Abstract
Summary
We investigated the efficacy of dynamic radiographs for diagnosing acute osteoporotic vertebral fractures (OVFs) compared with supine radiographs or sitting radiographs alone. Evaluation of the dynamic radiographs was superior to the other evaluations. Dynamic radiographs provide a convenient and useful method of diagnosing acute OVFs.
Introduction
Identifying acute OVFs on plain radiographs is difficult. We studied a new approach to identify acute OVFs on the basis of fracture mobility.
Methods
We performed a retrospective radiographic analysis of 472 acute OVFs (<3 weeks after onset), which were diagnosed on the basis of magnetic resonance imaging of T5 through L5 (a total of 5,239 vertebrae). Supine lateral radiographs were compared with sitting lateral radiographs to determine the presence or absence of mobility. Vertebrae showing changes in the vertebral body height were diagnosed as acute OVFs. We analyzed the diagnostic accuracy on the basis of comparative supine and sitting lateral radiographs and compared it with that of radiographs obtained in the supine or the sitting position alone.
Results
Of the 472 acute OVFs diagnosed, 313 (66 %) exhibited vertebral mobility on supine lateral and sitting lateral radiographs. Correct diagnoses of acute OVFs or no acute OVFs were made in 4,883 vertebrae. There were 159 unreadable OVFs (3 %), and 197 previous OVFs (4 %) were misdiagnosed as acute OVFs. The sensitivity was 66 % and the specificity was 96 %. Evaluation of the mobility of acute OVFs in the supine and the sitting position was superior to evaluation using radiographs in either the supine or the sitting position alone.
Conclusions
Dynamic radiographs provide a convenient way to identify acute OVFs.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a skeletal disorder characterized by a loss of bone strength—comprising bone quality and bone mineral density—and an increased risk of fractures. Osteoporotic vertebral fractures (OVFs) are the most common type of fragility fracture. The prevalence of OVFs increases steadily with age, reaching 40 % in 80-year-old females [1, 2]. OVFs not only cause height loss but also are a strong predictor of future fractures and mortality [2, 3]. Therefore, diagnosing OVFs is crucial for the proper treatment of acute back pain and prevention of postfracture sequelae.
The diagnosis of OVFs largely relies on the observation of vertebral deformations on plain radiographs. In order to minimize the subjective biases intrinsic to qualitative reading and to standardize data analyses, a number of morphometric systems have been developed. Currently, three general approaches are used to identify OVFs: (1) visual identification of fracture; (2) visual identification using either the semiquantitative assessment (SQ) grading developed by Genant et al. [4] or the algorithm-based approach for qualitative identification of vertebral fracture (ABQ) developed by Jiang et al. [5]; and (3) quantitative morphometry (QM), which was first developed in the 1960s [6]. Although SQ grading and QM assessment have been considered the gold standard methods for OVF assessment, they have limitations. Distinguishing acute OVFs from other conditions with a similar radiographic appearance, such as non-fracture deformities or previous OVFs, can be difficult in many cases if no previous radiograph is available for comparison. Moreover, in clinical practice, OVF does not always result in decreased vertebral height on lateral radiographs in the lateral position (Genant's Grade 0 deformation [4]) at presentation although acute OVFs can be confirmed by magnetic resonance imaging (MRI) [7]. Pham et al. reported that 63 % of acute OVFs displaying no visible deformation of the vertebral body on initial radiographs (Genant's grade 0), confirmed by MRI, worsened and eventually resulted in a reduction of vertebral height (Genant's grade ≥ 1) [7].
MRI has a high degree of accuracy for making a definite diagnosis of acute OVF and it continues to be used as the most useful tool. However, because of limitations in equipment as well as considerations that must be given to the economics of medical treatment, it is not possible to use MRI in all patients. Therefore, conventional radiography is still the mainstay of diagnosis when assessing OVFs in daily clinics.
