Abstract
Summary
Dietary vitamin C intake showed significant positive associations with BMD in postmenopausal women, especially with vitamin D deficiency.
Introduction
Although there is a positive role of vitamin C in osteoblastogenesis, debate remains about the contribution of vitamin C to bone mineral density (BMD) in humans.
Methods
Data were derived from the Fourth Korean National Health and Nutrition Examination Survey. Dietary information was assessed using a 24-h dietary recall questionnaire. BMD was measured by dual-energy X-ray absorptiometry at the lumbar and hip.
Results
A total of 1,196 postmenopausal women aged 50 years and older were stratified into tertiles by daily dietary vitamin C intake. After adjusting for traditional confounders, dietary vitamin C intake tertile was significantly positively associated with BMD at all sites (R = 0.513 for lumbar spine (LS) and R = 0.657 for femoral neck (FN), P < 0.05 for each). The subjects with osteoporosis had significantly lower dietary vitamin C intake than did subjects without osteoporosis (74.4 ± 66.2 vs 94.1 ± 78.6 mg/day for LS and 65.5 ± 56.6 vs 94.3 ± 79.2 mg/day for FN, respectively, P < 0.001). The multiple-adjusted odds ratio for osteoporosis for dietary vitamin C <100 mg/day was 1.790 (95 % CI 1.333–2.405, P < 0.001). However, the significant association between vitamin C intake and BMD was only observed in subjects with vitamin D deficiency and aged 50–59 years or >70 years.
Conclusion
Dietary vitamin C intake was positively associated with BMD in postmenopausal women, and inadequate vitamin C intake could increase the risk of osteoporosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a major public health problem worldwide because of the increased risk of fragility fracture and chronic disability later in life. The lifetime risk of osteoporotic fractures has been estimated as 40 % for white women aged 50 years in the USA [1, 2]. The incidence of hip fractures is increasing worldwide by 1–3 % per year and is expected to total 8.2 million in 2050 [3].
Several pathological mechanisms are involved in age-related bone loss. Menopause, in particular, is the most important predisposing factor for bone loss because of the rapid decline in the production of estrogen, a hormone that inhibits bone resorption in premenopausal women [4]. Oxidative stress is also thought to contribute to bone loss during aging in both women and men [5]. Accumulating data suggests that oxidative stress could induce bone loss by osteoclast activation [6] and osteoblast suppression [7]. Vitamin C is a well-known antioxidant and acts as a scavenger of superoxide anion and hydrogen peroxide [8, 9]. Administration of vitamin C in vivo prevented bone loss with decreased reactive oxygen species [10–12]. Some studies of humans also showed that high plasma levels or dietary intake of antioxidants is associated with increased bone mineral density [13–15]. In addition, vitamin C is a cofactor in collagen formation and hydroxylation of lysine and proline [16], which are important for bone maintenance [17]. This nutrient also stimulates in vitro osteoblast differentiation and alkaline phosphatase activity, thereby contributing to bone formation [18, 19]. In addition, some animal studies also showed the importance of vitamin C in skeletal development and homeostasis [20, 21]. Given the favorable roles of vitamin C on bone cells and its capacity as an antioxidant, we reasoned that dietary vitamin C might play a protective role against postmenopausal bone loss in humans.
Several epidemiological studies have reported a conflicting relationship between dietary vitamin C intake and bone mineral density (BMD) in postmenopausal women [22–27, 14]. The Women’s Health Initiative Study reported no independent association between dietary vitamin C and BMD [28]. By contrast, some studies have reported a positive relationship between dietary vitamin C and BMD, but this was significant only in women with a high calcium intake [24, 29, 30], those taking estrogen therapy [29], or smokers [31, 32]. Vitamin C is well tolerated and is easily taken from food and from supplement. Definite information about the effects of vitamin C on bone is important for establishing practical strategies for preventing bone loss in postmenopausal women.
The primary aim of this study was to investigate the association between dietary vitamin C intake and bone loss in postmenopausal women using the data from the Korea National Health and Nutrition Examination Survey IV (KNHANES IV). We also investigated whether the effect of dietary vitamin C on bone could be related to vitamin D status or age.
