Abstract
The synthetic cannabinoid ajulemic acid (CT-3) is a potent cannabinoid receptor agonist which was found to reduce pain scores in neuropathic pain patients in the absence of cannabis-like psychotropic adverse effects. The reduced psychotropic activity of ajulemic acid has been attributed to a greater contribution of peripheral CB receptors to its mechanism of action as well as to non-CB receptor mechanisms. Loss of inhibitory synaptic transmission within the dorsal horn of the spinal cord plays a key role in the development of chronic pain following inflammation or nerve injury. Inhibitory postsynaptic transmission in the adult spinal cord involves mainly glycine. As we hypothesised that additional non-CB receptor mechanisms of ajulemic acid might contribute to its effect in neuropathic pain, we investigated the interaction of ajulemic acid with strychnine-sensitive α1- and α1β-glycine receptors by using the whole-cell patch clamp technique. Ajulemic acid showed a positive allosteric modulating effect in a concentration range which can be considered close to clinically relevant concentrations (EC50 values: α1 = 9.7 ± 2.6 μM and α1β = 12.4 ± 3.4 μM). Direct activation of glycine receptors was observed at higher concentrations above 100 μM (EC50 values: α1 = 140.9 ± 21.5 μM and α1β = 154.3 ± 32.1 μM). These in vitro results demonstrate that ajulemic acid modulates strychnine-sensitive glycine receptors in clinically relevant concentrations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
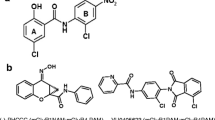
The therapeutic use of Δ9-tetrahydrocannabinol (Δ9-THC) has attracted considerable interest (Costa 2007). However, so far its psychoactive effects which are mediated via neuronal CB1 receptors in the central nervous system (CNS) have limited its therapeutic use as an analgesic (McCarberg and Barkin 2007). Ajulemic acid (AJA, Fig. 1) is a synthetic analog of Δ9-THC. It has anti-inflammatory and analgesic effects in models of acute and chronic pain and inflammation (Burstein et al. 2004; Burstein 2005; Dyson et al. 2005).
In clinical studies, AJA showed strong analgesic effects without marked cannabinoid-like side effects in patients with neuropathic pain (Karst et al. 2003; Salim et al. 2005). The latter finding is supported by the results of animal studies using the tetrad test package (inhibition of locomotor activity, catalepsy, analgesia and hypothermia) where CNS effects were observed at doses five to ten times higher than necessary to achieve analgesia and anti-inflammatory effects (Dyson et al. 2005). Mechanisms identified for these potent analgesic effects of AJA in the absence of central nervous effects comprise, among others, a greater contribution of peripheral CB1 receptors to its mechanism of action (Dyson et al. 2005; Mitrirattanakul et al. 2006; Agarwal et al. 2007).
In recent years, loss of inhibitory synaptic transmission within the dorsal horn of the spinal cord has been established as one of the major mechanisms involved in the development of chronic pain following inflammation or nerve injury (Bolay and Moskowitz 2002; Betz and Laube 2006; Knabl et al. 2008). Inhibitory postsynaptic transmission in the spinal cord involves mainly glycine (Laube et al. 2002) and γ-aminobutyric acid (GABA; Todd et al. 1996; Geiman et al. 2002). Due to its relatively restricted expression in lower areas of the brain and the spinal cord, the strychnine-sensitive glycine receptor family has been suggested as a target site for therapeutic agents aiming at inhibiting pain sensitisation without producing sedation or other central nervous effects (Zeilhofer 2005; Betz and Laube 2006; Lynch and Callister 2006).
We hypothesised that some AJA effects might be mediated via additional targets at the level of the spinal cord dorsal horn. The aim of this study was to investigate potential positive allosteric modulatory as well as directly activating effects of AJA at heterologously expressed α1 homomeric and α1β heteromeric strychnine-sensitive glycine receptors.
