Abstract
Summary
We determined hypovitaminosis D prevalence in men with psoriatic arthritis. This is a cross-sectional, analyst blinded, age- and sex-matched, case-control study. Men with psoriatic arthritis have significantly lower 25-hydroxyvitamin D levels. Men with psoriatic arthritis are at increased odds of suffering from hypovitaminosis D.
Introduction
Skeletal manifestations as a result of abrupted bone metabolism may be predominant in psoriatic arthritis (PsA). Vitamin D plays a vital role in maintenance of skeletal health and is known to modulate the immune system in various autoimmune diseases including PsA. The aim of the present study was to determine the prevalence of hypovitaminosis D in a treatment naïve, de novo psoriatic arthritis male cohort in a cross-sectional, analyst blinded, age- and sex-matched, case-control study.
Methods
25 hydroxyvitamin D (25OHD), parathyroid (PTH), osteocalcin (OC) and C-terminal telopeptides of type-I collagen (CTx) levels, and lumbar spine and femoral neck bone mineral density were compared between 53 PsA and controls.
Results
The prevalence of hypovitaminosis D (25 hydroxyvitamin D (25OHD) levels <75 nmol/L) was 81 and 57 % in the PsA and control groups, respectively. Compared to the healthy controls, 25OHD (67.2 (12–137) nmol/L vs. 51.9 (15–95) nmol/L; p = 0.001) was significantly lower, and osteocalcin (13.6 (5–33) μg/L vs. 18.2 (6–35) μg/L; p = 0.003) and C-terminal telopeptides of type-I collagen (0.20 (0.01–0.71) μg/L vs. 0.28 (0.06–0.69) μg/L; p = 0.008) were significantly higher in the PsA group. A significant association was found between hypovitaminosis D and PsA; the odds for patients with PsA of having hypovitaminosis D was 3.297 (95 % confidence interval 1.372 to 7.922).
Conclusion
The results of this study suggest that men with PsA have significantly lower 25-hydroxyvitamin D levels, and furthermore, men with PsA are at statistically significant increased odds of suffering from hypovitaminosis D.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Approximately 1–3 % of the world’s population is affected by psoriasis [1]. Inflammatory arthritis known as psoriatic arthritis (PsA), which contributes significantly to the patient’s disease burden with reduction in quality of life, develops in 6–39 % of psoriatic patients [2, 3]. Psoriatic arthritis presents with clinical features of joint inflammation, including erythema, swelling, and warmth. It presents initially in one or a few joints in an asymmetric manner and gradually involves more joints as time passes; ultimately presenting a polyarticular manifestation that is usually symmetric. Joint damage and deformity are typically present in this stage of the disease. In majority of patients, the arthritis follows the development of psoriasis, and in the remainder, it develops simultaneously or before the appearance of skin lesions [4–9]. As such, skeletal manifestations as a result of abrupted bone metabolism may be predominant.
Vitamin D plays a vital role in maintenance of skeletal health [10]. Vitamin D deficiency and consequent secondary hyperparathyroidism are known to cause a decrease in bone mineral density and increase in bone turnover [11–13].
Vitamin D performs different functions besides its traditional role in calcium-phosphorus metabolism, as suggested by the presence of CYP271B (enzyme responsible for 25-hydroxyvitamin D synthesis) and vitamin D receptors (VDRs) in various tissues [14–17]. The regulatory role for vitamin D in the immune system is indicated by the presence of VDRs on activated T lymphocytes, the suppressive or inhibiting effect of 1,25-dihydroxyvitamin D in different autoimmune diseases, and in vitro and in vivo findings of vitamin D-induced changes in immune functions [18, 19]. Furthermore, dermatologists and rheumatologists have observed the effectiveness of vitamin D analogs to treat psoriasis plaques and have observed statistically significant improvement in the tender joint count and physician global impression [20, 21]. Additionally, 1,25-dihydroxyvitamin D3 and its synthetic analogs are being increasingly recognized for their potent antiproliferative, prodifferentiative, and immunomodulatory activities [22].
Autoimmune conditions associated with decreased vitamin D levels include insulin-dependent diabetes mellitus, rheumatoid arthritis, and multiple sclerosis, which share certain immunologic characteristic with psoriasis, such as Th1/Th2 dysregulation [23–25]. We found no study in literature that compared vitamin D status of PsA men with age- and sex-matched controls. As such, the aim of the present study was to determine the prevalence of hypovitaminosis D in a treatment naïve, de novo psoriatic arthritis male cohort in a cross-sectional, analyst blinded, age- and sex-matched, case-control study.
