Abstract
Background:
Osteoporosis is characterized by microarchitectural disruption of the bone, decrease in bone mineral density, and increased skeletal fragility and risk of fracture. Osteoporosis occurs due to the decoupling of bone formation and bone resorption, with a significant increase in resorption. This review article focuses on the role of laboratory investigations in the diagnosis and monitoring of treatment in patients with osteoporosis.
Methods:
This review article collected literature from various databases using keywords such as ‘Laboratory investigations’, ‘Osteoporosis’, ‘Diagnosis’, ‘Monitoring’, and ‘Bone turnover markers’.
Results and Discussion:
Laboratory investigations, including serum calcium, alkaline phosphatase, vitamin D, and parathormone, are commonly performed tests to exclude secondary causes of osteoporosis and monitor the response to therapy. The biochemical markers of bone turnover are newly emerged tests for monitoring individual patients with osteoporosis. These markers are classified as bone formation and resorption markers, measurable in both serum and urine. The use of these markers is limited by biological and analytical variability. The International Federation of Clinical Chemistry and Laboratory Medicine and the International Osteoporosis Foundation recommend serum procollagen type 1 amino-terminal propeptide as the bone formation marker and β-form of C-terminal cross-linked telopeptide of type I collagen (β-CTx-1/β-CrossLaps) as the marker of choice, using standardized procedures. However, in specific cases, such as patients with chronic renal disease, CTx-1 is replaced by the resorption marker tartrate-resistant acid phosphatase 5b, as its levels are not affected by renal excretion.
Conclusion:
Bone turnover markers have emerged as tools for the assessment of osteoporosis, using standardized procedures, and are useful in monitoring therapy and treatment compliance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a condition marked by microarchitectural disruption, decreased bone mineral density, and increased skeletal fragility and fracture risk. Generalized osteoporosis may occur as either a primary condition or as a secondary manifestation of various underlying conditions (Table 1) [1]. Senile and post-menopausal are the most common forms of primary osteoporosis. Radiological investigations such as dual-energy X-ray absorptiometry (DEXA) are usually used for the initial work-up of osteoporosis, which provide static measures such as bone quantity and are limited by the fact that they reflect the effects of changes in the past. Laboratory investigations, such as bone markers, are dynamic measures that provide real-time information on bone status, including whether there is bone matrix loss or new bone formation. Laboratory evaluation is typically performed for post-menopausal women or men above 50 years of age who are at risk of osteoporosis fracture and falls. The laboratory investigations are important in differentiating primary and secondary causes of osteoporosis, in choosing appropriate therapy, and to monitor therapy [2].
The basic investigations performed for all forms of osteoporosis include complete blood counts (CBC), serum and 24-h urinary calcium, serum phosphate, parathormone (PTH), 25-hydroxy vitamin D (25(OH)D), and liver function tests including alkaline phosphatase (ALP).
The significance of each laboratory investigation is outlined in the following sections:
CBC may reveal anemia or multiple myeloma. Although anemia is not related to osteoporosis, it may indicate malnutrition.
Serum calcium has a significant role in bone metabolism. The normal serum calcium level in adults ranges from 8 to 10 mg/dl. Adequate dietary intake is required to maintain calcium levels, and the recommended daily intake of calcium for individuals aged 10–25 years is 1000–1200 mg/day [5]. Approximately 50% of the serum calcium in circulation is present as free-ionized calcium and 40% is bound to proteins such as albumin (80%) and globulin (20%). The remaining 10% comprises small diffusible inorganic and organic anions such as calcium lactate, calcium bicarbonate, and calcium citrate. Several factors influence the total serum calcium levels such as serum pH, and the levels of immunoglobulins and albumin. Hypoalbuminemia can cause falsely decreased calcium levels. The calcium concentration is regulated by PTH and vitamin D levels.
The total serum calcium level is measured using the spectrophotometric method and ionized calcium levels are measured using the ion-specific electrode method [6]. Elevated serum calcium levels suggest primary hyperparathyroidism or malignancy, and decreased serum calcium levels are indicative of malnutrition or malabsorption such as in celiac disease [7].
The 24-h urinary calcium excretion varies depending on the dietary changes. In non-fasting conditions, both genders can excrete up to 300 mg calcium/24 h in the urine, while in fasting conditions, the excretion is typically < 200 mg/24 h. Low urinary calcium (< 50 mg/24 h) suggests malnutrition or malabsorption. Conversely, a high urinary calcium (> 300 mg/hr) is indicative of hypercalciuria.
Hypercalciuria can occur due to three reasons:
-
1.
Renal calcium leak, seen commonly in males with osteoporosis.
-
2.
Decreased absorption by renal tubules, either of idiopathic nature or due to increased vitamin D.
-
3.
Malignancies such as multiple myeloma or disorders associated with elevated bone turnover such as hyperparathyroidism, Paget’s disease, or hyperthyroidism.
Urine calcium should be normalized to glomerular filtration and hence serum and urinary creatinine levels are also measured to estimate the calcium creatinine ratio. Urinary calcium concentration > 0.16 mg/100 mL GF is generally indicative of osteoclastic bone resorption. Therefore, it serves as a useful marker in the evaluation of high-turnover osteoporosis [6].
Phosphorus/phosphate is primarily stored (85%) in teeth and bones, with only 1% being found in the extracellular fluid. It is a component of cell membrane structure and ATP. Phosphorus and calcium make up hydroxyapatite, a major structural component of bone. PTH and vitamin D regulate its metabolism. Phosphate concentration levels can be assessed in both urine and serum. Phosphorus levels may be decreased in hyperparathyroidism and increased in chronic renal disease [7].