Materials and methods
Cell culture and transfection
α1- and α1β-glycine receptor subunits were transiently transfected into transformed human embryonic kidney cells (HEK 293). When co-transfecting the glycine receptor α1- and β-subunits, their respective complementary DNAs (cDNAs) were combined in a ratio of 1:10, since expression of β-polypeptides is less efficient than that of the β-subunits (Pribilla et al. 1992). Reduced sensitivity to 1,000 μM picrotoxin (Sigma-Aldrich, Steinheim, Germany) in α1β heteromeric receptors was used as an assay of the efficacy of β-subunit expression (Pribilla et al. 1992; Haeseler et al. 2005).
Cells were cultured in Dulbecco’s modified Eagle’s medium (Biochrom, Berlin, Germany), supplemented with 10% fetal calf serum (Biochrom), 100 U ml−1 penicillin and 100 μg ml−1 streptomycin at 37°C in a 5% CO2/air incubator. For transfection, cells were suspended in a buffer containing 50 mM K2HPO4 and 20 mM K-acetate, pH 7.35. The corresponding cDNA, each subcloned in the pCIS2 expression vector (Invitrogen, San Diego, USA) was added to the suspension. To visualise transfected cells, they were co-transfected with cDNA encoding for green fluorescent protein (10 μg ml−1). For transfection, we used an electroporation device by EquiBio (Kent, UK). Transfected cells were replated on glass coverslips and incubated 15–24 h before recording.
Solutions
AJA was a kind gift of Prof. Burstein, University of Massachusetts Medical School. AJA was prepared as 100 mM stock solution in dimethylsulfoxide (DMSO; Fluka, Steinheim, Germany), light-protected and stored in glass vessels at 4°C. The AJA stock solution was directly dissolved in bath solution to reach the final drug concentration. Concentrations were calculated from the amount injected into the glass vials. Drug-containing vials were vigorously vortexed for 30 min. Glycine (Sigma-Aldrich) was dissolved directly into the bath solution.
Patch electrodes contained (in mM) KCl 140, MgCl2 2, ethylene glycol bis(2-aminoethyl ether)-N,N,N′,N′-tetraacetic acid 11, N-2-hydroxyethylpiperazine-N′-2-ethanesulfonic acid (HEPES) 10 and glucose 10; the bath solution contained (in mM) NaCl 162, KCl 5.3, NaHPO4 0.6, KH2PO4 0.22, HEPES 15 and glucose 5.6.
Experimental setup
Standard whole-cell experiments (Hamill et al. 1981) were performed at a holding potential of −30 mV. A tight electrical seal of several GΩ formed between the cell membrane and a patch-clamp electrode allows inward currents, due to agonist-induced channel activation, to be resolved in the pA range. The electrical resistance of the recording pipettes was ∼6 MΩ, corresponding to a total access resistance in the whole-cell configuration of ∼10 MΩ. An ultra-fast liquid filament switch technique (Franke et al. 1987) was used for the application of the agonist, presented in pulses of 2 s duration. The agonist and/or the drug under investigation was applied to the cells via a smooth liquid filament achieved with a single outflow (glass tubing 0.15 mm inner diameter) connected to a piezo crystal. The cells were placed at the interface between this filament and the continuously flowing background solution. When a voltage pulse was applied to the piezo, the tube was moved up and down, onto, or away from the cell under investigation. The correct positioning of the cell, in respect to the liquid filament, was ensured by applying a saturating (1000 μM) glycine pulse before and after each test experiment. Care was taken to ensure that the amplitude and the shape of the glycine-activated current had stabilised before proceeding with the experiment. Test solution and glycine (1000 μM) were applied via the same glass-polytetrafluoroethylene perfusion system but from separate reservoirs. The contents of these reservoirs were mixed at a junction immediately before entering the superfusion chamber.
AJA was applied either alone, in order to determine its direct agonistic effects, or in combination with a sub-saturating (EC20) glycine concentration (10 μM), in order to determine its glycine-modulatory effects. A new cell was used for each protocol, and at least four different experiments were performed for each condition. The concentration of the diluent DMSO corresponding to the highest drug concentration used was 0.3%. We have shown that the DMSO itself has no effect at this concentration—neither on glycine-evoked response nor on direct activation of the receptor. The lack of effect of 0.1% DMSO on glycine receptors has also been demonstrated by other investigators (Weir et al. 2004).