Mobility refers to a change of vertebral height or configuration with changes in body positioning [8]. There have been occasional reports that many OVFs are mobile [9–11]. Comparative radiographs taken in weight-bearing positions (standing or sitting) and in supine positions have been used to determine the indication of percutaneous vertebroplasty for delayed union or nonunion of OVF [12–14]. Because many acute OVFs also exhibit mobility, comparative supine and sitting lateral radiographs help to identify acute OVFs [9]. In the present study, in which diagnoses were made on the basis of MRI, we analyzed the diagnostic accuracy of comparative supine and sitting lateral radiographs for diagnosing acute OVFs and evaluated their efficacy for predicting any subsequent reduction in vertebral height.
Materials and methods
Participants
Four hundred and three patients who presented with acute back pain and were diagnosed as having acute OVFs on MRI were enrolled in this study. OVFs were diagnosed in cases with no history of trauma or as a result of low-energy trauma (a fall on the ground or from a height of <1 m). Acute OVFs were defined within 3 weeks of injury or the onset of symptoms [15]. Patients who had a history of primary or metastatic bone tumors, infectious disease, or hematological disorders were excluded. Of the patients enrolled, 310 were female and 93 were male, with an average age of 80.4 ± 8.9 years [mean ± standard deviation (SD)]. Two hundred and nine patients had experienced a simple fall, 100 patients were unable to identify the cause of their injury, and 94 patients sustained injuries with no history of trauma.
Measurements
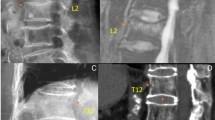
All radiographs were taken at the initial visit at a film-focus distance of 100 cm with the X-ray beam centered at T8 for the thoracic spine and at L3 for the lumbar spine. Fracture mobility was determined by comparing cross-table supine lateral radiographs with sitting lateral radiographs (Fig. 1), as reported by previous studies [9–11]. In brief, vertebral body height was measured to the nearest millimeter in the lateral digitized radiographs. Mobility was considered present when a measurable change in vertebral body height occurred between supine and sitting radiographs. In this study, we defined “dynamic radiography” as the comparison of measured vertebral height between cross-table supine lateral and sitting lateral views. Fractures that were not mobile were considered fixed (i.e., measurable change in vertebral body height did not occur between supine and sitting radiographs). For each participant, we recorded the presence of OVFs identified between the levels of T5 and L5. Follow-up radiographs were obtained >3 months after the initial radiographs to evaluate any subsequent reduction in vertebral height and to exclude other causes of fracture.
A 96-year-old female patient sustained an L1 acute osteoporotic vertebral fracture (OVF) following a fall. a Supine cross-table lateral radiograph of severe T12 and L2 OVFs. b Sitting lateral view of an L1 OVF showing mobility, whereas no height change was observed at T12 or L2. c Sagittal magnetic resonance imaging showing an acute OVF at L1 on a T1-weighted image
T1-weighted images, T2-weighted images, and T2-weighted fat suppression images were used in MRI {1.5 T, T1-weighted images [spin-echo (SE): repetition time (TR)/echo time (TE) = 550/12 ms]; T2-weigthed images [SE: TR/TE = 2500/100 ms]}. The criteria for the diagnosis of acute OVF were bone marrow signal anomalies in the form of a band-like homogenous bone marrow edema feature (low signal on T1-weighted and high signal on T2-weighted images), a horizontal linear fracture parallel to a vertebral plateau (low signal on all sequences) or both, and the absence of any tumor signs (nodular signal anomalies, posterior bulging of the vertebral body, involvement of the posterior elements of the vertebra, and epidural or soft tissue mass) [7]. Complete bone marrow signal replacement within the vertebral body did not rule out the diagnosis of osteoporotic collapse if a fracture line was identified and no other sign suggestive of a tumor was present [7]. In addition, vertebrae in which signal intensity was limited to the vicinity of the upper and lower end plates of the vertebral body were determined to be degenerative disk lesions. A diagnosis of acute OVF using MRI was made by two radiologists with >20 years of clinical experience, and by four orthopedic surgeons with >10 years of clinical experience. All assessors were blinded to the results of the plain radiographs. A diagnosis was considered correct when two investigators reached the same conclusion. MRI was performed within 3 days of the initial visit. A diagnosis of acute OVF using radiographs was made by the four orthopedic surgeons.
