Abstract
Summary
We measured urinary N-telopeptide of type I collagen (U-NTX) to monitor response to bisphosphonates for osteoporosis. Decrease in U-NTX was associated with increase in spine bone density. A lesser response in U-NTX was more likely in those with secondary osteoporosis or with poor compliance. U-NTX may be a useful early indicator of treatment non-compliance or secondary osteoporosis.
Introduction
This study aims to determine the utility of the bone resorption marker, U-NTX, in the clinical setting, to monitor the response to bisphosphonate therapy (alendronate and risedronate) for osteoporosis.
Methods
A retrospective evaluation of data collected as part of the bone turnover marker monitoring service in the Metabolic Bone Centre, Sheffield, UK. Treatment compliance, underlying causes of osteoporosis, change in U-NTX/creatinine (Cr) at 4 months and change in spine and hip bone mineral density (BMD) by dual-energy X-ray absorptiometry were recorded. Treatment response was defined as either a change in U-NTX/Cr greater than a pre-defined least significant change (LSC) of 54 % or to within the lower half of a pre-defined pre-menopausal reference interval (≤30 nM BCE/mmol Cr).
Results
A greater decrease in U-NTX/Cr at 4 months was associated with a greater increase in spine BMD at 18 months (r = −0.33; P < 0.0001, Pearson’s correlation). The mean U-NTX/Cr at 4 months was higher in patients with secondary osteoporosis compared with those with primary osteoporosis (P < 0.01, ANOVA). A lesser response in U-NTX/Cr increased the likelihood of secondary osteoporosis or poor treatment compliance (P = 0.04, Fisher’s exact test). A lack of response in U-NTX/Cr to within the lower half of the reference interval was a better indicator of secondary osteoporosis and treatment non-compliance than a change in U-NTX/Cr greater than LSC.
Conclusions
Treatment monitoring using U-NTX/Cr has a place in clinical practice for the early identification of non-compliance or presence of secondary osteoporosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ensuring that patients adhere and persist with their medication is a major challenge with any long-term therapy. Up to 50 % of patients taking a bisphosphonate will have stopped taking their medications at 1 year, and many of these patients stop within the first 3 months [1]. Monitoring patients improves adherence and persistence with therapy which ultimately results in increased treatment effectiveness and reduced risk of fracture [2]. We have previously shown that monitoring patients in nurse-led clinics at 3-, 6- and 9-month intervals improved adherence to treatment by 57 % compared with no monitoring [3].
Response to osteoporosis therapies may be monitored objectively by examining either change in bone mineral density (BMD) or in biochemical bone turnover marker (BTM). Change in lumbar spine BMD is the method most commonly used to identify response to treatment; however, this approach has drawbacks. Firstly, the change in BMD is small compared with the precision error of the measurement, which means that changes in an individual patient can only be reliably detected after 2 years of treatment. Secondly, lumbar spine BMD measurements become increasingly unreliable with ageing and this approach cannot be interpreted reliably in a proportion of patients. BTMs, on the other hand, may have some advantages over BMD in that they show a significant response within weeks of beginning medication. The ‘signal-to-noise’ ratio is also more favourable than that of dual-energy X-ray absorptiometry (DXA) measurements [4, 5]
The largest decreases in BTMs are observed with urinary N- and serum C-terminal telopeptides of type I collagen (U-NTX and S-CTX) [6]. These markers of bone resorption are also more strongly associated with BMD response than other markers and are the most widely used in clinical practice. Bone resorption markers also show a more rapid response (within 1 month) than bone formation markers where the change becomes significant between 3 and 9 months after commencing treatment. The choice of marker in clinical practice needs to be made on pragmatic grounds. U-NTX may be the preferred marker in the clinic setting as unlike S-CTX, it is not as sensitive to circadian changes and is not affected by food intake [7]. Patients may be asked to collect second morning void urine samples at home and bring these to their hospital appointment. This avoids the requirement for patients to attend fasting and means that they may have clinic appointments at any time of day.
