Abstract
Summary
Perceived stress is associated with several adverse health outcomes; however, little is known about the impact of stress on fracture risk. In this population-based cohort study, persons with high perceived stress have an increased 5-year risk of any osteoporotic fracture, in particular hip fracture.
Introduction
We conducted a population-based cohort study in Denmark to examine the association between perceived stress and risk of subsequent osteoporotic fracture.
Methods
A 2006 population-based health survey in the Central Danish Region (with 1.25 million inhabitants) was used to identify 7943 persons who were 55 years or older on the survey date and completed the Perceived Stress Scale. Individuals were categorized into two groups: high level of stress and low level of stress (including no stress). We obtained information on all osteoporotic fractures through linkage to the Danish National Registry of Patients. We used Cox regression to compute hazard ratios (HRs) with 95 % confidence interval (CI) adjusted for a number of lifestyle factors, socioeconomic data, perceived general health, and prescription history, comparing high- and low-stress persons.
Results
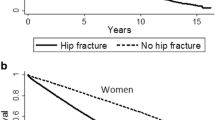
A total of 1799 persons (22.6 %) reported high level of perceived stress, whereas 6144 (77.4 %) reported low level or no stress. The 5-year risk of any osteoporotic fracture was 7.4 and 5.4 % in persons with high and low perceived stress, respectively, corresponding to adjusted HR of 1.37 (CI 1.00–1.89). The adjusted HR for hip fracture within 5 years associated with high perceived stress was 1.68 (CI 1.04–2.72). The associations weakened with increasing follow-up time.
Conclusions
Persons with high perceived stress have an increased risk of any osteoporotic fracture, in particular risk of hip fracture within 5 years of stress assessment even after adjusting for differences in lifestyle, comorbidities, osteoporosis presence, medication use, and socioeconomic status at the time of stress level evaluation. The association attenuated after longer follow-up time.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is characterized by reduced bone mass and deterioration of bone micro-architecture causing bone to become weak and fragile [1] and thus predisposing to fractures after a fall or even a mild trauma [2]. The prevalence of osteoporosis after age 50 years is approximately 7 % in men and 20 % in women [3]. Since women have more severe bone loss and experience falls more frequently than men, the incidence of any osteoporotic fracture is higher in women than in men [2]. Risk of fracture also increases with age, as a result of age-related decrease in bone mass density. Thus, the health-care burden of osteoporotic fractures will continue to increase due to population aging in all Western countries. Denmark and other Scandinavian countries have the highest 10-year risk of major osteoporotic fractures in the world [4].
Risk factors for osteoporotic fractures, in particular risk factors of falls resulting in hip fracture, include female gender; higher age; low socioeconomic status; alcohol consumption; specific comorbid conditions; physical functioning; and use of psychotropic, anxiolytic, and hypnotic drugs and use of corticosteroids [5, 6]. Perceived stress is associated with ischemic heart disease, asthma, and mortality [7–9], but less is known about the impact of stress on fracture risk. Peterson et al. observed higher numbers of major life events prior to hip fracture, including death and illness in the family and financial problems among 111 elderly hip fracture patients compared with 90 persons in the control group without fracture [10]. A cross-sectional study from Sweden based on 137 elderly hip fracture patients suggested that emotional stress is associated with a higher risk of falls and subsequent hip or pelvic fractures [11]. A cohort study of 5152 older men reported an increased risk of falls, but not of fractures 1 year following stressful life events [12]. The previous studies were either small and cross-sectional [10, 11], based on selected patient populations [12], or have not fully accounted for important confounders [10–12], such as body mass index, smoking, alcohol, perceived general health, marital status, medication use prior fracture, education, or physical exercise [13, 14]. We conducted a population-based cohort study to examine the association between perceived stress and risk of subsequent osteoporotic fracture in Danish men and women.
Material and methods
Setting
Denmark is a country of 5.6 million inhabitants. The Danish Health Service provides tax-supported health care for all Danish citizens, guaranteeing free medical care for emergency and general hospital admissions and outpatient clinic visits. The Danish Civil Registration System has maintained data on vital status, date of death, residence, and migration for the entire Danish population since 1968. All Danish citizens are assigned a unique 10-digit personal identification number at birth or upon immigration, permitting unambiguous linkage among all Danish registries, as well as tracking of patients who die, emigrate, or are transferred between hospitals [15].