Differences in the ability of the four orthopedic surgeons to interpret spinal radiographs were investigated in advance. The subjects of this investigation were 50 patients with OVF, and the surgeons received training to standardize their approach to diagnosis. To determine sample size, we used the recommendations of Loewen and Philp [16]. To determine the reliability of OVF assessment based on comparative supine and sitting lateral radiographs, we estimated the agreement corrected for chance using a simple kappa (k) coefficient inter-reader and intra-reader agreement and associated 95 % confidence interval (CI) [17]. All vertebrae were classified as either acute fracture or non-acute fracture. To interpret the agreement, we used the criteria described by Landis and Koch [18], which classified agreement as almost perfect (0.81–1.00), substantial (0.61–0.80), moderate (0.41–0.60), fair (0.21–0.40), slight (0.00–0.20), or poor (<0.00). The results revealed that inter-reader agreement was substantial with a k coefficient of 0.755 (95 % CI, 0.659–0.851), whereas intra-reader agreement was also substantial with a k coefficient of 0.730 (95 % CI, 0.651–0.809). Accordingly, we assumed that there was no difference in the ability of orthopedic surgeons to interpret radiographs using comparative supine and sitting lateral radiographs with good reproducibility.
Next, we analyzed the diagnostic accuracy of dynamic radiographs and compared this with radiographs obtained in the supine position alone or in the sitting position alone. A diagnosis of acute OVFs using plain radiographs (comparative supine and sitting position, supine position alone, or sitting position alone) was made by orthopedic surgeons who were blinded to the results of the other plain radiographs and MRI. Secondly, vertebral height was calculated as the distance in millimeters between the points on the superior and inferior end plates at the anterior (Ha), middle (Hm), or posterior (Hp) location. The magnitude and percentage change of the vertebral height between the supine and the sitting positions were evaluated to determine diagnostic accuracy. For the analyses, precision error was calculated for each dimension, Ha, Hm, and Hp by blinded, triplicate measurements of 20 randomly selected fractured vertebrae evaluated in sitting and supine position and expressed as percent coefficient of variation (%CV) and SD. Precision errors expressed as %CV were 6.7, 8.0, and 4.6 % for Ha, Hm, and Hp, respectively, in sitting position, and 4.4, 6.1, and 4.6 % for Ha, Hm, and Hp, respectively, in supine position. The precision errors correspond to SDs of 1.2 mm for Ha, 1.3 mm for Hm, and 1.3 mm for Hp in sitting position and 1.0 mm for Ha, 1.2 mm for Hm, and 1.4 mm for Hp in supine position. Magnification error between radiographs in sitting position and radiographs in supine position was also calculated by blinded, triplicate measurements of 20 randomly selected non-fractured vertebrae. Magnification errors expressed as %CV were 3.7, 3.3, and 3.1 % for Ha, Hm, and Hp, respectively, and compared favorably with previous report [11]. The precision errors correspond to SDs of 1.1 mm for Ha, 1.0 mm for Hm, and 1.0 mm for Hp. Accordingly, we assumed that there was an allowable error in calculating vertebral height using dynamic radiographs. Third, the magnitude of the reduction in vertebral height on follow-up radiographs, obtained after >3 months, compared with the initial radiographs, was evaluated between the following subgroups to evaluate efficacy for predicting subsequent reduction in vertebral height using the initial radiographs: (1) subgroup of acute OVFs correctly diagnosed on initial radiographs (correct group) and (2) subgroup of acute OVFs incorrectly diagnosed on initial radiographs (incorrect group).
Statistical analysis
Statistical analysis was performed using the chi-square test and the Mann–Whitney U test. Differences with P values of <0.05 were considered significant. The analysis was performed using the StatView statistical software package (version 5.0; SAS Institute, Cary, NC).
The study was conducted according to the ethical principles stated in the Declaration of Helsinki and was approved by the ethical committee of our institution. Written informed consent was obtained from the patients.
Results
We observed 472 OVFs in 403 patients. Almost two-thirds of fractures were identified between T11 and L2 on MRI. L1 was the most commonly affected level, identified in 112 cases, with T12 being the next most commonly affected level with 86 cases followed by 64 fractures at L3, 43 fractures at T11 and L2, 35 fractures at L4; the remaining fractures were evenly distributed among other levels (Fig. 2).
