Abstract
Introduction
No study is available summarizing earlier publications on the association between metformin use and risk of fracture. This systematic review and meta-analysis were conducted to summarize earlier findings on the association between metformin use and risk of fracture.
Methods
We conducted a systematic search on all published articles up to October 2018 using online databases including PubMed/Medline, ISI Web of Science, and Scopus. Observational studies that considered metformin use as the exposure variable and bone fracture as the main outcome variable or as one of the outcome variables and participants included were 18 years and older were included in the systematic review. Publications in which hazard ratios (HRs), rate or risk ratios (RRs), or odds ratios (ORs) were reported as effect size were included in the meta-analysis.
Results
Totally, three cohort studies, one cross-sectional study, one nested case-control study, and one case-control study were included in this systematic review and meta-analysis. When seven effect sizes from six studies were combined, a significant inverse association between metformin use and risk of fracture was observed (RR 0.82; 95% CI 0.72, 0.93). No significant between-study heterogeneity was found (I2 = 22.4%, Pheterogeneity = 0.25). In addition, no evidence of publication bias was seen using Egger’s test (P = 0.99).
Conclusion
We found that metformin use was inversely associated with the risk of fracture.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bone disorders, including osteoporosis and fractures, are major health concerns that can impose a huge burden on the individual and healthcare systems [1]. It has been estimated that osteoporosis leads to more than 8.9 million fractures annually in the world [2]. Bone fractures are associated with increased risk of disability, morbidity, and mortality [3]. Therefore, finding modifiable risk factors of fracture have attracted huge attention.
People with diabetes are at higher risk of bone fractures than those without diabetes [4]. It seems that oral hypoglycemic agents affect bone metabolism [5]. Metformin is the first-line pharmacological therapy in the management of type 2 diabetes [6]. Previous studies have investigated the association between metformin use and risk of fracture; however, results are inconsistent. A case-control study in Denmark reported an inverse association between metformin use and fracture risk [7]. This was also confirmed by a historical cohort study in which treatment with biguanides was protectively associated with risk of fracture [8]. In a cross-sectional study in Japan, metformin use was not associated with risk of fracture [9]. Such findings were also reported by prospective cohort studies [10,11,12]. However, in a cohort study in Scotland, metformin use was significantly associated with increased risk of hip fracture [13].
To the best of our knowledge, no previous systematic review and meta-analysis have summarized findings from earlier studies on the association between metformin use and risk of fracture. Therefore, we aimed to conduct a comprehensive systematic review and meta-analysis to summarize available data on the association between metformin use and risk of fracture.
Method and materials
Search strategy
We conducted a systematic search on all articles published until October 2018 using online databases including PubMed/Medline, ISI Web of Science, and Scopus using the following keywords: (“Metformin” OR “Glucophage” OR “dimethylbiguanide” OR “dimethylguanylguanidine” OR “metformin HCI”) AND (“bone” OR “bone fracture” OR “fracture” OR “osteoporotic fracture” OR “broken bone” OR “bone mineral density” OR “BMD” OR “bone mass density” OR “osteoporosis” OR “bone health”). We did not apply any language or time restrictions in this study. In addition, we did not include unpublished studies and gray literature. Then, a manual search was performed using references from studies already chosen for inclusion to avoid missing any relevant publications. Two reviewers screened the output of the search independently to identify potentially eligible studies.
Inclusion criteria
Each title and abstract was reviewed to identify relevant papers. Full texts of the articles were reviewed if the abstract deemed potentially relevant. Studies with the following criteria were eligible for inclusion: (1) observational studies that considered metformin as the exposure variable and fracture as the main outcome variable or as one of the outcome variables, (2) participants included were 18 years and older, and (3) odds ratios (ORs), rate or risk ratios (RRs), or hazard ratios (HRs) were reported as effect sizes (Table 1).
