae infection do not stimulate mouse sera-induced uptake of lipids by VSMC
PDGF has been shown to induce cell membrane ruffling associated with macropinocytosis (Anton et al. 2003; Bryant et al. 2007). Thus, to determine if PDGF present in mouse sera was responsible for lipid accumulation by VSMC, WT and APOE−/− mouse sera were pretreated with a neutralizing anti-PDGF antibody (40 μg/mL) prior to their addition to VSMC. Incubation of VSMC with untreated WT or APOE−/− serum was again associated with a marked increase in lipid uptake, and these effects were not affected by blocking PDGF (Fig. 3a, b).
PDGF and C. pneumoniae (Cpn) infection do not alter mouse serum-induced lipid uptake by VSMC. Preincubation of WT (a) or APOE−/− (b) mouse serum with a neutralizing anti-PDGF antibody (40 μg/mL) did not prevent their abilities to induce lipid accumulation by VSMC. c VSMC were incubated with either mock-containing or Cpn-containing (104–106 IFU) inoculum and subsequently treated with 20 % WT serum for 48 h. Lipid accumulation was quantified using the AdipoRed fluorescence assay. Values (mean ± SEM) are expressed as a percentage of the FCS control group (n = 3–6)
Macropinocytotic lipid uptake in macrophages has previously been linked to the activation of Toll-like receptors (Choi et al. 2009b). Since VSMC are known to express TLR2 and TLR4 (de Graaf et al. 2006), we postulated that C. pneumoniae, a Gram-negative proatherogenic bacteria and agonist of Toll-like receptors, would potentiate lipid accumulation in response to serum. Incubation of VSMC with C. pneumoniae was associated with the formation of inclusion bodies that were visible under a phase contrast microscope (×400 magnification) after 48 h (data not shown) (Rivera et al. 2012). Nonetheless, infection with C. pneumoniae had no additional effects on lipid accumulation in VSMC either in the presence of FCS or mouse serum (Fig. 3d).
Effect of mouse serum on the expression of genes related to LDL uptake and cholesterol efflux in VSMC
The previously described findings indicated that there is likely to be little or no role for classical, receptor-mediated lipid uptake pathways in the effects of mouse serum on VSMC phenotype. Consistent with this idea, we found that the expression of the scavenger receptor, SR-A1, was significantly downregulated in VSMC treated with 20 % WT or APOE−/− mouse sera (Fig. 4a). Exposure of cells to 20 % (non-heat-inactivated) FCS also appeared to reduce SR-A1 expression compared to levels seen in cells maintained under conventional culture conditions, although this effect failed to reach statistical significance. Sera from WT and APOE−/− mice also appeared to reduce expression of CD36, but again this effect was not statistically significant.
Effect of mouse sera on the expression of scavenger receptors in VSMC. VSMC were either maintained under normal culture conditions (i.e., 10 % heat-inactivated FCS; control) or were treated with 20 % FCS, WT, or APOE−/− mouse serum and harvested after 3, 6, 24, or 48 h to measure mRNA expression of a SR-A1 or b CD36 by real-time PCR. Values (mean ± SEM; n = 3–4) are expressed as fold changes relative to the control 3-h time-point. *P < 0.05 for two-way ANOVA with Bonferroni posttest for 24 comparisons
To provide an indication of cholesterol efflux capacity after serum treatment, we measured the expression of ABCA1. Interestingly, mRNA expression of ABCA1 was rapidly downregulated (i.e., within 3 h) following exposure of VSMC to WT or APOE−/− serum (Fig. 4). Furthermore, expression of ABCA1 in mouse serum-treated cells remained suppressed for the remainder of the 48-h treatment period (P < 0.001; Fig. 5).
