Abstract
Summary
Physical activity is essential for optimal bone strength accrual, but we know little about interactions between physical activity, sedentary time, and bone outcomes in older adolescents. Physical activity (by accelerometer and self-report) positively predicted bone strength and the distal and midshaft tibia in 15-year-old boys and girls. Lean body mass mediated the relationship between physical activity and bone strength in adolescents.
Purpose
To examine the influence of physical activity (PA) and sedentary time on bone strength, structure, and density in older adolescents.
Methods
We used peripheral quantitative computed tomography to estimate bone strength at the distal tibia (8% site; bone strength index, BSI) and tibial midshaft (50% site; polar strength strain index, SSIp) in adolescent boys (n = 86; 15.3 ± 0.4 years) and girls (n = 106; 15.3 ± 0.4 years). Using accelerometers (GT1M, Actigraph), we measured moderate-to-vigorous PA (MVPAAccel), vigorous PA (VPAAccel), and sedentary time in addition to self-reported MVPA (MVPAPAQ-A) and impact PA (ImpactPAPAQ-A). We examined relations between PA and sedentary time and bone outcomes, adjusting for ethnicity, maturity, tibial length, and total body lean mass.
Results
At the distal tibia, MVPAAccel and VPAAccel positively predicted BSI (explained 6–7% of the variance, p < 0.05). After adjusting for lean mass, only VPAAccel explained residual variance in BSI. At the tibial midshaft, MVPAAccel, but not VPAAccel, positively predicted SSIp (explained 3% of the variance, p = 0.01). Lean mass attenuated this association. MVPAPAQ-A and ImpactPAPAQ-A also positively predicted BSI and SSIp (explained 2–4% of the variance, p < 0.05), but only ImpactPAPAQ-A explained residual variance in BSI after accounting for lean mass. Sedentary time did not independently predict bone strength at either site.
Conclusion
Greater tibial bone strength in active adolescents is mediated, in part, by lean mass. Despite spending most of their day in sedentary pursuits, adolescents’ bone strength was not negatively influenced by sedentary time.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adolescence is a complex period of accelerated growth and maturation that marks the transition from childhood to adulthood. During adolescence, 39% of adult bone mass is accrued within 5 years around peak height velocity [1]. Rate of bone accrual peaks about a year after peak height velocity, around age 12.8 years for girls and 14.3 years for boys [2], followed by diminished gains in bone mass and strength during late adolescence. Importantly, weight-bearing physical activity has profound osteogenic effects during pre- and early puberty [3] and is fundamental to develop and maintain a strong skeleton. However, as few studies focused on the older adolescent (> 15 years) skeleton [3], we know relatively little about how bone adapts structurally to mechanical challenges imposed through weight-bearing physical activity during this period of growth.
This knowledge gap is due, in part, to the reliance on two-dimensional dual energy X-ray absorptiometry in previous studies of adolescent bone health, such as those that examined determinants of femoral bone geometry [4, 5]. As a planar instrument, DXA is unable to capture subtle adapations in bone structure and geometry in the adolescent skeleton in response to physical activity. More recently, three-dimensional imaging tools such as peripheral quantitative computed tomography (pQCT) and high-resolution pQCT (HR-pQCT) were used to investigate the influence of physical activity on bone (micro) structure, bone mineral density (BMD), and estimates of bone strength. However, only three studies used either of these imaging tools to investigate the relation between physical activity and bone strength, structure, and density at the tibia in recreationally active older adolescents (≥ 15 years) [6,7,8].
Given the central role of weight-bearing PA as the mechanical stimulus necessary to promote bone strength accrual, it is of concern that adolescents have become less physically active and increasingly sedentary. Specifically, a global report concluded that only about 20% of adolescents aged 13 to 15 years currently meet PA guidelines of 60 min/day of moderate-to-vigorous PA (MVPA) [9]. In addition, sedentary behaviors are on the rise; today’s youth spend 62% of their waking hours being sedentary [10]. The deleterious effects of sedentary time on adolescent bone strength, structure, and density have yet to be fully elucidated as results of previous studies are mixed [11,12,13,14,15]. Variability in results across studies is likely due, in part, to differences in methods used to assess both sedentary time and bone outcomes.
Mechanostat theory suggests that muscle contractions, such as those that occur during PA, incur high physiological loads on bone and may enhance bone formation, while low loads may enhance bone formation, while low loads from being sedentary (less muscle activity) may increase bone resorption [16]. In previous studies of children and adolescents, the relation between physical activity, bone mass, and estimates of bone strength were diminished [17] or disappeared [18] when muscle mass, a surrogate of muscle force, was added to prediction models. Therefore, we deem it essential to also consider the modulating role of muscle (mass/force) to better understand the relation between physical activity and bone outcomes.