Subjects and methods
Subjects
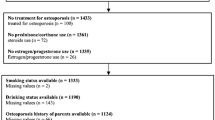
This cross-sectional study was based on public domain data from KNHANES IV performed in 2009. KNHANES has been conducted periodically for noninstitutionalized Koreans by the Korea Centers for Disease Control and Prevention since 1998. The data contain a health interview, nutritional survey, and health examination. Multistage probability design was used to select the household units [33]. The survey was conducted on subjects aged 19 years and older who were not pregnant and had been chosen from a randomly selected representative household through household interviews and by direct standardized physical examinations in mobile examination centers. All participants provided written informed consent. The institutional review board of the Korea Centers for Disease Control and Prevention approved the study protocol. We acquired data for 5,690 women and 4,843 men from the second year (2009) of the KNHANES IV. Among them, 2,073 women aged 50 years and older were included. Subjects were excluded if they were premenopausal (n = 138), took osteoporosis medication (n = 214), had renal insufficiency (serum creatinine (Cr) concentration ≥1.4 mg/dL, n = 210), used estrogen or progesterone (n = 211), or had missing data about dietary vitamin C intake (n = 104). A total of 1,196 postmenopausal women were finally included in the analysis.
Dietary assessment
Nutrient intakes, including total calorie and calcium intake, were assessed using a 24-h dietary recall questionnaire administered by a trained dietician. The results were calculated using the Food Composition Table provided by the National Rural Resources Development Institute (seventh revision).
BMD measurement
BMD (g/cm2) was measured at the lumbar spine (LS; L1–L4), femoral neck (FN), and total hip (TH) using dual-energy X-ray absorptiometry (DXA, QDR4500A; Hologic Inc., Bedford, MA, USA). The DXA equipment was housed in the mobile examination centers. The left hip was scanned routinely, but in participants with a left hip fracture or device, the right hip was scanned. Subjects with T-score ≤−2.5 at each skeletal site were defined as having osteoporosis at the corresponding site. The DXA data were analyzed using Hologic Discovery software version 12.1 in its default configuration.
Laboratory measurements
Participants fasted for 8 h, and blood samples were collected during the survey. The samples were immediately refrigerated and transported in cold storage to the Central Testing Institute in Seoul Korea (NeoDin Medical Institute, Seoul, Korea). All samples were analyzed within 24 h after transportation. Serum 25-hydroxyvitamin D [25(OH)D] concentration was measured with a radioimmunoassay (RIA, DiaSorin Inc., Stillwater, MN, USA) using a gamma counter (1470 Wizard; PerkinElmer, Turku, Finland). The interassay coefficient of variation (CV) was 2.8 to 6.2 %. The concentration of 25(OH)D was measured in the same institute for all samples to minimize analytical variation. We converted 25(OH)D concentration from nanogram per milliliter to nanomole per liter by multiplying the concentration by 2.49. Serum-intact parathyroid hormone (PTH) concentration was measured using a chemiluminescence assay (DiaSorin Inc., Stillwater, MN, USA). The CV of intact PTH concentration was 6.2 %. Serum Cr concentration was obtained using a kinetic compensated Jaffe assay (Roche Diagnostics Ltd., Lewis, UK).
Statistical analysis
The total sample was stratified into tertiles according to dietary vitamin C intake. Characteristics of the participants, including dietary intake and fracture history, were compared between vitamin C tertiles using one-way analysis of variance (ANOVA) and chi-square test. The differences between groups were evaluated further with Tukey’s post hoc analysis. To minimize the effects of confounding variables, the differences in BMD at each site between tertiles of dietary vitamin C intake were estimated using analysis of covariance (ANCOVA) after adjusting for age, body mass index (BMI), total energy intake, smoking, monthly income, and 25(OH)D concentration. Monthly household income was categorized into quartiles: lowest (<USD 500), medium-lowest (USD 500–1,000), medium-highest (USD 1,000–3,000), and highest (≥USD 3,000). Subjects with lower and higher T-scores at each site were compared using an independent t test. To analyze dietary vitamin C intake, ANCOVA was used after adjusting for age, BMI, serum 25(OH)D concentration, smoking, monthly income, and total energy intake.
