Abstract
The kinetic analysis of esterase inhibition by acylating compounds (organophosphorus carbamates and sulfonyl fluorides) is sometimes unable to yield consistent results by fitting simple inhibition kinetic models to experimental data of complex systems. In this work, kinetic data were obtained for phenylmethylsulfonyl fluoride (PMSF) tested at different concentrations incubated for up to 3 h with soluble fraction of chicken peripheral nerve. PMSF is a protease and esterase inhibitor causing protection or potentiation of the organophosphorus-induced delayed neuropathy and is unstable in water solution. The target of the promotion effect was proposed to be a soluble esterase not yet identified. A kinetic model equation was deduced assuming a multienzymatic system with three different molecular phenomena occurring simultaneously: (1) inhibition, (2) spontaneous chemical hydrolysis of the inhibitor and (3) ongoing inhibition (inhibition during the substrate reaction). A three-dimensional fit of the model was applied for analyzing the experimental data. The best-fitting model is compatible with a resistant component (16.5–18%) and two sensitive enzymatic entities (both 41%). The corresponding second-order rate constants of inhibition (ki = 12.04 × 10−2 and 0.54 × 10−2 μM−1 min−1, respectively) and the chemical hydrolysis constant of PMSF (kh = 0.0919 min−1) were simultaneously estimated. These parameters were similar to those deduced in fixed-time inhibition experiments. The consistency of results in both experiments was considered an internal validation of the methodology. The results were also consistent with a significant ongoing inhibition. The proportion of enzymatic components showed in this work is similar to those previously observed in inhibition experiments with mipafox, S9B and paraoxon, demonstrating that this kinetic approach gives consistent results in complex enzymatic systems.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Discrimination of esterases in tissue preparations has been achieved on the basis of their different sensitivities to inhibition by organophosphorus compounds (OPs) and other inhibitors. One of the best known examples is the operative discrimination of the so-called neuropathy target esterase (NTE) from other esterases in both neural and extraneural tissues. NTE is operationally defined as the fraction of phenylvalerate esterase (PVase) activity, which is resistant to paraoxon (40 μM), but sensitive to mipafox (50 μM), 20 min at 37°C (Johnson 1969, 1977). Brain NTE is selectively inhibited by 1-(saligenin cyclic phospho)-9-biotinyldiaminononane (S9B), which was the basis to the isolation of NTE and to its molecular and genomic characterization (Lush et al. 1998; Glynn et al. 1999; Kropp et al. 2004).
Some sulfonyl fluorides, such as phenylmethylsulfonyl fluoride (PMSF), can also covalently and irreversibly inhibit NTE without inducing neuropathy. In fact when given to hens at doses that block (inhibit) more than 30–40% of NTE, they protect against the neurotoxic effect of a subsequent high neuropathic dose of a neuropathic OP (Johnson 1987). However, when “protective” NTE inhibitors such as PMSF are dosed after a low non-neuropathic dose of a neuropathic OP (causing >40–50% NTE inhibition), its neurotoxicity is “potentiated” (Pope and Padilla 1990) or “promoted” (Lotti et al. 1991), causing severe neuropathy. Although the target of “potentiation” by PMSF remains unknown, it is suspected to be another esterase related to peripheral nerve soluble PVases (Moretto 2000; Moretto et al. 2001). However, the global interaction of PMSF with nerve tissue esterases has not been kinetically analyzed in detail, and it is necessary to identify which are the relevant sensitive esterases to PMSF as possible target(s) for promotion/potentiation of organophosphorus-induced delayed polyneuropathy (OPIDP) before isolation and molecular characterization. This is precisely the purpose of the present work.
The kinetic analysis of the inhibition of esterases by acylating compounds (organophosphates, carbamates and sulfonyl fluorides) is sometimes unable to yield consistent results by fitting simple inhibition kinetic models to the experimental data in complex systems. An additional problem for kinetic studies with PMSF comes its instability in aqueous solutions due to spontaneous chemical hydrolysis (James 1978), and an additional hydrolysis caused by the biological medium cannot be ruled out. One important contribution of this paper is the introduction of the hydrolysis of the inhibitor in the kinetic models for the inhibition process.
In vitro experiments involve pre-incubating the enzyme preparation with an inhibitor concentration (I) during increasing inhibition times (t) and then incubating with a substrate during the enzyme–substrate reaction time (ts) to measure residual enzyme activity (E) (Fig. 1). Model equations and approaches for analyzing the kinetic behavior of multienzymatic systems in the presence of an inhibitor, either with or without spontaneous reactivation, have been recently reviewed (Estévez and Vilanova 2009). However, the spontaneous hydrolysis of the inhibitor has not yet been included in inhibition kinetic models. Usually, the kinetic model assumes that inhibitor concentrations remain constant while the experiment is underway because the inhibitor is tested at least at nano- or micromolar concentrations, while the tested enzyme should be within pico- or femtomolar concentrations. A proposed model equation can only be accepted when different inhibitor concentrations are assayed and if consistent results are obtained as follows: the best-fitting model possesses the same number of components with the same amplitudes and kinetic constants for each tested inhibitor concentrations (Estévez and Vilanova 2009).
