Abstract
Summary
The association between baseline physical activity and sedentary time with 2-year longitudinal bone strength was evaluated. The effect of physical activity on bone depended on maturity status. Sedentary time did not negatively impact bone outcomes, regardless of maturity. Maturity should be considered when developing exercise interventions to improve bone outcomes.
Introduction
Physical activity during adolescence is important to obtain peak bone mass; however, adolescents are increasingly sedentary, potentially increasing risk for osteoporosis later in life. The aim of this study was to assess the association of physical activity and sedentary time with 2-year longitudinal bone outcomes in adolescent females (69% Hispanic/31% non-Hispanic).
Methods
Bone strength was assessed at the 66% tibia, 20% femur, and 66% radius of 9- to 12-year-old girls (n = 131) using peripheral quantitative computed tomography at baseline and 2-year follow-up. Physical activity and sedentary time were assessed via accelerometry. Linear regression analyses were used to assess whether baseline vigorous physical activity (VPA), moderate physical activity (MPA), light physical activity (LPA), or sedentary time predict longitudinal bone outcomes, adjusting for relevant confounders.
Results
Significant interactions were found between maturity offset and physical activity. In weight-bearing bones, significant interactions were primarily identified between VPA and maturity offset. Interactions indicated that VPA was associated with favorable bone outcomes at the tibia and femur in girls further past the age of PHV. However, this favorable effect was not observed in girls closer to the age of PHV. At the radius, interactions were primarily observed between LPA and maturity offset. Again, LPA was more beneficial for girls further past the age of PHV. Sedentary time did not significantly influence bone outcomes.
Conclusion
The effects of physical activity on bone may be dependent on maturity. Therefore, physical activity interventions, with attention to maturity status, may be required to optimize bone strength in girls.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Adolescence is a period of rapid bone accrual, making it a critical time to optimize peak bone mass for osteoporosis prevention later in life [1]. In females, peak height velocity (PHV) occurs around 11.8 ± 1.0 years of age and peak bone accrual occurs around 12.5 ± 0.90 years [2, 3]. In the 4 years surrounding peak bone accrual, approximately 39% of adult bone mineral is gained [2,3,4], with the most rapid accrual of bone mass occurring directly after the onset of PHV. Although peak bone mass is largely influenced by genetics, lifestyle choices (e.g., diet and physical activity) can determine up to 40% of adult peak bone mass [1]. Because of the established benefits of physical activity for developing bone [1, 5], the current physical activity guidelines in the USA recommend that children engage in at least 60 min of moderate-to-vigorous physical activity (MVPA) per day and incorporate high-impact activities at least 3 days per week for bone health [6]. The guidelines also emphasize the importance of decreasing time spent in sedentary activities. However, most adolescent girls do not meet the physical activity guidelines and time spent in MVPA tends to be even lower in Hispanic girls [7,8,9]. Lower MVPA is often accompanied by more sedentary time during waking hours. Accelerometry data from the National Health and Nutrition Examination Survey (NHANES) show that adolescent girls (12–15 years old) spend 7.7 waking hours/day engaging in sedentary behaviors [10], with even higher rates reported in recent literature [11,12,13]. This is cause for concern for both general health and bone outcomes.
There is evidence that suggests sedentary time may be detrimental for bone development in peri-pubertal children [11, 14]. However, studies assessing the relationship between sedentary time and bone outcomes are often limited by cross-sectional design, self-reported measurements of sedentary time, or bone measurement technique (e.g., quantitative ultrasound) [14]. Few studies have assessed the association between objectively measured physical activity and bone in adolescents using peripheral quantitative computed tomography (pQCT), a three-dimensional imaging tool that can analyze bone architecture and strength [15], which cannot be ascertained by two-dimension dual-energy x-ray absorptiometry (DXA) scans. Additionally, no research studies have examined the association between sedentary time and bone outcomes in a mainly Hispanic population. Therefore, the aim of the current study was to assess the association of objectively measured baseline physical activity and sedentary time with 2-year longitudinal bone outcomes in cohort of predominantly Hispanic adolescent females during the years surrounding PHV, a period of rapid bone growth. Based on the previous literature, we hypothesized that higher amounts of baseline vigorous physical activity (VPA) and moderate physical activity (MPA) would be associated with higher longitudinal bone strength at the tibia and femur, while a greater amount of sedentary time would be negatively associated with longitudinal tibia and femur bone strength.