Exclusion criteria
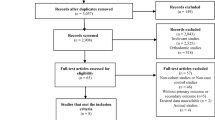
Letters, commentaries, reviews, and ecological and animal studies were excluded. In our initial search, 905 articles were identified. After elimination of duplicates, 483 papers remained. Finally, 465 studies were excluded on the basis of title and abstract and 18 potentially related articles remained for further assessment. There were eight clinical trials that assessed the effects of metformin use on BMD [14,15,16,17,18,19,20,21]. Since metformin use was compared with other medications, not with placebo in these eight studies, we excluded them from our review. The other four papers were excluded for the following reasons: one had reported the association between combination of biguanides, not just metformin, and risk of fracture [8], one had considered both children and adult population [7], and one had reported no effect size for the association between metformin use and risk of fracture [22]. In another study [23], the authors had reported the risk of fracture in the people with diabetes compared with those without diabetes and no comparison was made for the risk of fracture between patients who were on metformin and those who were not on this medication. Therefore, we excluded that study from our review. After these exclusions, six observational studies [9,10,11,12,13, 24] were considered for inclusion in this systematic review and meta-analysis (Fig. 1).
Data extraction
Two authors (ASM and OS) independently extracted the following data: first author’s last name, publication year, study design, country, follow-up duration, participants’ mean age or age range, sex, sample size, number of cases, outcome variables, methods used for assessment of fracture, comparison, the maximally adjusted ORs, RRs, or HRs with the corresponding 95% confidence intervals (CIs), and adjustments for potential confounders (Table 1). Any disagreements between the two reviewers were resolved in consultation with the principal investigator (AE).
Quality assessment of studies
The quality of studies included in this systematic review and meta-analysis was evaluated by the Newcastle-Ottawa Scale (NOS) [25]. Based on the NOS method, a maximum of 9 scores can be awarded to each study. In the current analysis, studies with quality scores of > 6 were considered high-quality studies; otherwise, studies were considered to be of low quality.
Statistical analysis
All reported ORs, RRs, and HRs and their 95% CIs for the risk of fracture were used to calculate log RRs and their standard errors (SEs). The overall effect size was calculated using the random effects model which incorporate between-study heterogeneity. Between-study heterogeneity was examined using Cochrane’s Q test and I-squared. Sensitivity analysis was used to explore the extent to which inferences might depend on a particular study or group of studies. Publication bias was assessed by visual inspection of funnel plots. Formal statistical assessment of funnel plot asymmetry was done using Egger’s regression asymmetry test. Statistical analyses were done using Stata MP software, version 14. P values < 0.05 were considered statistically significant.
Results
Study characteristics
Out of 905 retrieved papers, six studies including three cohort studies [10, 11, 13], one cross-sectional study [9], one nested case-control study [12], and one case-control study [24] were included in this systematic review and meta-analysis. Summary of these studies is provided in Table 1. These studies included 248,916 participants aged ≥ 20 years and were published between 2008 and 2016. Two studies were conducted in the USA [10, 11] and one each from Italy [12], Scotland [13], Japan [9], and Singapore [24]. Five studies were performed among both genders [9, 10, 12, 13, 24] and one study was performed on men only [11]. For fracture assessment, the included studies had used different methods including diagnosis by physician [10], self-reported questionnaire [11], X-ray [9], record linkage [13], and hospital discharge information [10, 12, 24]. Included studies had controlled the analyses for age (n = 5), sex (n = 3), race/ethnicity (n = 2), and duration of diabetes (n = 2).
Findings from the systematic review
Two cohort studies failed to find any significant association between metformin use and risk of fracture [10, 11]. However, findings from another cohort study revealed a significant inverse association between metformin use and risk of hip fracture [13]. In a cross-sectional study in Japan, the investigators observed no significant association between metformin use and risk of vertebral fracture in either gender [9]. A nested case-control study did not find a significant association between metformin use and risk of bone fractures [12]. In a case-control study in Singapore, a significant inverse association was reported between metformin use and risk of hip fracture [24].
Findings from the meta-analysis
There were three cohort studies [10, 11, 13], one cross-sectional study [9], one nested case-control study [12], and one case-control study [24] that examined the association between metformin use and risk of fracture. The study of Kanazawa et al., that had reported ORs separately for men and women, was considered as two separate studies [9]. Therefore, we had seven effect sizes obtained from six studies in this meta-analysis. When seven effect sizes were combined, a significant inverse association between metformin use and risk of fracture was found (RR 0.82; 95% CI 0.72, 0.93) (Fig. 2). No significant between-study heterogeneity was seen (I2 = 22.4%, Pheterogeneity = 0.25). In the sensitivity analysis, we found that no particular study influenced the findings significantly. In addition, we found no evidence of publication bias using Egger’s test (P = 0.99).
