Abstract
To review epidemiologic evidence on maternal exposure to particulate matter and adverse pregnancy outcomes, we performed a MEDLINE search of the literature up to June 2009. We considered all original studies published in English including information on total suspended particles (TSP), respirable (PM10) or fine (PM2.5) particles and the risk of preterm birth, low birth weight (LBW) or very low birth weight (VLBW) and small for gestational age (SGA). We identified a total of 30 papers, including 13 with information on preterm birth, 17 on LBW or VLBW, and 4 on SGA. Eight studies on preterm birth, 11 studies on LBW/VLBW and two studies on SGA reported some increased risk (by about 10–20%) in relation to exposure to PM; no meaningful associations was found in the remaining studies. However, even in studies reporting some excess risk, this was inconsistent across exposure levels and pregnancy periods. Epidemiologic studies on maternal exposure to PM during pregnancy thus do not provide convincing evidence of an association with the risk of preterm birth and LBW/VLBW and SGA. The excess risks, if any, are small, and it is unclear whether they are causal, due to misclassification of the exposure or some sources of bias/residual confounding.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Over the last decade, several epidemiologic studies have investigated the relation between air pollution and pregnancy outcomes. The fetus is in fact considered to be highly susceptible to a variety of toxicants, and prenatal exposure to environmental pollutants has been suggested to result in adverse reproductive outcomes (Perera et al. 1999; Triche and Hossain 2007).
With reference to preterm birth and low birth weight (LBW), a few studies published before 2001—and summarized in a few literature reviews—reported an increased risk in relation to exposure to some air pollutants, including particulate matter (PM), sulfur dioxide (SO2), carbon monoxide, nitrogen dioxide and ozone (Glinianaia et al. 2004; Maisonet et al. 2004; Šrám et al. 2005). Inconsistent results were, however, reported for different pollutants and periods of exposure. Moreover, the number of investigations was too limited to draw any definitive conclusion.
To better assess the relation between maternal exposure to air pollution and preterm birth and birth weight, we updated previous reviews on the issue, including epidemiologic studies published throughout middle 2009. In particular, we focused on studies including information on particulate, which is the air pollutant more widely investigated in the epidemiologic literature.
Methods
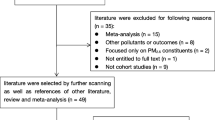
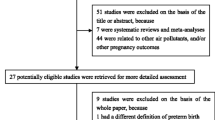
In the present review, we included all original investigations providing information on particulate exposure, measured either as total suspended particles (TSP) (in early publications), PM in aerodynamic diameter <10 μm (PM10), or fine particles in aerodynamic diameter <2.5 μm (PM2.5) and the risk of preterm birth, LBW, very low birth weight (VLBW) or small for gestational age (SGA). To identify the studies, we performed a MEDLINE search of the literature from 1966 to June 2009 using the keywords: “particulate matter” or “air pollution”, and “premature birth” or “preterm birth”, “birth weight”, “low birth weight” or “small for gestational age”. Papers were also searched among those quoted as references in the retrieved studies. We considered all original articles published in English. Among these, a total of 30 papers were identified, including 13 studies with information on preterm birth, 17 studies on LBW or VLBW and 4 studies on SGA. No studies were excluded a priori for weakness of design or data quality. Although we did not assign quality scores to studies, we have underlined some of the limitations and strengths of the studies included.
The main characteristics and results of each study are described in Tables 1–3, including the first author and year of publication, country, design and population of the study, the relative risk (RR) (approximated by the odds ratio, OR, in case–control studies) and 95% confidence intervals (CI) for exposure to TSP, PM10, or PM2.5 in various trimesters of pregnancy, the corresponding level of exposure, confounding factors allowed for in the analyses, and major limitations and strengths. Whenever possible, estimates from single pollutant models and adjustment for various covariates were shown.
Given the large heterogeneity in the published findings—including differences in the study design, methodology of exposure assessment and analyses and particularly in the measures and time windows considered in each study—no overall summary estimates of risk was provided.
Results
Preterm birth
Table 1 gives the main results from 13 studies on PM and preterm birth. In almost all studies, preterm birth was defined as a birth at <37 weeks of gestation; in one study, preterm birth was defined as a birth at <36 weeks of gestation (Sagiv et al. 2005), while in another one births at <30 weeks of gestation were also considered (Brauer et al. 2008). With reference to the pollutants investigated, two studies considered TSP (Bobak 2000; Xu et al. 1995), nine studies considered PM10 (Brauer et al. 2008; Hansen et al. 2006; Jiang et al. 2007; Kim et al. 2007; Lee et al. 2008; Leem et al. 2006; Ritz et al. 2000; Sagiv et al. 2005; Wilhelm and Ritz 2005), and four studies included information on PM2.5 (Brauer et al. 2008; Huynh et al. 2006; Ritz et al. 2007; Wilhelm and Ritz 2005). Among the main limitations of the studies, there is the selective reporting of time of exposure, since only 2 studies out of 13 provided data for all trimesters of exposure, leaving open the possibility of selective reporting of positive findings. Individual information on covariates was also limited since only a minority (3/13) studies were able to allow for maternal smoking. Moreover, only a limited number of studies were able to adjust for previous LBW or preterm infants.
