Abstract
Summary
Ibandronate reduces the risk of vertebral and non-vertebral fractures versus placebo in postmenopausal women with osteoporosis. This analysis, in which fractures were reported as safety events, showed that long-term use of ibandronate was associated with low fracture rates over 5 years of treatment.
Introduction
A previous post-hoc meta-analysis of 2–3 year studies found that ibandronate regimens with annual cumulative exposure (ACE) of ≥10.8 mg reduced the risk of vertebral and nonvertebral fractures (NVFs) versus placebo in postmenopausal women. This post-hoc analysis used individual patient data from the 2-year monthly oral ibandronate in ladies (MOBILE) and dosing intravenous administration (DIVA) studies, including the 3-year long-term extensions (LTEs), to assess fracture risk in patients treated with ibandronate for 5 years.
Methods
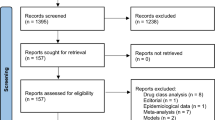
Patients treated for 2 years in MOBILE with monthly oral ibandronate 150 mg (n = 176) and in DIVA with IV ibandronate every 2 months 2 mg (n = 253) or quarterly 3 mg (n = 263) who continued on the same regimens for 3 additional years in the LTEs were included. Three-year placebo data (n = 1,924) were obtained from the ibandronate osteoporosis vertebral fracture trial in North America and Europe (BONE) and IV Fracture Prevention trials. The primary endpoint was clinical fracture rate; clinical fracture data were collected as adverse events. Time to fracture was analyzed using Kaplan–Meier and statistical analysis was conducted using the log-rank test. All clinical fractures included all NVFs and symptomatic vertebral fractures.
Results
For ibandronate regimens with ACE ≥10.8 mg, time to fracture was significantly longer for all clinical fractures, NVFs, and clinical vertebral fractures versus placebo (P = 0.005). For all fracture types, the rate of fracture appeared stable during the 5-year treatment period.
Conclusion
In women with postmenopausal osteoporosis, continuous treatment with ibandronate over 5 years results in low sustained clinical fracture rate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a chronic bone disease which leads to reduced bone mineral density (BMD), deterioration of bone microarchitecture, and increased susceptibility to fracture [1]. Vertebral and nonvertebral fractures (NVFs), as well as fractures of the hip, are associated with increased morbidity and mortality among postmenopausal women [2–4].
Bisphosphonates are the pharmacologic treatment of choice for osteoporosis, and were originally registered on the basis of requirements from licensing agencies, including the US Food and Drug Administration, to demonstrate that fracture data after 3 years of treatment show at least a trend (P < 0.2) toward decreased fracture incidence and no deterioration in the third year [5]. Daily treatment and, more recently, less-frequent dosing regimens (weekly, monthly, and quarterly) of those agents registered for daily treatment have been approved on the basis of “bridging” trials demonstrating improvements in BMD comparable to the approved daily regimens with proven anti-fracture efficacy [6–9]. The exception is annual intravenous zoledronic acid, which was approved on the basis of the same requirement as the daily formulations (3-year fracture risk reduction compared with placebo). Since the anti-fracture efficacy of zoledronic acid had not previously been tested, it was necessary to apply the same standards for registration as for the registration of the daily oral bisphosphonates.
Bridging registration trials are not fracture-endpoint trials but, rather, utilize surrogate markers of efficacy such as BMD and bone turnover markers, with the expectation that a non-inferior or equivalent increase in lumbar spine (LS) BMD seen between the fracture-proven daily formulations and the intermittent dosing formulations will translate into equal improvements in bone strength [8, 10–16]. Registration agencies accepted specific surrogate markers (non-inferior increases in BMD (primary endpoint) and non-inferior decreases in bone turnover markers (secondary endpoint) for approval of the intermittent bisphosphonate formulations if the daily formulation first had fracture endpoints.
Daily oral ibandronate 2.5 mg demonstrated reduced risk of vertebral fracture compared with placebo in the oral ibandronate osteoporosis vertebral fracture trial in North America and Europe (BONE) trial [17, 18]; however, the difference between daily ibandronate 2.5 mg and placebo in NVFs was not statistically significant. The marketed monthly oral ibandronate 150 mg and quarterly IV ibandronate 3 mg regimens provide an annual cumulative exposure (ACE; defined as annual dose × bioavailability (100 % for IV, 0.6 % for oral dosing) of approximately twice the daily oral 2.5-mg regimen. These regimens were approved on the basis of the 2-year monthly oral ibandronate in ladies (MOBILE) [19] and dosing intravenous administration (DIVA) [20] bridging trials. The DIVA and MOBILE trials were of similar study design and enrolled osteoporotic postmenopausal women with similar baseline characteristics [21]. In the MOBILE trial, monthly oral ibandronate 150 mg resulted in lumbar spine, total hip, femoral neck, and trochanter BMD increases that were superior to daily oral ibandronate 2.5 mg [19, 22]. The 2-year results from the DIVA study demonstrated that IV ibandronate 3 mg administered every 3 months (q3mo) significantly increased the BMD at the lumbar spine and total hip compared with daily oral ibandronate 2.5 mg [20, 23].