Discussion
In this systematic review and meta-analysis, we found a significant inverse association between metformin use and risk of fracture. To the best of our knowledge, this is the first systematic review and meta-analysis that summarize earlier publications on the association between metformin use and risk of fracture.
Individuals with diabetes are at higher risk of fracture and have worse fracture outcomes than individuals without diabetes [26]. Among several factors that might influence the risk of fracture, significant attention has been paid to glucose-lowering medications [5]. Several studies examined the association between metformin use and risk of fracture; however, results are contradictory. As pooling information can provide more precise results than those obtained from individual studies, we conducted a meta-analysis to summarize findings from previous studies on the association between metformin use and risk of fracture. In this systematic review and meta-analysis, we found a significant inverse association between metformin use and risk of fracture. In line with our results, a historical cohort study in the USA showed that treatment with biguanides was protectively associated with risk of fracture [8]. Vestergaard et al. reported that metformin use was associated with a significantly decreased risk of any fractures [7]. However, we did not include that study in our review because both children and adults were recruited into the study. Since the cause of fracture in children might be different from that in adults, we did not consider this publication in the analysis. In addition, Vestergaard et al. had included all types of fractures including fractures from high-energy trauma in their study, which made this study non-comparable to other studies. However, it must be kept in mind that all available studies on the association between metformin use and risk of fracture were of observational design. Limitations originating from observational studies must also be taken into account. In addition, due to limited number of studies on this subject, further studies are required on this topic.
The mechanisms through which metformin might protect against risk of fracture are not well understood yet. It has been shown that metformin stimulates osteoblastic cell differentiation and bone matrix synthesis through the activation of adenosine 5-monophosphate-activated protein kinase and expression of bone morphogenetic protein-2 [27]. Metformin also prevents advanced glycation end products–induced (AGE) alterations in osteoblastic cells [28] and inhibits formation of reactive oxygen species (ROS) and apoptosis in osteoblasts [29]. Given these findings, it seems that metformin may have a protective effect against risk of fracture.
Being the first systematic review and meta-analysis on the association between metformin use and risk of fracture is the strength of this study. However, some points need to be considered when interpreting our results. Our meta-analysis included a relatively small number of studies. Therefore, these results must be interpreted cautiously. Although all available studies were included, we excluded some studies due to the lack of required data for statistical analysis. Due to the small number of studies, we could not examine the association of metformin use and fracture in different sites and we had to combine fractures from all sites. We also limited our search to published studies only. Although we found no significant evidence of publication bias, lack of considering gray literature might have influenced our findings. In addition, studies included in our systematic review and meta-analysis differed in terms of methods used for assessing bone fractures (self-reported compared with record linkage, X-ray, and by physician and hospital discharge information).
In conclusion, summarizing earlier findings, we observed a significant inverse association between metformin use and risk of fracture. Due to limited information in this regard, further studies are required to reach a definite conclusion.