Hence, we conducted a cross-sectional study of healthy adolescent boys and girls aged 15 years, on average, to ascertain the following: (1) associations between MVPA and tibial bone strength, structure, and BMD (bone outcomes); (2) whether lean body mass, as a surrogate for muscle force, mediates the relationship between MVPA and bone outcomes; and (3) whether sedentary time attenuates the relationship between MVPA and bone outcomes. We hypothesized that positive associations between MVPA and bone outcomes would be mediated by lean mass and that sedentary time would attenuate associations between MVPA and bone outcomes.
Methods
Study design and participants
In this cross-sectional study, we included baseline data for a convenience sample of participants from the Health Promoting Secondary Schools (HPSS) study [19]. Briefly, HPSS was a ‘whole school’ program that aimed to improve PA and healthy eating behaviors of Grade 10 students in British Columbia, Canada. We recruited secondary schools from the Greater Vancouver and southern Vancouver Island school districts in fall, 2010. Of 48 eligible schools (offered physical education beyond grade 10), nine schools agreed to participate in the HPSS Bone Health Study. We acquired baseline measures between September and November 2011. Measurements were conducted in the Centre for Hip Health and Mobility’s Mobile Research Laboratory that is equipped with pQCT and DXA systems and an anthropometry station. The University of British Columbia’s Clinical and Behavioural Research Ethics Boards (H10-01917), University of Victoria’s Human Research Ethics Board (10-168), and participating school districts approved all study procedures.
From a possible 1914 Grade 10 students who attended nine volunteer schools, 210 (11%; 94 boys, 116 girls) provided written informed assent and parental consent to participate in the HPSS Bone Health Study. Of those, we excluded seven participants who declined to have pQCT scans due to concerns regarding additional radiation exposure beyond the dose received during recent clinical examinations. We also excluded a participant who did not complete the physical activity questionnaire, one whose limb length was measured incorrectly, and two participants who reported taking medication known to influence bone metabolism. Thus, we included 199 participants (89 boys, 110 girls) in our analyses.
Based on baseline information from the health history questionnaire, we considered participants white (n = 106) if both parents or three out of four grandparents were born in North America or Europe and Asian (n = 74) if both parents or three out of four grandparents were born in Asia (i.e., East Asia, South Asia, South-east Asia). We considered participants from other ethnic origins (e.g., Pacific Islanders) and those of mixed ethnicity as “other” (n = 19). We used this method to determine ethnicity in previous trials [11, 12].
Anthropometry and body composition
We measured stature to the nearest 0.1 cm with a wall-mounted digital stadiometer (Seca model 242; Seca, Hanover, MD) and body mass to the nearest 0.1 kg using an electronic scale (Tanita BWB 800, Japan). We assessed tibial length to the nearest 0.1 cm as the distance from the distal edge of the medial malleolus to the tibial plateau. We obtained two measures for each variable. We obtained a third measure if differences between measures for stature or tibial length differed by 0.4 cm or by 0.2 kg for body mass. We used the mean of two or the median of three measures for our analyses.
We used DXA (Hologic Discovery A, USA) to obtain measures of total body lean mass (kg) and fat mass (kg) from a standard whole body scan. A single technician conducted daily calibrations and obtained and analyzed all DXA scans (Apex 2.3 software). In our laboratory, short-term precision (CV%) for lean and fat mass with repositioning was 1.9 and 0.3, respectively, as determined in young adults (UBC Bone Health Research Group, unpublished data).
Maturity and dietary calcium
We used our recently revised sex-specific prediction equations [20] to estimate age at peak height velocity (APHV, years) in boys and girls. We calculated maturity offset (years) as chronological age—APHV, to generate a continuous measure of biological age. We also assessed girls’ maturity using self-reported menarcheal status, as menarche is a reliable indicator of sexual maturity that is related to peak bone mineral accrual [2] and accurately reported [21]. We asked girls to recall the date of their first menstrual period; we used prompts such as season (i.e., winter, spring), celebrations (i.e., Christmas, Thanksgiving) and school terms (i.e., exams, semester break), and grade in school to aid recall. We recorded day, month, and year. For girls who could recall the month and year only (85%), we used the 15th of the month as the date of menarche. All participants completed a valid food frequency questionnaire [22] to estimate dietary intake of calcium (mg/day).