Mouse serum downregulates the expression of ABCA1. VSMC were either maintained under normal culture conditions (i.e., 10 % heat-inactivated FCS; control) or were treated with 20 % FCS, WT, or APOE−/− mouse serum and harvested after 3, 6, 24, or 48 h to measure mRNA expression of ABCA1 by real-time PCR. Values (mean ± SEM; n = 4) are expressed as fold changes relative to the control 3-h time-point. *P < 0.05 versus control; # P < 0.05 versus FCS for two-way ANOVA with Bonferroni posttest for 24 comparisons
Effect of mouse sera on the expression of markers of VSMC differentiation and inflammation
A previous report demonstrated that, following treatment with cholesterol, mouse VSMC lose their VSMC properties and assume a macrophage-like phenotype (Rong et al. 2003). We, therefore, examined if lipid accumulation induced by mouse serum is associated with similar changes away from a VSMC phenotype. As reported previously (Afroze et al. 2003), MOVAS maintained under standard culture conditions expressed several markers of VSMC differentiation including smooth muscle α-actin, smooth muscle myosin heavy chain, and calponin H1. The levels of each of these markers varied considerably over the course of the 48-h study period, even when the cells were maintained under standard culture conditions (i.e., 10 % heat-inactivated FCS in DMEM). For example, expression of smooth muscle α-actin and calponin H1 appeared to initially increase from the 3-h time-point to the 6-h time-point, and then steadily declined throughout the remainder of the experiment. By contrast, expression of smooth muscle myosin heavy chain progressively increased over the 48-h incubation period (Fig. 6a). Of note, treatment with a higher concentration (20 %) of non-heat-inactivated FCS or with sera for either the WT or APOE−/− mouse strains had no significant effects on the expression levels of these VSMC differentiation markers at any of the time-points examined (Fig. 6a–c).
Effect of mouse serum on markers of cell differentiation. VSMC were either maintained under normal culture conditions (i.e., 10 % heat-inactivated FCS; control) or were treated with 20 % FCS, WT, or APOE−/− mouse serum and harvested after 3, 6, 24, or 48 h to measure mRNA expression of VSMC differentiation markers, such as smooth muscle α-actin (a), calponin HI (b), and smooth muscle myosin heavy chain (SM-MHC; c), and macrophage differentiation markers CD68 (d) and Mac-2 (e) by real-time PCR. Values (mean ± SEM; n = 3–4) are expressed as fold changes relative to the control 3-h time-point
To assess if VSMC gained a more macrophage-like phenotype in the presence of mouse serum, the expression of macrophage markers CD68 and Mac-2 were measured. In VSMC maintained under standard culture conditions, CD68 expression gradually increased during the incubation period such that it was 2.8-fold higher at the 48-h time-point versus the 3-h time-point (Fig. 6d). This temporal profile of CD68 expression was neither affected by increasing the FCS concentration to 20 % nor by exposure of VSMC to WT or APOE−/− serum (Fig. 6b). Contrasting the CD68 profile, the expression of Mac-2 remained relatively constant over the 48-h incubation period in cells maintained under standard culture conditions (Fig. 6e). Exposure to either WT or APOE−/− serum caused a sevenfold increase in Mac-2 expression at the 48-h time-point; however, so too did exposure to the higher concentration of FCS (Fig. 6b), suggesting that the change was not related to the uptake of lipids induced by mouse serum. Thus, to summarize, despite causing profound morphological changes, mouse serum does not appear to cause dedifferentiation of VSMC away from a VSMC phenotype nor does it promote a more macrophage-like phenotype.
Mouse serum also appeared to have no major effects compared to FCS on the expression of the pro-inflammatory chemokines/cytokines CCL2 and CCL5 (Fig. 7). For example, CCL2 expression in VSMC maintained under standard culture conditions gradually declined over the 48-h incubation period, with similar profiles observed in the presence of the higher FCS concentration and following exposure to WT mouse serum (Fig. 7a). Although there was a trend for the APOE−/− serum to cause an increase in CCL2 expression at 3 h (by 3.5-fold) and 6 h (by 2-fold), this was only transient, with expression levels declining thereafter such that, by 24 and 48 h, they were no different to the levels seen in the other treatment groups (Fig. 7a). CCL5 expression in the control group appeared to increase from the 3-h time-point to the 6-h time-point, and then remained relatively stable for the remainder of the experiment (Fig. 7b). By contrast, in cells treated with WT or APOE−/− serum, there was no evidence of any early increases in expression. In fact, expression of CCL5 appeared to decline and, by 48 h, levels of CCL5 appeared to be lower in the mouse sera-treated groups than in the FCS-treated cells (Fig. 7a). Thus, as for the macrophage differentiation markers, the expression of inflammatory markers was either unaffected or reduced by exposure to WT or APOE−/− mouse serum. Note, we also attempted to measure the effect of mouse serum on the expression of the pro-inflammatory cytokines TNF-α and IL-1β; however, these genes were below the detection limits of the assay in both the mouse sera-exposed and FCS-exposed cell groups (data not shown).