Typical timing in an inhibition experiment. Enzyme preparation is treated with an inhibitor (PMSF) (first vertical arrow) and is pre-incubated during the “inhibition time” (ti). Then, the substrate is added (PV) (second vertical arrow) and incubated during the “substrate time” (ts) to allow the substrate–enzyme reaction to measure the residual active enzyme. Finally, the reaction with the substrate is stopped (third vertical arrow) by adding SDS/AAP solution, and a color reagent is added before measuring absorbance. Activity is referred to as a percentage over the absorbance of the enzyme preparation without an inhibitor. The addition of a substrate usually stops inhibition due to dilution and competitive substrate protection, but in some cases, some “ongoing inhibition” may occur during the ts
The data of this work were obtained in peripheral nerve of chicken because this is the animal model used for testing and predicting organophosphorus-induced delayed neuropathy in humans (OECD 418 and 419 testing guide) and it is the classical animal model in studies of OPIDP and the first animal model in which NTE (the target protein of OPIDP) was found among the esterases of brain membranes (Johnson 1969, 1982; Williams and Johnson 1981). The in vivo promotion/potentiation effect of PMSF and other promoters has been also assayed in chicken. Chicken tissues also were chosen as the model system given the extensive studies performed on chicken brain and peripheral nerve using paraoxon, mipafox (Barril and Vilanova 1997; Barril et al. 1999) and others inhibitors and because chicken is a highly sensitive species to OPs for both cholinergic and delayed neuropathy effects.).
Highly sensitive esterases to paraoxon have been described and kinetically characterized in the soluble fraction of chicken peripheral nerve as measured with the substrate phenylvalerate (Barril et al. 1999; Estévez et al. 2010). Kinetic behavior was characterized by a transitory inhibition with spontaneous reactivation, which had been also observed in cholinesterases (Eyer et al. 2008; Bazire et al. 2011). It has been suggested that these esterases play potential roles in toxicity and/or detoxication during low-dose long-term exposure to organophosphorus compounds, which warrants further toxicological and epidemiological research (Barril et al. 1999; Estévez et al. 2011). Such esterases are sensitive to the permanent inhibition by mipafox (Estévez et al. 2004) and also to S9B (Estévez et al. 2010), a biotinylated OP used for the detection, labeling and isolation of NTE (Glynn et al. 1994).
On the other hand, the target of promotion of OPIDP was proposed to be in the soluble fraction of peripheral nerve (Gambalunga et al. 2010).
This paper deals with the interaction of PMSF with all esterases in the soluble fraction of chicken peripheral nerve that can be detected with phenylvalerate used as the substrate, but neither deals with OPIDP directly nor studies NTE, which is a membrane-bound protein. A kinetic model has been developed that considers (1) a complex multienzymatic system, (2) the inhibition process (sulfonylation) and (3) the concurrent hydrolysis of PMSF together with an ongoing inhibition during the substrate reaction for the most sensitive enzymatic component. These assumptions are based on the experimental behavior observed, and the results are compared with those obtained with several other OP inhibitors.
Materials and methods
Chemicals
Phenylmethylsulfonyl fluoride (PMSF) was obtained from Sigma–Aldrich S.A. (Madrid, Spain), and phenylvalerate was purchased from Lark Enterprise (Webster, MA, USA). A stock solution of 50 mM PMSF was prepared in DMSO and dissolved in 50 mM Tris–HCl buffer (pH 8.0) containing 1 mM EDTA immediately before the kinetic assays. A stock solution of substrate phenylvalerate (16.8 mM) was prepared in dried N,N-dimethylformamide and diluted in water to 5.4 mM immediately before the enzymatic assays. All the other chemicals were of analytical reagent grades. Sodium dodecyl sulfate [SDS)/4-aminoantipyrine (74.5 mM/1.23 mM)] was prepared in water and stored in a dark bottle. Potassium hexacyanoferrate III (12.1 mM) was prepared in water.
Preparation of the soluble fraction of chicken peripheral nerve
A soluble fraction of sciatic nerves of chicken legs was prepared as described by Estévez et al. (2004). In short, hen sciatic nerves were obtained from a commercial slaughtering house and kept in cold (0–5°C) Tris buffer until use (before 1 h). The tissue was cleaned of fat and blood. The sciatic nerve was homogenized with a Polytron homogenizer (Kinematica Gmbh, Germany) using a PTA 10 s head at 70% speed (3 times × 30 s) in Tris buffer at a concentration of 200 mg fresh tissue/ml. Then, particulate and soluble fractions were separated by ultracentrifugation at 100,000×g for 60 min at the 200 mg concentration of fresh tissue per milliliter in 50 mM Tris–HCl buffer (pH 8.0) containing 1 mM EDTA. For the inhibition process, this fraction was either concentrated or diluted with buffer (1/20) to obtain the desired concentration.