Parathormone (PTH) is a single-chain polypeptide consisting of 84 amino acids produced by the parathyroid gland. It plays a key role in calcium homeostasis (Fig. 1). Intact PTH, the biologically active hormone, exerts its action mainly on bone and kidney, independent of the glomerular filtration rate. Low plasma calcium stimulates PTH secretion, leading to the mobilization of stored calcium from the skeleton. In addition, it increases calcium absorption from the intestine by promoting the 1,25-dihydroxy vitamin D (1,25(OH)2D) synthesis in renal tubules. It also enhances calcium reabsorption from the ascending loop of Henley and facilitates the excretion of phosphorus. PTH serves as a major regulator of bone remodeling and osteoclast activity [8].
Calcium homeostasis [9]. PTH parathormone, ECF extracellular fluid
Hyperparathyroidism, a disorder characterized by increased PTH levels, is classically associated with hypercalcemia. Elevated PTH levels result in the upregulation of Receptor Activator of Nuclear Factor Kappa-B Ligand (RANKL), with subsequent activation of osteoclasts and increased bone resorption. This may be associated with osteopenia and osteoporosis, usually affecting the peripheral skeleton [10].
Vitamin D, a fat-soluble steroid prohormone, is mainly produced in the skin from 7-dehydrocholesterol, while only 10–20% is obtained through dietary sources such as fish, milk products, and fortified foods. Vitamin D2 (ergocalciferol) and vitamin D3 (cholecalciferol) are the two common forms of vitamin D. Vitamin D promotes intestinal absorption of calcium and phosphates. It is converted to 1,25(OH)2D (calcitriol), the biologically active form through hydroxylation reaction. Vitamin D undergoes conversion to 25(OH)D in the liver and further hydroxylation to 1,25(OH)2D occurs mainly in the proximal renal tubules of kidneys. The major storage form of vitamin D present in the blood is 25(OH)D, which has a half-life of 2–3 weeks. In contrast, the active form, 1,25(OH)2D, has a shorter circulating half-life of approximately 4 h [9].
The measurement of vitamin D involves assessing the two forms, 25(OH)D and 1,25(OH)2D. They are typically analyzed using chemiluminescence or liquid chromatography–mass spectrometry.
-
25(OH)D is considered the analyte of choice for measuring vitamin D levels [9]. Measuring both the vitamin D forms (total vitamin D) is useful for the assessment of bone health and growth, diagnosing vitamin D deficiency and hypervitaminosis, and monitoring patients on vitamin D supplements.
-
1,25(OH)2D test is useful in assessing calcium metabolism in subjects with hypercalcemia, renal failure, or those undergoing dialysis.
Vitamin D deficiency is associated with reduced calcium absorption, impaired calcium balance, and a compensatory elevation in PTH, resulting in excessive bone resorption.
Total alkaline phosphatase (ALP), a homodimeric protein with phosphorylating properties, occurs in numerous isozyme forms. The primary isoenzymes found in the bloodstream (serum) originate from the liver and bone (BSAP). Under physiological conditions, BSAP adheres to osteoblastic membrane with minimal quantities in serum and the levels increase only with bone remodeling. In the evaluation of osteoporosis, total ALP is nonspecific, as it cross-reacts with liver isoforms and can be mildly elevated in patients with fractures. Increased serum aminotransaminases, ALP, and gamma-glutamyl transferase may indicate underlying alcohol abuse. Elevated ALP with normal calcium and phosphate should prompt consideration of Paget’s disease [11].
Laboratory investigations help in differentiating primary osteoporosis from secondary causes. The serum phosphate, calcium, and ALP levels are usually normal in persons with primary osteoporosis. Besides the basic investigations, further testing can be conducted based on the findings to rule out secondary causes of osteoporosis (Table 2).
Bone Turnover Markers in Osteoporosis
Bone turnover markers (BTMs) serve as biochemical markers of continuous bone formation and resorption, which occurs at various sites in the bone during the process of remodeling. This remodeling process of the bone is tightly balanced in response to the biomechanical stress and plays a role in the repair of microfractures (Fig. 2). Osteoporosis occurs when there is imbalance in bone formation and resorption, which can be measured using biochemical reactions. BTMs are currently not recommended for the diagnosis of osteoporosis but are used for monitoring the patient on osteoporosis therapy.
Bone turnover markers in the management of osteoporosis [2, 11, 13]. BSAP, serum bone-specific alkaline phosphatase; OC, osteocalcin; C1NP or P1NP, serum type 1 procollagen (C-terminal/N-terminal); TRAP5b, tartrate-resistant acid phosphatase 5b; NTx-1, amino-terminal cross-linked telopeptide of type I collagen; PYD, pyridinoline; CTx-1, carboxy-terminal cross-linked telopeptides of type I collagen; DPD, deoxypyridoline; OPG, osteoprotegerin; RANKL+, receptor activator of nuclear factor kappa B ligand
The various biochemical markers can be analyzed in blood and urine samples. These markers show variable sensitivity and specificity in the assessment of bone formation and resorption, and are classified as depicted in Fig. 3 [14].
Regulators of bone turnover are currently not being used in clinical diagnosis due to analytical and biological variability and are still in the research phase [2].
The most sensitive markers of bone formation are serum osteocalcin, BSAP, and P1NP, while β-CTx-1/β-Cross Laps and NTx-1 are markers of bone resorption.