Physical activity
As in our previous studies [11, 12], we measured physical activity and sedentary time objectively using ActiGraph GT1M uniaxial accelerometers (Actigraph, USA), which detect vertical accelerations of 0.05 to 2.00 g. We attached each accelerometer to an elastic belt that participants wore with the accelerometer positioned anteriorly at their right iliac crest. Accelerometer data were collected in 15-s epochs. We asked participants to wear the accelerometer during waking hours for seven consecutive days and to remove the device during showering and water-based activities. We provided participants with a log sheet to record accelerometer on and off times each day and activities they partook of while the accelerometer was off.
We defined non-wear time as 60 min of continuous zero counts [8]. The same technician downloaded and analyzed all accelerometer data using Kinesoft version 3.3.67 (Sasketchewan, Canada). We included data from participants who had a minimum of three valid days of wear (at least 10 h/day of wear time). Using validated cut-points [23], we classified VPAAccel (≥ 6 METs) as ≥ 4012 counts per minute (cpm), MVPAAccel (≥ 4 METs) as ≥ 2296 cpm, and sedentary time (< 1.5 METs) as < 100 cpm. We had 127 participants (45 boys, 82 girls) who agreed to wear an accelerometer for 7 days.
We also administered a modified version of the validated Physical Activity Questionnaire for Adolescents (PAQ-A) [24], a 7-day recall questionnaire used to estimate habitual PA. We report three outcomes from the PAQ-A: (1) a general PA score (1–5 Likert scale with 1 = low active and 5 = highly active); (2) MVPA (MVPAPAQ-A; min/day), based on frequency and duration of time spent in common activities (item 1 of the questionnaire); and (3) impact-loading physical activity (ImpactPAPAQ-A, h/week), based on frequency and duration of time spent in sports and activities designated as impact loading (impact > walking).
Bone strength, structure, and BMD
We used pQCT (XCT3000, Stratec Medizintechnik, Germany) to assess bone strength, structure, and BMD of the left distal tibia (8% site) and tibia midshaft (50% site) as in previous studies. The 8% site is a primarily trabecular bone site that does not span the growth plate [25]; the 50% site is a primarily cortical bone site that experiences high bending and torsional forces during loading [26]. Briefly, one experienced technologist first conducted a scout scan over the ankle joint to locate the distal end of the tibial plafond, the standard anatomical reference. Moving proximally from the reference line, we acquired a 2.3-mm slice at a scan speed of 30 mm/s with a voxel size of 0.4 mm at the 8% (distal) and 50% (midshaft) tibial sites. In the event of movement artifacts, the technologist repeated the scan once. We excluded eight scans due to movement at the distal tibia (three boys, five girls) and seven scans (three boys, four girls) at the tibial midshaft. To ensure quality control, the technologist conducted daily calibration with a cone phantom supplied by the manufacturer. Short-term precision (% CV) for repeated scans in 14 participants (aged 12–27 years) was less than 2% for all bone outcomes.
A trained technician analyzed all scans using Stratec software (version 6.0) to generate values for the following bone variables. At the distal tibia, we used contour mode 3 (200 mg/cm3) and peel mode 5 to determine total bone cross-sectional area (Tt.Ar, mm2) and total bone density (Tt.Dn, mg/cm3). We calculated bone strength index (BSI, mg2/mm4), an estimate of bone strength in compression, as Tt.Ar multiplied by Tt.Dn squared [27]. At the midshaft, we used contour mode 1 (710 mg/cm3) and peel mode 2 to determine Tt.Ar, cortical area (Ct.Ar, mm2) and cortical density (Ct.Dn, mg/cm3) and applied separation mode 1 (480 mg/cm3) to assess the polar stress strain index (SSIp, mm3), an estimate of bone strength in torsion [28]. We calculated medullary area (Me.Ar, mm2) of the tibial midshaft as the difference between Tt.Ar and Ct.Ar.
Statistical analyses
Using Stata version 10.1 (StataCorp, College Station, TX, USA), we first summarized (means, standard deviations) descriptive characteristics, physical activity, sedentary time, and bone outcomes for the full cohort (n = 192) and the subset of participants with valid accelerometer data (n = 101). We used independent t-tests to compare descriptive characteristics and bone outcomes between participants with and without valid accelerometer data.