Patients and methods
Men, suffering from psoriasiform skin lesions with articular manifestations, referred to the out-patient division of the Department of Rheumatology, Faculty of Medicine, University of Debrecen, for initial assessment were invited to participate in the study. Recruitment was done consecutively between July 2009 and July 2014. All procedures were carried out after receiving written informed consent. The ethics committee of the Faculty of Medicine, University of Debrecen approved the study protocol.
Blood sampling was done after overnight fasting to measure levels of 25-hydroxyvitamin D (25OHD), PTH, osteocalcin (OC), C-terminal telopeptides of type-I collagen (CTX-I), and procollagen type I amino-terminal propeptide (PINP).
Dual energy X-ray absorptiometry examination was performed using the LUNAR Prodigy (GE-Lunar Corp., Madison, Wisc., USA) densitometer. Bone mineral density (BMD) was measured at L1–L4 lumbar spine (LS) and femoral neck (FN). The coefficient of variation (CV) of the technique at our institute was 0.8 % using the anatomical spine phantom measured daily. Samples from matched healthy controls were taken in the same meteorological season in order to control for seasonal variability.
Plasma 25-OH-D was analyzed by high pressure liquid chromatography (HPLC) using a Jasco HPLC system (Jasco, Tokyo, Japan) and Bio-Rad reagent kit (Bio-Rad Laboratories, Hercules, CA, USA). Serum PTH, OC, CTX-I, and PINP were measured using electrochemiluminescence immunoassay (Roche Diagnostics GmbH, Mannheim, Germany). The inter-assay CV was <3.5 % for 25-OH-D (lower detection limit: 16.5 nmol/L, upper detection limit: 624 nmol/L), <7 % for PTH (lower detection limit: 0.127 pmol/L, upper detection limit: 530 pmol/L), <4 % for OC (lower detection limit: 0.5 μg/L, upper detection limit: 300 μg/L), <7 % for CTX-I (lower detection limit: 0.010 μg/L, upper detection limit: 6 μg/L), and <6 % for PINP (lower detection limit: 5 μg/L, upper detection limit: 1200 μg/L). Hypovitaminosis D was defined as 25-OH-D levels <75 nmol/l as suggested by Dawson-Hughes et al. [26].
Disease severity was evaluated in the PsA group using the disease activity score (DAS28) and psoriasis area and severity index (PASI) [27, 28].
Data from men with psoriatic arthritis was compared to age- and gender-matched healthy volunteers. Men with the closest dates of birth and with blood drawn in the same meteorological season were selected for pairing with their PsA counterparts. Majority of the controls belonged to the HunMen cohort [29]. This matching was feasible for those over 50 years of age (n = 35); the younger healthy age-matched volunteers were escorts, generally family members of the PsA patients (n = 18). Only data from those healthy volunteers that confirmed to the inclusion and/or did not confirm to the exclusion criteria was included in the statistical analysis. Inclusion criteria were male sex, ambulatory, community dwelling, and generally regarded as healthy. Exclusion criteria were known prevalent metabolic bone disease, liver or renal disease (values ≥2× upper limit of normal for total bilirubin, aspartate aminotransferase, alanine aminotransferase, gamma-glutamyl transpeptidase, alkaline phosphatase, lactate dehydrogenase, cholinesterase, urea, creatinine, and uric acid resulted in exclusion), and use of medication influencing bone metabolism (excluding calcium and vitamin D supplementation).
Descriptive statistics are presented, as applicable, as mean, range, and standard deviation (SD). The Kolmogorov-Smirnov test was used to check for normality of distribution. Depending on the distribution of the parameters examined, the paired samples t test or the Wilcoxon signed ranks test was used to compare the age- and gender-matched pairs. The χ 2 test was used to compare categorical variables. The Spearman’s ρ was calculated for correlation analysis. All analyses were performed using the SPSS Statistics software, version 22.0 (IBM Corps., Armonk, NY, USA).
Results
Men (n = 53) presenting with de novo psoriatic arthritis, using CASPAR diagnostic criteria, were included in this cross-sectional, analyst blinded, age- and sex-matched, case-control study [30]. In terms of recruitment, there were no non-responders in either group. The mean age (range) of the individuals in both groups was 54.7 (31–84) years. The prevalence of hypovitaminosis D (25-OH-D <75 nmol/L) was 81 and 57 % in the PsA and control groups, respectively. Although outlined as non-exclusion criteria, we observed that none of the participants used calcium and vitamin D supplementations.