TSP
Among the investigations which considered TSP, a study conducted on a cohort of 25,370 women from four residential areas in Beijing, China, who gave first live births in 1988, and using a time-series approach, reported a RR of preterm birth of 1.10 for each 100 μg/m3 of TSP and estimated a decrease in the gestation age of 0.042 week for each 100 μg/m3 increase in TSP with a 7-day lag (Xu et al. 1995).
In a Czech study on a cohort of all singleton live births registered in 1990–1991 (N = 78,148), premature birth was associated with TSP exposure during the first trimester of pregnancy (RR = 1.18, for a 50 μg/m3 increase), but less so (and not significantly) for exposures in the second and third trimester (RR = 1.11 and 1.12, respectively) (Bobak 2000).
PM10
With reference to PM10, in a cohort of 97,518 births from Southern California registered between 1989 and 1993, a 16% increase in the risk of preterm birth was reported for a 50 μg/m3 increase in the average level of PM10 during the first month of pregnancy and a 20% increase during the 6 weeks before birth (Ritz et al. 2000). PM10 effects showed no regional pattern, while they were slightly reduced when several covariates (including a measure of tobacco smoking) were taken into consideration.
In a time-series analysis conducted in Pennsylvania on 187,977 singleton births recorded between 1997 and 2001, a non significant increased risk of preterm delivery was observed for exposure to average PM10 in the 6 weeks before birth (RR = 1.07, for a 50 μg/m3 increase) (Sagiv et al. 2005). In the week before birth, a significant association was observed only with 2-day and 5-day lag.
In an extended analysis of the Southern California birth cohort from 1994 to 2000 (Ritz et al. 2000), which examined the risk in relation to varying residential distances from monitoring stations, no significant associations between PM10 exposure and preterm birth were observed for any of the distances considered both for exposures during the first trimester and in the last 6 weeks. The results were comparable using a ZIP-code-level analysis (Wilhelm and Ritz 2005). None of the RR estimates were significant.
A study from Korea on 52,113 singleton births registered in 2001–2002 reported a RR of preterm birth of 1.27 for the highest quartile of exposure to PM10 during the first trimester, but no significant association during the third trimester (RR = 1.09) (Leem et al. 2006).
In 28,200 singleton live births from Brisbane, Australia, during the period 2000–2003, a 15% increased risk of preterm birth was found for exposure to PM10 during the first trimester (particularly during the first month, RR = 1.19), but no significant association was observed for exposure in the last trimester (RR = 1.04) (Hansen et al. 2006).
In a cohort of 1,514 births from Seoul, Korea, between 2001 and 2004, premature birth was non-significantly associated with exposure to PM10 during the third trimester (RR = 1.05, for a 10 μg/m3 increase) (Kim et al. 2007). During the first two trimesters no associations were observed.
A study form Shanghai, China, on 3,346 preterm births occurred in 2004, using a time-series approach, estimated that an increase of PM10 of 10 μg/m3 8 weeks before pregnancy corresponded to a 4.4% increase in preterm birth (95% CI 1.6–7.3) (Jiang et al. 2007). No meaningful increase was, however, observed for exposures 6, 4 or 1 week before birth.
An ecologic study on 482,568 births that occurred between 1988 and 2000 in London, using time-series regression techniques, reported that the risk of preterm birth did not increase with exposure to PM10 (Lee et al. 2008). No risk estimates were provided.
A study on 70,249 births registered between 1999 and 2002 in Vancouver, Canada, which estimated residential exposure to air pollutants using various methods (including nearest, inverse-distance weighting, and temporally adjusted land use regression) reported no consistent association for preterm birth <37 weeks with any of the exposure metrics used, and a non significant RR for preterm birth <30 weeks (RR = 1.13, for an increase in PM10 of 1 μg/m3 using an inverse-distance weighting approach) (Brauer et al. 2008).
PM2.5
With reference to PM2.5, in the birth cohort from Southern California, a non significant increase in the risk of preterm birth was observed for exposure during the last 6 weeks of pregnancy in women residing within a 1-mile distance of a monitoring station (RR = 1.25, for exposure ≥24.1 μg/m3), but not for women residing at larger distances (Wilhelm and Ritz 2005). In the first trimester, however, inverse associations for exposure to PM2.5 were observed for various distances considered.
A case–control study on 10,673 preterm births and 32,019 matched controls born in California in 1999–2000 found an OR of 1.15 for an increase of 10 μg/m3 during the whole pregnancy (Huynh et al. 2006). Similar results were found for exposures during the first trimester (RR = 1.13) and the last 2 weeks (RR = 1.06).
The effect of exposure to PM2.5 on preterm birth was also assessed within a cohort of 58,316 births registered in Los Angeles in 2003 and in a nested case–control sub-sample of 2,543 women with detailed risk factor information (Ritz et al. 2007). The RRs of preterm birth for exposure to PM2.5 > 21.4 μg/m3 in the first trimester were 1.10 in the overall cohort and 1.27 in the sub-sample. In the nested sample, the RR estimates were not materially modified by adjustments for additional factors, such as active and passive smoking, marital status and alcohol consumption (RR = 1.29).
