Abstract
Summary
This study explored the distribution of vertebral fractures in hip fracture patients. Unlike patients with intertrochanteric fractures, those with subcapital fractures were less likely to have vertebral fractures in the T4-T10 region of the spine. The dissimilar distribution of vertebral fractures among patients with intertrochanteric and subcapital fractures may indicate different underlying etiologies.
Introduction
There are two main types of hip fractures: intertrochanteric and subcapital. Both types can have associated vertebral fractures. In this study, we explored the distribution of vertebral fractures in the two hip fracture populations.
Methods
This was a retrospective analysis of a convenience sample of 120 patients: 40 with subcapital fractures and vertebral fractures, 40 with intertrochanteric fractures and vertebral fractures, and 40 with vertebral fractures only. Based on Genant’s semiquantitative assessment method of radiographic images, the distribution and severity of each patient’s vertebral fractures were explored [1].
Results
Patients with subcapital fractures had significantly fewer total vertebral fractures (93 vs. 144, p = 0.005; 93 vs. 127, p = 0.019), vertebral fractures from T4 to T10 (41 vs. 81, p = 0.005; 41 vs. 64, p = 0.042), and vertebral fractures at the T7-T8 peak (11 vs. 31, p = 0.002; 11 vs. 30, p = 0.003) than patients with intertrochanteric fractures and those with vertebral fractures alone, respectively, and they were more likely to have only one vertebral fracture (15 vs. 3, p < 0.001; 15 vs. 2, p < 0.001). The number of vertebral fractures from T11 to L4 and at the T12-L1 peak did not differ among the groups. The numbers of fractures at each vertebral level was significantly correlated only between those with intertrochanteric fractures and those with vertebral fractures alone (r = 0.65, p = 0.009).
Conclusion
The distribution of vertebral fractures among patients with subcapital fractures differed from the other fracture groups, which may indicate that subcapital fractures and some lumbar fractures have a different underlying etiology than intertrochanteric fractures and thoracic (T4-T10) fractures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The vertebral fracture is to a large extent the predominant fracture seen in patients with osteoporosis; however, such fractures can be caused by trauma (i.e., falling), and many people with vertebral fractures do not have low bone density [2]. The occurrence of a fracture is the result of an interaction between bone strength and the degree of trauma. For example, in younger men, there are more vertebral fractures than in younger women, likely reflecting their greater exposure to more traumatic sports and occupations [3]. Any vertebral damage sustained in earlier life will still be present in later life and so such fractures may not reflect the presence of osteoporosis. It is probable that the site of the fracture is a result of the nature of the trauma and the place in the spine where the force is highest.
The distribution of vertebral fractures in osteoporosis is bimodal: mid-thoracic fractures occur most frequently at T7-8 and thoracolumbar fractures occur most frequently at T12-L1 [1, 3–5]. Interestingly, this distribution was found irrespective of whether or not there was a previous history of trauma [3]. Analysis of data from the Fracture Intervention Trial (FIT), to address the issue of whether or not alendronate would preferentially prevent vertebral fractures in different areas of the spine, showed that new fractures in the upper spine (T4-T10) were more strongly associated with a low bone mineral density (BMD) than were new fractures in the lower spine (T11-L4) raising the possibility that thoracic fractures are more reflective of osteoporosis than those in the lower spine [4].
Defining osteoporosis in patients with a hip fracture presents further problems. Previous studies have described differences between subcapital and intertrochanteric hip fractures, the two main types, in terms of bone density, bone quality, and other clinical risk factors [6–10]. The Study of Osteoporotic Fractures concluded that subcapital and intertrochanteric fractures did have different risk factors. Poor functional status and BMD predicted femoral neck fractures, while aging and poor health predicted intertrochanteric fractures [6]. There have been conflicting reports about the frequency of vertebral fractures among these two fracture groups although, more recently, the BREAK study found that patients with intertrochanteric fractures had significantly more vertebral fractures than those with subcapital fractures [6, 8, 11–13]. Researchers have hypothesized that further understanding of these two fracture groups might represent an area for improvement in our current assessment of fracture risk [14]. It has been suggested that the intertrochanteric fracture may be the osteoporotic hip fracture, while the subcapital fracture may be more trauma-related and occur in those with better bones [15]. A different response to prevention might therefore be expected but, unfortunately, previous studies of osteoporosis treatments were not analyzed to show if one type of hip fracture was preferentially prevented by pharmacological treatment.