To investigate the effect of potential confounding factors on BMD, age and 25(OH)D concentration were stratified further. Age was stratified as 50–59, 60–69, and ≥70 years. For dietary vitamin C intake, we used binary categories divided by 100 mg/day for the recommended dietary allowance (RDA) of vitamin C in Korea [34] instead of the tertile categories. After adjusting for age, BMI, serum 25(OH)D concentration, smoking, monthly income, and total energy intake, the BMD at each site was compared between groups with high or low dietary vitamin C intake grouped according to 25(OH)D concentration (<50 and ≥50 nmol/L). The prevalence of osteoporosis after adjusting for BMI, serum 25(OH)D concentration, smoking, monthly income, and total energy intake was evaluated for groups with high or low dietary vitamin C intake according to age (50–59, 60–69, and ≥70 years).
Results
Baseline characteristics of the study participants
A total of 1,196 postmenopausal women aged ≥50 years were included; their mean age was 65.2 ± 9.0 years, BMI was 24.3 ± 3.3 kg/m2, and mean vitamin C intake was 86.8 ± 74.8 mg/day. The subjects’ characteristics grouped by tertiles of dietary vitamin C intake are shown in Table 1. The lowest tertile was defined as dietary vitamin C intake <46.9 mg/day, the middle as ≥46.9 and <92.6 mg/day, and the highest as ≥92.6 mg/day. The study participants in the first tertile were older than those in the second and third tertiles (68.2 ± 9.2, 64.6 ± 8.9, and 62.7 ± 8.1 years, respectively, P < 0.001). Women in the first tertile of vitamin C intake had the lowest total energy intake (1,194.1 ± 474.5, 1,526.2 ± 649.3, and 1,754.5 ± 599.5 kcal/day, respectively, P < 0.001) and dietary calcium intake (287.2 ± 689.2, 388.1 ± 227.9, and 475.6 ± 270.3 mg/day, P < 0.001). Subjects with lower vitamin C intake were more likely to have a history of smoking (P = 0.002). BMI, serum 25(OH)D concentration, and socioeconomic status evaluated by monthly household income did not differ between tertiles of dietary vitamin C intake.
BMDs at each site according to the dietary vitamin C intake tertiles
Figure 1 shows the BMD at each skeletal site according to the dietary vitamin C intake tertiles. The BMD at the three sites LS, FN, and TH correlated positively with vitamin C intake tertiles. The significance was maintained after further adjusting for age, BMI, serum 25(OH)D concentration, smoking, monthly income, and total energy intake (P < 0.05) (Fig. 1). The association was stronger at FN and TH than at LS (coefficient of multiple correlation, R = 0.513 for LS, 0.657 for FN, and 0.653 for TH, P < 0.05 for each) (Fig. 1). The fracture rate did not differ between groups probably because of the low prevalence of fracture (<2 %, data not shown).
Mean (± SE) BMD at each site by tertiles of dietary vitamin C (<46.9, 46.9–92.6, or ≥92.6 mg/day) in postmenopausal women; KNHANES IV, 2009. The P values for trend were produced by the general linear regression model after adjusting for age, body mass index, serum 25-hydroxyvitamin D concentration, smoking, monthly income, and total energy intake. BMD bone mineral density
Dietary vitamin C intake in the osteoporosis and nonosteoporosis groups
Next, we compared the clinical factors related to BMD and dietary vitamin C intake between the osteoporosis group and the nonosteoporosis group (Table 2). In the osteoporosis group, those with a T-score ≤–2.5 at each skeletal site were older and had lower BMI compared with those with a T-score >−2.5 at those sites. The PTH concentrations were higher in the osteoporosis groups at LS and FN, and 25(OH)D concentration did not differ between the groups. However, PTH concentrations did not show any significant differences between the groups, and only 25(OH)D level at TH was lower in the osteoporosis group after adjusting for age (41.8 ± 14.9 nmol/L vs 45.6 ± 16.4 nmol/L, P = 0.035). Household income was higher in the osteoporosis group at all skeletal sites (P < 0.05, respectively). Total energy intake was lower in osteoporosis groups at all skeletal site, but it was not significantly different after adjusting for age. Dietary calcium intake was lower only at LS, and the statistical difference was maintained even after multiple adjustment for covariates (321.3 ± 233.9 vs 417.0 ± 533.8, P < 0.001).