Methods
Study population
The Soft Tissue and Bone Development in Young Girls (STAR) study was a 2-year longitudinal study designed to assess the effects of body composition and metabolic risk factors on bone development in adolescent females (Clinical trials #NCT02654262). Three-hundred and fifty-eight girls aged 9–12 years old at baseline were recruited from local schools, pediatric clinics, and wellness community events in Tucson, AZ, between 2013 and 2018 to participate in the cross-sectional study. In line with the primary aim of the STAR study, a power analysis indicated that a subsample of 150 girls was required for the longitudinal study in order to detect statistically significant differences in 2-year pQCT bone changes between normal weight and obese girls, with and without cardiometabolic risk factors. One-hundred and sixty girls underwent 2-year longitudinal follow-up measures, of which 131 had complete data and comprise the sample that was used for the analysis reported herein (Fig. 1). The study protocol was approved by the University of Arizona Human Subjects Protection Committee. Written informed assent and consent was obtained from all participants and their parents or legal guardians, respectively. Exclusion criteria included the following: diagnosis of diabetes, taking any medications that alter body composition, physical disability that limits physical activity, and learning disability that limited completion of questionnaires or otherwise made the participant unable to comply with assessment protocols.
Questionnaires
At enrollment and 2-year follow-up, participants’ guardians were asked to complete a health history questionnaire, including questions regarding the participants’ race and ethnicity. Participants also completed the Harvard Youth/Adolescent Food Frequency Questionnaire at both time points to obtain information regarding normal dietary intake, including calcium intake.
Anthropometric measurements
Anthropometric measures were obtained according to standardized protocols, which have previously been described [16, 17]. Body mass was measured to the nearest 0.1 kg using a calibrated scale (Seca, Model 881, Hamburg, Germany). Standing and sitting height were measured at full inhalation to the nearest mm using a stadiometer (Shorr Height Measuring Board, Olney, MD). Body mass index (BMI) was calculated as weight divided by height squared (kg/m2).
Maturation
Maturation was assessed by pubertal status and somatic maturation. Pubertal status was determined via self-reported questionnaire. Girls were provided pictures depicting the Tanner stages of pubertal maturation and selected the image that represented the correct stage of maturity for both breast and pubic hair development [18]. Maturity offset was used to assess years from age at PHV. Maturity offset was estimated from age and anthropometric measures (height, weight, sitting height, leg length) using the Mirwald equation [19]. This equation explains approximately 89% of the variance in years from peak height velocity (PHV) [19]. A negative maturity offset represents years prior to PHV (PRE-PHV) and a positive maturity offset signifies years after PHV (POST-PHV).
Dual-energy X-ray absorptiometry
Measures of soft tissue composition were obtained from dual-energy x-ray absorptiometry (DXA) using GE/Lunar Radiation Corp (Madison, WI) following standard subject positioning and data acquisition protocols on the Prodigy and iDXA models. A single certified technician performed all DXA scan analyses. The DXA was calibrated daily according to manufacturer guidelines. Within-subject variation for soft tissue in our laboratory has been previously reported [20, 21].
Peripheral quantitative computed tomography
Measurements were taken at the 66% tibia, 20% femur, and 66% radius sites relative to the distal growth plate on the non-dominant limb to assess cortical (diaphyseal) strength using the STRATEC, XCT 3000 pQCT (Medizintechnik GmbH, Pforzheim, Germany, Division of Orthometrix; White Plains, NY). All Peripheral quantitative computed tomography (pQCT) scans were analyzed using Stratec XCT software, Version 6.0, and operators were trained for pQCT data acquisition and analyses following guidelines provided by Bone Diagnostic LLC (Spring Branch, TX). Instrument, image processing, and analysis protocols used in our laboratory have been published previously, as well as coefficients of within-subject variation for pQCT bone measurements [22].
Briefly, pQCT slice thicknesses were 2.3 mm and voxel sizes and scanner speed were set at 0.4 mm and 25 mm/s respectively. As described in the Stratec XCT software manual [23], Contour, Peel, and Cort modes were used to obtain measures of bone geometry and material properties. At diaphyseal sites, total bone area (mm2) was obtained using Contour mode (710 mg/cm3) and measures of cortical volumetric bone mineral density (vBMD) (mg/cm3), cortical bone mineral content (BMC) (mg/mm), cortical area (mm2), endosteal circumference (mm), periosteal circumference (mm), and cortical thickness (mm) were obtained using Cort mode 2 (710 mg/cm3). Scans at each site were reviewed for participant movement and excluded according to a visual inspection rating scale [24].
