Abstract
Summary
High direct incremental healthcare costs post-fracture are seen in the first year, but total costs from a third-party healthcare payer perspective eventually fall below pre-fracture levels. We attribute this to higher mortality among fracture cases who are already the heaviest users of healthcare (“healthy survivor bias”). Economic analyses that do not account for the possibility of a long-term reduction in direct healthcare costs in the post-fracture population may systematically overestimate the total economic burden of fracture.
Introduction
High healthcare costs in the first 1–2 years after an osteoporotic fracture are well recognized, but long-term costs are uncertain. We evaluated incremental costs of non-traumatic fractures up to 5 years from a third-party healthcare payer perspective.
Methods
A total of 16,198 incident fracture cases and 48,594 matched non-fracture controls were identified in the province of Manitoba, Canada (1997–2002). We calculated the difference in median direct healthcare costs for the year pre-fracture and 5 years post-fracture expressed in 2009 Canadian dollars with adjustment for expected age-related healthcare cost increases.
Results
Incremental median costs for a hip fracture were highest in the first year ($25,306 in women, $21,396 in men), remaining above pre-fracture baseline to 5 years in women but falling below pre-fracture costs by 5 years in men. In those who survived 5 years following a hip fracture, incremental costs remained above pre-fracture costs at 5 years ($12,670 in women, $7,933 in men). Incremental costs were consistently increased for 5 years after spine fracture in women. Total incremental healthcare costs for all incident fractures combined showed a large increase over pre-fracture costs in the first year ($137 million in women, $57 million in men), but fell below pre-fracture costs within 3–4 years. Elevated total healthcare costs were seen at year 5 in women after wrist, humerus and spine fractures, but these were somewhat offset by decreases in total healthcare costs for other fractures.
Conclusions
High direct healthcare costs post-fracture are seen in the first year, but total costs eventually fall below pre-fracture levels. Among those who survive 5 years following a fracture, healthcare costs remain above pre-fracture levels.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a common condition predisposing to low trauma fractures. About 40 % of women in developed countries will experience an osteoporosis-related fracture in the course of their lifetime with men experiencing approximately one-third to one-half the risk of women [1, 2]. There are significant health consequences to individuals who sustain fractures such as pain, reduced quality of life, loss of independence and increased morbidity and mortality [3–6].
Many studies have also highlighted the major economic burden of osteoporosis and fracture care to society given the significant excess costs related to osteoporotic hip fractures [7, 8] and non-hip fractures [9–13]. First year post-fracture costs are most commonly reported as long-term cost data are difficult to collect, particularly at the third-party healthcare payer level. A smaller number of studies have examined second year post-fracture costs [14–16], but to our knowledge there have been no previous studies that have determined longer term cost data that extend beyond 2 years. This is particularly important given that most health economic analyses for osteoporosis take a 5- or 10-year (or even remaining life) time horizon in determining the potential costs and benefits for new treatments.
We have previously reported the incremental first year healthcare costs associated with incident fractures in Manitoba, Canada [17]. The current analysis takes a third-party healthcare payer perspective and examines incremental costs of non-traumatic fracture (costs in the year following the fracture minus costs in the year before fracture) up to 5 years after the incident fracture event in a population-based cohort with comparison to sex- and age-matched controls.
Methods
Overview
We used the Population Health Research Data Repository held at the Manitoba Centre for Health Policy (MCHP) for the Province of Manitoba, Canada, to identify the incident fractures from April 1997 to March 2002 and healthcare costs for the year prior to the index fracture and for 5 years post-fracture for all women and men age 50 years and older who were resident in the province for 2 years prior to the date of fracture and who maintained continuous healthcare coverage (i.e., no gaps in coverage of more than 90 days) during the period of interest. Individuals who moved away from Manitoba at any time during the study or who had cancelled coverage for any reason other than death were excluded. For individuals who died partway through an observation year, costs up to the time of death were attributed to that observation year and were not otherwise prorated. In subgroup analyses, we also examined healthcare costs for individuals who were still alive 5 years post-fracture. The study was approved by the research ethics board for University of Manitoba and data access was granted by Manitoba’s Health Information and Privacy Committee.