Evaluation in the supine position
Table 1 depicts the results of evaluation of supine lateral radiographs. Overall, a correct diagnosis was made in 4,685 vertebrae (89.4 %) (agreement between correct diagnosis of acute fracture and correct diagnosis of non-acute fractures). There were 285 unreadable OVFs (5.4 %) between T5 and L5 on the supine lateral radiographs (unreadable rate) and 269 misdiagnosed OVFs (false positives). A breakdown shows that a correct diagnosis of acute OVF (true positive) was made in 187 fractures, and a correct diagnosis of non-acute OVF, which included non-fractured vertebra and previous OVF (true negative) was judged to be present in 4,498 vertebrae. Therefore, overall, the sensitivity was 39.6 % and the specificity was 94.4 % (Table 2). The positive predictive value (PPV) was 41.0 % and the negative predictive value (NPV) was 94.0 %.
Evaluation in the sitting position
Table 3 depicts the results of evaluation of sitting lateral radiographs. Overall, a correct diagnosis was made in 4,696 vertebrae (89.6 %) (agreement). There were 269 unreadable OVFs (5.1 %) on sitting lateral radiographs (unreadable rate) and 274 misdiagnosed OVFs (false positives). The details are shown in Table 2.
Evaluation in supine and sitting positions
Table 4 depicts the results of evaluation of comparative supine and sitting radiographs. Of 472 acute OVFs diagnosed on MRI, 313 vertebrae (66.3 %) exhibited mobility on supine lateral and sitting lateral radiographs. Overall, a correct diagnosis was made in 4,883 vertebrae (93.2 %) (agreement). There were 159 unreadable OVFs (3.0 %) between T5 and L5 on the supine lateral radiographs (unreadable rate) and 197 misdiagnosed OVFs (false positives). A breakdown shows that a correct diagnosis of acute fractures (true positive) was made in 313 OVFs, and non-acute OVFs (true negative) were judged to be present in 4,570 vertebrae. Therefore, the sensitivity was 66.3 % and the specificity was 95.9 % (Table 2). PPV was 61.4 % and NPV was 96.6 %. Prevalence of mobility based on location of the OVFs showed that mobility is the most common at the thoracolumbar junction. There was a significant difference of mobility based on location of OVFs (P < 0.01, Chi-square test) (Table 5)
Optimal cutoff value for diagnosis of acute OVF
We classified the 313 acute OVFs which exhibited mobility into two groups according to the magnitude or the rate of change of the vertebral height between the supine and the sitting positions. The results are shown in Table 6. The average reduction in vertebral height with mobile fractures was 5.4 ± 4.4 mm. Among 313 acute OVFs diagnosed on dynamic radiographs, 262 vertebrae (83.7 %) exhibited a change of >2 mm, 220 vertebrae (70.3 %) exhibited a change of >3 mm, and 192 vertebrae (61.5 %) exhibited a change of >4 mm. With regard to the vertebral percent height reduction, 220 vertebrae (70.3 %) exhibited a change of >10 %, 106 vertebrae (33.9 %) exhibited a change of >20 %, and 55 vertebrae (17.6 %) exhibited a change of >30 %. A QM assessment of OVFs suggested that a 2-mm reduction in vertebral height was the most reasonable cutoff value for screening for OVFs.
Subsequent reduction in vertebral height on follow-up radiographs
A mean reduction of 6.6 ± 4.2 mm in vertebral height occurred on subsequent radiographs in the correct group and a reduction of 3.0 ± 4.0 mm in vertebral height occurred in the incorrect group. There was a significant difference in the subsequent reduction in vertebral height between the correct group and the incorrect group (P < 0.01, Mann–Whitney U test). Therefore, a large future height loss of OVF was assumed when acute OVF was correctly diagnosed using dynamic radiographs, whereas a relatively small height loss was expected if acute OVF was not diagnosed using dynamic radiographs.
