Abstract
Summary
This study reports a high prevalence of hypovitaminosis D and low bone mineral density (BMD) in a healthy Hungarian male cohort over 50 years of age. Men with 25-hydroxyvitamin D levels of <75 nmol/L had a significantly higher 10-year hip and major osteoporotic fracture probability using the country-specific fracture risk assessment (FRAX) algorithm.
Introduction
The aim of this study is to characterize the prevalence and seasonal variation of hypovitaminosis D and its relationship to bone metabolism in healthy Hungarian men over 50 years of age.
Methods
We determined levels of 25-hydroxyvitamin D (25-OH-D), PTH, osteocalcin (OC), C-terminal telopeptides of type-I collagen (CTX-I), procollagen type 1 amino-terminal propeptide (PINP), BMD at L1–L4 (LS) and femur neck (FN), daily dietary calcium intake, and the 10-year probability of hip fracture and a major osteoporotic fracture using the country-specific FRAX algorithm in 206 randomly selected ambulatory men.
Results
The mean (range) age of the volunteers was 60 (51–81) years. The prevalence of hypovitaminosis D (25-OH-D, <75 nmol/L) was 52.9%. The prevalence of low (T-score < −1.0) BMD at the FN and LS was 45% and 35.4%, respectively. The mean (range) FRAX hip fracture and FRAX major osteoporotic fracture was 0.8% (0–9.4%) and 3.8% (1.7–16%), respectively. On comparing the vitamin D sufficient to the insufficient group, there was a statistically significant difference between the FRAX hip fracture and FRAX major osteoporotic fracture indexes. There was significant seasonal variation in the vitamin D levels; the lowest levels were measured in winter and the highest in summer.
Conclusions
A high prevalence of hypovitaminosis D and low BMD were observed in the studied Hungarian male population. This is the first study reporting higher 10-year hip and major osteoporotic fracture probability using the country-specific FRAX algorithm in individuals with hypovitaminosis D.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vitamin D plays a vital role in maintenance of skeletal health [1]. Vitamin D deficiency and consequent secondary hyperparathyroidism are known to cause a decrease in bone mineral density (BMD) and increase in bone turnover [2–4].
A low 25-hydroxyvitamin D (25-OH-D) concentration is the hallmark of vitamin D deficiency. As such, 25-OH-D is the most important clinically available measurement of vitamin D status, reflecting lifestyle and dietary habits [5, 6]. The determination of the prevalence of hypovitaminosis D has public health implications with regards to formulation of strategies to reduce the burden of metabolic bone diseases.
Although the effect of 25-OH-D on BMD in women has been considerably studied, data on healthy men is accumulating [7–22]. Studies of modifiable risk factors for low bone mass in men are important because of the high prevalence of low bone mass (osteopenia + osteoporosis) in men over 50 years of age (31–53%) [23]. Furthermore, the annual incidence of hip fracture in older men is between 1.5 and 2.4 per 1,000 [24].
With the possibility of assessing the 10-year probability of hip fracture and a major osteoporotic fracture (clinical spine, forearm, hip, or shoulder fracture) using the country-specific World Health Organization (WHO) fracture risk assessment (FRAX) algorithm [25], a novel tool is on the horizon that enables cross-sectional studies to assess relationship of fracture probability with know risk factors for osteoporosis. The aim of this study was to characterize the prevalence and seasonal variation of hypovitaminosis D and its relationship to 10-year probability of hip fracture and a major osteoporotic fracture using the country-specific FRAX algorithm, parathyroid hormone (PTH), daily dietary calcium intake, biochemical markers of bone turnover (osteocalcin (OC), C-terminal telopeptides of type-I collagen (CTX-I), total procollagen type 1 amino-terminal propeptide (PINP)), and BMD at the lumbar spine and femur neck in a random population sample of healthy, community dwelling men over 50 years of age in Hungary.
Materials and methods
Men residing in Debrecen, Hungary (latitude, 47°29′25″; longitude, 21°36′39″; altitude, 107.9 m) were invited to participate in the study from September 2009 to September 2010. During this period, a total of 229 randomly selected volunteers agreed to participate. Permission was received from the local ethics committee, after conception of the study design, and study procedures were carried out following receipt of written informed consent; volunteers not confirming to the inclusion and/or confirming to the exclusion criteria (n = 23) were excluded from the final statistical analysis.
Public attention to the initiative was achieved by placing posters summarizing the main aspects of the survey at general medical dispensaries.