Current recording and analysis
For data acquisition and further analysis, we used the EPC 9 digitally controlled amplifier in combination with Pulse and Pulse Fit software (HEKA Electronics, Lambrecht, Germany). Currents were filtered at 2 kHz. Fitting procedures were performed using a non-linear least-squares Marquardt–Levenberg algorithm. Details are provided in the appropriate figure legends or in the “Results” section.
The modulatory effect of the drugs was expressed as percentage of the potentiation of the current elicited by 10 μM glycine according to E(%) = 100[(I − I 0)/I 0], where I 0 is the current response to 10 μM glycine, respectively. Co-activated evoked currents were normalised to their own maximum response. The concentration–response curves for co-activation or direct activation by AJA were fitted according to \(\left( {I_{{\text{norm}}} = \left[ {1 + \left( {{\text{EC}}_{50} /\left[ C \right]} \right)^{n_{\text{H}} } } \right]^{ - 1} } \right)\). I norm is the current modulated (I − I 0) by the glycine (10 μM) cannabinoid mixture or directly activated by the cannabinoid in the absence of glycine. EC50 is the concentration required to evoke a response amounting to 50% of their own maximal response, and n H is the Hill coefficient. Direct activation of α1-subunits by the drugs was assessed in the absence of glycine, applying the drugs at concentrations of 1–300 μM.
Results
A total of 33 cells was included in the study. Expression of α1 and α1β mRNA in HEK 293 cells generated glycine receptors that showed glycine-activated inward currents with amplitudes of 0.8 ± 0.4 nA in α1 and 1.1 ± 0.8 nA in α1β-receptors following saturating (1000 μM) concentrations of the natural agonist. Successful co-expression of the β-subunit was verified with picrotoxin 1000 μM co-applied with 1000 μM glycine after each experiment. In this experimental setting, picrotoxin 1,000 μM blocked α1 homomeric receptors by 49 ± 8%, while α1β-receptors were hardly affected by picrotoxin (13 ± 4% block). When α and β cDNAs were used at a 1:10 ratio for co-transfection, successful co-expression of the β-subunit verified with picrotoxin was 100%. The current transient showed a fast increase, followed by a monophasic decay. The time constant of desensitisation was 836 ± 188 ms in α1 homomeric and 1029 ± 318 ms in α1β-receptors. Experiments with non-transfected HEK cells demonstrated a lack of effect of AJA in these cells (data not shown).
AJA potentiated the current response to glycine 10 μM and directly activated receptor-mediated inward currents in the absence of glycine in both α1- and α1β-receptors in a concentration-dependent manner. The estimates for half-maximum effect concentrations (EC50 ± SD) derived from fits of the Hill equation to the normalised response in α1-receptors are 9.7 ± 2.6 μM (co-activation) and 140.9 ± 21.5 μM (direct activation). The corresponding Hill coefficients (±SD) were 1.0 ± 0.3 and 1.3 ± 0.5, respectively. Representative current traces and concentration–response curves are shown in Fig. 2. EC50 values (±SD) at α1β-glycine receptors were 12.4 ± 3.4 μM (co-activation) and 154.3 ± 32.1 μM (direct activation). The corresponding Hill coefficients were 0.9 ± 0.3 and 1.4 ± 0.6, respectively. Representative current traces and concentration–response curves are shown in Fig. 3. As revealed by the current traces and by the EC50 values displayed in Figs. 2 and 3, AJA co-activates and directly activates currents via α1 homomeric receptors in a similar concentration range compared to α1β heteromeric receptors.
