Abstract
We investigated several behavioural responses induced by repeated administration of MDMA in mice that could be related to its potential abuse liability. Mice treated with MDMA at the dose of 10 mg/kg displayed a significant conditioned place preference with respect to saline treated controls, while lower doses (0.3, 1.0, 3.3 mg/kg) had no effect. The development of physical dependence was also investigated. Mice were treated with MDMA (10 mg/kg) twice daily for 5 days. On day 6, following a single administration of MDMA mice received the following monoaminergic antagonists: metergoline (0.1 and 1 mg/kg), ritanserin (0.25 and 1 mg/kg), timolol (2 and 10 mg/kg), prazosin (0.25 and 1 mg/kg), SCH 23390 (0.05 and 0.25 mg/kg), raclopride (0.1 and 0.5 mg/kg) or vehicle, and several somatic manifestations of withdrawal were evaluated for 45 min. Metergoline induced paw tremor, face rubbing, as well as an increase in locomotor activity in mice chronically treated with MDMA. Ritanserin, and timolol induced only paw tremor, while SCH 23390 and raclopride did not produce any somatic manifestation indicative of abstinence. The possible modification of the rewarding properties of MDMA (10 mg/kg) by the monoaminergic antagonists producing the most relevant somatic signs of withdrawal namely, metergoline (0.1 and 1 mg/kg) and timolol (2 and 10 mg/kg) were tested in the conditioned place preference paradigm. Results showed that metergoline did not significantly modify the rewarding properties of MDMA, whereas only the highest dose of timolol was able to decrease MDMA reward. No signs of dopaminergic neurotoxicity were observed following chronic treatment with MDMA as revealed by [3H] mazindol binding. The possible motivational and affective components of the withdrawal syndrome were assessed in the suppression of operant responding for food, the conditioned place aversion, and the lit/dark paradigms. Results showed that the somatic symptoms observed were not accompanied by any aversive/dysphoric or anxiogenic-like behaviours. These results reveal the rewarding properties of MDMA in mice, and suggest that chronic MDMA administration does not induce classical manifestations of physical dependence in mice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
MDMA (3,4-methylenedioxy-methylamphetamine, “ecstasy”) is a phenethylamine derivative with psychostimulant properties widely used by young adults during night parties. Its acute effects in humans include hyperactivity, emotional closeness, mental acuity and reduced fatigue (Greer and Tolbert 1986; Peroutka et al. 1988; Camí et al. 2000). Studies in laboratory animals have attributed its locomotor stimulating effects to both the activation of serotonergic and dopaminergic systems (Gold et al. 1989; Callaway et al. 1990).
Although the evidence for MDMA rewarding properties in experimental animals seems undoubtedly strong (Beardsley et al. 1986; Lamb and Griffiths 1987; Bilsky et al. 1991; Marona-Lewicka et al. 1996; Ratzenboeck et al. 2001; Braida and Sala 2002; Meyer et al. 2002), the question still remains as to whether or not MDMA produces these effects in mice. This is an important issue considering the species differences that exist with respect to MDMA neurochemical effects, and the prospect of using genetically modified mice to study the neurobiological substrates of these effects. Indeed, it has been shown that repeated MDMA administration induces a sustained loss in dopamine, but not in serotonin concentrations in the mouse striatum, while in rats the opposite occurs (Stone et al. 1987; Logan et al. 1988; Colado et al. 1999; O’Shea et al. 2001).
At doses that produce rewarding effects, MDMA increases the release of dopamine in the nucleus accumbens of rats (Yamamoto and Spanos 1988; Marona-Lewicka et al. 1996; White et al. 1996; Kankaanpää et al. 1998). Increased activity in the mesolimbic dopaminergic system is thought to be a common neuronal substrate mediating the rewarding properties of prototypical drugs of abuse including alcohol, psychostimulants, nicotine, opioids, and cannabinoids (Chen et al. 1990; Yoshimoto et al. 1992; Pontieri et al. 1996; Koob and Le Moal 2001). This effect on dopamine release has been reported to be responsible, at least in part, for MDMA rewarding properties (Bilsky et al. 1998).
An important aspect of MDMA action that is unexplored to date is the capacity of this substance for producing physical dependence. The majority of human studies have concentrated on correlating the cognitive and affective impairments observed in MDMA users with the neurotoxic damage produced, and on evaluating the duration of these effects (Reneman et al. 2000; Gouzoulis-Mayfrank et al. 2000). Clinical studies to date do not reveal the development of physical dependence in humans after MDMA consumption. However, this negative result could be biased by the pattern of consumption since most ecstasy users consume this drug intermittently during weekends. Furthermore, there are no studies in animals examining whether or not MDMA can produce physical dependence probably owing to the complexity of MDMA action involving a multiplicity of neurotransmitter systems. Animal studies are suitable to address this issue since they allow optimizing of pharmacological treatment conditions required to develop physical dependence. This is an important question given that there is a considerable amount of data suggesting the abuse liability of MDMA (Camí et al. 2000). Thus, human studies have recognized small sub-populations of long-time consumers of elevated quantities of MDMA fulfilling DSM-IV criteria for abuse or dependence (von Sydow et al. 2002). Furthermore, a variety of new different patterns of MDMA use has become known in recent years, including “bingeing” or taking multiple doses over a period of hours or days, and intravenous administration (Hammersley et al. 1999; Topp et al. 1999). These changing patterns of ecstasy use, in addition to increasing the health hazard related to ecstasy use, may also represent increase risk for abuse and dependence.
In this study, we first investigated the rewarding properties of MDMA in mice using the conditioned place preference paradigm. In addition, we attempted to develop a set of optimal experimental conditions for producing physical dependence to MDMA in the mouse. This protocol consisted in treating mice repeatedly twice daily for 5 days and once on day 6 with non-neurotoxic doses of MDMA (10 mg/kg), and subsequently blocking the action of different neurotransmitter systems known to be involved in the behavioural actions of MDMA namely, dopamine, serotonin and noradrenaline. Thus, we blocked β1/2-adrenergic receptors with timolol, α1-adrenergic receptors with prazosin, 5-HT1/2-serotonergic receptors with metergoline, 5-HT2-serotonergic receptors with ritanserin, D1-dopaminergic receptors with SCH 23390, and D2-dopaminergic receptors with raclopride. Furthermore, we examined whether the antagonists producing the most relevant somatic signs of withdrawal, metergoline and timolol were capable of modifying the rewarding properties of MDMA in the place-conditioning paradigm. Considering the predominant neurotoxic effects of MDMA on dopamine pathways in mice, dopamine terminal integrity was verified using [3H] mazindol binding. Finally, we examined the possible motivational and affective components of MDMA abstinence in the suppression of operant responding for food, the conditioned place aversion, and the lit/dark paradigms. Metergoline (0.1 mg/kg, i.p.) was selected for these studies since it produced the most prominent somatic manifestations of withdrawal in mice chronically treated with MDMA.