We then used the xi: nestreg command in Stata to fit multivariable regression models to examine relations between MVPA and bone outcomes. Dependent variables at the distal tibia (8% site) included BSI, Tt.Ar, and Tt.Dn and at the tibial midshaft (50% site) SSIp, Tt.Ar, Ct.Ar, Me.Ar, and Ct.Dn. To address our objectives, we developed two or three multivariable regression models for each dependent variable depending on the PA predictor of interest. In model 1, we evaluated the contribution of PA (MVPAAccel, VPAAccel, MVPAPAQ, or ImpactPAPAQ) to bone strength, structure, and BMD controlling for sex, ethnicity (dummy variables: 0-White, 1-Asian, 2-Other), maturity offset, and tibial length (a surrogate for moment arm in the context of mechanostat theory). In model 2, we additionally adjusted for lean mass (as a surrogate for muscle force). For accelerometry-derived physical activity models (MVPA or VPA), we fit an additional model, model 3, adjusting for sedentary time. For accelerometry-derived sedentary time, we fit an additional model, model 3, adjusting for wear time. All regression models met the assumptions of normal distribution and homoscedasticity of residuals, had no influential points or variance inflation factor values > 2. We explored interaction terms between sex, maturity offset, and PA, but did not include them in the final model because they did not improve model fit. We report unstandardized (B) and standardized (ß) regression coefficients, standard errors (SE), and total variance explained (R2). We set the significance level at p < 0.05.
Results
Descriptive characteristics
We provide descriptive characteristics of participants in Table 1 and we summarize bone outcomes in Table 2. We acquired valid accelerometer data (minimum of 3 days of wear, ≥ 10 h/day) for 101 participants (74%). Descriptive characteristics of participants with valid accelerometer data were no different than participants from whom we did not acquire accelerometer data (n = 91) for stature, body mass, body composition, dietary calcium, self-reported physical activity, or bone outcomes.
For participants with valid accelerometer data (n = 101), MVPAAccel was moderately associated with self-reported MVPAPAQ-A (r = 0.33, p < 0.001) and ImpactPAPAQ (r = 0.23, p = 0.02). VPAAccel was not associated with ImpactPAPAQ (r = 0.15, p = 0.15). On average, participants spent approximately 6% of their day in MVPAAccel, 2% of their day in VPAAccel, and were sedentary for approximately 72% of total accelerometer wear time.
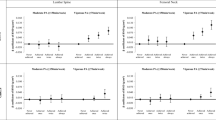
Accelerometry-derived physical activity and sedentary time in relation to bone outcomes
At the distal tibia, MVPAAccel was a positive predictor of BSI (6% of variance explained, p = 0.02) after controlling for covariates, but not after we accounted for lean mass (Table 3). VPAAccel was also a significant predictor of BSI (explained 7% of the variance, p = 0.01), and this association remained significant after adjusting for lean mass and sedentary time. Sedentary time was not a significant predictor of BSI. MVPAAccel, VPAAccel, and sedentary time were not significant predictors of Tt.Ar or Tt.Dn at the distal tibia (Supplementary Tables 1, 2 and 3).
At the tibial midshaft, MVPAAccel was a significant positive predictor of SSIp (explained 3% of the variance, p = 0.01) and this association remained significant after adjusting for lean mass and sedentary time (Table 3). In contrast, VPAAccel was not a significant predictor of SSIp. Similarly, sedentary time was not a significant predictor of SSIp. For bone structure and BMD outcomes, MVPAAccel positively predicted Tt.Ar and Ct.Ar (explained 2 and 3% of the variance, respectively, p < 0.05; Supplementary Table 1). The association between MVPAAccel and Ct.Ar was attenuated but remained significant after adjusting for lean mass, but was no longer significant after adjusting for sedentary time. VPAAccel also positively predicted Ct.Ar (explained 2% of the variance, p = 0.04), but this association was attenuated and no longer significant after adjusting for lean mass (Supplementary Table 2). Sedentary time was not associated with bone structure or BMD outcomes at the tibial midshaft (Supplementary Table 3).
Self-reported physical activity in relation to bone outcomes
At the distal tibia, MVPAPAQ-A was a significant predictor of BSI after controlling for maturity, ethnicity, and tibial length and accounted for 4% of the variance (p = 0.006, Table 3 and Fig. 1). However, MVPAPAQ-A was not a significant predictor of BSI after we added lean mass to the model (Fig. 1). In contrast, ImpactPAPAQ-A significantly predicted BSI after controlling for all covariates (explained 4% of the variance, p = 0.04), including lean body mass. MVPAPAQ-A was not a significant predictor of Tt.Ar or Tt.Dn whereas ImpactPAPAQ-A significantly predicted Tt.Dn, but not once we accounted for lean mass (Supplementary Tables 4 and 5).