The antifracture efficacy of monthly oral and quarterly IV ibandronate have been examined in previous pooled meta-analyses using the 2-year data [21, 24]. These analyses found that high-ACE ibandronate regimens (ACE ≥10.8 mg), including monthly oral 150 mg and quarterly IV 3 mg, significantly reduced NVF, including hip fracture, compared with placebo and low-ACE ibandronate. Additionally, a retrospective database analysis found that monthly oral and quarterly IV ibandronate treatment was associated with a similar fracture rate to weekly oral bisphosphonate treatment (alendronate and risedronate) [25, 26].
Long-term extension (LTE) trials of both MOBILE [27, 28] and DIVA were conducted to examine the efficacy and safety of ibandronate treatment for an additional 3 years beyond the original 2-year trials. In the MOBILE LTE, patients previously treated with monthly oral ibandronate 100 or 150 mg during MOBILE continued to receive the same regimens. Patients who had received daily oral ibandronate 2.5 mg or monthly 50 + 50 mg (two doses of 50 mg over 2 consecutive days) during MOBILE were reallocated to either the 100 mg or the 150 mg study regimen [28]. After 5 years, monthly oral ibandronate 100 and 150 mg resulted in continued increases in lumbar spine BMD [27]. In the DIVA LTE, patients who previously received IV ibandronate 2 mg every 2 months (q2mo) or 3 mg quarterly were maintained on these same regimens for an additional 3 years. Patients who had received daily oral ibandronate 2.5 mg were reallocated to either the q2mo IV 2-mg or the quarterly IV 3-mg study regimen.
This post-hoc analysis evaluated fracture data from patients who received monthly oral ibandronate 150 mg, q2mo IV ibandronate 2 mg, and quarterly IV ibandronate 3 mg continuously throughout the 5 years of the DIVA and MOBILE core and LTE studies, using the similar methodology to the previous meta-analysis of Harris et al. [21]. The placebo group for comparison of fracture rates was derived from different randomized trials: BONE [29] and the IV Fracture Prevention Trial [17].
Methods
Study design
This was a post-hoc pooled analysis of fracture rates seen with 5 years of treatment with ibandronate using individual patient data from randomized clinical trials of ibandronate. Ibandronate data from MOBILE, DIVA, and their respective LTE trials (MOBILE LTE and DIVA LTE) were included. These are the only randomized controlled trials providing up to 5 years of ibandronate treatment follow-up.
Active treatment data were included in this analysis from patients in the safety populations of MOBILE (and the MOBILE LTE) and DIVA (and the DIVA LTE) who received continuous treatment with ibandronate regimens providing ACE ≥10.8 mg (monthly oral 150 mg, q2mo IV 2 mg, or quarterly IV 3 mg) for 5 years. Patients were included in the analysis if they received ≥1 dose in both the core 2-year trial and the corresponding LTE study and had ≥1 post-baseline safety evaluation. Patients from the following groups in the MOBILE and DIVA trials were not included in this analysis: patients who received daily oral ibandronate 2.5 mg, since they were switched to monthly oral ibandronate 100 or 150 mg, or q2mo IV ibandronate 2 mg, or quarterly IV ibandronate 3 mg in the MOBILE and DIVA LTEs and therefore did not receive a single regimen for 5 years of follow-up; and patients who received monthly oral 100 mg, since this regimen provides a lower dose (ACE 7.2 mg) than the marketed regimens (ACE 10.8–12 mg), and did not provide statistically significant fracture protection compared with placebo in the analysis of Harris et al. [21]. No spine radiographs were obtained routinely in the MOBILE and DIVA extension studies; therefore, morphometric VFA was not assessed.
MOBILE and DIVA were active-controlled trials. The 3-year placebo data (n = 1,924) from the BONE [17] and IV Fracture Prevention [29] randomized controlled trials were used for comparison. This method is consistent with the method previously described by Harris et al. [25].
Patients
All four studies (MOBILE LTE, DIVA LTE, BONE, IV Fracture Prevention study) used similar inclusion and exclusion criteria, including postmenopausal women aged 55–80 years. Women included in MOBILE and DIVA had LS BMD T-score of −2.5 to −5.0; these studies did not require participants to have a prevalent vertebral fracture. Women included in BONE and the IV Fracture Prevention study had 1–4 prevalent vertebral fractures, and LS BMD T-score −2.0 to −5.0. Participants in all four studies received daily supplementation with 400 IU vitamin D and 500 mg calcium.
Fracture data were collected as adverse events, with mandatory X-ray confirmation. NVF confirmation was carried out locally in all four studies. Vertebral fracture confirmation was carried out locally in MOBILE and DIVA, and centrally in BONE and the IV fracture prevention trial.