Dietary vitamin C intake was lower in the osteoporosis group than in the nonosteoporosis group at all sites (74.4 ± 66.2 vs 94.1 ± 78.6 mg/day at LS, 65.5 ± 56.6 vs 94.3 ± 79.2 mg/day at FN, 46.3 ± 38.2 vs 89.2 ± 76.0 mg/day at TH, P < 0.001 at each site). After adjusting for covariates, age, BMI, serum 25(OH)D concentration, smoking, monthly income, and total energy intake, dietary vitamin C intake was significantly lower at FN and showed lower trend at TH (65.9 ± 57.1 vs 94.5 ± 79.0 mg/day at FN, 47.8 ± 39.1 vs 89.3 ± 76.0 mg/day at TH, P = 0.043 for FN and P = 0.054 for TH).
Associations between vitamin C intake and BMD according to vitamin D status
The study subjects were further stratified into two groups according to serum 25(OH)D concentrations (<50 and ≥50 nmol/L), and the relationship between dietary vitamin C intake and BMD was analyzed in each group (Fig. 2). In the vitamin D-deficient group (25(OH)D <50 nmol/L), after adjusting for age, BMI, serum 25(OH)D concentration, smoking, monthly income, and total energy intake, BMD at all sites was higher in subjects with dietary vitamin C intake of ≥100 mg/day than in those with <100 mg/day. However, in the vitamin D-nondeficient group serum (25(OH)D concentration ≥50 nmol/L), the adjusted BMD at all sites did not differ significantly between dietary vitamin C groups.
Mean (± SE) BMD at each site in the high and low dietary vitamin C intake groups presented according to serum 25(OH)D concentration. Dietary vitamin C intake was divided in two groups: higher and lower than the Korean RDA of 100 mg/day. The P values for trend were produced from the general linear regression model after adjusting for age, body mass index, serum 25-hydroxyvitamin D concentration, smoking, monthly income, and total energy intake. LS lumbar spine, FN femoral neck, TH total hip
Relationship between dietary vitamin C intake and BMD according to age
We also evaluated whether the favorable effects of dietary vitamin C on BMD differed between age groups. The subjects were stratified into three age groups (50–59, 60–69, and ≥70 years) (Table 3). The multiple-adjusted odds ratio for osteoporosis for dietary vitamin C <100 mg/day was 1.790 (95 % CI 1.333–2.405, P < 0.001) compared with higher vitamin C intake. Women aged 50–59 years had the highest adjusted odds ratio for lower vitamin C intake (2.756, 95 % CI 1.335–5.686, P = 0.006). In subjects aged ≥70 years, the adjusted odds ratio for osteoporosis for lower vitamin C intake was 1.888 (95 % CI 1.079–3.303, P = 0.026). Interestingly, in women in their 60s, the adjusted odds ratio for osteoporosis was not increased with lower vitamin C intake.
Discussion
This study showed that dietary vitamin C intake was positively associated with BMD at all sites measured in postmenopausal women. These relationships remained significant after adjusting for confounding factors in the multiple logistic regression. Subjects with lower dietary vitamin C intake (<100 mg/day) had a higher odds ratio for osteoporosis than those with higher vitamin C intake. However, the protective association between higher vitamin C intake and BMD was observed only in subjects with a deficient serum 25(OH)D concentration (<50 nmol/L). Age-stratified analysis revealed a significant association between vitamin C intake and BMD among women aged 50–59 years and ≥70 years, but not in women aged 60–69 years.
Although several observational studies have shown positive associations between dietary vitamin C and BMD, the results have not been consistent [22, 24–26, 14]. A 17-year longitudinal study reported a protective association between higher vitamin C intake and fracture, but this was attenuated after adjusting for potassium intake [27]. Other studies that failed to find a general association between vitamin C intake and BMD showed partial positive relationships only in the groups with higher dietary [23] or supplementary [29] calcium intake. This inconsistency might reflect the fact that dietary nutrients can be related to other parameters, including age, sex, and ethnicity, and that these parameters can also affect bone health directly or indirectly.
Vitamin C can alter bone resorption by osteoclasts [12] and is required for osteoblast differentiation [35]. Several experimental studies have shown favorable roles of vitamin C in skeletogenesis. Park et al. showed that vitamin C-deficient mice had high expression levels of receptor activator of nuclear factor κ-B ligand (RANKL), which plays a key role in osteoclast differentiation, and peroxisome proliferator-activated receptor gamma (PPARγ), which might promote the transition of osteoblasts to adipocytes [21]. Zhu et al. reported that vitamin C prevents bone loss in ovariectomized mice by activating the Runx2 promoter, a potent stimulator of osteoblast differentiation [20].