Study population
The study population consisted of participants of the Danish Health Survey called “How Are You?,” a self-reported questionnaire-based public health study. The survey was conducted by the Centre for Public Health in the Central Denmark Region, the second largest of the five regions in Denmark, with 1.25 million inhabitants [16]. From January to March 2006, a random sample of 31,500 Danish citizens between 25 and 79 years of age and living in the region were invited to participate in the study. Eligible participants were identified through the Civil Registration System. In total, 21,604 (69 % of those invited) completed a detailed questionnaire containing approximately 400 questions on perceived stress and general health, occurrence of chronic diseases, socioeconomic factors, and lifestyle factors. Three reminders were sent to non-respondents. The survey has been described in detail elsewhere (available in Danish: www.cfk.rm.dk/om-cfk/projektsite/hvordan-har-du-det/rapporter-og-analyser/).
Only participants who were 55 years or older on the date of the survey were included in order to avoid inclusion of non-osteoporosis-related fractures (n = 9182). We excluded participants who did not complete the entire Perceived Stress Scale (PSS) (n = 1099).
The Perceived Stress Scale
The study participants were asked to report perceived stress using the PSS. PSS is a widely used psychological instrument that measures the degree to which situations in one’s life are appraised as stressful [17]. The PPS consists of 10 question eliciting frequency of feelings and thoughts during the previous month using a five-point scale (0 = never, 1 = almost never, 2 = sometimes, 3 = fairly often, 4 = very often). The PSS score is a sum of the individual item scores, whereby for items 4, 5, 7, and 8, the rating is reversed (score range 0–40 points). PPS was translated into Danish and afterwards validated [18].
Because stress level measured with PSS was previously reported to be higher in women than men [19], we used different cutoff points for women and men to define level of stress. Since there is no generally accepted standard for defining the level of stress, the cutoff points were found by categorizing the female and male study population according to percentiles of stress scores and classifying participants in a high stress level by taking the 20 % percentile of the participants experiencing the highest levels of stress. The way of finding cutoff points used in this study was described previously [20] and was data driven. Thus, individuals were categorized as having high levels of stress (if PSS score ≥17 for women and PSS score ≥15 for men) or low levels of stress (if PSS score <17 for women and PSS score <15 for men). Persons reporting no stress were included in the group of low level of stress. We further used the following categorization both for women and men to describe in more details distribution of level of stress: PSS score 0–10, PSS score 11–15 and PSS score 16–20, and PSS score ≥21.
Osteoporotic fractures
Outcome was the first time hospitalization for one of the osteoporotic fractures (Table 1) after the survey completion date. Data on fractures were obtained from the Danish National Registry of Patients (DNRP). The DNRP has maintained data on all admissions to non-psychiatric hospitals in Denmark since 1977 (and on all emergency room visits and visits to hospital specialty clinics since 1995), including dates of admission and discharge and up to 20 discharge diagnoses classified according to the International Classification of Diseases (ICD), 8th Revision until the end of 1993 and 10th Revision thereafter. Both primary and secondary diagnoses, coded by the physician responsible for discharging the patient after hospitalization, were used to identify the outcome. The diagnose codes are provided after the suspicion for fracture has been confirmed radiologically and after the treatment has been initiated or finished at the hospital, as a standard procedure.
Covariates
We included information on the following covariates from the Danish survey “How Are You?”:
-
Age at the survey date as a continuous variable in years
-
Gender
-
Marital status in categories: married, unmarried, divorced/separated, and widowed
-
School education in four categories: 7 years of school or less, 8 to 10 years of education, more than 10 years of education, and unspecified
-
Personal gross income before tax in 2005 in five categories: as 0–99,000 DKK, 100,000–149,000 DKK, 150,000–249,000 DKK, 250,000–374,000 DKK, and 375,000 or more
-
Smoking in categories: current smoker, former smoker, and never smoker
-
Alcohol units per week in categories defined using different weekly units cutoffs for men and women: low, <7 for women/<14 for men; medium, 8–14 for women/15-21 for men; and high, ≥15 for women/≥22 for men
-
Body mass index (BMI, calculated as weight in kg/height squared in m2) in categories: underweight if BMI < 18.5 kg/m2, normal if BMI 18.5–24.9 kg/m2, and overweight if BMI ≥ 25.0 kg/m2
-
Physical exercise in days per week, number of days with minimum 30-min exercise each week in categories: 0 days, 1–2 days, 3–4 days, and ≥5 days
-
Diet in categories: healthy (high amount of fruit, vegetables, fish, and low amount of saturated fat), reasonably healthy (median high intake of fruit, vegetables, fish, and saturated fat), and unhealthy diet (low amount of fruit, vegetables, fish, and high amount of saturated fat)
-
Perceived general health in categories: excellent or very good, good, and fair or poor
-
Sleeping problems during the last 14 days in categories: no, yes but not bothered, and yes very bothered
-
Visual problems despite use of glasses or lenses during the last 14 days in categories: no, yes but not bothered, and yes very bothered
The inclusion of these covariates into analyses was based on previous literature. Considerable evidence exist consistently documenting factors such as age, gender, race, low bone mass, low body weight, estrogen deficiency, earlier fracture, visual deficiency, use of psychotropic/ anxiolytic/hypnotic drugs, use of corticosteroid, cigarette smoking, chronic alcoholism, osteoporosis, diabetes mellitus, and stroke to be risk factors for fall and hip fracture [5]. Association between perceived general health and various outcomes, including mortality, use of health services and development of musculoskeletal, cardiovascular, and psychiatric disorders was also reported previously [21].