Inclusion criteria were over 50 years of age, male, ambulatory, community dwelling, and generally regarded as healthy. Exclusion criteria were known prevalent metabolic bone disease, liver or renal disease (values ≥2× upper limit of normal (ULN) for total bilirubin, aspartate aminotransferase, alanine aminotransferase, gamma-glutamyl transpeptidase, alkaline phosphatase, lactate dehydrogenase, cholinesterase, urea, creatinine, and uric acid resulted in exclusion), and use of medication influencing bone metabolism (excluding calcium and vitamin D supplementation).
Detailed medical history was collected, and blood sampling was done after overnight fasting. All participants had normal values for serum total calcium and phosphate. A trained study nurse administered a validated questionnaire to assess daily dietary calcium intake [26] and the FRAX index [25].
The FRAX tool has been developed by WHO to evaluate fracture risk of patients. It is based on individual patient models that integrate the risks associated with clinical risk factors as well as BMD at the femoral neck. The FRAX models have been developed from studying population-based cohorts from Europe, North America, Asia, and Australia. In its most sophisticated form, the FRAX tool is computer-driven and is available on their website. The FRAX algorithms give the 10-year probability of fracture. The output is a 10-year probability of hip fracture and the 10-year probability of a major osteoporotic fracture (clinical spine, forearm, hip, or shoulder fracture) [27].
Dual energy X-ray absorptiometry examination was performed using the LUNAR Prodigy (GE-Lunar Corp., Madison, WI, USA) densitometer. BMD was measured at L1–L4 lumbar spine (LS) and femur neck (FN). The coefficient of variation (CV) of the technique at our institute was 0.8% using the anatomical spine phantom measured daily. BMD was expressed as T-score, number of standard deviations from the mean of young men attaining peak bone mass, using the normative reference values (German) provided by the manufacturer. Normalcy, osteopenia, and osteoporosis were defined according to the WHO classification [28].
Plasma 25-OH-D was analyzed by high pressure liquid chromatography (HPLC) using a Jasco HPLC system (Jasco, Tokyo, Japan) and Bio-Rad reagent kit (Bio-Rad Laboratories, Hercules, CA, USA). Serum PTH, OC, CTX-I, and PINP were measured using electrochemiluminescence immunoassay (Roche Diagnostics GmbH, Mannheim, Germany). The inter-assay CV was <3.5% for 25-OH-D (25-OH-D2: lower detection limit, 13.1 nmol/L; upper detection limit, 606 nmol/L; 25-OH-D3: lower detection limit, 16.5 nmol/L; upper detection limit, 624 nmol/L), <7% for PTH (lower detection limit, 0.127 pmol/L; upper detection limit, 530 pmol/L), <4% for OC (lower detection limit, 0.5 μg/L; upper detection limit, 300 μg/L), <7% for CTX-I (lower detection limit, 0.010 μg/L; upper detection limit, 6 μg/L), and <6% for PINP (lower detection limit, 5 μg/L; upper detection limit, 1,200 μg/L). Hypovitaminosis D was defined as 25-OH-D levels <75 nmol/l as suggested by Dawson-Hughes et al. [29]. The daily hours of sunshine in our region were obtained from the Hungarian Meteorological Service [30].
Descriptive statistics are presented, as applicable, as mean, range, and standard deviation (SD). The Kolmogorov–Smirnov test was used to check for normality of distribution. Depending on the distribution of the parameters examined, the Mann–Whitney U test or the independent samples T test was used to compare the means between two groups. One-way analysis of variance (ANOVA) was used for group comparison. Correlation between variables was tested using regression analysis. A value of p < 0.05 was considered statistically significant. All analyses were performed with the PASW Statistics software, version 18.0 (SPSS Inc., Chicago, IL, USA).
Results
The characteristics of the subjects in this cross-sectional study are shown in Table 1. The prevalence of hypovitaminosis D was 52.9%. The percentage of patients having normal, osteopenic, and osteoporotic T-scores at the LS was 64.6%, 27.8%, and 7.7%, respectively, and at the FN was 55%, 42.1%, and 2.9%, respectively. The average dietary calcium intake was lower than the recommended dietary calcium intake [31] in the studied population.