Data sources
The administrative health databases of the Repository, which are the sources used for this analysis, contain anonymized records for almost all contacts with the publicly funded provincial healthcare system, including physicians, hospitals, home care, nursing homes and pharmaceutical dispensations [18]. The MCHP Repository covers virtually the entire population of the province as there are no insurance premiums payable by residents for their healthcare coverage. A hospital abstract is completed when a patient is discharged from an acute care facility with diagnoses and procedures coded using the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) prior to 2004 (up to 16 diagnosis codes) and the 10th revision, Canadian version (ICD-10-CA) thereafter (up to 25 diagnosis codes). Physicians submit billing claims on almost all outpatient services and most inpatient services (single ICD-9-CM diagnosis code). A computerized record of all outpatient drugs dispensed from pharmacies as well as most prescription details was available since the start date of all of our analyses [19]. Files containing data on nursing home residence (long-term care) and home care (i.e., supportive) services are also maintained for Manitoba residents. The nursing home file contains records of the number of days individuals have resided in a nursing home in Manitoba. The file also contains records of the opening dates and closing dates of all home care episodes delivered, and these were summed to provide the total number of days of home care. These data, along with per diem cost information, were used to assign costs to all individuals in the study. We have previously reported that rates of transfer to a nursing home facility in the year after fracture are increased following hip and non-hip fractures even after adjustment for age and burden of co-morbidity, with men at greater risk than women [20].
Study population
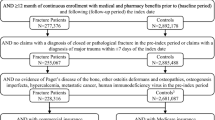
We defined as cases all men or women 50 years and older with continuous residence in Manitoba whose hospitalization records and/or physician billing claims contained an incident fracture diagnosis in the period from April 1, 1997 to March 31, 2002. The date of earliest qualifying fracture code was considered the index date. Individuals living in nursing home facilities at the time of the fracture were not excluded.
The fracture case definitions used in this analysis have been previously validated and reported [17]. Briefly, each subject’s longitudinal health service record was assessed for the presence of fracture codes (excluding craniofacial, hand and foot fractures) that were not associated with trauma as documented by trauma codes in the medical record. Specific fracture sites of interest were those of the hip, spine, wrist, and humerus. An incident fracture was identified if there was one hospitalization or two physician visits (within 3 months) with the relevant diagnosis code, provided that this was preceded by a 6-month period (washout) without any codes for the same diagnosis. To identify an incident wrist fracture we also required the presence of a site-specific physician claim for reduction, fixation or casting within 3 months. For an incident hip fracture, we required the presence of a hospitalization with a hip fracture diagnosis code and a physician claim for fracture reduction or fixation within 3 months of the index date. We grouped together all “other fractures” (including ribs/sternum, shoulder and arm, pelvis, clavicle, patella, tibia/fibula, ankle, scapula, trunk not otherwise specified, and forearm/femur fractures that did not meet the previous cases wrist/hip definitions). We did not exclude pathological fractures as they represent a small proportion of all fractures and their exclusion can lead to underestimation of the fracture burden due to osteoporosis [21]. Simultaneously occurring fractures at different sites were included if they did not result from high force trauma, and were assigned randomly to one single category from amongst the various fractures sustained by the individual. A detailed list of the codes used for each type of fracture is available from the authors.
Three controls for each case were selected and matched on fiscal year, sex, and age (within 5 years of birthdate), and were assigned the same index date as their matched case’s index fracture date. Controls were also required to have continuous health insurance coverage, starting 5 years prior to the case’s index fracture date, and to be free of fracture diagnosis codes during that period.
Healthcare resource costs
The costing methods we used are in accordance with national guidelines [22–25] and have been reported previously in detail [17]. In brief, micro-costing techniques were used for physician services and prescription and average costs were used for hospital care, home care and nursing (long-term care) homes with all costs expressed in constant dollars (2009 Canadian) using the Consumer Price Index for Manitoba health services from the Canadian Socio-Economic Information Management System (CANSIM) [26].
The physician services database records almost all encounters an individual has with a physician, both in the physician’s office and in other settings such as hospitals and nursing homes. Claims for each service provided include a code used to determine the fee that is paid to the physician. A small number of physicians who are not paid on a fee-for-service basis (about 15 %) are required to submit “shadow claims,” and these claims were included in computing physician costs using the equivalent fee-for-service value. To determine the cost of physician services for an individual, we summed the fees paid to all physicians for that individual during the given time interval.