Scatterplots of accelerometer-derived moderate-to-vigorous physical activity (MVPA) and VPA regression residuals and distal tibia bone strength index (BSI, mg2/cm4) (a, b) and tibial midshaft polar strength strain index (SSIp, mm3) (c, d). Solid circles and lines represent the relation of MVPAaccel or VPAaccel to BSI or SSIp adjusted for sex, tibial length, ethnicity, and maturity offset. Open circles and dashed lines represent the relation of MVPA or VPA to BSI or SSIp additionally adjusted for lean mass.. R2 indicate variance explained by PA variable
In adjusted models at the tibial midshaft, MVPAPAQ-A and ImpactPAPAQ-A were positive predictors of SSIp and accounted for 2% of the variance (p < 0.01, Table 3 and Fig. 1). However, MVPAPAQ-A and ImpactPAPAQ-A were no longer significant predictors of SSIp after adjusting for lean mass (Fig. 1). MVPAPAQ-A and ImpactPAPAQ-A also positively predicted Tt.Ar and Ct.Ar and accounted for 1–4% of the variance (p < 0.01, Supplementary Tables 4 and 5). The strength of these associations was attenuated after adjusting for lean mass, but MVPAPAQ-A and ImpactPAPAQ-A remained significant predictors of Ct.Ar, but not Tt.Ar.
Comparison of bone outcomes between sexes was not a specific objective of our study; however, we noted a general trend across all models whereby sex was not a significant predictor of bone strength or structure after we adjusted for lean mass. Exceptions included models for BSI, Tt.Dn, and Ct.Dn with accelerometry-derived physical activity. Specifically, in the adjusted model with MVPAAccel, sex was a significant predictor of BSI after adjusting for lean mass (girls > boys, B = 2069.6, SE = 1033.5, p = 0.048), but the sex difference in BSI was not apparent after we added sedentary time to the model. In contrast, in the adjusted models with MVPAAccel, sex differences in Tt.Dn (girls > boys, B = 64.3, SE = 29.6, p = 0.03) and Ct.Dn (girls > boys, B = 31.4, SE = 13.3, p = 0.02) persisted after adjusting for lean mass and sedentary time. A similar picture emerged in adjusted models with VPAAccel; sex remained a significant predictor of BSI, Tt.Dn, and Ct.Dn (girls > boys for all 3) after adjusting for lean mass and sedentary time. In contrast, in models with self-reported physical activity, sex only remained a significant predictor of Ct.Ar in the adjusted model with MVPAPAQ-A (girls > boys, B = 24.9, SE = 11.5, p = 0.03).
Discussion
We extend a relatively scant body of literature that reports bone strength, structure, and BMD at the distal and midshaft tibia and their association with objectively measured physical activity and sedentary time in older adolescents. Adolescents who participated in more physical activity, measured objectively and by self-report, had greater bone strength at the distal and midshaft sites of the tibia. Lean mass, a surrogate for muscle force, appeared to mediate the physical activity-bone strength association. Despite spending most of their day in sedentary pursuits, adolescents’ bone strength was not negatively influenced by sedentary time.
Objective measures of physical activity and sedentary time are unique aspects of our study. However, we acknowledge that participation in this component of our study was limited, as less than 50% of boys agreed to wear accelerometers for 7 days. We did not follow up with participants who chose not to wear the accelerometer to identify barriers to wear. However, adolescents reported barriers to wear such as bullying risk, feelings of embarrassment, and concerns about size and comfort of the devices [29]. Compliance with accelerometer wear among adolescents who volunteered for this part of the study (74%) was higher, on average, than previous studies of this age group [30]. Our findings highlight the need to explore the use of incentives and/or wrist-worn accelerometers, which youth may prefer [31]. Wrist-worn devices and traditional hip-worn accelerometers were similary associated with ground-reaction forces [32].
Both objective and subjective measures of physical activity positively predicted adolescents’ bone strength at the distal tibia and tibial shaft. We were unable to relate the specific physical activities participants engaged in to intensity as measured by accelerometry. However, based on participants’ PAQ-A responses, common activities included walking, soccer, basketball, and volleyball and 5% of participants were involved in weight-bearing organized sport. Overall, the physical activity-bone strength relationships we observed align with those of our previous cross-sectional [7, 11, 33] and longitudinal pQCT and HR-pQCT studies [12] as well as those of others who reported positive associations between accelerometry-derived physical activity and bone strength and structure in older adolescents [6, 8]. However, we extend this literature by clarifying the role of sedentary time in this population. Our data suggest that adolescents who are physically active counter the potential detrimental effect of large bouts of sedentary time.