Statistical analyses
The primary outcome measure in this analysis was fracture rate, which was analyzed according to treatment received throughout the 5 years. All clinical fractures were radiologically confirmed and included all NVFs (excluding fractures of the skull, fingers, and toes since these are not generally considered osteoporotic) and symptomatic vertebral fractures. Fracture rates were calculated as the proportion of patients with ≥1 fracture over 5 years’ treatment and analyzed by fracture type (all clinical fractures, clinical vertebral fractures, osteoporotic NVFs, and key osteoporotic NVFs) and treatment group. Key osteoporotic NVFs were defined as those of the clavicle, humerus, wrist, hip, pelvis, and leg.
Time to fracture (number of days from day 1 to the date of onset of the first fracture event) was analyzed using Kaplan–Meier analysis. Data from the monthly oral 150 mg, q2mo IV 2 mg, and quarterly IV 3 mg arms were combined for Kaplan–Meier analysis and analyzed as a single high-ACE group (ACE ≥10.8 mg) (Table 1). Time to first all clinical fracture was also analyzed separately for the monthly oral ibandronate 150 mg and IV ibandronate (q2mo 2 mg and quarterly 3 mg; ACE 12 mg) groups. The log-rank test was used to evaluate statistical differences between the active treatment group and placebo. Fracture rate per 100 patient-years was calculated as 100 x (total number of fracture events/total patient-years of treatment). All statistical analyses were conducted using the SAS® software package version 8.2 (SAS Institute, Cary, NC, USA).
Results
A total of 692 patients who received continuous treatment for 5 years with either oral (monthly 150 mg) or IV (q2mo 2 mg or quarterly 3 mg) ibandronate were included in this analysis. Baseline patient characteristics were similar across all treatment arms and placebo (Table 2). Average age was slightly higher in the placebo group.
The rate of all clinical fractures was comparable with all ibandronate treatments in MOBILE LTE and DIVA LTE and for the pooled high-dose ACE group (Table 3). Similar results were also obtained for NVFs, key NVFs, and all clinical fractures per 100 patient-years. A lower rate of vertebral fractures was observed in the monthly oral 150 mg group than the IV treatment groups (1.70 % compared with 5.53 % and 5.32 % for the IV q2mo 2 mg and quarterly 3 mg groups, respectively; Table 3). The Kaplan–Meier analysis found that time to fracture for all clinical fractures (Fig. 1), NVFs (Fig. 2), and clinical vertebral fractures (Fig. 3) were all significantly longer with ibandronate treatments with ACE ≥ 10.8 mg compared with placebo (P = 0.001, P = 0.036, and P = 0.003, respectively). Time to fracture for key NVFs was longer with ibandronate than placebo treatment, but the difference was not statistically significant (P = 0.073, Fig. 4). For all clinical fractures, the time to first fracture was significantly longer compared with placebo for monthly oral ibandronate 150 mg (P = 0.0174) and IV ibandronate (q2mo 2 mg and quarterly 3 mg, ACE 12 mg, P = 0.002). For all fracture types, the rate of fractures appeared stable throughout the 5-year follow-up.
Discussion
This post-hoc pooled analysis of 5-year fracture data found that time to fracture for clinical fractures, NVFs, and clinical vertebral fractures was significantly longer for women with postmenopausal osteoporosis treated with monthly oral or IV ibandronate with ACE ≥10.8 mg compared with those receiving placebo, though the placebo rates were derived from two different ibandronate trials. The doses of ibandronate regimens that showed this outcome include the marketed monthly oral 150 mg and quarterly IV 3 mg regimens. These data suggest that ibandronate provides long-term anti-fracture benefit to women with postmenopausal osteoporosis, with a similar rate of fractures sustained throughout up to 5 years of treatment.
Our results are consistent with those previously reported in two recent meta-analyses of individual patient data, which assessed fracture risk reduction with ibandronate using pooled individual patient data from ibandronate clinical trials, and showed that higher ACE regimens are associated with greater NVF risk reduction [21, 30]. The analysis by Cranney et al. pooled data from the DIVA and MOBILE studies and reported that ibandronate ACE ≥10.8 mg significantly reduced the risk of NVF compared with ACE = 5.5 mg (HR 0.62 (95 % CI 0.396-0.974), P = 0.038) [31]. Harris et al. [21] pooled data from the BONE, IV fracture prevention study, DIVA, and MOBILE studies to assess fracture risk over 2–3 years and found that ibandronate ACE ≥10.8 mg was associated with significantly reduced relative risk of NVFs (29.9 %, P = 0.04), clinical fractures (28.8 %, P = 0.010) and key NVFs (34.4 %, P = 0.032) compared with placebo. Additionally, time to fracture was significantly longer for all clinical fractures, NVFs, and key NVFs. Differences between the mid-ACE group (ACE 5.5–7.2 mg) and placebo were not statistically significant.