Hospital costs were based upon the provincial average direct cost per weighted case [24]. Resource Intensity Weights (RIW™) are the relative case weights for Case Mix Groups (CMG™) used to measure the intensity of resource use (relative cost) associated with different diagnostic, surgical procedure and demographic characteristics of an individual [27, 28]. The Day Procedure Group (DPG™) is a classification system for ambulatory care provided in hospitals, most commonly surgical procedures that can be performed without the need for an overnight stay. Total direct hospital costs for each individual were calculated using the following formula: cost = average direct cost per weighted case × sum (RIW, DPG weight). Hospital costs do not include physician services, which are captured separately as described above, and also do not include costs that cannot be directly assigned to patient care (e.g., hospital administration, electricity and heating) or building capital costs (e.g., mortgages). Hospital records do not include visits to ambulatory clinics including emergency department care, and will in some cases tend to under–estimate the total costs of hospitalization.
The prescription drug cost for an individual is the total expenditure for all dispensed outpatient prescriptions for the given period of time. Inpatient drug use is not captured in this system but the total hospital costs include the cost of drugs administered while in hospital and comprise an unknown proportion of the total hospital-related costs. A similar situation arises in some nursing homes where drugs are obtained from a hospital pharmacy, but the great majority of nursing homes (about three-quarters in a given year) obtain their drugs through retail pharmacy. The pharmacy database does not capture non-prescription (over-the-counter) medication use.
The per diem for residence in a nursing home was calculated by dividing total expenditures for these facilities for a year by the total number of resident days. The cost for an individual is determined by multiplying this mean cost by the number of days that person was a nursing home resident; a similar approach was used for home care services.
Statistics
Incremental costs for fracture cases were calculated for each person as the difference in costs for each year after the fracture (up to 5 years) versus costs during the year prior to the fracture; this approach is similar to that described by Kilgore et al. [29]. Incremental costs for controls relative to the matching index date were calculated in an analogous manner. The median of these differences was computed over individuals alive at the start of that year. Data were analyzed using median values, which are less sensitive to deviations from normality, outliers and extreme costs. Mean costs are provided as an on-line supplement. A general age-related increase in healthcare utilization and costs is expected over 5 years. Therefore, to more accurately reflect fracture-associated costs, incremental increases in median total healthcare costs for controls alive at the start of each observation year were subtracted from the incremental increases in median total healthcare costs of the fracture cases alive at the start of the same observation year. In a sensitivity analysis, we restricted analyses to only those fracture cases and controls who survived for 5 years after their index fracture. This was done to explore the possibility that those who died soon after fracture were frailer and already heavy users of healthcare resources, and thus not representative of the overall post-fracture population. Population total incremental costs were calculated by summing all costs for incident fracture cases and their matched controls during the observation period. P values were not computed, and confidence intervals were not estimated since we are reporting on the entire population, and not a sample. Descriptive analyses were performed using SAS (version 9.1; SAS Institute, Cary, NC).
Role of the funding source
This study was funded through a research grant from Amgen Canada Ltd. The funding source had no access to the data prior to publication, no input into the writing of the manuscript, and no input in the decision to publish the results.
Results
Table 1 indicates the numbers of fracture cases and their matched controls available for analysis in our cohort of 64,792 subjects. A total of 11,234 women with fractures (including 1,957 hip fractures) and 4,964 men with fractures (857 hip fractures) were matched with 33,702 control women and 14,892 control men, respectively. Five years following the index date, 73 % of women with fractures (83 % of control women) and 67 % of men with fractures (80 % of control men) were still alive. Mortality was considerably greater among hip fracture cases with 51 % of women (72 % of controls) and 36 % of men (67 % of controls) alive at year 5.
Median baseline costs in the year prior to the index date are shown in Table 2. Fracture cases had higher pre-fracture costs than controls, and the disparity was greatest for hip and spine fractures. Baseline healthcare costs were also affected by survivorship. Median pre-fracture costs for all hip fracture cases were more than 3-fold the median pre-fracture costs for those who survived to 5 years after hip fracture. Median pre-fracture costs for all spine fracture cases were 1.8 times the median pre-fracture costs for those who survived to 5 years after spine fracture.