Materials and methods
Animals
CD1 male mice weighing from 25 to 30 g were housed five per cage and acclimatized to the laboratory conditions (12 h light/dark cycle, 21±1°C room temperature, 55±10% humidity) 1 week before the experiment with ad libitum access to food and water. Behavioural tests and animal care were conducted in accordance with the standard ethical guidelines (National Institutes of Health, publication 85-23, revised 1985; European Communities Directive 86/609) and approved by the local ethical committee. The observer was blind to the treatments in all experiments.
Drugs
MDMA hydrochloride [(+/-) 3,4-methylenedioxymethamphetamine] was obtained from Lipomed, A.G. (Arlesheim, Switzerland), and dissolved in 0.9% physiological saline. Metergoline, ritanserin, timolol maleate and prazosin hydrochloride (Sigma, Spain) were dissolved in 0.5% carboxymethylcellulose. SCH 23390 and raclopride (Sigma, Spain) were dissolved in 0.9% physiological saline. All compounds were injected intraperitoneally (i.p.) in a volume of 0.1 ml per 10 g body weight.
Chronic MDMA administration
Mice were treated twice daily (9:00 a.m. and 7:00 p.m.), with MDMA (10 mg/kg i.p.) or with saline for 5 consecutive days. Since spontaneous withdrawal manifestations were not observed after this chronic MDMA treatment, on the 6th day mice received the morning injection of MDMA or saline and 4 h later, they were injected with one of the following antagonists: the 5HT1/2-serotonergic-antagonist, metergoline (0.1 and 1.0 mg/kg), the 5HT2-serotonergic antagonist, ritanserin (0.25 and 1.0 mg/kg), the D1-dopaminergic antagonist SCH 23390 (0.05 and 0.25 mg/kg), the D2-dopaminergic antagonist raclopride (0.1 and 0.5 mg/kg), the β1/2-adrenergic antagonist, timolol (2 and 10 mg/kg), the α1-adrenergic antagonist, prazosin (0.25 and 1.0 mg/kg), or vehicle. Immediately after the antagonist injection, mice were placed in a circular clear plastic observation area (25 cm diameter, 40 cm height) for a 45 min observation period. Measurements of somatic signs after the antagonist challenge were divided into 5 min time intervals, as previously described (Maldonado et al. 1996). The number of wet dog shakes, face rubbing and front paw tremor were counted. Body tremor, ptosis, and piloerection were scored 1 for appearance and 0 for non-appearance within each 5 min time period. Scores for the level of activity were made by giving in each 5 min period a value of 0 for low activity (less than 5 complete crossings of the observation area), 1 for normal activity (between 5 and 20 complete crossings of the observation area), or 2 for increased activity (more than 20 complete crossings of the observation area). A quantitative value was calculated in each animal for the different checked signs by adding the scores obtained in each 5-min time period. Immediately after the observation period, animals were sacrificed in order to quantitatively assess presynaptic dopamine transporter binding sites. In order to assess a possible influence of vegetative effects of chronic MDMA administration in the behaviour of mice, measures of temperature and weight were taken 30 min before, and 4 h after the first and last injection of MDMA and saline.
Place conditioning paradigm
The place conditioning protocol used was non-biased. The apparatus is composed of two main square conditioning compartments (15×15×15 cm) separated by a triangular central area (Maldonado et al. 1997). The light intensity within the conditioning chambers was 30±5 lux. During the pre-conditioning phase, drug-naive mice were placed in the middle of the central area and had free access to both compartments (striped and dotted) of the apparatus for 20 min. The time spent in each compartment was recorded by computerized monitoring software (Videotrack; View Point, Lyon, France). In Experiment 1, during the conditioning phase, mice were pre-treated with MDMA (0.3, 1.1, 3.3 and 10 mg/kg, i.p.) or saline 30 min before being confined into one of the two conditioning compartments for 30 min. In Experiment 2, animals were pre-treated with MDMA (10 mg/kg, i.p.) or saline 30 min before conditioning and with either vehicle, metergoline (0.1 and 1 mg/kg, i.p.) or timolol (2 and 10 mg/kg, i.p.) 15 min before conditioning. In both experiments, four pairings were carried out with MDMA and four pairings with vehicle. MDMA and saline were administered on alternate days, and the animals were exposed to only one pairing per day. Treatments were counterbalanced as closely as possible between compartments. Control animals received vehicle every day. The test phase was conducted exactly as the preconditioning phase, i.e., free access to each compartment for 20 min. A preference score was calculated for each group as the difference between the times spent in the drug-paired compartment during the test and pre-conditioning phases.
Aversive/dysphoric effects induced by the administration of metergoline to animals chronically treated with MDMA
Two different paradigms were used to study the possible aversive/dysphoric effects of MDMA withdrawal: the suppression of operant responding for food and the conditioned place aversion paradigms.
A non-biased conditioned place aversion procedure was conducted in the same apparatus previously described for the conditioned place preference. During the preconditioning phase on day 1, animals freely explored both compartments, and the time spent in each one was measured during 20 min. On days 2–5 mice were treated twice daily (9:00 a.m. and 7:00 p.m.) with MDMA (10 mg/kg, i.p) or saline in order to induce a dependence-like state. During the conditioning phase, on day 6, animals received the morning injection of MDMA (10 mg/kg, i.p) or saline, and returned to their home cages. Four hours later, metergoline (0.1 mg/kg, i.p.) or vehicle was administered and the animals were confined in one of the compartments for 45 min. This same day, the animals received the afternoon injection of MDMA or saline, and returned to their home cages. On day 7, 4 h after the morning injection of MDMA (10 mg/kg, i.p.) or saline, all animals received vehicle and were confined in the other compartment for 45 min. The afternoon injection of MDMA or saline was administered at 7:00 p.m. On day 8, the possible expression of a place aversion to the compartment associated with MDMA withdrawal was tested allowing the mice to visit both compartments during 20 min. A score value was calculated for each mouse as the difference between the time spent in the drug-paired compartment during the post-conditioning and preconditioning phases.
