Abstract
Summary
This analysis was conducted to assess the effect of high versus lower doses of ibandronate on nonvertebral fractures. The results were adjusted for clinical fracture, age, and bone density. The treatment effect was dose-dependent. Higher doses of ibandronate significantly reduced the risk of nonvertebral fractures more effectively compared with lower doses.
Introduction
The objective of this study was to assess the efficacy of different doses of ibandronate on nonvertebral fractures in a pooled analysis.
Methods
Eight randomized trials of ibandronate were reviewed for inclusion. Alternative definitions of high versus low doses based on annual cumulative exposure (ACE) were explored. A time-to-event analysis was conducted using Kaplan–Meier methodology. Hazard ratios (HR) were derived using Cox regression and adjusted for covariates.
Results
Combining higher ACE doses of ≥ 10.8 mg (150 mg once monthly, 3 mg i.v. quarterly, and 2 mg i.v. every 2 months) versus ACE doses of 5.5 mg, from two trials, resulted in an HR 0.62 (95% CI 0.396–0.974, p = 0.038). There was a dose–response trend with increasing ACE doses (7.2–12 mg) versus ACE of 5.5 mg.
Conclusions
A dose–response effect on nonvertebral fractures was observed when comparing high with low ACE doses. A significant reduction in nonvertebral fractures was noted when pooling data from trials using ACE doses of ≥ 10.8 mg versus ACE ≤ 7.2 mg; and with ACE ≥ 10.8 mg versus ACE of 5.5 mg (38% reduction). Higher ibandronate dose levels (150 mg monthly or 3 mg i.v. quarterly) significantly reduced nonvertebral fracture risk in postmenopausal women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ibandronate is a potent nitrogen-containing bisphosphonate that has been approved for the treatment of postmenopausal osteoporosis in a number of countries. The higher potency of ibandronate relative to other bisphosphonates allows for less frequent dosing intervals such as once monthly and quarterly intravenous administration, with continued clinical efficacy in postmenopausal osteoporosis. Eight randomized treatment trials of ibandronate in women with postmenopausal osteoporosis were reviewed [1–8]. Of these, two large placebo-controlled randomized trials evaluated the effect of either daily or intermittent oral and intravenous ibandronate on vertebral fractures [1, 2]. A 3-year double-blind multicenter trial in 2,946 postmenopausal women (aged 55–80 years with prevalent fractures) evaluated the efficacy of 2.5 mg of ibandronate given daily (annual cumulative exposure, ACE, 5.5 mg), and intermittently (20 mg given q 2 days for 12 doses every 3 months = ACE 5.8 mg) compared with placebo on new morphometric vertebral fractures [1, 9]. The mean age of participants was 69 years, the mean lumbar spine BMD T-score was −2.8 and the mean total hip BMD T-score was −1.7. Compared with placebo, ibandronate 2.5 mg daily resulted in a significant reduction in both radiographic vertebral fractures and clinical vertebral fractures. The primary outcome was vertebral fractures and this trial was not designed to assess the efficacy of ibandronate on nonvertebral fractures. There was no reduction in nonvertebral fractures observed with 2.5 mg of ibandronate daily, except in a post hoc analysis of women at higher risk of fracture, based on a femoral neck BMD T-score of −3.0. In an earlier, similarly designed, 3-year trial of 2,962 postmenopausal women, Recker et al. evaluated the fracture efficacy of two intravenous doses of ibandronate 0.5 mg (= ACE 2 mg) and 1.0 mg (= ACE 4 mg) given quarterly compared with placebo. In this trial there was no significant difference in incident vertebral fractures in the ibandronate arms (8.7%, 9.2%) compared with the controls (10.7%), and there was no effect on nonvertebral fractures, although there was a significant difference in incident vertebral fractures with ibandronate in the per protocol analysis [2]. Only a modest suppression of bone resorption was seen with these doses, suggesting that perhaps a higher dose of intravenous ibandronate relative to a longer dose-free interval