In the cohort of 70,249 births from Vancouver, Canada, the RR of preterm birth <37 weeks was 1.06 for an increase in PM2.5 of 1 μg/m3 using an inverse-distance weighting approach (Brauer et al. 2008). When preterm birth at <30 week was considered, the RR was 1.13 using an inverse-distance weighting approach, and of 1.07 using a temporally adjusted land use regression. The latter estimates were based on a small number of cases and were not significant.
Low birth weight
Table 2 gives the main findings from 17 epidemiologic studies on PM and LBW or VLBW. In most studies, LBW (birth weight <2,500 g) was the outcome studied; 2 studies (Rogers and Dunlop 2006; Rogers et al. 2000) considered VLBW infants (birth weight <1,500 g), and another one considered infants with a birth weight between 2,500 and 3,000 g (Slama et al. 2007). Eleven studies considered also the reduction in birth weight corresponding to a unit increase in the air pollutant studied using linear regression models (Bell et al. 2007; Bobak 2000; Chen et al. 2002; Gouveia et al. 2004; Ha et al. 2001; Kim et al. 2007; Maisonet et al. 2001; Salam et al. 2005; Wang et al. 1997; Yang et al. 2003). As for studies on preterm birth, several of the investigations had major limitations. One study was purely ecologic and could allow for socioeconomic indicators only. Only 8 out of 17 gave risk estimates for all the trimesters of exposure, again leaving open the issue of selective reporting of positive findings. Allowance for smoking was made only in a minority of studies (7/17).
With reference to the pollutant investigated, five studies considered exposure to TSP (Bobak 2000; Bobak and Leon 1999; Ha et al. 2001; Rogers et al. 2000; Wang et al. 1997), 12 exposure to PM10 (Bell et al. 2007; Brauer et al. 2008; Chen et al. 2002; Dugandzic et al. 2006; Gouveia et al. 2004; Kim et al. 2007; Lee et al. 2003; Maisonet et al. 2001; Rogers et al. 2000; Salam et al. 2005; Wilhelm and Ritz 2005; Yang et al. 2003), and three exposure to PM2.5 (Bell et al. 2007; Brauer et al. 2008; Slama et al. 2007).
TSP
Among the investigations which considered TSP, a study on 74,671 women from four residential areas in Beijing, China, who gave first live births between 1988 and 1991, reported an increased risk of LBW for exposure to TSP during the third trimester (RR = 1.10, for a 100 μg/m3 increase), with a significant dose-risk relation (Wang et al. 1997). The estimated reduction in birth weight was, however, only 6.9 g (SE = 1.4 g) for a 100 μg/m3 increase in TSP. Although the authors did not give the results for the second and third trimesters, they stated that small inverse associations with LBW were observed in these periods, too.
In an ecologic study conducted in 45 administrative districts in the Czech Republic in 1986–1988, the RR of LBW was 1.04 (not significant) for a 50 μg/m3 increment in TSP (Bobak and Leon 1999).
In another Czech study including all singleton live births registered in 1990–1991 (N = 108,173), a significant association between exposure to TSP and LBW was observed in each trimester of exposure (RR = 1.15, 1.12 and 1.11 for a 50 μg/m3 increase, respectively) (Bobak 2000). The estimates were slightly attenuated after allowance for gestational age. The mean reduction in weight was 10.8 g (95% CI 3.1–18.4) for each 50 μg/m3 increment in TSP in the first trimester, while results were not provided for the other trimesters.
A population-based case–control study conducted between 1986 and 1988 in the USA, on 143 VLBW babies and 202 controls, which measured air pollutants using an environmental transport modeling, reported an OR of 0.99 for exposures to TSP and SO2 combined between 9.94 and 25.18 μg/m3 as compared to 9.94 μg/m3, of 1.27 for exposures between 25.18 and 56.75 μg/m3, and of 2.88 for exposures >56.75 μg/m3 (>95th percentile) (Rogers et al. 2000).
A study on a group of 276,763 singletons born between 1996 and 1997 in Seoul, Korea found an increased risk of LBW for exposure to TSP in the first trimester (RR = 1.04, for an interquartile increase), but not in the third one (RR = 0.95) (Ha et al. 2001). The mean reduction in weight was 6.1 g (95% CI 3.9–8.3) for an interquartile increase in TSP during the first trimester, while it was not given for trimesters two and three.
PM10
With reference to PM10, a study on 89,557 live births between 1994 and 1996 from six northeastern cities of the USA found no association between exposure to PM10 and term LBW in any of the trimesters of pregnancy (OR = 0.93, 0.93, and 0.96 in the 3 trimesters, respectively, after adjusting for tobacco smoking and various other covariates) (Maisonet et al. 2001). Moreover, linear regression analyses showed that the magnitude of the birth weight reductions was small.
In a study on 36,305 singletons from Washoe County, Nevada, born between 1991 and 1999, PM10 was not significantly related to the risk of LBW after adjustment for tobacco smoking and various other covariates (RR = 1.11, for the highest exposure level) (Chen et al. 2002). A 10 μg/m3 increase in PM10 was, however, associated with a reduction in 10 g in birth weight (SE = 5.2 g).
A reduction in birth weight of 0.52 g (95% CI 0.19–0.85) for a 1 μg/m3 increase of PM10 during the first trimester of pregnancy was reported among 54,624 singletons born between 1995 and 1997 in Taiwan (Yang et al. 2003). No significant reductions in weight were, however, reported in the second and third trimester (0.16 g and 0.33 g, respectively).