Information on death due to any cause or emigration following the survey date was collected from The Danish Civil Registration System [22].
The complete hospitalization history of all persons for 10 years preceding the survey date was obtained from the DNRP. As a measure of comorbidity, we computed the Charlson Comorbidity Index (CCI) score [23, 24] for each person at the index date. We defined three comorbidity levels: a score of 0 (low), given to patients with no previous record of diseases included in the CCI; a score of 1–2 (medium); and a score of 3 or more (high) [25]. Only persons hospitalized or treated at outpatient clinics were included (emergency room patients were excluded). Both primary and secondary diagnoses in individuals hospitalized or treated at outpatient clinics were included in the CCI (emergency room diagnoses were excluded due to low accuracy).
We obtained information on use of medication from the Aarhus University Prescription Database (AUPD) during the 1 year before survey date. The AUPD tracks all prescriptions for reimbursable drugs dispensed at all community pharmacies and hospital-based outpatient pharmacies in Northern Denmark [26, 27]. Drugs are coded according to the Anatomical Therapeutic Chemical (ATC) classification system and the prescriptions fill dates. Data are available for four regions of Northern Denmark: North Jutland (complete since 1992), Aarhus (since 1996), Viborg (since 1998), and Ringkobing (since 1998). For all patients, we considered the following drugs: analgesics (ATC codes NO2A, NO2B), antidepressants (ATC codes N06A), psychotropic drugs (NO3A, NO4, NO5), antihypertensive drugs (C03, C08, C09, C07A, C02A), systemic and topical corticosteroids (H02A and A07EA), statins (ATC code C1OAA), and osteoporotic drugs (M05BA, M05BB bisphosphonates; G03XC01-raloxifene; M05BX01 ipriflavone; M05BX03 strontium ranelate; M05BX04 denosumab; H05AA teriparatide or parathyroid hormone; H05BA calcitonin).
Statistical analyses
We tabulated characteristics of the study population overall and by PSS level, presenting age as mean value in years with a range. We estimated the risk of any fracture within 5 years of index date, as well as within the entire follow-up after the survey date with 95 % confidence intervals (CIs) for participants with high and low PSS score, as well as for participants categorized within following level of stress groups: PSS score 0–10, PSS score 11–15 and PSS score 16–20, and PSS score ≥21. Chi-squared statistic for trend was used to examine the trend in the risk of fracture by four PSS score categories. p value of <0.05 was considered to be statistically significant. We estimated mean PSS score with standard deviation (SD).
For example, among all persons with high level of stress at the time of inclusion into the study, we calculated the number of first time fractures within 5 years of index date.
We tabulated the risk of different fracture types by PSS level during the 5 years of survey date and the entire follow-up period. We followed participants from the index date until first hospitalization for any fracture, emigration, death, or 31 December 2013, whichever came first. We calculated the median follow-up time in years with range.
We used Cox regression with age as the timescale to compute crude hazard ratios (HRs) as a measure for relative risk with 95 % CI comparing persons with high level of stress to those with low or no reported stress. In addition, we estimated adjusted HRs with 95 % CI using the following models: model 1: HR adjusted for gender; model 2: HR adjusted for gender and perceived general health; model 3: HR adjusted for gender, perceived general health, school education, and marital status; and model 4: HR adjusted for gender, school education, marital status, income, smoking, alcohol, body mass index, physical exercise, perceived general health, diet, and redeemed prescription drugs. We fitted and expanded the models based on clinical and evidence-based relevant association of covariates with fracture risk and stress, not on the level of p values from the unadjusted model. Thus, we started with gender as the most important confounder, adding perceived general health, education, and marital status. In model 4, we further included all covariates because of their equal clinical association with fracture risk and stress. Inclusion of variables one at the time in model 4 was not an option because the order of variables inclusion was not straight forward, even after considering p values from the unadjusted model. We calculate HRs separately for men and women, except for model 1. In addition, we estimated the risk of first hip fracture separately because of high morbidity and mortality associated with hip fracture [28, 29].