Exposure to mouse serum does not induce a pro-inflammatory state in VSMC. VSMC were either maintained under normal culture conditions (i.e., 10 % heat-inactivated FCS; control) or were treated with 20 % FCS, WT, or APOE−/− mouse serum and harvested after 3, 6, 24, or 48 h to measure mRNA expression of the chemokines CCL2 (a) and CCL5 (b) by real-time PCR. Values (mean ± SEM; n = 3–4) are expressed as fold changes relative to the control 3-h time-point
Discussion
Here, we have shown that exposure of murine VSMC to serum from mice causes them to take up lipids and store them in intracellular vacuoles. Accumulation of serum lipids within VSMC was associated with the downregulation of the reverse cholesterol transporter ABCA1 and appeared to be dependent on the process of bulk fluid-phase endocytosis known as macropinocytosis.
As the major cellular component of DIT, VSMC are prevalent in arterial intima prior to the development of atherosclerotic plaques (Stary et al. 1992). Although the physiological function of DIT is largely unknown, its well-organized structure combined with its near universal presence in humans from early childhood irrespective of ethnicity, gender, or family history of cardiovascular disease has led to the belief that it is a normal feature of healthy blood vessels and should not be considered as early evidence of atherosclerosis (Restrepo et al. 1979; Stary et al. 1992; Nakashima et al. 2008). Nevertheless, DIT occurs mainly at sites along the vascular tree that are predisposed to later development of atherosclerotic plaques (Stary et al. 1992; Nakashima et al. 2002). Hence, a better understanding of how the various cellular and noncellular elements that make up DIT respond to potential proatherogenic insults may provide insight into the early events that either trigger or protect against atherosclerotic plaque formation.
According to the “response to retention” hypothesis, atherosclerotic plaque formation begins with the entry of unmodified serum lipids into the subendothelial intima. These lipids then undergo ionic interactions with ECM proteoglycans rendering them susceptible to oxidation (Camejo et al. 1998; Chait and Wight 2000). Following modification, serum lipids, especially LDL, act as inducers of endothelial activation, chemoattractants for inflammatory cells, and fodder for macrophage-derived foam cells (Tabas et al. 2007). Hence, mechanisms that limit the interaction of LDL with proteoglycans and their subsequent modification in the vascular wall are likely to be atheroprotective.
VSMC present in DIT and early atherosclerotic plaques are likely to be exposed to serum lipids that enter the subendothelial intima even prior to them becoming proteoglycan-bound and modified. However, to our knowledge, there is little information on the effects of unmodified serum lipids on VSMC morphology and function. Here, we have shown that exposure of murine VSMC in culture to sera from either normocholesterolemic or hypercholesterolemic mice was associated with marked morphological changes, in particular the formation of lipid-filled vacuoles, which were apparent as early as 6 h after initiation of treatment. Yet, despite these changes, the VSMC retained their expression of several markers of VSMC differentiation and did not appear to assume a pro-inflammatory phenotype.
Traditionally, foam cell formation involves the uptake of lipids, especially those that have been chemically modified through oxidation, acetylation, glycation, or enzymatic processes by scavenger receptors such as CD36, SR-A1, SR-A2, and LOX-1 (Webb and Moore 2007). Although macrophages are the major cell type that undergoes transformation into foam cells within the vessel wall, it is well established that VSMC also express several of these scavenger receptors and can become engorged with lipids when exposed to modified LDL, VLDL, or chylomicrons (Floren et al. 1981; Klouche et al. 2000; Ishii et al. 2002). Uptake of lipids from modified lipoproteins by VSMC in vitro is associated with transdifferentiation into a more macrophage-like phenotype, characterized by reduced expression of VSMC-related genes and elevated expression of macrophage-related genes (Rong et al. 2003). In addition, expression of several pro-inflammatory chemokines (CX3CL1 and CCL2), cytokines (TNF-α and macrophage migration inhibitory factor), and transcription factors (NF-κB and JNK) are also upregulated (Barlic et al. 2007; Chen et al. 2009; Sima et al. 2010; Sun and Chen 2010). In the present study, we examined the effects of inhibitors (shown in parentheses) of signaling enzymes that are essential for the uptake of modified lipids via scavenger receptor-dependent mechanisms including JNKs (SP600125), Src kinases (AG1879), and clathrin-dependent endocytosis (MDC), which is partially responsible for the uptake of oxidized and acetylated LDL by macrophages (Jones and Willingham 1999; Coller and Paulnock 2001; Rahaman et al. 2006). We found none of these compounds to have any inhibitory effects on VSMC lipid uptake induced by serum from WT or APOE−/− mice. As a further indicator that scavenger receptors were not involved, we found that exposure to mouse sera had either no effect or only transiently modulated expression levels of CD36 and SR-A1 in VSMC.