In clinical practice, there are two possible approaches to estimate what constitutes a treatment response using BTM: (1) a target of the lower half of the pre-menopausal reference interval or (2) a change greater than the ‘least significant change’ (LSC) [8].
The first approach requires the establishment of a robust reference interval. A reference interval is best estimated in women with a mature skeleton who have not yet reached menopause. We have developed a reference interval locally from a group of 153 healthy pre-menopausal women between the ages of 35–45 years [8]. We determined this age range to be the most suitable as BTM reach a nadir during this period.
We have previously estimated that that the LSC for urinary N-telopeptide of type I collagen corrected for creatinine (U-NTX/creatinine (Cr)) is 54 %, i.e. 95 % of repeat measurements will not exceed 54 % change [1].
The most common drugs currently used for the treatment of osteoporosis are the oral bisphosphonates (such as alendronate and risedronate). Response to bisphosphonate therapy is generally good but can be variable. Currently, if a response to treatment is not detected, we would act by (1) checking for good compliance and (2) investigating for secondary osteoporosis or (3) considering a change in treatment.
Secondary osteoporosis is common and may be due to the direct pathophysiology of a disease such as primary hyperparathyroidism or indirectly from conditions causing periods of immobilisation such as multiple sclerosis [9]. Glucocorticoid treatment may also lead to osteoporosis by its action on osteoblast activity and by decreasing calcium absorption [10, 11].
In this study, we examined data collected from patients in the clinical setting. The aims of the study were to determine (a) the proportion of patients with a response in U-NTX/Cr to bisphosphonate treatment at 4 months, (b) the association between change in U-NTX/Cr at 4 months and change in BMD at 18 months, (c) the causes and outcome of non-response, e.g. presence of poor compliance or secondary osteoporosis and (d) the proportion of clinical patients in whom BMD by DXA results are uninterpretable.
Subjects and methods
Study design
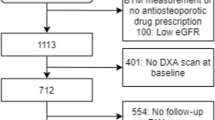
This was a retrospective evaluation of the BTM monitoring service in Sheffield, UK. Study subjects were 200 patients who attended the Metabolic Bone Centre (MBC), Northern General Hospital, Sheffield, between 1st April 2004 and 31st October 2009.
Approximately 650 patients/month attend the MBC for evaluation of fracture risk. Most patients are referred by the general practitioner (GP) or from the orthopaedic fracture clinic. A small number are referred by other secondary care departments. Patients undergo a clinical evaluation which includes completion of a baseline questionnaire, assessment of BMD by DXA and spinal radiographs if necessary. Around 85 % of patients are referred back to their GP with management advice and the remainder, with more severe or complicated osteoporosis, return to the physician-led clinics for further investigation and treatment. This group includes patients with vertebral fractures, those with low BMD for age (Z-score below −2) and those with unexplained bone loss. Patients treated in the physician-led clinics are routinely monitored using BTM. Subjects for this analysis were identified through a database held by the MBC. We identified 200 subjects who met the inclusion/exclusion criteria and were included in this analysis.
The study subject inclusion criteria were: no previous treatment for osteoporosis (excluding calcium and vitamin D or oestrogen replacement therapy); osteoporosis or osteopenia requiring treatment; patients who were about to commence either alendronate or risedronate therapy; patients with a baseline U-NTX/Cr measured after 31st March 2004 (after the introduction of triplicate pooled urine samples into the clinical service); and a follow-up BMD by DXA scan by 1st November 2009.
The study subject exclusion criteria were: previous bisphosphonate treatment; the current use of an osteoporosis treatment; absence of a baseline measurement; measurements that were carried out in laboratories other than the Clinical Chemistry laboratory at the Northern General Hospital, Sheffield; and absence of a follow-up BMD by DXA scan.
As part of the usual clinical monitoring procedure for the MBC, urine samples for measurement of U-NTX/Cr are collected at several time points as follows:
-
Before attending the clinic (when patients attend for investigation for underlying causes of osteoporosis)
-
At the first physician clinic visit
-
At the nurse clinic after 4 months on treatment
-
At the nurse clinic after 7 months on treatment (if the response to treatment at 4 months is poor).