Oxidative stress activates nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) proteins, which are important for osteoclastogenesis. Fruits and vegetables are abundant sources of antioxidant vitamins such as vitamin C and carotenoids. Previous studies have shown that a higher intake of fruit and vegetables has a positive effect on BMD [36–38]. Maggio et al. reported that plasma antioxidant concentrations are markedly decreased in older osteoporotic women [13]. Based on these findings, vitamin C may have a positive association with bone density through its antioxidant activities by scavenging single oxygen and peroxyl radicals [39, 40].
In our study, dietary vitamin C intake was positively associated with multiple factor-adjusted BMD only in the group with deficient serum 25(OH)D concentration but not in the group with repleted 25(OH)D concentration (≥50 nmol/L). Low serum 25(OH)D concentration increases the release of PTH, which stimulates bone resorption and bone loss [41]. Vitamin C has been reported to reduce bone resorption by inhibiting osteoclastogenesis and inducing osteoclast apoptosis, especially in high bone-turnover states [12, 42]. Moreover, previous study reported significant inverse relationship between plasma vitamin C level and serum PTH concentration, indicating that higher vitamin C concentrations could suppress PTH elevation [43]. Based on those reports and our findings, vitamin C might have fortified the preventive effects with low serum 25(OH)D status by attenuating high bone turnover.
We observed the strong association in women aged 50–59 years, but this positive association was diminished in women aged 60–69 years and reappeared—albeit weakly—in women ≥70 years. The reasons of this finding are not clear, but we suggest that the differences in the rate of bone loss between those age groups could affect the negative influence of lower vitamin C intake on BMD. The rate of bone loss differs according to postmenopausal status; bone loss initiates and accelerates in transmenopausal period up to 5–10 years after menopause, but the rate then slows [44, 45]. Therefore, we cautiously suggest that the negative effect of lower dietary vitamin C intake on bone might be most influential in vulnerable postmenopausal period of bone metabolism and could explain why the risk of lower vitamin C intake for developing osteoporosis was highest in women aged 50–59 years. However, further studies are needed to clarify such age differences in the effects of vitamin C intake on bone metabolism.
This study has several limitations. First, this was a cross-sectional study and it cannot indicate any direct causal relationships or identify associated mechanisms. Second, we could not obtain data about the blood levels of other oxidants such as flavonoid and serum vitamin C concentration. Third, because of the low incidence of fractures, our study does not have enough power to investigate the association between dietary vitamin C intake and fracture.
To our knowledge, we are the first to investigate the association between dietary vitamin C intake and BMD in relation to serum 25(OH)D concentration and age. This study population had a lower serum 25(OH)D concentration compared with the US and other Caucasian population [46–48] possibly because of the limited exposure to sunlight or inadequate vitamin D intake [49]. Positive associations between dietary vitamin C and multiple factor-adjusted BMD were evident in the group with lower serum 25(OH)D concentration compared with other studies. Based on this, we propose that sufficient dietary vitamin C intakes should be encouraged in postmenopausal women, who are at high risk of bone loss. Moreover, further longitudinal studies are needed to clarify the protective role of dietary vitamin C on future BMD loss.