Standard phenylvalerate esterase activity (PVase) assay
Enzyme assays were carried out as previously described (Estévez et al. 2004) following a procedure based on the colorimetric method for the NTE assay, developed by Johnson (1977), using phenylvalerate (PV) as a substrate. One milliliter of tissue preparation and 0.1 ml of inhibitor (buffer in controls) at the appropriate concentration were pre-incubated for the corresponding time and then incubated with 1 ml of substrate (phenylvalerate 0.54 mM) for 10 min. The reaction was stopped by adding 1 ml of a 2% SDS solution with 1.23 mM aminoantipyrine and 0.5 ml of 12.1 mM potassium hexacyanoferrate III. After 10 min, absorbance was read at 510 nm. Blanks and spontaneous hydrolysis controls (samples without tissue) were included in the same procedure.
Inhibition procedure
The PMSF inhibition kinetic data were analyzed in a peripheral nerve soluble fraction at 37°C. A 1-ml volume of peripheral nerve soluble fraction (at an equivalent concentration of 20 mg ml−1 of original fresh tissue) was incubated with 100 μl PMSF to reach the indicated PMSF concentrations at 37°C for the inhibition time indicated in each experiment. Then, the substrate was added and incubated for 10 min to measure residual enzymatic activity, following the procedure described by Johnson (1977), which was modified by Estevez et al. (2004). The residual PMSF concentration in the presence of PV was 0.52 of the initial concentration. The reaction was stopped; the results were expressed as percentage of activity (E/E 0 × 100) over the control without an inhibitor and were plotted versus the time (t) for each data set for the respective inhibitor concentration. Figure 1 shows the scheme of the inhibition procedure.
Kinetics of reactivation after removing PMSF by ultrafiltration
Inhibition and removal procedure: a 1.5-ml volume containing the soluble fraction corresponding to 200 mg fresh tissue/ml was incubated with 80 μM of PMSF for 30 min at 37°C in a total volume of 1.65 ml. Controls were incubated only with buffer, and the sample was incubated with PMSF. Both the non-inhibited control and the pre-inhibited samples were diluted to 15 ml with cold buffer to be then subjected to two washes through Millipore ultrafree-15 biomax 50 K (15 ml) filters by centrifuging at 1,500–2,000×g and at 4°C. Centrifugation continued until the sample volume was reduced to 0.15 ml. Concentrates were diluted to 15 ml with cold buffer and filtered as before. At the end of the process, buffer was added to obtain the sample concentration used in the PVase assay (soluble fraction from 20 mg of fresh tissue/ml). The PVase activity lost in the process was around 23–25%. The residual PMSF concentration was negligible (from the above-indicated volumes, estimated to be approximately 7.2 nM) and was therefore unable to significantly inhibit the remaining enzyme activity. This residual concentration was estimated from two concentration steps at 0.15 ml and three dilution steps at 15 ml. At the end of first step (one dilution at 15 ml, one concentration at 0.15 ml and one dilution at 15 ml), the residual concentration was estimated to be 720 nM and to be 7.2 nM at the end of second step (one concentration at 0.15 ml and one dilution at 15 ml). Moreover, the actual concentration is much lower due to the spontaneous hydrolysis of PMSF.
Reactivation: after diluting, ultrafiltrated samples were incubated at 37°C, and 1 ml aliquots were taken at 0 min, 30 min and overnight (14 h and 27 min) to allow for reactivation. The results are expressed as percentage of activity (E/E 0 × 100) over the control without the inhibitor.
Computerized estimation of the kinetic parameters
Model equations were fitted to the experimental inhibition kinetic data by a non-linear computerized method based on the least-square principle using the Sigma Plot software, versions 6 and 8. Equations were applied, and fits were fulfilled according to the software user’s guide.
Model equation for inhibition
Model equations were applied according to the recommendations provided in previous publications (Estévez and Vilanova 2009).
In short, the concentration of a reversible non-covalent Michaelis-like intermediate is considered negligible in this paper as the low solubility of the inhibitor does not allow concentrations to cause significant saturation (Aldridge and Reiner 1972) and because similar values of residual activity were obtained in inhibited samples when the inhibitor is in the medium during the substrate reaction in comparison with inhibited samples where the inhibitor is removed. This supports the approach of using kinetic models considering that the concentration of reversible Michaelis-like intermediate is negligible. The reaction may be expressed as follows:
For the case of PMSF, the meaning of PX, E–P and X is described in Fig. 2.
The expected kinetic equation is as follows:
In a biological preparation, esterase activity may contain several sensitive enzymatic fractions (E1, E2, E3, etc.), as well as a resistant component (E R). For example, given a situation of two sensitive enzymatic fractions (exponential components) and a resistant component, the model equation is expressed as follows:
where k1 and k2 are the second-order rate constants; E10 and E20 are the amplitude or proportion of the enzymatic sensitive components at the initial time; a1 and a2 are the parameters involving the rate constant and the inhibitor concentration (a1 = k1·I and a2 = k2·I); and E R is the resistant component. To properly fit the model to the experimental data, the following restrictions are applied: all the parameters are positive (k1, k2, E10, E20, E R > 0) and E10 + E20 + E R = 100%.