In a study from Seoul, Korea—extending a previous one (Ha et al. 2001) through 1998—and including 388,105 singletons, the RR of LBW for exposure to PM10 was 1.03 for the first trimester, 1.04 for the second and 1.00 for the third one (RR = 1.06 for the overall period) (Lee et al. 2003). The mean reduction in birth weight was 19.6 g for an interquartile increase in PM10 during the second trimester, while no results were given for other trimesters.
A study on 179,460 live births from São Paulo, Brazil, during 1997 observed a significant increase in LBW risk in relation to PM10 exposure during the second trimester (RR = 1.25 for the fourth quartile), but not in the first and third one (RR = 1.14 and 0.97, respectively) (Gouveia et al. 2004). A significant reduction in birth weight (13.7 g, 95% CI 0.4–27.0, for each 10 μg/m3 increase) was observed in the first trimester, while a smaller reduction was observed in the second trimester (4.4 g), and an increase in weight was reported in the third trimester (14.6 g).
In the study from southern California that analyzed the risk of pregnancy outcome in relation to varying distances from air monitoring stations, an increased risk of LBW was found in relation to PM10 exposure during the third trimester of pregnancy in women residing within a 1-mile distance from a monitoring station (RR = 1.48, for exposure ≥44.4 μg/m3 as compared to < 33.4 μg/m3) (Wilhelm and Ritz 2005). No significant excess risks were found when the distances between home and monitoring stations were greater nor when a ZIP-code-analysis was performed.
In a group of 6,259 children born in California between 1975 and 1987, no significant excess risk of LBW was reported for an interquartile increase in exposure to PM10 (RR = 1.0, 1.2, and 1.3 for the first, second and third trimester, respectively). A significant reduction in birth weight of 21.7 g (95% CI 1.1–42.2) for an interquartile increase in PM10 during the third trimester was observed (Salam et al. 2005), while weight reductions for exposures during the first and second trimesters, as well as in the entire pregnancy, were smaller and not significant (3.0, 15.7, and 19.9 g, respectively). Moreover, the reduction for exposure in the third trimester was attenuated (10.8 g) and no longer significant after adjustment for O3.
Among 74,284 singleton births between 1988 and 2000 in Nova Scotia, Canada, an increased risk of LBW for exposure to PM10 was observed in the first trimester (RR = 1.09, for an interquartile increase), but not in the second or third trimester (Dugandzic et al. 2006). Moreover, the association in the first trimester was attenuated when birth year was controlled for in the analysis (RR = 1.03).
A further analysis of an US population-based case–control study (Rogers et al. 2000) based on 128 VLBW preterm infants and 197 term infants weighing >2,500 g, reported a non significant association with exposure to PM10 (RR = 1.94, for the fourth quartile of exposure versus the first one) (Rogers and Dunlop 2006). A comparison between 59 VLBW preterm infants appropriate for gestational age with the 197 term infants reported a significant association with exposure to PM10 (OR = 3.68), thus suggesting that the association between PM and LBW was at least in part attributable to an effect of duration of gestation.
In a US study, among 358,504 births from 1999 to 2002, in Massachusetts and Connecticut and the RR of LBW for an interquartile increase in the exposure to PM10 was 1.03, and the corresponding birth weight reduction was 8.2 g (95% CI 5.3–11.1) (Bell et al. 2007). The most relevant change in birth weight was observed during the third trimester.
In the cohort of 1,514 births from Korea, LBW was affected by PM10 exposure during the entire pregnancy (RR = 1.07, 1.07 and 1.05, respectively for a 10 μg/m3 increase in the three trimesters) (Kim et al. 2007). However, none of these findings were significant. Birth weight was reduced by 0.3 g (95% CI −7.3 to 14.5) in the second trimester, 2.1 (95% CI −7.5 to 3.4) in the third one, but it increased by 7.8 g (95% CI 1.2–14.5) in the first trimester.
In the cohort of 70,249 births from Canada, a non significant RR of 1.01 was reported for LBW for an increase of 1 μg/m3 in PM10 (Brauer et al. 2008).
PM2.5
With reference to PM2.5, a study from Munich, Germany, on 1,016 births, using a GIS-based land use regression model, estimated that the prevalence of birth weight <3,000 g increased by 13% for each 1 μg/m3 increase in the exposure to PM2.5 during the whole pregnancy (Slama et al. 2007). Further, LBW prevalence increased by 45% for an increment of 0.5 × 10−5/m in PM2.5 absorbance (a marker of traffic-related air pollution that depends on the blackness of PM2.5). With reference to trimester-specific analyses, a significant association was found with PM2.5 in the third trimester only (prevalence ratio, PR = 1.14), and with PM2.5 absorbance in the second one only (PR = 1.27).
In a US study, the RR of LBW for an interquartile increase in the exposure to PM2.5 during the whole pregnancy was 1.05, with corresponding birth weight reduction in 14.7 g (95% CI 12.3–17.1) (Bell et al. 2007). The most important trimesters for exposure to PM2.5 were the second and the third.
In the cohort of 70,249 births from Vancouver, Canada, a non significant RR of 0.98 was reported for LBW and for an increment of 1 μg/m3 in PM2.5 (Brauer et al. 2008). Similar results were obtained using a temporally adjusted land use regression.