For the suppression of operant responding for food paradigm, mice were first deprived of food (3.5 g of food were provided daily) in order to obtain 95% of their initial weight. The same food deprivation regime was maintained during the whole evaluation of food-maintained operant behaviour. Water was available ad libitum during this experimental phase. Five days after starting food deprivation mice were trained in operant chambers (Med Associates, Georgia VT, USA) to nose-poke for food pellets. First, mice were trained under a fixed ratio (FR1) schedule of reinforcement, where they performed 1 nose-poke in the active hole to obtain 1 food pellet. A 10 s time-out period was imposed after each reinforcement. During this 10-s period the cue light was off and no reward was provided on the active hole. Responses on the inactive hole and all the responses during the 10-s timeout period were also recorded. The session was terminated after 100 reinforcers or after 1 h, whichever occurred first. When mice maintained their number of responses in the active hole for 3 consecutive days with more than 75% of the total possible reinforcers earned (100), the FR schedule was progressively increased to FR3 and FR5. Stable responding on a FR5 was defined using the same criteria. Once animals maintained this response, they were treated with MDMA (10 mg/kg) or vehicle twice daily (9:00 a.m. and 7:00 p.m.) during 5 days, and once on day 6 (9:00 a.m.). On the first day of this chronic treatment, after the morning injection of MDMA or saline, animals were immediately placed in the operant chambers for a test session of 60 min (acute effect). On the 5th day, mice received the morning injection of MDMA or saline and were returned to the home cage. Four hours later they were injected with vehicle and placed in the operant chambers for a 60-min test session. On the 6th day, animals received the morning injection of MDMA or saline, were returned to their home cages, and 4 h later they were treated with metergoline (0.1 mg/kg) and placed in the operant chambers for a test session of 60 min.
Anxiogenic-like effects induced by metergoline in mice chronically treated with MDMA
The possible anxiogenic-like effects of MDMA withdrawal were evaluated in the lit/dark box. Mice were individually exposed for 5 min to the lit/dark box consisting of a small compartment (15×20×25 cm) with black walls and black floor dimly lit (5 lux) connected by a 4 cm long tunnel to a large compartment (30×20×25 cm) with white walls and a white floor, under intense illumination (500 lux). Lines were drawn on the floor of both compartments to allow measurement of locomotor activity by counting the number of squares (5×5 cm) crossed. Floor lines separated the lit compartment into three equal zones, from the tunnel to the opposite wall, designated as proximal, median and distal zone. On days 1 to 5, mice were treated twice daily (9:00 a.m. and 7:00 p.m.) with MDMA (10 mg/kg, i.p) or vehicle. The 6th day, animals received MDMA (10 mg/kg, i.p) or saline in the morning, and 4 h later they received an injection of metergoline (0.1 mg/kg, i.p.) or vehicle. Thirty minutes later, each animal was placed in the dark compartment of the lit/dark box facing the tunnel. The latency for the first entry into the white compartment, the number of entries, and number of squares crossed, and the time spent in each compartment were recorded during 5 min.
Autoradiography of [3H]-mazindol binding
In order to quantitatively assess presynaptic dopamine transporter binding sites in the striatum of control and MDMA-treated mice, [3H]-mazindol autoradiographic studies were carried out according to the protocol used was by Ryan et al. (2001) with slight modifications. Briefly, animals were decapitated and their brains were quickly removed and frozen by immersion in 2-methyl-butane surrounded by dry ice. All samples were stored at −80°C before use. Coronal sections 20 μm-thick were cut in a cryostat according to the Paxinos and Franklin atlas (1997), and thaw-mounted on gelatine/chrome-coated slides. To determine total mazindol binding, sections were preincubated at 4°C for 15 min in 50 mM Tris-HCl buffer (pH 7.9) containing 300 mM NaCl and 5 mM KCl, before incubation for 60 min in the same buffer containing 300 nM desipramine (Sigma Chemical Co., Madrid Spain) and 4 nM [3H]-mazindol (New England Nuclear; specific activity 24 Ci/mmol). Desipramine was included to block the binding of [3H]-mazindol to noradrenaline uptake sites. Sections were then washed twice for 3 min in the Tris-HCl preincubation buffer and dried under a stream of cold, dry air. To determine the non-specific binding, consecutive sections were incubated in the same buffer for 60 min at 4°C with the addition of 100 μM nomifensine (Sigma Chemical Co., Madrid Spain). Autoradiograms were generated by apposing the labelled tissues, together with autoradiographic standards ([3H] micro-scales, Amersham), to tritium-sensitive film (Hyperfilm-[3H], Amersham) for a period of 6 weeks and developed for 5 min at 20°C. Films were analysed and quantified with a computer-assisted video-densitometer (MCID, St. Catherine, Ontario Canada) using the standard curve generated from [3H]-standards. Specific binding measured in the entire striatum was determined by subtracting the non-specific binding image from that of total binding.
Statistics
The data were analysed using two-way ANOVAs between subjects. When significant interactions between factors were observed, individual comparisons were carried out using one-way ANOVAs followed by the Dunnett’s post-hoc test. The CPP data in regard to the time spent in the drug-paired compartment during the pretest and the test sessions was analyzed using one-way ANOVA and paired Student’s t-test.
Results
MDMA-induced conditioned place preference in mice
One-way ANOVA revealed a significant effect of treatment with MDMA, F(4,75)=3.69, p<0.01, and the post-hoc test showed that the dose of 10 mg/kg MDMA produced a significant place preference with respect to saline (p<0.05; Fig. 1).
Effects of MDMA (0.3, 1.1, 3.3 and 10 mg/kg, i.p.), or saline on the conditioned place preference paradigm in mice. Data are expressed as mean ± SEM of score values. MDMA and saline were administered 30 min before conditioning. Four pairings were carried out with MDMA and four pairings with vehicle on alternate days (n=14 per group). Black star indicates p<0.05 vs. saline (Dunnett’s post-hoc test)
Behavioural manifestations induced by serotonergic, adrenergic and dopaminergic antagonists in mice chronically treated with MDMA
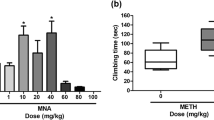
Timolol challenge
The following somatic signs were significantly revealed in the different experimental groups: paw-tremor, body tremor, piloerection, wet-dog shakes, locomotor activity and ptosis. For paw-tremor, a main effect of chronic treatment, F(1,62)=21.62, p<0.001, antagonist treatment, F(2,62)=6.46, p<0.01, and a significant interaction between these two factors, F(2,62)=4.90, p<0.01, were observed. A significant main effect of chronic treatment was also observed for locomotor activity, F(1,62)=23.79, p<0.001, piloerection, F(1,62)=4.95, p<0.05, and wet-dog shakes, F(1,62)=12.26, p<0.001, but no main effect of antagonist treatment or significant interaction between these two factors was obtained for these signs. For body tremor, only a main effect of antagonist treatment was observed, F(2,62)=4.91, p<0.01 (Fig. 2).