With the exception of the first pre-clinic measurement, all U-NTX/Cr measurements were performed on a pooled sample of three second morning void samples collected between 0900 and 1100 hours as we have previously found this approach to reduce variability by between 20 and 61 % [12].
The U-NTX measurements were carried out in the NHS Clinical Chemistry laboratory at the Northern General Hospital, Sheffield. Measurements of U-NTX and Cr were performed using the Ortho-Clinical Diagnostics, Vitros ECi autoanalyser (Johnson & Johnson, New Brunswick, NJ). The measurement is expressed as a ratio of U-NTX to Cr. The intra-assay coefficient of variation (CV) for this assay was between 1.1 and 6.7 %, and the inter-assay CV was between 3.8 and 6.1 %.
A value for LSC of 54 % was derived from previously published data [1] using the formula: \( {\text{LSC}} = 1.96 \times \surd 2 \times {\text{CV}} \), where CV is the CV calculated from the standard deviation of the measurement divided by the population mean. The target response of the lower half of the pre-menopausal reference interval (≤30 nMBCE/mmol Cr) was derived from previously published data from women living in Sheffield [8].
BMD measurements were performed by DXA (Hologic Discovery A or C, Bedford, MA) at the lumbar spine and hip. Serial measurements for each patient were performed using the same densitometer. Instrument stability was monitored using daily measurements of a semi-anthropomorphic hydroxyapatite phantom. A value for LSC for change in BMD of 4.5 % was derived from previously published data [13]. All DXA spine and hip scans were scrutinised before being regarded as being of sufficient quality for inclusion in the analysis. DXA scans were considered to be unsuitable for this analysis according to the criteria presented in Table 1.
Treatment compliance was established qualitatively at the monitoring visit by asking the patient an open question to describe how they were taking their medication. Further direct questioning was used to define the nature and extent of sub-optimal compliance and enable the nurse practitioner to form a clinical judgement of whether there was a problem with compliance likely to affect the clinical response to treatment. Poor compliance was defined as (1) failing to take treatment on a weekly basis, which included patients who had stopped treatment altogether and those who missed more than 1 tablet/month and (2) taking treatment incorrectly, which included patients who had not fasted prior to taking their bisphosphonate, those who took their tablet with a beverage other than tap water and those who took calcium-containing supplements shortly after the bisphosphonate.
Statistical methods
Statistical analyses were performed using SPSS v16.0 (SPSS Inc, Chicago, IL) and GraphPad Prism (GraphPad Software Inc, La Jolla, CA). Log transformation or non-parametric testing was used for analysis of skewed data. Association between change in U-NTX/Cr and change in BMD was assessed by Pearson’s correlation after log transformation of the U-NTX/Cr data. The association between treatment compliance and U-NTX/Cr response was assessed by Fisher’s exact test. The association between diagnosis and U-NTX/Cr response was assessed by Chi-square test. Unpaired t tests were used to compare unpaired data. A P value of less than 0.05 was considered to be significant.
Results
The demographics of the 200 participating subjects are shown in Table 2. We identified 161 women and 39 men who met the inclusion/exclusion criteria. The age of the men (66; range, 32–86 years) was lower than that of the women (69; range, 50–91 years), but this was not statistically significant (P = 0.08, unpaired t test). Four patients were changed to alternative intravenous bisphosphonate therapies at 4 months due to poor compliance or side effects of oral therapy. These patients were not included in the BMD analysis.
Secondary osteoporosis was identified in 35 % of patients (15 % due to glucocorticoid use and 20 % due to other causes). Causes other than glucocorticoid use included coeliac disease (either poorly controlled or undiagnosed), rheumatoid arthritis, primary and secondary hyperparathyroidism and the use of medications such as phenytoin. Seven patients were diagnosed with primary hyperparathyroidism: two patients underwent surgery between the 4- and 18-month follow-up visits, one received surgery before attending the clinic, one patient declined surgery and the remainder were treated conservatively. Baseline U-NTX/Cr was higher in patients with an underlying cause of osteoporosis other than glucocorticoid use compared with those with primary osteoporosis (60.8 vs. 46.1 nM BCE/mmol Cr; P < 0.01, ANOVA).