The mean (range) disease duration for psoriasis was 10.8 (0–50.9) years. In a small percentage of the patients (n = 12, 22.6 %), the diagnosis of psoriasis was confirmed following the diagnosis of PsA (on an average in 3 months).
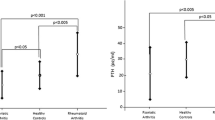
Compared to the healthy controls, 25OHD (67.2 (12–137) nmol/L vs. 51.9 (15–95) nmol/L; p = 0.001, Fig. 1) was significantly lower, and OC (13.6 (5–33) μg/L vs. 18.2 (6–35) μg/L; p = 0.003) and CTX-I (0.20 (0.01–0.71) μg/L vs. 0.28 (0.06–0.69) μg/L; p = 0.008) were significantly higher in the PsA group. There was no statistically significant difference in LS and FN BMD between the two groups (Table 1).
In order to reduce the confounding effect of age, using the median age of 55 years, the study population was divided into two broad age groups, i.e., ≤55 years (n = 27) and >55 years (n = 28) of age. Comparing the PsA and the healthy age-matched groups, vitamin D levels were significantly lower in PsA patients in ≤55 years (49.1 (18–95) nmol/L vs. 67 (12–125) nmol/L, p = 0.015) and >55 years (54.8 (15–91) nmol/L vs. 67.3 (14–137) nmol/L, p = 0.015) age groups.
A significant association was found between hypovitaminosis D and PsA; the odds for PsA patients to suffer with hypovitaminosis D was 3.297 (95 % confidence interval 1.372 to 7.922).
Although DAS28 score did not correlate with 25-OH-D values (r = 0.107, p = 0.610), there was a statistically significant inverse correlation between vitamin D levels and psoriasis extension as measured by PASI (r = −0.440, p = 0.001).
Discussion
In this cross-sectional, age- and gender-matched case-control study, we observed a higher prevalence of hypovitaminosis D in Hungarian men with psoriatic arthritis. Our finding of high hypovitaminosis D prevalence is in concordance with results from one previous study comparing men and women with psoriatic patients (without arthritis) with healthy controls [31]. Another study has reported that there is no difference in vitamin D levels between patients suffering from psoriasis with and without arthritis [32]. We found no study in literature that compared vitamin D status of PsA men with age- and sex-matched controls. A probable assumption for the decreased vitamin D levels in the PsA cohort may be due to the limiting nature of their condition, and as such, they may not involve in physical activity that may be assumed for a healthy age- and sex-matched counterpart; in addition, the psychological burden related to the skin condition may further limit outdoor activity in this patient population.
Based on the levels of the biochemical markers of bone turnover, our study supports assumptions of high bone turnover in the PsA population [33]. High bone turnover, where bone loss is expected, may explain the decreased, although statistically non-significant, BMD in our PsA cohort. Nonetheless, the literature on BMD findings in PsA patients in non-conclusive [34–36].
One recent study has reported that fracture risk is increased in patients with PsA [37]. The comparatively high bone turnover complemented with low vitamin D levels may explain this finding.
There are limitations to our study. Due to no commercially available population registers and difficulties in getting access to the local population register, we employed a method where recruitment of healthy volunteers may have been biased; we compensated for this by screening all volunteers using uniform inclusion/exclusion criteria, and only those results were included in the final data analysis where criteria were adhered to. Nonetheless, all the subjects studied were Caucasian, which is true for the majority of the Hungarian population. Since the demographic and ethic constitution of the population of Debrecen is not different from other regions of Hungary, we consider our control population representative of the general population. Physical activity habits of the subjects were not recorded, as such we cannot account for the contribution of this strong confounder. Foods such as fortified diary products, eggs, and fish contain vitamin D; in general, food is not fortified in Hungary and in addition, there is no uniform fortification policy in Europe. Nonetheless, a dietary questionnaire was not administered in the present study. Determining the amount provided by the sun or food is difficult. The duration and intensity of exposure to sunlight are not easily measurable, and age, skin pigmentation, sunscreens, clothing, and even window glass reduce its effects [38]. In equatorial regions, exposure to the sun alone is adequate, but at latitudes above 40° north or south, people make little vitamin D in the winter. Measurement of 25-OH-D provides direct information, and its concentration depends on age, sunlight exposure, vitamin D dietary intake, or supplementation.
The relatively low number of study participants is the main limitation of this study; nonetheless, we report findings from one of the largest male psoriatic population with arthritis studied as far, and report increased prevalence of hypovitaminosis D in a male PsA cohort complemented with high bone turnover; furthermore, the comparison to a systematically selected healthy age- and gender-matched population discards the effect of confounding risk factors.