On comparing the participants with normal and low 25-OH-D, significant difference was found only in the 10-year probability of hip fracture (0.58% versus 0.89%; p < 0.05) and a major osteoporotic fracture (clinical spine, forearm, hip, or shoulder fracture; 3.4% versus 4.0%; p < 0.05) using the country-specific WHO FRAX algorithm (Table 1). There was no statistical significance upon multivariate analysis on association between 25-OH-D and BMD even after adjusting for age, BMI, PTH, and daily dietary calcium intake.
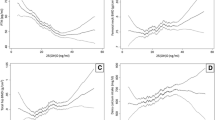
There was a significant correlation between 25-OH-D and the daily hours of sunshine (r = 0.242; p = 0.001), and 10-year probability of hip fracture (r = −0.166; p = 0.017) and a major osteoporotic fracture (clinical spine, forearm, hip, or shoulder fracture; r = −0.175; p = 0.012) using the country-specific WHO FRAX algorithm.
Table 2 shows the patient characteristics in the different seasons. On comparing the means in the different seasons, there was a statistically significant difference (p < 0.01) in the daily hours of sunshine between the seasons, the only exception was between autumn and winter; in PTH levels between autumn and the other seasons; in 25-OH-D levels between summer and the other seasons; in daily dietary calcium intake between winter and spring, and summer; in FRAX (major osteoporotic fracture) index between autumn and spring, and summer and between winter and spring, and summer; and in FRAX (hip fracture) index between autumn and the other seasons. Plasma 25-OH-D values were the highest in summer (mean (range), 83.0 (17–185) nmol/L) followed by spring (mean (range), 67.1 (11–164) nmol/L), autumn (mean (range), 62.7 (16–144) nmol/L), and winter (mean (range), 58.3 (12–113) nmol/L).
Due to a small number of individuals with T-scores ≤ −2.5, for statistical analysis, these individuals were included with those having an osteopenic T-score into a subgroup named the low BMD group.
Table 3 shows patient characteristics based on FN and LS T-scores. Based on the FN T-score, there was a significant difference between normal and low BMD subgroups in mean age (59.2 versus 61.4 years; p = 0.012), BMI (30.2 versus 27.8 kg/m2; p < 0.001), FRAX (major osteoporotic fracture) index (2.9% versus 4.8%; p < 0.001), FRAX (hip fracture) index (0.3% versus 1.3%; p < 0.001), and LS BMD (1.236 versus 1.093 g/cm2; p < 0.001). Comparing the subjects with normal LS T-score to those with low BMD (T-score ≤ −1.0), there was a significant difference in mean BMI (29.6 versus 28.3 kg/m2; p = 0.027), FRAX (major osteoporotic fracture) index (3.4% versus 4.5%; p < 0.001), FRAX (hip fracture) index (0.5% versus 1.2%; p < 0.001), OC (13.6 versus 16.6 μg/L; p < 0.001), CTX-I (0.202 versus 0.256 μg/L; p = 0.006), PINP (35.8 versus 42.7 μg/L; p = 0.004), and FS BMD (1.018 vs. 0.885 g/cm2; p < 0.001).
After controlling for dietary calcium intake and PTH, FRAX (major osteoporotic fracture) and FRAX (hip fracture) indexes were significantly associated with age, FN BMD, and 25-OH-D levels (r 2 = 0.486, p < 0.001 and r 2 = 0.471, p < 0.001, respectively).
Discussion
Vitamin D is needed to maintain calcium absorption and skeletal integrity as much in older as in younger people. We get vitamin D from sunlight exposure and food. In the skin, sunlight (ultraviolet radiation) stimulates the conversion of 7-dehydrocholesterol to previtamin D, which is spontaneously converted to cholecalciferol. Foods such as fortified diary products, eggs, and fish contain vitamin D; in general, food is not fortified in Hungary, and in addition, there is no uniform fortification policy in Europe. Whatever the source of vitamin D, it is then converted sequentially to 25-OH-D in the liver and 1,25-dihydroxyvitamin D, the active hormone, in the kidneys.
Determining the amount provided by the sun or food is difficult. The duration and intensity of exposure to sunlight are not easily measurable, and age, skin pigmentation, sunscreens, clothing, and even window glass reduce its effects [32]. In equatorial regions, exposure to the sun alone is adequate, but at latitudes above 40° north or south, people make little vitamin D in the winter. Measurement of 25-OH-D provides direct information, and its concentration depends on age, sunlight exposure, vitamin D dietary intake, or supplementation.