of 3 months was required for fracture reduction. The effects of higher doses of ibandronate were investigated in two non-inferiority trials with similar eligibility criteria that used higher ACE doses for extended dose-free intervals [3, 4, 10]. The first trial compared 2 mg intravenously (i.v.) every 2 months (ACE 12 mg) or 3 mg i.v. given quarterly (ACE 12 mg) with an active control (oral daily 2.5 mg ibandronate, ACE 5.5 mg) [4]. The second non-inferiority trial compared monthly ibandronate 100 mg orally (ACE 7.2 mg) or 150 mg orally (ACE 10.8 mg) with 2.5 mg daily [3, 10]. All intravenous and oral monthly regimens proved to be non-inferior to 2.5 mg daily in terms of BMD and markers of bone turnover. In addition, the two intravenous and 150-mg oral dose regimens were superior to the 2.5-mg daily dose based on lumbar spine BMD [3, 4]. Clinical fracture data, including nonvertebral fractures were collected in both of these trials. The eligibility criteria of participants in the placebo-controlled fracture trials were similar to eligibility criteria of participants enrolled in the two non-inferiority trials, with two notable exceptions. In the fracture trials, at least one prevalent vertebral fracture was required and in the BMD non-inferiority trials, a more stringent lumbar spine BMD entry requirement of a T-score less than −2.5 was required.
The objective of the current analysis was to estimate the treatment effect of ibandronate at different annual cumulative exposure levels on nonvertebral fractures relative to low ACE doses in postmenopausal women with osteoporosis.
Materials and methods
Study selection
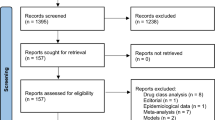
We evaluated all randomized clinical treatment trials of ibandronate of at least 1 year in duration that were identified from our systematic literature search of MEDLINE, EMBASE, and Cochrane Central Register of Controlled Trials (1999 to December 2006). Search terms included osteoporosis, postmenopausal women, fractures, bone density, and ibandronate. Treatment trials were defined as those trials in which the baseline lumbar spine (LS) T-score was ≤ −2.5, or the baseline prevalent vertebral fracture rate was >20%, or the mean age of participants was over 60 years. Baseline demographic characteristics were extracted for these trials. These studies were all conducted by the industry sponsor and as a result, all the individual patient data were available. All relevant data were transferred to the University of Ottawa where the statistical analyses were performed independently and without influence or input from the sponsor. The outcome was osteoporosis-related non-vertebral fractures defined as fractures of one of six key sites: humerus, clavicle, wrist, pelvis, hip, and leg. Nonvertebral fractures were ascertained in an identical fashion in the four main trials [1–4] and required radiographic confirmation.
Statistical analyses
An intention-to-treat (ITT) approach was used in the analysis of nonvertebral fractures. Doses of ibandronate that were included in the analyses were: 2.5 mg daily, 50/50 mg monthly, 100 mg monthly, 2 mg q 2 months i.v., 2 mg q 3 months i.v., and 20 mg orally q 2 days for 12 weeks every 3 months. This is in addition to the doses that are used in clinical practice: 150 mg oral once monthly and 3 mg i.v. q 3 months. Homogeneity of treatment effect was assessed and we conducted an exploratory approach of combining higher with lower doses of ibandronate. The varying definitions of high versus low ibandronate doses were developed a priori using the annual cumulative exposure (ACE) as a basis to group the different doses. Recognizing the different pharmacokinetics of the oral and intravenous forms of ibandronate, ACE was defined as the total annual dose of bisphosphonate absorbed and therefore available to the bone tissue taking into account the fact that 100% of an intravenous bisphosphonate and 0.6% of an oral dose are absorbed [11, 12]. For example, 2 mg i.v. every 2 months or 3 mg i.v. administered quarterly is equivalent to an ACE of 12 mg. Similarly, 150 mg orally given monthly is equivalent