At this time, the optimal duration of bisphosphonate treatment is not known [32]. The long-term safety and effects on BMD of daily bisphosphonates have been examined and three recent review articles have detailed the benefit/risk ratio of bisphosphonate use and agree with the recent Food and Drug Administration (FDA) suggestion that lower risk patients could be given a “drug-holiday” after 3–5 years of use, but that high-risk patients have a benefit that outweighs any risks with longer duration of therapy [33–38]. The majority of clinical trials examining the vertebral fracture and NVF efficacy of the approved bisphosphonates (alendronate, risedronate, ibandronate, and zoledronic acid) where a placebo arm has been retained have been 3 to 4 years in duration [17, 39–43], and few studies have examined the long-term benefits of bisphosphonate therapy with respect to fracture risk reduction [44]. The FDA stated that scientific evidence for the long-term (beyond 5 years) efficacy data for bisphosphonates does not exist [38]. While the FDA statement is accurate, the reality is that true scientific evidence that requires the maintenance of a placebo group will never be achieved in bisphosphonate clinical trials due to the unethical nature of maintaining a placebo arm in higher risk patients. Hence, longer term efficacy data compares either incident rates of fracture to the original 3-year placebo arm, or incident rates in the treatment arms (annualized) to the original treatment arm incident rates for the registration trials.
Long-term studies of daily alendronate and daily risedronate have provided data ranging in duration from 5–10 years. An extension trial of the 3-year Vertebral Efficacy with Risedronate Therapy (VERT) multinational study found that daily risedronate (5 mg) significantly reduced the risk of new vertebral fractures (59 %, P < 0.01) over 2 additional years compared with placebo [44]. However, NVF risk was not significantly reduced compared with placebo, possibly reflecting the small number of NVFs in this study. A study by Bone et al. found that 10 years of oral daily alendronate therapy resulted in improved or sustained BMD at all skeletal sites and long-term stabilization of BTMs, but this study did not evaluate fracture risk reduction [33]. The Fracture Intervention Trial Long-term Extension (FLEX) examined the impact of discontinuing alendronate therapy after 5 years of continuous therapy versus remaining on therapy for an additional 5 years [45]. Women who discontinued alendronate therapy for 5 years after 5 years of continuous therapy experienced gradual decreases in the LS and total hip BMD and increases in BTMs. While women off alendronate had a significant increase in clinical vertebral fractures if their BMD T-score at the femoral neck was −2.5 or lower; the remaining lower risk women had no differences in fracture rates to the women who continued on alendronate for 10 years. [45, 46]. In a separate post-hoc analysis of the FLEX trial, only those women who had a FN T-score ≤2.5 and no prevalent vertebral compression fracture appeared to have an increased risk of NVF while remaining off alendronate [46]. Thus, consistent with the FDA position, high-risk patients benefit from long-term therapy.
A number of case series has reported atypical subtrochanteric femur fractures in patients receiving long-term alendronate treatment [47–51]; these associations have been reported with longer duration of bisphosphonate use [52, 53], and have contributed to concerns about the potential for long-term bisphosphonate treatment. The American Society for Bone and Mineral Research (ASBMR) has published their working group analysis of the data regarding these atypical subtrochanteric femur fractures [54] and concluded that, while there appears to be an association between long-term bisphosphonate use and these rare events, no causality has been established. No atypical fractures were reported, though assessment of these fractures was not pre-planned in the bisphosphonates trials, but it is reassuring to note that no apparent increase in fracture rate was observed in the later years of ibandronate treatment in our analysis, which used placebo groups from different randomized trials for comparison of fracture rates. Furthermore, no significant differences between groups were observed in the MOBILE and DIVA LTEs in treatment-related AEs, serious AEs, or life-threatening AEs [27, 28].
Limitations
The findings of our analysis need to be considered in the light of several limitations. This was a post-hoc pooled meta-analysis, not a randomized prospective clinical trial. However, the analysis does use individual patient data, which may be preferable to the use of summary data [55, 56]. The studies pooled in this analysis had generally similar study designs and patient populations, and the analysis was adjusted for differences in baseline characteristics; however, it is possible that unmeasured or uncontrolled differences between groups or residual confounding could have resulted in bias in our findings. P values were not adjusted for multiple comparisons, and since MOBILE and DIVA were not placebo-controlled clinical trials, the placebo data used in this analysis were derived from the 3-year BONE and IV fracture trials.
Fractures were not an endpoint in MOBILE and DIVA; however, clinical fractures and NVFs were collected as AEs across all the trials, and X-ray confirmation was required. Findings in the populations included in randomized clinical trials may not be generalizable to the general population with osteoporosis.
Conclusions
This pooled analysis of data from the MOBILE and DIVA trials showed that continued treatment with oral or IV ibandronate, in women previously treated for 2 years, provided long-term clinical benefit as demonstrated by significantly longer time to fracture for all clinical fractures, NVFs, and clinical vertebral fractures compared with placebo over 5 years of treatment. Ibandronate formulations that provide higher ACE (the 150 mg/month oral or the 3 mg every 3 months IV) appear to provide a long-term benefit on both vertebral as well as nonvertebral fractures. These results appear to support those of previous studies that showed improvements in BMD and bone turnover with the same ibandronate regimens used here.