Incremental median healthcare costs for each of the 5 observation years were calculated for fracture cases and matched controls (mean costs are provided as an on-line supplement). The largest incremental costs at year 1 were seen for hip fractures ($25,306 in women and $21,396 in men) (Table 3). In the second year after hip fracture, the incremental costs declined to $4,164 in women and remained elevated at this level until year 5. Incremental median healthcare costs in men showed a progressive decline over time and by year 5 were $981 below baseline pre-fracture costs. When analysis was limited to 5-year survivors after hip fracture, there was a similar year 1 increase in incremental median costs ($27,498 in women and $20,719 in men); costs declined in year 2 ($10,030 in women and $3,743 in men) and remained above baseline pre-fracture costs out to year 5 ($12,670 in women and $7,933 in men).
Next to hip fractures, spine fractures resulted in the largest year 1 incremental costs while wrist fractures resulted in the lowest incremental healthcare costs. The only subgroup in which median incremental costs consistently exceeded $1,000 throughout the 5 years of observation were spine fractures in women (in year 5, $6,663 for all subjects and $8,373 for 5-year survivors).
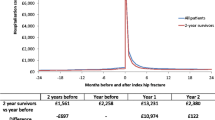
At the third-party healthcare payer level, total healthcare costs for all incident fractures combined showed a large increase over pre-fracture costs in the first year ($137 million in women, $57 million in men), but these fell progressively and were below the pre-fracture baseline in years 4–5 for women, and below the pre-fracture baseline in years 3–5 for men (Fig. 1). By year 5, total incremental healthcare costs were $14 million lower than the pre-fracture baseline for women and $20 million lower for men. In contrast, among the controls, total healthcare costs showed little change over time. Fracture site and sex influenced the change in total healthcare costs. The decline was greatest for hip fractures where total costs remained below the pre-fracture baseline from year 3 onwards in women and from year 2 onwards in men. Sex affected the persistence of total incremental healthcare costs for non-hip fractures. At year 5, total healthcare costs after non-hip fractures were $3 million above the pre-fracture baseline for women but $6 million below baseline for men. In descending order, elevated total healthcare costs of non-hip fractures in women were seen at year 5 for prior wrist ($8.2 million), humerus ($3.1 million) and spine fractures ($2.2 million), but these were somewhat offset by lower total healthcare costs for other fractures ($11.2 million below baseline).
Total incremental healthcare costs over baseline costs from a third-party healthcare payer perspective for fracture cases (solid figures and lines) and controls (open figures and dotted lines, costs for controls divided by 3 due to 1 to 3 matching). Costs are in millions of 2009 Canadian constant dollars
The breakdown in total healthcare costs is presented in Table 4 for all fracture types combined. Hospital-related expenditures accounted for the majority of the year 1 costs (51.2 % in women and 60.0 % in men). Hospital costs fell to the pre-fracture baseline in year 2 and remained at or below this level to year 5. After year 1, nursing homes were the single largest expenditure and accounted for 48.1–52.3 % of total healthcare costs in women and 41.2–43.2 % of costs in men. Nursing home costs accounted for the majority of the costs after year 1 following hip fracture (60.8–67.6 % in women and 55.9–60.3 % in men)
Discussion
Direct incremental healthcare costs for non-traumatic fractures peaked in the first year. At the third-party healthcare payer level, however, we observed that total incremental healthcare costs fell below pre-fracture levels by 5 years in both women and men. Among those who survived 5 years following a fracture, costs remained above pre-fracture levels. Therefore, the decrease in total costs after fracture should not be interpreted as resulting from a reduction in resource consumption of fracture survivors but rather as resulting from higher mortality among patients with fractures.
Most fractures, and especially hip fracture, are associated with elevated post fracture costs [30]. Median costs fell below baseline after hip fracture for all men, but remained elevated for long-term survivors. Men have higher mortality after fracture than women, particularly following hip fracture [30]. The observed differences in hip fracture costs according to 5-year survivorship is likely attributed to higher short term mortality among fracture cases who were especially frail and who were already the greatest users of healthcare (“healthy survivor bias”) — this type of bias has been observed in other settings, such as the counter-intuitive increase in mortality associated with early initiation of chronic hemodialysis [31].