The prevalence of hypovitaminosis D, in this male cohort, is lower than that previously reported in a postmenopausal Hungarian cohort [33]. Comparing our results with other male studies (Table 4), the mean 25-OH-D level of our study population is higher than those reported in European studies, but is lower than most published from the USA. Although fortification of food in the USA is the most likely reason for the differences in vitamin D status between the two continents [34], there is a possibility that different assay techniques used to determine 25-OH-D levels may yield different results [35].
As reported previously [18, 33], we too observed a seasonal variation in the vitamin D levels of the studied population. This variation went hand in hand with the daily hours of sunshine measured in the different seasons. However, the most probable explanation for the observation that FRAX varies statistically significantly with season is non-similarity in the number of volunteers recruited, and their FRAX-related risk factors, in the different seasons.
The only other study where a representative Hungarian male cohort (n = 431) has been assessed is the multicentric European Male Ageing Study (EMAS), where Szeged, Hungary contributed as one of the eight European centers. Here, quantitative ultrasound heel (qUH) measurement and not axial BMD measurements were carried out, and the qUH parameters were associated with age and lifestyle factors [36]. Although the mean 25-OH-D level of the overall EMAS population is below that observed in our cohort, the vitamin D status of the EMAS Hungarian cohort has not been detailed [22]. Nonetheless, the mean 25-OH-D value of the Hungarian male cohort (n = 19) in the SENECA study [8] is below that observed in the present study. The relationship of vitamin D levels and bone health status of the Hungarian male population has not been characterized as systematically as it has been in this study. Perhaps one major limitation of BMD assessment in Hungary is the lack of a local reference population and non-uniformity in the use of the NHANES III reference population to determine the T-scores.
The fact that vitamin D status did not show any correlation with the LS and FN BMD values is in disagreement with a previous Hungarian postmenopausal study [33], where vitamin D levels showed good correlation with FN BMD. However, Kudlacek et al. [15] and Hannan et al. [20] have also reported non-association between BMD and vitamin D values in the studied male population.
This study shows an apparent discrepancy that FRAX, but not BMD, is associated with vitamin D levels. The FRAX index integrates the risks associated with clinical risk factors as well as BMD at the femoral neck, as such gives a complex account of the confounders related to fracture risk. Low vitamin D levels have been reported to coincide with increased fracture prevalence, and our study concludes this for the FRAX index.
There was a statistically significant negative correlation between FN and LS BMD with OC, PINP and OC, CTX-I, and PINP, respectively. It is known from previous studies that there is an inverse correlation between bone loss and markers of bone resorption and bone formation [37–39].
We are not aware of previous results for daily dietary calcium intake from Hungarian men, but daily dietary calcium intake in our male cohort is higher than that reported previously in two Hungarian postmenopausal cohorts [33, 40].
There are limitations to our study. Due to no commercially available population registers and difficulties in getting access to the local population register, we employed a method where recruitment may have been biased; we compensated for this by screening all volunteers using uniform inclusion/exclusion criteria, and only those results were included in the final data analysis where criteria were adhered to. Nonetheless, all the patients studied were Caucasian, which is true for the majority of the Hungarian population. As such, the study population can be regarded as representative of the general population. Study participation was possible between Septembers of 2009 and 2010, but the majority volunteered in spring and summer; although there was no difference in the mean age and BMI of the participants volunteering in the different seasons, the non-similar number of volunteers in the different seasons may have distorted the statistical findings pertaining to the seasonality of the factors studied. Although our results support findings from prospective studies showing seasonal variations of vitamin D level, the cross-sectional design of our study has limitations with this regard. Physical activity habits of the subjects were not recorded; as such, we cannot account for the contribution of this strong confounder. Furthermore, the small sample size of our study necessitated the use of less clinically meaningful intermediate low values for both the primary exposure (vitamin D) and outcome (BMD).
Although the absolute overall fracture probability in the studied cohort may not be considered grave, this is the first study that reports significant differences in fracture probability, using the FRAX tool, between healthy individuals with normal and low vitamin D levels. As more FRAX data is being published from various countries, there may eventually be a possibility of ranking the fracture probabilities not only by age and sex but also by the nationality of the studied population.
The high prevalence of hypovitaminosis D and its association with increased fracture probability, not disregarding the favorable effects of vitamin D supplementation on the overall health status of an individual, warrant the use of the recent cut-off value to define optimal vitamin D status [41].