Lean mass, a surrogate for muscle force, mediated the relationship between physical activity and tibial bone strength. Interestingly, the influence of lean mass varied between skeletal sites and how physical activity was measured. Our findings for VPA and MVPA at the distal and midshaft tibia align with earlier DXA- and pQCT-based studies of recreationally active adolescents [34] and non-elite gymnasts. In these studies, differences in bone outcomes between active and inactive youth and between gymnasts and non-gymnasts did not persist after indices of muscle force were accounted for. In contrast, our findings for VPA at the tibial midshaft align with DXA-based results from the Iowa Bone Development Study. In that study, residual variance in boys’ femoral neck cross-sectional area and section modulus (by hip structure analysis) was explained by MVPAAccel after lean mass was accounted for [17]. Thus, physical activity influences change in muscle forces that in turn, impart the largest loads on bone. However, our findings suggest a possible direct link between non-muscular factors associated with weight-bearing activity and bone adaptation.
Importantly, within these general observations, we noted site-specific relationships between physical activity intensity and bone strength after adjusting for lean mass. The distal tibia experiences high compressive loads during regular locomotion. Thus, the association between bone strength and high-intensity physical activity (VPAAccel; but not MVPAAccel) suggests that more intense stimuli are needed to trigger bone adapation at this weight-bearing site. Further, self-reported impact physical activity predicted bone strength whereas moderate physical activity did not (after adjusting for lean mass). In contrast, the tibial shaft incurs mainly torsional and bending loads and moderate levels of physical activity predicted bone strength at that site, after adjusting for lean mass. It is not clear why intense physical activity did not predict bone strength at that site, but it may be due to our limited sample size or the large variability in VPAAccel as compared with MVPAAccel. We note, however, a positive association between VPAAccel and SSIp that approached significance (B = − 0.1, SE = 9.4; p = 0.055). Adequately powered longitudinal studies would clarify the biological significance of these relationships.
Extreme and prolonged periods of bedrest may upset the bone formation-resorption balance in adults [35]. However, the mechanism by which sedentary time influences adolescent bone strength is not known. Notably, participants in our cohort were sedentary for most of their waking hours. However, this was countered by almost 50 min/day of physical activity, on average, which exceeds the national MVPA average of 39 min/day [10]. Thus, the influence of sedentary time on bone outcomes appears to be offset by adolescents’ participation in moderately intense physical activity. In contrast, sedentary time was negatively associated with whole body bone mineral content (BMC; by DXA) in adolescents [14] and proximal femur BMC in children, adolescents, and young adults [13]. Body size and maturation were not controlled for in the DXA-based studies. Alternatively, self-reported sitting time was negatively associated with bone strength (SSIp by pQCT) at the 20% site of the tibia in 6- to 20-year olds (mediated by lean mass). Longitudinal studies are needed to examine how different trajectories of sedentary time across childhood and adolescence influence bone strength accrual.
We acknowledge several limitations of our study. First, based on its cross-sectional design, we cannot infer causality. Second, we were unable to assess stage of maturation using the method of Tanner due to ethical concerns raised by the participating School Districts. Bone age assessments were also not feasible in our study, as our Mobile Laboratory is not equipped with standard X-ray technology. We therefore estimated biological age using a valid prediction equation. At age 15 years, girls were 2.5 years and boys 2 years post-APHV, on average. In our mixed longitudinal Healthy Bones III Study, 53 and 44% of girls self-reported as Tanner stage 4 and 5, respectively, at age 15 and 57 and 36% of boys self-reported as Tanner stage 4 and 5, respectively, at age 15 (unpublished data). Given similarities in demographic characteristics between cohorts, we would expect a similar distribution of Tanner stages in the HPSS cohort. However, we acknowledge that our results may not apply to adolescents of other ages or stages of maturity. Third, to estimate APHV and determine maturity offset, we used a prediction equation validated in white youth only [20]. As Asian children are known to mature earlier as compared with their white peers [36], we may have underestimated APHV in Asian adolescents in our cohort.