References
McClung MR (2000) Bisphosphonates in osteoporosis: recent clinical experience. Expert Opin Pharmacother 1:225–238
Bliuc D, Nguyen ND, Milch VE, Nguyen TV, Eisman JA, Center JR (2009) Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA 301:513–521
Ioannidis G, Papaioannou A, Hopman WM, Akhtar-Danesh N, Anastassiades T, Pickard L, Kennedy CC, Prior JC, Olszynski WP, Davison KS, Goltzman D, Thabane L, Gafni A, Papadimitropoulos EA, Brown JP, Josse RG, Hanley DA, Adachi JD (2009) Relation between fractures and mortality: results from the Canadian Multicentre Osteoporosis Study. Cmaj 181:265–271
Sweet MG, Sweet JM, Jeremiah MP, Galazka SS (2009) Diagnosis and treatment of osteoporosis. Am Fam Physician 79:193–200
US Food and Drug Administration (1994) Guidelines for preclinical and clinical evaluation of agents used in the prevention or treatment of postmenopausal osteoporosis, Silver Spring
Boonen S, Orwoll ES, Wenderoth D, Stoner KJ, Eusebio R, Delmas PD (2009) Once-weekly risedronate in men with osteoporosis: results of a 2-year, placebo-controlled, double-blind, multicenter study. J Bone Miner Res 24:719–725
Delmas PD, McClung MR, Zanchetta JR, Racewicz A, Roux C, Benhamou CL, Man Z, Eusebio RA, Beary JF, Burgio DE, Matzkin E, Boonen S (2008) Efficacy and safety of risedronate 150 mg once a month in the treatment of postmenopausal osteoporosis. Bone 42:36–42
Schnitzer T, Bone HG, Crepaldi G, Adami S, McClung M, Kiel D, Felsenberg D, Recker RR, Tonino RP, Roux C, Pinchera A, Foldes AJ, Greenspan SL, Levine MA, Emkey R, Santora AC 2nd, Kaur A, Thompson DE, Yates J, Orloff JJ (2000) Therapeutic equivalence of alendronate 70 mg once-weekly and alendronate 10 mg daily in the treatment of osteoporosis. Alendronate Once-Weekly Study Group. Aging (Milano) 12:1–12
Eisman JA, Garcia-Hernandez PA, Ortiz-Luna G, Ste-Marie LG, Hughes C, Mairon N, Masanauskaite D, Delmas PD (2006) Intermittent intravenous ibandronate injections are an effective treatment option in postmenopausal osteoporosis: 2-year results from DIVA [abstract P316SA]. Osteoporos Int 17:S212
Bonnick SL, Shulman L (2006) Monitoring osteoporosis therapy: bone mineral density, bone turnover markers, or both? Am J Med 119:S25–S31
Hochberg MC, Greenspan S, Wasnich RD, Miller P, Thompson DE, Ross PD (2002) Changes in bone density and turnover explain the reductions in incidence of nonvertebral fractures that occur during treatment with antiresorptive agents. J Clin Endocrinol Metab 87:1586–1592
Miller PD (2005) Bone density and markers of bone turnover in predicting fracture risk and how changes in these measures predict fracture risk reduction. Curr Osteoporos Rep 3:103–110
Miller PD (2007) Monitoring osteoporosis therapies. Curr Osteoporos Rep 5:38–43
Miller PD, Zapalowski C, Kulak CA, Bilezikian JP (1999) Bone densitometry: the best way to detect osteoporosis and to monitor therapy. J Clin Endocrinol Metab 84:1867–1871
Wasnich RD, Miller PD (2000) Antifracture efficacy of antiresorptive agents are related to changes in bone density. J Clin Endocrinol Metab 85:231–236
Miller PD (2012) Bone strength and surrogate markers: the first, second, and third fiddle. J Bone Miner Res 27:1623–1626
Chesnut CH, Ettinger MP, Miller PD, Baylink DJ, Emkey R, Harris ST, Wasnich RD, Watts NB, Schimmer RC, Recker RR (2005) Ibandronate produces significant, similar antifracture efficacy in North American and European women: new clinical findings from BONE. Curr Med Res Opin 21:391–401
Chesnut CH, Skag A, Christiansen C, Recker R, Stakkestad JA, Hoiseth A, Felsenberg D, Huss H, Gilbride J, Schimmer RC, Delmas PD (2004) Effects of oral ibandronate administered daily or intermittently on fracture risk in postmenopausal osteoporosis. J Bone Miner Res 19:1241–1249
Reginster JY, Adami S, Lakatos P, Greenwald M, Stepan JJ, Silverman SL, Christiansen C, Rowell L, Mairon N, Bonvoisin B, Drezner MK, Emkey R, Felsenberg D, Cooper C, Delmas PD, Miller PD (2006) Efficacy and tolerability of once-monthly oral ibandronate in postmenopausal osteoporosis: 2 year results from the MOBILE study. Ann Rheum Dis 65:654–661