Representative current traces and concentration–response plots for co-activated and directly activated currents at α1-glycine receptors. Left panel Representative current traces elicited by a 2-s application of AJA in the absence of glycine with respect to the current elicited by 1000 μM glycine in the same experiment. AJA directly activated glycine receptor function in a concentration-dependent manner. Right panel Representative current traces elicited by a 2-s co-application of 10 μM glycine and AJA with respect to the current elicited by 1000 μM glycine in the respective control experiment (upper trace). AJA increased the amplitude of the response evoked by 10 μM glycine (second trace from top) in a concentration-dependent manner (third and next traces from top). Currents reached a maximum response of ∼90% with respect to the current elicited by 1000 μM glycine. Lower diagram Concentration response plots for co-activated (triangles) and directly activated currents (circles) plotted against the concentration of AJA (mean ± SD). Solid lines are Hill fits to the data with the indicated parameters
Representative current traces and concentration–response plots for co-activated and directly activated currents at α1β-glycine receptors. Left panel Representative current traces elicited by a 2-s application of AJA in the absence of glycine with respect to the current elicited by 1000 μM glycine in the same experiment. AJA directly activated glycine receptor function in a concentration-dependent manner. Right panel Representative current traces elicited by a 2-s co-application of 10 μM glycine and AJA with respect to the current elicited by 1000 μM glycine in the respective control experiment (upper trace). AJA increased the amplitude of the response evoked by 10 μM glycine (second trace from top) in a concentration-dependent manner (third and next traces from top). Currents reached a maximum response of ∼90% with respect to the current elicited by 1000 μM glycine. Lower diagram Concentration–response plots for co-activated (triangles) and directly activated currents (circles) plotted against the concentration of AJA (mean ± SD). Solid lines are Hill fits to the data with the indicated parameters
DMSO itself has no effect at a maximum concentration of 0.3%—neither on glycine-evoked response nor on direct activation of the receptor (data not shown).
Discussion
In this study, we were able to demonstrate that AJA modulates strychnine-sensitive glycine receptor function in the low micromolar concentration range in vitro. The effects were seen both at homomeric α1- and heteromeric α1β-glycine receptors expressed in HEK 293 cells. The concentration range which was effective in vitro can be considered as close to clinically relevant concentrations because AJA plasma concentrations of ∼2 μM have been measured in blood samples from patients during anti-neuropathic treatment with AJA (Batista et al. 2005). It is worth noting in this context that tenfold higher doses of AJA have been tried in animal experiments without effects on motor function (rotarod assay), indicating a high margin of safety with regard to analgesic versus Δ9-THC-like central nervous effects of the compound (Burstein 2005; Dyson et al. 2005).
Radioligand binding studies have revealed that AJA binds with high affinity to CB1 (range of K i = 11 to 52 nM; Yamamoto et al. 1998; Rhee et al. 1997; Dyson et al. 2005) and peripheral CB2 cannabinoid receptors (K i = 170 nM; Rhee et al. 1997). These binding concentrations at cannabinoid receptors are more than 20-fold lower than the effect concentrations of AJA found for glycine receptor modulation in this study. Despite these differences in the apparent affinity to cannabinoid receptors and the effect concentrations at glycine receptors, we hypothesise that glycine receptor modulation by AJA might be a mechanism contributing to its analgesic and anti-inflammatory effects for two reasons.
First, high-affinity binding of AJA at CB1 and CB2 in vitro does not translate into high potency of the compound to modulate the transduction pathway through G protein-coupled inhibition of adenylylcyclase activity (Rhee et al. 1997). Despite its high receptor affinity, the AJA concentrations required for half-maximum inhibition of CB1-mediated adenylylcyclase activity are around 1 μM (Rhee et al. 1997) and, thus, close to the effect concentrations we found for glycine receptor modulation. This difference in binding and effect concentration is apparently absent for the CB2 receptor (EC50 for CB2-meditated inhibition of adenylylcycase activity 116 nM; Rhee et al. 1997). These results are in line with the assumption that AJA mediates its anti-inflammatory effects primarily via CB2 receptors located in the periphery (Guindon and Hohmann 2008; Ashton 2007). Still, there is experimental evidence for the existence of glycine receptor on leucocytes and macrophages (Froh et al. 2002). Thus, it is conceivable that AJA exerts some of its anti-inflammatory effects via glycine receptors outside the CNS.