Somatic manifestations induced by the acute administration of the β1/2-adrenergic antagonist, timolol (2 and 10 mg/kg, i.p.) in mice chronically treated with MDMA (10 mg/kg twice daily for 5 days, and once on day 6; black bars) or saline (white bars). Data are expressed as mean ± SEM incidents of checked and counted signs observed over a period of 45 min (n=10–12 per group). Two white stars indicate p<0.01 vs. similar chronic treatment group receiving vehicle (Dunnett’s post-hoc test). One black star indicates p<0.05, two black stars p<0.01 vs. similar acute treatment group receiving chronic saline (ANOVA one-way). Paw tremor was increased in animals chronically treated with MDMA, F(2,33)=6.60, p<0.01, but not in those receiving saline. In animals chronically treated with MDMA, only the dose of 10 mg/kg of timolol significantly increased paw tremor (p<0.01) compared to vehicle (Dunnett’s). Comparisons between groups for each dose of antagonist revealed a significant increase in paw tremor in mice treated with MDMA and receiving timolol 2.0 mg/kg, F(1,20)=7.63, p<0.05, and 10.0 mg/kg F(1,20)=12.58, p<0.01, with respect to similar groups of mice treated with saline
Prazosin challenge
The following somatic signs were significantly revealed in the different experimental groups: paw-tremor, body tremor, piloerection, wet-dog shakes, locomotor activity and ptosis. For locomotor activity, wet-dog shakes and body tremor a main effect of chronic treatment, F(1,61)=11.37, p<0.01; F(1,61)=4.29, p<0.05; F(1,61)=12.94, p<0.05 respectively, and a main effect of antagonist treatment, F(2,61)=20.86, p<0.001; F(2,61)=6.60, p<0.01; F(2,61)=27.57, p<0.001 respectively, but no interaction between these two factors were observed. For paw tremor and piloerection only a main effect of chronic treatment was observed, F(1,61)=9.59, p<0.01 and F(1,61)=14.85, p<0.001 respectively. For ptosis, only a main effect of the antagonist treatment was observed, F(2,61)=89.50, p<0.001 (Table 1).
Metergoline challenge
The following somatic signs were significantly revealed in the different experimental groups: paw-tremor, face rubbing, body tremor, piloerection, wet-dog shakes and locomotor activity. For paw tremor, face rubbing and body tremor a significant main effect of chronic treatment, F(1,60)=21.35, p<0.001; F(1,25)=44.01, p<0.001; F(1,60)=8.82, p<0.01 respectively, antagonist treatment, F(2,60)=7.53, p<0.001; F(2,25)=18.27, p<0.001; F(2,60)=4.88, p<0.01 respectively, and significant interaction between these two factors were observed, F(2,60)=7.09, p<0.01; F(2,25)=17.07, p<0.001; F(2,60)=10.10, p<0.001 respectively. For locomotor activity, a significant main effect of chronic treatment, F(1,60)=66.69, p<0.001, and a significant interaction between chronic and antagonist treatments, F(2,60)=6.32, p<0.01] were observed. For piloerection, a significant main effect of chronic treatment, F(1,60)=5.46, p<0.05, and antagonist treatment, F(2,60)=10.98, p<0.001, but no interaction between these two factors was observed (Fig. 3).
Somatic manifestations induced by the acute administration of the 5-HT1/2-serotonergic antagonist metergoline (0.1 and 1.0 mg/kg) in mice chronically treated with MDMA (10 mg/kg twice daily for 5 days, and once on day 6; black bars) or saline (white bars). Data are expressed as mean ± SEM incidents of checked and counted signs observed over a period of 45 min (n=9–12 per group). One white star indicates p<0.05, two white stars p<0.01 vs. similar chronic treatment group receiving vehicle (Dunnett’s post-hoc test), one black star indicates p<0.05, two black stars p<0.01, three black stars p<0.001 vs. similar acute treatment group receiving chronic saline (ANOVA one-way). A significant effect of metergoline treatment in MDMA treated mice was observed for paw-tremor, body tremor, and face rubbing, F(2,27)=6.13, p<0.01; F(2,27)=5.47, p<0.01; F(2,10)=12.04, p<0.01 respectively. The dose of 0.1 mg/kg significantly increased paw-tremor and face rubbing in this group (p<0.01) compared to vehicle. A significant effect of metergoline treatment for body tremor, F(2,33)=10.23, p<0.001, was observed only in the saline group. Both doses of metergoline significantly increased body tremor in this group (p<0.01) with respect to vehicle. Comparisons between groups for each dose of the antagonist showed that body tremor was significantly higher in mice treated with MDMA receiving vehicle, F(1,21)=21.99, p<0.001, and metergoline 0.1 mg/kg, F(1,20)=10.35, p<0.01, compared to similar groups of mice treated with saline. Paw tremor was also higher in mice treated with MDMA receiving vehicle, F(1,21)=5.62, p<0.05, metergoline 0.1 mg/kg, F(1,19)=29.61, p<0.001, and 1.0 mg/kg, F(1,20)=11.12, p<0.01, with respect to similar groups of mice treated with saline. Face rubbing was increased in mice treated with MDMA receiving metergoline 0.1 mg/kg, F(1,8)=11.56, p<0.01, and 1.0 mg/kg, F(1,8)=31.80, p<0.001, with respect to similar groups treated with saline. For locomotor activity, a significant effect of the antagonist was observed only in the group treated with MDMA, F(2,27)=3.98, p<0.05. Metergoline 1.0 mg/kg significantly increased locomotor activity with respect to vehicle (p<0.05) in this group. Comparisons between groups for each dose of the antagonist showed a significant increase in locomotor activity in mice treated with MDMA receiving vehicle, F(1,21)=4.79, p<0.05, metergoline 0.1 mg/kg, F(1,20)=19.80, p<0.001, and 1.0 mg/kg, F(1,19)=90.10, p<0.001, compared to similar groups of mice treated with saline
Ritanserin challenge
The following somatic signs were significantly revealed in the different experimental groups: paw-tremor, face rubbing, body tremor, piloerection, wet-dog shakes and locomotor activity. For paw-tremor, a significant main effect of chronic treatment, F(1,63)=37.39, p<0.001, antagonist treatment, F(2,63)=5.63, p<0.01, and significant interaction between these two factors were observed, F(2,63)=4.35, p<0.01. For locomotor activity, body tremor, ptosis and face rubbing only a significant main effect of chronic treatment was observed, F(1,63)=28.26, p<0.001; F(1,63)=22.80, p<0.001; F(1,63)=4.29, p<0.05; F(1,28)=16.40, p<0.001 respectively). For piloerection, only a significant main effect of antagonist treatment was observed, F(2,63)=3.25, p<0.05 (Fig. 4).