to an ACE of 10.8 mg. Treatment arms and doses were grouped for comparison so that trial randomization was maintained. Only studies that contributed data to both dose categories (e.g., low ACE versus high ACE or low ACE versus placebo) were included in each comparison, thus maintaining the original randomization. A time-to-event analysis was conducted using the Kaplan–Meier method to account for the differential time exposure across patients. The log-rank test and Cox proportional hazards regression models were used to assess for statistical differences and to calculate hazard ratios and their 95% CI. Fracture data were expressed as results after the 2-year time interval, although we also assessed the effect after 1 year of treatment (Table 1). Hazard ratios were adjusted to control for the effect of covariates (full model and stepwise fashion). Patient-level covariates adjusted for in the analysis included a previous history of clinical fracture, age, and baseline lumbar spine BMD. Age and lumbar spine BMD were treated as continuous variables instead of defining specific cut-off points. Study level characteristics were not available so we did not perform multi-level modeling. We did include an indicator for study as a covariate in the adjusted analysis. Prevalent vertebral fracture was not included as a covariate since this information was only available for two studies [1, 2]. We also assessed for potential interactions between patient level variables and study, by adding an interaction term to the model. All statistical analyses were conducted with SAS version 9.0 (SAS Institute, Cary, NC, USA).
Results
Eight trials were considered for inclusion in the pooled analysis and all were treatment trials. The baseline demographic characteristics, including baseline BMD T-scores and baseline clinical fractures are summarized in Table 1. Only two trials provided data on prevalent vertebral fractures [1, 2]. Of the eight trials, two contributed data to both higher and lower ACE dose categories [3, 4]. Although both trials used different doses and routes of administration, their study design and inclusion criteria were similar (Table 1).
High ACE versus low ACE doses
We pooled doses equivalent to an ACE of ≥ 10.8 mg (150 mg oral monthly, 2 mg i.v. 2-monthly, and 3 mg i.v. 3-monthly) compared with doses with an ACE of ≤ 7.2 mg (100 mg oral monthly, 50/50 mg monthly, and 2.5 mg daily). This comparison resulted in the pooling of nonvertebral fracture data from the two non-inferiority trials (n = 2,924) [3, 4] and resulted in an unadjusted HR of 0.635 (95% CI 0.43–0.94), p = 0.024 (Table 2). Similar treatment effects were seen when comparing higher doses, ACE ≥ 10.8 mg compared with an ACE of 5.5 mg (n = 2,137), and resulted in a HR of 0.621 (95% CI 0.396–0.974), p = 0.038 (Fig. 1). There was also a dose–response effect seen with increasing ACE doses (7.2–12 mg) compared with ACE of 5.5 mg, with hazard ratios ranging from 0.746 to 0.573 (Table 2). Using the 1-year data for the comparison of doses ≥ 12 versus 5.5 mg from two trials resulted in an adjusted (all covariates) HR (95% CI) of 0.550 (0.242–1.247). For ACE dose levels of ≥ 10.8 versus ≤ 7.2 mg, the adjusted HR (95% CI) was 0.601 (0.353–1.025).
Table 2 presents the hazard ratios (95% CI), both unadjusted and after adjustment, for all covariates. Adjustment of covariates had a minimal effect on the results, although combined ACE doses of 12 mg compared with 5.5 mg from one non-inferiority trial [4] resulted in a small change in the HR to 0.569 with upper limit of the 95% CI changing from 1.004 to 0.997. There were no significant interactions between patient-level characteristics with the study indicator variable.
We compared three trials that used doses equivalent to an ACE of 5.5 mg versus placebo (n = 3,212), and the unadjusted HR was 1.073 (95% CI 0.79–1.46). The results of these analyses remained nonsignificant, even when the size of the placebo group was increased by either including ineffective doses in the placebo group or by expanding the doses in the low ACE group, HR 0.99 (0.798–1.228; n = 6,465).