Small for gestational age
Four studies considered SGA births as the outcome of interest (Table 3), defined as a weight more than 2 standard deviations below the mean birth weight according to gestational age in one study (Mannes et al. 2005), as a birth weight below the 10th percentile for age and sex in the cohort in two other studies (Brauer et al. 2008; Hansen et al. 2007), and as birth weight <2,872 g for girls and <2,986 for boys in another one (Parker et al. 2005). Of these studies, three considered also the reduction in birth weight corresponding to a unit increase in the air pollutant studied using linear regression models (Hansen et al. 2007; Mannes et al. 2005; Parker et al. 2005). Three studies included information on PM10, (Brauer et al. 2008; Hansen et al. 2007; Mannes et al. 2005) and 3 on PM2.5 (Brauer et al. 2008; Mannes et al. 2005; Parker et al. 2005).
Among the limitations of those studies, 2/4 gave risk estimates for all the trimesters of exposure and 2/4 allowed for smoking in the analyses.
PM10
With reference to PM10, a group of 138,056 singletons from Sydney, Australia, between 1998 and 2000 reported an inverse association between exposure to PM10 and SGA in the second trimester, with a RR of 1.01 for a 1 μg/m3 increment, and a corresponding birth weight reduction of 2.1 g (95% CI 0.74–3.4) (Mannes et al. 2005). No meaningful associations or weight reductions were found for exposures in the first or the third trimester. Similar findings were reported in a sub-sample of women residing within 5 km from a monitoring station.
In a study from Brisbane, Australia, on 26,617 singletons born between 2000 and 2003, trimester and monthly specific exposures to PM10 were not significantly associated with a reduction in birth weight or an increased risk of SGA (Hansen et al. 2007).
In a cohort of 70,249 births from Canada, a non significant RR of 1.02 for SGA for an increment of 1 μg/m3 in PM10 was reported (Brauer et al. 2008).
PM2.5
With reference to PM2.5, a study from Sydney, Australia, reported a RR for SGA of 1.03 for a 1 μg/m3 increment in PM2.5 exposure in the second trimester, with a corresponding birth weight reduction of 4.1 g (95% CI 1.4–6.8) (Mannes et al. 2005). No significant association or weight reduction was reported for exposures in the first and third trimester. Similar findings were reported in women residing within 5 km from a monitoring station.
In a group of 18,247 singleton births from California between 1999 and 2000, an increased risk of SGA was reported in relation to the exposure to PM2.5 in all the trimesters, the RRs for the highest level of exposure (>18.4 μg/m3) being 1.26, 1.24 and 1.21, respectively (Parker et al. 2005). The corresponding reductions in birth weight were 35.8 g (95% CI 13.3–58.4), 46.6 g (95% CI 24.6–68.6) and 31.6 g (95% CI 11.1–52.0), respectively.
In a cohort of 70,249 births from Vancouver, Canada, a non significant RR of 0.98 was reported for LBW and of 1.02 for SGA for an increment of 1 μg/m3 in PM2.5 (Brauer et al. 2008). Similar results were obtained using a temporally adjusted land use regression.
Discussion
Eight of the 13 studies that considered PM in relation to preterm birth and 11 out of 17 studies that analyzed the relation with LBW reported modest increases in risk (by about 10–20%) in at least one pregnancy period. Although SGA is a better and more sensitive outcome than LBW—which can be due either to a preterm birth or a retarded fetal growth—only limited and inconsistent data are available on SGA.
Most of the studies analyzed PM10, with only a few older studies measuring particulate as TSP and a few others including information on PM2.5. Although TSP, PM10 and PM2.5 are measures of different exposures (in particular PM10 and PM2.5, the former measuring more the resuspension and the latter the exhaust), they are generally positively correlated, and the studies that analyzed both PM10 and PM2.5 did not report meaningfully different estimates for the two pollutants.
Substantial inconsistencies in the trimester-specific results were observed both within and across studies. For preterm birth, two studies reported increased risks in the overall pregnancy period (Brauer et al. 2008; Xu et al. 1995), two studies reported increased risks in the first and third trimester of pregnancy only (Huynh et al. 2006; Ritz et al. 2000), and four other studies reported significant associations only when PM exposure occurred during the first trimester of pregnancy (Bobak 2000; Hansen et al. 2006; Leem et al. 2006; Ritz et al. 2007). Similarly, various studies reported an association between PM and the risk of LBW limited to exposures in the first (Dugandzic et al. 2006; Ha et al. 2001; Lee et al. 2003) or the second trimester (Gouveia et al. 2004; Lee et al. 2003), and a few others found significant associations only for exposures during the third trimester (Slama et al. 2007; Wang et al. 1997; Wilhelm and Ritz 2005). For SGA, one study reported increased risks in all pregnancy trimesters (Parker et al. 2005), and another one in the second trimester only (Parker et al. 2005). Thus, the available epidemiologic evidence does not allow to establish the critical time window, if any, of PM exposure, which is also unclear from a biological point of view. Moreover, most of the studies showed the results for specific trimesters only; thus it is possible that findings for other pregnancy periods were not significant (Boffetta et al. 2008). Given the high number of comparisons performed in each study, some of the trimester-specific associations could be due to chance alone.