In contrast to its lack of effect on the expression of scavenger receptors, mouse serum caused marked downregulation of ABCA1 in VSMC. ABCA1 plays an important role in many cell types as the primary mediator of cholesterol efflux by facilitating its transfer across the plasma membrane and onto extracellular ApoA1 (Yvan-Charvet et al. 2010). A previous report showed that ABCA1 expression was reduced in intimal versus medial VSMC from human atherosclerotic arteries and that this was associated with an impaired ability to bind ApoA1 and transport lipids to the extracellular compartment (Choi et al. 2009a). Hence, downregulation of ABCA1, leading to a reduction in reverse cholesterol transport, could provide at least some of the explanation for why, in the present study, VSMC accumulated lipids when exposed to mouse sera.
Macropinocytosis is a specialized form of endocytosis that allows the uptake of extracellular fluid in a bulk and nonselective manner (Kerr and Teasdale 2009). Macropinocytosis is characterized by the formation of cup-shaped invaginations (or “ruffles”) of the plasma membrane, which eventually become closed off to form intracellular vacuoles known as macropinosomes (Kerr and Teasdale 2009). Macropinocytosis is now recognized as an alternative pathway of lipid uptake in macrophages (Kruth et al. 2005; Yao et al. 2009). Unlike traditional scavenger receptor-dependent mechanisms, which lead to preferential uptake of modified lipoproteins, macropinocytosis in macrophages is associated with the accumulation of lipids from unmodified or minimally modified lipoproteins (Kruth et al. 2005; Choi et al. 2009b; Yao et al. 2009). Macropinocytosis is dependent on both actin polymerization and PI-3 kinase activity (Araki et al. 1996; Kerr and Teasdale 2009). Hence, our observation that VSMC lipid uptake in response to WT mouse serum was sensitive to treatment with either cytochalasin D or LY294002, which inhibit actin polymerization and PI-3 kinase activity, respectively (Araki et al. 1996; Kruth et al. 2005), is consistent with a role for macropinocytosis in the process. While PI-3 kinase inhibition also partially prevented lipid uptake by VSMC following exposure to APOE−/− serum, cytochalasin D appeared to have no effect. The reason for the differential effect of cytochalasin D on lipid uptake induced by WT versus APOE−/− serum is currently unknown. It may simply relate to the different efficacies of the WT versus the APOE−/− serum in evoking lipid uptake, with the more powerful actions of the latter requiring a higher concentration of inhibitor to be surmounted. Unfortunately, we were unable to test this as higher concentrations of cytochalasin D reduced cell viability (data not shown). Thus, we cannot exclude the possibility that alternative/additional mechanisms to macropinocytosis were at least partially responsible for lipid uptake following exposure to serum from APOE−/− mice.
Initiation of macropinocytosis occurs largely independently of the cargo that is endocytosed. Rather, it is thought to be a consequence of the stimulation of growth factor or pattern recognition receptors (Kerr and Teasdale 2009). Regarding the former, PDGF is one such growth factor that has been shown to stimulate membrane ruffling and macropinocytosis in other vascular (Zhao et al. 2011) and nonvascular (Anton et al. 2003) cell types. However, in the present study, depletion of PDGF from mouse sera with a neutralizing antibody failed to prevent lipid accumulation by VSMC. Likewise, treatment of VSMC with C. pneumoniae, a bacterial species that is known to activate Toll-like receptors in VSMC, did not potentiate serum-induced lipid uptake by VSMC. Hence, at this point, we can only speculate on which factor(s) present in mouse serum may have been responsible for triggering macropinocytosis.
One of the most striking observations from the present study was that, despite the marked morphological changes in VSMC cells following macropinocytotic uptake of lipids, the cells retained the expression levels of VSMC differentiation markers and did not appear to become pro-inflammatory. Were this to hold true in vivo, it might suggest that macropinocytotic lipid uptake by VSMC is a means of removing lipids from the extracellular compartment within the vascular wall, thereby limiting their interaction with ECM proteoglycans and preventing them from undergoing oxidative modification. Hence, the presence of VSMC in DIT and early atherosclerotic lesions, and their ability to act as a “sink” for unmodified serum lipoproteins that enter the vessel wall, might be important factors for limiting the initiation and/or progression of atherosclerotic plaques.