The study was approved by the Danish Data Protection Agency (Central Denmark Region, record number 2013-41-1924). All statistical analyses were performed using SAS version 9.1.3 (SAS Institute Inc., Cary, North Carolina).
Results
Characteristics of the study population
A total of 1099 persons were excluded due to lack of information on PSS at the survey date (12.2 % of those who completed survey questionnaire and were age 55 years and older). Compared with the included persons, those without data on PSS were slightly older (mean age 69.7 years; range 55.1–80.1), more likely to be women (60 vs. 40 %); to have fair or poor perceived general health (30 vs. 17 %); to have lower school education level (58 vs. 38 % had less than 7 years of school); to have comorbidities before the index date (34 vs. 24 %); and to have almost twofold higher consumption of analgesics, antidepressants, psychotropic drugs, antihypertensive drugs, systemic, and topical corticosteroids but lower consumption of statins. Persons who did not complete PSS were also more likely to omit other information from the questionnaire, with missing information in the range between 7 % for school education and 49 % for income. The risk of any fracture among persons with lack of PSS data was 10 % (109 of 1099 persons) within 5 years and 12 % during the entire follow-up time (131 of 1099 persons).
A total of 7943 participants with reported information on PSS were included in the final analyses (Table 2); 4007 (50 %) were men. The mean age at the index date was 64.6 (range 55.0–80.1) years. A total of 6144 (77.4 %) of participants had low perceived stress, and 1799 (22.6 %) had high perceived stress.
Looking at distribution of PSS score, 3780 (47.5 %) of all participants had PSS score 0–10 points, whereas 2275 (28.6 %), 1402 (17.7 %), and 483 (6.1 %) of the participants had PSS score 11–15, PSS score 16–20 points, and PSS score ≥21 points, respectively. Level of perceived stress was higher for women compared with men. Thus, among women, 41.4 % had PSS score 0–10 points, 30.7 % had PSS score 11–15 points, 19.8 % had PSS score 16–20 points, and 8.1 % had PSS score ≥21 points. Among men, 53.7 % had PSS score 0–10 points, 26.6 % had PSS score 11–15 points, 15.6 % had PSS score 16–20 points, and 4.1 % had PSS score ≥21 points. The mean PSS scores were 12.8 (SD ± 6.2) for women and 10.5 (SD ± 5.8) for men.
Perceived stress and participants’ characteristics
Compared with those with low perceived stress, persons with high perceived stress were more likely to be unmarried, divorced, or separated (11.0 vs. 8.0 %); to have fair or poor perceived health (37.5 vs. 10.6 %); and to have comorbidity (31.3 vs. 21.1 %). In addition, persons with high perceived stress were more likely to have less than 7 years of schooling, lower personal gross income, to be current smokers and consume more alcohol, to be obese, and to have sleeping problems and visual problems despite use of glasses or lenses (Table 1). On the other hand, they were less likely to do physical exercises and eat healthy food (Table 2). Persons with high perceived stress were also more likely to take any kind of medication compared with low perceived stress persons (Table 3).
Perceived stress and risk of fracture
The risk of any osteoporotic fracture within 5 years after assessment of stress was 5.8 % (462 of 7943 persons), being 7.4 and 5.4 % in patients with high and low perceived stress, respectively. This corresponds to crude HR of 1.38 (CI 1.12–1.68) and adjusted HR from model four of 1.37 (1.00–1.89). The adjusted HR (based on model 4) for any osteoporotic fracture within 5 years was 1.23 (CI 0.80–1.91) in women and 1.55 (CI 0.96–2.52) in men (Table 4).
The risk of any osteoporotic fracture was 8.2 % (652 of 7943 persons) (Table 5) during the entire follow-up time (with a median follow-up time of 6.8 years, ranging from 1 to 6.8 years). A total of 170 (9.5 %) persons with high perceived stress and 482 (7.9 %) persons with low perceived stress sustained any osteoporotic fracture during the entire follow-up (Table 5), corresponding to crude HR of 1.21 (CI 1.02–1.44) (Table 4). The estimates became imprecise in the model 4 when we adjusted for gender, school education, marital status, perceived general health, income, smoking, alcohol, body mass index, physical exercise, diet, and redeemed prescription drugs (HR = 1.20, CI 0.91–1.59) (Table 4). The direction and magnitude of the association were similar in women and men (Table 4).