Eisman JA, Civitelli R, Adami S, Czerwinski E, Recknor C, Prince R, Reginster JY, Zaidi M, Felsenberg D, Hughes C, Mairon N, Masanauskaite D, Reid DM, Delmas PD, Recker RR (2008) Efficacy and tolerability of intravenous ibandronate injections in postmenopausal osteoporosis: 2-year results from the DIVA study. J Rheumatol 35:488–497
Harris ST, Blumentals WA, Miller PD (2008) Ibandronate and the risk of non-vertebral and clinical fractures in women with postmenopausal osteoporosis: results of a meta-analysis of phase III studies. Curr Med Res Opin 24:237–245
Miller PD, McClung MR, Macovei L, Stakkestad JA, Luckey M, Bonvoisin B, Reginster JY, Recker RR, Hughes C, Lewiecki EM, Felsenberg D, Delmas PD, Kendler DL, Bolognese MA, Mairon N, Cooper C (2005) Monthly oral ibandronate therapy in postmenopausal osteoporosis: 1-year results from the MOBILE study. J Bone Miner Res 20:1315–1322
Delmas PD, Adami S, Strugala C, Stakkestad JA, Reginster JY, Felsenberg D, Christiansen C, Civitelli R, Drezner MK, Recker RR, Bolognese M, Hughes C, Masanauskaite D, Ward P, Sambrook P, Reid DM (2006) Intravenous ibandronate injections in postmenopausal women with osteoporosis: one-year results from the dosing intravenous administration study. Arthritis Rheum 54:1838–1846
Cranney A, Wells G, Adachi R (2007) Non-vertebral fracture reduction with high- versus low-dose ibandronate: a meta-analysis of individual patient data. Ann Rheum Dis 66:681
Harris ST, Reginster JY, Harley C, Blumentals WA, Poston SA, Barr CE, Silverman SL (2009) Risk of fracture in women treated with monthly oral ibandronate or weekly bisphosphonates: the eValuation of IBandronate Efficacy (VIBE) database fracture study. Bone 44:758–765
Silverman SL (2010) Osteoporosis therapies: evidence from health-care databases and observational population studies. Calcif Tissue Int 87:375–384
Miller PD, Recker RR, Felsenberg D, Reginster JY, Riis BJ, Czerwinski E, Lorenc RS, Stakkestad JA, Dasic G, Barr CE, Lakatos P (2009) 5-year efficacy and safety of monthly oral ibandronate: results of the MOBILE long-term extension study. Osteoporos Int 20:S191–S229
Stakkestad JA, Lakatos P, Lorenc R, Sedarati F, Neate C, Reginster JY (2008) Monthly oral ibandronate is effective and well tolerated after 3 years: the MOBILE long-term extension. Clin Rheumatol 27:955–960
Recker R, Stakkestad JA, Chesnut CH 3rd, Christiansen C, Skag A, Hoiseth A, Ettinger M, Mahoney P, Schimmer RC, Delmas PD (2004) Insufficiently dosed intravenous ibandronate injections are associated with suboptimal antifracture efficacy in postmenopausal osteoporosis. Bone 34:890–899
Cranney A, Tugwell P, Adachi J, Weaver B, Zytaruk N, Papaioannou A, Robinson V, Shea B, Wells G, Guyatt G (2002) Meta-analyses of therapies for postmenopausal osteoporosis. III. Meta-analysis of risedronate for the treatment of postmenopausal osteoporosis. Endocr Rev 23:517–523
Cranney A, Wells GA, Yetisir E, Adami S, Cooper C, Delmas PD, Miller PD, Papapoulos S, Reginster JY, Sambrook PN, Silverman S, Siris E, Adachi JD (2009) Ibandronate for the prevention of nonvertebral fractures: a pooled analysis of individual patient data. Osteoporos Int 20:291–297
National Osteoporosis Foundation (2008) Clinician's guide to prevention and treatment of osteoporosis. Washington, 1–37
Bone HG, Hosking D, Devogelaer JP, Tucci JR, Emkey RD, Tonino RP, Rodriguez-Portales JA, Downs RW, Gupta J, Santora AC, Liberman UA (2004) Ten years' experience with alendronate for osteoporosis in postmenopausal women. N Engl J Med 350:1189–1199
Devogelaer JP, Brown JP, Burckhardt P, Meunier PJ, Goemaere S, Lippuner K, Body JJ, Samsioe G, Felsenberg D, Fashola T, Sanna L, Ortmann CE, Trechsel U, Krasnow J, Eriksen EF, Garnero P (2007) Zoledronic acid efficacy and safety over five years in postmenopausal osteoporosis. Osteoporos Int 18:1211–1218
Boonen S, Ferrari S, Miller PD, Eriksen EF, Sambrook PN, Compston J, Reid IR, Vanderschueren D, Cosman F (2012) Postmenopausal osteoporosis treatment with antiresorptives: effects of discontinuation or long-term continuation on bone turnover and fracture risk–a perspective. J Bone Miner Res 27:963–974