Second, the CNS concentration of AJA might be considerably higher at the site of a nerve injury. Under normal conditions, only 30–40% of the AJA plasma concentrations have been found in the CNS (Dyson et al. 2005; Fox and Bevan 2005). However, recent studies have shown that chronic nerve lesions lead to an increase in permeability of the blood–spinal cord barrier (Brooks et al. 2005; Gordh et al. 2006). Thus, the permeation of AJA into the spinal cord CNS might be improved in conditions of neuropathic pain. This might generate spinal concentrations of AJA in a range needed for potentiation of glycinergic inhibition. Increased neuronal excitability in chronic pain states involves loss of inhibition mediated by GABAA or glycinergic neurons in the superficial dorsal horn of the spinal cord that control the relay of nociceptive signals from the periphery to higher areas of the CNS (Ahmadi et al. 2002; Moore et al. 2002; Coull et al. 2003). Thus, potentiation or restoration of glycinergic inhibition at the level of the spinal cord might contribute to the analgesic effects of AJA. However, animal experiments will be needed to show the involvement of glycinergic with respect to cannabinergic mechanisms in the analgesic effects of AJA. The assumption that the effects of AJA at strychnine-sensitive glycine receptors might complement its cannabinergic effects is indirectly supported by studies in transgenic mice lacking CB1 receptors in peripheral neurons which revealed a major reduction in analgesia produced by systemic cannabinoids like Δ9-THC, indicating that these peripheral CB1 receptors, not those inside the CNS, constitute a prime target for producing cannabinoid analgesia (Agarwal et al. 2007). One potential mechanism underlying this observation is that the CB1-mediated impact on network activity might be considerably different between central nervous and peripheral cannabinoid receptors.
Glycine receptor modulation has previously been shown for Δ9-THC, the endogenous cannabinoid anandamide (Hejazi et al. 2006) and the synthetic cannabinoid WIN55,212-2 (Iatsenko et al. 2007). There is evidence that significant amino acid sequence homologies exist between glycine receptor subunits and putative ligand-binding regions of the CB2 receptor (Tao et al. 1999; Betz and Laube 2006). It is conceivable that strychnine-sensitive glycine receptors and CB2 receptors both are targets for cannabinoid receptor ligands due to structural similarities in the receptor binding site.
Furthermore, we have demonstrated in this study that the interaction of AJA with the glycine receptor is not influenced by the subunit composition of the glycine receptor. In line with these results, we have previously shown that co-expression of the glycine β-subunit does not affect the response of heterologously expressed α1-subunits to different phenol derivatives including the anaesthetic propofol (Ahrens et al. 2004; Haeseler et al. 2005). Glycine receptors belong to the ligand-gated ion channel superfamily which has a common structure in which five subunits form an ion channel (Jentsch et al. 2002). Initial cross-linking studies using spinal cord glycine receptors suggested that α- and β-subunits assemble into a pentameric receptor with a proposed in vivo stochiometry of 3α:2β (Langosch et al. 1988; Laube et al. 2002). A recent study brought evidence that Xenopus laevis oocytes assemble glycine receptors composed of two α- and three β-subunits (Grudzinska et al. 2005). Upon activation, these receptors usually inhibit neuronal firing by opening the associated chloride channel and the consequent decrease in neuronal input resistance (Jentsch et al. 2002). α1-Glycine receptor subunits efficiently form homomeric receptors in heterologous expression systems. β-Subunits do not form homomeric receptors but affect the function of heteromeric receptors by changing the sensitivity to various agonists (among them the natural agonist glycine) and antagonists (e.g. picrotoxin; Shan et al. 2003; Grudzinska et al. 2005). Apparently, the effect of both AJA and propofol analogues is not affected by co-expression of the β-subunit.