As described elsewhere [15, 25], estimates of bone strength were calculated using the pQCT derived measures of bone density and geometry. A strength strain index (SSI, mm3) that accounts for both the structural and material properties of bone was calculated using the equation described by Shedd et al. to estimate the resistance of diaphyseal bone to bending and torsional loading [25]. This calculated SSI predicts up to 80% of the variance in bending failure load in human tibias [15]: SSI = Σ((dZ2 × AV) × (cortical vBMD/ND))/dmax, where dZ is the distance of voxel from the center of gravity, AV is the area of the voxel (mm2), Cort vBMD is the cortical bone density (mg/cm3), ND is the estimated normal physiological bone density (1200 mg/cm3), and dmax is the maximum distance of a voxel from the center of gravity [25].
Physical activity and sedentary time
Physical activity and sedentary time variables were measured using GT3X+ tri-axial accelerometers (ActiGraph, Pensacola, FL). Participants were instructed to wear the accelerometer on their hip for 7 consecutive days during all waking hours, except for showering, or other water activities. The accelerometers were initialized for data collection at 30 hz. Data were saved in 1-s epochs with the “low frequency extension” option selected and analyzed using ActiLife Software version 6.13.4 (ActiGraph, Pensacola, FL). Non-wear time was classified as ≥ 30 min of continuous zeros as this algorithm has been show to most accurately assess sedentary time in youth [26]. Girls who wore the accelerometer for at least 10 h/day on 3 or more days were included in the analyses. Evenson cut points were used to classify sedentary activity (≤ 100 counts per minute; cpm), light physical activity (101–2295 cpm, LPA), moderate physical activity (2296–4011 cpm), and vigorous physical activity (≥ 4012 cpm) [27]. Moderate and vigorous activities were combined to estimate MVPA.
Statistical analyses
Descriptive statistics, including mean and standard deviation for normally distributed variables or median and interquartile range for skewed variables, were used to describe participant characteristics. Multiple linear regression analyses were used to test the relationship of the independent variables of interest (baseline VPA, MPA, LPA, and sedentary time) with the primary outcome of interest, 2-year SSI, and secondary pQCT bone outcomes. All covariates were selected a priori based on their established association with bone strength. Covariates included in all models were baseline bone outcome of interest, baseline accelerometer wear time (minutes), ethnicity (non-Hispanic or Hispanic), 2-year height (cm), 2-year lean soft tissue mass (kg), and 2-year maturity offset (years from age at PHV). Calcium intake was also considered as a covariate; however, it did not improve model prediction and therefore was not included in the final models. Due to the known impact of maturity on the physical activity-bone relationship [28, 29], interactions between physical activity variables and maturity offset were tested in each model. For models with statistically significant interactions, post-hoc contrasts were used to obtain the simple regression slopes for the mean± 1 SD values of 2-year maturity offset to further characterize the influence of maturity offset on the relationships between physical activity and sedentary time with 2-year bone outcomes. As a sensitivity analysis, we fit a second model for sedentary time that additionally controlled for MVPA (min/day) to determine the effect of sedentary time on bone outcomes independent of MVPA.
Linearity between outcome variables and each covariate was assessed with scatter plots. All models were checked for the assumptions of linear regression: linearity, normality of residuals, and homoscedasticity. A residual versus predictors plot was used to visually assess the assumptions of linearity and homoscedasticity. Normal distribution of residuals for the model was assessed using a histogram. Collinearity of variables was assessed via variance inflation factor, with a value > 5 indicating collinearity.
All analyses were performed in R version 3.5.2 (R Foundation for Statistical Computing, Vienna, Austria) using the stats package lm() function for linear regression and emmeans package to obtain estimated marginal means. A p value of < 0.05 was considered statistically significant.
Results
Descriptive characteristics of this sample are reported in Table 1. The majority of girls identified as white race (70%) and Hispanic ethnicity (69%). Girls were on average 12.9 ± 1.1 years old at follow-up. There was high correlation (r = 0.98) between baseline maturity offset and 2-year maturity offset. As expected during a period of growth, girls showed increases in total body weight (12.1 ± 6.6 kg gain) and lean body mass (5.86 ± 3.6 kg gain) between baseline and 2-year follow-up. At baseline, 3% of girls were classified as underweight, 56% normal weight, 17% overweight, and 24% obese. The rates of underweight and obesity stayed consistent between baseline and 2-year follow-up, but there was a slight decline in the number of girls who were classified as normal weight (51% at follow-up) and an increase in girls classified as overweight (22% at follow-up).