Discussion
Ibandronate has an extensive portfolio of randomized trials of treatment regimens examining different doses, routes of administration, and dosing intervals. From these trials we have learned which treatment regimens are ineffective and which are effective in preventing vertebral fractures. In a randomized placebo controlled trial, ibandronate (2.5 mg daily) was shown to reduce the risk of vertebral fractures by 62% after 3 years [1]. In a post hoc analysis of a high-risk subgroup of women in this trial, with femoral neck T-scores less than −3.0, a significant reduction in nonvertebral fractures (relevant risk reduction = 69%, p = 0.012) was also shown. More recently, trials that examined higher ACE have been conducted [3, 4, 10]. These non-inferiority trials compared intermittent doses, using higher doses administered intermittently, with daily oral ibandronate (2.5 mg daily). Both trials demonstrated greater reductions in bone turnover and larger increases in bone mineral density (BMD) in the treatment arms with higher ACE doses of ibandronate than 2.5 mg daily. For example, after 2 years, 150 mg monthly increased the lumbar spine BMD by 6.6% compared with 5% with 2.5 mg (p < 0.001). Significantly larger increases were also noted at hip BMD sites with higher ACE doses of 150 mg orally monthly and 3 mg i.v. quarterly [3, 4, 10]. Given these results, we hypothesized that the nonvertebral fracture efficacy of ibandronate may be dependent on using higher ACE associated with longer drug-free intervals. The results of our analyses suggest that ibandronate with an ACE ≥ 10.8 mg is significantly more effective at reducing nonvertebral fractures than lower ACE ibandronate. These analyses of higher ACE doses included doses used in clinical practice: 150 mg monthly and 3 mg i.v. every 3 months. The results also are consistent with nonvertebral fracture efficacy with an ibandronate ACE of 12 mg, resulting in a 43% reduction in nonvertebral fractures, and an ACE ≥ 10.8 mg resulting in a 38% reduction in nonvertebral fracture risk, while an ACE ≥ 7.2 mg produced a nonsignificant reduction of 25%. The significant effect on nonvertebral fractures with intermittent doses of ≥10.8 mg is consistent with larger effects on bone resorption and BMD demonstrated with these doses [13].
These results suggest that doses of ibandronate currently used in clinical practice confer nonvertebral fracture protection and that this effect was observed after 2 years of treatment. In addition, these results suggest that ibandronate at higher ACE would be another form of bisphosphonate that could be used to decrease the risk of nonvertebral fractures, in addition to other bisphosphonates that have been shown to be effective in reducing nonvertebral and hip fractures [14, 15].
Our analyses are not without limitations. This is not a direct placebo-controlled fracture trial demonstrating nonvertebral fracture efficacy, rather we conducted a pooled analysis of commonly used doses in the treatment trials using a time-to-event analysis. To minimize bias, we did not simply combine placebo groups and compare them with the combined doses of ibandronate from the different trials, but ensured that we maintained the randomization of participants and compared groups through common doses of ibandronate. This methodology has an effect of widening the confidence intervals, which results in a more conservative estimate of treatment effect. Another limitation was that we were unable to include prevalent vertebral fractures as a covariate in our analysis, since baseline vertebral fractures were not captured in all the comparator studies. Instead, we used history of clinical fracture as a covariate, since this was available in all trials. We adjusted for age, study, clinical fracture, and BMD, although this adjustment had little impact on the results. We did not have access to data on change in lumbar spine BMD so were unable to analyze the relationship between change in BMD and nonvertebral fracture risk, but BMD at baseline was not significantly related to nonvertebral fractures risk reduction, after adjusting for treatment and other covariates. It should also be noted that there was no statistical adjustment for the multiple comparisons performed. Finally, we were not able to comment on whether ibandronate decreased the risk of hip fractures, since the number of hip fractures was too small in both the treatment and placebo groups. The analysis for ACE ≥ 10.8 mg involved pooling two i.v. doses (2 mg every 2 months and 3 mg every 3 months) with the 150-mg oral dose. Thus, these results provided direct evidence of the high ACE dose level of ibandronate rather than individual oral and i.v. doses separately. The pooled results support a reduction in nonvertebral fractures with higher annual cumulative exposure to ibandronate, based on the significant reductions shown and the dose–response trend that was noted. Our results, while not providing the same level of evidence that is available from randomized trials, are consistent with a significant reduction in nonvertebral fractures with higher doses of ibandronate and are similar to risk reductions seen with other bisphosphonates [14, 15].