Bone Formation Markers
These markers are enzymes or by-products released by the active osteoblasts during the various stages of their development [2]. They are briefly described in the sections provided below:
-
a.
Osteocalcin, a non-collagenous, hydroxyapatite-binding protein with a molecular weight of 5800 Daltons, is composed of 49 amino acids. It is also known as bone γ-carboxyglutamic protein, as it has γ-carboxyglutamic acid residues. It is secreted by mature osteoblasts, hypertrophic chondrocytes, and odontoblasts [12]. Elevated osteocalcin is seen in high bone turnover conditions and is a specific marker of bone formation with a low within-person variation. However, there are limitations to its use including rapid degradation in serum, follows circadian rhythm, and significant variations with the menstrual cycle, renal function, and vitamin K levels.
-
b.
Bone-specific alkaline phosphatase (BSAP) is an enzyme anchored to the osteoblast cell membrane and has vital function in osteoid formation and primary mineralization. The enzyme is active at alkaline pH and it is antigenically distinct from other isoforms of ALP such as liver and placental ALP. Immunoassays have been developed to measure the bone-specific isomer of ALP, which has better specificity and sensitivity, compared to the measurement of the total ALP. BSAP is unaffected by renal function and serves as a valuable bone formation marker for the management of osteoporosis in cases with chronic renal failure [14]. A high BSAP, with levels above the biological reference interval, may be helpful in excluding the presence of a dynamic bone disease. However, other causes of increased BSAP must be ruled out, as it can also be elevated in other conditions such as hyperparathyroidism, Paget’s disease, recent fracture, or osteomalacia, which can lead to elevations of BSAP.
-
c.
Propeptides of type 1 collagen have a significant role in bone formation. More than 90% of bone matrix is composed of type 1 collagen, which is derived from type 1 procollagen, synthesized by proliferating osteoblasts and fibroblasts. The N- and C-terminal extensions of procollagen are removed by specific proteases during the synthesis of collagen-1. These extensions are subsequently incorporated into bone matrix. The amino-terminal of type I collagen (P1NP) and carboxy-terminal propeptide of type I collagen (P1CP) are peptides formed by the posttranslational cleavage of type I procollagen molecules by proteases at N- and C-terminals, respectively.
Propeptides of type 1 collagen amino-terminal (P1NP) and propeptides of type 1 collagen C-terminal (P1CP) are markers of bone formation. These peptides have low affinity to remain in the bone matrix and are secreted into the plasma. Hence, the amount detected in the blood corresponds directly to the osteoid-producing activity of the osteoblast. P1NP is preferred over P1CP, as P1CP has high biological variation due to its short half-life and is influenced by growth hormone and thyroid hormone [15].
P1NP has been recommended by the Bone Marker Standards Working Group and the International Osteoporosis Foundation (IOF) as the preferred bone formation marker considering its several functional advantages, predictable response to treatment, and reliability [15]. It has low interindividual variability, smaller circadian variation, and relatively good stability in serum at room temperature. Current immunoassays can detect the trimeric intact form or have the potential to detect both the fractions, i.e., trimeric intact and monomeric forms referred to as total P1NP assays (automated electrochemiluminescence assay by Roche) [16].
Bone Resorption Markers
These markers are by-products released by osteoclasts in the process of bone resorption and remodeling. They are usually collagen breakdown products but include non-collagenous matrix protein (BSA) or osteoclast-specific enzymes such as TRAP5b [13].
-
a.
Urinary hydroxyproline, a component of bone collagen, is released in both free and bound forms into the bloodstream and subsequently excreted through urine. Hydroxyproline is a degradation byproduct of newly synthesized collagen in bone and collagens found in other tissues and dietary sources. It is considered as a nonspecific marker of bone turnover due to its low sensitivity and specificity and has been replaced by other assays [17, 18].
-
b.
Hydroxy-pyridinium cross-links of collagen, namely pyridinoline (PYD) and deoxypyridinoline (DPD), are pyridinium compounds formed during the extracellular maturation of fibrillar collagens. These cross-linked collagen compounds are released into the bloodstream upon proteolytic degradation of mature collagen. The urinary excretion of PYD and DPD is unaffected by diet, and they are present in both free form and bound to peptides. The free forms can be measured either through direct immunoassays, such as ELISA on a 24-h sample of urine, or as creatinine-corrected spot urine measurements. Although pyridinium cross-links are considered as reliable indices for evaluating bone resorption, these assays are time-consuming and cumbersome [19].
-
c.
Bone sialoprotein (BSP) is a phosphorylated glycoprotein that constitutes 5–10% of the non-collagenous matrix in bones. It plays a role in the mineralization of newly formed bone matrix and calcification of other tissues. It binds to factor H in the serum, which is involved in the complement pathway. Currently recommended immunoassays can detect only a fraction of the bioavailable BSP. The serum BSP levels primarily reflect processes associated with bone resorption [18, 20].
-
d.
Tartrate-resistant acid phosphatase 5b (TRAP5b), secreted by osteoclasts, is an enzyme that cleaves type 1 collagen during bone resorption. It is typically increased in high bone turnover conditions and reflects increase in number of osteoclasts. Serum TRAP5b activity shows minimal diurnal variation and is not excreted in the urine, hence there is no accumulation of this marker in the blood in hepatic or renal failure. The blood levels are increased in 80% of osteoporosis patients, whereas they decrease by around 40–50% following antiresorptive treatment with bisphosphonate alendronate and estrogen [21].