Discussion
This study attempted to analyze the potential benefits offered by dynamic radiographs in the diagnosis of acute OVFs compared with information obtained from supine lateral radiographs or sitting lateral radiographs alone. According to our results, the detection rate of acute OVFs was much higher on dynamic radiographs than on either supine lateral radiographs or sitting lateral radiographs alone. In addition, dynamic radiographs were useful for estimating the prognosis of acute OVFs.
Plain radiographs are the mainstay for initial diagnosis of OVFs. Nonetheless, reaching a clear diagnosis of acute OVFs is difficult in many vertebrae. Identifying acute OVFs on plain radiographs is problematic because (1) “normal” radiological appearances in the spine vary greatly both among and within individuals, (2) “abnormal” appearances due to non-fracture deformities and normal variants are common but can be difficult to differentiate from true OVFs, (3) osteoporosis can often cause asymptomatic OVFs and make it difficult to distinguish between acute OVFs and previous OVFs, and (4) OVFs do not always result in a reduction in vertebral height on lateral radiographs. Therefore, a correct diagnosis of acute OVFs can be difficult. Ito et al. reported that acute OVF was correctly diagnosed in 51.5 % of cases [19]. The false-negative rates of diagnosis of acute OVFs on conventional radiographs have been reported to range from 27 to 48.5 % [20, 21]. Hence MRI is often performed in elderly patients with vertebral disease because it is currently the only available definitive diagnostic tool; however, it is costly and not always immediately available.
On the basis of the problems raised above, we investigated whether the correct diagnostic rates for acute OVFs using radiographic diagnosis could be improved by the use of dynamic radiographs compared with either supine lateral radiographs or sitting lateral radiographs alone. To the best of our knowledge, this type of comparison has not been carried out to date; however, a search of the literature has revealed that various datasets are available on the diagnostic rate of acute OVF using radiographs. Ito et al. evaluated diagnosis of acute OVFs using the criteria of Genant et al. [4], which are commonly used in the diagnosis of acute OVFs, but only 45.5 % of acute OVFs could be diagnosed correctly [19]. Nakano et al. also evaluated diagnosis of acute OVFs using Japanese guidelines [22] which are essentially the same as those used for QM assessment [6]. They reported that sensitivity was 45.9 %, specificity was 89.3 %, PPV was 41.5 %, and NPV was 91.2 %. In contrast, Kanchiku et al. reported a high correct diagnosis rate of 87 % [23]. In this study, using dynamic radiographs, we demonstrated sensitivity of 66 %, specificity of 96 %, PPV of 61 %, and NPV of 97 % for diagnosing acute OVFs. These results were superior to evaluation using either supine or sitting radiographs alone. However, it is necessary to keep in mind the fact that many factors, such as the skill levels of the examiners, the background of the patients, or radiographic conditions, make the simple comparison of a correct diagnosis rate difficult. However, these results offer concrete insights, and we therefore recommend that dynamic radiographs should be used in the management of patients with acute low back or back pain who are suspected of having acute OVFs.
Dynamic radiographs identify acute OVFs on the basis of fracture mobility. This method differs in concept from conventional morphology-based fracture diagnosis such as SQ, ABQ, and QM. Identifying the presence of mobility by dynamic radiography furthers our understanding of the pathophysiology of OVF and provides clinicians with an opportunity to correctly identify the cause of an elderly osteoporotic patient's back pain by requesting an axially loaded (standing or sitting) radiographs than simply requesting the standard radiographs which may well be a non-axially loaded lateral decubitus film. Kawaguchi et al. [9] analyzed 41 acute OVFs diagnosed on dynamic radiographs and revealed dynamic vertebral mobility in 81 % of fractures. In this study, dynamic vertebral mobility was found in 66 % of fractures, with an average reduction in vertebral height of 5.4 ± 4.4 mm on subsequent radiographs observed in the mobile acute OVFs.