According to one report, in the year 2010, the greatest economic burden on the Hungarian National Health Care System was imposed by the treatment of hip fractures (13 billion HUF/≈48 million EUR) [42], surprisingly, surpassing treatment costs of stroke or cardiovascular complications. In light of these grave socioeconomic considerations, our results have demonstrated that the bone health status can be effectively assessed by using the open access web-based, country-specific WHO FRAX calculator, BMD measurement, and readily accessible laboratory examinations. The implication of this algorithm may prevent the much dreaded osteoporotic fractures by helping to identify the target population that needs prompt medical attention in due time.
References
Omdahl JL, Garry PJ, Hunsaker LA, Hunt WC, Goodwin JS (1982) Nutritional status in a healthy elderly population: vitamin D. Am J Clin Nutr 36:1225–1233
Khaw KT, Sneyd MJ, Compston J (1992) Bone density parathyroid hormone and 25-hydroxyvitamin D concentrations in middle aged women. BMJ 305:273–277
Ooms ME, Lips P, Roos JC et al (1995) Vitamin D status and sex hormone binding globulin: determinants of bone turnover and bone mineral density in elderly women. J Bone Miner Res 10:1177–1784
McAuley KA, Jones S, Lewis-Barned NJ, Manning P, Goulding A (1997) Low vitamin D status is common among elderly Dunedin women. N Z Med J 110:275–277
Dawson-Hughes B, Dallal GE, Krall EA, Harris S, Sokoll LJ, Falconer G (1991) Effect of vitamin D supplementation on wintertime and overall bone loss in healthy postmenopausal women. Ann Int Med 115:505–512
Hollis BW (1996) Assessment of vitamin D nutritional and hormonal status: what to measure and how to do it. Calcif Tissue Int 58:4–5
Sherman SS, Hollis BW, Tobin JD (1990) Vitamin D status and related parameters in a healthy population: the effects of age, sex, and season. J Clin Endocrinol Metab 71:405–413
van der Wielen RP, Lowik MR, van den Berg H et al (1995) Serum vitamin D concentrations among elderly people in Europe. Lancet 346:207–210
Dawson-Hughes B, Harris SS, Dallal GE (1997) Plasma calcidiol, season, and serum parathyroid hormone concentrations in healthy elderly men and women. Am J Clin Nutr 65:67–71
Jacques PF, Felson DT, Tucker KL et al (1997) Plasma 25-hydroxyvitamin D and its determinants in an elderly population sample. Am J Clin Nutr 66:929–936
Chapuy MC, Preziosi P, Maamer M et al (1997) Prevalence of vitamin D insufficiency in an adult normal population. Osteoporos Int 7:439–443
Woitge HW, Scheidt-Nave C, Kissling C et al (1998) Seasonal variation of biochemical indexes of bone turnover: results of a population-based study. J Clin Endocrinol Metab 83:68–75
Lamberg-Allardt CJ, Outila TA, Karkkainen MU, Rita HJ, Valsta LM (2001) Vitamin D deficiency and bone health in healthy adults in Finland: could this be a concern in other parts of Europe? J Bone Miner Res 16:2066–2073
Looker AC, Dawson-Hughes B, Calvo MS, Gunter EW, Sahyoun NR (2002) Serum 25-hydroxyvitamin D status of adolescents and adults in two seasonal subpopulations from NHANES III. Bone 30:771–777
Kudlacek S, Schneider B, Peterlik M et al (2003) Assessment of vitamin D and calcium status in healthy adult Austrians. Eur J Clin Invest 33:323–331
Szulc P, Munoz F, Marchand F, Chapuy MC, Delmas PD (2003) Role of vitamin D and parathyroid hormone in the regulation of bone turnover and bone mass in men: the MINOS study. Calcif Tissue Int 73:520–530
Maggio D, Cherubini A, Lauretani F et al (2005) 25(OH)D Serum levels decline with age earlier in women than in men and less efficiently prevent compensatory hyperparathyroidism in older adults. J Gerontol A Biol Sci Med Sci 60:1414–1419
Bolland MJ, Grey AB, Ames RW, Mason BH, Horne AM, Gamble GD, Reid IR (2006) Determinants of vitamin D status in older men living in a subtropical climate. Osteoporos Int 17:1742–1748