Response in U-NTX/Cr to bisphosphonate treatment at 4 months
Using the target of the lower half of the reference interval, after 4 months of alendronate or risedronate therapy, 81 % of patients could be classified as ‘responders’. Using a U-NTX/Cr response of greater than LSC as the target response, 53 % could be classified as responders; 45 % of patients met both criteria for response whilst seven patients (3.5 %) showed no response.
Uninterpretable BMD by DXA results
Spine DXA scans were uninterpretable in 28 (14 %) of the 200 patients. Reasons included presence of severe scoliosis, vertebral fractures, extensive degenerative changes, change in weight between scans and incorrect positioning. Hip DXA scans were either not done or were not interpretable in seven (3.5 %) due to the presence of total hip replacement, increase in weight or poor positioning.
Association between change in U-NTX/Cr at 4 months and change in BMD at 18 months
Figure 1 shows the relationship between change in spine BMD at 18 months and change in U-NTX/Cr at 4 months in response to risedronate or alendronate. There was a significant inverse correlation between change in spine BMD and change in U-NTX/Cr (r = −0.33; P < 0.0001, Pearson’s correlation). In addition, 70 % of patients with a decrease in U-NTX/Cr of >54 % subsequently had an increase in spine BMD of greater than 4.5 %. Patients meeting both criteria (i.e. U-NTX/Cr of >54 % and U-NTX/Cr of ≤30 nM BCE/mmol Cr) had a greater percentage increase in spine BMD than those meeting one or no response criteria (+7.00 ± 0.57 vs. +3.86 ± 0.64 %; P = 0.0003).
The relationship between change in U-NTX/Cr at 4 months with change in spine BMD at 18 months. The vertical broken line shows the least significant change for U-NTX/Cr (54 %) and the horizontal broken line shows the least significant change for spine BMD (4.5 %). The number of patients responding by U-NTX/Cr change was 105 (52.5 %); the number by BMD change was 100 (50 %). The upper left shaded area shows the number of patients who responded by both U-NTX/Cr and spine BMD (64, 32 %)
There was no significant association between change in U-NTX/Cr and change in hip BMD. This is not surprising in light of the fact that the magnitude of change in response to treatment with anti-resorptive agents is typically smaller at the hip in comparison to the spine [14] and that BMD measurement at the hip is somewhat less precise than that at the spine [11]. Furthermore, patients meeting both criteria for U-NTX/Cr response did not have a significantly greater increase in hip BMD (data not shown).
Causes and outcome of non-response
When we examined the impact of the initial diagnosis, we observed no difference in the percentage of patients who responded to therapy using the LSC criterion (primary osteoporosis, 54 %; secondary osteoporosis, 50 %; and glucocorticoid-induced osteoporosis (GIOP), 57 %). U-NTX/Cr was greater than 30 nM BCE/mmol Cr after 4 months bisphosphonate treatment in 33 % of patients with secondary osteoporosis. This compared with 15 % of patients with primary disease and 20 % of patients with GIOP (P = 0.04, Chi-square test) (Table 3). The mean U-NTX/Cr at 4 months was higher in patients with secondary osteoporosis compared with primary osteoporosis. However, mean U-NTX/Cr at 4 months in patients with GIOP was not different to primary or secondary osteoporosis (Fig. 2).
Box and whisker plots to show the absolute values of U-NTX/Cr at 4 months. There was a significant difference in U-NTX/Cr between patients with primary and secondary osteoporosis (**P < 0.01). The shaded area shows the pre-menopausal reference interval; the geometric mean is indicated with a dotted line
On the basis of the 4-month assessment, 23 patients were given further advice about the correct way to take treatment and/or correction of reversible underlying causes such as additional vitamin D supplementation. They were reviewed again after a further 3 months. At the 7-month review, 13 of 23 had a U-NTX/Cr of <30 nM BCE/mmol Cr and 9 of 23 had a change in U-NTX/Cr which exceeded the LSC in comparison to the pre-treatment level. Eight patients showed response by both criteria, six responded by one criterion and nine were complete non-responders. Management at that stage depended on the individual circumstances and involved, for example, surgical intervention for primary hyperparathyroidism; continued use of first-line treatment for compliant patients with an underlying cause of their osteoporosis; and change in treatment for persistent non-compliers.