In conclusion, beyond the critical period of peak bone accrual, high-intensity physical activity continues to influence adolescent bone strength. However, muscle force should be considered as a potential mediator in models that investigate physical activity-bone strength relationship. Further, intervention studies that objectively evaluate physical activity dose (frequency, duration, intensity) independent of sedentary time (quantity, patterns) are needed to better understand their shared and counteractive effects on bone strength in adolescents. Finally, studies that more objectively and precisely differentiate between high- versus moderate- or low-intensity physical activity would allow us to better understand their contributions to bone strength accrual during growth.
References
Baxter-Jones ADG, Faulkner RA, Forwood MR, Mirwald RL, Bailey DA (2011) Bone mineral accrual from 8 to 30 years of age: an estimation of peak bone mass. J Bone Miner Res 26:1729–1739
Bailey DA, McKay HA, Mirwald RL, Crocker PR, Faulkner RA (1999) A six-year longitudinal study of the relationship of physical activity to bone mineral accrual in growing children: the University of Saskatchewan Bone Mineral Accrual Study. J Bone Miner Res 14:1672–1679
Tan VPS, Macdonald HM, Kim S, Nettlefold L, Gabel L, Ashe MC, McKay HA (2014) Influence of physical activity on bone strength in children and adolescents: a systematic review and narrative synthesis. J Bone Miner Res 29:2161–2181
van der Meulen MC, Ashford MW, Kiratli BJ, Bachrach LK, Carter DR (1996) Determinants of femoral geometry and structure during adolescent growth. J Orthop Res 14:22–29
van der Meulen MC, Moro M, Kiratli BJ, Marcus R, Bachrach LK (2000) Mechanobiology of femoral neck structure during adolescence. J Rehabil Res Dev 37:201–208
Sayers A, Mattocks C, Deere K, Ness A, Riddoch C, Tobias JH (2011) Habitual levels of vigorous, but not moderate or light, physical activity is positively related to cortical bone mass in adolescents. J Clin Endocrinol Metab 96:E793–E802
McKay H, Liu D, Egeli D, Boyd S, Burrows M (2011) Physical activity positively predicts bone architecture and bone strength in adolescent males and females. Acta Paediatr 100:97–101
Janz KF, Letuchy EM, Burns TL, Eichenberger Gilmore JM, Torner JC, Levy SM (2014) Objectively measured physical activity trajectories predict adolescent bone strength: Iowa bone development study. Br J Sports Med 48:1032–1036
Hallal PC, Andersen LB, Bull FC, Guthold R, Haskell W, Ekelund U, Lancet Physical Activity Series Working Group (2012) Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet 380:247–257
Colley RC, Garriguet D, Janssen I, Craig CL, Clarke J, Tremblay MS (2011) Physical activity of Canadian children and youth: accelerometer results from the 2007 to 2009 Canadian health measures survey. Health Rep 22:15–23
Gabel L, McKay HA, Nettlefold L, Race D, Macdonald HM (2015) Bone architecture and strength in the growing skeleton: the role of sedentary time. Med Sci Sports Exerc 47:363–372
Gabel L, Macdonald HM, Nettlefold L, McKay HA (2017) Physical activity, sedentary time, and bone strength from childhood to early adulthood: a mixed longitudinal HR-pQCT study. J Bone Miner Res 32:1525–1536
Chastin SFM, Mandrichenko O, Helbostadt JL, Skelton DA (2014) Associations between objectively-measured sedentary behaviour and physical activity with bone mineral density in adults and older adults, the NHANES study. Bone 64:254–262
Gracia-Marco L, Rey-Lopez JP, Santaliestra-Pasías AM, Jiménez-Pavón D, Díaz LE, Moreno LA, Vicente-Rodríguez G (2012) Sedentary behaviours and its association with bone mass in adolescents: the HELENA cross-sectional study. BMC Public Health 12:1–1
Binkley TL, Specker BL (2016) The negative effect of sitting time on bone is mediated by lean mass in pubertal children. J Musculoskelet Neuronal Interact 16:18–23
Frost HM (1987) Bone "mass" and the “mechanostat”: a proposal. Anat Rec 219:1–9
Janz KF, Gilmore JME, Levy SM, Letuchy EM, Burns TL, Beck TJ (2007) Physical activity and femoral neck bone strength during childhood: the Iowa bone development study. Bone 41:216–222
Erlandson MC, Kontulainen SA, Baxter-Jones ADG (2011) Precompetitive and recreational gymnasts have greater bone density, mass, and estimated strength at the distal radius in young childhood. Osteoporos Int 22:75–84