Conclusion
In conclusion, the results of this study suggest that men with PsA have significantly lower 25-hydroxyvitamin D levels, and furthermore, men with PsA are at statistically significant increased odds of suffering from hypovitaminosis D.
References
Myers WA, Gottlieb AB, Mease P (2006) Psoriasis and psoriatic arthritis: clinical features and disease mechanisms. Clin Dermatol 24:438–447
Leonard DG, O’Duffy JD, Rogers RS (1978) Prospective analysis of psoriatic arthritis in patients hospitalized for psoriasis. Mayo Clin Proc 53:511–508
Shbeeb M, Uramoto KM, Gibson LE, O’Fallon WM, Gabriel SE (2000) The epidemiology of psoriatic arthritis in Olmstead County, Minnesota, USA, 1982–1991. J Rheumatol 27:1247–1250
Henseler T, Christophers E (1985) Psoriasis of early and late onset: characterization of two types of psoriasis vulgaris. J Am Acad Dermatol 13:450–456
Ferrandiz C, Pujol RM, Garcia-Patos V, Bordas X, Smandia JA (2002) Psoriasis of early and late onset: a clinical and epidemiologic study from Spain. J Am Acad Dermatol 46:867–873
McHugh NJ, Balachrishnan C, Jones SM (2003) Progression of peripheral joint disease in psoriatic arthritis: a 5-yr prospective study. Rheumatology (Oxford) 42:778–783
Gelfand JM, Gladman DD, Mease PJ, Smith N, Margolis DJ, Nijsten T, Stern RS, Feldman SR, Rolstad T (2005) Epidemiology of psoriatic arthritis in the population of the United States. J Am Acad Dermatol 53:573
Gladman D, Antoni C, Mease P, Clegg DO, Nash P (2005) Psoriatic arthritis: epidemiology, clinical features, course, and outcome. Ann Rheum Dis 64:ii14–ii17
Mease PJ, Goffe BS (2005) Diagnosis and treatment of psoriatic arthritis. J Am Acad Dermatol 52:1–19
Omdahl JL, Garry PJ, Hunsaker LA, Hunt WC, Goodwin JS (1982) Nutritional status in a healthy elderly population: vitamin D. Am J Clin Nutr 36:1225–1233
Khaw KT, Sneyd MJ, Compston J (1992) Bone density parathyroid hormone and 25-hydroxyvitamin D concentrations in middle aged women. BMJ 305:273–277
Ooms ME, Lips P, Roos JC, van der Vijgh WJ, Popp-Snijders C, Bezemer PD, Bouter LM (1995) Vitamin D status and sex hormone binding globulin: determinants of bone turnover and bone mineral density in elderly women. J Bone Miner Res 10:1177–1784
McAuley KA, Jones S, Lewis-Barned NJ, Manning P, Goulding A (1997) Low vitamin D status is common among elderly Dunedin women. N Z Med J 110:275–277
Stumpf WE, Sar M, Clark SA, DeLuca HF (1982) Brain target sites for 1,25-dihydroxyvitamin D3. Science 215:1403–1405
Clemens TL, Garrett KP, Zhou XY, Pike JW, Haussler MR, Dempster DW (1988) Immunocytochemical localization of the 1,25-dihydroxyvitamin-D3 receptor in target cells. Endocrinology 122:1224–1230
Haussler MR, Whitfield GK, Haussler CA, Hsieh JC, Thompson PD, Selznick SH, Dominguez CE, Jurutka PW (1998) The nuclear vitamin D receptor: biological and molecular regulatory properties revealed. J Bone Miner Res 13:325–349
Zehnder D, Bland R, Williams MC, McNinch RW, Howie AJ, Stewart PM, Hewison M (2001) Extrarenal expression of 25-hydroxyvitamin D(3)-1 alpha-hydroxylase. J Clin Endocrinol Metab 86:888–894
Bhalla AK, Amento EP, Clemens TL, Holick MF, Krane SM (1983) Specific high-affinity receptors for 1,25-dihydroxyvitamin D3 in human peripheral blood mononuclear cells: presence in monocytes and induction in T lymphocytes following activation. J Clin Endocrinol Metab 57:1308–1310
Provvedini DM, Tsoukas CD, Deftos LJ, Manolagas SC (1983) 1,25-Dihydroxyvitamin D3 receptors in human leukocytes. Science 221:1181–1183
Huckins D, Felson DT, Holick M (1990) Treatment of psoriatic arthritis with oral 1,25-dihydroxyvitamin D3: a pilot study. Arthritis Rheum 33:1723–1727