-
e.
Collagen type 1 cross-linked telopeptide N-terminal (NTx-1) and C-terminal (CTx-1) are degradation products of type I collagen, which forms the major component of bone matrix (90%). These markers are generated by the cathepsin K enzyme activity during bone resorption and are indicators of osteoclast activity [22].
CTx-1, the native CTx, is present in α and β isomerized forms. As the bone ages, the α-aspartic acid within the CTx gets converted to the β-form (β-CTx-1/β-CrossLaps). In the serum CrossLaps assay, only the β-CTx-1 is measured, which is a representation of degraded bone. Urinary CrossLaps assay detects both α- and β-isomers and has shown significant rise in elevated bone turnover conditions and also detectable reaction in healthy individuals. The serum β-CTx-1/β-CrossLaps has been recommended as a reference marker of bone resorption by IOF and International Federation of Clinical Chemistry and Laboratory Medicine (IFCC). The major challenge associated with β-CTx-1/β-CrossLaps measurement is its diurnal variation and variability linked to food intake. Hence, the sample should be collected in fasting state [23]. The serum CTx-1/β-CrossLaps levels return to normal during resorption-inhibiting therapy, therefore, it is recommended for monitoring the efficacy of antiresorptive medications [24, 25].
NTx-1 measurement is done using a monoclonal antibody that targets specific N-terminal epitope. The assay can be performed both in serum and urine samples. It should be noted that urine NTx-1 exhibits greater postprandial variability compared to CTx-1. To avoid the effects of diurnal variation, a 24-h urine collection is required and can be cumbersome [26]. Additionally, urine creatinine levels are needed to report normalized levels of NTx-1.
Factors Affecting Measurement of BTMs
The BTMs’ measurement in the serum and urine is complicated due to the wide biological variability, preanalytical causes, and variations in assay methods and procedures. It is important to understand the variations intrinsic to each marker in order to minimize them where possible. Understanding the sources of variability is necessary for the correct interpretation of the results (Table 3).
Measurement variability In addition to the biologic variability, there can be variability in the measurement of BTMs due to the differences in methods and standardization of the assays across laboratories. The preanalytical technical variations such as type of specimen (serum or urine), whether it is a random 2nd void sample or a 24-h urine, the timing of sample collection, the stability of marker in the collected sample, and the storage conditions will affect the results of the BTMs [32].
Measures to control the variability of BTM assays It is important to maximize the accuracy and precision of assays and control the modifiable variables for the successful use and interpretation of BTMs [33]. The important measures to be followed are listed below:
-
1.
The sample must be collected, processed, and stored following established standardized procedures.
-
2.
A fasting serum sample should be collected in the morning between 7 and 10 a.m. to reduce the variability due to circadian rhythm.
-
3.
In a patient on therapy, it is preferable to collect the sample in the same season, if possible, otherwise account for the variations due to seasonal changes while interpreting the results.
-
4.
Urine collection should also be standardized with a preference for fasting 2nd void sample.
-
5.
Patients should avoid excessive exercise on the day before giving the sample.
-
6.
The sample should be stored properly to avoid deterioration and analyzed within a defined stability period.
-
7.
The sample should preferably be processed in an automated analyzer using standardized procedures.
The results should be interpreted by considering variables such as menstrual cycle and drug history.
The National Bone Health Alliance launched a project in the United States in 2012 with the aim of standardizing BTM sample collection procedures and establishing a reference range for serum BTMs [34].
When monitoring the response to therapy, the changes in BTM values should be clinically significant and large, considering biological and analytical variations. The change in the BTM levels is expressed as the ‘least significant change (LSC)’. The LSC of the BTM is 2.77 times the precision error with a 95% confidence interval. For urinary excretion markers like NTx-1, the decrease should be 50%, and for serum markers such as β-CTx-1/β-CrossLaps, P1NP, and BSAP, the decline should be 30% [3, 13, 35].
The IOF and IFCC recommend the use of P1NP as the reference bone formation marker and β-CTx-1/β-CrossLaps as reference bone resorption marker. These markers should be measured using standardized procedures for assessing fracture risk and therapeutic monitoring [4].
Utility of BTMs
BTMs’ levels are elevated in osteoporosis; however, they are not used for initial diagnosis, which is currently based on clinical and (BMD) evaluation using DEXA. BTM levels are elevated in both primary and also in osteoporosis due to secondary causes and the mechanisms are detailed below (Table 4).
The major applications of measuring BTM levels are [13]:
-
1.
Monitoring patients on therapy for osteoporosis
-
2.
Enhancing patient compliance with therapy
-
3.
Predicting fracture risk
Monitoring Patients on Therapy for Osteoporosis
BTMs show a rapid response to osteoporosis treatment compared to the slow changes seen with DEXA. Hence, they are useful for monitoring treatment outcomes. The response of the BTMs will vary based on the mode of action of the specific osteoporosis therapy. Antiresorptive agents, such as bisphosphonates, cause a rapid reduction in markers of bone resorption, followed by a decrease in bone formation markers [15]. Treatment with anabolic agents, such as recombinant human parathyroid hormone (rhPTH), triggers a rapid elevation in bone formation markers and subsequent increase in markers of bone resorption.
-
1.
Antiresorptive therapy
-
2.