The purpose of this study was to describe the distribution and spinal deformity index (SDI) of vertebral fractures among patients with vertebral fractures drawn from three fracture groups: those with subcapital fractures, those with intertrochanteric fractures, and those with only vertebral fractures. We hypothesized that if the etiology of the subcapital fracture is different from that of the intertrochanteric fracture, this might be reflected in a different distribution of vertebral fractures in the two groups and the distribution of vertebral fractures in the intertrochanteric fracture patients might be closer to that seen in the osteoporotic vertebral fracture patients.
Methods
Patient selection
This was a retrospective data review of a sample of patients with vertebral fractures, but no hip fracture, presenting to the St. Joseph’s Health Care Outpatient Osteoporosis Clinic, and patients with subcapital or intertrochanteric hip fractures and concomitant vertebral fractures admitted to the Parkwood Hospital Geriatric Rehabilitation Unit (GRU) in London, Ontario, between 2007 and 2013. Patients were included in the study if they had lateral and anteroposterior (AP) radiographs of the thoracic and lumbar spine. An AP view of the pelvis was also needed if they were being considered for one of the patient groups with concurrent hip and vertebral fractures. Working in reverse order from 2013, patient charts were sequentially selected from a list of patients who had been seen in either the osteoporosis clinic or the GRU. Enrolment in each group was completed when 40 patients were found that met the aforementioned inclusion criteria. Some of the radiographs and vertebral fracture height measurements analyzed in this study were previously used in a study by Crilly et al., where a comparison was made between groups of patients with hip fractures, vertebral fractures, or both, to show that those with vertebral fractures have the worst and those with hip fractures, but no vertebral fractures, the best bone mineral density [16]. All patients from the osteoporosis clinic were referred for the management of osteoporosis, defined as the presence of spinal compression fractures and reduced spinal bone mineral density.
There were 120 patients included in this study: 80 patients from the GRU and 40 patients from the Osteoporosis Clinic. Of the patients from the GRU, 40 patients had a trochanteric fracture and at least one associated vertebral fracture and 40 patients had a subcapital fracture and at least one associated vertebral fracture. All 40 patients from the Osteoporosis Clinic had previously sustained vertebral fractures, but none had a history of hip fracture. Each patient’s age at the time of hip fracture was taken from the patient’s chart. The age of each patient with only vertebral fractures was calculated from information on their electronic health record and the date on their initial outpatient radiographs. For patients admitted to the GRU, the height and weight were recorded upon admission to rehabilitation, while this information was taken from BMD data for patients at the Osteoporosis Clinic.
Measurements
Lateral radiographs of the thoracic and lumbar spine were used to assess each vertebra from T4 to L5 for the presence and severity of vertebral fractures based on the methodology of Genant et al. [1]. Each vertebral fracture was then assigned a grade (0, 1, 2, or 3). A grade of 0 means that there is no fracture. A grade 1 fracture represents a mild deformity and it has a 20–25 % reduction in height at either the anterior, middle, or posterior location of the vertebral body. Grade 2 fractures represent a more moderate deformity as evidenced by a 25–40 % reduction in height at the anterior, middle, or posterior locations. A grade 3 fracture is the most severe form of vertebral fracture with evidence of >40 % height loss at the anterior, middle, or posterior locations. The SDI was calculated by taking the sum of the grades assigned to each vertebral fracture. The total number of vertebral fractures and their distribution throughout the spine was recorded.
Analysis
Patients’ baseline characteristics were compared using standard descriptive statistics (mean and standard deviation). The one-way analysis of variance (ANOVA) was used to detect differences between means of samples of numerical data. Fisher’s LSD test was used to do follow-up analyses for between-group differences. A chi-square test was used to calculate p values when groups of categorical variables were compared. The Pearson’s r correlation was used to indicate if there was a correlation between the number of vertebral fractures measured at each spinal vertebrae (T4-L4) between the three fracture groups. Results were considered to be statistically significant at p < 0.05. Statistical analysis was performed using GraphPad Prism Software, version 6.02.