Mean days of accelerometer wear was 5.7 ± 1.3 days with an average of 803 ± 60 min of wear time per day. The median time spent in MVPA was 46.6 (35.2, 57.9) minutes per day and only 5 girls met the physical activity guidelines of at least 60 min of MVPA per day. Bone parameters are characterized in Table 2. The greatest 2-year percent increases for tibia and femur outcomes were evident for SSI (mm3), cortical BMC (mg/mm), cortical area (mm2), and total area (mm2), while the greatest increases for the radius were SSI (mm3), cortical BMC (mg/mm), cortical area (mm2), and cortical thickness (mm).
The results for the linear regression models for weight-bearing bones (tibia and femur) and non-weight-bearing bone (radius) are presented in Table 3. Significant interactions between physical activity and maturity offset were identified for all bone sites. In the weight-bearing bones, interactions were most common between higher intensity physical activity (i.e., VPA and MPA) and maturity offset. At the tibia, VPA explained ~ 1% of the variation in SSI and ~ 2% of the variation in cortical BMC, cortical thickness, and cortical area. In separate models, MPA explained ~ 1–2% in the variance of cortical BMD and cortical thickness and LPA explained < 1% of the variance in total bone area. Similarly, at the femur, VPA explained < 1% of variance in SSI, periosteal circumference, and endosteal circumference and ~ 1–2% variance in cortical BMC and cortical area. For all bone sites, the greatest amount of variance in 2-year bone outcomes was explained by the baseline bone measurement and total body lean mass.
At the radius, interactions were most common between LPA and sedentary time with maturity offset. LPA explained the greatest amount of variance in bone outcomes at the radius, explaining ~ 6% variance in cortical vBMD, 2.5% in cortical BMC, 2.3% in cortical area, 1.8% in periosteal circumference, and ~ 1% in SSI and cortical thickness. In separate models, sedentary time explained the next greatest amount of variance, explaining approximately 4% of cortical vBMD and ~ 1–2% of variability in cortical BMC, cortical area, and cortical thickness. VPA explained ~ 1.3% of variance in cortical BMC, cortical area, and cortical thickness.
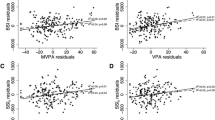
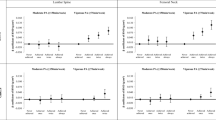
Simple slopes and 95% confidence intervals from post-hoc contrasts of interactions between physical activity/sedentary time and maturity offset on bone outcomes at the tibia, femur, and radius are presented in Table 4 and select interactions are depicted in Fig. 2. Since interactions between VPA, MPA, and LPA with maturity offset were positive at all bone sites, the primary outcome of interest (SSI) was selected to represent the positive interactions. However, since the interaction between sedentary time and maturity offset was not significant in any models for SSI, the model for cortical BMC at the radius was also included to illustrate the negative interaction observed between sedentary time and maturity offset at the radius. Figure 2 depicts the influence of maturity offset (± 1 standard deviation from the mean at 2 years) on the relationship between physical activity and bone outcomes while holding all other variables in the model constant. Since baseline bone measurements were controlled in the models, Fig. 2 also shows that girls with a lower maturity offset (− 1 SD from mean) had overall greater gains in SSI at all bone sites as compared to girls with a higher maturity offset, particularly at lower levels of physical activity.
Predicted regression slopes and 95% confidence intervals for the relationship between baseline physical activity or sedentary time on 2-year bone outcomes at the 66% tibia, 20% femur, and 66% radius at varying levels of 2-year maturity offset (years past age of peak height velocity–PHV), holding baseline bone, ethnicity, height, lean mass, and accelerometer wear time constant
For the sensitivity analysis, average time spent in MVPA was included in the sedentary time models. In all models that showed sedentary time as a significant predictor, sedentary time remained a significant predictor even after inclusion of MVPA in the models. However, inclusion of MVPA in sedentary time models lead to collinearity between sedentary time and accelerometer wear time that was not observed in the initial models. Therefore, only the results of the initial sedentary models are reported.
Discussion
The aim of this study was to assess the association of objectively measured physical activity and sedentary time with 2-year longitudinal bone outcomes at the tibia, femur, and radius during the years surrounding PHV. In our sample comprised primarily of Hispanic female adolescents (9–12 years old at baseline), we found the relationship between baseline physical activity and 2-year bone outcomes did not stay consistent throughout maturity. In girls further past the age of PHV at study outcome (+ 1 SD from the mean, approximately corresponding to girls POST-PHV baseline), higher intensity physical activity (i.e., VPA and MPA) was favorably associated with 2-year bone outcomes at the tibia and femur; however, in girls earlier in maturity offset at study outcome (− 1 SD from the mean, approximately corresponding to girls PRE-PHV baseline), this favorable effect of physical activity was not observed.