Besides the inconsistencies in trimester-specific risk estimates, limitations in the methodologies used to investigate the associations between air pollution and adverse pregnancy outcomes make the interpretations of the published findings uncertain (Ritz and Wilhelm 2008; Slama et al. 2008; Woodruff et al. 2009). One of the main problems is the relatively crude exposure assessment used. In almost all studies conducted so far, exposure to ambient PM has in fact been estimated on the basis of routinely collected data from stationary air pollution monitors in the area closest to the mother’s residence. No additional information was available on the characteristics of the home, as well as on the pattern and duration of the exposure of mothers, a large proportion of who may have moved for part of the day or of the overall pregnancy. Thus, a misclassification of the individual exposure to PM is possible. Only two studies used land use regression models (Brauer et al. 2008; Slama et al. 2007) and another one used an environmental transport modeling (Rogers et al. 2000) to take into account mobility (Nethery et al. 2008).
Most studies controlled for various confounding factors, including maternal and infant characteristics derived from birth certificate records, as well as a few seasonal factors. Only a limited number of studies were able, however, to adjust for other covariates, including in particular tobacco smoking, which is an important determinant of adverse pregnancy outcomes. Tobacco smoking during pregnancy has indeed been associated to a twofold increased risk of LBW, and to a mean reduction in infant weight of about 150–250 g, and environmental tobacco smoking has been associated to a 20% increase of LBW, and to a reduction in weight of about 25–40 g (Andres and Day 2000; Lindbohm et al. 2002; Windham et al. 1999). Tobacco smoking may be indirectly associated to air pollution, since smokers are more likely to have a lower socioeconomic status, and consequently to live in poorer residential areas, characterized by higher levels of air pollution. Among the studies that controlled for maternal tobacco smoking in their analyses (Bell et al. 2007; Brauer et al. 2008; Chen et al. 2002; Dugandzic et al. 2006; Maisonet et al. 2001; Mannes et al. 2005; Ritz et al. 2000; Rogers and Dunlop 2006; Salam et al. 2005; Slama et al. 2007) six did not find an association with PM exposure (Brauer et al. 2008; Chen et al. 2002; Dugandzic et al. 2006; Maisonet et al. 2001; Rogers and Dunlop 2006; Salam et al. 2005) One study reported that the associations were attenuated when a number of covariates (including a measure of tobacco smoking during pregnancy) was taken into consideration (Ritz et al. 2000), although in a detailed interview survey within a subset of the overall cohort, smoking and other potential confounders did not show a large impact on the relation between PM and preterm birth (Ritz et al. 2007). Moreover, a study of the potential confounding effect of smoking reported that maternal tobacco smoking did not confound the association between PM and infant mortality (Darrow et al. 2006).
Furthermore, no adjustment has been made for maternal nutrition before and during pregnancy, which has been recently suggested to be a potentially important confounding factor of the association between PM exposure and adverse reproductive outcomes (Kannan et al. 2006).
Confounding from other pollutants is also possible, since the exposure to various air pollutants is likely to occur concomitantly. Although some studies gave the results from multi-pollutants models, the high correlation between various air pollutants makes it difficult to interpret those models and disentangle the effect of each single pollutant.
Several biologic mechanisms by which PM could cause premature births or LBW have been suggested, but none of them has been clearly established. Air pollution may affect maternal respiratory and general health, and in turn cause oxidative stress, inflammatory responses, as well as disturbances of the blood flow (Kannan et al. 2006; Kelly 2003; Peters et al. 1997; Sorensen et al. 2003; Srăm 1999). Moreover, toxic components of PM (which is a complex mixture of a number of components) or other unmeasured compounds which are correlated with PM (such as polycyclic aromatic hydrocarbons, PAHs) absorbed in the maternal bloodstream can affect placental function and directly interfere with the development of the fetus, causing fetal distress, and reducing fetal growth and development (Choi et al. 2006, 2008). Molecular epidemiologic studies have shown increased DNA adducts in maternal blood and placentas in areas with higher pollution, which in turn have been related to increased risk of LBW and preterm birth (Perera et al. 1999).
In conclusion, the results from epidemiologic studies available to date on maternal exposure to PM during pregnancy do not provide convincing evidence of an association with the risk of preterm birth, LBW or SGA. Any association, if any, would be relatively small. The critical time window for the exposure remains also unclear. Moreover, it is unclear whether some of the associations observed in various studies are due to misclassification of the exposure, to some sources of bias or residual confounding not accounted for in the analyses, to selective reporting of positive findings, or the play of chance (Boffetta et al. 2008; Morfeld 2009). Further and better studies are needed to clarify whether there is a real effect of PM on these adverse pregnancy outcomes (Ritz and Wilhelm 2008; Slama et al. 2008; Woodruff et al. 2009). The studies should include: better assessment of exposure using, for example geographic information system techniques, such as land use regression or air dispersion models, which take mobility into account (Nethery et al. 2008); better information on confounders and analyze potential residual confounding; and measurement of biomarkers of exposure or personal exposure monitoring in order to validate exposure estimates. Other studies focused on better outcomes, such as ultrasound measurements during birth (Hansen et al. 2008), may also help understand the effect of air pollution on adverse pregnancy outcomes.