Our study has implications for health-economic models of interventions for fracture prevention (e.g., medications, hip protectors) which must make long-term cost projections relying on relatively short-term published data. Indeed, it has been noted that cost-effectiveness analyses are very sensitive to the assumed or projected long-term costs of fracture [14]. For example, one proposed framework for cost-effectiveness analyses of osteoporosis is based upon a Markov model that simulates patients in 6–12 monthly cycles from start of treatment until either 100 years of age or death [32, 33], and this framework can also include treatment adherence and persistence characteristics [34]. Cost data for these models were primarily derived from questionnaires collected at baseline, 4 months and 12 months in 635 recent hip, vertebral and wrist fracture patients who survived 1 year after fracture [35]. Long-term costs after the first year for hip fractures were estimated; wrist and vertebral fractures were assumed to incur costs only in the first year after fracture, although a subsequent report from this cohort suggested that “long-term” costs for vertebral fractures remained elevated during 13–18 months [14]. Our study extends previous observations by providing direct healthcare cost data up to 5 years post-fracture, and avoids biases inherent in questionnaire based data collection.
Few people receive pharmacologic secondary prevention in the first year after a major osteoporotic fracture [36]. Population based data for Manitoba in 2008–2010 showed pharmacologic secondary prevention initiation in the first year after a non trauma major osteoporotic fracture were 12 % for women and 7 % for men [37]. The elevated direct costs of post fracture care in survivors would support an argument that more aggressive treatment policies could lead to cost savings from further fracture avoidance.
Despite its novelty and strengths, our study has several limitations. A number of these relate to the data sources that we used for analyses and have already been acknowledged. In addition, indirect costs (e.g., lost wages, informal caregiver support) have not been included in this study as the focus is on the direct cost of care for the healthcare system. Clearly, not all incremental healthcare costs are purely related to fracture care, and also reflect care required for co-morbidities contributing to fracture risk as well as unrelated conditions. An incremental costing approach attenuates but does not necessarily eliminate this concern. Another limitation to this study is that our fracture cases are limited to fractures that come to medical attention. By definition, these will result in greater costs than fractures that are undiagnosed which are also likely to be less severe. Spine fractures would be particularly susceptible to this spectrum bias, and an unknown number of hospitalized patients with back pain will not be coded as having a spine fracture or osteoporosis. Majority of spine fractures are not clinically diagnosed, but still may have health and economic implications, [38]. Some of the post-fracture costs could potentially be related to a second fracture, either affecting the same skeletal site (e.g., a second vertebral fracture) or a second site (e.g., hip fracture after a wrist fracture). In general, the limitations outlined would suggest a systematic underestimate of healthcare costs compared with the control population. Although the fracture cases were from 1997 to 2002, our findings are likely still valid as we have shown relatively very little change in first year post-fracture costs 1996–2006 (largest increase in women was for hip fracture, $13 [0.1 %] per year, and in men was for humerus fracture, $11 [0.4 %] per year) [17].
In conclusion, high direct incremental healthcare costs post-fracture are seen in the first year, but total costs from a third-party healthcare payer perspective eventually fall below pre-fracture levels. Among those who survive 5 years, however, costs remain above pre-fracture levels. Our findings suggest that economic analyses from a third-party healthcare payer perspective that do not account for the possibility of a long-term reduction in direct healthcare costs in the post-fracture population may systematically overestimate the total economic burden of fracture.