The glycine receptor is positively modulated by anaesthetics and alcohols (Mihic et al. 1997). This effect is supposed to contribute to the anti-nociceptive but not to the hypnotic actions of anaesthetics (Ahrens et al. 2004; Chen et al. 2007). We have recently shown that mutation of the S267 residue at the glycine receptor α1-subunit abolished direct receptor activation by propofol and strongly decreased its potency to co-activate the receptor (Ahrens et al. 2008). Further studies are needed to address the question whether the respective amino acids are equally involved in the action of cannabinoids on glycine receptors. A more detailed knowledge of the amino acid residues crucial for the positive allosteric modulatory effect of AJA at strychnine-sensitive glycine receptors may ultimately allow to investigate the contribution of glycinergic mechanisms to the in vivo effect of AJA in a knock in animal model.
In conclusion, our in vitro study shows that AJA positively modulates one of the main inhibitory receptors in the spinal cord, the strychnine-sensitive glycine receptor. This might constitute a synergic mechanism complementing the analgesic and anti-inflammatory effects of AJA which are mediated via peripheral CB1 and CB2 receptors (Dyson et al. 2005; Agarwal et al. 2007; Guindon and Hohmann 2008).
References
Agarwal N, Pacher P, Tegeder I, Amaya F, Constantin CE, Brenner GJ, Rubino T, Michalski CW, Marsicano G, Monory K, Mackie K, Marian C, Batkai S, Parolaro D, Fischer MJ, Reeh P, Kunos G, Kress M, Lutz B, Woolf CJ, Kuner R (2007) Cannabinoids mediate analgesia largely via peripheral type 1 cannabinoid receptors in nociceptors. Nat Neurosci 10(7):870–879
Ahmadi S, Lippross S, Neuhuber WL, Zeilhofer HU (2002) PGE(2) selectively blocks inhibitory glycinergic neurotransmission onto rat superficial dorsal horn neurons. Nat Neurosci 5(1):34–40
Ahrens J, Haeseler G, Leuwer M, Mohammadi B, Krampfl K, Dengler R, Bufler J (2004) 2,6 Di-tert-butylphenol, a nonanesthetic propofol analog, modulates alpha1beta glycine receptor function in a manner distinct from propofol. Anesth Analg 99(1):91–96
Ahrens J, Leuwer M, Stachura S, Krampfl K, Belelli D, Lambert JJ, Haeseler G (2008) A transmembrane residue influences the interaction of propofol with the strychnine-sensitive glycine α1 and α1β receptor. Anesth Analg 107, (in press)
Ashton JC (2007) Cannabinoids for the treatment of inflammation. Curr Opin Investig Drugs 8(5):373–384
Batista C, Berisha M, Karst M, Salim K, Schneider U, Brenneisen R (2005) Determination of ajulemic acid and its glucuronide in human plasma by gas chromatography–mass spectrometry. J Chromatogr B Analyt Technol Biomed Life Sci 820(1):77–82
Betz H, Laube B (2006) Glycine receptors: recent insights into their structural organization and functional diversity. J Neurochem 97(6):1600–1610
Bolay H, Moskowitz MA (2002) Mechanisms of pain modulation in chronic syndromes. Neurology 59(5 Suppl 2):S2–S7
Brooks TA, Hawkins BT, Huber JD, Egleton RD, Davis TP (2005) Chronic inflammatory pain leads to increased blood–brain barrier permeability and tight junction protein alterations. Am J Physiol Heart Circ Physiol 289(2):H738–H743
Burstein S (2005) Ajulemic acid (IP-751): synthesis, proof of principle, toxicity studies, and clinical trials. AAPS J 7(1):E143–E148
Burstein SH, Karst M, Schneider U, Zurier RB (2004) Ajulemic acid: a novel cannabinoid produces analgesia without a “high”. Life Sci 75(12):1513–1522