Dynamic radiographs are useful for estimating the subsequent loss in vertebral height of acute OVFs. To the best of our knowledge, this is also the first attempt to evaluate this parameter. Why some OVFs did not result in mobility is unclear. OVFs that could not be diagnosed on dynamic radiographs might contain micro-trabecular fracture, which are considered to be a step prior to OVF with mobility. Otherwise, OVFs that could be diagnosed on dynamic radiographs exhibited severe breakage of interconnected bone fibers of both cortical and cancellous bone; therefore, the mobile OVFs collapsed easily compared with OVFs that were not mobile.
There are two major drawbacks of dynamic radiographs. One is radiation exposure. The other is back pain during examination. Assessment by fracture mobility requires radiographs in weight-bearing position and supine position. Back pain during radiographic examination (e.g., lie down on the X-ray table, adjust the position on the table, and sit up from the table) has the possibility to disturb the later radiographic examination. Back pain during radiographic examination was common in the lateral decubitus position, but back pain in the supine positions is partially stronger than the lateral decubitus position. Although there were no patients who could not take radiographic examination due to back pain in our institution, Kawaguchi et al. reported one of 38 patients was unable to sit up for the radiographs due to back pain [9].
This study has several limitations that should be kept in mind when interpreting its results. First, although the k coefficients of inter-reader and intra-reader agreement were acceptable, the manual measurement of the images might have caused intra-observer and inter-observer error. The second limitation was that the manual measurement of the images also might have caused the precision and magnification errors, although they were acceptable. The third limitation was that although we compared the accuracy of dynamic radiographs with information obtained from either supine lateral radiographs or sitting lateral radiographs alone in this study, with the results revealing that comparative evaluation was superior to the other evaluations, there was no control group. Lateral radiographs are usually obtained in the lateral decubitus position in most institutions which has neither the features of the axially loaded (standing or sitting) lateral views or the hyperextended (cross table) lateral views. Comparison of the accuracy between dynamic radiographs and standard lateral radiographs in the lateral decubitus position is required. Fourth, distortion of the vertebral body and end plates in oblique projection might reduce the accuracy, which is a common problem in other methods of OVF assessment [21, 24, 25]. Fifth, the dynamic radiography has not previously been discussed and needs to be standardized. Further study is warranted.
In conclusion, dynamic radiographic examinations are an effective tool for correctly identifying acute OVFs. By incorporating these scans into routine clinical assessments, clinicians can reduce costs and MRI examination which is occasionally painful for the patients, and thereby enhance the care of patients suspected of having OVFs.
References
Ross PD, Davis JW, Epstein RS, Wasnich RD (1994) Pain and disability associated with new vertebral fractures and other spinal conditions. J Clin Epidemiol 47:231–239
Kado DM, Browner WS, Palermo L, Nevitt MC, Genant HK, Cummings SR (1999) Vertebral fractures and mortality in older women: a prospective study. Study of Osteoporotic Fractures Research Group. Arch Intern Med 159:1215–1220
Black DM, Arden NK, Palermo L, Pearson J, Cummings SR (1999) Prevalent vertebral deformities predict hip fractures and new vertebral deformities but not wrist fractures. Study of Osteoporotic Fractures Research Group. J Bone Miner Res 14:821–828
Genant HK, Wu CY, van Kuijk C, Nevitt MC (1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 8:1137–1148
Jiang G, Eastell R, Barrington NA, Ferrar L (2004) Comparison of methods for the visual identification of prevalent vertebral fracture in osteoporosis. Osteoporos Int 15:887–896