References
Kanis JA, Johnell O, Oden A et al (2000) Long-term risk of osteoporotic fracture in Malmo. Osteoporos Int 11:669–674
Melton LJ III, Chrischilles EA, Cooper C et al (1992) Perspective. How many women have osteoporosis? J Bone Miner Res 7:1005–1010
Adachi JD, Ioannidis G, Berger C et al (2001) The influence of osteoporotic fractures on health-related quality of life in community-dwelling men and women across Canada. Osteoporos Int 12:903–908
Hallberg I, Rosenqvist AM, Kartous L et al (2004) Health-related quality of life after osteoporotic fractures. Osteoporos Int 15:834–841
Abrahamsen B, van ST, Ariely R et al (2009) Excess mortality following hip fracture: a systematic epidemiological review. Osteoporos Int 20:1633–1650
Papaioannou A, Wiktorowicz ME, Adachi JD et al (2000) Mortality, independence in living and re-fracture, one year following hip fracture in Canadians. J Soc Obstet Gynaecol Can 22:591–597
Wiktorowicz ME, Goeree R, Papaioannou A et al (2001) Economic implications of hip fracture: health service use, institutional care and cost in Canada. Osteoporos Int 12:271–278
De Laet CE, van Hout BA, Burger H et al (1999) Incremental cost of medical care after hip fracture and first vertebral fracture: the Rotterdam study 1. Osteoporos Int 10:66–72
Pike C, Birnbaum HG, Schiller M et al (2010) Direct and indirect costs of non-vertebral fracture patients with osteoporosis in the US. Pharmacoeconomics 28:395–409
Shi N, Foley K, Lenhart G et al (2009) Direct healthcare costs of hip, vertebral, and non-hip, non-vertebral fractures. Bone 45:1084–1090
Mackey DC, Lui LY, Cawthon PM et al (2007) High-trauma fractures and low bone mineral density in older women and men. JAMA 298:2381–2388
Lindsay R, Burge RT, Strauss DM (2005) One year outcomes and costs following a vertebral fracture. Osteoporos Int 16:78–85
Ohsfeldt RL, Borisov NN, Sheer RL (2006) Fragility fracture-related direct medical costs in the first year following a nonvertebral fracture in a managed care setting. Osteoporos Int 17:252–258
Strom O, Borgstrom F, Zethraeus N et al (2008) Long-term cost and effect on quality of life of osteoporosis-related fractures in Sweden. Acta Orthop 79:269–280
Pike C, Birnbaum HG, Schiller M et al (2011) Economic burden of privately insured non-vertebral fracture patients with osteoporosis over a 2-year period in the US. Osteoporos Int 22:47–56
Nikitovic M, Wodchis WP, Krahn MD et al. (2012) Direct health-care costs attributed to hip fractures among seniors: a matched cohort study. Osteoporos Int
Leslie WD, Metge CJ, Azimaee M et al (2011) Direct costs of fractures in Canada and trends 1996-2006: a population-based cost-of-illness analysis. J Bone Miner Res 26:2419–2429
Manitoba Centre for Health Policy (2011) Population Health Research Data Repository. University of Manitoba: U of M — Medicine Last accessed: Nov. 11, 2012. URL: http://umanitoba.ca/faculties/medicine/units/mchp/resources/repository/health_admin.html
Kozyrskyj AL, Mustard CA (1998) Validation of an electronic, population-based prescription database. Ann Pharmacother 32:1152–1157
Morin S, Lix LM, Azimaee M et al (2012) Institutionalization following incident non-traumatic fractures in community-dwelling men and women. Osteoporos Int 23:2381–2386
Curtis JR, Taylor AJ, Matthews RS et al (2009) "Pathologic" fractures: should these be included in epidemiologic studies of osteoporotic fractures? Osteoporos Int 20:1969–1972
Shanahan M, Steinbach C, Burchill C et al (1999) Adding up provincial expenditures on health care for Manitobans: a POPULIS project. Population Health Information System. Med Care 37:JS60–JS82
Baladi JF, Canadian Coordinating Office for Health Technology Assessment (1996) A Guidance Document for the Costing Process. Health Technology Assessment, Ottawa, Canada Accessed: Nov. 11, 2012. URL: http://www.cadth.ca/media/pdf/costing_e.pdf.
Finlayson G, Reimer J, Dahl J et al. (2010) The direct cost of hospitalizations in Manitoba 2005/06. Manitoba Centre for Health Policy. Accessed: Nov. 11, 2012. URL: http://mchp-appserv.cpe.umanitoba.ca/reference/HospCost_fullreport.pdf#page=27&view=Fit.
Finlayson G, Ekuma O, Yogendran MS et al. (2010) The additional cost of chronic disease in Manitoba. Manitoba Centre for Health Policy. Accessed: Nov. 11, 2012. URL: http://mchp-appserv.cpe.umanitoba.ca/reference/Chronic_Cost.pdf.