Somatic manifestations induced by the acute administration of the 5HT2-serotonergic antagonist, ritanserin (0.25 and 1.0 mg/kg) in mice chronically treated with MDMA (10 mg/kg twice daily for 5 days, and once on day 6; black bars) or saline (white bars). Data are expressed as mean ± SEM incidents of checked and counted signs observed over a period of 45 min (n=11–12 per group). Two white stars indicate p<0.01 vs. similar chronic treatment group receiving vehicle (Dunnett’s post-hoc test), one black star indicates p<0.05, two black stars p<0.01, three black stars p<0.001 vs. similar acute treatment group receiving chronic saline (ANOVA one-way). A significant effect of ritanserin treatment, F(2,30)=4.75, p<0.05, was observed in the MDMA group. Ritanserin 0.25 mg/kg significantly increased paw-tremor (p<0.01) compared to vehicle. Comparisons between groups for each dose of the antagonists showed a significant increase in paw-tremor in mice treated with MDMA receiving vehicle, F(1,20)=6.49, p<0.05, ritanserin 0.25 mg/kg, F(1,21)=12.58, p<0.01, and 1.0 mg/kg, F(1,21)=42.61, p<0.001, as compared to similar groups of mice treated with saline
Raclopride challenge
The following somatic signs were significantly revealed in the different experimental groups: paw-tremor, body tremor, piloerection and locomotor activity. For locomotor activity, a main effect of chronic treatment, F(1,54)=17.31, p<0.001] and antagonist treatment, F(2,54)=14.23, p<0.001, but no interaction between these two factors was observed. For body tremor and piloerection, only a main effect of antagonist treatment was observed F(2,54)=10.98, p<0.001; F(2,54)=6.27, p<0.004 respectively. For paw tremor, only a main effect of chronic treatment was revealed, F(1,54)=5.75, p<0.02 (Table 1)
SCH 23390 challenge
The following somatic signs were significantly revealed in the different experimental groups: body tremor, piloerection, wet-dog shakes and locomotor activity. For locomotor activity, a significant main effect of chronic treatment, F(1,54)=7.78, p<0.01, antagonist treatment, F(2,54)=41.63, p<0.001 and significant interaction between these two factors were observed, F(2,54)=5.72, p<0.01. For piloerection, a significant main effect of antagonist treatment, F(2,54)=10.08, p<0.001, and a significant interaction between chronic and antagonist treatments were observed, F(2,54)=3.42, p<0.05. For body tremor, only a main effect of the antagonist treatment was observed, F(2,54)=14.33, p<0.001. For wet-dog shakes, only a main effect of chronic treatment was revealed, F(1,54)=5.80, p<0.05 (Fig. 5).
Somatic manifestations induced by the acute administration of the D1-dopaminergic antagonist SCH 23390 (0.05 and 0.25 mg/kg) in mice chronically treated with MDMA (10 mg/kg twice daily for 5 days, and once on day 6; black bars) or saline (white bars). Data are expressed as mean ± SEM incidents of checked and counted signs observed over a period of 45 min (n=10 per group). One white star indicates p<0.05, two white stars p<0.01, three white stars p<0.001 vs. similar chronic treatment group receiving vehicle (Dunnett’s post-hoc test), one black star indicates p<0.05, two black stars p<0.01 vs. similar acute treatment group receiving chronic saline (ANOVA one-way). A significant effect of SCH 23390 for locomotor activity was observed in both of these groups, F(2,27)=7.49, p<0.01; F(2,27)=43.58, p<0.001 respectively. Both doses of SCH 23390 (0.25 and 0.05 mg/kg) significantly decreased locomotor activity in the saline and MDMA treated groups (p<0.01 and p<0.001 respectively) compared to vehicle. Comparisons between groups showed that locomotor activity was significantly increased in mice treated with MDMA receiving vehicle, F(1,18)=11.66, p<0.01, as compared to the same group treated with saline. For piloerection, a significant effect of SCH 23390 was observed only in the group treated chronically with MDMA, F(2,27)=16.62, p<0.001. The dose of 0.25 mg/kg and 0.05 mg/kg significantly increased piloerection in this group (p<0.001 and p<0.05 respectively) with respect to vehicle. Between group comparisons for each dose of the antagonist showed a significant increase in piloerection in mice treated with MDMA receiving SCH 23390 0.25 mg/kg, F(1,18)=7.67, p<0.05, with respect to the same group treated with saline
Effects of MDMA on body temperature and weight
For body weight and temperature, two-way ANOVAs revealed no significant effects of chronic treatment, time of measurement, or interaction between these two factors indicating that both groups of animals showed similar basal temperature and weight, and that chronic treatment with MDMA did not affect these parameters (data not shown).
Effects of metergoline and timolol on MDMA-induced conditioned place preference in mice
A two-way ANOVA analyzing the effects of treatment with MDMA or saline and treatment with different doses of metergoline on the preference scores revealed a significant effect of treatment with MDMA, F(1,73)=11.24 p<0.05], but no significant effect of antagonist treatment or interaction between factors (Fig. 6A). Further paired wise comparisons (paired t-test) within each group for pre-test vs. test revealed significant differences in the groups treated with MDMA + vehicle (p<0.05), metergoline 0.1 mg/kg (p<0.05) and 1.0 mg/kg (p<0.05) (Fig. 6B). Similarly, statistical analysis of the effects of timolol treatment on MDMA-induced CPP on preference scores showed a significant effect of MDMA treatment, F(1,71)=6.45, p<0.05, but no significant effects of timolol treatment or interaction (Fig. 6C). One-way ANOVA for the time spent in the drug-paired compartment during the pre-test sessions showed no significant differences between groups. Paired wise comparisons (paired t-test) within each group for pre-test vs. test revealed significant differences in the group treated with MDMA + timolol 2 mg/kg (p<0.01), but no significant differences in the group treated with MDMA + timolol 10 mg/kg, indicating that only this latter dose of timolol abolished MDMA-induced CPP (Fig. 6D).
Effects of the serotonergic 5-HT1/2-receptor antagonist metergoline (A, B), and the β1/2 adrenergic receptor antagonist, timolol (C, D) on the rewarding properties of MDMA in the conditioned place preference paradigm (n=10–20 per group). In the left panels white and black bars represent the preference scores for the drug-paired compartment in animals treated with saline and MDMA (10 mg/kg, i.p.) respectively, 30 min before conditioning. Vehicle (VEH), metergoline at the dose of 0.1 mg/kg (MET 0.1), and 1.0 mg/kg (MET 1), timolol at the dose of 2 mg/kg (TIM 2) and 10 mg/kg (TIM 10) were injected 15 min before conditioning. In the right panels white and hatched bars represent the time spent in the drug-paired compartment by the groups treated with MDMA during the pretest and the test sessions respectively. One black star indicates p<0.05, two black stars p<0.01 (paired t-test)
Lack of aversive/dysphoric effects induced by MDMA withdrawal
In the conditioned place aversion paradigm, two-way ANOVA did not show any significant main effect of chronic treatment with MDMA, antagonist treatment, nor interaction between these two factors (Fig. 7A). In the suppression of operant responding for food, acute administration of MDMA did not significantly modify operant responding for food with respect to the administration of saline. In addition, two-way ANOVA showed no significant main effect of chronic treatment, antagonist treatment or interaction between these two factors (Fig. 7B). Together, these results indicate that the behavioural manifestations of withdrawal precipitated by metergoline (0.1 mg/kg, i.p.) in mice chronically treated with MDMA did not induce aversive/dysphoric properties.