Chen Y, Dai TJ, Zeng YM (2007) Strychnine-sensitive glycine receptors mediate the analgesic but not hypnotic effects of emulsified volatile anesthetics. Pharmacology 80(2–3):151–157
Costa B (2007) On the pharmacological properties of Delta9-tetrahydrocannabinol (THC). Chem Biodivers 4(8):1664–1677
Coull JA, Boudreau D, Bachand K, Prescott SA, Nault F, Sik A, De Koninck P, De Koninck Y (2003) Trans-synaptic shift in anion gradient in spinal lamina I neurons as a mechanism of neuropathic pain. Nature 424(6951):938–942
Dyson A, Peacock M, Chen A, Courade JP, Yaqoob M, Groarke A, Brain C, Loong Y, Fox A (2005) Antihyperalgesic properties of the cannabinoid CT-3 in chronic neuropathic and inflammatory pain states in the rat. Pain 116(1–2):129–137
Fox A, Bevan S (2005) Therapeutic potential of cannabinoid receptor agonists as analgesic agents. Expert Opin Investig Drugs 14(6):695–703
Franke C, Hatt H, Dudel J (1987) Liquid filament switch for ultra-fast exchanges of solutions at excised patches of synaptic membrane of crayfish muscle. Neurosci Lett 77(2):199–204
Froh M, Thurman RG, Wheeler MD (2002) Molecular evidence for a glycine-gated chloride channel in macrophages and leukocytes. Am J Physiol Gastrointest Liver Physiol 283(4):856–863
Geiman EJ, Zheng W, Fritschy JM, Alvarez FJ (2002) Glycine and GABA(A) receptor subunits on Renshaw cells: relationship with presynaptic neurotransmitters and postsynaptic gephyrin clusters. J Comp Neurol 444(3):275–289
Gordh T, Chu H, Sharma HS (2006) Spinal nerve lesion alters blood–spinal cord barrier function and activates astrocytes in the rat. Pain 124(1–2):211–221
Grudzinska J, Schemm R, Haeger S, Nicke A, Schmalzing G, Betz H, Laube B (2005) The beta subunit determines the ligand binding properties of synaptic glycine receptors. Neuron 45(5):727–739
Guindon J, Hohmann AG (2008) Cannabinoid CB2 receptors: a therapeutic target for the treatment of inflammatory and neuropathic pain. Br J Pharmacol 153(2):319–334
Haeseler G, Ahrens J, Krampfl K, Bufler J, Dengler R, Hecker H, Aronson JK, Leuwer M (2005) Structural features of phenol derivatives determining potency for activation of chloride currents via alpha(1) homomeric and alpha(1)beta heteromeric glycine receptors. Br J Pharmacol 145(7):916–925
Hamill OP, Marty A, Neher E, Sakmann B, Sigworth FJ (1981) Improved patch-clamp techniques for high-resolution current recording from cells and cell-free membrane patches. Pflugers Arch 391(2):85–100
Hejazi N, Zhou C, Oz M, Sun H, Ye JH, Zhang L (2006) Delta9-tetrahydrocannabinol and endogenous cannabinoid anandamide directly potentiate the function of glycine receptors. Mol Pharmacol 69(3):991–997
Iatsenko NM, Tsintsadze T, Lozova NO (2007) The synthetic cannabinoid analog WIN 55,212-2 potentiates the amplitudes of glycine-activated currents. Fiziol Zh 53(3):31–37
Jentsch TJ, Stein V, Weinreich F, Zdebik AA (2002) Molecular structure and physiological function of chloride channels. Physiol Rev 82(2):503–568
Karst M, Salim K, Burstein S, Conrad I, Hoy L, Schneider U (2003) Analgesic effect of the synthetic cannabinoid CT-3 on chronic neuropathic pain: a randomized controlled trial. JAMA 290(13):1757–1762
Knabl J, Witschi R, Hosl K, Reinold H, Zeilhofer UB, Ahmadi S, Brockhaus J, Sergejeva M, Hess A, Brune K, Fritschy JM, Rudolph U, Mohler H, Zeilhofer HU (2008) Reversal of pathological pain through specific spinal GABAA receptor subtypes. Nature 451(7176):330–334
Langosch D, Thomas L, Betz H (1988) Conserved quaternary structure of ligand-gated ion channels: the postsynaptic glycine receptor is a pentamer. Proc Natl Acad Sci U S A 85(19):7394–7398