For analysis, we considered the thoracic spine to be composed of the vertebrae from T4 to T10 and the lumbar spine to be composed of vertebrae from T11 to L4. The point of division represents the nadir of the bimodal distribution and it was previously used in an analysis by Nevitt et al. [4].
Ethics approval was obtained through the Western University Health Sciences Research Ethics Board.
Results
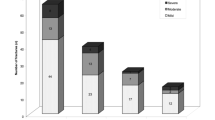
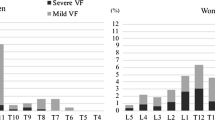
The baseline characteristics of the 40 patients in each of the three fracture groups are outlined in Table 1. Apart from the patients in the vertebral fracture group being younger than their counterparts with subcapital fractures (p < 0.001) and trochanteric fractures (p = 0.02), the three fracture groups were not significantly different in terms of height, weight, or number of women in each group at baseline. Age, although significantly lower in the vertebral fracture group, did not correlate with the number of fractures either within or between groups. The distribution by region (T4-T10 and T11-L4) and type of vertebral fracture in the three groups is shown in Fig. 1. The vertebral fractures in the group of patients with only vertebral fractures were of the expected bimodal form and they were mirrored by the distribution in the intertrochanteric fracture patients; however, the subcapital fracture patients lacked a clear thoracic peak.
This graph illustrates the distribution of fractures among the spinal vertebrae. The total number of vertebral fractures at each spinal vertebral was significantly correlated between the group of patients with intertrochanteric fractures and vertebral fractures only (r = 0.65, p < 0.001), while there was no significant correlation found between the groups of patients with subcapital fractures and intertrochanteric fractures (r = 0.24, p = 0.091) or the groups of patients with subcapital fractures and vertebral fractures only (r = 0.29, p = 0.055)
There were significantly fewer vertebral fractures among those patients in the subcapital fracture group than in the intertrochanteric fracture group (93 vs. 144, p < 0.001) or the vertebral fracture group (93 vs. 127, p = 0.019). The number of vertebral fractures did not differ among the group of patients with only vertebral fractures and those in the intertrochanteric fracture group (127 vs. 144, p = 0.23). Patients with subcapital fractures had fewer vertebral fractures from T4 to T10 than either the patients in the intertrochanteric fracture group (41 vs. 81, p < 0.001) or the group with vertebral fractures alone (41 vs. 64 p = 0.042), but there was no significant difference in the number of vertebral fractures from T4 to T10 between those patients with intertrochanteric fractures and those with vertebral fractures alone (81 vs. 64, p = 0.13). When the number of vertebral fractures from T11 to L4 was compared between those with subcapital fractures and intertrochanteric fractures (52 vs. 63, p = 0.31), those with subcapital fractures and vertebral fractures alone (52 vs. 63, p = 0.31), and those with intertrochanteric fractures and vertebral fractures alone (63 vs. 63, p = 1.0), there were no significant differences found. Patients in the subcapital fracture group had significantly fewer vertebral fractures at the T7-8 peak than either the intertrochanteric group (11 vs. 31, p = 0.002) or the vertebral fracture group (11 vs. 30, p = 0.003), while the intertrochanteric and vertebral groups did not differ (31 vs. 30, p = 0.87). In contrast, there was no difference seen in the number of vertebral fractures at the T12-L1 peak between those with subcapital fractures and intertrochanteric fractures (29 vs. 28, p = 0.86), those with subcapital fractures and vertebral fractures (29 vs. 31, p = 0.73), or those with intertrochanteric fractures and vertebral fractures alone (28 vs. 31, p = 0.60).
The mean SDI of the subcapital fracture group was significantly lower than that of the intertrochanteric fracture group (4.03 vs. 5.50, p = 0.02) and the vertebral fracture group (4.03 vs. 5.53, p = 0.018). The mean SDI did not vary significantly between the intertrochanteric fracture group and the vertebral fracture group (5.50 vs. 5.53, p = 0.97). When the severity of each individual vertebral fracture was analyzed, there were no significant differences seen among those with subcapital fractures and intertrochanteric fractures (1.80 vs. 1.61, p = 0.18), those with subcapital fractures and vertebral fractures (1.80 vs. 1.76, p = 0.79), or those with intertrochanteric fractures and vertebral fractures alone (1.61 vs. 1.76, p = 0.29).