Effects of metergoline (MET, 0.1 mg/kg, i.p.) or vehicle in mice treated chronically with MDMA (10 mg/kg twice daily for 5 days, and once on day 6) or saline in the place-conditioning paradigm (A), the suppression of operant responding for food paradigm (B), and the lit/dark box (C). In A, data are expressed as mean ± SEM of the score for the drug-paired compartment (n=12–13 per group). In B, MDMA did not significantly modify responding for food following one administration (ACUTE), or following chronic treatment (VEH; see Materials and methods for details). Animals chronically treated with MDMA receiving metergoline (MET, 0.1 mg/kg) did not show any suppression of operant responding for food (n=4–5 per group). In C, data represent latency (sec) for first white entry and time (sec) spent in black and white compartments in the different groups. No significant simple effects were observed in any of the different parameters measured (see Materials and methods for details; n=7–10 per group)
Lack of anxiogenic-like responses induced by MDMA withdrawal
In the lit/dark paradigm, for time spent in the black compartment, two-way ANOVA revealed a significant interaction between chronic and antagonist treatments, F(1,16)=4.86, p<0.05. Further analysis (one-way ANOVAs) showed no significant differences among the different experimental groups. For entries into the black compartment, statistical analysis revealed a significant main effect of chronic treatment only, F(1,16)=14.92, p<0.01. For latency to enter the white compartment, number to entries into the white compartment, squares crossed and time spent in the black and white compartments, no significant main effects or interactions between factors were observed (Fig. 7C).
Autoradiography of [3H]-mazindol binding
The distribution of [3H]-mazindol binding in the striatum of mice treated chronically with MDMA (10 mg/kg, i.p.; twice a day during 5 days, and once on day 6) was similar to that observed in mice treated chronically with saline. Quantitative autoradiography of [3H]-mazindol binding in the striatum of mice repeatedly treated with MDMA did not significantly differ from that of mice treated repeatedly with saline (MDMA: 86.43±13.93 fmol/mg, n=4; saline: 88.49±9.739 fmol/mg, n=5), indicating that this MDMA injection regimen does not produce dopaminergic neurotoxicity in the striatum of mice (Fig. 8).
Representative autoradiogram of [3H]-mazindol binding in the striatum of mice chronically treated with MDMA (10 mg/kg, i.p. twice daily for 5 days and once on day 6; right panel) or saline (left panel) (A). Quantitative density of [3H]-mazindol binding sites (fmol/mg) in mice chronically treated with MDMA (black bar) or saline (white bar) (B)
Discussion
Using the conditioned place preference paradigm, this study corroborates previous findings showing that MDMA is able to induce rewarding effects in mice (Salzmann et al. 2003). The establishment of an easy and reliable model to reveal rewarding effects in mice represents an important advantage considering the different lines of genetically modified mice now available. These results are also in line with previous studies in rats using this experimental model (Bilsky et al. 1990; Schechter 1991; Marona-Lewicka et al. 1996; Meyer et al. 2002). The rewarding effects observed in the present study were observed with high (10 mg/kg), but not low doses (0.3, 1.0 or 3.0 mg/kg) of MDMA. One possible explanation for the absence of rewarding effects with low doses of MDMA in mice might be the induction of motivational states that are in conflict with its rewarding properties. In this sense, mice studies using the elevated plus maze indicate that MDMA at the dose of 4 mg/kg has anxiogenic-like properties, while higher doses (20 mg/kg) have anxiolytic-like effects (Lin et al. 1999). However, anxiogenic effects have also been reported in the lit/dark box after administration of high doses (8 and 15 mg/kg) of MDMA (Maldonado and Navarro 2000).
Although the abuse liability of MDMA has been documented in humans (Camí et al. 2000), it has been difficult to study the capacity of MDMA to induce physical dependence due to the current pattern of consumption, i.e. discontinuous intake mainly during weekends. In order to investigate whether MDMA is able to produce physical dependence in animals, we have developed a protocol of chronic administration of MDMA in mice at doses that do not produce neurotoxic effects on the dopaminergic system, the most sensitive pathway in mice to MDMA toxicity. The absence of neurotoxicity on the dopaminergic terminals was demonstrated using [3H] mazindol autoradiography techniques, which revealed that the chronic administration of MDMA (10 mg/kg twice a day for 5 days, and once on day 6) did not change the density or distribution of presynaptic dopamine transporter binding sites in the striatum. The possible development of a physical withdrawal syndrome after chronic MDMA was investigated by acutely blocking different neurotransmitter receptors known to be involved in the behavioural actions of MDMA, including dopamine, noradrenaline and serotonin receptors.
Some of these monoaminergic antagonists produced non-specific responses in both chronic MDMA- and saline-treated mice, which revealed their intrinsic sedative effects. Thus, the dopaminergic antagonists, SCH23390 and raclopride, as well as the α1-adrenergic antagonist prazosin induced a decrease in locomotor activity and ptosis in all experimental groups. Furthermore, these three monoaminergic antagonists also induced an increase in body tremor in all animals.
Mice chronically treated with MDMA receiving an acute injection of vehicle showed increased locomotor activity with respect to mice chronically treated with saline, indicating that the stimulating effects of MDMA at the dose of 10 mg/kg persist after eleven consecutive administrations. Metergoline specifically potentiated this hyperlocomotion in mice chronically treated with MDMA. These results are in line with other studies showing that blockade of 5-HT1/2-serotonergic receptors with methysergide also potentiates the acute locomotor activating properties of MDMA (Gold and Koob 1988). The possible involvement of serotonergic neurotoxicity in the observed effects can be neglected since it has been reported that repeated injections of MDMA (20 mg/kg) twice daily during 4 days, do not produce significant changes in serotonin uptake sites in the striatum of mice (Battaglia et al. 1988a). Furthermore, three injections of MDMA (20 and 30 mg/kg) given 3 h apart, a neurotoxic regimen producing a marked depletion in striatal dopamine content in mice, was reported to be ineffective for depleting striatal serotonin or its metabolites (O’Shea et al. 2001).
Acute administration of the different monoaminergic antagonists also induced several somatic manifestations in mice chronically treated with MDMA that could be specifically related to a withdrawal syndrome since they were not observed in control saline-treated animals. Thus, the 5-HT1/2-serotonergic antagonist, metergoline induced a significant presence of paw tremor and face rubbing, while the 5-HT2-serotonergic antagonist, ritanserin induced only a significant incidence of paw tremor. The presence of face rubbing in addition to other classical behavioural signs related to a withdrawal syndrome such as paw tremor in mice treated with metergoline, suggests that this antagonist produces more relevant behavioural manifestations of abstinence to MDMA, and supports a role for serotonergic 5HT1 receptors in these behavioural changes. With respect to the adrenergic antagonists, only the β1/2-adrenergic antagonist, timolol significantly increased the incidence of paw tremor, while the α1 antagonist, prazosin had no significant effects. Although it is known that some vegetative responses induced by MDMA involve the adrenergic system (Battaglia et al. 1988b), the role of this neurotransmitter in mediating the behavioural effects of MDMA has been poorly studied. The present results suggest that β-adrenoceptors could also participate in the adaptive changes produced by chronic MDMA administration. However, in general, the somatic manifestations observed following these drug challenges are minor compared to those observed for other drugs of abuse. Finally, the D1-dopaminergic antagonist, SCH 23390 induced only piloerection, while the D2 antagonist raclopride did not produce any specific behavioural manifestation of withdrawal. These data indicate that dopamine D1 and D2 antagonists play a negligible role in the adaptive responses induced by chronic MDMA treatment, and contrast with the role played by the dopaminergic system in several behavioural responses induced by MDMA (Gold et al. 1989; Bilsky et al. 1998).