Khosla S, Bilezikian JP, Dempster DW, Lewiecki EM, Miller PD, Neer RM, Recker RR, Shane E, Shoback D, Potts JT (2012) Benefits and risks of bisphosphonate therapy for osteoporosis. J Clin Endocrinol Metab 97:2272–2282
McClung M, Harris ST, Miller PD, Bauer DC, Davison KS, Dian L, Hanley DA, Kendler DL, Yuen CK, Lewiecki EM (2013) Bisphosphonate therapy for osteoporosis: benefits, risks, and drug holiday. Am J Med 126:13–20
Whitaker M, Guo J, Kehoe T, Benson G (2012) Bisphosphonates for osteoporosis–where do we go from here? N Engl J Med 366:2048–2051
Reginster J, Minne HW, Sorensen OH, Hooper M, Roux C, Brandi ML, Lund B, Ethgen D, Pack S, Roumagnac I, Eastell R (2000) Randomized trial of the effects of risedronate on vertebral fractures in women with established postmenopausal osteoporosis. Vertebral Efficacy with Risedronate Therapy (VERT) Study Group. Osteoporos Int 11:83–91
Black DM, Delmas PD, Eastell R, Reid IR, Boonen S, Cauley JA, Cosman F, Lakatos P, Leung PC, Man Z, Mautalen C, Mesenbrink P, Hu H, Caminis J, Tong K, Rosario-Jansen T, Krasnow J, Hue TF, Sellmeyer D, Eriksen EF, Cummings SR (2007) Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N Engl J Med 356:1809–1822
Cummings SR, Black DM, Thompson DE, Applegate WB, Barrett-Connor E, Musliner TA, Palermo L, Prineas R, Rubin SM, Scott JC, Vogt T, Wallace R, Yates AJ, LaCroix AZ (1998) Effect of alendronate on risk of fracture in women with low bone density but without vertebral fractures: results from the Fracture Intervention Trial. JAMA 280:2077–2082
McClung MR, Geusens P, Miller PD, Zippel H, Bensen WG, Roux C, Adami S, Fogelman I, Diamond T, Eastell R, Meunier PJ, Reginster JY (2001) Effect of risedronate on the risk of hip fracture in elderly women. Hip Intervention Program Study Group. N Engl J Med 344:333–340
Black DM, Reid IR, Boonen S, Bucci-Rechtweg C, Cauley JA, Cosman F, Cummings SR, Hue TF, Lippuner K, Lakatos P, Leung PC, Man Z, Martinez RL, Tan M, Ruzycky ME, Su G, Eastell R (2012) The effect of 3 versus 6 years of zoledronic acid treatment of osteoporosis: a randomized extension to the HORIZON-Pivotal Fracture Trial (PFT). J Bone Miner Res 27:243–254
Sorensen OH, Crawford GM, Mulder H, Hosking DJ, Gennari C, Mellstrom D, Pack S, Wenderoth D, Cooper C, Reginster JY (2003) Long-term efficacy of risedronate: a 5-year placebo-controlled clinical experience. Bone 32:120–126
Black DM, Schwartz AV, Ensrud KE, Cauley JA, Levis S, Quandt SA, Satterfield S, Wallace RB, Bauer DC, Palermo L, Wehren LE, Lombardi A, Santora AC, Cummings SR (2006) Effects of continuing or stopping alendronate after 5 years of treatment: the Fracture Intervention Trial Long-term Extension (FLEX): a randomized trial. JAMA 296:2927–2938
Schwartz AV, Bauer DC, Cummings SR, Cauley JA, Ensrud KE, Palermo L, Wallace RB, Hochberg MC, Feldstein AC, Lombardi A, Black DM (2010) Efficacy of continued alendronate for fractures in women with and without prevalent vertebral fracture: the FLEX trial. J Bone Miner Res 25:976–982
Kwek EB, Koh JS, Howe TS (2008) More on atypical fractures of the femoral diaphysis. N Engl J Med 359:316–317, author reply 317–318
Lee P, Seibel MJ (2008) More on atypical fractures of the femoral diaphysis. N Engl J Med 359:317, author reply 317–318
Lenart BA, Lorich DG, Lane JM (2008) Atypical fractures of the femoral diaphysis in postmenopausal women taking alendronate. N Engl J Med 358:1304–1306
Odvina CV, Zerwekh JE, Rao DS, Maalouf N, Gottschalk FA, Pak CY (2005) Severely suppressed bone turnover: a potential complication of alendronate therapy. J Clin Endocrinol Metab 90:1294–1301
Visekruna M, Wilson D, McKiernan FE (2008) Severely suppressed bone turnover and atypical skeletal fragility. J Clin Endocrinol Metab 93:2948–2952
Dell RM, Adams AL, Greene DF, Funahashi TT, Silverman SL, Eisemon EO, Zhou H, Burchette RJ, Ott SM (2012) Incidence of atypical nontraumatic diaphyseal fractures of the femur. J Bone Miner Res 27:2544–2550