In a simple classical irreversible inhibition mechanism by organophosphorylation or organosulfonylation (reaction [1]), an exponential decay (Eq. 1a, 1b) is expected with lines of E versus t lowering to the same residual level. The decay rate depends on the inhibitor concentration (PX or I), but long-term tendency is at the same residual level. This tendency is expected to be zero if all the activity is sensitive or to be at the residual level if a fraction of activity is resistant to the inhibitor.
This model has been extended to consider not only a multienzymatic system with a significant spontaneous reactivation of the inhibited enzyme, but also possible interference, which is the most sensitive component undergoing additional “ongoing inhibition” during the substrate reactions according to Estevez and Vilanova (2009). These additional considerations are provided in detail in the "Results" section.
Results
PMSF inhibition and reactivation on the esterases of peripheral nerve soluble fraction
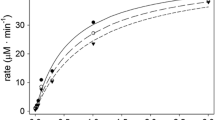
Figure 3 illustrates a fixed-time inhibition curve where around 90% of activity is inhibited at 30 min with 500 μM of PMSF and around 50% inhibition is obtained at 4–6 μM.
PMSF fixed-time inhibition curve of the phenylvalerate esterase activity of the peripheral nerve soluble fraction. Activity was assayed as described in the “Materials and methods” section using a preparation containing the soluble fraction of 20 mg fresh tissue/ml that was pre-incubated with 0, 0.2, 0.6, 0.8, 1, 2, 4, 6, 8, 10, 20, 40, 60, 80, 100 and 500 μM PMSF for 30 min. Then, the enzymatic activity was assayed with phenylvalerate for 10 min. Percentages refer to the activity of the sample pre-incubated with 0 μM PMSF. The curve was fitted with exponential model equations by selecting the best-fitting multiexponential equation according to the F test
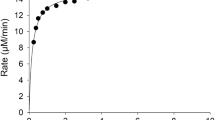
Inhibition of peripheral nerve soluble PVase activity with PMSF shows a time-progressive inhibition, which is coherent with covalent irreversible inactivation. Figure 4 presents the curves corresponding to the best fit according to the F test of the individual curve for each PMSF concentration used. For a long inhibition time, curves do not converge at the same residual activity point, but show a parallel line tendency at a given level depending on the inhibition concentration being used.
Kinetics of the time-progressive inhibition at different PMSF concentrations. PVase activity was assayed as described in the “Materials and methods” section using a preparation containing the soluble fraction of 20 mg fresh tissue/ml that was pre-incubated with 0, 0.2, 0.8, 4 and 10 μM PMSF (upper to lower plots) at the indicated times. Then, enzymatic activity was assayed with phenylvalerate for 10 min. Percentages refer to the activity of the samples pre-incubated with 0 μM PMSF at each time. Each curve was fitted with multiexponential model equations by selecting the best-fitting equation according to the F test
Although each curve apparently shows a good, graphical fit with the experimental data, no consistent values for the kinetic constants, numbers and the proportion of the components have been obtained when each curve was separately analyzed to a model with 1, 2, 4 and 5 exponential components (as indicated in “Materials and methods”) when considering only inhibition. Therefore, the data cannot be interpreted with exponential decay models as they consider only the inhibition by sulfonylation reaction. The introduction of two exponential components and/or a resistant component did not improve the consistency of the results and their properties. The number and proportions of sensitive components vary with the inhibition concentration. The first-order constants obtained in the inhibition curves are not linearly dependent on the PMSF concentration, and the values of the second-order kinetic constants are not consistent.
Two possible interpretations of these observations are (a) the spontaneous hydrolysis of PMSF (James 1978) and/or (b) the existence of spontaneous reactivation (Estévez and Vilanova 2009).
No spontaneous reactivation was observed in the peripheral nerve soluble fraction pre-inhibited with PMSF after removing the inhibitor by ultrafiltration. Activity remained inhibited and at same activity level throughout the assay. The values of the residual activity for three independent samples were 16.9, 15.9 and 17.4% at 0 min of reactivation time and 17.7, 17.6 and 17.6% at 867 min of reactivation time. Therefore, no spontaneous reactivation took place, and the kinetic model did not contemplate spontaneous reactivation. The residual activity was 16.3% in the not ultrafiltrated control where the inhibitor was not removed.
Extrapolating the data in Fig. 4 to the pre-incubation zero time did not converge to 100%. This indicates that ongoing inhibition during substrate incubation under the assayed conditions is apparently significant, at least for the highest inhibitor concentrations (4 and 10 μM). Therefore, ongoing inhibition during substrate incubation needs to be considered in the model, at least for the most sensitive components (Estévez and Vilanova 2009; Estévez et al. 2010). This effect is not highly significant as it is only approximately 10% of the highest inhibitor concentration. Nonetheless, it could hinder the data analysis if not considered.
The results of these observations suggest that PMSF interacts with these esterases without spontaneous reactivation and that PMSF is chemically spontaneously hydrolyzed while the experiment lasts. Therefore, the kinetic model needs to consider (a) several components, (b) PMSF hydrolysis and (c) ongoing inhibition.