Laube B, Maksay G, Schemm R, Betz H (2002) Modulation of glycine receptor function: a novel approach for therapeutic intervention at inhibitory synapses? Trends Pharmacol Sci 23(11):519–527
Lynch JW, Callister RJ (2006) Glycine receptors: a new therapeutic target in pain pathways. Curr Opin Investig Drugs 7(1):48–53
McCarberg BH, Barkin RL (2007) The future of cannabinoids as analgesic agents: a pharmacologic, pharmacokinetic, and pharmacodynamic overview. Am J Ther 14(5):475–483
Mihic SJ, Ye Q, Wick MJ, Koltchine VV, Krasowski MD, Finn SE, Mascia MP, Valenzuela CF, Hanson KK, Greenblatt EP, Harris RA, Harrison NL (1997) Sites of alcohol and volatile anaesthetic action on GABA(A) and glycine receptors. Nature 389(6649):385–389
Mitrirattanakul S, Ramakul N, Guerrero AV, Matsuka Y, Ono T, Iwase H, Mackie K, Faull KF, Spigelman I (2006) Site-specific increases in peripheral cannabinoid receptors and their endogenous ligands in a model of neuropathic pain. Pain 126(1–3):102–114
Moore KA, Kohno T, Karchewski LA, Scholz J, Baba H, Woolf CJ (2002) Partial peripheral nerve injury promotes a selective loss of GABAergic inhibition in the superficial dorsal horn of the spinal cord. J Neurosci 22(15):6724–6731
Pribilla I, Takagi T, Langosch D, Bormann J, Betz H (1992) The atypical M2 segment of the beta subunit confers picrotoxinin resistance to inhibitory glycine receptor channels. EMBO J 11(12):4305–4311
Rhee MH, Vogel Z, Barg J, Bayewitch M, Levy R, Hanus L, Breuer A, Mechoulam R (1997) Cannabinol derivatives: binding to cannabinoid receptors and inhibition of adenylylcyclase. J Med Chem 40(20):3228–3233
Salim K, Schneider U, Burstein S, Hoy L, Karst M (2005) Pain measurements and side effect profile of the novel cannabinoid ajulemic acid. Neuropharmacology 48(8):1164–1171
Shan Q, Nevin ST, Haddrill JL, Lynch JW (2003) Asymmetric contribution of alpha and beta subunits to the activation of alphabeta heteromeric glycine receptors. J Neurochem 86(2):498–507
Tao Q, McAllister SD, Andreassi J, Nowell KW, Cabral GA, Hurst DP, Bachtel K, Ekman MC, Reggio PH, Abood ME (1999) Role of a conserved lysine residue in the peripheral cannabinoid receptor (CB2): evidence for subtype specificity. Mol Pharmacol 55(3):605–613
Todd AJ, Watt C, Spike RC, Sieghart W (1996) Colocalization of GABA, glycine, and their receptors at synapses in the rat spinal cord. J Neurosci 16(3):974–982
Weir CJ, Ling AT, Belelli D, Wildsmith JA, Peters JA, Lambert JJ (2004) The interaction of anaesthetic steroids with recombinant glycine and GABAA receptors. Br J Anaesth 92(5):704–711
Yamamoto I, Kimura T, Kamei A, Yoshida H, Watanabe K, Ho IK, Yoshimura H (1998) Competitive inhibition of delta8-tetrahydrocannabinol and its active metabolites for cannabinoid receptor binding. Biol Pharm Bull 21(4):408–410
Zeilhofer HU (2005) The glycinergic control of spinal pain processing. Cell Mol Life Sci 62(18):2027–2035
Acknowledgements
We are grateful to J. Kilian and A. Niesel, Dept. of Neurology, Hannover, for technical support and Prof. Dr. Sumner Burstein, Dept. of Biochemistry and Molecular Pharmacology, University of Massachusetts Medical School, USA, for his kind supply of AJA.
Conflict of interest statement
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ahrens, J., Leuwer, M., Demir, R. et al. Positive allosteric modulatory effects of ajulemic acid at strychnine-sensitive glycine α1- and α1β-receptors. Naunyn-Schmied Arch Pharmacol 379, 371–378 (2009). https://doi.org/10.1007/s00210-008-0366-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-008-0366-8