The most common type of any first fracture within the entire follow-up was fracture of the forearm, accounting for 33.5 % of all fractures among respondents with high perceived stress and 38.6 % of all fractures among respondents with low perceived stress. The second most common fracture is the fracture of hand or wrist accounting for 14.7 and 21.0 % of all fracture among respondent with high and low perceived stress, respectively. The third most common fracture is the fracture of femur accounting for 27.1 and 14.9 % of all fractures among respondent with high and low perceived stress, respectively.
Persons with high and low perceived stress were at similar risk of sustaining fractures of neck, spine/pelvis, humerus/shoulder, forearm, and hand/wrist (Table 5). However, compared to person with low perceived stress, persons with high perceived stress were more likely to sustain fracture of femur within 5 years of survey date (1.83 vs. 0.75 %) and within the entire period (2.56 vs. 1.17 %) corresponding to adjusted HR within 5 years of 1.68 (CI 1.04–2.72) and adjusted HR of 1.53 (CI 1.04–2.25) within the entire follow-up period.
Extra analyses
Among women, the risk of any osteoporotic fracture within 5 years after assessment of stress was 8.0 % (130 of 1621) for persons with PSS score 0–10 points, 7.6 % (92 of 1208) for persons with PSS score 11–15 points, 9.1 % (71 of 779) for persons with PSS score 16–20 points, and 9.7 % (31 of 321) for persons with PSS ≥21 points (p value = 0.062 for trend). Among men, the risk of any osteoporotic fracture within 5 years after assessment of stress was 2.6 % (56 of 2152) for persons with PSS score 0–10 points, 4.0 % (43 of 1067) for persons with PSS score 11–15 points, 4.2 % (26 of 623) for persons with PSS score 16–20 points, and 7.9 % (13 of 165) for persons with PSS ≥21 points (p value < 0.0001 for trend).
The risks of any osteoporotic fracture within the entire follow-up period were 11.2, 11.0, 13.1, and 11.2 % for four PSS score groups among women (p value = 0.077 for trend) and 4.0, 5.9, 5.3, and 10.3 % for four PSS score groups among men (p value <0.0001 for trend).
Discussion
In this population-based cohort study of 7943 persons, 5.8 % sustained any osteoporotic fracture within 5 years of stress assessment and 8.2 % within median follow-up time of 6.8 years. Persons with high perceived stress were at 37 % increased risk of any osteoporotic fracture and 68 % increased risk of hip fracture within 5 years of follow-up, compared with persons with low perceived stress, even after adjusting for differences in persons characteristics. The direction of risk increase was similar in men than in women. The association attenuated after longer follow-up time.
Comparison with previous literature
To our knowledge, this is the first prospective population-based study including both women and men to evaluate the association between perceived stress and risk of any osteoporotic facture as well as femur fracture using long-term follow-up and accounting for multiple confounders. In contrast to our findings, a study of 4981 men aged 65 years from six cities in USA found no association between any stressful life events and risk of first time fracture within 1 year of follow-up [12]. Our findings are in line with the results from two studies. In a case-control study of 111 hip fracture patients and 90 controls with no fracture among community-dwelling elderly, the hip fracture group reported significant more major negative life events than the non-fracture group in the period of 1 year before sustaining a fracture or becoming a control (the p value was less than 0.0007) [10]. Moller et al. reported that among 122 persons aged 65 and older with fall-related hip or pelvic fracture of which 12 experienced emotional stress during the 24 h before injury, anger (relative risk = 12.2, CI 2.7–54.7), sadness (relative risk = 5.7, CI 1.1–28.7), and stress (relative risk = 20.6, CI 4.5–93.5) were associated with increased risk of fracture [11]. However, comparison between our study and the abovementioned three studies is difficult due to several reasons. We measured stress with PSS, which is a widely used validated psychological instrument that measures the degree to which situations in one’s life are appraised as stressful [17]. Other studies used self-developed questions about stressful life event such as death of close family member or friend, personal illness or injury, separation form child, serious financial troubles, or change of residence [10, 12] or about feeling of anger or sadness on the day of fracture [11]. These events may not be equally stressful for all persons. No information on perceived stress or how the persons were coping with these life events was available in any of previous studies limiting the validity of the associations and hampering the conclusions on the association between stress and fracture risk. Second, the data on stress were collected retrospectively potentially introducing recall-bias. Third, two of the studies did not fully account for important confounders [10–12], such as body mass index, smoking, alcohol, perceived general stress, marital status, medication use prior fracture, education, income, or physical exercises [13, 14]. Our findings show a clear difference in characteristics of persons with high and low perceived stress; justifying the inclusion of these factors into regression analyses was also described previously in another Danish survey from 2005, based on a national representative sample of the Danish population [20].