A kinetic model considering inhibition, the simultaneous hydrolysis of the inhibitor and ongoing inhibition
The reactions to be considered are the following:
where PX is the inhibitor (PMSF in this case), X the leaving group (fluoride in this case) and PO− the other hydrolysis product (phenylmethylsulphonic acid in this case) (Fig. 2).
For a single enzyme component, the deduced model equations are as follows:
where ki is second-order inhibition constant, kh is the chemical hydrolysis constant, E is the free enzyme concentration, PX is the inhibitor concentration, v d E is the enzyme’s disappearance rate, v d PX 2 is the inhibitor’s disappearance rate through Reaction [2] and v d PX 3 is the inhibitor’s disappearance rate inhibitor through Reaction [3].
By considering that the inhibitor’s disappearance rate through Reaction [3] is higher than through Reaction [2], the following approach is applied:
The deduced equations become
By rearranging Eq. 6, it is deduced that
while integrating Eq. 7, we obtain
then
when t = 0, PX = PX 0 (the initial inhibitor concentration). Therefore, A = PX 0 and
By substituting PX (Eq. 8) in Eq. 5, we see that
By rearranging the last equation, we achieve the following:
Then by integrating Eq. 10, we note that
then
when t = 0, E = E 0 (the initial free enzyme concentration). Therefore,
and
By substituting B (Eq. 12) into Eq. 11, we accomplish
When rearranging the last equation, the equation below is obtained for a sensitive enzymatic component:
Analysis of the fixed-time inhibition curve considering the simultaneous hydrolysis of the inhibitor
Models that consider inhibition with a simultaneous spontaneous hydrolysis of the inhibitor were fitted to the PMSF fixed-time inhibition data (Fig. 3). One, two and three sensitive enzymatic components with or without a resistant enzymatic component were used. The model of three sensitive enzymatic components was the best fit according to the F test:
where kh is the spontaneous hydrolysis constant of the inhibitor, E10 is the proportion (amplitude) of the most sensitive enzymatic component, E20 is the proportion (amplitude) of the second most sensitive enzymatic component, E30 is the proportion (amplitude) of the third most sensitive enzymatic component and 30 is the fixed reaction time. The following restriction was applied: E10 + E20 + E30 = 100% and k1, k2, k3, kh, E10, E20 and E30 > 0.
The model describes three sensitive components, E1, E2 and E3 (44, 40 and 17%), with I 50 (30 min) of 0.77, 17.10 and 564 μM, respectively. Table 1 provides the resulting kinetic parameters in line (A). The I 50 (30 min) value of the sensitive component (Ei) was obtained by approximation by applying the following equation:
The previously estimated kinetic constants were fixed, and then successive iterations with different I values were carried out in an electronic spreadsheet to obtain the PX 0 value for the percentage of activity that equals 50 ± 0.1%. Therefore, this I 50 is the initial concentration required for a 50% inhibition in 30 min under the experimental conditions in which the PMSF concentration decreases over time due to hydrolysis.
Analysis of the time-progressive inhibition curves by PMSF
The time-progressive inhibition data were analyzed by considering inhibition with a simultaneous spontaneous hydrolysis of the inhibitor with one, two or three enzymatic components by contemplating the ongoing inhibition effect in the most sensitive component.
It is reasonable to assume that ongoing inhibition is significant only for the most sensitive enzymatic component. Therefore, an additional exponential factor may be applied to the most sensitive component to correct the effect (Estévez and Vilanova 2009; Estévez et al. 2010). This factor is [e–ka′·PX], and it is added in the most sensitive component (E1) equation (see Eq. 14). Parameter ka′ represents the apparent first-order kinetic constant of the observed inhibition without pre-incubation caused by inhibition during the substrate reaction time applied to measure activity. However, this additional factor is also modified because the PX concentration changes during the whole reaction time because of the hydrolysis. Thus, PX = PX 0·e−kh·t (Eq. 8) and the additional exponential factor are reflected as \( {\text{e}}^{{ - ka^{'} \cdot PX_{0} \cdot {\text{e}}^{ - kh \cdot t} }} \) where t is the reaction time.
The model that considers inhibition with a simultaneous spontaneous hydrolysis of the inhibitor was used for one, two and three sensitive enzymatic components with or without a resistant enzymatic component by considering the factor for the “ongoing inhibition” effect in the most sensitive component. The best-fitting model (according to the F test) consisted in two sensitive enzymatic entities plus resistant one:
where k1 and k2 are the inhibition constants, E10, E20 and Er are the proportions (amplitude) of enzymatic components E1, E2 and E3, respectively, kh is the spontaneous hydrolysis constant of the inhibitor and ka′ is the apparent constant of ongoing inhibition.