Conclusions
Higher monthly and quarterly intravenous doses of ibandronate have been shown to have significantly greater effects on surrogates of fracture risk, such as lumbar spine and hip BMD and markers of bone turnover, compared with lower daily doses [3, 4]. The results of this analysis using individual patient level data suggest that higher ibandronate doses given for 2 years, including the marketed doses of 150 mg monthly and 3 mg i.v. quarterly, significantly reduce the risk of nonvertebral fractures by 38–43%, in comparison to the 2.5-mg daily dose.
References
Chesnut CH III, Skag A, Christiansen C, Recker R, Stakkestad JA, Hoiseth A et al (2004) Effects of oral ibandronate administered daily or intermittently on fracture risk in postmenopausal osteoporosis. J Bone Miner Res 8:1241–1249
Recker R, Stakkestad JA, Chesnut CH III, Christiansen C, Skag A, Hoiseth A et al (2004) Insufficiently dosed intravenous ibandronate injections are associated with suboptimal antifracture efficacy in postmenopausal osteoporosis. Bone 34(5):890–899
Miller PD, McClung MR, Macovei L, Stakkestad JA, Luckey M, Bonvoisin B et al (2005) Monthly oral ibandronate therapy in postmenopausal osteoporosis: 1-year results from the MOBILE study. J Bone Miner Res 20(8):1315–1322
Delmas PD, Adami S, Strugala C, Stakkestad JA, Reginster JY, Felsenberg D et al (2006) Intravenous ibandronate injections in postmenopausal women with osteoporosis: one-year results from the dosing intravenous administration study. Arthritis Rheum 54(6):1838–1846
Ravn P, Neugebauer G, Christiansen C (2002) Association between pharmacokinetics of oral ibandronate and clinical response in bone mass and bone turnover in women with postmenopausal osteoporosis. Bone 30(1):320–324
Adami S, Felsenberg D, Christiansen C, Robinson J, Lorenc RS, Mahoney P et al (2004) Efficacy and safety of ibandronate given by intravenous injection once every 3 months. Bone 34(5):881–889
Riis BJ, Ise J, von Stein T, Bagger Y, Christiansen C (2001) Ibandronate: a comparison of oral daily dosing versus intermittent dosing in postmenopausal osteoporosis. J Bone Miner Res 16(10):1871–1878
Thiebaud D, Burckhardt P, Kriegbaum H, Huss H, Mulder H, Juttmann JR et al (1997) Three monthly intravenous injections of ibandronate in the treatment of postmenopausal osteoporosis. Am J Med 103(4):298–307
Delmas PD, Recker RR, Chesnut CH III, Skag A, Stakkestad JA, Emkey R et al (2004) Daily and intermittent oral ibandronate normalize bone turnover and provide significant reduction in vertebral fracture risk: results from the BONE study. Osteoporos Int 15(10):792–798
Reginster JY, Adami S, Lakatos P, Greenwald M, Stepan JJ, Silverman SL et al (2006) Efficacy and tolerability of once-monthly oral ibandronate in postmenopausal osteoporosis: 2 year results from the MOBILE study. Ann Rheum Dis 65(5):654–661
Barrett J, Worth E, Bauss F, Epstein S (2004) Ibandronate: a clinical pharmacological and pharmacokinetic update. J Clin Pharm 44(9):951–965
Cremers SC, Pillai G, Papapoulos SE (2005) Pharmacokinetics/pharmacodynamics of bisphosphonates: use for optimization of intermittent therapy for osteoporosis. Clin Pharmacokinet 44(6):551–570
Papapoulos SE, Schimmer RC (2007) Changes in bone remodelling and antifracture efficacy of intermittent bisphosphonate therapy: implications from clinical studies with ibandronate. Ann Rheum Dis 66(7):853–858
Harrington JT, Ste-Marie LG, Brandi ML, Civitelli R, Fardellone P, Grauer A et al (2004) Risedronate rapidly reduces the risk for nonvertebral fractures in women with postmenopausal osteoporosis. Calcif Tissue Int 74(2):129–135
Papapoulos SE, Quandt SA, Liberman UA, Hochberg MC, Thompson DE (2005) Meta-analysis of the efficacy of alendronate for the prevention of hip fractures in postmenopausal women. Osteoporos Int 16(5):468–474
Acknowledgements
Funding for this project was from an unrestricted research grant from F. Hoffman-La Roche. The authors would like to thank Hoffman La Roche and GlaxoSmithKline for supplying the individual patient data utilized in the analysis, and acknowledge that the analysis was completed without influence from either company. A. Cranney (AC) would like to acknowledge salary support from the Canadian Institutes of Health Research.