Several mechanisms may explain our findings. The response to stress (allostasis) and following allostatic load or overload has been described in details previously [30]. A number of mediators have been proposed to trigger and change the neuroendocrine, immune, metabolic, and cardiovascular response in the body leading to increased allostatic load, promoting adverse health outcomes [30], some being protective and other being harmful. For example, the body responds to stress by releasing catecholamine that increases heart rate and blood pressure, which could over time lead to stroke and myocardial infarction [31]. In addition, the level of cholesterol and glucose predisposes to diabetes [32] and atherosclerosis [33]. One of the main mediators that is produced in response to stress is glucocorticoids [31]. Glucocorticoids work protectively against infection, injury, and inflammation. Further, glucocorticoids are associated with reduced activity of the bone-forming cell osteoblasts [34], increased bone resorption leading to osteoporosis [35], and increased fracture risk [36]. Even a small dose of glucocorticoids increase the fracture risk [37]. However, it is unknown what “dose” of natural glucocorticoids the body is receiving during stress and if these doses are comparable with synthetic glucocorticoids used as treatment of various diseases. Stress is also closely related to depression, and both stress and depression are found to be negatively associated with bone mineral density and thereby fracture risk [38]. But again, this association is most likely mediated by glucocorticoids [38].
The 75 % of fractures included in our study were the fractures of forearm, hand, wrist, and femur, which are fall related. The association between stressful life events and falls was observed previously [12]. This association could work through activation of the neuroendocrine system causing multi-system physiological dysregulation, physical function unbalance, or visual disturbance, leading to fall and fracture [11, 30]. In addition, it has been suggested that high personal stress is strongly associated with low self-care, potentially leading to fall and fracture [39].
It has been suggested that the effects of stress on health outcomes are different for men and women, possibly explained by sex differences in vulnerability or in ability to cope with stress [40, 41]. However, we found no clear difference in the risk of any osteoporotic fracture between women and men.
Significance and implications of the study results
Knowledge about a possible association between stress and risk of osteoporotic fracture may improve our understanding of clinical course of patients sustaining fractures and guide future stress prevention efforts.
Limitations of the study
The survey is based on the population sample from the Danish Central Regions, which is considered to be representative of the Danish population. However, we excluded 12.2 % of the study population due to lack of stress data and we know that non-responders differed from responders in terms of unhealthier lifestyle, comorbidities, and lower socioeconomic status [42]. This may have introduced selection and information bias if missingness of stress data was related to later fracture risk, which is rather unlikely due to prospective registration of data. Persons with missing stress data did not know that they will later develop fracture. Thus, it is even likely that inclusion of missing PSS data would strengthen the association of interest in our study. Although we adjusted for comorbidity, we lacked information on the severity of some medical conditions included in the Charlson Comorbidity Index score, which may have introduced residual confounding into our analyses. Since data on comorbidity were collected independently on the stress data, the size of residual confounding is limited. We did not have information of bone mineral density of participants, which is a risk factor for osteoporotic fracture and was found to be associated with depression and stress [38]. However, we included into the model a number of clinical risk factors for fracture risk; some of them are independent, while others are dependent on bone mineral density [43]. We also adjusted for the presence of osteoporosis at the time of PSS scoring as a surrogate measure of bone mineral density. Several HR estimates based on the regression model 4, where we adjusted for a number of confounders, were unstable and imprecise. As outcome, we only included person that had been in contact with hospital due to symptoms and suspicion for fracture; thus, any person with silence compression fractures is not included.
We have only assessed stress at baseline and did not have information on stress level or stressful events that occurred during the follow-up period. Thus, it is possible that stress level has changed over time. This may explain why the association between perceived stress and fracture in our study attenuated with longer follow-up.