For the purpose of obtaining a coherent solution in the interactive computing estimation, some restrictions were applied: (1) all the parameters (rate constants and amplitudes) should have positive values (>0); (2) component 1 is the most sensitive; therefore, k1 > k2; and (3) the following complementary restriction was also applied: E10 + E20 + Er = 100%. A three-dimensional fitting (percentage of phenylvalerate esterase activity versus t and I) was performed with the data described in Fig. 4. Table 1 provides the results (line B), and the deduced 3D surface is plotted in Fig. 5. The system allows more than one solution, although this depends on the initial value in the interactive computing estimation. The results were accepted only if the kinetic constants and amplitudes were of the same order of magnitude as in the fixed-time inhibition experiment. The consistency of the results significantly improved (according to the F test) if a correction factor for the ongoing inhibition during the substrate reaction was included in the most sensitive component.
Representation of the inhibition kinetics of soluble peripheral nerve PVases by PMSF. The inhibitory surface obtained by fitting the 3D model equation to all the data corresponding to PMSF inhibition at different concentrations and times. The surface reflects the result of the best model according to the F test. It corresponds to a model with three enzymatic components. Details are provided in “Materials and methods”
Discussion
The soluble peripheral nerve samples and complex kinetic model have been used in this work because the knowledge about the kinetic behavior of the interaction of peripheral nerve soluble esterases with PMSF is necessary in order to identify the relevant carboxylesterases in the potentiation of the delayed neuropathy before purifying them for isolation and molecular identification and characterization.
This paper provides evidence that micromolar concentrations of PMSF, a protease and esterase inhibitor causing both protection and potentiation of the organophosphorus-induced delayed neuropathy, is able to inhibit about 85% of the total soluble phenylvalerate esterases in chicken peripheral nerve (the animal model for predicting OPIDP in humans) in a time-progressive manner, suggesting covalent irreversible binding by sulfonylation. The kinetic behavior is coherent with the existence of two sensitive esterase components plus a resistant one.
The concentration of reversible Michaelis-like complex can be considered negligible in order to simplify the kinetic model because after pre-incubation with 80 μM PMSF for 30 min at 37°C and removing the inhibitor by ultrafiltration, the residual activity was about 17% and was similar to the residual activity of the preinhibited non-ultrafiltrated controls where the inhibitor was not removed. PMSF-inhibited esterases were not reactivated, suggesting permanent covalent binding; therefore, spontaneous reactivation is not considered in the mathematical modeling for inhibition kinetics.
The mathematical equations for a simple kinetic model (E + I → EI) has not proved to be an appropriate data fit in the time-progressive inhibition curves. The curves in Fig. 4 tend to reach a “plateau” and do not converge at the same point, even though no spontaneous reactivation is detected (Estévez and Vilanova 2009).
PMSF is spontaneously hydrolyzed in Tris pH 8.0 solutions (James 1978), which is the most likely cause of these apparent steady states reached at long inhibition times (around 80 min) because PMSF progressively disappears and the inhibition rate decreases until it stops when the inhibitor concentration comes close to zero. Another kinetic model is then required when the esterase inhibition and the spontaneous hydrolysis of PMSF are considered to occur simultaneously. Binding to sensitive esterases is not usually considered to be significant to modify the inhibitor concentrations if it is tested at initial levels from nanomolar concentrations upwards, as individual sensitive active proteins are within a picomolar or femtomolar concentrations. The concentration of active centers is expected to be lower than 0.2–2 nM because the inhibitor S9B is able to inhibit the 50% of the two PMSF-sensitive enzymatic components at these levels of concentration in 30 min (Table 2). PMSF is tested in the time-progressive inhibition study (Fig. 4) at 200, 400, 4,000 and 10,000 nM concentrations; therefore, the PMSF concentrations are at least between 100 and 5,000 times higher than the possible active centers for binding, and consequently, although the binding to proteins cannot be excluded, it is reasonable to consider that the disappearance of PMSF along the time of the experiment is mainly due to the chemical hydrolysis. Therefore, the inhibitor concentration is usually regarded as constant in inhibition studies with organophosphorus compounds. However, it is well known that PMSF is unstable in the aqueous solutions as used in biochemical studies as a serine protease inhibitor. This instability is an advantage when used as a research tool in, for instance, protein purification schemes, because proteases or esterases are permanently inhibited, while the compound disappears from the medium without disturbing further studies with biological preparations.
A reasonable approach which assumes that PMSF’s disappearance due to PVase inhibition is negligible versus PMSF’s chemical hydrolysis was considered in order to solve the differential equations in the kinetic model. The model predicts the same number of components, with equivalents amplitude and kinetic constants between the fixed-time and the time-progressive inhibition experiments (Table 1). The mathematical model applied in this work could be useful for analyzing the inhibition by other compounds that are spontaneously hydrolyzed in studies with esterases and proteases.
A 3D fit is the best tool to fit equations to the time-progressive inhibition data in this complex model (Estévez et al. 2004). Furthermore, it simultaneously takes into account all the data at different concentrations and inhibition times. The “ongoing inhibition” effect is considered for the most sensitive enzymatic component (Estévez and Vilanova 2009; Estévez et al. 2010).