In conclusion, we have demonstrated for the first time that VSMC have a high capacity for uptake and intracellular storage of serum lipoproteins and that this process is likely the result of a macropinocytosis-like uptake pathway and possibly downregulation of ABCA1-mediated cholesterol efflux. While insights into the (patho)physiological significance of these findings require further in vivo studies, we speculate that macropinocytotic uptake of serum lipid by VMSC may be an atheroprotective response to limit oxidative modification of lipids and the subsequent chemoattraction of inflammatory leukocytes.
References
Afroze T, Yang LL, Wang C, Gros R, Kalair W, Hoque AN, Mungrue IN, Zhu Z, Husain M (2003) Calcineurin-independent regulation of plasma membrane Ca2+ ATPase-4 in the vascular smooth muscle cell cycle. Am J Physiol Cell Physiol 285:C88–C95
Anton IM, Saville SP, Byrne MJ, Curcio C, Ramesh N, Hartwig JH, Geha RS (2003) WIP participates in actin reorganization and ruffle formation induced by PDGF. J Cell Sci 116:2443–2451
Araki N, Johnson MT, Swanson JA (1996) A role for phosphoinositide 3-kinase in the completion of macropinocytosis and phagocytosis by macrophages. J Cell Biol 135:1249–1260
Barlic J, Zhang Y, Murphy PM (2007) Atherogenic lipids induce adhesion of human coronary artery smooth muscle cells to macrophages by up-regulating chemokine CX3CL1 on smooth muscle cells in a TNFalpha–NFkappaB-dependent manner. J Biol Chem 282:19167–19176
Bobryshev YV (2006) Monocyte recruitment and foam cell formation in atherosclerosis. Micron 37:208–222
Bryant DM, Kerr MC, Hammond LA, Joseph SR, Mostov KE, Teasdale RD, Stow JL (2007) EGF induces macropinocytosis and SNX1-modulated recycling of E-cadherin. J Cell Sci 120:1818–1828
Camejo G, Hurt-Camejo E, Wiklund O, Bondjers G (1998) Association of apo B lipoproteins with arterial proteoglycans: pathological significance and molecular basis. Atherosclerosis 139:205–222
Chait A, Wight TN (2000) Interaction of native and modified low-density lipoproteins with extracellular matrix. Curr Opin Lipidol 11:457–463
Chen L, Yang G, Zhang X, Wu J, Gu Q, Wei M, Yang J, Zhu Y, Wang N, Guan Y (2009) Induction of MIF expression by oxidized LDL via activation of NF-kappaB in vascular smooth muscle cells. Atherosclerosis 207:428–433
Choi HY, Rahmani M, Wong BW, Allahverdian S, McManus BM, Pickering JG, Chan T, Francis GA (2009a) ATP-binding cassette transporter A1 expression and apolipoprotein A-I binding are impaired in intima-type arterial smooth muscle cells. Circulation 119:3223–3231
Choi SH, Harkewicz R, Lee JH, Boullier A, Almazan F, Li AC, Witztum JL, Bae YS, Miller YI (2009b) Lipoprotein accumulation in macrophages via Toll-like receptor-4-dependent fluid phase uptake. Circ Res 104:1355–1363
Coller SP, Paulnock DM (2001) Signaling pathways initiated in macrophages after engagement of type A scavenger receptors. J Leukoc Biol 70:142–148
de Graaf R, Kloppenburg G, Kitslaar PJ, Bruggeman CA, Stassen F (2006) Human heat shock protein 60 stimulates vascular smooth muscle cell proliferation through Toll-like receptors 2 and 4. Microbes Infect 8:1859–1865
Floren CH, Albers JJ, Bierman EL (1981) Uptake of chylomicron remnants causes cholesterol accumulation in cultured human arterial smooth muscle cells. Biochim Biophys Acta 663:336–349
Garcia-Perez BE, Hernandez-Gonzalez JC, Garcia-Nieto S, Luna-Herrera J (2008) Internalization of a non-pathogenic mycobacteria by macropinocytosis in human alveolar epithelial A549 cells. Microb Pathog 45:1–6
Goldfischer S, Schiller B, Wolinsky H (1975) Lipid accumulation in smooth muscle cell lysosomes in primate atherosclerosis. Am J Pathol 78:497–504