References
Melton LJ 3rd (2000) Who has osteoporosis? A conflict between clinical and public health perspectives. J Bone Miner Res 15(12):2309–2314. doi:10.1359/jbmr.2000.15.12.2309
Dawson-Hughes B, Harris SS, Krall EA, Dallal GE (1997) Effect of calcium and vitamin D supplementation on bone density in men and women 65 years of age or older. N Engl J Med 337(10):670–676
Cummings SR, Melton LJ (2002) Epidemiology and outcomes of osteoporotic fractures. Lancet 359(9319):1761–1767. doi:10.1016/S0140-6736(02)08657-9
Manolagas SC, Kousteni S, Jilka RL (2002) Sex steroids and bone. Recent Prog Horm Res 57:385–409
Manolagas SC (2010) From estrogen-centric to aging and oxidative stress: a revised perspective of the pathogenesis of osteoporosis. Endocr Rev 31(3):266–300. doi:10.1210/er.2009-0024
Garrett IR, Boyce BF, Oreffo RO, Bonewald L, Poser J, Mundy GR (1990) Oxygen-derived free radicals stimulate osteoclastic bone resorption in rodent bone in vitro and in vivo. J Clin Invest 85(3):632–639. doi:10.1172/JCI114485
Wauquier F, Leotoing L, Coxam V, Guicheux J, Wittrant Y (2009) Oxidative stress in bone remodelling and disease. Trends Mol Med 15(10):468–477. doi:10.1016/j.molmed.2009.08.004
Nishikimi M (1975) Oxidation of ascorbic acid with superoxide anion generated by the xanthine-xanthine oxidase system. Biochem Biophys Res Commun 63(2):463–468
Deutsch JC (1998) Ascorbic acid oxidation by hydrogen peroxide. Anal Biochem 255(1):1–7. doi:10.1006/abio.1997.2293
Morikawa D, Nojiri H, Saita Y, Kobayashi K, Watanabe K, Ozawa Y, Koike M, Asou Y, Takaku T, Kaneko K, Shimizu T (2013) Cytoplasmic reactive oxygen species and SOD1 regulate bone mass during mechanical unloading. J Bone Miner Res 28(11):2368–2380. doi:10.1002/jbmr.1981
Nojiri H, Saita Y, Morikawa D, Kobayashi K, Tsuda C, Miyazaki T, Saito M, Marumo K, Yonezawa I, Kaneko K, Shirasawa T, Shimizu T (2011) Cytoplasmic superoxide causes bone fragility owing to low-turnover osteoporosis and impaired collagen cross-linking. J Bone Miner Res 26(11):2682–2694. doi:10.1002/jbmr.489
Sanbe T, Tomofuji T, Ekuni D, Azuma T, Tamaki N, Yamamoto T (2007) Oral administration of vitamin C prevents alveolar bone resorption induced by high dietary cholesterol in rats. J Periodontol 78(11):2165–2170. doi:10.1902/jop.2007.070181
Maggio D, Barabani M, Pierandrei M, Polidori MC, Catani M, Mecocci P, Senin U, Pacifici R, Cherubini A (2003) Marked decrease in plasma antioxidants in aged osteoporotic women: results of a cross-sectional study. J Clin Endocrinol Metab 88(4):1523–1527
Sugiura M, Nakamura M, Ogawa K, Ikoma Y, Ando F, Shimokata H, Yano M (2011) Dietary patterns of antioxidant vitamin and carotenoid intake associated with bone mineral density: findings from post-menopausal Japanese female subjects. Osteoporos Int 22(1):143–152. doi:10.1007/s00198-010-1239-9
Chuin A, Labonte M, Tessier D, Khalil A, Bobeuf F, Doyon CY, Rieth N, Dionne IJ (2009) Effect of antioxidants combined to resistance training on BMD in elderly women: a pilot study. Osteoporos Int 20(7):1253–1258. doi:10.1007/s00198-008-0798-5
Peterkofsky B, Gosiewska A, Kipp DE, Shah V, Wilson S (1994) Circulating insulin-like growth factor binding proteins (IGFBPs) 1 and 2 induced in vitamin C-deficient or fasted guinea pigs inhibit IGF-I action in cultured cells. Growth Factors 10(4):229–241
Bonucci E (2012) Bone mineralization. Front Biosci (Landmark Ed) 17:100–128
Takamizawa S, Maehata Y, Imai K, Senoo H, Sato S, Hata R-I (2004) Effects of ascorbic acid and ascorbic acid 2-phosphate, a long-acting vitamin C derivative, on the proliferation and differentiation of human osteoblast-like cells. Cell Biol Int 28(4):255–265