The number of vertebral fractures from T4 to L4 was not significantly correlated between the subcapital and intertrochanteric groups (r = 0.24, p = 0.091) nor was there a significant correlation between the subcapital and vertebral fracture groups (r = 0.29, p = 0.055); whereas, there was a significant correlation between the intertrochanteric and vertebral fracture groups (r = 0.65, p < 0.001).
Patients in the subcapital fracture group were significantly more likely to have only one vertebral fracture than both the intertrochanteric group (15 vs. 3, odds ratio (OR) 5.94, 95 % CI 1.5–22.9, p = 0.010) and the vertebral fracture group (15 vs. 2, OR 9.15, 95 % CI 1.9–43.9, p = 0.003). There was no difference in the number of patients who had only one vertebral fracture when those in the intertrochanteric and vertebral fracture groups were compared (3 vs. 2, OR 0.65, 95 % CI 0.10–4.11, p = 0.64).
Discussion
This study has found that patients with intertrochanteric fractures and concomitant vertebral fractures have a distribution of vertebral fractures similar to the group of osteoporotic patients with only vertebral fractures. On the other hand, patients with a subcapital fracture differ from those patients with only vertebral fractures in terms of both the number and distribution of their vertebral fractures—these being fewer, frequently single, and more often confined to the lower spine. In keeping with previous studies, there was a greater prevalence of vertebral fractures among patients with intertrochanteric fractures than their counterparts with subcapital fractures [8, 11–13]. Although patients with intertrochanteric fractures have more vertebral fractures, we found that the individual severity of each fracture does not differ between hip fracture types.
The novel finding in this study is that patients with intertrochanteric fractures show the well-described bimodal vertebral fracture distribution, peaking at T7-8 and T12-L1, while the subcapital fracture patients with vertebral fractures lack the thoracic peak showing only a peak at the T12-L1 region. This could mean that the vertebral fractures observed in patients with intertrochanteric fractures reflect a pathophysiology similar to that seen in those patients with only vertebral fractures, while the vertebral fractures seen in the patients with subcapital fractures may reflect a different etiology. This may be explained by bone morphology and the mechanism of fracture. In terms of morphology, the intertrochanteric region is composed of a greater percentage of trabecular bone, much like spinal vertebrae, while the femoral neck region has a greater percentage of cortical bone [17, 18]. Various reports, though not totally consistent, suggest that the subcapital fracture patients have better bone mineral density than those with intertrochanteric fractures pointing toward a greater degree of osteoporosis in the latter [6, 13, 15]. With regard to the mechanism of fracture, it is likely that almost all hip fractures are traumatic in nature to a significant degree. The energy produced in a fall from standing height has been shown to be sufficient to fracture any hip if the patient lands on the greater trochanter and biomechanics likely play an important role in sustaining a hip fracture [19–21]. It has been suggested that trabecular osteoporosis, if present, will make the intertrochanteric region vulnerable, while if the intertrochanteric region is strong, the force gets passed along to shear off the head of the femur [22].
The pattern of falls among elderly people differs from that of younger patients (hence the hip fracture). The type of fall that breaks the hip might put the greatest force on the lumbar spine and this may be sufficient to break a normal vertebra; however, in the thoracic spine, where the force is less, fractures would occur only if the bone density was compromised with, perhaps, the greatest force acting at T7-8 where the natural thoracic kyphosis is greatest [23]. This interpretation would be consistent with the findings of a follow-up study from the Fracture Intervention Trial (FIT), which found that new fractures in the upper spine (T4-T10) were more likely to be associated with a low bone mineral density (BMD) than were new fractures in the lower spine (T11-L4) [4]. The authors also found that while prevalent vertebral fractures were associated with an increased risk of subsequent vertebral fractures, this risk was greatest for new vertebral fractures in the T4-T10 region. Additionally, the analysis of data from the Fracture Intervention Trial found that there was a tendency toward greater fracture reduction at the T7-8 peak than at the T12-L1 peak with the use of alendronate, which again suggests that those with thoracic fractures are more osteoporotic [4].