Impact of fracture on monitoring response
There were 23 patients who had sustained a fracture in the year prior to baseline. They had higher baseline U-NTX/Cr in comparison to those without fracture (68 vs. 47 nM BCE/mmol Cr; P < 0.001) but at 4 months there was no significant difference in the proportion of responders between those with and without fracture (proportion of <30 nM BCE/mmol Cr, 74 vs. 82 %; mean decrease in U-NTX, 59 vs. 49 %). Four patients experienced an incident fracture between their baseline measurement and the 4-month measurement (three of digits and one vertebral). All four of these patients were classified as responders at 4 months by both criteria.
Compliance
Poor compliance was observed in 22 (11 %) of our patients. Patients assessed as having poor compliance had a higher U-NTX/Cr at the 4-month follow-up visit than those who had good compliance (27.2 vs. 22.5 nM BCE/mmol Cr; P = 0.05). The proportion of patients with poor compliance who were defined as responders was lower than the proportion among patients who had good compliance (proportion of <30 nM BCE/mmol Cr, 64 vs. 83 % (P = 0.04); proportion with U-NTX change greater than LSC, 36 vs. 54 % (P = 0.01), Fisher’s exact test) (Table 4).
Discussion
The overall aim of this study was to determine the usefulness of bisphosphonate treatment monitoring using U-NTX/Cr in the clinical setting. There has been only one previous report describing the utility of BTM in clinical practice. Eekman et al. [15] observed that 81 % of a small cohort of 31 patients commencing osteoporosis treatment had a decrease greater than the LSC in both S-CTX and S-PINP at 3 months. In a further cross-sectional evaluation of 95 patients (including the 31 in the prospective analysis), they observed that levels of S-CTX and S-PINP after 3 months of bisphosphonate treatment were below the pre-menopausal mean in 95 % of their cohort. Our study adds to this clinical evaluation by showing data for another BTM in a larger cohort of patients. This has enabled us to examine the impact of underlying causes and poor compliance in more detail and to evaluate the relationship of the change in BTM to the change in BMD.
We found that about one half of patients (53 %) had a decrease in response to bisphosphonate greater than the LSC of 54 % after 4 months of treatment. This is similar to the data presented in the fosamax actonel comparison trial (FACT) [14]. In the FACT study, a lower LSC of 40 % was used for U-NTX/Cr, and the follow-up period was 12 months; 67 % of alendronate-treated patients and 49 % of risedronate-treated patients were responders. Given the different duration and the smaller LSC, these response rates may be regarded as being similar to ours. In this study, a greater proportion of patients (81 %) had values for U-NTX/Cr in the lower half of the reference range after 4 months compared with those having a response greater than LSC after 4 months. The higher proportion of patients exceeding LSC and with 3-month values below the pre-menopausal mean in Eekman’s analysis is likely to be explained by the use of serum-based markers with a smaller CV [15]
We found that the U-NTX/Cr response to alendronate and risedronate at 4 months was weakly associated with change in spine BMD (but not total hip BMD) at 18 months (r = −0.33). A previous study reported the 6-month change in U-NTX/Cr in response to alendronate was related to change in total hip BMD (r = −0.34) but not spine BMD over 3 years [16]. The finding of only modest association between changes in BMD and changes in BTM is not surprising in view of the considerable variability in both types of measurement which are being used as a surrogate for the outcome of interest, namely change in fracture risk, which cannot be determined directly.