Franceschi RT, Iyer BS, Cui Y (1994) Effects of ascorbic acid on collagen matrix formation and osteoblast differentiation in murine MC3T3‐E1 cells. J Bone Miner Res 9(6):843–854
Zhu LL, Cao J, Sun M, Yuen T, Zhou R, Li J, Peng Y, Moonga SS, Guo L, Mechanick JI, Iqbal J, Peng L, Blair HC, Bian Z, Zaidi M (2012) Vitamin C prevents hypogonadal bone loss. PLoS One 7(10), e47058. doi:10.1371/journal.pone.0047058
Park JK, Lee EM, Kim AY, Lee EJ, Min CW, Kang KK, Lee MM, Jeong KS (2012) Vitamin C deficiency accelerates bone loss inducing an increase in PPAR-gamma expression in SMP30 knockout mice. Int J Exp Pathol 93(5):332–340. doi:10.1111/j.1365-2613.2012.00820.x
Yano K, Heilbrun L, Wasnich R, Hankin J, Vogel J (1985) The relationship between diet and bone mineral content of multiple skeletal sites in elderly Japanese-American men and women living in Hawaii. Am J Clin Nutr 42(5):877–888
Leveille SG, LaCroix AZ, Koepsell TD, Beresford SA, Van Belle G, Buchner DM (1997) Dietary vitamin C and bone mineral density in postmenopausal women in Washington State, USA. J Epidemiol Community Health 51(5):479–485
Hall SL, Greendale GA (1998) The relation of dietary vitamin C intake to bone mineral density: results from the PEPI study. Calcif Tissue Int 63(3):183–189
Kaptoge S, Welch A, McTaggart A, Mulligan A, Dalzell N, Day NE, Bingham S, Khaw KT, Reeve J (2003) Effects of dietary nutrients and food groups on bone loss from the proximal femur in men and women in the 7th and 8th decades of age. Osteoporos Int 14(5):418–428. doi:10.1007/s00198-003-1391-6
Ilich JZ, Brownbill RA, Tamborini L (2003) Bone and nutrition in elderly women: protein, energy, and calcium as main determinants of bone mineral density. Eur J Clin Nutr 57(4):554–565. doi:10.1038/sj.ejcn.1601577
Sahni S, Hannan MT, Gagnon D, Blumberg J, Cupples LA, Kiel DP, Tucker KL (2009) Protective effect of total and supplemental vitamin C intake on the risk of hip fracture–a 17-year follow-up from the Framingham Osteoporosis Study. Osteoporos Int 20(11):1853–1861. doi:10.1007/s00198-009-0897-y
Wolf RL, Cauley JA, Pettinger M, Jackson R, Lacroix A, Leboff MS, Lewis CE, Nevitt MC, Simon JA, Stone KL, Wactawski-Wende J (2005) Lack of a relation between vitamin and mineral antioxidants and bone mineral density: results from the Women’s Health Initiative. Am J Clin Nutr 82(3):581–588
Morton DJ, Barrett-Connor EL, Schneider DL (2001) Vitamin C supplement use and bone mineral density in postmenopausal women. J Bone Miner Res 16(1):135–140. doi:10.1359/jbmr.2001.16.1.135
Nieves JW, Komar L, Cosman F, Lindsay R (1998) Calcium potentiates the effect of estrogen and calcitonin on bone mass: review and analysis. Am J Clin Nutr 67(1):18–24
Simon JA, Hudes ES (2001) Relation of ascorbic acid to bone mineral density and self-reported fractures among US adults. Am J Epidemiol 154(5):427–433
Melhus H, Michaelsson K, Holmberg L, Wolk A, Ljunghall S (1999) Smoking, antioxidant vitamins, and the risk of hip fracture. J Bone Miner Res 14(1):129–135. doi:10.1359/jbmr.1999.14.1.129
Lee ES, Forthofer RN (2006) Analyzing complex survey data, 2nd edn. Sage, Thousand Oaks
The Korean Nutrition Society (2010) Dietary reference intakes for Koreans. First revision. Kookjin, Seoul
Takamizawa S, Maehata Y, Imai K, Senoo H, Sato S, Hata R (2004) Effects of ascorbic acid and ascorbic acid 2-phosphate, a long-acting vitamin C derivative, on the proliferation and differentiation of human osteoblast-like cells. Cell Biol Int 28(4):255–265. doi:10.1016/j.cellbi.2004.01.010
New SA, Robins SP, Campbell MK, Martin JC, Garton MJ, Bolton-Smith C, Grubb DA, Lee SJ, Reid DM (2000) Dietary influences on bone mass and bone metabolism: further evidence of a positive link between fruit and vegetable consumption and bone health? Am J Clin Nutr 71(1):142–151