The logical conclusion of this hypothesis is that not all vertebral fractures reflect osteoporosis and may not automatically indicate a need for treatment with osteoporosis medications. The findings of our study lend further support to the argument that not all vertebral fractures should be treated as equal when being considered in fracture risk assessment tools. Our results, combined with those of the FIT, further suggest that the location of fractures may also be an important factor to consider when assessing a patient’s fracture risk [4].
The study previously done by Crilly and Cox found that patients with vertebral fractures alone had lower bone mineral densities than those patients with both vertebral fractures and hip fractures and that both of the aforementioned groups had lower bone mineral densities than the group of patients with only hip fractures [16]. Unfortunately, there are several limitations to both studies that limit direct comparisons between them. Our current study lacked bone mineral density data for most of the patients with concurrent hip and vertebral fractures, while the study by Crilly and Cox did not divide the group of patients with hip fractures by hip fracture type.
There are several weaknesses in our study methodology. First of all, this is a retrospective study based on a convenience sample of patients with hip fractures who were admitted to the Geriatric Rehabilitation Unit. Patients who were discharged home from the orthopedic unit or directly to Long Term Care establishments were excluded from our study sample. Hip fracture patients whose physical condition was adequate to return home without rehabilitation were also not represented in this study. Second, the patients with vertebral fractures were outpatients seen in an osteoporosis clinic so these patients may have differences in baseline characteristics, such as level of frailty, which were not accounted for in this study. Third, clinical information regarding the circumstances under which the vertebral and hip fractures occurred, including whether or not they were the result of trauma, is also not known, reflecting the retrospective nature of the study. Fourth, the study population consisted of both men and women, which may have influenced the nature of the vertebral and hip fractures; however, each of the groups had a similar number of men and women. The study populations also differed in that the group of patients with only vertebral fractures was significantly younger than the other two groups. A prospective study to describe the interrelationships between bone strength, fall type, vertebral fracture location and hip fracture type is needed.
Conclusion
In comparing those patients with vertebral fractures alone, or in association with subcapital or intertrochanteric hip fractures, we found that the patients with subcapital fractures have a vertebral fracture distribution that differentiates them from the patients with intertrochanteric fractures and those patients with vertebral fractures alone. This may indicate that patients with intertrochanteric fractures who have multiple fractures throughout the thoracolumbar spine, in particular those with thoracic fractures, may be more osteoporotic than their counterparts with subcapital fractures. Furthermore, additional research into the vertebral fractures of the thoracic spine may enhance our current understanding of the pathophysiology of osteoporosis and help us to better target patients who can benefit from osteoporosis treatments in the future.
References
Genant HK, Jergas M, Palermo L, Nevitt M, Valentin RS, Black D, Cummings SR (1996) Comparison of semiquantitative visual and quantitative morphometric assessment of prevalent and incident vertebral fractures in osteoporosis. J Bone Miner Res 11:984–96
Siris ES, Chen Y, Abbott TA, Barrett-Connor E, Miller PD, Wehren LE, Berger ML (2004) Bone mineral density thresholds for pharmacological intervention to prevent fractures. Arch Intern Med 164:1108–12
Cooper C, Atkinson EJ, O’Fallon WM, Melton LJ (1992) Incidence of clinically diagnosed vertebral fractures: a population-based study in Rochester, Minnesota, 1985–1989. J Bone Miner Res 7:221–7