Summary
In this large population-based cohort study of 7943 individuals, persons with high perceived stress were at increased risk of any osteoporotic fracture within 5 years of follow-up, in particular increased risk of hip fracture compared with persons with low or no perceived stress, even after adjusting for differences in lifestyle, comorbidities, osteoporosis presence, medication use, and socioeconomic status at the time of stress level evaluation. The risk of fracture was similar in women and men. The association attenuated after longer follow-up time. Clinicians should consider including perceived stress level as an important clinical risk factor when assessing the 5-year probability of fracture. Further research is needed and longer follow-up period in order to draw any firm conclusion about association of stress and 10-year fracture risk.
References
Lane JM, Russell L, Khan SN (2000) Osteoporosis. Clin Orthop 372:139–150
Morrison A, Fan T, Sen SS, Weisenfluh L (2013) Epidemiology of falls and osteoporotic fractures: a systematic review. Clinicoecon Outcomes Res 5:9–18
Hernlund E, Svedbom A, Ivergard M, Compston J, Cooper C, Stenmark J, McCloskey EV, Jonsson B, Kanis JA (2013) Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos 8:136
Kanis JA, Oden A, McCloskey EV, Johansson H, Wahl DA, Cooper C (2012) A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int 23:2239–2256
Lauritzen JB, McNair PA, Lund B (1993) Risk factors for hip fractures. A review. Dan Med Bull 40:479–485
Taylor BC, Schreiner PJ, Stone KL, Fink HA, Cummings SR, Nevitt MC, Bowman PJ, Ensrud KE (2004) Long-term prediction of incident hip fracture risk in elderly white women: study of osteoporotic fractures. J Am Geriatr Soc 52:1479–1486
Keller A, Litzelman K, Wisk LE, Maddox T, Cheng ER, Creswell PD, Witt WP (2012) Does the perception that stress affects health matter? The association with health and mortality. Health Psychol 31:677–684
Rod NH, Gronbaek M, Schnohr P, Prescott E, Kristensen TS (2009) Perceived stress as a risk factor for changes in health behaviour and cardiac risk profile: a longitudinal study. J Intern Med 266:467–475
Rod NH, Kristensen TS, Lange P, Prescott E, Diderichsen F (2012) Perceived stress and risk of adult-onset asthma and other atopic disorders: a longitudinal cohort study. Allergy 67:1408–1414
Peterson MG, Allegrante JP, Augurt A, Robbins L, MacKenzie CR, Cornell CN (2000) Major life events as antecedents to hip fracture. J Trauma 48:1096–1100
Moller J, Hallqvist J, Laflamme L, Mattsson F, Ponzer S, Sadigh S, Engstrom K (2009) Emotional stress as a trigger of falls leading to hip or pelvic fracture. Results from the ToFa study—a case-crossover study among elderly people in Stockholm, Sweden. BMC Geriatr 9:7
Fink HA, Kuskowski MA, Marshall LM (2014) Association of stressful life events with incident falls and fractures in older men: the osteoporotic fractures in men (MrOS) study. Age Ageing 43:103–108
Peel NM, Bartlett HP, McClure RJ (2007) Healthy aging as an intervention to minimize injury from falls among older people. Ann N Y Acad Sci 1114:162–169
Peel NM, McClure RJ, Hendrikz JK (2007) Psychosocial factors associated with fall-related hip fractures. Age Ageing 36:145–151
Frank L (2000) Epidemiology. When an entire country is a cohort. Science 287:2398–2399
The StatBank Denmark. http://statbank.dk 2015
Cohen S, Kamarck T, Mermelstein R (1983) A global measure of perceived stress. J Health Soc Behav 24:385–396
Eskildsen A, Dalgaard VL, Nielsen KJ, Andersen JH, Zachariae R, Olsen LR, Jorgensen A, Christiansen DH (2009) Cross-cultural adaption and validation of the Danish consensus version of the 10-item perceived stress scale. Scand J Work Environ Health 35:145–152
Cohen S, Janicki-Deverts D (2012) Who’s stressed? Distribution of psychological stress in the United States in probability samples from 1983, 2006, and 2009. J Appl Soc Psychol 42:1320–1334
Nielsen L, Curtis T, Kristensen TS, Rod NN (2008) What characterizes persons with high levels of perceived stress in Denmark? A national representative study. Scand J Public Health 36:369–379
Goldberg P, Gueguen A, Schmaus A, Nakache JP, Goldberg M (2001) Longitudinal study of associations between perceived health status and self-reported diseases in the French Gazel cohort. J Epidemiol Community Health 55:233–238