Schilcher J, Koeppen V, Ranstam J, Skripitz R, Michaelsson K, Aspenberg P (2013) Atypical femoral fractures are a separate entity, characterized by highly specific radiographic features. A comparison of 59 cases and 218 controls. Bone 52:389–392
Shane E, Burr D, Ebeling PR, Abrahamsen B, Adler RA, Brown TD, Cheung AM, Cosman F, Curtis JR, Dell R, Dempster D, Einhorn TA, Genant HK, Geusens P, Klaushofer K, Koval K, Lane JM, McKiernan F, McKinney R, Ng A, Nieves J, O'Keefe R, Papapoulos S, Sen HT, van der Meulen MC, Weinstein RS, Whyte M (2010) Atypical subtrochanteric and diaphyseal femoral fractures: report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res 25:2267–2294
Berlin JA, Santanna J, Schmid CH, Szczech LA, Feldman HI (2002) Individual patient- versus group-level data meta-regressions for the investigation of treatment effect modifiers: ecological bias rears its ugly head. Stat Med 21:371–387
Li Z, Meredith MP (2003) Exploring the relationship between surrogates and clinical outcomes: analysis of individual patient data vs. meta-regression on group-level summary statistics. J Biopharm Stat 13:777–792
Acknowledgments
This study was funded by Genentech and GlaxoSmithKline. Medical writing assistance was provided by Gill Sperrin CBiol MSB CMPP and Andrew Cooper PhD CMPP of Envision Scientific Solutions and funded by Genentech and GlaxoSmithKline. The authors received no financial support for this work and had complete control of the data.
Conflicts of interest
Dr Miller’s institution has received payment for consultancy from Amgen, Merck & Lilly, expert testimony from Novartis, and grants from Amgen, Merck & Lilly. Dr. Robert R. Recker is a paid consultant for Merck, Lilly, Wyeth, Procter and Gamble, Amgen, Roche, GlaxoSmithKline, Novartis, and NPS Allelix and has received grant/research support from Merck, Lilly, Wyeth, Procter and Gamble, Amgen, Roche, GlaxoSmithKline, Novartis, NPS Allelix, and Sanofi‐Aventis through grants to his institution. Dr. Jean‐Yves Reginster is a paid consultant for/has received payment for advisory boards from Servier, Novartis, Negma, Lilly, Wyeth, Amgen, GlaxoSmithKline, Roche, Merckle, Nycomed, NPS, Theramex, and UCB. He has received lecture fees when speaking at the invitation of a commercial sponsor for Merck Sharp and Dohme, Lilly, Rottapharm, IBSA, Genevrier, Novartis, Servier, Roche, GlaxoSmithKline, Teijin, Teva, Ebewee Pharma, Zodiac, Analis, Theramex, Nycomed, and Novo‐Nordisk. He has also received grant support from Bristol Myers Squibb, Merck Sharp & Dohme, Rottapharm, Teva, Lilly, Novartis, Roche, GlaxoSmithKline, Amgen, and Servier. Dr Harris has served as a Board member for Eli Lilly & Company, Merck; received consultancy fees from Amgen, Eli Lilly & Company, Merck, and Roche; has served as an expert advisor for Roche; and has received honoraria for Speakers Bureax from Amgen, Eli Lilly & Company, Genentech, GlaxoSmithKline, Procter & Gamble, Roche, Novartis, Warner Chilcott. De Silverman has received consultancy fees from The Alliance for Better Bone Health (Procter & Gamble Pharmaceuticals and Sanofi Aventis). Dr Felsenberg has received consulting fees or paid advisory board fees from Amgen, Chugai, GlaxoSmithKline, Lilly, MSD, Novartis, Nycomed, Roche, Servier, and TEVA; lecture fees from Amgen, Chugai, GE, GlaxoSmithKline, Lilly, MSD, Novartis, Nycomed, Roche, Servier, Teva, and WC; and grant support from Amgen, Chugai, Lilly, MSD, Novartis, Nycomed, Roche, Teva, Servier. Drs Bann‐Mo Day and Charles Barr are full‐time employees of Genentech. Dr. Daiva Masanauskaite is a full‐time employee of F. Hoffmann-La Roche.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Miller, P.D., Recker, R.R., Harris, S. et al. Long-term fracture rates seen with continued ibandronate treatment: pooled analysis of DIVA and MOBILE long-term extension studies. Osteoporos Int 25, 349–357 (2014). https://doi.org/10.1007/s00198-013-2518-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-013-2518-z