Nevitt MC, Ross PD, Palermo L, Musliner T, Genant HK, Thompson DE (1999) Association of prevalent vertebral fractures, bone density, and alendronate treatment with incident vertebral fractures: effect of number and spinal location of fractures. Bone 25:613–9
Waterloo S, Ahmed LA, Center JR, Eisman JA, Morseth B, Nguyen ND, Nguyen T, Sogaard AJ, Emaus N (2012) Prevalence of vertebral fractures in women and men in the population-based Tromso Study. BMC Musculoskelet Disord 13:3–11
Fox KM, Cummings SR, Williams E, Stone K (2000) Femoral neck and intertrochanteric fractures have different risk factors: a prospective study. Osteoporos Int 11:1018–23
Partanen J, Jamsa T, Jalovaara P (2001) Influence of the upper femur and pelvic geometry on the risk and type of hip fractures. J Bone Miner Res 16:1540–6
Gonnelli S, Caffarelli C, Maggi S, Rossi S, Siviero P, Gandolini G, Cisari C, Rossini M, Iolascon G, Letizia Mauro G, Crepaldi G, Nuti R (2013) The assessment of vertebral fractures in elderly women with recent hip fractures: the BREAK Study. Osteoporos Int 24:1151–9
Greenspan SL, Myers ER, Maitland LA, Kido TH, Krasnow MB, Hayes WC (1994) Trochanteric bone mineral density is associated with type of hip fracture in the elderly. J Bone Miner Res 9:1889–94
Szulc P, Duboeuf F, Schott AM, Dargent-Molina P, Meunier PJ, Delmas PD (2006) Structural determinants of hip fracture in elderly women: a re-analysis of the data from the EPIDOS study. Osteoporos Int 17:231–6
Gallagher JC, Melton LJ, Riggs BL, Bergstrath E (1980) Epidemiology of fractures of the proximal femur in Rochester, Minnesota. Clin Orthop Relat Res 150:163–71
Lips P, Taconis WK, Van Ginkel FC, Netelenbos JC (1984) Radiologic morphometry in patients with femoral neck fractures and elderly control subjects: comparison with histomorphometric parameters. Clin Orthop 183:64–9
Vega E, Mautalen C, Gomez H, Garrido A, Melo L, Sahores AO (1991) Bone mineral density in patients with cervical and trochanteric fractures of the proximal femur. Osteoporos Int 1:81–6
Pulkkinen P, Gluer CC, Jamsa T (2011) Investigation of differences between hip fracture types: a worthy strategy for improved risk assessment and fracture prevention. Bone 49:600–4
Nakamura N, Kyou T, Takaoka K, Ohzono K, Ono K (1992) Bone mineral density in the proximal femur and hip fracture type in the elderly. J Bone Miner Res 7:755–9
Crilly RG, Cox L (2013) A comparison of bone density and bone morphology between patients presenting with hip fractures, spinal fractures or a combination of the two. BMC Musculoskelet Disord 14:68–76
Riggs BL, Wahner HW, Seeman E, Offord KP, Dunn WL, Mazess RB, Johnson KA, Melton LJ (1982) Changes in bone mineral density of the proximal femur and spine with aging: differnces between the postmenopausal and senile osteoporosis syndromes. J Clin Investig 70:716–23
Eastell R, Mosekile L, Hodgson SF, Riggs BL (1990) Proportion of human vertebral body bone that is cancellous. J Bone Miner Res 5:1237–41
Lotz JC, Hayes WC (1990) Estimates of hip fracture risk from falls using quantative computed tomography. J Bone Joint Surg 72:689–700
Cummings SR, Nevitt MC, for the Study of Osteoporotic Fractures Research Group (1994) Non-skeletal determinants of fractures: the potential importance of the mechanics of fall. Osteoporos Int 4:83–91
Hayes WC, Myers ER, Morris JN, Gerhart TN, Yett HS, Lipsitz LA (1993) Impact near the hip dominates fracture risk in elderly nursing home residents who fall. Calcif Tissue Int 52:192–8
Tanner DA, Kloseck M, Crilly RG, Chesworth B, Gilliland J (2010) Hip fracture types in men and women change differently with age. BMC Geriatr 10:12–15
Melton LJI, Chao EYS, Lane J (1988) Biomechanical aspects of fractures. In: Riggs BL, Melton LJI (eds) Osteoporosis: Etiology, Diagnosis and Management. Raven Press, New York, pp 111–131
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Watt, J., Cox, L. & Crilly, R.G. Distribution of vertebral fractures varies among patients according to hip fracture type. Osteoporos Int 26, 885–890 (2015). https://doi.org/10.1007/s00198-014-2887-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-014-2887-y