Since metergoline and timolol induced the most relevant signs of withdrawal, their possible involvement in the rewarding properties of MDMA was evaluated in the conditioned place preference paradigm. We found that the motivational effects of MDMA were not significantly modified by metergoline. On the other hand, timolol attenuated conditioned place preference to MDMA but only when administered at the highest dose. Although there is no existing data corroborating the contribution of β1/2-adrenergic receptors in MDMA rewarding effects, some studies have reported a modulatory action of propanolol in the rewarding properties of other psychostimulants such as cocaine and amphetamine (Yokel and Wise 1975; Harris et al. 1996). Together, these studies suggest that the motivational properties of MDMA and the somatic manifestations of MDMA withdrawal are probably mediated through different mechanisms. We cannot exclude however, the possible involvement of dopamine receptors in the motivational properties of MDMA.
Withdrawal from a chronic treatment with all the prototypical drugs of abuse is associated with the presence of negative motivational and/or emotional effects, even in the case of drugs that are unable to develop somatic manifestations of withdrawal (Koob and Le Moal 2001). In order to better understand the significance of our results, we therefore evaluated if the somatic manifestations precipitated by monoaminergic antagonists in MDMA chronically treated mice were associated to these negative effects. For this purpose, we chose the monoaminergic antagonist producing the most severe somatic manifestations in MDMA-treated mice, i.e., metergoline at the dose of 0.1 mg/kg. First, the possible aversive/dysphoric manifestations of withdrawal were evaluated in the suppression of operant responding for food, and the conditioned place aversion paradigms. Mice chronically treated with MDMA receiving an acute administration of metergoline did not show suppression of operant responding for food. Similarly, metergoline did not induce conditioned place aversion in mice chronically treated with MDMA. These results indicate that the somatic manifestations of MDMA withdrawal precipitated by this serotonergic antagonist are not associated to dysphoric/aversive properties. Finally, we evaluated if these somatic manifestations appeared together with anxiogenic-like effects. Metergoline administration to mice treated chronically with MDMA did not significantly modify any of the parameters studied in the lit/dark box, suggesting the absence of anxiogenic-like properties in the observed withdrawal syndrome. These results contrast with other data showing that drugs of abuse, including those that do not produce physical dependence, such as psychostimulants, induce a motivational withdrawal syndrome characterized by dysphoria/aversion and/or negative emotional effects (Koob and Le Moal 2001).
In conclusion, this study indicates that blockade of 5-HT1/2-serotonin receptors induces several somatic manifestations in mice chronically treated with MDMA, which are not accompanied by dysphoric or anxiogenic-like behaviours, and does not modify the rewarding properties of MDMA. Timolol on the other hand, induces some somatic manifestations of MDMA abstinence, but only modifies MDMA reward when administered at the highest dose. Therefore, chronic administration of MDMA in these experimental conditions does not develop a relevant state of dependence since it was not possible to precipitate a withdrawal syndrome with the classical properties reported for the abstinence of prototypical drugs of abuse.
References
Battaglia G, Yen SY, De Souza EB (1988a) MDMA-induced neurotoxicity: parameters of degeneration and recovery of brain serotonin neurons. Pharmacol Biochem Behav 29:269–274
Battaglia G, Brooks BP, Kulsakdinun C, De Souza EB (1988b) Pharmacologic profile of MDMA (3,4-methylenedioxymethamphetamine) at various brain recognition sites. Eur J Pharmacol 149:159–163
Beardsley PM, Balster RL, Harris LS (1986) Self-administration of MDMA by rhesus monkeys. Drug Alcohol Depend 18:149–157
Bilsky EJ, Hui Y, Hubbell CL, Reid LD (1990) Methylenedioxymethamphetamine’s capacity to establish place preferences and modify intake of an alcoholic beverage. Pharmacol Biochem Behav 37:633–638
Bilsky EJ, Hubbell CL, Delconte JD, Reid LD (1991) MDMA produces a conditioned place preference and elicits ejaculation in male rats: a modulatory role for the endogenous opioids. Pharmacol Biochem Behav 40:443–447
Bilsky EJ, Montegut MJ, Nichols ML, Reid LD (1998) CGS 10746B, a novel dopamine release inhibitor, blocks the establishment of cocaine and MDMA conditioned place preferences. Pharmacol Biochem Behav 59:215–220
Braida D, Sala M (2002) Role of the endocannabinoid system in MDMA intracerebral self-administration in rats. Br J Pharmacol 136:1089–1092
Callaway CW, Wing LL, Geyer MA (1990) Serotonin release contributes to the locomotor stimulant effects of 3,4-methylenedioxymethamphetamine in rats. J Pharmacol Exp Ther 254:456–464
Camí J, Farré M, Mas M, Roset, PN, Poudevida S, Mas A, San L, de la Torre R (2000) Human pharmacology of 3,4-methylenedioxymethamphetamine (“Ecstasy”): psychomotor performance and subjective effects. J Clin Psychopharmacol 20:455–466
Chen J, Paredes W, Li J, Smith D, Lowinson J, Gardner EL (1990) Delta9-tetrahydrocannabinol produces naloxone-blockade enhancement of presynaptic basal dopamine efflux in nucleus accumbens of conscious, freely-moving rats as measured by intracerebral microdialysis. Psychopharmacology 102:156–162
Colado MI, O’Shea E, Granados R, Esteban B, Martin AB, Green AR (1999) Studies on the role of dopamine in the degeneration of 5-HT nerve endings in the brain of Dark Agouti rats following 3,4-methylenedioxymethamphetamine (MDMA or ‘ecstasy’) administration. Br J Pharmacol 126:911–924
Gold LH, Koob GF (1988) Methysergide potentiates the hyperactivity produced by MDMA in rats. Pharmacol Biochem Behav 29:645–648
Gold LH, Hubner CB, Koob GF (1989) A role for the mesolimbic dopamine system in the psychostimulant actions of MDMA. Psychopharmacology 99:40–47