At the tibia, we found that baseline VPA was associated with increased SSI in girls further past the age of PHV. The positive relationship observed between VPA and SSI was likely influenced by the positive association seen between VPA and increased cortical BMC, cortical area, and cortical thickness. Similarly, researchers have previously found that MVPA is associated with greater longitudinal tibia bone strength as assessed by failure load using HR-pQCT [11] and polar moment of inertia derived from pQCT [30]. Unlike our results that showed this relationship in only the subset of the sample POST-PHV at baseline, Gabel et al. and Janz et al. were both able to detect these results for their entire cohorts of males and females, potentially due to the older age and greater maturity status of their samples at baseline (Gabel: females 14.4 ± 3.5 years old and 2.9 ± 3.6 years past the age of PHV; males 14.9 ± 2.9 years and 1.8 ± 3 years past the age of PHV) and final follow-up (Janz: 17.5 ± 0.4 years males and females with age at PHV 11.8 ± 0.6 and 13.7 ± 0.7 for females and males, respectively). Previous cross-sectional results from an observational study showed that the variance explained by MVPA on pQCT bone outcomes was relatively small (< 5%) [12]. Likewise, we found that VPA explained only about 1–2% of the variance in 2-year tibia bone outcomes. Therefore, it is possible that girls earlier in maturity offset (PRE-PHV at baseline) were rapidly accruing bone, regardless of physical activity, such that the beneficial effect of physical activity was masked. In line with this, the interactions depicted in Fig. 2 show that after controlling for baseline SSI, girls earlier in maturity offset have greater 2-year SSI (i.e., gained more bone strength during 2-year follow-up) than girls later in maturity offset at all but the highest amounts of VPA.
Ducher et al. showed that physical activity promotes periosteal bone deposition in girls of similar ages to the girls in our cohort [31]. Based on this theory that physical activity increases periosteal apposition during adolescence, we hypothesized that VPA and MPA would be associated with higher total bone area and periosteal circumference at 2-year follow-up. While we did not observe a beneficial effect of physical activity on periosteal circumference at the tibia, we did find that girls further past the age of PHV with higher baseline physical activity (VPA, MPA) had a greater femur periosteal circumference at 2-year follow-up, although this did not reach statistical significance in post-hoc testing. There was also evidence that greater VPA was associated with larger femur bone area, greater SSI, and greater cortical BMC for girls who were past the age of PHV and who did more VPA at baseline. Counter to our hypothesis, we found that girls earlier in maturity offset showed a negative relationship between VPA and femur periosteal circumference. It is possible that not all girls earlier in maturity offset had reached the period of peak bone mineral accretion even at 2-year follow-up, transiently showing no beneficial effect of physical activity for girls earlier in maturity offset until more bone mineral is deposited. To our knowledge there are no other studies assessing the relationship between accelerometer derived physical activity and longitudinal pQCT outcomes at the femur. However, Janz et al. similarly found that girls who participated in more MVPA during childhood and early adolescence had a higher DXA derived femur cross-sectional area later in adolescence (age 17.5 ± 0.4) [30].
At the radius, we observed a general trend that LPA was associated with less favorable bone outcomes in girls with a lower maturity offset, but sedentary time appeared to be beneficial for bone outcomes in this group. Although this finding is counter-intuitive, we are not the first to observe a beneficial effect of more sedentary time on bone outcomes. A longitudinal study by Gabel et al. observed a favorable effect of sedentary time on trabecular thickness, cortical thickness, and cortical BMD [11], while a cross-sectional study by Chastin et al. reported a positive association between sedentary time and DXA-derived BMC at the spine and proximal femur [8]. It is currently theorized that physical activity patterns might be important for explaining this relationship. Chastin et al. found that clustered, short bouts of high intensity activity with longer periods of sedentary time in between appeared to be more osteogenic than more consistent physical activity throughout the day [8]. Therefore, it is possible that girls in our sample with higher amounts of sedentary time do short bouts of high intensity activity at the arm with longer recovery periods in between, while girls with more LPA do more continuous activities that may not be as osteogenic. While the exact reason for the positive relationship between sedentary time and bone outcomes remains unclear, this association at the radius in our sample appears to be transient. In girls further past the age of PHV, we observed a favorable relationship between higher baseline LPA and bone outcomes with the statistical interactions. Additionally, the favorable effect of sedentary time on bone outcomes seen in girls closer to the age of PHV appeared to be less beneficial as girls matured. To our knowledge ,there are no other studies that assess the relationship between LPA and bone outcomes at the radius which limits our ability to compare and interpret these findings. Gabel et al. did, however, assess the relationship between sedentary time and longitudinal outcomes at the radius and found no relationship between sedentary time and longitudinal bone outcomes in their cohort of males and females after controlling for relevant covariates.