In this study, secondary osteoporosis was associated with higher U-NTX/Cr at follow-up which is a novel observation. The causes of secondary osteoporosis included primary hyperparathyroidism, and bisphosphonates do reduce bone turnover in these patients [17]. In one randomised controlled trial of alendronate in patients with primary hyperparathyroidism, the mean urinary NTX/Cr ranged between 30 and 50 nmol BCE/mmol Cr higher than that found in patients with primary osteoporosis treated with alendronate [14]. However, in another major clinical trial of alendronate in patients with primary hyperparathyroidism, U-NTX/Cr decreased by a mean value of 66 % [18]. In this study, we observed a significant difference in U-NTX/Cr at 4 months between patients with primary and various causes of secondary osteoporosis (21.2 vs. 28.5 nMBCE/mmol Cr; P < 0.05).
The occurrence of a fracture in the months prior to commencement of treatment or between the time of the baseline and monitoring measurements might be anticipated to increase or decrease the apparent BTM response to treatment, respectively. However, in this evaluation, we did not find a significant effect of fracture. Those patients with fracture within a year before treatment did have higher baseline BTM values, and there was a trend for a greater mean decrease in U-NTX between baseline and 4 months but this did not result in a higher proportion of patients being classified as responders. Furthermore, the occurrence of fractures between the baseline and 4-month measurements did not lead to a diagnosis of non-response. Fracture is however an important consideration in the interpretation of BTM measurements and fracture of a large bone might be expected to impair the ability to monitor that individual using BTM.
Treatment compliance is an important issue when considering the effects of long-term therapies. In this study, poor compliance was associated with higher U-NTX/Cr after 4 months of therapy. We have previously reported that poor compliance with raloxifene (assessed by electronic caps) is associated with poorer NTX response to treatment over 12 months [3]. Our data suggest that the target of the lower half of the reference interval appears to be a better indicator of treatment compliance than use of LSC.
As we were evaluating retrospective data collected in the clinical setting rather than from a controlled research study, certain limitations of these data should be acknowledged. Our patient population consisted of both men and women but the thresholds for LSC and references intervals were derived from studies of women alone. However, our aim was to determine the usefulness of monitoring with U-NTX/Cr in the clinical setting using the available background reference data, and as yet there are no data for change in U-NTX/Cr and change in fracture risk in men. We observed a lesser response in U-NTX/Cr in those patients who went on to have a lesser response in BMD. This association may have been underestimated as a poor response in U-NTX at 4 months led to further intervention and possible improved response in BMD.
In summary, in this clinical evaluation, we have shown that measurements of U-NTX/Cr in patients treated with alendronate or risedronate may be a useful early indicator of the presence of underlying causes of osteoporosis or poor compliance. In the evaluation of treatment response, it may be helpful to consider whether the U-NTX/Cr value lies within the lower half of the pre-menopausal reference interval and also whether there has been a change in U-NTX/Cr greater than the LSC.
References
Eastell R (2003) Bone turnover markers: their place in the investigation of osteoporosis. In: Orwoll E, Bliziotes M (eds) Oteoporosis. Pathophysiology and clinical management. Contemporary endocrinology. Humana, Totowa, pp 185–197
Seibel MJ (2006) Biochemical markers of bone turnover part II: clinical applications in the management of osteoporosis. Clin Biochem Rev 27:123–138
Clowes JA, Peel NF, Eastell R (2004) The impact of monitoring on adherence and persistence with antiresorptive treatment for postmenopausal osteoporosis: a randomized controlled trial. J Clin Endocrinol Metab 89(3):1117–1123