Hurxthal LM (1968) Measurement of anterior vertebral compressions and biconcave vertebrae. Am J Roentgenol Radium Ther Nucl Med 103:635–644
Pham T, Azulay-Parrado J, Champsaur P, Chagnaud C, Legré V, Lafforgue P (2005) “Occult” osteoporotic vertebral fractures: vertebral body fractures without radiologic collapse. Spine (Phila Pa 1976) 30:2430–2435
Facizewski T, McKiernan F (2002) Calling all vertebral fractures: a consensus for comparison of treatment and outcome. J Bone Miner Res 17:185–191
Kawaguchi S, Horigome K, Yajima H, Oda T, Kii Y (2011) Comparative supine-sitting lateral radiographs identifying incident osteoporotic vertebral fractures. Eur Orthop Traumatol 1:157–162
McKiernan F, Faciszewski T, Jensen R (2006) Latent mobility of osteoporotic vertebral compression fractures. J Vasc Interv Radiol 17:1479–1487
McKiernan F, Jensen R, Faciszewski T (2003) The dynamic mobility of vertebral compression fractures. J Bone Miner Res 18:24–29
Wu MH, Huang TJ, Cheng CC, Li YY, Hsu RW (2010) Role of the supine lateral radiograph of the spine in vertebroplasty for osteoporotic vertebral compression fracture: a prospective study. BMC Musculoskelet Disord 11:164
Mehta JS, Reed MR, McVie JL, Sanderson PL (2004) Weight-bearing radiographs in thoracolumbar fractures: do they influence management? Spine (Phila Pa 1976) 29:564–567
Faciszewski T, McKiernan F (2002) Calling all vertebral fractures classification of vertebral compression fractures: a consensus for comparison of treatment and outcome. J Bone Miner Res 17:185–191
Reinhold M, Knop C, Beisse R, Audigé L, Kandziora F, Pizanis A, Pranzl R, Gercek E, Schultheiss M, Weckbach A, Bühren V, Blauth M (2010) Operative treatment of 733 patients with acute thoracolumbar spinal injuries: comprehensive results from the second, prospective, Internet-based multicenter study of the Spine Study Group of the German Association of Trauma Surgery. Eur Spine J 19:1657–1676
Loewen S, Philp J (2006) Recasts in the adult L2 classroom: characteristics, explicitness, and effectiveness. Mode Lang J 90:536–556
Cohen J (1960) A coefficient of agreement for nominal scales. Educ Psychol Meas 20:37–46
Landis JR, Koch GG (1977) An application of hierarchical kappa-type statistics in the assessment of majority agreement among multiple observers. Biometrics 33:363–374
Ito Z, Harada A, Matsui Y, Takemura M, Wakao N, Suzuki T, Nihashi T, Kawatsu S, Shimokata H, Ishiguro N (2006) Can you diagnose for vertebral fracture correctly by plain X-ray? Osteoporos Int 17:1584–1591
Binkley N, Krueger D, Gangnon R, Genant HK, Drezner MK (2005) Lateral vertebral assessment: a valuable technique to detect clinically significant vertebral fractures. Osteoporos Int 16:1513–1518
Link TM, Guglielmi G, van Kuijk C, Adams JE (2005) Radiologic assessment of osteoporotic vertebral fractures: diagnostic and prognostic implications. Eur Radiol 15:1521–1532
Nakano T, Abe Y, Shimizu Y, Ochi R, Seike I, Iwamoto K, Fujiwara K, Takagi K (1999) Rate of correct diagnosis for vertebral fracture by plain roentgenograms (in Japanese). Fracture 21:586–588
Kanchiku T, Taguchi T, Kawai S (2003) Magnetic resonance imaging diagnosis and new classification of the osteoporotic vertebral fracture. J Orthop Sci 8:463–466
Paggiosi MA, Finigan J, Peel N, Eastell R, Ferrar L (2012) Supine vs decubitus lateral patient positioning in vertebral fracture assessment. J Clin Densitom 15:454–460
Sanfélix-Genovés J, Arana E, Sanfélix-Gimeno G, Peiró S, Graells-Ferrer M, Vega-Martínez M (2012) Agreement between semi-automatic radiographic morphometry and Genant semi-quantitative method in the assessment of vertebral fractures. Osteoporos Int 23:2129–2134
Acknowledgments
The authors thank Miss Kana Nakanishi, Mr. Kenji Kuroda, Mr. Haruyoshi Mizuno, Mrs. Akiko Hattori, Mr. Masashi Kawamura, Mr. Yasuhiro Hyodo, Mr. Takuya Yamashita, and Mr. Hiroto Takeno for their diligence in preparing the clinical recordings.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Niimi, R., Kono, T., Nishihara, A. et al. Efficacy of the dynamic radiographs for diagnosing acute osteoporotic vertebral fractures. Osteoporos Int 25, 605–612 (2014). https://doi.org/10.1007/s00198-013-2456-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-013-2456-9