The half-life of 20 μM PMSF was calculated to be about 35 min at pH 8.0 (Tris–HCl, pH 8.0) and 25°C (James 1978). Therefore, the hydrolysis constant at 25°C is estimated to be 0.0198 min−1. For the biological preparations at 37°C in the inhibition experiments, it is estimated to be comparable, but with some higher values (around 0.0919–0.1302 min−1; see Table 1). The higher temperature (37°C) in the assay conditions in addition to a possible enzymatic hydrolysis and/or binding to other esterases or proteins (such as proteases) as well to other biochemical components in the solution may increase the global hydrolysis rate of PMSF in the biological preparations.
Table 1 shows how both the inhibition (and the corresponding I 50 for 30 min) and PMSF hydrolysis constants are consistent between the fixed-time and time-progressive inhibition protocols. The results of the fixed-time experiment (Fig. 3) and the time-progressive inhibition experiment (Fig. 4) must be considered as a whole, although they are two different assays with different designs. Similar kinetic parameters are obtained in these two independent experiments. This is considered as internal validation strongly supporting the value of the results and the applied kinetic model.
In short, it is concluded that the mathematical model developed herein indicates that peripheral nerve soluble PVases with PMSF behave as three different enzymatic entities, two of them are PMSF sensitive of a 41–44% and 40–41% amplitude (I 50 = 0.58–0.77 and 7–17 μM, respectively, for a 30-min incubation time) and that around 16.5–18% of total activity may be considered resistant to the highest tested PMSF concentration in the time-progressive inhibition assay.
The number and amplitudes (proportion) of the activity components obtained with PMSF by 3D fitting in the time-progressive inhibition data and fixed-time inhibition data are equivalent to those obtained for the inhibition with mipafox, paraoxon and S9B in the same fraction and tissue (Estévez et al. 2004, 2010, 2011; Table 2).
However, the relative sensitivity of the time-progressive inhibition components for mipafox, paraoxon, S9B and PMSF differs (Table 2). The first component (EI) is the most sensitive one for PMSF and mipafox, whereas the second component (EII) is the most sensitive one for S9B and paraoxon. Both sensitive components (EI and EII) showed spontaneous reactivation after the inhibition with paraoxon (Estévez et al. 2011), EI is permanently inhibited with S9B, and EII is spontaneously reactivated after the inhibition with S9B (Estévez et al. 2010). The component EI might be related to the so-called soluble NTE (Escudero et al. 1997) because it is permanently inhibited with mipafox, S9B and PMSF but it is spontaneously reactivated after the inhibition by paraoxon.
In any case, both components are highly sensitive enzymes if compared with other esterases as, for example, the neuropathy target esterase bound to brain membranes (Milatovic et al. 1997). The consistency of the results obtained in the experiments performed with PMSF versus those obtained with mipafox, paraoxon and S9B on the same fraction and tissue may be considered as an internal validation of the strategies followed to characterize kinetic behavior.
Enough evidence is available showing that molecular target for the already mentioned potentiation/promotion of neuropathy is not the membrane-bound protein NTE (Milatovic et al. 1997). Such a “promotion/potentiation” phenomenon may be significant for our understanding of the potential neurotoxicological consequences of the exposure to environmental pollutants that are not regarded as neurotoxicants. PMSF is a promoter of delayed neuropathy after systemic (Lotti et al. 1991; Pope and Padilla 1990) or local dosing in the peripheral nerve of a low non-neuropathic dose of neuropathic OP (Carrera et al. 1992), and based on the differential sensitivity to neuropathic versus promoter compounds, some authors have suggested that the molecular target for the potentiation/promotion of neuropathies (such as OPIDP) could be among the PVases present in the soluble fraction of peripheral nerve (Moretto 2000; Gambalunga et al. 2010). This work proves that most soluble PVases of peripheral nerve can be time-progressively inhibited by PMSF in an irreversible and permanent manner. Its chemical insults to these esterases remain after the compound has disappeared from the medium, and the toxicological meaning of such interactions remains unknown. With the results of this work, we now have the appropriate criteria to monitor the isolation of PMSF-sensitive esterases for their further molecular identification and for more robust toxicological studies in order to understand their toxicological involvement through both in vivo and in vitro studies.