Wharf Higgins J, Naylor PJ, Bellows Riecken K, Gibbons S, Rhodes R, Sulz L, McKay H (2014) One, two, three strikes and You're out? Examining youth physical activity in the context of the health promoting secondary schools model and teacher job action. Educ Health 32:110–117
Moore SA, McKay HA, Macdonald H, Nettlefold L, Baxter-Jones ADJ, Cameron N, Brasher PM (2015) Enhancing a somatic maturity prediction model. Med Sci Sports Exerc 47:1755–1764
Koo MM, Rohan TE (1997) Accuracy of short-term recall of age at menarche. Ann Hum Biol 24:61–64
Barr SI (1994) Associations of social and demographic variables with calcium intakes of high school students. J Am Diet Assoc 94:260–266
Evenson KR, Catellier DJ, Gill K, Ondrak KS, McMurray RG (2008) Calibration of two objective measures of physical activity for children. J Sports Sci 26:1557–1565
Kowalski KC, Crocker P, Faulkner RA (1997) Validation of the physical activity questionnaire for older children. Pediatr Exerc Sci 9:174–186
Burrows M, Liu D, Ahamed Y et al (2008) High-resolution peripheral QCT imaging of bone micro-structure in adolescents. Osteoporos Int 21:515–520
Burr DB, Milgrom C, Fyhrie D, Forwood M, Nyska M, Finestone A, Hoshaw S, Salag E, Simkin A (1996) In vivo measurement of human tibial strains during vigorous activity. Bone 18:405–410
Kontulainen SA, Johnston JD, Liu D, Leung C, Oxland TR, McKay HA (2008) Strength indices from pQCT imaging predict up to 85% of variance in bone failure properties at tibial epiphysis and diaphysis. J Musculoskelet Neuronal Interact 8:401–409
Schiessl H, Ferretti JL, Tysarczyk-Niemeyer G, Willnecker J (1995) Noninvasive bone strength index as analyzed by peripheral quantitative computed tomography (pQCT). In: Schönau E (ed) Paediatric osteology: new developments in diagnostics and therapy. Elsevier, Amsterdam, pp 141–114
Kirby J, Tibbins C, Callens C, Lang B, Thorogood M, Tigbe W, Robertson W (2012) Young People's views on accelerometer use in physical activity research: findings from a user involvement investigation. ISRN Obes 2012:948504
Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M (2008) Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc 40:181–188
Scott JJ, Rowlands AV, Cliff DP, Morgan PJ, Plotnikoff RC, Lubans DR (2017) Comparability and feasibility of wrist- and hip-worn accelerometers in free-living adolescents. J Sci Med Sport 20:1101–1106
Rowlands AV, Stiles VH (2012) Journal of biomechanics. J Biomech 45:448–454
Macdonald H, Kontulainen S, Petit M, Janssen P, McKay H (2006) Bone strength and its determinants in pre- and early pubertal boys and girls. Bone 39:598–608
Forwood MR, Baxter-Jones AD, Beck TJ, Mirwald RL, Howard A, Bailey DA (2006) Physical activity and strength of the femoral neck during the adolescent growth spurt: a longitudinal analysis. Bone 38:576–583
Zerwekh JE, Ruml LA, Gottschalk F, Pak CY (1998) The effects of twelve weeks of bed rest on bone histology, biochemical markers of bone turnover, and calcium homeostasis in eleven normal subjects. J Bone Miner Res 13:1594–1601
Eveleth PB, Tanner JM (1990) Worldwide variation in human growth. Cambridge University Press
Acknowledgements
We gratefully acknowledge the HPSS Bone Health Study participants and their families along with the support of teachers and principals from participating schools. Our heartfelt gratitude to the main HPSS research team, from both UBC and UVIC, for their teamwork, recruitment efforts, and overall research management; to the Bone Health Study team—SoJung Kim and Paul Drexler for their dedicated and quality data collection efforts; Douglas Race, for accelerometer data management and participant scheduling; and especially to Dr. Danmei Liu for supervising and training bone imaging technicians and for her invaluable input in image acquisition and processing.
Funding
This study was funded by a Catalyst Grant from the Canadian Institutes of Health Research (227967). The authors declare no competing financial interests.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The University of British Columbia’s Clinical and Behavioural Research Ethics Boards (H10-01917), University of Victoria’s Human Research Ethics Board (10-168), and participating school districts approved all study procedures.
Conflicts of interest
None.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Tan, V.P., Macdonald, H.M., Gabel, L. et al. Physical activity, but not sedentary time, influences bone strength in late adolescence. Arch Osteoporos 13, 31 (2018). https://doi.org/10.1007/s11657-018-0441-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-018-0441-9