Adam T, Koopmanschap MA, Evans DB (2003) Cost-effectiveness analysis: can we reduce variability in costing methods? Int J Technol Assess Health Care 19:407–420
Pink GH, Bolley HB (1994) Physicians in health care management: 4. Case Mix Groups and Resource Intensity Weights: physicians and hospital funding. CMAJ 150:1255–1261
Pink GH, Bolley HB (1994) Physicians in health care management: 3. Case Mix Groups and Resource Intensity Weights: an overview for physicians. CMAJ 150:889–894
Kilgore ML, Morrisey MA, Becker DJ et al (2009) Health care expenditures associated with skeletal fractures among Medicare beneficiaries, 1999–2005. J Bone Miner Res 24:2050–2055
Morin S, Lix LM, Azimaee M, Metge C, Caetano P, Leslie WD (2011) Mortality rates after incident non-traumatic fractures in older men and women. Osteoporos Int 22(9):2439–48
Rosansky SJ, Eggers P, Jackson K et al (2011) Early start of hemodialysis may be harmful. Arch Intern Med 171:396–403
Zethraeus N, Strom O, Borgstrom F et al (2008) The cost-effectiveness of the treatment of high risk women with osteoporosis, hypertension and hyperlipidaemia in Sweden. Osteoporos Int 19:81–827
Strom O, Borgstrom F, Kleman M et al (2010) FRAX and its applications in health economics—cost-effectiveness and intervention thresholds using bazedoxifene in a Swedish setting as an example. Bone 47:430–437
Strom O, Borgstrom F, Kanis JA et al (2009) Incorporating adherence into health economic modelling of osteoporosis. Osteoporos Int 20:23–34
Borgstrom F, Zethraeus N, Johnell O et al (2006) Costs and quality of life associated with osteoporosis-related fractures in Sweden. Osteoporos Int 17:637–650
Cooper C, Mitchell P, Kanis JA (2011) Breaking the fragility fracture cycle. Osteoporos Int 22:2049–2050
Leslie WD, LaBine L, Klassen P et al (2012) Closing the gap in postfracture care at the population level: a randomized controlled trial. CMAJ 184:290–296
Nevitt MC, Ettinger B, Black DM et al (1998) The association of radiographically detected vertebral fractures with back pain and function: a prospective study. Ann Intern Med 128:793–800
Acknowledgements
The authors acknowledge the Manitoba Centre for Health Policy for use of data contained in the Population Health Research Data Repository (HIPC project # 2008/2009-16). The authors also thank Mr. Mahmoud Azimaee for SAS programming support. The results and conclusions are those of the authors and no official endorsement by the Manitoba Centre for Health Policy, Manitoba Health, or other data providers is intended or should be inferred. This work was funded through a research grant from Amgen Canada Ltd. The funding source had no access to the data prior to publication, no input into the writing of the manuscript, and no input in the decision to publish the results. S.R.M. holds the Endowed Chair in Patient Health Management from the Faculties of Medicine and Dentistry and Pharmacy and Pharmaceutical Sciences (University of Alberta) and receives salary support from the Alberta Heritage Foundation for Medical Research–AIHS (Health Scholar). L.M.L. receives salary support from the University of Saskatchewan Centennial Chair Program. S.N.M. is chercheur-clinicien boursier des Fonds de la Recherche en Santé du Québec.
Conflicts of interest
William Leslie — speaker bureau: Amgen; research grants: Novartis, Amgen, Genzyme; advisory boards: Novartis, Amgen. Colleen Metge — research grant: Amgen. Lisa Lix — research grant: Amgen. Suzanne Morin — consultant to: Amgen, Novartis, Eli Lilly, Merck; speaker bureau: Amgen, Novartis; research grant: Amgen. Sumit Majumdar — none. Gregory Finlayson — none.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Leslie, W.D., Lix, L.M., Finlayson, G.S. et al. Direct healthcare costs for 5 years post-fracture in Canada. Osteoporos Int 24, 1697–1705 (2013). https://doi.org/10.1007/s00198-012-2232-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-012-2232-2