Ishii I, Satoh H, Kawachi H, Jingami H, Matsuoka N, Ohmori S, Bujo H, Yamamoto T, Saito Y, Kitada M (2002) Intimal smooth muscle cells up-regulate beta-very low density lipoprotein-mediated cholesterol accumulation by enhancing beta-very low density lipoprotein uptake and decreasing cholesterol efflux. Biochim Biophys Acta 1585:30–38
Jones NL, Willingham MC (1999) Modified LDLs are internalized by macrophages in part via macropinocytosis. Anat Rec 255:57–68
Kerr MC, Teasdale RD (2009) Defining macropinocytosis. Traffic 10:364–371
Klouche M, Rose-John S, Schmiedt W, Bhakdi S (2000) Enzymatically degraded, nonoxidized LDL induces human vascular smooth muscle cell activation, foam cell transformation, and proliferation. Circulation 101:1799–1805
Kruth HS, Jones NL, Huang W, Zhao B, Ishii I, Chang J, Combs CA, Malide D, Zhang WY (2005) Macropinocytosis is the endocytic pathway that mediates macrophage foam cell formation with native low density lipoprotein. J Biol Chem 280:2352–2360
Li H, Freeman MW, Libby P (1995) Regulation of smooth muscle cell scavenger receptor expression in vivo by atherogenic diets and in vitro by cytokines. J Clin Invest 95:122–133
Lim HJ, Lee S, Lee KS, Park JH, Jang Y, Lee EJ, Park HY (2006) PPARgamma activation induces CD36 expression and stimulates foam cell like changes in rVSMCs. Prostaglandins Other Lipid Mediat 80:165–174
Martinez-Argudo I, Jepson MA (2008) Salmonella translocates across an in vitro M cell model independently of SPI-1 and SPI-2. Microbiology 154:3887–3894
Matsumoto K, Hirano K, Nozaki S, Takamoto A, Nishida M, Nakagawa-Toyama Y, Janabi MY, Ohya T, Yamashita S, Matsuzawa Y (2000) Expression of macrophage (Mphi) scavenger receptor, CD36, in cultured human aortic smooth muscle cells in association with expression of peroxisome proliferator activated receptor-gamma, which regulates gain of Mphi-like phenotype in vitro, and its implication in atherogenesis. Arterioscler Thromb Vasc Biol 20:1027–1032
Nakashima Y, Chen YX, Kinukawa N, Sueishi K (2002) Distributions of diffuse intimal thickening in human arteries: preferential expression in atherosclerosis-prone arteries from an early age. Virchows Arch 441:279–288
Nakashima Y, Wight TN, Sueishi K (2008) Early atherosclerosis in humans: role of diffuse intimal thickening and extracellular matrix proteoglycans. Cardiovasc Res 79:14–23
Rahaman SO, Lennon DJ, Febbraio M, Podrez EA, Hazen SL, Silverstein RL (2006) A CD36-dependent signaling cascade is necessary for macrophage foam cell formation. Cell Metab 4:211–221
Restrepo C, Strong JP, Guzman MA, Tejada C (1979) Geographic comparisons of diffuse intimal thickening of the aorta. Atherosclerosis 32:177–193
Ricci R, Sumara G, Sumara I, Rozenberg I, Kurrer M, Akhmedov A, Hersberger M, Eriksson U, Eberli FR, Becher B, Boren J, Chen M, Cybulsky MI, Moore KJ, Freeman MW, Wagner EF, Matter CM, Luscher TF (2004) Requirement of JNK2 for scavenger receptor A-mediated foam cell formation in atherogenesis. Science 306:1558–1561
Rivera J, Walduck AK, Strugnell RA, Sobey CG, Drummond GR (2012) Chlamydia pneumoniae induces a pro-inflammatory phenotype in murine vascular smooth muscle cells independently of elevating reactive oxygen species. Clin Exp Pharmacol Physiol 39:218–226
Rong JX, Shapiro M, Trogan E, Fisher EA (2003) Transdifferentiation of mouse aortic smooth muscle cells to a macrophage-like state after cholesterol loading. Proc Natl Acad Sci U S A 100:13531–13536
Ruan XZ, Moorhead JF, Tao JL, Ma KL, Wheeler DC, Powis SH, Varghese Z (2006) Mechanisms of dysregulation of low-density lipoprotein receptor expression in vascular smooth muscle cells by inflammatory cytokines. Arterioscler Thromb Vasc Biol 26:1150–1155