Gouzoulis-Mayfrank E, Daumann J, Tuchtenhagen F, Pelz S, Becker S, Kunert HJ, Fimm B, Sass H (2000) Impaired cognitive performance in drug free users of recreational ecstasy (MDMA). J Neurol Neurosurg Psychiatry 68:719–725
Greer G, Tolbert R (1986) Subjective reports of the effects of MDMA in a clinical setting. J Psychoactive Drugs 18:319–327
Hammersley R, Ditton J, Smith I, Short E (1999) Patterns of ecstasy use by drug users. Br J Criminol 39:625–647
Harris GC, Hedaya MA, Pan WJ, Kalivas, P (1996) B-adrenergic antagonism alters the behavioral and neurochemical responses to cocaine. Neuropsychopharmacology 14:195–204
Kankaanpää A, Meririnne E, Lillsunde P, Seppala T (1998) The acute effects of amphetamine derivatives on extracellular serotonin and dopamine levels in rat nucleus accumbens. Pharmacol Biochem Behav 59:1003–1009
Koob GF, Le Moal M (2001) Drug addiction, dysregulation of reward, and allostasis. Neuropsychopharmacology 24:97–129
Lamb RJ, Griffiths RR (1987) Self-injection of (d,l)-3,4-methylenedioxymethamphetamine (MDMA) in the baboon. Psychopharmacology 91:268–272
Lin HQ, Burden PM, Christie MJ, Johnston GA (1999) The anxiogenic-like and anxiolytic-like effects of MDMA on mice in the elevated plus-maze: a comparison with amphetamine. Pharmacol Biochem Behav 62:403–408
Logan BJ, Laverty R, Sanderson WD, Yee YB (1988) Differences between rats and mice in MDMA (methylenedioxymethylamphetamine) neurotoxicity. Eur J Pharmacol 152:227–234
Maldonado E, Navarro JF (2000) Effects of 3,4-methylenedioxy-methamphetamine (MDMA) on anxiety in mice tested in the light-dark box. Prog Neuropsychopharmacol Biol Psychiatry 24:463–472
Maldonado R, Blendy JA, Tzavara E, Gass P, Roques BP, Hanoune J, Schutz G (1996) Reduction of morphine abstinence in mice with a mutation in the gene encoding CREB. Science 273:657–659
Maldonado R, Saiardi A, Valverde O, Samad TA, Roques BP, Borrelli E (1997) Absence of opiate rewarding effects in mice lacking dopamine D2 receptors. Nature 388:586–589
Marona-Lewicka D, Rhee GS, Sprague JE, Nichols DE (1996) Reinforcing effects of certain serotonin-releasing amphetamine derivatives. Pharmacol Biochem Behav 53:99–105
Meyer A, Mayerhofer A, Kovar KA, Schmidt WJ (2002) Rewarding effects of the optical isomers of 3,4-methylenedioxy-methylamphetamine (‘Ecstasy’) and 3,4-methylenedioxy-ethylamphetamine (‘Eve’) measured by conditioned place preference in rats. Neurosci Lett 330:280–284
O’Shea E, Esteban B, Camarero J, Green AR, Colado MI (2001) Effect of GBR 12909 and fluoxetine on the acute and long term changes induced by MDMA (ecstasy) on the 5-HT and dopamine concentrations in mouse brain. Neuropharmacology 40:65–74
Paxinos G, Franklin KBJ (1997) The mouse brain in stereotaxic coordinates. Academic, San Diego
Peroutka SJ, Newman H, Harris H (1988) Subjective effects of 3,4-methylenedioxymethamphetamine in recreational users. Neuropsychopharmacology 1:273–277
Pontieri FE, Tanda G, Orzi F, Di Chiara G (1996) Effects of nicotine on the nucleus accumbens and similarity to those of addictive drugs. Nature 18:255–257
Ratzenboeck E, Saria A, Kriechbaum N, Zerning G (2001) Reinforcing effects of MDMA (‘Ecstasy’) in drug-naive and cocaine-trained rats. Pharmacology 62:138–144
Reneman L, Booij J, Schmand B, Van den Brink W, Gunning B (2000) Memory disturbances in “Ecstasy” users are correlated with an altered brain serotonin neurotransmission. Psychopharmacology 148:322–324
Ryan RE, Ross SA, Drago J, Loiacono RE (2001) Dose-related neuroprotective effects of chronic nicotine in 6-hydroxydopamine treated rats, and loss of neuroprotection in α4 nicotinic receptor subunit knockout mice. Br J Pharmacol 132:1650–1656
Salzmann J, Marie-Claire C, Le Guen S, Roques BP, Noble F (2003) Importance of ERK activation in behavioral and biochemical effects induced by MDMA in mice. Br J Pharmacol 140:831–838
Schechter MD (1991) Effect of MDMA neurotoxicity upon its conditioned place preference and discrimination. Pharmacol Biochem Behav 38:539–544
Stone DM, Hanson GR, Gibb JW (1987) Differences in the central serotonergic effects of methylenedioxymethamphetamine (MDMA) in mice and rats. Neuropharmacology 26:1657–1661
Topp L, Hando J, Dillon P, Roche A, Solowij (1999) Ecstasy use in Australia: patterns of use and associated harm. Drug Alcohol Depend 55:105–115
Von Sydow K, Lieb R, Pfister H, Höfler M, Wittchen HU (2002) Use, abuse and dependence of ecstasy and related drugs in adolescents and young adults—a transient phenomenon? Results from a longitudinal community study. Drug Alcohol Depend 66:147–159
White SR, Obradovic T, Imel KM, Wheaton MJ (1996) The effects of methylenedioxymethamphetamine (MDMA, “Ecstasy”) on monoaminergic neurotransmission in the central nervous system. Prog Neurobiol 49:455–479
Yamamoto BK, Spanos LJ (1988) The acute effects of methylenedioxymethamphetamine on dopamine release in the awake-behaving rat. Eur J Pharmacol 148:195–203
Yokel RA, Wise RA (1975) Increased lever pressing for amphetamine after pimozide in rats: implications for a dopamine theory or reward. Science 187:547–549
Yoshimoto K, McBride WJ, Lumeng L, Li TK (1992) Alcohol stimulates the release of dopamine and serotonin in the nucleus accumbens. Alcohol 9:17–22
Acknowledgements
This work was supported by FIS grant number 01/1325, HFSO, Ministerio de Educación, Cultura y Deporte (SB2000–0019), Distinción de la Generalitat de Catalunya, Generalitat de Catalunya 2002SGR00193, Plan Nacional sobre Drogas, and Marató de TV3. PR is supported by a FIS investigator contract. GB is supported by Fundación Carolina. We would like to thank Ms. Raquel Martín for her expert assistance in the behavioural experiments, and Ms. Araceli Cabrero for her assistance in the histological procedures.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Robledo, P., Balerio, G., Berrendero, F. et al. Study of the behavioural responses related to the potential addictive properties of MDMA in mice. Naunyn-Schmiedeberg's Arch Pharmacol 369, 338–349 (2004). https://doi.org/10.1007/s00210-003-0862-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-003-0862-9