References
Aldridge WN, Reiner E (1972) Enzyme inhibitors as substrates. North-Holland, Amsterdam
Barril J, Vilanova E (1997) Reversible inhibition can profoundly mislead studies on progressive inhibition of enzymes: the interaction of paraoxon with soluble neuropathy target esterase. Chem Biol Interact 108:19–25
Barril J, Estévez J, Escudero MA, Céspedes MV, Ñíguez N, Sogorb MA, Monroy A, Vilanova E (1999) Peripheral nerve soluble esterases are spontaneously reactivated after inhibition by paraoxon: implication for a new definition of neuropathy target esterase. Chem Biol Interact 119–120:541–550
Bazire A, Gillon E, Lockridge O, Vallet V, Nachon F (2011) The kinetic study of the inhibition of human cholinesterases by demeton-S-methyl shows that cholinesterase-based titration methods are not suitable for this organophosphate. Toxicol In Vitro 25(3):754–759
Carrera V, Barril J, Mauricio M, Pellín M, Vilanova E (1992) Local application of neuropathic organophosphorus compounds to hen sciatic nerve: inhibition of neuropathy target esterase and peripheral neurological impairments. Toxicol Appl Pharmacol 117(2):218–225
Escudero MA, Céspedes MV, Vilanova E (1997) Chromatographic discrimination of soluble neuropathy target esterase isoenzymes and related phenyl valerate esterases from chicken brain, spinal cord, and sciatic nerve. J Neurochem 68(5):2170–2176
Estévez J, Vilanova E (2009) Model equations for the kinetics of covalent irreversible enzyme inhibition and spontaneous reactivation: esterases and organophosphorus compounds. Crit Rev Toxicol 39(5):427–448
Estévez J, García-Pérez AG, Barril J, Pellín M, Vilanova E (2004) The inhibition of the high sensitive peripheral nerve soluble esterases by mipafox: a new mathematical processing for the kinetics of inhibition of esterases by organophosphorus compounds. Toxicol Lett 151:171–181
Estévez J, Barril J, Vilanova E (2010) Inhibition with spontaneous reactivation and the “ongoing inhibition” effect of esterases by biotinylated organophosphorus compounds: S9B as a model. Chem Biol Interact 187:397–402
Estévez J, García-Pérez A, Barril J, Vilanova E (2011) Inhibition with spontaneous reactivation of carboxyl esterases by organophosphorus compounds: paraoxon as a model. Chem Res Toxicol 24:135–143
Eyer P, Radtke M, Worek F (2008) Reactions of isodimethoate with human red cell acetylcholinesterase. Biochem Pharmacol 75:2045–2053
Gambalunga A, Pasqualato F, Lotti M (2010) Soluble phenyl valerate esterases of hen sciatic nerve and the potentiation of organophosphate induced delayed polyneuropathy. Chem Biol Interact 187:340–343
Glynn P, Read DJ, Guo R, Wylie S, Johnson MK (1994) Synthesis and characterization of a biotinylated organophosphorus ester for detection and affinity purification of a brain serine esterase: neuropathy target esterase. Biochem J 301:551–556
Glynn P, Read DJ, Lush MJ, Li Y, Atkins J (1999) Molecular cloning of neuropathy target esterase (NTE). Chem Biol Interact 119–120:513–517
James GT (1978) Inactivation of the protease inhibitor phenylmethylsulfonyl fluoride in buffers. Anal Biochem 86(2):574–579
Johnson MK (1969) The delayed neurotoxic effect of some organophosphorus compounds. Identification of the phosphorylation site as an esterase. Biochem J 114:711–717
Johnson MK (1977) Improved assay of neurotoxic esterase for screening organophosphates for delayed neurotoxicity potential. Arch Toxicol 37:113–115
Johnson MK (1982) The target for initiation of delayed neurotoxicity by organophosphorus esters: biochemical studies and toxicological applications. Rev Biochem Toxicol 4:141–212
Johnson MK (1987) Receptor or enzyme: the puzzle of NTE and organophosphorus-induced delayed polyneuropathy target esterase of hen brain. Trends Pharmacol Sci 8:174–179
Kropp TJ, Glynn P, Richardson RJ (2004) The mipafox-inhibited catalytic domain of human neuropathy target esterase ages by reversible proton loss. Biochemistry 43(12):3716–3722
Lotti M, Caroldi S, Capodicasa E, Moretto A (1991) Promotion of organophosphate-induced delayed polyneuropathy by phenylmethanesulfonyl fluoride. Toxicol Appl Pharmacol 108:234–241
Lush MJ, Li Y, Read DJ, Willis AC, Glynn P (1998) Neuropathy target esterase and a homologous Drosophila neurodegeneration-associated mutant protein contain a novel domain conserved from bacteria to man. Biochem J 15, 332 (Pt 1):1–4
Milatovic D, Moretto A, Osman KA, Lotti M (1997) Phenyl valerate esterases other than neuropathy target esterase and the promotion of organophosphate polyneuropathy. Chem Res Toxicol 10:1045–1048
Moretto A (2000) Promoters and promotion of axonopaties. Toxicol Lett 112(113):17–21
Moretto A, Gardiman G, Panfilo S, Colle MA, Lock EA, Lotti M (2001) Effects of S-ethyl hexahydro-1H-azepine-1-carbothioate (molinate) on di-n-butyl dichlorovinyl phosphate (DBDCVP) neuropathy. Toxicol Sci 62(2):274–279
Pope CN, Padilla S (1990) Potentiation of organophosphorus-induced delayed neurotoxicity by phenylmethylsulfonyl fluoride. J Toxicol Environ Health 31:261–273
Williams DG, Johnson MK (1981) Gel electrophoretic identification of hen brain neurotoxic esterase labeled with tritiated diisopropylphosphofluridate. Biochem J 199(2):323–333
Conflict of interest
The authors declare that there are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Estévez, J., Barril, J. & Vilanova, E. Kinetics of inhibition of soluble peripheral nerve esterases by PMSF: a non-stable compound that potentiates the organophosphorus-induced delayed neurotoxicity. Arch Toxicol 86, 767–777 (2012). https://doi.org/10.1007/s00204-012-0817-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00204-012-0817-3