Conflicts of interest
Ethel S. Siris: consultant for Wyeth, Procter & Gamble/sanofi-aventis, Novartis, Eli Lilly, Roche/GlaxoSmithKline, Amgen; speaker for Eli Lilly, Procter & Gamble/Sanofi-aventis, Novartis.
Stuart L. Silverman: speaker’s bureau for Eli Lilly, Merck, Procter & Gamble, Roche; consultant for Merck, Procter & Gamble, Wyeth, Roche, Novartis; research support: Novartis, Eli Lilly, Wyeth, Roche, Procter & Gamble, Merck; board of directors, Compumed
Philip Sambrook: consultant/speaker: for Amgen, GSK, Merck, Novartis, sanofi-aventis, Servier; clinical trials for Amgen, Servier, GSK, Merck, Novartis
Jean-Yves Reginster: consulting fees or paid advisory boards, Servier, Novartis, Negma, Eli Lilly, Wyeth, Amgen, GlaxoSmithKline, Roche, Merckle, Nycomed, NPS, Theramex; lecture fees when speaking from Merck Sharp and Dohme, Eli Lilly, Rottapharm, IBSA, Genevrier, Novartis, Servier, Roche, GlaxoSmithKline, Teijin, Teva, Ebewee Pharma, Zodiac, Analis, Theramex, Nycomed, Novo-Nordisk; grant support from Bristol Myers Squibb, Merck Sharp & Dohme, Rottapharm, Teva, Eli Lilly, Novartis, Roche, GlaxoSmithKline, Amgen, Servier
Socrates Papapoulos: consulting fees from Amgen, Eli Lilly, Merck & Co, Novartis, Procter & Gamble, Roche/GSK, Servier; research grant support from Merck Sharp & Dohme, Procter & Gamble
Pierre D. Delmas: research grants from Procter & Gamble, Eli Lilly, Amgen; consultation for and/or speaker fees from: Acceleron, Amgen, Eli Lilly, GSK, MSD, Novartis, Nycomed, Organon, Pfizer, Procter & Gamble, Roche, Sanofi-Aventis, Servier, Wyeth, Zelos
Jonathan D. Adachi: consultant/speaker: for Amgen, Astra Zeneca, Eli Lilly, GSK, Merck, Novartis, Pfizer, Procter & Gamble, Roche, Sanofi-Aventis, Servier; clinical trials for Amgen, Eli Lilly, GSK, Merck, Novartis, Pfizer, Procter & Gamble, Roche
A. Cranney: consultant fees from Amgen, Merck Frosst, Procter & Gamble
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cranney, A., Wells, G.A., Yetisir, E. et al. Ibandronate for the prevention of nonvertebral fractures: a pooled analysis of individual patient data. Osteoporos Int 20, 291–297 (2009). https://doi.org/10.1007/s00198-008-0653-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-008-0653-8