References
Andres RL, Day MC (2000) Perinatal complications associated with maternal tobacco use. Semin Neonatol 5:231–241
Bell ML, Ebisu K, Belanger K (2007) Ambient air pollution and low birth weight in Connecticut and Massachusetts. Environ Health Perspect 115:1118–1124
Bobak M (2000) Outdoor air pollution, low birth weight, and prematurity. Environ Health Perspect 108:173–176
Bobak M, Leon DA (1999) Pregnancy outcomes and outdoor air pollution: an ecological study in districts of the Czech Republic 1986–8. Occup Environ Med 56:539–543
Boffetta P, McLaughlin JK, La Vecchia C, Tarone RE, Lipworth L, Blot WJ (2008) False-positive results in cancer epidemiology: a plea for epistemological modesty. J Natl Cancer Inst 100:988–995
Brauer M, Lencar C, Tamburic L, Koehoorn M, Demers P, Karr C (2008) A cohort study of traffic-related air pollution impacts on birth outcomes. Environ Health Perspect 116:680–686
Chen L, Yang W, Jennison BL, Goodrich A, Omaye ST (2002) Air pollution and birth weight in northern Nevada, 1991–1999. Inhal Toxicol 14:141–157
Choi H, Jedrychowski W, Spengler J, Camann DE, Whyatt RM, Rauh V, Tsai WY, Perera FP (2006) International studies of prenatal exposure to polycyclic aromatic hydrocarbons and fetal growth. Environ Health Perspect 114:1744–1750
Choi H, Perera F, Pac A et al (2008) Estimating individual-level esposure to airbone polycyclic aromatic hydrocarbons throughout the gestational period based on personal, indoor, and outdoor monitoring. Environ Health Perspect 116:1509–1518
Darrow LA, Woodruff TJ, Parker JD (2006) Maternal smoking as a confounder in studies of air pollution and infant mortality. Epidemiology 17:592–593
Dugandzic R, Dodds L, Stieb D, Smith-Doiron M (2006) The association between low level exposures to ambient air pollution and term low birth weight: a retrospective cohort study. Environ Health 5:3
Glinianaia SV, Rankin J, Bell R, Pless-Mulloli T, Howel D (2004) Particulate air pollution and fetal health: a systematic review of the epidemiologic evidence. Epidemiology 15:36–45
Gouveia N, Bremner SA, Novaes HM (2004) Association between ambient air pollution and birth weight in Sao Paulo, Brazil. J Epidemiol Community Health 58:11–17
Ha EH, Hong YC, Lee BE, Woo BH, Schwartz J, Christiani DC (2001) Is air pollution a risk factor for low birth weight in Seoul? Epidemiology 12:643–648
Hansen C, Neller A, Williams G, Simpson R (2006) Maternal exposure to low levels of ambient air pollution and preterm birth in Brisbane, Australia. BJOG 113:935–941
Hansen C, Neller A, Williams G, Simpson R (2007) Low levels of ambient air pollution during pregnancy and fetal growth among term neonates in Brisbane, Australia. Environ Res 103:383–389
Hansen CA, Barnett AG, Pritchard G (2008) The effect of ambient air pollution during early pregnancy on fetal ultrasonic measurements during mid-pregnancy. Environ Health Perspect 116:362–369
Huynh M, Woodruff TJ, Parker JD, Schoendorf KC (2006) Relationships between air pollution and preterm birth in California. Paediatr Perinat Epidemiol 20:454–461
Jiang LL, Zhang YH, Song GX, Chen GH, Chen BH, Zhao NQ, Kan HD (2007) A time series analysis of outdoor air pollution and preterm birth in Shanghai, China. Biomed Environ Sci 20:426–431
Kannan S, Misra DP, Dvonch JT, Krishnakumar A (2006) Exposures to airborne particulate matter and adverse perinatal outcomes: a biologically plausible mechanistic framework for exploring potential effect modification by nutrition. Environ Health Perspect 114:1636–1642
Kelly FJ (2003) Oxidative stress: its role in air pollution and adverse health effects. Occup Environ Med 60:612–616
Kim OJ, Ha EH, Kim BM et al (2007) PM10 and pregnancy outcomes: a hospital-based cohort study of pregnant women in Seoul. J Occup Environ Med 49:1394–1402
Lee BE, Ha EH, Park HS, Kim YJ, Hong YC, Kim H, Lee JT (2003) Exposure to air pollution during different gestational phases contributes to risks of low birth weight. Hum Reprod 18:638–643
Lee SJ, Hajat S, Steer PJ, Filippi V (2008) A time-series analysis of any short-term effects of meteorological and air pollution factors on preterm births in London, UK. Environ Res 106:185–194
Leem JH, Kaplan BM, Shim YK, Pohl HR, Gotway CA, Bullard SM, Rogers JF, Smith MM, Tylenda CA (2006) Exposures to air pollutants during pregnancy and preterm delivery. Environ Health Perspect 114:905–910
Lindbohm ML, Sallmen M, Taskinen H (2002) Effects of exposure to environmental tobacco smoke on reproductive health. Scand J Work Environ Health 28(Suppl 2):84–96
Maisonet M, Bush TJ, Correa A, Jaakkola JJ (2001) Relation between ambient air pollution and low birth weight in the Northeastern United States. Environ Health Perspect 109(Suppl 3):351–356
Maisonet M, Correa A, Misra D, Jaakkola JJ (2004) A review of the literature on the effects of ambient air pollution on fetal growth. Environ Res 95:106–115