Prior studies by Ivuškāns et al. (n = 169) and Vaitkeviciute et al. (n = 147 at 2-year follow-up) utilizing DXA imaging showed that sedentary time was negatively associated with areal bone mineral density at the femur in male adolescents [32, 33]. Additionally, Gabel et al. (n = 309, 142 female and 115 male) showed sedentary time is inversely related to tibia bone strength obtained from HR-pQCT, although this relationship did not remain statistically significant after controlling for MVPA [11]. Unlike these studies, we did not find sedentary time to negatively impact weight-bearing bones, although there was a negative association between sedentary time and tibia SSI that approached statistical significance (p = 0.08). It should be noted that the studies by Ivuškāns and Vaitkeviciute assessed bone density using DXA which is limited by two-dimensional imaging and therefore cannot ascertain the details pertaining to bone strength and structure that were assessed in the current study. Additionally, all of the previous studies either assessed males only [32, 33] or combined both males and females [11] while we only assessed adolescent females. Thus, we cannot discount the possibility that there may be a sex difference or a sex by maturity difference for how sedentary time affects bone development. As previously reported by Janz et al., boys have a stronger relationship between physical activity and bone development than girls [34], likely due to a combination of biological differences (e.g., hormones) and differences in physical activity between sexes.
Gunter et al. suggested that approximately 40 min of MVPA is necessary to see beneficial effects to hip structure and strength [35]. On average, the girls in our study participated in 46.6 (interquartile range: 35.2, 57.9) minutes MVPA per day, indicating that as a whole, they are likely meeting the threshold required to see the benefits of physical activity on bone. Regardless, our observation that only about 4% of our sample met the physical activity guideline recommending at least 60 min/day of MVPA per day supports international findings that adolescents are not engaging in enough MVPA [36] and emphasizes the importance of health promotion efforts designed to increase MVPA and decrease sedentary time in youth.
We acknowledge that this study had limitations. First, due to the nature of bone growth in adolescents, it is not possible to measure the exact bone cross-section over time. However, the use of anatomical landmarks allowed for measurement of the same site relative to the growth plate over time. Additionally, only peripheral bone sites were measured, limiting our understanding of how MVPA and sedentary time may affect the hip and spine. Finally, accelerometers cannot measure ground reaction forces, thereby failing to distinguish high-impact MVPA from lower impact MVPA which affect bone strength differently.
Our study also had many strengths including a longitudinal study design allowing for assessment of bone development over time, use of pQCT to assess bone strength and architecture, and objective assessment of physical activity. This study adds to the literature by showing that the effect of physical activity and sedentary time on bone outcomes may depend on the stage of maturity in a relatively inactive and primarily Hispanic female population. Based on our findings, interventions are needed to increase physical activity in young Hispanic and non-Hispanic females to improve compliance with the physical activity guidelines and improve overall health outcomes, including bone. Further research is needed to better understand the relationship between maturity, physical activity, and bone outcomes to help determine whether there is an ideal maturity stage to provide physical activity interventions to improve bone strength.