Bisphosphonate therapy
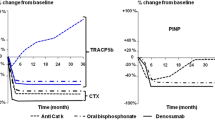
Zoledronate, risedronate, ibandronate, and alendronate are the commonly used drugs for the treatment of osteoporosis. These drugs reduce bone resorption by inhibiting the osteoclasts, increasing BMD, and lowering the risk of vertebral and nonvertebral fractures. When administered at recommended doses, β-CTx-1/β-CrossLaps exhibits a rapid reduction of around 50–80%, with maximum suppression achieved within approximately 2 months. On the other hand, the suppression of P1NP is lesser and reaches its lowest values after approximately 6 months [37]. Clinical studies have shown a correlation between decreased BTM levels and a reduced risk of fractures (vertebral and nonvertebral) following antiresorptive therapy [15, 38, 39].
The changes in the BTM levels may vary based on the type of bisphosphonates used. A study of post-menopausal osteoporotic women showed that treatment with alendronate and ibandronate resulted in greater suppression of β-CTx-1/β-CrossLaps and NTx-I levels compared to risedronate [39, 40]. Recently, the European Calcified Tissue Society Working Group and the IOF have recommended monitoring oral bisphosphonate treatment by measuring serum β-CTX-I and P1NP at baseline and after 3 months. Based on this recommendation, if the reduction in BTM levels is less than the LSC, the clinician should review to identify treatment-related problems such as poor adherence (Fig. 4) [41].

Source: Diez-Perez A, Naylor KE, Abrahamsen B, et al. International Osteoporosis Foundation and European Calcified Tissue Society Working Group. Recommendations for the screening of adherence to oral bisphosphonates. Osteoporos Int. 2017;28(3):767–774
Algorithm for monitoring BTM levels in patients on antiresorptive therapy [42]. . BTM, bone turnover markers; P1NP, procollagen type I amino-terminal propeptide; CTx-1, carboxy-terminal cross-linked telopeptides of type I collagen
If baseline BTM levels have not been assessed before initiating the therapy, the reference interval method should be adopted for clinical evaluation [42, 43].
Bisphosphonates are used for long-term osteoporosis treatment and may rarely have adverse side effects such as atypical femoral fractures and osteonecrosis of the jaw. This has led to the emergence of the ‘drug holiday’ concept. Continuous monitoring is necessary to assess the risk of fracture and to resume the treatment if required. Roberts et al. recommended that an increase of BTMs > 30% during a drug holiday help guide to restart treatment [44].
-
b.
Denosumab
It is a subcutaneously administrated monoclonal antibody that targets RANKL, and is a potent inhibitor of bone resorption. Patients receiving denosumab show a rapid decrease in β-CTx-1/β-CrossLaps within a few days of drug administration. The suppression of serum P1NP and BSAP in response to the treatment is slow and takes approximately 3–6 months to complete.[45]
-
2.
Anabolic agents
-
iii.
Recombinant human parathyroid hormone (rhPTH), teriparatide
Treatment with rhPTH, specifically teriparatide, causes a dose-dependent and rapid elevation in bone formation markers such as P1NP, P1CP, and osteocalcin within days of treatment. This response reaches peak levels after 3 months, with P1NP being the most responsive marker [46]. Subsequently, there is a mild elevation in bone resorption markers.
-
d.
Romosozumab
It is a monoclonal antibody that increases bone formation by binding to sclerostin secreted by osteocytes, an inhibitor of osteoblast activity. Treatment with romosozumab causes a transient elevation in bone formation markers and a consistent reduction in resorption markers. The levels of P1NP start to rise within 1 week, reaching peak values at 4 weeks, and then gradually falls to pretreatment levels over 6 months. Initially, there is a decrease in β-CTx-1/β-CrossLaps and it remains low even at 12 months.[47]
Enhancing patient compliance with therapy
A major challenge with osteoporosis treatment is poor long-term compliance. Monitoring the BTM levels and sharing the data with patients has been shown to improve compliance [44]. The IOF has proposed measuring P1NP or β-CTx-1/β-CrossLaps before the start of therapy and after 3 months to identify patients with poor adherence to treatment or ineffective treatment [48]. For patients who are reluctant to continue treatment for long, higher BTM values compared to premenopausal values can help demonstrate evidence of increased risk of bone loss and fracture, thereby convincing the patient to continue osteoporosis therapy.
Role of BTMs in Predicting Bone Loss and Fracture Risk
BTMs are valuable tools for predicting rates of bone loss in populations [49]. Clinical studies have demonstrated a correlation between elevated BTM levels and higher risk of vertebral and nonvertebral fractures in elderly patients, regardless of BMD [15, 50, 51]. However, a few studies indicate a weak or no correlation between BTM levels and fracture risk prediction [52]. When compared to other BTMs, the bone resorption markers and BSAP show a stronger association with fracture risk. BTMs are helpful for fracture risk prediction over shorter time periods (within a few years) compared to longer periods beyond 10 years. Hence, the value of BTMs is limited in the commonly used long-term fracture risk assessment tools such as Fracture Risk Assessment Tool (FRAX). In view of the limitations of the use of BTMs in long-term fracture risk prediction, the challenges with the test procedures, and the variability in the different BTMs, FRAX Position Development Conference committee has inferred that BTMs should not be used in the FRAX tool [45].