Mannes T, Jalaludin B, Morgan G, Lincoln D, Sheppeard V, Corbett S (2005) Impact of ambient air pollution on birth weight in Sydney, Australia. Occup Environ Med 62:524–530
Morfeld P (2009) A plea for rigorous and honest science: false positive findings and biased presentations in epidemiological studies. Arch Toxicol 83:105–106
Nethery E, Leckie SE, Teschke K, Brauer M (2008) From measures to models: an evaluation of air pollution exposure assessment for epidemiological studies of pregnant women. Occup Environ Med 65:579–586
Parker JD, Woodruff TJ, Basu R, Schoendorf KC (2005) Air pollution and birth weight among term infants in California. Pediatrics 115:121–128
Perera FP, Jedrychowski W, Rauh V, Whyatt RM (1999) Molecular epidemiologic research on the effects of environmental pollutants on the fetus. Environ Health Perspect 107(Suppl 3):451–460
Peters A, Doring A, Wichmann HE, Koenig W (1997) Increased plasma viscosity during an air pollution episode: a link to mortality? Lancet 349:1582–1587
Ritz B, Wilhelm M (2008) Ambient air pollution and adverse birth outcomes: methodologic issues in an emerging field. Basic Clin Pharmacol Toxicol 102:182–190
Ritz B, Yu F, Chapa G, Fruin S (2000) Effect of air pollution on preterm birth among children born in Southern California between 1989 and 1993. Epidemiology 11:502–511
Ritz B, Wilhelm M, Hoggatt KJ, Ghosh JK (2007) Ambient air pollution and preterm birth in the environment and pregnancy outcomes study at the University of California, Los Angeles. Am J Epidemiol 166:1045–1052
Rogers JF, Dunlop AL (2006) Air pollution and very low birth weight infants: a target population? Pediatrics 118:156–164
Rogers JF, Thompson SJ, Addy CL, McKeown RE, Cowen DJ, Decoufle P (2000) Association of very low birth weight with exposures to environmental sulfur dioxide and total suspended particulates. Am J Epidemiol 151:602–613
Sagiv SK, Mendola P, Loomis D, Herring AH, Neas LM, Savitz DA, Poole C (2005) A time-series analysis of air pollution and preterm birth in Pennsylvania, 1997–2001. Environ Health Perspect 113:602–606
Salam MT, Millstein J, Li YF, Lurmann FW, Margolis HG, Gilliland FD (2005) Birth outcomes and prenatal exposure to ozone, carbon monoxide, and particulate matter: results from the Children’s Health Study. Environ Health Perspect 113:1638–1644
Slama R, Morgenstern V, Cyrys J, Zutavern A, Herbarth O, Wichmann HE, Heinrich J (2007) Traffic-related atmospheric pollutants levels during pregnancy and offspring’s term birth weight: a study relying on a land-use regression exposure model. Environ Health Perspect 115:1283–1292
Slama R, Darrow L, Parker J et al (2008) Meeting report: atmospheric pollution and human reproduction. Environ Health Perspect 116:791–798
Sorensen M, Daneshvar B, Hansen M, Dragsted LO, Hertel O, Knudsen L, Loft S (2003) Personal PM2.5 exposure and markers of oxidative stress in blood. Environ Health Perspect 111:161–166
Srăm R (1999) Impact of air pollution on reproductive health. Environ Health Perspect 107:A542–A543
Šrám RJ, Binkova B, Dejmek J, Bobak M (2005) Ambient air pollution and pregnancy outcomes: a review of the literature. Environ Health Perspect 113:375–382
Triche EW, Hossain N (2007) Environmental factors implicated in the causation of adverse pregnancy outcome. Semin Perinatol 31:240–242
Wang X, Ding H, Ryan L, Xu X (1997) Association between air pollution and low birth weight: a community-based study. Environ Health Perspect 105:514–520
Wilhelm M, Ritz B (2005) Local variations in CO and particulate air pollution and adverse birth outcomes in Los Angeles County, California, USA. Environ Health Perspect 113:1212–1221
Windham GC, Eaton A, Hopkins B (1999) Evidence for an association between environmental tobacco smoke exposure and birthweight: a meta-analysis and new data. Paediatr Perinat Epidemiol 13:35–57
Woodruff TJ, Parker JD, Darrow LA et al (2009) Methodological issues in studies of air pollution and reproductive health. Environ Res 109:311–320
Xu X, Ding H, Wang X (1995) Acute effects of total suspended particles and sulfur dioxides on preterm delivery: a community-based cohort study. Arch Environ Health 50:407–415
Yang CY, Tseng YT, Chang CC (2003) Effects of air pollution on birth weight among children born between 1995 and 1997 in Kaohsiung, Taiwan. J Toxicol Environ Health A 66:807–816
Acknowledgments
The authors thank Mrs M.P. Bonifacino and I. Garimoldi for editorial assistance. This work was conducted with the support of the Flagship Project “ProLife”, Comune di Milano, Milan.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bosetti, C., Nieuwenhuijsen, M.J., Gallus, S. et al. Ambient particulate matter and preterm birth or birth weight: a review of the literature. Arch Toxicol 84, 447–460 (2010). https://doi.org/10.1007/s00204-010-0514-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00204-010-0514-z