References
Weaver CM, Gordon CM, Janz KF, Kalkwarf HJ, Lappe JM, Lewis R, O’Karma M, Wallace TC, Zemel BS (2016) The National Osteoporosis Foundation’s position statement on peak bone mass development and lifestyle factors: a systematic review and implementation recommendations. Osteoporos Int 27(4):1281–1386. https://doi.org/10.1007/s00198-015-3440-3
Baxter-Jones AD, Faulkner RA, Forwood MR, Mirwald RL, Bailey DA (2011) Bone mineral accrual from 8 to 30 years of age: an estimation of peak bone mass. J Bone Miner Res 26(8):1729–1739
MacKelvie KJ, Khan KM, McKay HA (2002) Is there a critical period for bone response to weight-bearing exercise in children and adolescents? A systematic review. Br J Sports Med 36(4):250–257
Bailey DA, Martin AD, McKay HA, Whiting S, Mirwald R (2000) Calcium accretion in girls and boys during puberty: a longitudinal analysis. J Bone Miner Res 15(11):2245–2250. https://doi.org/10.1359/jbmr.2000.15.11.2245
Kohrt WM, Bloomfield SA, Little KD, Nelson ME, Yingling VR, American College of Sports Medicine (2004) American College of Sports Medicine position stand: physical activity and bone health. Med Sci Sports Exerc 36(11):1985–1996
Piercy KL, Troiano RP, Ballard RM, Carlson SA, Fulton JE, Galuska DA, George SM, Olson RD (2018) The physical activity guidelines for Americans. JAMA 320(19):2020–2028
Treuth MS, Catellier DJ, Schmitz KH, Pate RR, Elder JP, McMurray RG, Blew RM, Yang S, Webber L (2007) Weekend and weekday patterns of physical activity in overweight and normal-weight adolescent girls. Obesity 15(7):1782–1788
Chastin SF, Mandrichenko O, Skelton DA (2014) The frequency of osteogenic activities and the pattern of intermittence between periods of physical activity and sedentary behaviour affects bone mineral content: the cross-sectional NHANES study. BMC Public Health 14(1):4
Webber LS, Catellier DJ, Lytle LA, Murray DM, Pratt CA, Young DR, Elder JP, Lohman TG, Stevens J, Jobe JB (2008) Promoting physical activity in middle school girls: trial of activity for adolescent girls. Am J Prev Med 34(3):173–184
Matthews CE, Chen KY, Freedson PS, Buchowski MS, Beech BM, Pate RR, Troiano RP (2008) Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol 167(7):875–881. https://doi.org/10.1093/aje/kwm390
Gabel L, Macdonald HM, Nettlefold L, Mckay HA (2017) Physical activity, sedentary time, and bone strength from childhood to early adulthood: a mixed longitudinal HR-pQCT study. J Bone Miner Res 32(7):1525–1536
Osborn W, Simm P, Olds T, Lycett K, Mensah FK, Muller J, Fraysse F, Ismail N, Vlok J, Burgner D, Carlin JB, Edwards B, Dwyer T, Azzopardi P, Ranganathan S, Wake M (2018) Bone health, activity and sedentariness at age 11-12 years: cross-sectional Australian population-derived study. Bone 112:153–160. https://doi.org/10.1016/j.bone.2018.04.011
Tan VP, Macdonald HM, Gabel L, McKay HA (2018) Physical activity, but not sedentary time, influences bone strength in late adolescence. Arch Osteoporos 13(1):31. https://doi.org/10.1007/s11657-018-0441-9
Koedijk J, van Rijswijk J, Oranje W, van den Bergh J, Bours S, Savelberg H, Schaper N (2017) Sedentary behaviour and bone health in children, adolescents and young adults: a systematic review. Osteoporos Int 28(9):2507–2519
Kontulainen S, Johnston J, Liu D, Leung C, Oxland T, McKay H (2008) Strength indices from pQCT imaging predict up to 85% of variance in bone failure properties at tibial epiphysis and diaphysis. J Musculoskelet Neuronal Interact 8(4):401–409
Lohman TG, Roche AF, Martorell R (1988) Anthropometric standardization reference manual, vol 177. Human Kinetics, Champaign
Hetherington-Rauth M, Bea JW, Lee VR, Blew RM, Funk J, Lohman TG, Going SB (2017) Comparison of direct measures of adiposity with indirect measures for assessing cardiometabolic risk factors in preadolescent girls. Nutr J 16(1):15. https://doi.org/10.1186/s12937-017-0236-7
Marshall WA, Tanner JM (1969) Variations in pattern of pubertal changes in girls. Arch Dis Child 44(235):291–303
Mirwald RL, Baxter-Jones AD, Bailey DA, Beunen GP (2002) An assessment of maturity from anthropometric measurements. Med Sci Sports Exerc 34(4):689–694
Going S, Lohman T, Houtkooper L, Metcalfe L, Flint-Wagner H, Blew R, Stanford V, Cussler E, Martin J, Teixeira P (2003) Effects of exercise on bone mineral density in calcium-replete postmenopausal women with and without hormone replacement therapy. Osteoporos Int 14(8):637–643