Tucker KL, Chen H, Hannan MT, Cupples LA, Wilson PW, Felson D, Kiel DP (2002) Bone mineral density and dietary patterns in older adults: the Framingham Osteoporosis Study. Am J Clin Nutr 76(1):245–252
Prynne CJ, Mishra GD, O’Connell MA, Muniz G, Laskey MA, Yan L, Prentice A, Ginty F (2006) Fruit and vegetable intakes and bone mineral status: a cross sectional study in 5 age and sex cohorts. Am J Clin Nutr 83(6):1420–1428
Baeuerle PA, Rupec RA, Pahl HL (1996) Reactive oxygen intermediates as second messengers of a general pathogen response. Pathol Biol (Paris) 44(1):29–35
Iotsova V, Caamano J, Loy J, Yang Y, Lewin A, Bravo R (1997) Osteopetrosis in mice lacking NF-kappaB1 and NF-kappaB2. Nat Med 3(11):1285–1289
Lips P (2001) Vitamin D deficiency and secondary hyperparathyroidism in the elderly: consequences for bone loss and fractures and therapeutic implications. Endocr Rev 22(4):477–501. doi:10.1210/edrv.22.4.0437
Hie M, Tsukamoto I (2011) Vitamin C-deficiency stimulates osteoclastogenesis with an increase in RANK expression. J Nutr Biochem 22(2):164–171. doi:10.1016/j.jnutbio.2010.01.002
Richter A, Kuhlmann MK, Seibert E, Kotanko P, Levin NW, Handelman GJ (2008) Vitamin C deficiency and secondary hyperparathyroidism in chronic haemodialysis patients. Nephrol Dial Transplant 23(6):2058–2063. doi:10.1093/ndt/gfn084
Warming L, Hassager C, Christiansen C (2002) Changes in bone mineral density with age in men and women: a longitudinal study. Osteoporos Int 13(2):105–112
Riggs BL, Melton LJ, Robb RA, Camp JJ, Atkinson EJ, McDaniel L, Amin S, Rouleau PA, Khosla S (2008) A population-based assessment of rates of bone loss at multiple skeletal sites: evidence for substantial trabecular bone loss in young adult women and men. J Bone Miner Res 23(2):205–214. doi:10.1359/jbmr.071020
Bischoff-Ferrari HA, Kiel DP, Dawson-Hughes B, Orav JE, Li R, Spiegelman D, Dietrich T, Willett WC (2009) Dietary calcium and serum 25-hydroxyvitamin D status in relation to BMD among U.S. adults. J Bone Miner Res 24(5):935–942. doi:10.1359/jbmr.081242
Steingrimsdottir L, Gunnarsson O, Indridason OS, Franzson L, Sigurdsson G (2005) Relationship between serum parathyroid hormone levels, vitamin D sufficiency, and calcium intake. JAMA 294(18):2336–2341. doi:10.1001/jama.294.18.2336
Joo NS, Dawson-Hughes B, Kim YS, Oh K, Yeum KJ (2013) Impact of calcium and vitamin D insufficiencies on serum parathyroid hormone and bone mineral density: analysis of the fourth and fifth Korea National Health and Nutrition Examination Survey (KNHANES IV-3, 2009 and KNHANES V-1, 2010). J Bone Miner Res 28(4):764–770. doi:10.1002/jbmr.1790
Choi HS, Oh HJ, Choi H, Choi WH, Kim JG, Kim KM, Kim KJ, Rhee Y, Lim SK (2011) Vitamin D insufficiency in Korea–a greater threat to younger generation: the Korea National Health and Nutrition Examination Survey (KNHANES) 2008. J Clin Endocrinol Metab 96(3):643–651. doi:10.1210/jc.2010-2133
Acknowledgments
This study was supported by a research grant (02-2008-036) and (02-2013-051) from Seoul National University Bundang Hospital.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Y. A. Kim and K. M. Kim contributed equally to this work.
Rights and permissions
About this article
Cite this article
Kim, Y.A., Kim, K.M., Lim, S. et al. Favorable effect of dietary vitamin C on bone mineral density in postmenopausal women (KNHANES IV, 2009): discrepancies regarding skeletal sites, age, and vitamin D status. Osteoporos Int 26, 2329–2337 (2015). https://doi.org/10.1007/s00198-015-3138-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-015-3138-6