Use of BTMs in Chronic Renal Disease
Various serum and urinary BTM markers, including β-CTX-I/β-CrossLaps, are excreted by the kidneys and are therefore affected by kidney dysfunction. The bone formation markers, BSAP and P1NP, and resorption marker TRAP5b are reliable BTMs in CKD patients. [51, 53,54,55] The CKD-MBD recommendation suggests monitoring serum levels of PTH, phosphate, calcium, and ALP activity from CKD G3a (1C) to G5D, and 25(OH)D may also be used. However, the guidelines do not advocate routine use of BTMs such as P1NP and breakdown telopeptides. In patients with CKD G3a–G5D, assessing serum PTH or BSAP levels can be used to evaluate and predict underlying bone turnover [49, 56].
Conclusion
Laboratory investigations play an important role in osteoporosis. Laboratory tests are not used for the primary diagnosis of osteoporosis; however, they are useful for ruling out secondary causes of osteoporosis. BTMs have emerged as tools for the assessment of osteoporosis. The major challenge in the use of BTMs in osteoporosis is their biological variability and variable analytical performance. Hence, it is important to use standardized procedures on automated analyzers. The IOF has recommended serum P1NP (a bone formation marker) and serum and urinary β-CTx-1/β-CrossLaps (a bone resorption marker) as markers of choice. BTMs are useful in monitoring patients on osteoporosis treatment and predicting bone loss and fracture risk. BTM levels are analyzed before starting treatment and then followed up at regular intervals to monitor the response to therapy. Repeated measurement of these biomarkers improves adherence to treatment and assists in better management of osteoporosis patients.
References
Robbins & Cotran Pathologic Basis of Disease—10th edition [Internet]. https://shop.elsevier.com/books/robbins-and-cotran-pathologic-basis-of-disease/kumar/978-0-323-53113-9. Cited 4 July 2023.
Wheater, G., Elshahaly, M., Tuck, S. P., Datta, H. K., & van Laar, J. M. (2013). The clinical utility of bone marker measurements in osteoporosis. Journal of Translational Medicine, 29(11), 201.
Lee, J., & Vasikaran, S. (2012). Current recommendations for laboratory testing and use of bone turnover markers in management of osteoporosis. Annals of Laboratory Medicine, 32(2), 105–112.
About | International Osteoporosis Foundation [Internet]. https://www.osteoporosis.foundation/health-professionals/about-osteoporosis. Cited 4 July 2023.
Garnero, P. (2008). Biomarkers for osteoporosis management. Molecular Diagnosis & Therapy, 12(3), 157–170.
Bone markers in osteoporosis: bone turnover markers, bone formation markers, bone resorption markers. 2022. https://emedicine.medscape.com/article/128567-overview?icd=login_success_email_match_norm. Cited 4 July 2023.
Day, A. L., Morgan, S. L., & Saag, K. G. (2018). Hypophosphatemia in the setting of metabolic bone disease: Case reports and diagnostic algorithm. Therapeutic Advances in Musculoskeletal Disease., 10(7), 151–156.
Holick, M. F., Binkley, N. C., Bischoff-Ferrari, H. A., Gordon, C. M., Hanley, D. A., Heaney, R. P., et al. (2011). Evaluation, treatment, and prevention of vitamin D deficiency: An Endocrine Society clinical practice guideline. Journal of Clinical Endocrinology and Metabolism, 96(7), 1911–1930.
Carroll, M., Alliston, T., & Dole, N. (2023). The multifaceted effects of osteocytic TGFβ signaling on the skeletal and extraskeletal functions of bone. Current Osteoporosis Reports, 3, 1–2.
Rolighed, L., Rejnmark, L., & Christiansen, P. (2014). Bone involvement in primary hyperparathyroidism and changes after parathyroidectomy. European Journal of Endocrinology, 10(1), 84.
Shaker, J. L. (2009). Paget’s disease of bone: A review of epidemiology, pathophysiology and management. Therapeutic Advances in Musculoskeletal Diseases, 1(2), 107–125.
Ganesan, K., Jandu, J. S., Anastasopoulou, C., Ahsun, S., & Roane, D. (2023). Secondary osteoporosis. In: StatPearls [Internet]. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK470166/. Cited 4 July 2023.
Shetty, S., Kapoor, N., Bondu, J. D., Thomas, N., & Paul, T. V. (2016). Bone turnover markers: Emerging tool in the management of osteoporosis. Indian Journal of Endrocrinology and Metabolism, 20(6), 846.
Barco, C. M., Arija, S. M., & Perez, M. R. (2012). Biochemical markers in osteoporosis: Usefulness in clinical practice. Reumatologia Clinica (English Edition)., 8(3), 149–152.
Vasikaran, S., Eastell, R., Bruyere, O., Foldes, A. J., Garnero, P., Griesmacher, A., et al. (2011). Markers of bone turnover for the prediction of fracture risk and monitoring of osteoporosis treatment: A need for international reference standards. Osteoporosis International, 22(2), 391–420.
Garnero, P., Vergnaud, P., & Hoyle, N. (2008). Evaluation of a fully automated serum assay for total N-terminal propeptide of type I collagen in postmenopausal osteoporosis. Clinical Chemistry, 54(1), 188–196.
Kuo, T. R., & Chen, C. H. (2017). Bone biomarker for the clinical assessment of osteoporosis: Recent developments and future perspectives. Biomark Res., 5(1), 1–9.
Seibel, M. J. (2005). Biochemical markers of bone turnover part I: Biochemistry and variability. Clinical Biochemist Reviews, 26(4), 97.
Halleen, J. M. (2003). Tartrate-resistant acid phosphatase 5B is a specific and sensitive marker of bone resorption. Anticancer Research, 23(2A), 1027–1029.