Bea JW, Cussler EC, Going SB, Blew RM, Metcalfe LL, Lohman TG (2010) Resistance training predicts 6-yr body composition change in postmenopausal women. Med Sci Sports Exerc 42(7):1286–1295. https://doi.org/10.1249/MSS.0b013e3181ca8115
Farr JN, Chen Z, Lisse JR, Lohman TG, Going SB (2010) Relationship of total body fat mass to weight-bearing bone volumetric density, geometry, and strength in young girls. Bone 46(4):977–984. https://doi.org/10.1016/j.bone.2009.12.033
Stratec Medizintchnik XCT (2004) 3000 manual, software version 6.0. Pforzheim, Germany
Blew RM, Lee VR, Farr JN, Schiferl DJ, Going SB (2014) Standardizing evaluation of pQCT image quality in the presence of subject movement: qualitative versus quantitative assessment. Calcif Tissue Int 94(2):202–211
Shedd KM, Hanson KB, Alekel DL, Schiferl DJ, Hanson LN, Van Loan MD (2007) Quantifying leisure physical activity and its relation to bone density and strength. Med Sci Sports Exerc 39(12):2189–2198. https://doi.org/10.1249/mss.0b013e318155a7fe
Vanhelst J, Vidal F, Drumez E, Béghin L, Baudelet J-B, Coopman S, Gottrand F (2019) Comparison and validation of accelerometer wear time and non-wear time algorithms for assessing physical activity levels in children and adolescents. BMC Med Res Methodol 19(1):72
Evenson KR, Catellier DJ, Gill K, Ondrak KS, McMurray RG (2008) Calibration of two objective measures of physical activity for children. J Sports Sci 26(14):1557–1565
Tan VP, Macdonald HM, Kim S, Nettlefold L, Gabel L, Ashe MC, McKay HA (2014) Influence of physical activity on bone strength in children and adolescents: a systematic review and narrative synthesis. J Bone Miner Res 29(10):2161–2181
Janz KF, Gilmore JM, Levy SM, Letuchy EM, Burns TL, Beck TJ (2007) Physical activity and femoral neck bone strength during childhood: the Iowa Bone Development Study. Bone 41(2):216–222
Janz KF, Letuchy EM, Burns TL, Eichenberger Gilmore JM, Torner JC, Levy SM (2014) Objectively measured physical activity trajectories predict adolescent bone strength: Iowa Bone Development Study. Br J Sports Med 48(13):1032–1036. https://doi.org/10.1136/bjsports-2014-093574
Ducher G, Bass SL, Saxon L, Daly RM (2011) Effects of repetitive loading on the growth-induced changes in bone mass and cortical bone geometry: a 12-month study in pre/peri-and postmenarcheal tennis players. J Bone Miner Res 26(6):1321–1329
Ivuškāns A, Mäestu J, Jürimäe T, Lätt E, Purge P, Saar M, Maasalu K, Jürimäe J (2015) Sedentary time has a negative influence on bone mineral parameters in peripubertal boys: a 1-year prospective study. J Bone Miner Metab 33(1):85–92
Vaitkeviciute D, Lätt E, Mäestu J, Jürimäe T, Saar M, Purge P, Maasalu K, Jürimäe J (2014) Physical activity and bone mineral accrual in boys with different body mass parameters during puberty: a longitudinal study. PLoS One 9(10):e107759
Janz KF, Letuchy EM, Eichenberger Gilmore JM, Burns TL, Torner JC, Willing MC, Levy SM (2010) Early physical activity provides sustained bone health benefits later in childhood. Med Sci Sports Exerc 42(6):1072–1078. https://doi.org/10.1249/MSS.0b013e3181c619b2
Gunter KB, Almstedt HC, Janz KF (2012) Physical activity in childhood may be the key to optimizing lifespan skeletal health. Exerc Sport Sci Rev 40(1):13–21
Cooper AR, Goodman A, Page AS, Sherar LB, Esliger DW, van Sluijs EM, Andersen LB, Anderssen S, Cardon G, Davey R (2015) Objectively measured physical activity and sedentary time in youth: the International Children’s Accelerometry Database (ICAD). Int J Behav Phys Act 12(1):113
Acknowledgments
This study was executed at the University of Arizona, Collaboratory for Metabolic Disease Prevention and Treatment.
Funding
This study was funded by the National Institute of Child Health and Human Development (Award #HD074565).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study protocol was approved by the University of Arizona Human Subjects Protection Committee. Written informed assent and consent was obtained from all participants and their parents or legal guardians, respectively.
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bland, V., Bea, J., Roe, D. et al. Physical activity, sedentary time, and longitudinal bone strength in adolescent girls. Osteoporos Int 31, 1943–1954 (2020). https://doi.org/10.1007/s00198-020-05406-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-020-05406-z