Abbreviations
- AGE:
-
Advanced glycation end products
- BMD:
-
Bone mineral density
- CI:
-
Confidence interval
- F:
-
Female
- HR:
-
Hazard ratio
- M:
-
Male
- NOS:
-
Newcastle-Ottawa Scale
- OR:
-
Odds ratio
- ROS:
-
Reactive oxygen species
- RR:
-
Risk ratio
- SE:
-
Standard error
References
Rivas A, Romero A, Mariscal-Arcas M, Monteagudo C, Feriche B, Lorenzo ML, Olea F (2013) Mediterranean diet and bone mineral density in two age groups of women. Int J Food Sci Nutr 64(2):155–161
Hernlund E, Svedbom A, Ivergard M, Compston J, Cooper C, Stenmark J, McCloskey EV, Jönsson B, Kanis JA (2013) Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 8:136
Feart C, Lorrain S, Ginder Coupez V, Samieri C, Letenneur L, Paineau D, Barberger-Gateau P (2013) Adherence to a Mediterranean diet and risk of fractures in French older persons. Osteoporos Int 24(12):3031–3041
Janghorbani M, Van Dam RM, Willett WC, Hu FB (2007) Systematic review of type 1 and type 2 diabetes mellitus and risk of fracture. Am J Epidemiol 166(5):495–505
Palermo A, D’Onofrio L, Eastell R, Schwartz AV, Pozzilli P, Napoli N (2015) Oral anti-diabetic drugs and fracture risk, cut to the bone: safe or dangerous? A narrative review. Osteoporos Int 26(8):2073–2089
Gu Q, Gu Y, Yang H, Shi Q (2017) Metformin enhances osteogenesis and suppresses adipogenesis of human chorionic villous mesenchymal stem cells. Tohoku J Exp Med 241(1):13–19
Vestergaard P, Rejnmark L, Mosekilde L (2005) Relative fracture risk in patients with diabetes mellitus, and the impact of insulin and oral antidiabetic medication on relative fracture risk. Diabetologia 48(7):1292–1299
Melton LJ III, Leibson CL, Achenbach SJ, Therneau TM, Khosla S (2008) Fracture risk in type 2 diabetes: update of a population-based study. J Bone Miner Res 23(8):1334–1342
Kanazawa I, Yamaguchi T, Yamamoto M, Sugimoto T (2010) Relationship between treatments with insulin and oral hypoglycemic agents versus the presence of vertebral fractures in type 2 diabetes mellitus. J Bone Miner Metab 28(5):554–560
Majumdar SR, Josse RG, Lin M, Eurich DT (2016) Does sitagliptin affect the rate of osteoporotic fractures in type 2 diabetes? Population-based cohort study. J Clin Endocrinol Metab 101(5):1963–1969
Napoli N, Strotmeyer ES, Ensrud KE, Sellmeyer DE, Bauer DC, Hoffman AR, Dam TT, Barrett-Connor E, Palermo L, Orwoll ES et al (2014) Fracture risk in diabetic elderly men: the MrOS study. Diabetologia 57(10):2057–2065
Monami M, Cresci B, Colombini A, Pala L, Balzi D, Gori F, Chiasserini V, Marchionni N, Rotella CM, Mannucci E (2008) Bone fractures and hypoglycemic treatment in type 2 diabetic patients: a case-control study. Diabetes Care 31(2):199–203
Colhoun HM, Livingstone SJ, Looker HC, Morris AD, Wild SH, Lindsay RS, Reed C, Donnan PT, Guthrie B, Leese GP et al (2012) Hospitalised hip fracture risk with rosiglitazone and pioglitazone use compared with other glucose-lowering drugs. Diabetologia 55(11):2929–2937
de Zegher F, Garcia Beltran C, Lopez-Bermejo A, Ibanez L (2018) Metformin for rapidly maturing girls with central adiposity: less liver fat and slower bone maturation. Horm Res Paediatr 89(2):136–140
Hegazy SK (2015) Evaluation of the anti-osteoporotic effects of metformin and sitagliptin in postmenopausal diabetic women. J Bone Miner Metab 33(2):207–212
Bilezikian JP, Josse RG, Eastell R, Lewiecki EM, Miller CG, Wooddell M, Northcutt AR, Kravitz BG, Paul G, Cobitz AR, Nino AJ, Fitzpatrick LA (2013) Rosiglitazone decreases bone mineral density and increases bone turnover in postmenopausal women with type 2 diabetes mellitus. J Clin Endocrinol Metab 98(4):1519–1528
Borges JL, Bilezikian JP, Jones-Leone AR, Acusta AP, Ambery PD, Nino AJ, Grosse M, Fitzpatrick LA, Cobitz AR (2011) A randomized, parallel group, double-blind, multicentre study comparing the efficacy and safety of Avandamet (rosiglitazone/metformin) and metformin on long-term glycaemic control and bone mineral density after 80 weeks of treatment in drug-naive type 2 diabetes mellitus patients. Diabetes Obes Metab 13(11):1036–1046