Braga de Castro Machado A, Hannon R, Hannon R, Eastell R (1999) Monitoring alendronate therapy for osteoporosis. J Bone Miner Res 14(4):602–608. doi:10.1359/jbmr.1999.14.4.602
Rogers A, Glover SJ, Eastell R (2009) A randomised, double-blinded, placebo-controlled, trial to determine the individual response in bone turnover markers to lasofoxifene therapy. Bone 45(6):1044–1052. doi:10.1016/j.bone.2009.07.089
Delmas PD, Eastell R, Garnero P, Seibel MJ, Stepan J (2000) The use of biochemical markers of bone turnover in osteoporosis. Osteoporos Int 11:2–17
Henriksen DB, Alexandersen P, Bjarnason NH, Vilsboll T, Hartmann B, Henriksen EE, Byrjalsen I, Krarup T, Holst JJ, Christiansen C (2003) Role of gastrointestinal hormones in postprandial reduction of bone resorption. J Bone Miner Res 18(12):2180–2189. doi:10.1359/jbmr.2003.18.12.2180
Glover SJ, Garnero P, Naylor K, Rogers A, Eastell R (2008) Establishing a reference range for bone turnover markers in young, healthy women. Bone 42(4):623–630. doi:10.1016/j.bone.2007.12.218
Kelman A, Lane NE (2005) The management of secondary osteoporosis. Best Pract Res Clin Rheumatol 19(6):1021–1037. doi:10.1016/j.berh.2005.06.005
Kaufman JM, Goemaere S (2008) Osteoporosis in men. Best Pract Res Clin Rheumatol 22(5):787–812. doi:10.1016/j.beem.2008.09.005
Kok C, Sambrook PN (2009) Secondary osteoporosis in patients with an osteoporotic fracture. Best Pract Res Clin Rheumatol 23(6):769–779. doi:10.1016/j.berh.2009.09.006
Clowes JA, Peel NFA, Blumsohn A, Gossiel E, Eastell R (2004) Can multiple measurements or pooled measurements reduce within subject variability? J Bone Miner Res 19(10):S375–S375
Patel R, Blake GM, Rymer J, Fogelman I (2000) Long-term precision of DXA scanning assessed over seven years in forty postmenopausal women. Osteoporos Int 1:68–75
Sebba AI, Bonnick SL, Kagan R, Thompson DE, Skalky CS, Chen E, de Papp AE, Fosamax Actonel Comparison Trial i (2004) Response to therapy with once-weekly alendronate 70 mg compared to once-weekly risedronate 35 mg in the treatment of postmenopausal osteoporosis. Curr Med Res Opin 20(12):2031–2041
Eekman DA, Bultink IEM, Heijboer AC, Dijkmans BAC, Lems WF (2011) Bone turnover is adequately suppressed in osteoporotic patients treated with bisphosphonates in daily practice. BMC Musculoskelet Disord 12:167. doi:10.1186/1471-2474-12-167
Greenspan SL, Beck TJ, Resnick NM, Bhattacharya R, Parker RA (2005) Effect of hormone replacement, alendronate, or combination therapy on hip structural geometry: a 3-year, double-blind, placebo-controlled clinical trial. J Bone Miner Res 20(9):1525–1532. doi:10.1359/JBMR.050508
Lewiecki EM (2010) Management of skeletal health in patients with asymptomatic primary hyperparathyroidism. J Clin Densitom 13(4):324–334. doi:10.1016/j.jocd.2010.06.004
Khan AA, Bilezikian JP, Kung AW, Ahmed MM, Dubois SJ, Ho AY, Schussheim D, Rubin MR, Shaikh AM, Silverberg SJ, Standish TI, Syed Z, Syed ZA (2004) Alendronate in primary hyperparathyroidism: a double-blind, randomized, placebo-controlled trial. J Clin Endocrinol Metab 89(7):3319–3325. doi:10.1210/jc.2003-030908
Acknowledgements
IB was assisted by the clinical staff at the Metabolic Bone Centre and research support staff at the NIHR Musculoskeletal Biomedical Research Unit, Sheffield. IB’s studentship was funded by Inverness Medical, UK. This work was supported by the NIHR-funded Sheffield Musculoskeletal Biomedical Research Unit. Authors would like to acknowledge the assistance of the Editorial Board of the Musculoskeletal Biomedical Research Unit for preparing and reviewing the manuscript. The views expressed in this publication are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Baxter, I., Rogers, A., Eastell, R. et al. Evaluation of urinary N-telopeptide of type I collagen measurements in the management of osteoporosis in clinical practice. Osteoporos Int 24, 941–947 (2013). https://doi.org/10.1007/s00198-012-2097-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-012-2097-4