Schmidt M, Pedersen L, Sorensen HT (2014) The Danish Civil Registration System as a tool in epidemiology. Eur J Epidemiol 29:541–549
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Thygesen SK, Christiansen CF, Christensen S, Lash TL, Sorensen HT (2011) The predictive value of ICD-10 diagnostic coding used to assess Charlson Comorbidity Index conditions in the population-based Danish National Registry of Patients. BMC Med Res Methodol 11:83
de Groot V, Beckerman H, Lankhorst GJ, Bouter LM (2003) How to measure comorbidity. A critical review of available methods. J Clin Epidemiol 56:221–229
Ehrenstein V, Antonsen S, Pedersen L (2010) Existing data sources for clinical epidemiology: Aarhus University prescription database. Clin Epidemiol 2:273–279
Gaist D, Sorensen HT, Hallas J (1997) The Danish prescription registries. Dan Med Bull 44:445–448
de Luise C, Brimacombe M, Pedersen L, Sorensen HT (2008) Comorbidity and mortality following hip fracture: a population-based cohort study. Aging Clin Exp Res 20:412–418
Nielsen KA, Jensen NC, Jensen CM, Thomsen M, Pedersen L, Johnsen SP, Ingeman A, Bartels PD, Thomsen RW (2009) Quality of care and 30 day mortality among patients with hip fractures: a nationwide cohort study. BMC Health Serv Res 9:186
Juster RP, McEwen BS, Lupien SJ (2010) Allostatic load biomarkers of chronic stress and impact on health and cognition. Neurosci Biobehav Rev 35:2–16
McEwen BS (2008) Central effects of stress hormones in health and disease: understanding the protective and damaging effects of stress and stress mediators. Eur J Pharmacol 583:174–185
Crews DE (2007) Composite estimates of physiological stress, age, and diabetes in American Samoans. Am J Phys Anthropol 133:1028–1034
Sabbah W, Watt RG, Sheiham A, Tsakos G (2008) Effects of allostatic load on the social gradient in ischaemic heart disease and periodontal disease: evidence from the third national health and nutrition examination survey. J Epidemiol Community Health 62:415–420
Chavassieux P, Pastoureau P, Chapuy MC, Delmas PD, Meunier PJ (1993) Glucocorticoid-induced inhibition of osteoblastic bone formation in ewes: a biochemical and histomorphometric study. Osteoporos Int 3:97–102
van Staa TP, Leufkens HG, Cooper C (2002) The epidemiology of corticosteroid-induced osteoporosis: a meta-analysis. Osteoporos Int 13:777–787
Ioannidis G, Pallan S, Papaioannou A, Mulgund M, Rios L, Ma J, Thabane L, Davison KS, Josse RG, Kovacs CS, Kreiger N, Olszynski WP, Prior JC, Towheed T, Adachi JD (2014) Glucocorticoids predict 10-year fragility fracture risk in a population-based ambulatory cohort of men and women: Canadian Multicentre Osteoporosis Study (CaMos). Arch Osteoporos 9:169
van Staa TP, Leufkens HG, Cooper C (2001) Use of inhaled corticosteroids and risk of fractures. J Bone Miner Res 16:581–588
Erez HB, Weller A, Vaisman N, Kreitler S (2012) The relationship of depression, anxiety and stress with low bone mineral density in post-menopausal women. Arch Osteoporos 7:247–255
Albright TL, Parchman M, Burge SK (2001) Predictors of self-care behavior in adults with type 2 diabetes: an RRNeST study. Fam Med 33:354–360
Ferraro KF, Nuriddin TA (2006) Psychological distress and mortality: are women more vulnerable? J Health Soc Behav 47:227–241
Verma R, Balhara YP, Gupta CS (2011) Gender differences in stress response: role of developmental and biological determinants. Ind Psychiatry J 20:4–10
Rothman KJ (2002) Epidemiology. An introduction
Kanis JA, Borgstrom F, De LC, Johansson H, Johnell O, Jonsson B, Oden A, Zethraeus N, Pfleger B, Khaltaev N (2005) Assessment of fracture risk. Osteoporos Int 16:581–589
Acknowledgments
The study was supported by a grant from Aarhus University Research Foundation and by the Program for Clinical Research Infrastructure (PROCRIN) established by the Lundbeck Foundation and the Novo Nordisk Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Pedersen, A.B., Baggesen, L.M., Ehrenstein, V. et al. Perceived stress and risk of any osteoporotic fracture. Osteoporos Int 27, 2035–2045 (2016). https://doi.org/10.1007/s00198-016-3490-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-016-3490-1