Ladson G, Dodson WC, Sweet SD, Archibong AE, Kunselman AR, Demers LM, Williams NI, Coney P, Legro RS (2011) The effects of metformin with lifestyle therapy in polycystic ovary syndrome: a randomized double-blind study. Fertil Steril 95(3):1059–1066
Dutta M, Pakhetra R, Garg M (2012) Evaluation of bone mineral density in type 2 diabetes mellitus patients before and after treatment. Med J Armed Forces India 68(1):48–52
Kahn SE, Zinman B, Lachin JM, Haffner SM, Herman WH, Holman RR, Kravitz BG, Yu D, Heise MA, Aftring RP, Viberti G, for the A Diabetes Outcome Progression Trial (ADOPT) Study Group (2008) Rosiglitazone-associated fractures in type 2 diabetes: an analysis from a diabetes outcome progression trial (ADOPT). Diabetes Care 31(5):845–851
Kanazawa I, Yamaguchi T, Yano S, Yamamoto M, Yamauchi M, Kurioka S, Sugimoto T (2010) Baseline atherosclerosis parameter could assess the risk of bone loss during pioglitazone treatment in type 2 diabetes mellitus. Osteoporos Int 21(12):2013–2018
Solomon DH, Cadarette SM, Choudhry NK, Canning C, Levin R, Sturmer T (2009) A cohort study of thiazolidinediones and fractures in older adults with diabetes. J Clin Endocrinol Metab 94(8):2792–2798
Napoli N, Schwartz AV, Schafer AL, Vittinghoff E, Cawthon PM, Parimi N, Orwoll E, Strotmeyer ES, Hoffman AR, Barrett-Connor E, Black DM, for the Osteoporotic Fractures in Men (MrOS) Study Research Group (2018) Vertebral fracture risk in diabetic elderly men: the MrOS study. J Bone Miner Res 33(1):63–69
Puar TH, Khoo JJ, Cho LW, Xu Y, Chen YT, Chuo AM, Poh CB, Ng JM (2012) Association between glycemic control and hip fracture. J Am Geriatr Soc 60(8):1493–1497
Wells GASB, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P (2009) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa Hospital Research Institute, Ottawa
Sellmeyer DE, Civitelli R, Hofbauer LC, Khosla S, Lecka-Czernik B, Schwartz AV (2016) Skeletal metabolism, fracture risk, and fracture outcomes in type 1 and type 2 diabetes. Diabetes 65(7):1757–1766
Kanazawa I, Yamaguchi T, Yano S, Yamauchi M, Sugimoto T (2008) Metformin enhances the differentiation and mineralization of osteoblastic MC3T3-E1 cells via AMP kinase activation as well as eNOS and BMP-2 expression. Biochem Biophys Res Commun 375(3):414–419
Schurman L, McCarthy AD, Sedlinsky C, Gangoiti MV, Arnol V, Bruzzone L, Cortizo AM (2008) Metformin reverts deleterious effects of advanced glycation end-products (AGEs) on osteoblastic cells. Exp Clin Endocrinol Diabetes 116(6):333–340
Zhen D, Chen Y, Tang X (2010) Metformin reverses the deleterious effects of high glucose on osteoblast function. J Diabetes Complicat 24(5):334–344
Acknowledgments
The authors wish to thank Cheryl Nickurak RD, Edmonton, Canada, for her help in editing the final version of the manuscript.
Funding
This study was financially supported by the Tehran University of Medical Sciences, Tehran, Iran.
Author information
Authors and Affiliations
Contributions
ASM and OS contributed to the conception, design, search, statistical analyses, data interpretation, and manuscript drafting. AHK contributed to the manuscript drafting. BL contributed to the design, data interpretation, and manuscript drafting. AE contributed to the conception, design, statistical analyses, data interpretation, and manuscript drafting. AE supervised the study. All authors approved the final manuscript for submission.
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Salari-Moghaddam, A., Sadeghi, O., Keshteli, A.H. et al. Metformin use and risk of fracture: a systematic review and meta-analysis of observational studies. Osteoporos Int 30, 1167–1173 (2019). https://doi.org/10.1007/s00198-019-04948-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-019-04948-1