Dubertret L, Wallach D, Souteyrand P, Perussel M, Kalis B, Meynadier J, Chevrant-Breton J, Beylot C, Bazex JA, Jurgensen HJ (1992) Efficacy and safety of calcipotriol (MC 903) ointment in psoriasis vulgaris: a randomized, double-blind, right/left comparative, vehicle-controlled study. J Am Acad Dermatol 27:983–988
Nagpal S, Na S, Rathnachalam R (2005) Noncalcemic actions of vitamin D receptor ligands. Endocr Rev 26:662–687
Nieves J, Nieves J, Cosman F, Herbert J, Shen V, Lindsay R (1994) High prevalence of vitamin D deficiency and reduced bone mass in multiple sclerosis. Neurology 44:1687–1692
Merlino LA, Curtis J, Mikuls TR, Cerhan JR, Criswell LA, Saag KG (2004) Vitamin D intake is inversely associated with rheumatoid arthritis: results from the Iowa women’s health study. Arthritis Rheum 50:72–77
Devaraj S, Yun JM, Duncan-Staley CR, Jialal I (2011) Low vitamin D levels correlate with the proinflammatory state in type 1 diabetic subjects with and without microvascular complications. Am J Clin Pathol 135:429–433
Dawson-Hughes B, Heaney RP, Holick MF, Lips P, Meunier PJ, Vieth R (2005) Estimates of optimal vitamin D status. Osteoporos Int 16:713–716
Fredriksson T, Pettersson U (1978) Severe psoriasis—oral therapy with a new retinoid. Dermatologica 157:238–244
Prevoo ML, Van’t Hof MA, Kuper HH, Van Leeuwen MA, Van de Putte LB, Van Riel PL (1995) Modified disease activity scores that include twenty-eight-joint counts: development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis Rheum 38:44–48
Bhattoa HP, Nagy E, More C, Kappelmayer J, Balogh A, Kalina E, Antal-Szalmas P (2013) Prevalence and seasonal variation of hypovitaminosis D and its relationship to bone metabolism in healthy Hungarian men over 50 years of age. The HunMen study. Osteoporos Int 24:179–186
Taylor W, Gladman D, Helliwell P, Marchesoni A, Mease P, Mielants H (2006) Classification criteria for psoriatic arthritis: development of new criteria from a large international study. Arthritis Rheum 54:2665–2673
Orgaz-Molina J, Buendía-Eisman CA, Arrabal-Polo MA, Ruiz JC, Arias-Santiago S (2012) Deficiency of serum concentration of 25-hydroxyvitamin D in psoriatic patients: a case-control study. J Am Acad Dermatol 67:931–938
Orgaz-Molina J, Magro-Checa C, Rosales-Alexander JL, Arrabal-Polo MA, Buendía-Eisman A, Raya-Alvarez E, Arias-Santiago S (2013) Association of 25-hydroxyvitamin D serum levels and metabolic parameters in psoriatic patients with and without arthritis. J Am Acad Dermatol 69:938–946
Del Puente A, Esposito A, Parisi A, Atteno M, Montalbano S, Vitiello M, Esposito C, Bertolini N, Foglia F, Costa L, Scarpa R (2012) Osteoporosis and psoriatic arthritis. J Rheumatol 89:36–38
Borman P, Babaoglu S, Gur G, Bingol S, Bodur H (2008) Bone mineral density and bone turnover in patients with psoriatic arthritis. Clin Rheumatol 27:443–447
Attia EA, Khafagy A, Abdel-Raheem S, Fathi S, Saad AA (2011) Assessment of osteoporosis in psoriasis with and without arthritis: correlation with disease severity. Int J Dermatol 50:30–35
Frediani B, Allegri A, Falsetti P, Storri L, Bisogno S, Baldi F, Filipponi P, Marcolongo R (2001) Bone mineral density in patients with psoriatic arthritis. J Rheumatol 28:138–143
Pedreira PG, Pinheiro MM, Szejnfeld VL (2011) Bone mineral density and body composition in postmenopausal women with psoriasis and psoriatic arthritis. Arthritis Res Ther 13:R16
Holick MF (1994) Vitamin D—new horizons for the 21st century. Am J Clin Nutr 60:619–630
Acknowledgments
This work is supported by the Hungarian Scientific Research Fund (OTKA) 105073 research grant (H.P.B.).
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Petho, Z., Kulcsar-Jakab, E., Kalina, E. et al. Vitamin D status in men with psoriatic arthritis: a case-control study. Osteoporos Int 26, 1965–1970 (2015). https://doi.org/10.1007/s00198-015-3069-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-015-3069-2