Silverstein RL, Li W, Park YM, Rahaman SO (2010) Mechanisms of cell signaling by the scavenger receptor CD36: implications in atherosclerosis and thrombosis. Trans Am Clin Climatol Assoc 121:206–220
Sima AV, Botez GM, Stancu CS, Manea A, Raicu M, Simionescu M (2010) Effect of irreversibly glycated LDL in human vascular smooth muscle cells: lipid loading, oxidative and inflammatory stress. J Cell Mol Med 14:2790–2802
Stary HC, Blankenhorn DH, Chandler AB, Glagov S, Insull W Jr, Richardson M, Rosenfeld ME, Schaffer SA, Schwartz CJ, Wagner WD et al (1992) A definition of the intima of human arteries and of its atherosclerosis-prone regions. A report from the Committee on Vascular Lesions of the Council on Arteriosclerosis, American Heart Association. Arterioscler Thromb 12:120–134
Stary HC, Chandler AB, Glagov S, Guyton JR, Insull W Jr, Rosenfeld ME, Schaffer SA, Schwartz CJ, Wagner WD, Wissler RW (1994) A definition of initial, fatty streak, and intermediate lesions of atherosclerosis. A report from the Committee on Vascular Lesions of the Council on Arteriosclerosis, American Heart Association. Arterioscler Thromb 14:840–856
Sun Y, Chen X (2010) Ox-LDL-induced LOX-1 expression in vascular smooth muscle cells: role of reactive oxygen species. Fundam Clin Pharmacol 25:572–579
Tabas I, Williams KJ, Boren J (2007) Subendothelial lipoprotein retention as the initiating process in atherosclerosis: update and therapeutic implications. Circulation 116:1832–1844
Takebayashi S, Kubota I, Kamio A, Takagi T (1972) Ultrastructural aspects of human atherosclerosis; role of the foam cells and modified smooth muscle cells. J Electron Microsc (Tokyo) 21:301–313
Wagsater D, Olofsson PS, Norgren L, Stenberg B, Sirsjo A (2004) The chemokine and scavenger receptor CXCL16/SR-PSOX is expressed in human vascular smooth muscle cells and is induced by interferon gamma. Biochem Biophys Res Commun 325:1187–1193
Webb NR, Moore KJ (2007) Macrophage-derived foam cells in atherosclerosis: lessons from murine models and implications for therapy. Curr Drug Targets 8:1249–1263
Williams KJ, Tabas I (1995) The response-to-retention hypothesis of early atherogenesis. Arterioscler Thromb Vasc Biol 15:551–561
Yao W, Li K, Liao K (2009) Macropinocytosis contributes to the macrophage foam cell formation in RAW264.7 cells. Acta Biochim Biophys Sin (Shanghai) 41:773–780
Yvan-Charvet L, Wang N, Tall AR (2010) Role of HDL, ABCA1, and ABCG1 transporters in cholesterol efflux and immune responses. Arterioscler Thromb Vasc Biol 30:139–143
Zhao Y, Mangalmurti NS, Xiong Z, Prakash B, Guo F, Stolz DB, Lee JS (2011) Duffy antigen receptor for chemokines mediates chemokine endocytosis through a macropinocytosis-like process in endothelial cells. PLoS One 6:e29624
Acknowledgments
The authors would like to thank Mr. Stephen Firth for his expertise and assistance in acquiring the time-lapse videos of the VSMC. This work was supported by research grants from the National Health and Medical Research Council of Australia (NHMRC; ID nos. 545942 and 436825). JR was supported by a scholarship from the Monash University Faculty of Medicine, Nursing and Health Sciences, while GRD and CGS were supported by fellowships from the NHMRC (ID nos. APP1006017 and 350327, respectively).
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
(AVI 35917 kb)
(AVI 35881 kb)
(AVI 35917 kb)
Rights and permissions
About this article
Cite this article
Rivera, J., Walduck, A.K., Thomas, S.R. et al. Accumulation of serum lipids by vascular smooth muscle cells involves a macropinocytosis-like uptake pathway and is associated with the downregulation of the ATP-binding cassette transporter A1. Naunyn-Schmiedeberg's Arch Pharmacol 386, 1081–1093 (2013). https://doi.org/10.1007/s00210-013-0909-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-013-0909-5