Saquib N, von Muhlen D, Garland CF, Barrett-Connor E (2006) Serum 25-hydroxyvitamin D, parathyroid hormone, and bone mineral density in men: the Rancho Bernardo study. Osteoporos Int 17:1734–1741
Hannan MT, Litman HJ, Araujo AB et al (2008) Serum 25-hydroxyvitamin D and bone mineral density in a racially and ethnically diverse group of men. J Clin Endocrinol Metab 93:40–46
Araujo AB, Travison TG, Esche GR, Holick MF, Chen TC, McKinlay JB (2009) Serum 25-hydroxyvitamin D and bone mineral density among Hispanic men. Osteoporos Int 20:245–255
McBeth J, Pye SR, O'Neill TW et al (2010) Musculoskeletal pain is associated with very low levels of vitamin D in men: results from the European Male Ageing Study. Ann Rheum Dis 69(8):1448–1452
Looker AC, Orwoll ES, Johnston CC Jr et al (1997) Prevalence of low femoral bone density in older U.S. adults from NHANES III. J Bone Miner Res 12:1761–1768
Zingmond DS, Melton LJ 3rd, Silverman SL (2004) Increasing hip fracture incidence in California Hispanics, 1983 to 2000. Osteoporos Int 15:603–610
Fardellone P, Sebert JL, Bouraya M, Bonidan O, Leclercq G, Doutrellot C, Bellony R, Dubreuil A (1991) Evaluation of the calcium content of diet by frequential self-questionnaire. Rev Rhum Mal Osteoartic 58(2):99–103
Kanis JA, Melton LJ 3rd, Christiansen C, Johnston CC, Khaltaev N (1994) The diagnosis of osteoporosis. J Bone Miner Res 9:1137–1141
Dawson-Hughes B, Heaney RP, Holick MF, Lips P, Meunier PJ, Vieth R (2005) Estimates of optimal vitamin D status. Osteoporos Int 16:713–716
Anonymous (1994) National Institute of Health Consensus Conference. Optimal calcium intake. JAMA 272:1942–1948
Holick MF (1994) Vitamin D—new horizons for the 21st century. Am J Clin Nutr 60:619–630
Bhattoa HP, Bettembuk P, Ganacharya S, Balogh A (2004) Prevalence and seasonal variation of hypovitaminosis D and its relationship to bone metabolism in community dwelling postmenopausal Hungarian women. Osteoporos Int 15(6):447–451
Holick MF (2007) Vitamin D deficiency. N Engl J Med 357:266–281
Binkley N, Krueger D, Cowgill CS et al (2004) Assay variation confounds the diagnosis of hypovitaminosis D: a call for standardization. J Clin Endocrinol Metab 89:3152–3157
Pye SR, Devakumar V, Boonen S et al (2010) Influence of lifestyle factors on quantitative heel ultrasound measurements in middle-aged and elderly men. Calcif Tissue Int 86(3):211–219
Khosla S, Melton LJ 3rd, Atkinson EJ, O'Fallon WM, Klee GG, Riggs BL (1998) Relationship of serum sex steroid levels and bone turnover markers with bone mineral density in men and women: a key role for bioavailable estrogen. J Clin Endocrinol Metab 83(7):2266–2274
Ross PD, Knowlton W (1998) Rapid bone loss is associated with increased levels of biochemical markers. J Bone Miner Res 3(2):297–302
Nguyen TV, Meier C, Center JR, Eisman JA, Seibel MJ (2007) Bone turnover in elderly men: relationships to change in bone mineral density. BMC Musculoskelet Disord 8:13
Bruyere O, De Cock C, Mottet C, Neuprez A, Malaise O, Reginster JY (2009) Low dietary calcium in European postmenopausal osteoporotic women. Public Health Nutr 12(1):111–114
Adams JS, Hewison M (2010) Update in vitamin D. J Clin Endocrinol Metab 95(2):471–478
Acknowledgements
This work is supported by the János Bolyai Research Scholarship of the Hungarian Academy of Science (H.P. Bhattoa), the DE OEC Mec-3/2008 research grant (H.P. Bhattoa), and the TÁMOP 4.2.1./B-09/1/KONV-2010-0007 project (H.P. Bhattoa, E. Nagy, C. More, J. Kappelmayer, A. Balogh, and P. Antal-Szalmas), which is implemented through the New Hungary Development Plan, co-financed by the European Social Fund.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bhattoa, H.P., Nagy, E., More, C. et al. Prevalence and seasonal variation of hypovitaminosis D and its relationship to bone metabolism in healthy Hungarian men over 50 years of age: the HunMen Study. Osteoporos Int 24, 179–186 (2013). https://doi.org/10.1007/s00198-012-1920-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-012-1920-2