Habas Sr, E., Eledrisi, M., Khan, F., Elzouki, A. N., Khan, F. Y. (2021). Secondary hyperparathyroidism in chronic kidney disease: pathophysiology and management. Cureus, 13(7).
Tu, K. N., Lie, J. D., Wan, C. K. V., Cameron, M., Austel, A. G., Nguyen, J. K., et al. (2018). Osteoporosis: a review of treatment options. P T., 43(2), 92–104.
Qvist, P., Christgau, S., Pedersen, B. J., Schlemmer, A., & Christiansen, C. (2002). Circadian variation in the serum concentration of C-terminal telopeptide of type I collagen (serum CTx): Effects of gender, age, menopausal status, posture, daylight, serum cortisol, and fasting. Bone, 31(1), 57–61.
Ravn, P., Clemmesen, B., Riis, B. J., & Christiansen, C. (1996). The effect on bone mass and bone markers of different doses of ibandronate: A new bisphosphonate for prevention and treatment of postmenopausal osteoporosis: A 1-year, randomized, double-blind, placebo-controlled dose-finding study. Bone, 19(5), 527–533.
Rosenquist, C., Fledelius, C., Christgau, S., Pedersen, B. J., Bonde, M., Qvist, P., et al. (1998). Serum CrossLaps One Step ELISA. First application of monoclonal antibodies for measurement in serum of bone-related degradation products from C-terminal telopeptides of type I collagen. Clinical Chemistry, 44(11), 2281–2289.
Baxter, I., Rogers, A., Eastell, R., & Peel, N. (2013). Evaluation of urinary N-telopeptide of type I collagen measurements in the management of osteoporosis in clinical practice. Osteoporosis International, 24(3), 941–947.
Corder, C. J., Rathi, B. M., Sharif, S., & Leslie, S. W. (2023). (24-hour urine collection. In: StatPearls [Internet]. StatPearls Publishing. http://www.ncbi.nlm.nih.gov/books/NBK482482/. Cited 4 July 2023.
Lorentzon, M., Branco, J., Brandi, M. L., Bruyère, O., Chapurlat, R., Cooper, C., Cortet, B., Diez-Perez, A., Ferrari, S., Gasparik, A., & Herrmann, M. (2019). Algorithm for the use of biochemical markers of bone turnover in the diagnosis, assessment and follow-up of treatment for osteoporosis. Advances in Therapy, 36, 2811–2824.
Marini, S., Barone, G., Masini, A., Dallolio, L., Bragonzoni, L., Longobucco, Y., & Maffei, F. (2020). The effect of physical activity on bone biomarkers in people with osteoporosis: A systematic review. Frontiers in Endocrinology, 23(11), 585689.
Schlemmer, A., Hassager, C., Risteli, J., Risteli, L., Jensen, S. B., & Christiansen, C. (1993). Possible variation in bone resorption during the normal menstrual cycle. European Journal of Endocrinology, 129(5), 388–392.
Scharla, S. H., Scheidt-Nave, C., Leidig, G., Woitge, H., Wuster, C., Seibel, M. J., et al. (1996). Lower serum 1-hydroxyvitamin D is associated with increased bone resorption markers and lower bone density at the proximal femur in normal females: A population-based study. Experimental and Clinical Endocrinology & Diabetes, 104(3), 289–292.
Brown, J. P., Malaval, L., Chapuy, M. C., Delmas, P. D., Edouard, C., & Meunier, P. J. (1984). Serum bone Gla-protein: A specific marker for bone formation in postmenopausal osteoporosis. Lancet, 323(8386), 1091–1093.
Delanghe, J., & Speeckaert, M. (2014). Preanalytical requirements of urinalysis. Biochemia Medica., 24(1), 89–104.
Afzal, A., Samee, A. M., Jilte, R. D., Islam, M. T., Manokar, A. M., & Razak, K. A. (2021). Battery thermal management: An optimization study of parallelized conjugate numerical analysis using Cuckoo search and Artificial bee colony algorithm. International Journal of Heat and Mass Transfer., 1(166), 120798.
Szulc, P., Naylor, K., Hoyle, N. R., Eastell, R., & Leary, E. T. (2017). National Bone Health Alliance Bone Turnover Marker Project. Use of CTX-I and PINP as bone turnover markers: National Bone Health Alliance recommendations to standardize sample handling and patient preparation to reduce pre-analytical variability. Osteoporosis International, 28(9), 2541–2556.
Rosen, H. N., Moses, A. C., Garber, J., Ross, D. S., Lee, S. L., & Greenspan, S. L. (1998). Utility of biochemical markers of bone turnover in the follow-up of patients treated with bisphosphonates. Calcified Tissue International, 63, 363–368.
Sheu, A., & Diamond, T. (2016). Secondary osteoporosis. Australian Prescriber, 39(3), 85.
Glover, S. J., Eastell, R., McCloskey, E. V., Rogers, A., Garnero, P., Lowery, J., et al. (2009). Rapid and robust response of biochemical markers of bone formation to teriparatide therapy. Bone, 45(6), 1053–1058.
Bauer, D. C., Black, D. M., Garnero, P., Hochberg, M., Ott, S., Orloff, J., et al. (2004). Fracture Intervention Trial Study Group. Change in bone turnover and hip, non-spine, and vertebral fracture in alendronate-treated women: the fracture intervention trial. Journal of Bone and Mineral Research, 19(8), 1250–1258.
Naylor, K. E., Jacques, R. M., Paggiosi, M., Gossiel, F., Peel, N. F., McCloskey, E. V., et al. (2016). Response of bone turnover markers to three oral bisphosphonate therapies in postmenopausal osteoporosis: The TRIO study. Osteoporosis International, 27(1), 21–31.
Sobh, M. M., Abdalbary, M., Elnagar, S., Nagy, E., Elshabrawy, N., Abdelsalam, M., et al. (2022). Secondary osteoporosis and metabolic bone diseases. Journal of Clinical Medicine, 11(9), 2382.
Jorgensen, H. S., Behets, G., Viaene, L., Bammens, B., Claes, K., Meijers, B., et al. (2022). Diagnostic accuracy of noninvasive bone turnover markers in renal osteodystrophy. American Journal of Kidney Diseases, 79(5), 667–676.
Diez-Perez, A., Naylor, K. E., Abrahamsen, B., Agnusdei, D., Brandi, M. L., Cooper, C., et al. (2017). International osteoporosis foundation and european calcified tissue society working group. Recommendations for the screening of adherence to oral bisphosphonates. Osteoporosis International, 28(3), 767–847.
Park, S. Y., Ahn, S. H., Yoo, J. I., Chung, Y. J., Jeon, Y. K., Yoon, B. H., et al. (2019). Position statement on the use of bone turnover markers for osteoporosis treatment. Journal of Bone Metabolism, 26(4), 213–224.
Crandall, C. J., Vasan, S., LaCroix, A., LeBoff, M. S., Cauley, J. A., Robbins, J. A., et al. (2018). Bone turnover markers are not associated with hip fracture risk: A case-control study in the Women’s Health Initiative. Journal of Bone and Mineral Research, 33(7), 1199–1208.
Ivaska, K. K., Gerdhem, P., Vaananen, H. K., Akesson, K., & Obrant, K. J. (2010). Bone turnover markers and prediction of fracture: A prospective follow-up study of 1040 elderly women for a mean of 9 years. Journal of Bone and Mineral Research, 25(2), 393–403.
Shiraki, M., Sugimoto, T., & Nakamura, T. (2013). Effects of a single injection of teriparatide on bone turnover markers in postmenopausal women. Osteoporosis International, 24, 219–226.
Lorentzon, M., Branco, J., Brandi, M. L., Bruyère, O., Chapurlat, R., Cooper, C., et al. (2019). Algorithm for the use of biochemical markers of bone turnover in the diagnosis, assessment and follow-up of treatment for osteoporosis. Advances in Therapy, 36(10), 2811–2824.
Garnero, P., Sornay-Rendu, E., Claustrat, B., & Delmas, P. D. (2000). Biochemical markers of bone turnover endogenous hormones and the risk of fractures in postmenopausal women: The OFELY study. Journal of Bone and Mineral Research, 15(8), 1526–1536.
Bauer, D. C., Garnero, P., Harrison, S. L., Cauley, J. A., Eastell, R., Ensrud, K. E., et al. (2009). Biochemical markers of bone turnover, hip bone loss, and fracture in older men: The MrOS study. Journal of Bone and Mineral Research, 24(12), 2032–2038.
Ross, P. D., Kress, B. C., Parson, R. E., Wasnich, R. D., Armour, K. A., & Mizrahi, I. A. (2000). Serum bone alkaline phosphatase and calcaneus bone density predict fractures: A prospective study. Osteoporosis International, 11(1), 76–82.
Garnero, P., Hausherr, E., Chapuy, M. C., Marcelli, C., Grandjean, H., Muller, C., et al. (1996). Markers of bone resorption predict hip fracture in elderly women: The EPIDOS Prospective Study. Journal of Bone and Mineral Research, 11(10), 1531–1538.
McClung, M. R., Grauer, A., Boonen, S., Bolognese, M. A., Brown, J. P., Diez-Perez, A., et al. (2014). Romosozumab in postmenopausal women with low bone mineral density. New England Journal of Medicine, 370(5), 412–420.
Eastell, R., Christiansen, C., Grauer, A., Kutilek, S., Libanati, C., McClung, M. R., et al. (2011). Effects of denosumab on bone turnover markers in postmenopausal osteoporosis. Journal of Bone and Mineral Research, 26(3), 530–537.
Marques, E. A., Gudnason, V., Lang, T., Sigurdsson, G., Sigurdsson, S., Aspelund, T., et al. (2016). Association of bone turnover markers with volumetric bone loss, periosteal apposition, and fracture risk in older men and women: The AGES-Reykjavik longitudinal study. Osteoporosis International, 27(12), 3485–3494.
Ojeda-Bruno, S., Naranjo, A., Francisco-Hernandez, F., Erausquin, C., Rua-Figueroa, I., Quevedo, J. C., et al. (2011). Secondary prevention program for osteoporotic fractures and long-term adherence to bisphosphonates. Osteoporosis International, 22(6), 1821–1828.
Roberts, J., Castro, C., Moore, A. E., Fogelman, I., & Hampson, G. (2016). Changes in bone mineral density and bone turnover in patients on ‘drug holiday’following bisphosphonate therapy: Real-life clinic setting. Clinical Endocrinology, 84(4), 509–515.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard statement
This article does not contain any studies with human or animal subjects performed by the any of the authors.
Informed consent
For this type of study, informed consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Panchagnula, R., Amarnath, S.S. Osteoporosis: Investigations and Monitoring. JOIO 57 (Suppl 1), 70–81 (2023). https://doi.org/10.1007/s43465-023-01019-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43465-023-01019-w